Preceptorship Journal 2
Diunggah oleh
api-3544166500 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
32 tayangan3 halamanJudul Asli
preceptorship journal 2
Hak Cipta
© © All Rights Reserved
Format Tersedia
DOCX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
32 tayangan3 halamanPreceptorship Journal 2
Diunggah oleh
api-354416650Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 3
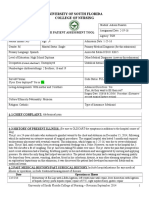
Reflective Journaling #2
Adison Pusateri March 31, 2017
Noticing
Subjective and objective data
o The patient was admitted to the burn ICU for a 16% TBSA
flash burn that occurred while he was smoking a cigarette
while on supplemental oxygen. Pertinent medical history of
the patient includes severe multiple sclerosis, requiring the
patient to have a tracheostomy. His tracheostomy cuff was
deflated, and he was on 10L of oxygen and 40% FiO2. I
cared for this patient on his first day out of the ICU on the
step-down unit.
How did you know there was a problem? Abnormal
patient presentation or your gut feeling?
o From the start of shift until approximately 10:00, the
patient required suctioning of his tracheostomy multiple
times an hour to deal with the copious amount of clear,
thick secretions he was producing. The patient was NPO for
a scheduled procedure to place a peg tube, so instead of
administering medications to help decrease the secretions,
respiratory was called to perform a nebulizer treatment.
The treatment did not greatly improve his condition, and
about an hour after the respiratory therapist left the
patients SpO2 began desatting.
Interpreting
What other information do I need to make a decision? Is
there anyone else I need to involve or notify? What could
be happening and how critical is this situation?
o After the respiratory treatment had failed to alleviate the
problem, my preceptor and I decided it necessary to
contact the department in which the patient was to have
his Peg tube placed in order to get an estimate on when
they would be taking him for the procedure. We were told
there were three patients ahead of him, so we had a
considerable amount of time. Because of this, we decided
to administer Guafenesin via dobhoff tube in order to help
the patient clear his secretions.
Responding
Should I do something now or wait and watch? How will I
know if I am making the best decision? What
interventions can I delegate to other members of the
healthcare team? Include evidence-based practice (peer
reviewed) to justify why you might make one decision
over another.
o After administering both a nebulizer treatment and a
medication to help thin the patients secretions there was
still no improvement. It was at this time we called for the
respiratory therapist to come up and assess the patient
again, along with the plastics team who was following him.
The plastics team ordered a chest X-ray, which showed
infiltrates in the lower lobe of the patients left lung. It was
with this information that the respiratory therapist and MD
came to the conclusion that, because the patients cuff was
deflated, he was aspirating his own saliva. Therefore, the
respiratory therapist inflated the cuff and bumped the
patients oxygen to 50% FiO2. When inflated, a cuff, or
balloon, in a tracheostomy prevents administered oxygen
from escaping in order to allow it to reach the lower lobes
of the lungs, while simultaneously preventing aspiration
(Weiss & Denman, 2010). The patients condition improved
greatly after this, however, it was concerning because 50%
FiO2 is the highest a patient is allowed to go on oxygen
without being in an ICU (per TGH protocol). Therefore, even
though the patients condition had stabilized, the care team
decided it safest to transfer the patient back to an ICU in
case his oxygen requirement further increased.
Reflecting
Did I make the right decision? Did I achieve the desired
outcome? What did I do really well? What could I have
done better?
o I believe that my preceptor and I did the right thing by
utilizing respiratory therapy and the patients care team in
making a plan for this patient, as the problem fell in their
realm of expertise. I also believe that the care team made
the right decision by moving the patient back into an ICU,
as he was not in a code bed on the step down unit and,
had he decompensated more later on, there would have
been nothing different that could be done in the
environment he was in. The decision to move him back into
an ICU was by far the safest.
Works Cited
Weiss, M. & Denman, W. (2010). Patent No. US7686019 B2. IFI Claims
Patent
Services.
Anda mungkin juga menyukai
- Community Health Capstone Paper-1Dokumen15 halamanCommunity Health Capstone Paper-1api-354416650Belum ada peringkat
- ms1 PatDokumen23 halamanms1 Patapi-354416650Belum ada peringkat
- Synthesis Paper SummativeDokumen13 halamanSynthesis Paper Summativeapi-354416650Belum ada peringkat
- Quality Care Movement PresentationDokumen9 halamanQuality Care Movement Presentationapi-354416650Belum ada peringkat
- Resume Adison PusateriDokumen2 halamanResume Adison Pusateriapi-354416650Belum ada peringkat
- ms2 PatDokumen23 halamanms2 Patapi-354416650Belum ada peringkat
- Fund NPWDokumen1 halamanFund NPWapi-354416650Belum ada peringkat
- Cover Letter MicuDokumen1 halamanCover Letter Micuapi-354416650Belum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Chapter-4 PHPDokumen9 halamanChapter-4 PHPgamingw470Belum ada peringkat
- Práctica 5 Curva Dosis-Respuesta Cuantal: Escuela Superior de MedicinaDokumen5 halamanPráctica 5 Curva Dosis-Respuesta Cuantal: Escuela Superior de MedicinaOsvaldoBelum ada peringkat
- Ultimate Pre-Reg BNF NotesDokumen29 halamanUltimate Pre-Reg BNF NotesBob100% (7)
- Unit 3, Novel Drug Delivery Systems, B Pharmacy 7th Sem, Carewell PharmaDokumen33 halamanUnit 3, Novel Drug Delivery Systems, B Pharmacy 7th Sem, Carewell Pharmaayush pathak100% (1)
- Cambodia Requirement SPCDokumen3 halamanCambodia Requirement SPCAfaz UddinBelum ada peringkat
- Best Evidence-Based Practices To Treat Intravenous InfiltrationDokumen1 halamanBest Evidence-Based Practices To Treat Intravenous InfiltrationSasha Hidayat FullBelum ada peringkat
- Tabel Zona Sensitivitas Antibiotik: 1. Enterobactericeae (Klebsiella SP., E.coli, Proteus SP.,)Dokumen7 halamanTabel Zona Sensitivitas Antibiotik: 1. Enterobactericeae (Klebsiella SP., E.coli, Proteus SP.,)puriartini-1Belum ada peringkat
- Final - Hospital Bill FormatDokumen2 halamanFinal - Hospital Bill FormatH C50% (2)
- Pharmacovigilance and RMPDokumen15 halamanPharmacovigilance and RMPЗухра ИбрагимоваBelum ada peringkat
- Endotracheal Intubation: A Step-by-Step GuideDokumen28 halamanEndotracheal Intubation: A Step-by-Step Guidejeevan ghimireBelum ada peringkat
- DAFTAR OBAT APOTEK ARBAIDokumen5 halamanDAFTAR OBAT APOTEK ARBAIika dian savitriBelum ada peringkat
- Hamdard Medicine List 2019Dokumen4 halamanHamdard Medicine List 2019DrRaghvendra Kumar SinghBelum ada peringkat
- English Medication and Medical Equipment GlossaryDokumen7 halamanEnglish Medication and Medical Equipment GlossaryVeronicaGelfgrenBelum ada peringkat
- Respiratory System DrugsDokumen4 halamanRespiratory System DrugsArienne Janine MalabananBelum ada peringkat
- Hydralazine 1Dokumen3 halamanHydralazine 1BrittanyBelum ada peringkat
- Dosage Form ExamDokumen9 halamanDosage Form ExamsongaBelum ada peringkat
- Lassaletta A, Cancer Reports, 2022, E1729, Asparaginase Activity Monitoring in Pediatric Acute Lymphoblastic Leukemia ADokumen8 halamanLassaletta A, Cancer Reports, 2022, E1729, Asparaginase Activity Monitoring in Pediatric Acute Lymphoblastic Leukemia AgemaBelum ada peringkat
- Borang CP2 (Hospital Manual)Dokumen2 halamanBorang CP2 (Hospital Manual)William TanBelum ada peringkat
- Introduction To Pharma LecDokumen22 halamanIntroduction To Pharma LecFrancis Polycarp DiazBelum ada peringkat
- Biopharmaceutics and Pharmacokinetics - A Treatise - Brahmankar, Jaiswal - Pharma Dost PDFDokumen206 halamanBiopharmaceutics and Pharmacokinetics - A Treatise - Brahmankar, Jaiswal - Pharma Dost PDFSiddhi Rao100% (1)
- Risk Management in PVDokumen40 halamanRisk Management in PVSutirtho Mukherji100% (1)
- Flupentixol Drug StudyDokumen3 halamanFlupentixol Drug StudyEmJay Balansag0% (1)
- Vildagliptin A New Oral Treatment For Type 2Dokumen12 halamanVildagliptin A New Oral Treatment For Type 2Andhi Fahrurroji100% (1)
- Poveda, V de B Doc 31eDokumen7 halamanPoveda, V de B Doc 31eThiago DiasBelum ada peringkat
- Christian Medical College Antimicrobial Therapy GuidelinesDokumen43 halamanChristian Medical College Antimicrobial Therapy Guidelinesharshita guglaniBelum ada peringkat
- Pacop Violet Module 4Dokumen122 halamanPacop Violet Module 4metBelum ada peringkat
- CSSC, SerembanDokumen2 halamanCSSC, SerembanKatthiraavan ThiruvengadamBelum ada peringkat
- Bisphosphonates 2014 11Dokumen75 halamanBisphosphonates 2014 11Ako KareemBelum ada peringkat
- Perbekalan Farmasi RekapDokumen556 halamanPerbekalan Farmasi RekapChelseaBelum ada peringkat
- Nonbinary HormonesDokumen9 halamanNonbinary HormonesBiniam GrafféBelum ada peringkat