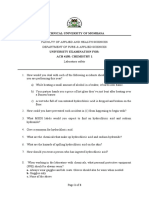
Anti Infectives 1
Diunggah oleh
Wenn Joyrenz ManeclangHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Anti Infectives 1
Diunggah oleh
Wenn Joyrenz ManeclangHak Cipta:
Format Tersedia
WJM 2NUR-6
The Cell Mechanism of action:
- Basic structural unit of the body Interfere with bacterial wall synthesis
- Make up living organisms which are arranged into Penicillins, Cephalosporins, Carbapenams,
tissues & organs, all have same basic structure Vancomycin (pp 402)
*safe enough to protect the body but lethal to Prevention of utilizing substances essential for
kill the bacteria growth & development
Cell Membrane - Sulfonamides, Antimycobacterials (TB meds)
- Is a lipoprotein structure that separates the interior & trimethoprim
of a cell from the external environment; regulates *Amoxicillin comes from the group of penicillin
what can enter & leave a cell (not wide selective toxicity)
- Lipoprotein * Vancomycin - broad spectrum
Allows cytoplasm to remain intact Interfere with protein synthesis
Polar regions = mix well with water - Macrolides, chloramphenicol, tetracyclines,
Non-polar regions = repel water aminoglycosides
Receptor Sites Interfere with DNA synthesis
- Reacts with specific chemicals outside the cell - Fluoroquinolones, antimycobacterium
- Identifying markers Alter cell membrane permeability
- Histocompatibility antigens or Human Leukocyte - Antifungal and antiprotozoal
Antigen
Identifies a cell as self cell TERMS
Can be classified through several ways; Treatment to prevent an infection
cell injury; viral invasion; age, etc. before it occurs, as in the use of
Channels Prophylaxis antibiotics to prevent a disease
- Pores within the cell membrane made by the protein (given 30-45 min before a procedure
in the cell wall for passage of small substances or days before a procedure)
Cell Cycle Range of bacteria against which an
antibiotic is effective (e.g. broad-
G0 Resting Phase Spectrum
spectrum antibiotics are effective
G1 Stimulation of DNA Formation against a wide range of bacteria)
S Phase Energy Consuming Activities, Synthesis Ability of bacteria over time to adapt
of DNA to an antibiotic produce cells that are
G2 DNA has doubled no longer affected by the drug
M Phase Mitosis, Splits to 2 daughter cells Resistance Example: If you are given Amoxicillin
whenever you have fever, they will
ANTI- INFECTIVE AGENTS give you Co-amoxiclav (amoxicillin +
Drug that are designed to act selectively on foreign clavulanic acid)
organisms that have invaded and infected the body HOW ORGANISMS DEVELOP RESISTANCE
of a human host Producing an enzyme that deactivates an
With selective toxicity antimicrobial agents
*Some anti-infectives are compatible with gram (+)
Changing cellular permeability to prevent the drug
or gram (-)
from entering the cell or altering transport systems
*Antibiotic that affects only aerobic; anaerobic
Agents found on mold samples are the first sources Altering binding sites on the membranes or
of anti-infective agents ribosomes which then no longer accept the drugs
Producing chemicals that act as antagonist to the
drug
WJM 2NUR-6
TREATMENT OF SYSTEMIC INFECTIVES DEFINITIONS
Identification of the pathogen Chemical that is able to inhibit
- Culture the growth of specific bacteria or
Sample of the bacteria to grow in a cause the death of susceptible
bacteria
laboratory to determine the species of Antibiotic
Agents derived from other living
bacteria that is causing an infection microorganisms
Sensitivity of the pathogen *some antibiotic may kill the
- Sensitivity testing infection or only stop or prevent
Evaluation of bacteria obtained in a culture Substance that causes the death
to determine to which antibiotic the of bacteria, usually by interfering
with cell membrane stability or
organisms are sensitive and which agent Bactericidal
proteins or enzyme necessary to
would be appropriate for treatment of a
maintain the cellular integrity of
particular infection the bacteria
Substance that prevents the
replication of bacteria, usually by
Bacteriostatic interfering with proteins or
enzyme systems necessary for
reproduction
Beta Lactam Ring
Beta Lactamase BACTERIA
e.g. Clavulanic
Beta Lactamase Inhibitor
acid Aerobic
Combination Therapy - Bacteria that depend on oxygen for survival
- Use smaller doses of the drugs (because these drugs Anaerobic
have side effects & adverse effects; to prevent - Survive without oxygen
severe side effects and adverse effects from - Seen when blood flow is cut off to an area of the
occurring) body
- Synergism (if given at the same time, increases Gram negative (-)
mechanism of action) - GI & GU
- Many microbial infection usually caused by more - Negative stain
than one microorganism Gram positive (+)
- Delay the emergence of resistant strain - Positive stain
- Respiratory and soft tissues
ADVERSE REACTIONS TO ANTI-INFECTIVE THERAPY
PREVENTING THE DEVELOPMENT OF RESISTANCE
Kidney Disease
GI Toxicity Identify bacteria
Neurotoxicity Correct drug use
Hypersensitivity reactions Full course of therapy
Superinfections Avoid inappropriate use
Resistant to almost all drugs
WJM 2NUR-6
PENICILLINS Adverse Rxns:
Bactericidal GI upset
Gram (+) - Glossitis, stomatitis, sore mouth, N/V
Inhibit cell wall synthesis - Diarrhea
Also called Beta lactams Allergy (most common)
Thrombophlebitis
Common Drugs
Anaphylaxis
Penicillins
Thrombocytopenia & Leukopenia
pen G
pen V If patients have allergic rxns to
Azithromycin penicillin; Allergic reaction to
Extended Spectrum Penicillin
Erythromycin penicillin = allergic rxn to
carbenicillin (Geocillin)
cephalosporin
amoxicillin (Amoxil, Himox)
ticarcillin (Ticar) DRUG INTERACTIONS OF PENICILLIN
ampicillin (Pensyn) Increased plasma concentration
Penicillinase Resistant Antibiotics - Whe n combined with Probenecid
dicloxacillin Decreased secretion of Methotrexate
oxacillin (Prostaphillin) Tetracycline & Chloramphenicol
natcillin - Decreases penicillin action
Bacteria produce enzymes capable of destroying Decreases effectiveness of hormonal contraceptives
penicillins called penicillinase or beta-lactamase Aminoglycosides
As a result, the medication is not effective Dont give oral medications with fruit juices
Chemicals have been developed to inhibit these
enzymes AMINOGLYCOSIDES
- Clavulanic acid Bactericidal inhibits protein synthesis
- Tazobactam Used to kill gram (-) bacteria such as
- Sulbactam Pseudomonas spp, E.coli, Proteus spp, Klebsiella
These chemicals bind with beta-lactamase and spp, Serratia spp
prevent the enzyme from breaking down the Effective with gram (-)
penicillin Nosocomial infections, UTI, CNS & eye
Amoxicillin infections
No effect with food
Bacapicillin Often used in combination with other antibiotics
- Given 1hour before or 2hours after or vise versa for synergistic effect
PENICILLIN-BETA-LACTAMASE INHIBITOR COMBINATION Absorbed poorly in the GI tract
DRUGS - Usually given IV
- Serious side effects and adverse effects
Ampicillin + sulbactam = Unasyn GANTS (Common Drugs)
Amoxicillin + clavulanic acid = Augmentin Gentamycin (Servigenta, Garamycin)
Ticarcillin + clavulanic acid = Timentin Amikacin (Amikin)
Neomycin (Maxitrol, Terramycin)
Piperacillin + tazobactam = Zosyn
Tobramycin (Tobrex)
Streptomycin
Kanamycin
WJM 2NUR-6
DRUG INTERACTIONS
FLUOROQUINOLONES
Anesthetics, Muscle Relaxants
Diuretics Bactericidal & Bacteriostatic
Other antibiotics Effective against gram (-)
UTI, Respiratory, Dermatological, eye, ear, bone
Adverse Effects
& joint infection, after anthrax, typhoid fever
Neurotoxicity
Ototoxicity Adverse effects
Risk for Nephropathy
Headache, dizziness
Cardiac effects
Bone marrow depression GI upset
- blood levels Photosensitivity
GI irritation Common Drugs (CLONG)
Ciprofloxaxin (Ciprobay)
CEPHALOSPORINS
Levofloxacin (Levox, Floxel)
Semisynthetic derivations from a fungus
Ofloxacin
Structurally and pharmacologically related to
penicillins Drug Interactions
Bactericidal & bacteriostatic theophylline level
- Inhibits cell wall synthesis Cardiac dysrhythmias (procainamide, quindine,
Broad spectrum amiodarone, tricyclic)
Divided into groups according to their NSAIDs increased risk of CNS stimulation
antimicrobial activity
Numerous sensitive bacteria MACROLIDES
- Respiratory, dermatological, middle ear infection Bactericidal or Bacteriostatic
(page 409 highlight table 29-4) - Binds to cell membrane to change protein function
*Cephalosporins are better than penicillins because in RNA synthesis
it is divided into 4 generations Effective against many sensitive organisms &
intestinal amoebiasis
ADVERSE REACTIONS Usually enteric coated
GI N/V, Diarrhea (pronounced)
CNS headache, dizziness Common Drugs (DACE)
Hypoprothrombinemia dirithromycin (Dynabac)
Phlebitis azithromycin (Zithromax)
DRUG INTERACTIONS clarithromycin (Klaricid)
Aminoglycosides erythromycin (Ilosone, Erythrocin, Erycin)
Alcohol *duodenum = site of absorption; GI upset (p445)
COMMON DRUGS Adverse effect
1st Gen Cephalosporin (Ceporex, Keflex), cefazolin (severe) GI upset N/V, GI irritation, abnormal taste
(Ancef) Thrombophlebitis
These Drugs Can Interact
2nd Gen cefaclor (Ceclor), cefoxitin (mefoxin) Fever, anaphylaxis
- Theophylline
3rd Gen cefotaxime (Rocephin) Various resistant salt
- Digoxin
4th Gen cefeprime (Cepimax) *pp416 = eryhthromycin ethylsuccinate - Coumadin
= erythrocin sterase
WJM 2NUR-6
LINCOSAMIDES Peptides (Polymyxin B)
Inhibits bacterial protein synthesis - Uses a surfactant like reaction to penetrate
Similar to macrolides in terms of coverage bacterial cell wall
Associated with severe toxicity - Can be toxic to human host
Drugs - Neurotoxicity
o clindamycin (Dalacine) - seen in association facial flushing, dizziness, ataxia, paresthesia
with severe GI upset; seen in Derma clinics Paresthesia is the tingling of extremities
o lincomycin (Lincocin) - Nephrotoxicity
Careful monitoring Watch out for creatinine & kidney
Stop once bloody diarrhea occurs function
Monobactam Antibiotic SULFONAMIDES
- Bactericidal Bactericidal
- Effective against gram (-) enterobacteria o Blocks para amino benzoic acid to inhibit
- Caution use for patients allergic to folic acid synthesis
penicillins/Cephalosporins Effective against gram (-) & gram (+) bacteria
- aztreonam (Azactam) and many resistant strains
Adverse Reactions: Common drugs
Local GI effects o cotrimoxazole (Bactrim, Septra)
Elevated liver enzymes For UTI
Inflammation o sulfadiozine (Flammazine)
Vancomycin Sulfonylurea (glyboride, glypizide) OHA
- Used to treat methicillin-resistant S. Aureus Cyclosporine - increased risk of nephrotoxicity
(MRSA) Nephrotoxicity lowers kidney function,
- With high incidence of vancomycin resistant creatinine, BUN
therefore should be used when C&S confirms Nursing Consideration: increase fluid intake
need for it Watch out for photosensitivity
Adverse Reactions Crystalluria
Renal failure, ototoxicity, supeinfections Caution on its use during
Red man syndrome
Pregnancy - cause birth defects, kernicterus
sudden & severe hypotension, fever, chills,
Lactation - kernicterus & diarrhea
paresthesia & erythema of the neck & back
Kidney disorders
Nursing Consideration: infuse slowly
Adverse Effects
Chloramphenicol
GI disturbance increases hepatic injury
- Prevents bacterial cell wall division
Renal - crystalluria, hematuria, proteinuria
- Common treatment for typhoid fever Prevent proteinuria by increasing fluid
- Gray Syndrome - abdominal distention, cyanosis, intake not less than 2L/day
vasomotor collapse, irregular respiration and CNS
even death Dermatologic
- Bone marrow depression - aplastic anemia Bone marrow suppression
WJM 2NUR-6
TETRACYCLINES Adverse Reactions
Natural & semi-synthetic N/V, diarrhea, fatal pseudomembranous colitis
Obtained from cultures of streptomycin Hypersensitivity reactions
Bacteriostatic Confusion & seizure
o Inhibit protein synthesis Common drugs
Effective against wide range of bacteria
imipinem - cilastatin (Tienam)
Acne treatment
meropenem (Meronem)
Absorption affected by food; calcium & iron
ertapenem (Invanz)
Caution use on:
o Pregnant women
ANTIMYCOBACTERIALS
o Children under 8 yrs old ( cause retarded
Mycobacteria - group of microorganisms that
skeletal development & teratogenic effect)
has the ability to hold a stain (acid fast bacilli) in
Discoloration of permanent teeth (green &
yellow patches on teeth)
the presence of
Fetal-skeletal development & retardation Destaining - termed as acid fast bacilli
Drug to food interaction a. M.tuberculosis
High affinity to Calcium, Aluminum, b. M.leprae
Magnesium & Irons c. M.avium-intracellulare
Don't use on food with high Calcium, Bactericidal
aluminum, magnesium, and iron Long term therapy (6 months - 2 years)
Short term use only RIPES
Adverse Effects Antituberculosis Drugs & Common Side Effects
GI disturbances o affects mycoloic acid coating
Give yakult Ioniazid (INH) - Peripheral Neuropathies,
Alteration in intestinal flora may result in Gynecomastia
o Superinfection (Overgrowth of nonsusceptible o alters DNA & RNA activity
organisms such as Candida) Don't use contact lenses
o Diarrhea Rifampicin
because it produces orange-
o Pseudomembranous colitis colored output
Fetal hepatotoxicity o inhibits cellular metabolism
Skeletal effects Ethambutol
- Optic neuritis
Photosensitivity & rash Pyrazinamide o Bactericidal & Bacteriostatic
Steven Johnson Syndrome o Nephrotoxicity
o Scaling of skin (all over the body) Antituberculosis drugs -
Drug Interactions causes patients to always
Penicillin G Streptomycin
feel sleepy; usually during
Oral contraceptives afternoon they are already
Digoxin tired
Ca, Mg, Al, Bi, Fe salts - ototoxicity
Anti-Leprosy
Common Drugs: DOM-T
o Inhibits folate synthesis
doxycycline (Doxin) Dapsone
o Used to treat P.carinii pneumonia
oxytetracycline (Terramycin)
on AIDS client
minocycline (Minocin)
Clofazimone o Binds to bacterial DNA sites &
tetracycline
(Lamprene) causes cell death
o Treatment of erythema nodosum
CARBAPENEMS
leprosum
Bactericidal - inhibit cell wall synthesis
o Caution use for pregnant women
Broad spectrum and used for serious life Thalidomide
Babies with no hands or feet
threatening gram (+) & gram (-) infections No leprosy cases now
because there's treatment
WJM 2NUR-6
Interactions
Drug - Drug
o Rifampicin & INH - liver toxicity
o Increased metabolism of drugs when given with
quinidine, metoprolol, oral contraceptives, oral
antidiabetic agents, ketoconazole
Drug - Food
o Take combination of anti-TB early am with an
empty stomach
Nursing Considerations on Antibiotic Therapy
Check for allergies, HX
Assessment
Upset on GI
o Take with full glass of water if not tolerated,
small frequent feedings & mouth care
Small/light meals/snack
All antibiotics cause GI upset but it should be
given on an empty stomach because food limited
the absorptive effect of GI mucosa
Site of absorption = duodenum
Variant resistant salts are added to vancomycin
(macrolides). They protect erythromycin from
being broken down or metabolizer and protects
patient from severe GI upset
Variant salts - page 416
Teachings
o Take full course of medication
If you forgot, adjust the dose and take meds
ASAP then back to the original time where you
should take the meds
o Use full course
o Use Barrier contraceptives
Increase fluid intake specific for sulfonamides
because it causes crystalluria and hematuria
Interactions
Digoxin, Theophylline, Coumarin, Synergism
Food, milk (Tetracycline)
Macrolides, penicillin, sulfonamides & Tetracyclines
should be given 1h before meals
Others
Prepare for any allergic reactions
Note: Labs, Normal results, Pregnancy & Lactation
Rifampicin - orange output
Special Consideration
o Refrigerate IV solutions after reconstitution
o Administe Co-amoxiclav immediately (within 30
mins)
Anda mungkin juga menyukai
- Health HX Taking - 20180821202221 PDFDokumen5 halamanHealth HX Taking - 20180821202221 PDFWenn Joyrenz ManeclangBelum ada peringkat
- Wenn HemaDokumen63 halamanWenn HemaWenn Joyrenz ManeclangBelum ada peringkat
- Health HX Taking - 20180821202221 PDFDokumen5 halamanHealth HX Taking - 20180821202221 PDFWenn Joyrenz ManeclangBelum ada peringkat
- CA Case 3 FINALDokumen18 halamanCA Case 3 FINALWenn Joyrenz ManeclangBelum ada peringkat
- Hinduism 1Dokumen10 halamanHinduism 1Wenn Joyrenz ManeclangBelum ada peringkat
- Health HX Taking - 20180821202221 PDFDokumen5 halamanHealth HX Taking - 20180821202221 PDFWenn Joyrenz ManeclangBelum ada peringkat
- Genetic TreeDokumen5 halamanGenetic TreeWenn Joyrenz ManeclangBelum ada peringkat
- BEMONC Ob Part (Compatibility Mode)Dokumen49 halamanBEMONC Ob Part (Compatibility Mode)Sven Ordanza100% (2)
- High Risk NewbornDokumen4 halamanHigh Risk NewbornWenn Joyrenz ManeclangBelum ada peringkat
- Parts of SyllogismDokumen4 halamanParts of SyllogismAditya RajBelum ada peringkat
- Aspects of Academic Writing-1Dokumen4 halamanAspects of Academic Writing-1Wenn Joyrenz ManeclangBelum ada peringkat
- Mission, Vison, Central ObjectivesDokumen2 halamanMission, Vison, Central ObjectivesWenn Joyrenz ManeclangBelum ada peringkat
- Kirby Bauer Test MBC Test: Maneclang. Wenn Joyrenz U. 2NUR-6Dokumen15 halamanKirby Bauer Test MBC Test: Maneclang. Wenn Joyrenz U. 2NUR-6Wenn Joyrenz ManeclangBelum ada peringkat
- LabelsDokumen11 halamanLabelsWenn Joyrenz ManeclangBelum ada peringkat
- DRRM Tool RevisedDokumen3 halamanDRRM Tool RevisedJaica Mangurali TumulakBelum ada peringkat
- ANTI Inflams 1Dokumen8 halamanANTI Inflams 1Wenn Joyrenz ManeclangBelum ada peringkat
- Student Handbook 2015-2016Dokumen9 halamanStudent Handbook 2015-2016Alexis TrinidadBelum ada peringkat
- The AdolescentDokumen1 halamanThe AdolescentWenn Joyrenz ManeclangBelum ada peringkat
- DR FolderDokumen1 halamanDR FolderWenn Joyrenz ManeclangBelum ada peringkat
- Dosage & Solution (Pharma)Dokumen8 halamanDosage & Solution (Pharma)Wenn Joyrenz ManeclangBelum ada peringkat
- Philippine LawsDokumen1 halamanPhilippine LawsWenn Joyrenz ManeclangBelum ada peringkat
- IDEOGENESISDokumen1 halamanIDEOGENESISWenn Joyrenz Maneclang75% (4)
- Pharmacokinetics: Distribution: Blood-Brain BarrierDokumen3 halamanPharmacokinetics: Distribution: Blood-Brain BarrierWenn Joyrenz ManeclangBelum ada peringkat
- High Risk NewbornDokumen4 halamanHigh Risk NewbornWenn Joyrenz ManeclangBelum ada peringkat
- Breast ScreeningDokumen2 halamanBreast ScreeningWenn Joyrenz ManeclangBelum ada peringkat
- Pharmacokinetics: Distribution: Blood-Brain BarrierDokumen3 halamanPharmacokinetics: Distribution: Blood-Brain BarrierWenn Joyrenz ManeclangBelum ada peringkat
- Intro To LogicDokumen19 halamanIntro To LogicWenn Joyrenz ManeclangBelum ada peringkat
- Dosage & Solution (Pharma)Dokumen8 halamanDosage & Solution (Pharma)Wenn Joyrenz ManeclangBelum ada peringkat
- What Is CommunicationDokumen6 halamanWhat Is CommunicationWenn Joyrenz ManeclangBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Recycling of Li Ion Batteries EUDokumen28 halamanRecycling of Li Ion Batteries EUdcahyasturaBelum ada peringkat
- Geas FinalDokumen489 halamanGeas FinalroselleBelum ada peringkat
- Binding Energy Worksheet - 3Dokumen4 halamanBinding Energy Worksheet - 3Ysabela BernardoBelum ada peringkat
- Rinnai 26e Service Manual PDFDokumen68 halamanRinnai 26e Service Manual PDFteddiprintBelum ada peringkat
- Exotic TarantulasDokumen82 halamanExotic TarantulasThiago MartinsBelum ada peringkat
- Khairat Al-Emar Co. For Oil Services: Material Safety Data SheetDokumen6 halamanKhairat Al-Emar Co. For Oil Services: Material Safety Data SheetqwaszxcdeBelum ada peringkat
- 2045 6063 1 PB PDFDokumen5 halaman2045 6063 1 PB PDFPradeep ShivaBelum ada peringkat
- 13 - Chapter 3Dokumen32 halaman13 - Chapter 3Wahab Al-QaisiBelum ada peringkat
- B Pharma-1 PDFDokumen2 halamanB Pharma-1 PDFHIMANSHU YADAVBelum ada peringkat
- Good Introduction To ElastomerDokumen12 halamanGood Introduction To ElastomerAnirudhreddy SafalBelum ada peringkat
- Fill Rite Series 5200 Piston Hand Pump OIPMDokumen8 halamanFill Rite Series 5200 Piston Hand Pump OIPMElmeri Fidel Gomez AriasBelum ada peringkat
- Axis TurbineDokumen7 halamanAxis TurbineBhertrand GomesBelum ada peringkat
- Pretreatment of Wool - Part-1Dokumen5 halamanPretreatment of Wool - Part-1Mohammed Atiqul Hoque Chowdhury50% (2)
- Nutrients Deficiency SymptomsDokumen4 halamanNutrients Deficiency SymptomsJodie Mer DayamaBelum ada peringkat
- Shell Rl3 MsdsDokumen8 halamanShell Rl3 MsdsHitesh ShahBelum ada peringkat
- Applications and Impact of Nanocellulose Based AdsorbentsDokumen24 halamanApplications and Impact of Nanocellulose Based AdsorbentsLuiz CardBelum ada peringkat
- Sika PDS E Intraplast ZDokumen2 halamanSika PDS E Intraplast Zlwin_oo2435100% (1)
- The Mole Volume Relationships of GasesDokumen15 halamanThe Mole Volume Relationships of GasesMaku MichaelBelum ada peringkat
- ET-88 MSDS - Electrical Contact Cleaner & Moisture DisplacerDokumen4 halamanET-88 MSDS - Electrical Contact Cleaner & Moisture DisplacerVishnu NBelum ada peringkat
- I. Reading Development A. Before You ReadDokumen11 halamanI. Reading Development A. Before You Readhilda wirandaBelum ada peringkat
- Process UtilityDokumen13 halamanProcess UtilityAnupam Manoj100% (1)
- Division9 FinishesDokumen159 halamanDivision9 FinishesJosh HabanBelum ada peringkat
- LEE 30031 enDokumen3 halamanLEE 30031 enanamarieBelum ada peringkat
- Laboratory SafetyDokumen2 halamanLaboratory Safetyann wamburaBelum ada peringkat
- Atf Dexron Iii: Data SheetDokumen7 halamanAtf Dexron Iii: Data Sheetwilliam bryantBelum ada peringkat
- Atago PAL-1 Refractometer Instruction ManualDokumen5 halamanAtago PAL-1 Refractometer Instruction ManualJosé CamposBelum ada peringkat
- Geopolymer Book Chapter1Dokumen37 halamanGeopolymer Book Chapter1Aslam HutagiBelum ada peringkat
- TP7 TP8manualDokumen10 halamanTP7 TP8manualJuanita Ariza BernalBelum ada peringkat
- Circular No.322017ttbct Specifying and Guiding The Implementation of A Number of Articles of The Law On Chemicals and Decree No.1132017nd-Cp SampleDokumen5 halamanCircular No.322017ttbct Specifying and Guiding The Implementation of A Number of Articles of The Law On Chemicals and Decree No.1132017nd-Cp Samplegun nandaBelum ada peringkat
- Concentration Term Jee Main Selected 2Dokumen3 halamanConcentration Term Jee Main Selected 2aebafbigiBelum ada peringkat