1 Patho5 - Kidney I 2015b
Diunggah oleh
miguel cuevasJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
1 Patho5 - Kidney I 2015b
Diunggah oleh
miguel cuevasHak Cipta:
Format Tersedia
5.1.
KIDNEY PATHOLOGY I:
GLOMERULAR DISEASES
Ma. Josefa D. Mesina, M.D., F.P.S.P. December 13, 2012
Objectives:
Review the normal gross and microscopic features of the kidney
RENAL PATHOLOGY
Define/describe the different clinical manifestations/syndromes pertaining to Definition of Terms:
renal diseases
*Azotemia
Describe the pathologic mechanisms behind glomerular, tubulointerstitial and
vascular diseases Biochemical abnormality that refers to an elevation of the
Describe the morphologic changes blood urea nitrogen (BUN) and creatinine levels
Discuss the clinical outcome/prognosis of the different diseases in the kidney
Related largely to a decreased glomerular filtration rate
(GFR)
LEGEND:
Powerpoint and lecture Consequence of many renal disorders, but it also arises from
Robbins extrarenal disorders
Must remember Prerenal Azotemia: encountered when there is
hypoperfusion of the kidneys that impairs renal function
ANATOMY without parenchymal damage (e.g. hemorrhage, shock,
volume depletion, congestive heart failure)
2 MAJOR DIVISIONS Postrenal Azotemia: encountered whenever urine flow is
Upper urinary tract (kidney) obstructed beyond the level of the kidney, wherein relief of
Lower urinary tract (pelvicalcyceal system, ureters, the obstruction is followed by the correction of the azotemia
bladder and urethra)
*Uremia
When azotemia becomes associated with a constellation of
PHYSIOLOGIC FUNCTIONS OF THE KIDNEY__ clinical signs and symptoms and biochemical abnormalities
Excretes the waste products of metabolism Characterized by: failure of renal excretory function,
Serves to convert more than 1,700 liters of blood per day into metabolic and endocrine alterations resulting from renal
about 1 liter of a highly specialized concentrated fluid called damage
urine Manifests secondary involvements of the GIT (uremic
Regulates the bodys concentration of water and salt gastroenteritis), peripheral nerves (neuropathy), and heart
With the lungs, it maintains the acid-base balance (uremic fibrinous pericarditis)
Serves as an endocrine organsecreting hormones
such as erythropoietin, renin and prostaglandins
Clinical Manifestations of Renal Diseases
The study of kidney diseases is facilitated by dividing them into those that NEPHRITIC SYNDROME
affect the four basic morphologic components: glomeruli, tubules, Acute onset of usually grossly visible hematuria, mild
interstitium, blood vessels. to moderate proteinuria, hypertension
This approach is useful since the early manifestations of disease Classic presentation of acute poststreptococcal
affecting each of these components tend to be distinct.
glomerulonephritis
GROSS FEATURES OF THE KIDNEY RAPIDLY PROGRESSIVE GLOMERULONEPHRITIS
Nephritic syndrome with rapid decline (hours to
days) in GFR
NEPHROTIC SYNDROME
Heavy proteinuria (>3.5 gm/day), hypoalbuminemia,
severe edema, hyperlipidemia, lipiduria
ASYMPTOMATIC HEMATURIA OR PROTEINURIA
OR COMBINATION
Manifestation of subtle or mild glomerular
Fig. 1. Normal Kidney abnormalities
150 g - average weight of adult kidney
ACUTE RENAL FAILURE
1 -1.5 cm - cortical thickness
Dominated by oliguria or anuria and recent onset of
Normal to have a minimal amount of fat
azotemia (see acute tubular necrosis)
Major parts:
Cortexouter region RENAL TUBULAR DEFECTS
Medullainner region Dominated by polyuria, nocturia and electrolyte
Collecting systemwhich consists of the proximal disorders
portion of the ureter that is connected to the renal Result of diseases that either directly affect tubular
pelvis, which branches inward to the kidney towards structure or cause defects in specific tubular functions
the major calices and branches further to the minor
calices URINARY TRACT INFECTION
Bacteriuria amd pyuria (bacteria and lymphocytes)
May be symptomatic or not
May affect the kidney (pyelonephritis) or the bladder
(cystitis)
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 1 of 10
NEPHROLITHIASIS
Renal stones
Manifested by severe spasms of pain (renal colic) and
hematuria
Often with recurrent stone formation
URINARY TRACT OBSTRUCTION OR
RENAL TUMORS Fig. 2. Components of Glomerulus
Varied clinical manifestations Comprises of:
Endothelial cellsattach inward to the capillary
CHRONIC RENAL FAILURE lumen
Prolonged signs and symptoms of uremia Visceral epithelial celloutside the endothelial
End result of all chronic renal parenchymal diseases cell
Stage I (Diminished Renal Reserve): GFR is 50% of Mesangial cellssupporting cells (together with
normal. Serum BUN and creatinine levels normal. the mesangial matrix: makes up the mesangium)
Asymptomatic. More susceptible to develop azotemia *Mesangiumserves as the supporting
with additional renal insult. framework of the interconnecting capillary
Stage II (Renal Insufficiency): GFR is 20-50% of lumen
normal. Azotemia is present, with anemia and Parietal epithelial cellscomprises of the
hypertension, as well as polyuria and nocturia. Bowmans capsule
Sudden stress may precipitate uremia. Main function: maintains the integrity of
Stage III (Chronic Renal Failure): <20-25% of normal. glomerular filtration barrier
Edema, metabolic acidosis and hyperkalemia present.
Overt uremia may ensue, with neurologic, GIT and
CV complications.
Stage IV (End-Stage Renal Disease): <5% GFR of
normal. Terminal stage of uremia.
Table 1: Principal Systemic Manifestations of Chronic Kidney
Disease and Uremia:
Fluid and Electrolytes: MEHD Metabolic acidosis
Edema Normal Glomerulus
Hyperkalemia
Dehydration Fig. 3. Histology of Glomerulus
Calcium Phosphate and Bone: Hyperphosphatemia
Hyper PP LowC RO Hyperparathyroidism GLOMERULAR FILTRATION BARRIER
(secondary)
Hypocalcemia Composed of:
Renal Osteodystrophy Fenestrated endothelial cells
Hematologic: AB Anemia Basement membrane
Bleeding diathesis Epithelial podocytes layer or visceral layer
Cardiopulmonary: C-CHUP Cardiomyopathy
Congestive heart failure 2 Factors that will Determine Filtration
Hypertension Size of the molecule - <70 kilodalton (molecular
Uremic pericarditis
weight of albumin) will allow solutes to pass through.
Pulmonary edema
>70kd will not pass through.
Gastrointestinal: BEN Bleeding
Esophagitis, gastritis, colitis *Responsible for the slit like diaphragm cells called your
Nausea and vomiting visceral epithelial cells or your podocytes.
Neuromuscular: PEM Peripheral neuropathy
Encephalopathy Charge of the barrier - the more cationic the substance
Myopathy is, the more it is permeable to the filtrating
Dermatologic: PSD Pruritus membrane. Such that your albumin is anionic ---->
Sallow color can't pass.
Dermatitis
*Responsible for this charged selective barrier is your
proteoglycans and sialoglycans proteins that coat the
OVERVIEW: GLOMERULAR DISEASES membranes of your endothelial and visceral epithelial together
Normal Glomerulus with your basement membrane.
Most important functional unit of the kidney
Histologically: an interconnection of capillary loops Glomerular Syndromes
like a specialized vascular unit 1. Acute Nephritic Syndrome (inflammation in glomeruli)
Glomerulus consists of an anastomosing network of Hematuria and red cell casts in urine
capillaries lined by fenestrated endothelium invested Associated with azotemia - increase in blood urea and
by two layers of epithelium. BUN without signs and symptoms of CRF. Also
The visceral epithelium is incorporated into and accompanied with:
becomes an intrinsic part of the capillary wall, o Variable proteinuria non-nephrotic range
separated from endothelial cells by a basement o Oliguria
membrane. o Edema and hypertension
The parietal epithelium, situated on the Bowmans 2. Rapid Progressive Glomerulonephritis
capsule, lines the urinary space, the cavity in which Characterized by a rapid/fast renal deterioration
plasma filtrate first collects. associated with
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 2 of 10
o Oliguria Common feature of focal segmental
o Nephritic syndrome glomerulosclerosis.
3. Nephrotic Syndrome By electron microscopy, the hyaline is extracellular
4. Chronic Renal Failure (CRF) and amorphous. It is made up of plasma proteins that
Increase in BUN and creatinine with have insudated from the circulation into glomerular
development of uremia in time structures.
Uremia - can cause systemic manifestation When extensive, it contributes to obliteration of the
With isolated cases of hematuria and proteinuria. capillary lumens of the glomerular tuft.
5. Asymptomatic hematuria or proteinuria Usually a consequence of endothelial or capillary wall
6. Isolated Urinary Abnormalities
Glomerular hematuria and/or subnephrotic
proteinuria
Histologic Alterations
HYPERCELLULARITY_________________________
Increase in number of cells in the glomerular tufts.
Characterized by one or more combinations of the following:
Cellular Proliferation of mesangial and
endothelial cells.
Leukocytic infiltration of neutrophils, monocytes injury.
and lymphocytes. Fig. 6. Hyalinization Pattern. Due to accumulations of plasma proteins
Formation of crescents - these are accumulations from the capillary loops.
of cells composed of proliferating parietal
epithelial cells + leukocytes. Sclerosis
This epithelial cell proliferation occurs Characterized by accumulations of extracellular
following an immune/inflammatory injury. collagenous matrix, either confined to mesangial
The molecule that elicits this crescentic areas or involving the capillary loops, or both.
response is fibrin. May also result to capillary lumen obliteration, which
could lead to the formation of fibrous adhesions
between the sclerotic portions of the glomeruli and
the nearby parietal epithelium and Bowmans
capsule.
Fig. 4. Hypercellular Pattern. Hypercellularity = proliferation. Glomeruli
are enlarged. Cannot appreciate capillary because it is enlarged.
BASEMENT MEMBRANE THICKENING________ Fig. 7. Sclerosis Pattern. Increase or accumulation of ECM that will
eventually obliterate the lumen of the capillary.
Thickening of the capillary walls.
Best seen with periodic acid-Schiff (PAS) stain
Takes one or two forms: Classification according to Histologic Patterns
Thickening of basement membrane due to increased DIFFUSE - all glomeruli involved
synthesis of its protein components e.g diabetic FOCAL - some glomerulus are affected, some are not
glomerulosclerosis (only a proportion are involved)
GLOBAL - one whole glomerulus
SEGMENTAL - only portions of the glomerulus are
injured.
Pathogenesis of Glomerular Injury
Note: In general, glomerular diseases are immune-mediated in that it
requires a reaction between the Ag and Ab.
Deposition of amorphous electron-dense material,
most often immune complexes,on the endothelial and
epithelial side of the basement membrane or within
GBM itself.
Fig. 5. Basement Membrane Thickening Pattern due to deposition of
immune complexes. BM thickening = equates to the word membranous
HYALINOSIS AND SCLEROSIS_______________
Hyalinosis
Denotes accumulation of material that is
homogenous and eosinophilic by light microscopy. Fig. 8. Pathogenesis of Glomerular Disease (Robbins has a good
discussion on this topic. Please read )
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 3 of 10
MECHANISM 1: PATHOGENESIS______________________________
CIRCULATING IMMUNE COMPLEXES_________ Immune complex-mediated mechanism:
Ag can either be endogenous (self Ag e.g SLE) or Circulating Ab-Ag complexes Entrapped in the glomeruli
exogenous (invading pathogens) Glomerular injury by activation of complement by the immune
These circulating immune complexes are trapped and complexes
activate your alternate complement system -->
activating MAC --> glomerular disease MORPHOLOGY_______________________________
In Light Microscopy:
MECHANISM 2:
IN SITU IMMUNE COMPLEX DEPOSITION____
Ab reacts directly with an intrinsic tissue Ag that is
found already or native in your glomerular B.M. Its
comparable to your auto-immune mechanism.
Or an Ag circulating that gets planted in the
glomerulus.
Other mechanisms that can damage your glomerulus:
Fig. 10. Histology of Poststrep GN. Enlarged Hypercellularity
Desensitization of your T-cells (leukocytic infiltration, endothelial & mesangial cell proliferation; in severe =
Activation of your Alternate Complement Pathway crescent formation) Diagnostic feature of Acute Diffuse Proliferative GN.
Diffuse: All glomeruli are affected.
In Immunofluorescence:
Fig. 11. Granular pattern due to focal and sparse deposition of IgG,
IgM and C3 (Ab-Ag complex deposition) in the mesangium and along
the GBM. Because of the deposition, there will be a decreased level of IgG,
Fig. 9. Immune Complex Deposition would be described as a granular IgM and C3 in the serum
appearance because of the random deposition of the immune complexes within
the BM. As compared to your In situ in which your Ag is within the BM In Electron Microscopy:
itself and is distributed uniformly projecting a linear pattern. Discrete amorphous electron dense deposit on the
epithelial side of the membrane: humps appearance
PRIMARY GLOMERULAR DISEASES
These diseases show characteristic: CLINICAL COURSE___________________________
Acute Nephritis
Overall prognosis is good in both children (95%) and
o Acute diffuse glomerulonephritis
o Rapid progressive/crescentic glomerulonephritis adults
Nephrotic Presentation Classic case: Young child develops malaise, fever,
o Minimal change disease nausea, oliguria and hematuria (smoky or cola-
o Focal segmental glomerulosclerosis
o Membranous glomerulonephritis
colored urine) 1-2 weeks after recovery from sore
o Membranoproliferative glomerulonephritis throat.
Primary Hematuria Since it is proliferative, it is nephritic syndrome.
o IgA neuropathy
Other Postinfectious (Non-Streptococcal) GN:
Acute Diffuse Glomerulonephritis Seen in other bacterial disease (staphylococcal endocarditis,
Prototype: Postinfectious / Poststreptococcal pneumococcal pneumonia & meningococcemia), viral diseases
Glomerulonephritis (Hep, B & C, mumps, varicella, HIV infection & infectious
Inflammation of the glomerulus causing histologic mononucleosis) and parasitic infection (malaria,
alterations in the form of hypercellularity and toxoplasmosis)
clinically present as nephritic syndrome
Appears 1 4 weeks after a streptococcal infection of
Rapid Progressive Glomerulonephritis
the pharynx or skin (impetigo)
Severe glomerular injury resulting to rapid and
Most frequently affected are children 6-10 yrs. old
progressive decline in renal function.
Manifests with hematuria, edema, hypertension
Manifests with severe oliguria and nephritis
Proteinuria is also manifested but not that severe.
Main histologic feature: epithelial proliferation -
Can be endogenous (like SLE) or exogenous (post-
Crescent formation
infection)
Proliferation obliterates the glomerular tuft, making it
Skin infections are commonly associated with
one of the dreaded diseases
overcrowding and poor hygiene.
Not a specific disease entity, more of a sequelae or
Antigenic determinants: Strep pyogenic exotoxin B
complication.
(SpeB) and its zymogen precursor (zSpeB)
Etiologic agent: nephritogenic strains of group A -
3 GROUPS BASED ON IMMUNO MECHANISM_
hemolytic Streptococci (types 12, 4 and 1)
Type1: ANTI-GBM ANTIBODY-INDUCED DISEASE (renal
Identified by typing of M protein of the cell
limited)
wall
Its antibodies attack the glomerular basement
membranes intrinsic antigen.
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 4 of 10
Manifests as hemoptysis and nephritis Disccusing Nephrotic Syndrome
If anti-GBM antibodies cross-react with the
pulmonary alveolar basement membranes: known as
the Goodpasture syndrome (pulmonary hemorrhage
with renal failure; clinical manifestation is recurrent
hemoptysis)
Linear pattern of IgG and C3 deposition in the GBM
in immunoflouresence
Treatment: plasmapheresis (to remove the pathogenic
circulating antibodies) or therapy to suppress the
immune response
Most severe and aggressive of the 3 types
Worst prognosis
Type2: IMMUNE COMPLEX MEDIATED
Complication of a previous GN such as Post-
infectious glomerulonephritis, lupus nephritis,
Henoch-Schonlein purpura (Treatment is for the Fig. 13. Pathophysiology of Nephrotic Syndrome. Insidious onset.
underlying disease)
Cellular proliferation in glomerular tuft and crescent Derangement of capillary walls Increased permeability to plasma
Allows proteins to escape plasma to glomerular filtrate Massive
formation
proteinuria Depletes serum albumin levels at a rate beyond the
Granular pattern in immunoflourescence (lumpy- compensatory synthetic capacity of the liver AND increased catabolism of
bumpy appearance) filtered albumin Hypoalbuminemia with a reversed albumin-to-
globulin ratio
Type3: PAUCI-IMMUNE TYPE
Lack of anti-GBM Ab or immune complexes by Decreased colloid osmotic pressure Fluid accumulation in interstitial
immunofluorescence and electron microscopy. tissues AND sodium and water retention (due to compensatory secretion of
aldosterone via the hypovolemia-enhanced renin secretion, stimulation of the
Has circulating anti-neutrophil cytoplasmic Ab
sympathetic system, a reduction in the secretion of natriuretic factors such as
(ANCAs) which attacks visceral epithelial cells ->
atrial peptides) Generalized edema
Thus associated with some vasculitis disease like
microscopic polyangitis, Wegener granulomatosis. Increased blood levels of cholesterol, triglyceride, VLDL, LDL, apoprotein and
decreased concentration of HDL Increased synthesis of lipoproteins in the
Note from 2014B Trans:
liver, abnormal transport of circulating lipid particles and decreased
What is common among these three? SEVERE GLOMERULAR
catabolism Hyperlipidemia Lipiduria
INJURY, basta if we are talking about RPGN, think about severe,
aggressive, very fast, complicated disorder. CAUSES______________________________________
Vary depending on age: Children (<15 y/o) Primary
glomerular disease
MORPHOLOGY_______________________________ Adults (2nd glomerular disease like SLE)
Gross: Enlarged, pale with cortical petechial most important Primary Glomerular Disease:
hemorrhage 1. Lipoid Nephrosis : children
Light Microscopy 2. Membranous GN: adults
o Crescent formation by proliferation of 3. Focal Segmental GS: all ages
parietal epithelial cells
o Obliterated Bowmans space MANIFESTATIONS___________________________
o WBC migration and some fibrin strands seen 1. Massive proteinuria, with the daily loss of 3.5 gm or more of
between the cell layers in the crescents protein (less in children)
2. Hypoalbuminemia, with plasma albumin levels less than 3
Immunofluorescence: gm/dL
o Variable (granular or linear) Ex.
3. Generalized edema
Goodpastures syndrome Linear
Postinfectious GN Granular 4. Hyperlipidemia
Electron Microscopy: 5. Lipiduria lipoprotein leak across the glomerular capillary
Subepithelial deposits & rupture of the GBM wall lipid in urine: free fat or oval fat bodies
(all types) Representing lipoprotein resorbed by tubular
Cause the fibrin to escape the glomerulus epithelial cells and then shed along with the
and settle in the space. degenerated cells
Globinuria: May also occur, making the patient
susceptible to infection (especially with staphylococci
and pneumococci)
Loss of anticoagulant factors (antithrombin III and
antiplasmins) May cause thrombotic and
thromboembolic complications
Membranous Glomerulonephritis/Nephropathy
Most common cause of nephrotic syndrome in adults
Fig. 12. RPGN: Left Visible crescent shape, plus shrinkage of the glomerulus. Characterized by diffuse thickening of the glomerular
Right Immunoflourescence of type 1 RPGN
capillary wall without an increase in number of cells
and the accumulation of electron-dense
immunoglobulin-containing deposits along the
subepithelial side of basement membrane
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 5 of 10
PATHOGENESIS______________________________ Minimal Change Disease
Form of chronic immune complex-mediated disease (Lipoid Nephrosis)
Immune complexes form in situ or circulating Ag Most frequent cause of nephrotic syndrome in children
being trapped in the glomeruli and later on followed Characterized by diffuse effacement/flattening out of
by antibody deposition foot processes of visceral epithelial cells (podocytes) that
Membrane damage due to attack of complements appear normal under light microscopy
Leakage of solutes, such as protein Mainly seen in children 2-6 years old
Direct action of C5b-C9, which activates the Sometimes follows a respiratory infection or routine
glomerular epithelial and mesangial cells Liberate prophylactic immunization
proteases and oxidants Capillary wall injury Most characteristic feature: Dramatic response to
Increased protein leakage corticosteroid therapy
Lesions similar to those of experimental Heymann
nephritisinduced by Ab to a megalin antigenic complex
ETIOLOGY AND PATHOGENESIS_____________
and is considered an autoimmune disease linked to
susceptibility genes and caused most likely by Ab to a renal Immunologic basis despite the absence of immune
autoantigen complexes
Immune dysfunction elaboration of a cytokine-
2 GROUPS BASED ON ETIOLOGY_____________ like circulating substance affects visceral
1. Idiopathic or Primary (85% of cases) epithelial cells Proteinuria
2. Secondary or in association with other systemic diseases Proteinuria is selective to albumin only (since visceral
Development of immune complexes due to the epithelial cells are the size-selective barrier of GBM);
presence of abnormal circulating antigens therefore, there is good response to steroids
Infectious: Hepatitis B & C, syphilis, schistosomiasis
Drug-related: penicillamine, captopril, gold therapy, MORPHOLOGY_______________________________
NSAIDs Light microscopy: NORMAL
Tumor-associated: Lung cancer, colon, melanomas Immunofluorescence: NORMAL (No deposits)
SLE: 15% of GN in SLE is of the membranous type Can only be detected with electron microscopy
MORPHOLOGY_______________________________
Light microscopy and immunofluorescence:
Fig. 14. Normal podocytes
Fig. 13. Left: Silver methenamine stain. Note the uniform, diffuse
thickening of the capillary walls. There are prominent irregular
"spikes" of silver-staining matrix (arrow) projecting from the GBM
lamina densa toward the urinary space, which separate and surround
the deposited immune complexes that lack affinity for the silver stain.
Immune complexes are between the GBM and epithelial cells, the
latter having effaced foot processes.
Right: Characteristic granular immunofluorescent deposits of
IgG and C3 along GBM.
Fig. 15. Minimal Change Disease: visceral epithelial cells showing
uniform and diffuse flattened foot processes, these being replaced by
CLINICAL COURSE___________________________ a rim of cytoplasm often showing vacuolization, swelling and
Variable, irregular hyperplasia of villi.
Progression is associated with
Increase in sclerosis of glomeruli CLINICAL FEATURES_________________________
Increase in BUN Despite massive proteinuria, renal function remains good.
Develop hypertension Commonly NO hypertension or hematuria
Proteinuria is NONSELECTIVE Highly-selective proteinuria (mostly albumin)
Any proteins are flushed out In adults, MCD can be associated with Hodgkins
Poor and unpredictable response to corticosteroid lymphoma
therapy Secondary MCD may follow NSAID therapy (usually
Patients : Adults>children associated with acute interstitial nephritis)
Urine : poorly selective proteinuria
Course: Sudden presentation, usually only minimal Focal Segmental Glomerulosclerosis (FSGS)
trace of hematuria Sclerosis of some, but not all, glomeruli (focal) and
Treatment: poor response to steroid therapy affectation of a portion of the glomerular tuft (segmental)
LM: thick capillary walls Clinical presentation: Nephrotic syndrome or persistent,
IF: granular deposits of IgG & C3 heavy proteinuria
EM: think SUBEPITHELIAL IMMUNE COMPLEX Most common form of glomerulosclerosis in adults
DEPOSITS Various settings in which it occurs:
o Idiopathic or Primary FSGS
o Secondary associated with other disorders
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 6 of 10
Ex. Associated with HIV (HIV nephropathy),
heroin addiction, sickle cell diseases, and From Robbins (was not discussed in class):
Morphologic variant of FSGS: Collapsing Glomerulopathy
massive obesity
Retraction and/or collapse of the entire glomerular tuft
o As a secondary event reflecting scarring of Proliferation and hypertrophy of glomerular visceral
previously active necrotizing lesions epithelial cells
Ex. IgA nephropathy Idiopathic BUT is the most characteristic lesion of HIV-
associated nephropathy
o
As a component of an adaptive response to loss
Associated prominent tubular injury with formation of
of renal tissue in advanced stages of other renal
microcysts; poor prognosis
disorders such as reflux nephropathy,
hypertensive nephropathy, or unilateral renal
Membranoproliferative Glomerulonephritis
agenesis
HALLMARK of FSGS Epithelial damage (MPGN)
Also known as Mesangiocapillary GN
Clinical presentation: May be nephrotic (10-20% of cases)
or mixed nephrotic/nephritic with low C3
TYPES________________________________________1.
Primary or Idiopathic
Type I MPGN Immune complexes in the
glomerulus and activation of both classic and
alternative pathways
Type II MPGN Dense-deposit disease that has
abnormalities that suggest activation of the
alternative complement pathway
Consistently decreased serum C3 but normal C1
and C4 (the immune complex-activated early
Fig. 16. Degeneration and focal disruption of visceral epithelial
components of the complement)
cellsdifference from MCDs diffuse epithelial cell change.
Diminished serum levels of factor B and
PATHOGENESIS______________________________ properdin (from alternative complement
Circulating cytokines and genetically determined pathway)
defects affecting components of the slit diaphragm In the glomeruli, C3 and properdin are
complex (key factor: nephrin, which is the zipper-like deposited, but IgG is not. Recall: C3 is directly
structure between podocyte foot processes that might cleaved by C3b upon contact with Ag and with the aid
control glomerular permeability) Epithelial of IgA aggregates in the presence of factors B and D
damage Generates the labile C3bBb, which is the alternative
Entrapment of plasma proteins in extremely pathway C3 convertase Stabilized by properdin
hyperpermeable foci and increased ECM deposition IN DENSE DEPOSIT DISEASE, C3 nephritic factor
Hyalinosis and sclerosis (C3NeF; a circulating antibody that binds to C3bBb)
Circulating cytokine Recurrence of proteinuria
is present Binding of C3bBb and C3NeF
(sometimes within 24 hours of transplantation with
subsequent progression to overt lesions of FSGS) Stabilizes C3bBb Protected from enzymatic
degradation Favoring persistent C3 activation
Hypocomplementemia
MORPHOLOGY_____________________________
Decreased C3 synthesis in the liver
On light microscopy: focal and segmental lesions involve
only a minority of the glomeruli
Initially, involves only the juxtamedullary glomeruli 2. Secondary MPGN
Then, it becomes more generalized Chronic immune complex disorders like SLE, Hep B
In the sclerotic segments: collapse of capillary loops, and C infections
increase in matrix, segmental deposition of plasma Alpha 1-antitrypsin deficiency
proteins along the capillary wall (hyalinosis) which Malignant diseases (CLL, lymphoma)
could occlude the lumen Hereditary deficiencies of complement regulatory
Lipid droplets and foam cells present proteins
Glomeruli that do not show segmental lesions:
normal on LM but may show increased mesangial
matrix
On electron microscopy: both sclerotic and non-sclerotic areas
show diffuse effacement of foot processes
Focal detachment of epithelial cells
Denudation of underlying GBM
By immunofluorescence: IgM and C3 may be present in
sclerotic areas and/or mesangium
Pronounced hyalinosis and thickening of afferent
Fig. 17. MPGN. Basement membrane thickening. Proliferation of
arterioles
glomerular cells. Glomeruli are large and hypercellular. Leukocytic
In time: lead to global glomerulosclerosis with infiltration especially in the mesangium. Enlarged glomeruli showing
pronounced tubular atrophy and interstitial fibrosis mesangial cell proliferation. Lobular appearance of glomerular tuft.
MORPHOLOGY_______________________________
GBM thickened; often segmentally: most evident in
peripheral capillary loops
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 7 of 10
Capillary wall: double-contour or tram-track
appearance (especially evident in silver or PAS stains)
Caused by BM duplication/splitting
Split basement membrane: result of new BM
synthesis in response to subendothelial deposits of
immune complexes
Type I MPGN
Subendothelial electron-dense deposits
C3 is deposited in granular pattern
IgG and early complement components (C1q and C4) Fig. 18. Alport Syndrome. GBM and tubular BM show irregular foci of
are often present thickening alternating with attenuation (thinning) and pronounced
splitting and lamination of the lamina densa, often producing a
Type II MPGN distinctive basket-weave appearance.
Lamina densa of GBM becomes an irregular, ribbon-
like, extremely electron-dense structure due to the THIN BASEMENT MEMBRANE DISEASE_______
deposition of dense material a.k.a. Benign Familial Hematuria
C3 is present in irregular granular or linear foci in Clinically manifested by familial asymptomatic
the BM on either side but not within the dense hematuria discovered on routine urinalysis
deposits Diagnosed morphologically through electron
C3 is also present in the mesangium in characteristic microscopy by thinning of GBM between 150-250 nm
circular aggregates (mesangial rings) (Normal: 300-400 nm)
IgG absent Mode of inheritance: Heterozygous
Pathogenesis:
IgA Nephropathy (Berger Disease) Defective genes encoding 3 or 4 chains of
Isolated urinary abnormality Type IV collagen
Form of glomerulonephritis characterized by the presence
of prominent IgA deposits in the mesangial regions
detected ONLY by immunofluorescence microscopy
(immunocytochemical techniques)
Frequent cause of recurrent gross or microscopic
hematuria
Clinical presentation: Hematuria (gross/microscopic) and
mild proteinuria
Most common form of GN worldwide (except among Fig. 19. Thin Basement Membrane
African-Americans)
Chronic Glomerulonephritis
Course: 15-40% in a span of 20 years End-Stage Renal
Disease
Prognosis: Proteinuria > 1g/day and hypertension are bad
PATHOGENESIS______________________________
Polymeric IgA links with antigen and is carried into circulation
Deposition into mesangium Activates complement
Glomerular injury
Fig. 20. Chronic glomerulonephritis is more of an end-stage pool of the
previously discussed glomerulopathies. If these diseases progress
MORPHOLOGY_______________________________ further, they end up as chronic GM.
By immunofluorescence: mesangial deposition of
IgA, often with C3 and properdin and lesser
amounts of IgG or IgM
C1q and C4 absent
TREATMENT_________________________________
ACE inhibitors/Angiotensin receptor blockers (ARB)
If recurrent Renal transplantation
Hereditary Nephritis
Refers to a group of heterogenous familial renal diseases
associated primarily with glomerular injury.
ALPORT SYNDROME_________________________ Fig. 21. Cross-section of kidney with chronic GM where you are able to
Hematuria progressing to chronic renal failure, appreciate several features: symmetrically contracted, diffusely
accompanied by nerve deafness and various eye granular cortical surface, thinned-out cortex, increased peripelvic fat.
With the ruler you can observe that these kidneys are small. Normal diameter
disorders (including lens dislocation, posterior
is 10cm. Here it is 8cm (size reduction).
cataracts, corneal dystrophy)
Mode of inheritance: X-linked
Pathogenesis:
Mutation of gene encoding Type IV collagen
(main component of GBM) defective assembly
of Type IV collagen (seen in GBM, lens of the eye,
cochlea)
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 8 of 10
Class I - Minimal or no detectable abnormality
Seen in 5% of SLE patients
Class II Mesangial Lupus Glomerulonephritis
Mesangial cell proliferation and lack of involvement
Fig. 22: In Chronic GM, there is difficulty stripping off the renal of the glomerular capillary walls.
capsule. If ever you are able to do so it will reveal a coarsely granular
Seen in 10-25% of SLE patients
cortical surface.
Minimal renal manifestation in the form of mild
hematuria or transient proteinuria.
Immunofluorescense: granular mesangial deposits of
Ig and complement are present.
Fig. 23. Special stain showing hyalinosis of glomeruli in Chronic GM.
Hyalinosis of glomeruli indicates end-stage changes in glomeruli.
Tubular atrophy. Interstitial fibrosis.
MORPHOLOGY_______________________________ Fig. 25. Class II Mesangial GN
Early cases: evidence of primary disease
Progression: obliteration of glomeruli acellular
eosinophilic masses (trapped plasma proteins, Class III Focal Proliferative Glomerulonephritis
increased mesangial matrix, BM-like material and 20-25% of SLE cases
collagen) Focal = some glomeruli normal, some are not
Arterial and arteriolar sclerosis may be conspicuous: Proliferative = hypercellularity
because of co-morbid hypertension
Marked atrophy of associated tubules, irregular
interstitial fibrosis and mononuclear leukocytic
interstitial infiltration
Dialysis changes: arterial intimal thickening caused
by accumulation of smooth muscle-like cells and a
loose, proteoglycan-rich stroma, focal calcification,
extensive deposition of calcium oxalate crystals in
tubules and intersitium, acquired cystic disease,
increased numbers of renal adenomas and
adenocarcinomas
Uremic complications (see table on page 2)
Fig. 26: Class III Focal Proliferative GN
Class IV Diffuse Proliferative GN
GLOMERULAR LESIONS ASSOCIATED WITH Most serious form of lupus nephritis
SYSTEMIC DISEASE 35-60% of SLE patient
Systemic Lupus Erythematosus Diffuse = all glomeruli are abnormal
Fig. 27. Class IV Diffuse GN
Fig. 28. wire loop usually appreciated in Class IV because it is your
capillary basement membrane thickening. Usually when this lesion is
present in biopsy in SLE it connotes active disease. Individual is
Fig. 24. Pathogenesis of SLE. SLE is a multisystemic disorder: antibodies
continually forming these immune complexes. Need to treat with
against self-antigens. Since it is immune mediated, one of organs not spared is
steroids.
the kidneys.
W.H.O. CLASSIFICATION OF LUPUS NEPHRITIS Class V Membranous GN
Clinical picture is similar to that of Idiopathic
BASED ON MORPHOLOGY
membranous GN.
Usually if you have a patient visiting a nephrologist, the first thing
would like to note is the extent of kidney damage. Want to know
prognosis by doing renal biopsy then classifying based on the Diabetic Nephropathy
following criteria: Diabetes mellitus is now one of the most common causes of
end-stage renal failure.
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 9 of 10
Diabetes can affect the kidney in three forms: POP QUIZ!
1. Complications of diabetic vasculature 1. What glomerular syndrome manifests as hematuria,
2. Diabetic glomerular damage azotemia, variable proteinuria, oliguria, edema and
3. Increased susceptibility to infection and papillary hypertension?
necrosis 2. At what value of proteinuria can one classify the case as
nephrotic syndrome?
3. What is the GFR associated with Stage II Renal Failure?
CONTRIBUTORS TO RENAL TISSUE INJURY___ 4. What condition are ANCAs associated with?
Glucose toxicity (hyperglycemia) -- metabolic effect causes 5. This condition can only be diagnosed through
biochemical alterations in glomerular basement membrane immunoflurorescence testing.
Non-enzymatic glycosylation of proteins AGE (advanced 6. What condition is associated with Kimmelstiel-Wilson
glycosylation end products) that are toxic to the glomerulus disease?
Hemodynamic changes (inc. GFR, inc. glomerular 7. What condition has a characteristic tram-track appearance of
the capillary wall?
capillary pressure, glomerular hypertrophy and inc.
8. What are the most common etiologic agents of acute diffuse
glomerular filtration area) glomerulonephritis?
9. What condition can be described grossly as symmetrically
MORPHOLOGIC CHANGES IN GLOMERULI___ contracted, diffusely granular cortical surface, thinned-out
Capillary basement membrane thickening cortex, increased peripelvic fat?
Diffuse mesangial sclerosis 10. What condition manifests as hematuria progressing to
Nodular sclerosis (pathognomonic lesion of diabetic chronic renal failure, accompanied by nerve deafness and
various eye disorders?
nephropathy) - intercapillary glomerulosclerosis or
Kimmelstiel Wilson disease
REFERENCES
Dr. Mesinas lecture and powerpoint
Robbins
2014B Trans
Hey 2015B HAPPY CHRISTMAS ;D
Since its Christmas break na, then New Year, we just wanna share stuff with you
and baka its the end of the world, and thisll be the last thing youll read
(ASA) :p
Beeteedub, CONGRATULATIONS FAITH :D
P.S. EVERYONE, LETS EOWS a.k.a. End of the World S.. ;))
Pag nilalandi ka ng crush mo, sabihin mo: WAAAAAAAAGmong itigil
Kung may rabies ka, handa akong maulol..makahalik lang sa yo
Kung single ka, mahalin mo muna sarili mo. Tapos kapag ready ka na, isunod mo na ako
Fig. 29. Diffuse and nodular diabetic glomerulosclerosis. Sclerosis of :D
some of capillary loops. Sclerosis is due to accumulation of extracellular Why do students choose to shade the wrong answer? Because we accept the grade we
collagenous matrix that eventually obliterates lumen of capillary loops. think we deserve #PerksofBeingACrammer
Aabsent na lang ako sa lahat ng klase ko..makapasok lang sa puso mo
Buti pa ang mga aso, alam kung paano mag-STAY.
Henoch-Schonlein Kapag payat, COSPLAYER. Kapag mataba, MASCOT ;)))))
Purpuric skin lesions characteristically affecting the Sa panahon ngayon: uso na ang mag-move-on..kahit hindi nagiging kayo ;))
extensor surface of the arms and legs and buttocks,
Baka kaya tayo iniiwan ng mga taong mahal natin, kasi baka merong bagong darating na
abdominal manifestation (abdominal pain, vomiting,
mas okay. Na mas mamahalin tayo. Yung taong hindi tayo sasaktan at paaasahin. Yung
intestinal bleeding), non-migratory abnormalities and nag-iisang taong magtatama ng mali sa buhay natin, nang lahat ng mali sa buhay mo.
urinary abnormalities. P
Renal manifestation: gross or microscopic hematuria,
Maybe I dont wanna be saved the trouble. Maybe I want the trouble. I havent wanted
proteinuria, and nephrotic syndrome. the trouble in a long time. But with you, the trouble doesnt seem so troubling. I dont
IgA is deposited in the glomerular mesangium, know. I thought.. I guess I thought you felt the same way. B
sometimes with IgG and C3, similar to that of IgA
T: Okay, I'm going to say something out loud that I've been doing a pretty good job of
nephropathy.
not saying out loud lately. What you and Tony have, what I thought for a second you and
Usually seen in children. If seen in adults, it carries a poor I had, what I know that Marshall and Lily have, I want that. I do. I keep waiting for it to
prognosis. happen. I'm waiting for it to happen. I guess I'm just tired of waiting. And that is all I'm
going to say on that subject.
S: I know that you're tired of waiting. And you might have to wait a little while more
Amyloidosis but, she's on her way, Ted. And she's getting here as fast as she can.
Amyloid (a pathologic protein) is deposited in the GBM and
L: Okay, yes, its a mistake. I know its a mistake. But there are certain things in life
mesangium. where you know its a mistake but you dont really know its a mistake because the only
Permeability is increased proteinuria way to really know its a mistake is to make the mistake, and look back, and say, Yep.
Amyloid deposits may be found in the blood vessel wall That was a mistake. So, really, the bigger mistake would be to not make the mistake,
because then you go your whole life not really knowing if something is a mistake or not.
and interstitium
And, damn it, Ive made no mistakes! Ive done all of this my life, my relationship, my
career mistake-free. Does any of this make sense to you?
ANSWER KEY:
1. Nephritic syndrome
2. >3.5 gm/day
3. 20-50% of normal
4. Type III Pauci Immune Type RPGN
5. IgA Nephropathy (Bergers Disease)
6. Diabetic Nephropathy
Fig. 30. Pink. How to differentiate from sclerosis and hyalinosis. Use congo 7. Membranoproliferative Glomerulonephritis
red stain to document as amyloidosis. 8. Group A -hemolytic Streptococci (types 12, 4 and 1)
9. Chronic Glomerulonephritis
10. Alport Syndrome
Melgar|Mendoza|Montenegro|Pascual|Santos, P. Kidney Pathology I: 2015B Page 10 of 10
Anda mungkin juga menyukai
- Robbin's Chapter 20 Kidney PathologyDokumen4 halamanRobbin's Chapter 20 Kidney Pathologynbaumgartner0100% (1)
- Endocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologyDokumen3 halamanEndocrine Gland Hormone(s) Secreted Stimulus Effect of Hormone Inhibition PathologySamuelBelum ada peringkat
- Pathology of Liver, Biliary, and PancreasDokumen52 halamanPathology of Liver, Biliary, and PancreasHassan.shehri100% (11)
- Pulmonary PathologyDokumen6 halamanPulmonary PathologyjamesjaanBelum ada peringkat
- Approximate Equivalents:: 0.100 Gmn. 1.00 GMDokumen8 halamanApproximate Equivalents:: 0.100 Gmn. 1.00 GMakane ryuBelum ada peringkat
- Robbins Ch. 20 The Kidney Review QuestionsDokumen10 halamanRobbins Ch. 20 The Kidney Review QuestionsPA2014100% (4)
- Inflammation and Repair OverviewDokumen10 halamanInflammation and Repair OverviewMiguel Cuevas DolotBelum ada peringkat
- Pharmacology of EthanolDokumen5 halamanPharmacology of EthanolJoshua RemonBelum ada peringkat
- Endocrine Disorders and Exam QuestionsDokumen6 halamanEndocrine Disorders and Exam QuestionsMartina GarciaBelum ada peringkat
- Endocrine PathologyDokumen13 halamanEndocrine Pathologysarguss14100% (1)
- Patho4-6 - Liver (Dr. Dy)Dokumen13 halamanPatho4-6 - Liver (Dr. Dy)miguel cuevas100% (1)
- 4 PEDIA 8 - Bleeding DisordersDokumen5 halaman4 PEDIA 8 - Bleeding DisordersRainy Liony DuhBelum ada peringkat
- Surgery Tips and ResourcesDokumen2 halamanSurgery Tips and ResourcesAbeebs SalahouBelum ada peringkat
- Gastrointestinal PathologyDokumen14 halamanGastrointestinal PathologyRahul ShuklaBelum ada peringkat
- WBC Pathology: Lecturer: Associate Professor T. A. GrekovaDokumen49 halamanWBC Pathology: Lecturer: Associate Professor T. A. GrekovaFaheem MusthafaBelum ada peringkat
- Pancreatic Hormones and Antidiabetic AgentsDokumen3 halamanPancreatic Hormones and Antidiabetic AgentsChristian DeeBelum ada peringkat
- Gastroenterology 0321Dokumen12 halamanGastroenterology 0321laraib fatima0% (1)
- Patho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Dokumen12 halamanPatho A 1. 5 Hemodynamic Disorders (Bongat, 2015)Grant GarcesBelum ada peringkat
- Cholinergic Drugs - TablesDokumen7 halamanCholinergic Drugs - TablesThuan Tăng NguyenBelum ada peringkat
- Robbins Ch. 18 Liver and Biliary Tract Review QuestionsDokumen12 halamanRobbins Ch. 18 Liver and Biliary Tract Review QuestionsPA2014Belum ada peringkat
- Pathology Cell InjuryDokumen57 halamanPathology Cell InjuryMajd MustafaBelum ada peringkat
- IVMS Hematology-Oncology Summary Table-Notes For USMLE Step 1 Prep.Dokumen16 halamanIVMS Hematology-Oncology Summary Table-Notes For USMLE Step 1 Prep.Marc Imhotep Cray, M.D.100% (1)
- Table of Genetic Disorders: Download A Copy of This Study GuideDokumen11 halamanTable of Genetic Disorders: Download A Copy of This Study Guideerica perezBelum ada peringkat
- Charts For Kidney and Lower Urinary Tract Pathology. NephrologyDokumen34 halamanCharts For Kidney and Lower Urinary Tract Pathology. NephrologyM PatelBelum ada peringkat
- Patho Robbins Sumary Pereira MDDokumen22 halamanPatho Robbins Sumary Pereira MDNicole SarcosBelum ada peringkat
- Nephrolithiasis: An Overview of Kidney Stone Types and PathogenesisDokumen81 halamanNephrolithiasis: An Overview of Kidney Stone Types and PathogenesisOmar Zaman KhanBelum ada peringkat
- Ch.1 Baby Robbins OutlineDokumen11 halamanCh.1 Baby Robbins OutlinePA2014100% (3)
- SurgeryDokumen83 halamanSurgeryHamba Yg Betaubat100% (1)
- Medical MnemonicsDokumen65 halamanMedical MnemonicsMIRZA MUHAMMAD ADNAN100% (1)
- Pathology Week 6 p18-35Dokumen18 halamanPathology Week 6 p18-35zeroun24Belum ada peringkat
- Diseases and Deficiencies - USMLE / COMLEXDokumen15 halamanDiseases and Deficiencies - USMLE / COMLEXtBelum ada peringkat
- PhysiologyWorkbook7 5Dokumen267 halamanPhysiologyWorkbook7 5SophiaBelum ada peringkat
- PD 17 To 21Dokumen148 halamanPD 17 To 21Loai Mohammed IssaBelum ada peringkat
- (Pedia 3A) NEPHRO COMPILED PDFDokumen40 halaman(Pedia 3A) NEPHRO COMPILED PDFNoreenBelum ada peringkat
- Pathology Checklist DR Preeti SharmaDokumen5 halamanPathology Checklist DR Preeti SharmaAvi Khanna100% (1)
- Glomerulonephritis PresentationDokumen23 halamanGlomerulonephritis Presentationjacksonyu1234Belum ada peringkat
- Sickle Cell Anemia - 27Dokumen42 halamanSickle Cell Anemia - 27M.AhmedBelum ada peringkat
- Gi - PathophysiologyDokumen96 halamanGi - Pathophysiologyjmosser100% (4)
- Nephrology ReviewerDokumen3 halamanNephrology ReviewerNix14Belum ada peringkat
- 'Aliah's Physio NotesDokumen30 halaman'Aliah's Physio NotesLuqman Al-Bashir FauziBelum ada peringkat
- GI Board ReviewDokumen176 halamanGI Board Reviewjosh hagsBelum ada peringkat
- Venous congestion in the liverDokumen135 halamanVenous congestion in the liverJustin JannatiBelum ada peringkat
- Factors Affecting Glomerular Filtration Rate (GFRDokumen10 halamanFactors Affecting Glomerular Filtration Rate (GFRManish ChoudharyBelum ada peringkat
- Renal Pathology Lectures - PPT SeriesDokumen267 halamanRenal Pathology Lectures - PPT SeriesMarc Imhotep Cray, M.D.100% (12)
- 2021 Systemic Pathology S4T1 - RBC and Bleeding Disorders PDFDokumen27 halaman2021 Systemic Pathology S4T1 - RBC and Bleeding Disorders PDFAlexis Bondad100% (1)
- Chapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFDokumen9 halamanChapter 7 Neoplasia 1 2 Robbins and Cotran Pathologic Basis of Disease PDFChethranBelum ada peringkat
- Complete Genetics Disease ChartDokumen14 halamanComplete Genetics Disease ChartJames FlanneryBelum ada peringkat
- Pathoma Lecture Notes 2017Dokumen42 halamanPathoma Lecture Notes 2017Priyesh PrinceBelum ada peringkat
- Respiratory Physio UsmleDokumen61 halamanRespiratory Physio UsmleDr.G.Bhanu Prakash100% (2)
- Interpreting the Biochemisty PanelDokumen4 halamanInterpreting the Biochemisty PanelNatalie KingBelum ada peringkat
- Secret Pathology NotesDokumen60 halamanSecret Pathology NotesJamee MmsBelum ada peringkat
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- Practical Gastroenterology and Hepatology Board Review ToolkitDari EverandPractical Gastroenterology and Hepatology Board Review ToolkitKenneth R. DeVaultBelum ada peringkat
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Kidney (Part 1)Dokumen13 halamanKidney (Part 1)Kathlene EmbodoBelum ada peringkat
- Cytogenetics Disorders PDFDokumen7 halamanCytogenetics Disorders PDFmiguel cuevasBelum ada peringkat
- Vitamins Notes PDFDokumen3 halamanVitamins Notes PDFmiguel cuevas100% (1)
- Minerals SummaryDokumen2 halamanMinerals Summarymiguel cuevasBelum ada peringkat
- Histo Pracs - Respi and Brain PDFDokumen17 halamanHisto Pracs - Respi and Brain PDFmiguel cuevasBelum ada peringkat
- Male PhysiologyDokumen2 halamanMale Physiologymiguel cuevasBelum ada peringkat
- Sex Determination and DifferentiationDokumen3 halamanSex Determination and Differentiationmiguel cuevasBelum ada peringkat
- Surgical Pathology Trans No 7. The LIVER DR ROXAS by MCD Recoverd 1Dokumen14 halamanSurgical Pathology Trans No 7. The LIVER DR ROXAS by MCD Recoverd 1miguel cuevasBelum ada peringkat
- Pathology Final Practical ExaminationDokumen40 halamanPathology Final Practical Examinationmiguel cuevasBelum ada peringkat
- Infectious Diseases - BacteriaDokumen9 halamanInfectious Diseases - Bacteriamiguel cuevas100% (1)
- Diseases of The Peripheral Nervous SystemDokumen8 halamanDiseases of The Peripheral Nervous Systemmiguel cuevasBelum ada peringkat
- First Aid: FM 4-25.11 NTRP 4-02.1 AFMAN 44-163 (I)Dokumen224 halamanFirst Aid: FM 4-25.11 NTRP 4-02.1 AFMAN 44-163 (I)Giuseppe TrovatoBelum ada peringkat
- Anti-Viral and Anti-Fungal AgentsDokumen212 halamanAnti-Viral and Anti-Fungal Agentsmiguel cuevas100% (1)
- Hypolipedemic AgentsDokumen9 halamanHypolipedemic Agentsmiguel cuevasBelum ada peringkat
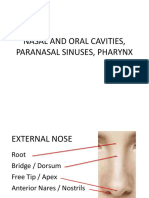
- Nasal and Oral Cavities, Paranasal Sinuses, PharynxDokumen112 halamanNasal and Oral Cavities, Paranasal Sinuses, Pharynxmiguel cuevasBelum ada peringkat
- (New) Drugs Used For Gastrointestinal DiseasesDokumen59 halaman(New) Drugs Used For Gastrointestinal Diseasesmiguel cuevasBelum ada peringkat
- Female Genital Tract Infections and PathologyDokumen16 halamanFemale Genital Tract Infections and Pathologymiguel cuevasBelum ada peringkat
- Glycogenolysis and GlycogenesisDokumen11 halamanGlycogenolysis and Glycogenesismiguel cuevas100% (2)
- SynapseDokumen45 halamanSynapsemiguel cuevasBelum ada peringkat
- 1.18 MycobacteriumDokumen6 halaman1.18 Mycobacteriummiguel cuevasBelum ada peringkat
- CHF and Diuretics Trans Limpin MissionDokumen12 halamanCHF and Diuretics Trans Limpin Missionmiguel cuevasBelum ada peringkat
- Subcutaneous Mycoses Identification and TreatmentDokumen75 halamanSubcutaneous Mycoses Identification and Treatmentmiguel cuevasBelum ada peringkat
- RBC - Patho BDokumen129 halamanRBC - Patho Bmiguel cuevasBelum ada peringkat
- Breast PathologyDokumen27 halamanBreast Pathologymiguel cuevasBelum ada peringkat
- Anesthesia - Dr. FirmalinoDokumen14 halamanAnesthesia - Dr. Firmalinomiguel cuevasBelum ada peringkat
- Anti-Psychotic NewestDokumen118 halamanAnti-Psychotic Newestmiguel cuevasBelum ada peringkat
- He Ma To PoiesisDokumen98 halamanHe Ma To Poiesismiguel cuevasBelum ada peringkat
- Microbiology Lecture 8 & 9 - Systemic & Opportunistic Mycoses (Raroromiki Trans)Dokumen3 halamanMicrobiology Lecture 8 & 9 - Systemic & Opportunistic Mycoses (Raroromiki Trans)miguel cuevasBelum ada peringkat
- Cell Cycle, Apoptosis and CancerDokumen13 halamanCell Cycle, Apoptosis and Cancermiguel cuevas100% (1)
- Second Messengers-OLFU-MD 2017Dokumen66 halamanSecond Messengers-OLFU-MD 2017Melissa SalayogBelum ada peringkat
- Reye'S Syndrome: Mrs. Smitha.M Associate Professor Vijaya College of Nursing KottarakkaraDokumen7 halamanReye'S Syndrome: Mrs. Smitha.M Associate Professor Vijaya College of Nursing KottarakkarakrishnasreeBelum ada peringkat
- Ap Eamcet 2020: Instruction BookletDokumen34 halamanAp Eamcet 2020: Instruction BookletSri Bhavani BoyinaBelum ada peringkat
- Certificate of Accreditation: Swift Silliker (Pty) LTDDokumen10 halamanCertificate of Accreditation: Swift Silliker (Pty) LTDpham xuan tinh tinhBelum ada peringkat
- GI ExamDokumen1 halamanGI ExamCharlz ZipaganBelum ada peringkat
- Acute GastroenteritisDokumen2 halamanAcute Gastroenteritisrobert tucayBelum ada peringkat
- Standard LFT and It's Clinical SignificanceDokumen28 halamanStandard LFT and It's Clinical SignificanceanimathzBelum ada peringkat
- Prak Ospe PK FMS 3 2021Dokumen7 halamanPrak Ospe PK FMS 3 2021Angelique NatalieBelum ada peringkat
- Patient Information: DateDokumen8 halamanPatient Information: Datemehdi chahrour100% (1)
- Camca Prelim Reviewer 2Dokumen11 halamanCamca Prelim Reviewer 2Danna MedranaBelum ada peringkat
- Rpms Lesson PlanDokumen6 halamanRpms Lesson PlanEric John VegafriaBelum ada peringkat
- Bcsci 10 Unit 1 Topic1 2Dokumen20 halamanBcsci 10 Unit 1 Topic1 2DemisBelum ada peringkat
- University of Barisal: AssignmentDokumen7 halamanUniversity of Barisal: AssignmentFiroj AhmedBelum ada peringkat
- Argumentative EssayDokumen7 halamanArgumentative Essayapi-294732914Belum ada peringkat
- 1536106348Dokumen144 halaman1536106348Saman SarKoBelum ada peringkat
- ArthropodaDokumen36 halamanArthropodatapas kunduBelum ada peringkat
- Parameters of Mechanics of BreathingDokumen16 halamanParameters of Mechanics of BreathingKaioBelum ada peringkat
- Benefits Analysis Application Process FAX COVER LETTERDokumen10 halamanBenefits Analysis Application Process FAX COVER LETTERmdugan5026Belum ada peringkat
- Mechanical Treatment For The Cervical SpineDokumen36 halamanMechanical Treatment For The Cervical SpineMohamed ElMeligieBelum ada peringkat
- RH BLOOD GROUPDokumen23 halamanRH BLOOD GROUPWho KnowsBelum ada peringkat
- Universal Credit Work Capability QuestionnaireDokumen24 halamanUniversal Credit Work Capability QuestionnaireSteven Preece100% (2)
- The Sense of Stopping Migraine ProphylaxisDokumen20 halamanThe Sense of Stopping Migraine ProphylaxisdedeadamBelum ada peringkat
- Seri Final NotesDokumen179 halamanSeri Final Notesbharath gowdaBelum ada peringkat
- 7 Vs 14days Gram Negative SepsisDokumen8 halaman7 Vs 14days Gram Negative SepsisPavan KumarBelum ada peringkat
- Integumentary SystemDokumen30 halamanIntegumentary SystemLourizMavericS.SamonteBelum ada peringkat
- 17-Ebcpg Thyroid2013Dokumen20 halaman17-Ebcpg Thyroid2013Mi MingkaiBelum ada peringkat
- Nakshatra DhanishtaDokumen7 halamanNakshatra DhanishtaANTHONY WRITER100% (3)
- Observership ApplicationDokumen5 halamanObservership ApplicationPratiksha KapartiwarBelum ada peringkat
- Shade Establishment and Management in Tea FieldsDokumen55 halamanShade Establishment and Management in Tea Fieldschinthaka100% (1)
- PharmacokineticsDokumen7 halamanPharmacokineticsRonica MendozaBelum ada peringkat
- Rajiv Gandhi University of Health Sciences, Bangalore, KarnatakaDokumen17 halamanRajiv Gandhi University of Health Sciences, Bangalore, KarnatakayashramawatBelum ada peringkat