Traumatic Hyphema
Diunggah oleh
Finy FaradisaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Traumatic Hyphema
Diunggah oleh
Finy FaradisaHak Cipta:
Format Tersedia
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 15, Issue 12 Ver. VIII (December. 2016), PP 16-19
www.iosrjournals.org
Traumatic Hyphema: A Case Series on Admitted Patients in
RIMS Hospital, Imphal
Chelsia Nongtdu1, Sagarika Majumder1, A Suchitra Devi1, Rintu Marak2,
Andrea Tongbram1, Irengbam Supriya1
1
Department Of Ophthalmology, RIMS Imphal,2Department Of Internal Medicine
Abstract
Background: Hyphema is a common sequelae following blunt trauma.
Aims: To determine the causes, associated ocular findings and visual acuity on presentation and at discharge in
accordance with the hyphema grades on presentation.
Materials and methods: A case series study was carried out on admitted patients in Department of
Ophthalmology, RIMS Imphal during the period of January 2015 to June 2015. The data were analysed using
SPSS v 21 program.
Results: A total number of 15 patients were studied. The mean age of the patients was 24.33 13years. There
were 80% males and 20% females. Maximum eye injury occurred at home (40%) during play with toygun.
Conjunctival congestion(73.33%) was seen in most patients. About 33.33% of patients presented with Grade II
hyphema , Grade I and III with 26.67% each and Grade IV with 13.33%. The initial visual acuity of 6/18 was
seen in (33.33%) and < 6/18 in (66.67%). But following treatment the visual acuity of 6/18 was seen in
(73.33%) and < 6/18 in (26.67%) on discharge.
Conclusion: Traumatic hyphema is common in children and young adult during play. It's important to supervise
and use protection during play. However early presentation and the lower grades of hyphema determines better
visual outcome.
Keywords: Blunt trauma, hyphema, visual outcome.
I. Introduction
Hyphema is the accumulation of blood in the anterior chamber of the eye. The mean annual
incidence of hyphema from all causes is approximately 17 per 100,000 1. Clinical symptoms of hyphema include
pain, photophobia, blurring of vision and restlessness. Traumatic hyphema is mostly due to blunt trauma. Blunt
trauma ruptures vessels of iris stroma and ciliary body by antero-posterior compression and equatorial globe
expansion, which causes stress2. In any cases of traumatic hyphema, urgent ophthalmologic consultation is
mandatory as timely diagnosis and treatment can help to prevent many complications such as, increase
intraocular pressure, cataract, optic nerve injury and blindness. The purpose of this study was to determine the
causes, associated ocular findings and visual acuity on presentation and at discharge in accordance with the
hyphema grades on presentation in the Department of Ophthalmology, RIMS, Imphal for the period of six
months from January 2015 to June 2015.
II. Materials And Methods
This was a case series study conducted for the period of six months from Jan 2015 to Jun 2015 on
admitted traumatic patients at Regional Institute of Medical Sciences, Imphal. All admitted patients of blunt
trauma with closed globe injury causing hyphema were included in the study. Variables included were age, sex,
eye involvement, objects causing injury, location of injury, activities at the time of injury, symptoms and other
ocular findings, visual acuity on admission and at discharge and grades of hyphema. The data collected were
calculated and analysed using SPSS software v 21.
III. Results
A total of 15 eyes in 15 patients were seen during the study period. This comprised 12 males (80%)
and 3 females (20%). The mean age was 24.33 13years. There were 8 (53.33%) right eyes and 7 (46.67%) left
eyes involvement. The details of different objects responsible for blunt injury and resulted in hyphema are
shown in Table (1). The highest incidence of eye injury occurred at home (40%) during play, followed by the
workplace (33.33%) during work, playground (13.33%) during sports and others(13.33%) during fight. Patients
mostly presented with symptoms of blurred vision (100%), redness of eye (100%) and eyeache (93.33%). In
addition to hyphema there were other ocular findings (Table 2). Conjunctival congestion was seen in most
patients (73.33%). Iridodialysis was seen in 33.3% of patients. One patient had lens subluxation and associated
DOI: 10.9790/0853-1512081619 www.iosrjournals.org 16 | Page
Traumatic Hyphaema: A Case Series On Admitted Patients In RIMS Hospital, Imphal
fundus findings were macular edema (6.67%) and vitreous haemorrhage (6.67%). Fig (2) shows the visual
acuity of patients on admission and at discharge. It was seen that (33.33%) of patients had visual acuity 6/18
and (66.67%) < 6/18 on admission., whereas, (73.33%) of patients had visual acuity 6/18 and (26.67%) < 6/18
on discharge. The most common form of hyphema in our study was Grade II , seen in 5 (33.33%) patients,
Grade I in 4 (26.67%), Grade III in 4 (26.67%) and Grade IV in 2 (13.33%) as shown in fig (3) above. No
surgical intervention was required in any case as all hyphema cleared up medically without any rise of IOP.
IV. Discussion
In this study the incidence rate of admitted traumatic hyphema patients in Regional Institute of Medical
Sciences, Imphal in the period of January 2015- June 2015 was 80% in male and 20% in female (i.e. 4:1), mean
age was 24.3313 yrs and the highest age frequency was in the age group of 5-15 yrs. High frequency of male
gender and age group of the patients in our study correspond with the study done by Ghafari AB et al3and Cho J
et al4. Males are more commonly encountered with trauma as they are more involved with outdoor activities,
sports and other social activities. Our study found that right eye was most commonly injured than the left eye.
Even Ulagantheran V et al5 and Raju KV et al6 did highlighted the same, whereas Ghafari AB et al3 found the
left eye was more commonly injured than the right. The majority of eye injuries occured in the home
environment7. In our study the location of injury was mostly at home which was play related and toygun
accounted for 33.33% of the injuring agent. This is in congruent with studies conducted by Raju KV et al6 and
Ashaye AO8 where most of the injuries were play related at home. However, in another study done by Al Ali
AK et al9 it was reported that most common trauma was at worksites with projectiles as the commonest injuring
agent. Vision typically follows the severity of the hyphema itself10. In this present work, grade II hyphema was
found in 33.33% of patients followed by grade I and grade III each 26.67%. The lesser grade can be due to
lesser force of impact as it was mostly by toyguns. The vision on admission ranges from 6/9 (13.33%) to PL
(20%). On discharge, 100% of patients having grade I and 80% of grade II had vision > 6/18. Whereas 50% of
grade III hyphema had vision of 6/18, but those with grade IV had vision < 6/18. This compares well with the
work done by Uhumwangho OM et al11 and Cho J et al4. But Al Ali AK et al9 found that neither a poor final
visual outcome nor complications were associated with the size of the hyphema. And Rahmani B et al12 were
unable to show an association between the final visual outcome and the size of a hyphema. In addition to
hyphema, our study also found that conjunctiva was the most affected stucture (73.33%), followed by lid and
adnexa (66.67%). A similar finding was noted in a study done by Pai SG et al13.
V. Conclusion
Hyphema is a sequelae of blunt trauma. In our study we found that majority of the patients were males
and the commonest age of presentation were 5-15 years. The patients were mostly injured at home due to play
related activities. The right eye was most commonly affected and eye structure mostly involved was
conjunctiva, followed by lid and adnexa. Majority of patients had grade II hyphema which clears off with
medical treatment. No surgical intervention was needed and (73.33%) of patients had vision 6/18 on
discharge. This study shows that blunt trauma can be prevented by supervising during play or use of any
protection at work. Also an early initial presentation for early diagnosis and treatment can help to prevent many
ocular complications and better final vision after trauma.
References
[1]. Walton W, Von Hagen S, Grigorian R, Zarbin M. Management of traumatic hyphaema. Surv Ophthalmol 2002 Jul-Aug;47(4):297-
334.
[2]. Khan BS, Hussain I, Nawaz A. Management of traumatic hyphaema with raised intraocular pressure. Pak J Ophthalmol
2007;23(4):217-20.
[3]. Ghafari AB, Siamian H, Aligolbandi K, Vahedi M. Hyphaema caused by trauma. Med Arh. 2013 Oct;67(5):354-6.
[4]. Cho J, Jun BK, Lee YJ, Uhm KB. Factors associated with the poor final visual outcome after traumatic hyphaema. Korean J
Ophthalmol 1998;12(2):122-9.
[5]. Ulagantheran V, Ahmad Fauzi MS, Reddy SC. Hyphema due to blunt injury: a review of 118 patients. Int J Ophthalmol
2010;3(3):272-6.
[6]. Raju KV, Nima CA, Anju AK. Closed globe injuries- A tertiary care experience. Kerela Journal of Ophthalmology 2009
March;11(1):25-30.
[7]. Nelson-Imoru JC, Mowatt L, Walters CA. Patterns of ocular trauma presenting to the University Hospital of the West Indies in
Jamaica. WIMJ Open 2014;1(2):45-50.
[8]. Ashaye AO. Traumatic hyphaema: A report of 472 consecutive cases. BMC Ophthalmol [serial online] 2008;8(24):1-7. Available
from http://www.biomedcentral.com/1471-2415/8/24. Accessed September 30,2016.
[9]. Al Ali AK, Al Mass D, Bener A. Poor final visual outcome after traumatic hyphema: A retrospective study of associated factors.
Journal of Emergency Trauma & Acute Care 2012;16:1-9. Available from http://dx.doi.org/10.5339/jemtac.2012.16. Accessed
October 1,2016.
[10]. Lenihan P, Hitchmoth D. Traumatic hyphaema: A teaching case report. The Journal of Optometric Education 2014;39(3):110-18.
[11]. Uhumwangho OM, Umolo OC. Traumatic hyphema in Benin City, Nigeria. Sahel Med J 2014;17:128-31.
[12]. Rahmani B, Jahadi HR, Rajaeefard A. An analysis of risk for secondary haemorrhage in traumatic hyphema. Ophthalmology
1999;106:380-85.
DOI: 10.9790/0853-1512081619 www.iosrjournals.org 17 | Page
Traumatic Hyphaema: A Case Series On Admitted Patients In RIMS Hospital, Imphal
[13]. Pai SG, Kamath SJ, DSouza S, Dudeja L. A Clinical Study of Blunt Ocular Trauma in a Tertiary Care Centre. Online J Health
Allied Scs [serial online] 2013;12(2):1-4. Available from URL: http://www.ojhas.org/issue46/2013-2-10.html. Accessed October
5,2016.
Fig 1: Grade IV hyphema
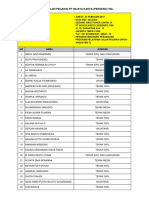
Table 1: Objects causing injury
Objects Number %
Stick 4 26.67
Badminton racket 1 6.67
Pistol 1 6.67
Stone 2 13.33
Toygun 5 33.33
Fist 1 6.67
Cricket ball 1 6.67
Table 2: Associated ocular findings with hyphema
OCULAR FINDINGS NUMBER %
Eyelid edema and 10 66.67
ecchymosis
Conj. Congestion 11 73.33
SCH 7 46.67
Conj.chemosis 4 26.67
Corneal edema 9 60
Corneal abrasion 5 33.33
Hyphema 15 100
AC reaction 15 100
Iridodialysis 5 33.33
Traumatic mydriasis 7 46.67
Lens subluxation 1 6.67
Vitreous hge 1 6.67
Macular odema 1 6.67
DOI: 10.9790/0853-1512081619 www.iosrjournals.org 18 | Page
Traumatic Hyphaema: A Case Series On Admitted Patients In RIMS Hospital, Imphal
12 73.33%
66.67%
10
No. of patients
8
6 33.33% Visual Acuity <6/18
26.67%
4 Visua Acuity 6/18
0
On Admission On Discharge
Fig 2: Visual acuity on admission and discharge in percentages
33.3
35
30 26.7 26.7
Percentage of patients
25
20
13.3 Grade of hyphema in
15
%
10
0
Grade Grade Grade Grade
1 2 3 4
Fig 3: Grades of hyphaema in percentages
DOI: 10.9790/0853-1512081619 www.iosrjournals.org 19 | Page
Anda mungkin juga menyukai
- The Diary of Anne Frank PacketDokumen24 halamanThe Diary of Anne Frank Packetcnakazaki1957Belum ada peringkat
- Modesto Mabunga Vs PP (GR 142039)Dokumen3 halamanModesto Mabunga Vs PP (GR 142039)Ericha Joy GonadanBelum ada peringkat
- Gantt Chart Engr110 - Gantt Chart Template 3Dokumen1 halamanGantt Chart Engr110 - Gantt Chart Template 3api-375485735Belum ada peringkat
- Goldenhar PDFDokumen4 halamanGoldenhar PDFDaniel FernandezBelum ada peringkat
- C++ NotesDokumen129 halamanC++ NotesNikhil Kant Saxena100% (4)
- Telegra Manual - DatasheetDokumen79 halamanTelegra Manual - DatasheetNilanjan Chakravortty100% (1)
- Traumatic Hyphema Case Series at RIMS HospitalDokumen4 halamanTraumatic Hyphema Case Series at RIMS HospitalheidyBelum ada peringkat
- Jurnal HifemaDokumen10 halamanJurnal HifemaAndi NugrohoBelum ada peringkat
- Pattern of Ocular Trauma Seen in Grarbet Hospital, Butajira, Central EthiopiaDokumen6 halamanPattern of Ocular Trauma Seen in Grarbet Hospital, Butajira, Central Ethiopiatrisya putri meliaBelum ada peringkat
- Aes 04 9Dokumen6 halamanAes 04 9Ignasius HansBelum ada peringkat
- Glaucoma After Congenital Cataract SurgeryDokumen6 halamanGlaucoma After Congenital Cataract SurgerySamawi RamudBelum ada peringkat
- Retrospective study of pediatric ocular trauma in Eastern IndiaDokumen3 halamanRetrospective study of pediatric ocular trauma in Eastern IndiamanognaaaaBelum ada peringkat
- Chemical Eye Injuries: Presentation and Management DifficultiesDokumen5 halamanChemical Eye Injuries: Presentation and Management DifficultiesMuhammad SubhanBelum ada peringkat
- International Glaucoma Association: Abebe Bejiga MDDokumen2 halamanInternational Glaucoma Association: Abebe Bejiga MDDhika KusumaBelum ada peringkat
- Pellet Gun Injury As A Source of Ocular Trauma A Retrospective Review of One Hundred and Eleven CasesDokumen6 halamanPellet Gun Injury As A Source of Ocular Trauma A Retrospective Review of One Hundred and Eleven CasesAgung Bhakti WiratamaBelum ada peringkat
- The Prevalence of Vision Impairment and Refractive Error in 3654 First Year Students at Tianjin Medical UniversityDokumen6 halamanThe Prevalence of Vision Impairment and Refractive Error in 3654 First Year Students at Tianjin Medical Universitymahvd2010Belum ada peringkat
- Jurnal Mata 1 (Corpal)Dokumen9 halamanJurnal Mata 1 (Corpal)verren natalieBelum ada peringkat
- tmp1617 TMPDokumen7 halamantmp1617 TMPFrontiersBelum ada peringkat
- Endogenous Endophthalmitis: A 9-Year Retrospective Study at A Tertiary Referral Hospital in MalaysiaDokumen17 halamanEndogenous Endophthalmitis: A 9-Year Retrospective Study at A Tertiary Referral Hospital in MalaysiaWahyudi Bambang SukocoBelum ada peringkat
- Sjams 34C1760 1764Dokumen5 halamanSjams 34C1760 1764Agung SetiawanBelum ada peringkat
- Clinical Manifestations of Ocular Toxoplasmosis in Yogyakarta, Indonesia: A Clinical Review of 173 CasesDokumen7 halamanClinical Manifestations of Ocular Toxoplasmosis in Yogyakarta, Indonesia: A Clinical Review of 173 CasesRiza Haida WardhaniBelum ada peringkat
- Dhaiban 2021Dokumen7 halamanDhaiban 2021Eric PavónBelum ada peringkat
- Relationship Between Trauma Onset and Visual AcuityDokumen6 halamanRelationship Between Trauma Onset and Visual AcuityNurlaila IshaqBelum ada peringkat
- Changes of Patterns and Outcomes of Ocular and Facial Trauma Among Children in JordanDokumen11 halamanChanges of Patterns and Outcomes of Ocular and Facial Trauma Among Children in JordanMoiz AhmedBelum ada peringkat
- Surgical Treatment of NLP Eyes Improves VisionDokumen6 halamanSurgical Treatment of NLP Eyes Improves VisionpaulpiensaBelum ada peringkat
- Intracranial Tumors: An Ophthalmic Perspective: DR M Hemanandini, DR P Sumathi, DR P A KochamiDokumen3 halamanIntracranial Tumors: An Ophthalmic Perspective: DR M Hemanandini, DR P Sumathi, DR P A Kochamiwolfang2001Belum ada peringkat
- Jurnal OftamologiDokumen6 halamanJurnal Oftamologinurul_sharaswatiBelum ada peringkat
- Retinal Detachment after Open Globe Injury Risk FactorsDokumen7 halamanRetinal Detachment after Open Globe Injury Risk FactorsRudolf Fernando WibowoBelum ada peringkat
- Correlation of Visual Field Defects and Optical Coherence Tomography Finding in Migraine PatientsDokumen5 halamanCorrelation of Visual Field Defects and Optical Coherence Tomography Finding in Migraine Patientsmara 11Belum ada peringkat
- Traumatic Hyphema Frequency and Management Evaluation A Retrospective StudyDokumen11 halamanTraumatic Hyphema Frequency and Management Evaluation A Retrospective StudyNeneng LukmanBelum ada peringkat
- P ('t':'3', 'I':'669487937') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Dokumen3 halamanP ('t':'3', 'I':'669487937') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)abdi31Belum ada peringkat
- A Study of Refractive Errors On Students of Baroda Medical CollegeDokumen2 halamanA Study of Refractive Errors On Students of Baroda Medical CollegeLopez Alvarado JheisonBelum ada peringkat
- The Epidemiology of Mandibular Fractures Treated at Chiang Mai University Hospital: A Review of 198 CasesDokumen7 halamanThe Epidemiology of Mandibular Fractures Treated at Chiang Mai University Hospital: A Review of 198 CasesMohammed TarekBelum ada peringkat
- Maxillofacial Trauma and Head Injury Risk Factors at Indonesian HospitalDokumen3 halamanMaxillofacial Trauma and Head Injury Risk Factors at Indonesian HospitalJacky JunaediBelum ada peringkat
- Resiko Jatuh GlaukomaDokumen5 halamanResiko Jatuh GlaukomayohanaBelum ada peringkat
- Amj 06 560Dokumen5 halamanAmj 06 560paulpiensaBelum ada peringkat
- LubisDokumen4 halamanLubisqaylaalainaBelum ada peringkat
- Characteristics and Surgical Outcomes of Paediatric Retinal DetachmentDokumen4 halamanCharacteristics and Surgical Outcomes of Paediatric Retinal Detachmentdrvishalkulkarni2007Belum ada peringkat
- Evaluation of Hearing Results in Otosclerotic Patients After StapedectomyDokumen5 halamanEvaluation of Hearing Results in Otosclerotic Patients After StapedectomytheffanyBelum ada peringkat
- Ruptur BulbiDokumen5 halamanRuptur BulbiseptrealtiBelum ada peringkat
- 1545-6110 - v099 - p133 RhabdomyoDokumen12 halaman1545-6110 - v099 - p133 RhabdomyoBrave RikazBelum ada peringkat
- Bmjophth 2018 000215Dokumen7 halamanBmjophth 2018 000215rahayuBelum ada peringkat
- Pattern of eye injuries in NigeriaDokumen5 halamanPattern of eye injuries in NigeriapaulpiensaBelum ada peringkat
- LUTFI-FULL PAPER-PIT 2024Dokumen6 halamanLUTFI-FULL PAPER-PIT 2024Lutfi MaulanaBelum ada peringkat
- Clinical Characteristics and Visual Outcome of Severe Ocular Chemical Injuries in Shanghai PDFDokumen5 halamanClinical Characteristics and Visual Outcome of Severe Ocular Chemical Injuries in Shanghai PDF-Yohanes Firmansyah-Belum ada peringkat
- An Examination of The Ocular Signs of Blunt Eye Injuries in A Prospective ResearchDokumen4 halamanAn Examination of The Ocular Signs of Blunt Eye Injuries in A Prospective ResearchInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Prevalence of Blindness in Patients With Uveitis: Original ResearchDokumen4 halamanPrevalence of Blindness in Patients With Uveitis: Original ResearchMuhammad RaflirBelum ada peringkat
- Management of Paediatric Traumatic Cataract by Epilenticular Intraocular Lens Implantation: Long-Term Visual Results and Postoperative ComplicationsDokumen5 halamanManagement of Paediatric Traumatic Cataract by Epilenticular Intraocular Lens Implantation: Long-Term Visual Results and Postoperative ComplicationsWahyu Tri UtomoBelum ada peringkat
- Abc 1Dokumen1 halamanAbc 1ashnagupta1571Belum ada peringkat
- Acute Concomitant Esotropia of Adulthood: Abraham Spierer, MDDokumen4 halamanAcute Concomitant Esotropia of Adulthood: Abraham Spierer, MDFarah Basotjatjo KaharBelum ada peringkat
- Diagnosis and Surgical Management of Isolated InferiorDokumen7 halamanDiagnosis and Surgical Management of Isolated InferiorKelly Herencia AnayaBelum ada peringkat
- A New Ocular Trauma Score in Pediatric Penetrating Eye InjuriesDokumen5 halamanA New Ocular Trauma Score in Pediatric Penetrating Eye InjuriespaulpiensaBelum ada peringkat
- Traumatic Hyphema: Clinical Features and DiagnosisDokumen3 halamanTraumatic Hyphema: Clinical Features and DiagnosisSheira T. TayebBelum ada peringkat
- Clinical Profile and Visual Outcome of Ocular Injuries in Tertiary Care Rural HospitalDokumen8 halamanClinical Profile and Visual Outcome of Ocular Injuries in Tertiary Care Rural HospitalIJAR JOURNALBelum ada peringkat
- Relation between onset of trauma and visual acuity in eye injury patientsDokumen6 halamanRelation between onset of trauma and visual acuity in eye injury patientsNiKomangDhanaGitaiswariBelum ada peringkat
- JOVRDokumen5 halamanJOVRkrishan bansalBelum ada peringkat
- Kjo 25 1Dokumen7 halamanKjo 25 1netifarhatiiBelum ada peringkat
- Esferofauia Aislada y GlaucomaDokumen3 halamanEsferofauia Aislada y GlaucomaManuel VasquezBelum ada peringkat
- Clinical Presentation and Microbial Analyses of Contact Lens Keratitis An Epidemiologic StudyDokumen4 halamanClinical Presentation and Microbial Analyses of Contact Lens Keratitis An Epidemiologic StudyFi NoBelum ada peringkat
- Etiology and Incidence of Zygomatic Fracture: A Retrospective Study Related To A Series of 642 PatientsDokumen4 halamanEtiology and Incidence of Zygomatic Fracture: A Retrospective Study Related To A Series of 642 Patientsstoia_sebiBelum ada peringkat
- Manejo Quirurgico de La Paralisis Del Iii ParDokumen7 halamanManejo Quirurgico de La Paralisis Del Iii ParMiguel HernandezBelum ada peringkat
- Visual Acuity Recovery Following Traumatic Hyphema in A Pediatric PopulationDokumen4 halamanVisual Acuity Recovery Following Traumatic Hyphema in A Pediatric PopulationDian Putri NingsihBelum ada peringkat
- Classification of Visual Field Abnormalities in Highly Myopic Eyes Without Pathologic ChangeDokumen26 halamanClassification of Visual Field Abnormalities in Highly Myopic Eyes Without Pathologic Change钟华Belum ada peringkat
- 2nd Article - Ferreira2005Dokumen9 halaman2nd Article - Ferreira2005Sai VyshuBelum ada peringkat
- Biophysical Properties in Glaucoma: Diagnostic TechnologiesDari EverandBiophysical Properties in Glaucoma: Diagnostic TechnologiesIngrida JanulevicieneBelum ada peringkat
- 162 BakteriDokumen13 halaman162 BakteriFiny FaradisaBelum ada peringkat
- Dehidrasi Dan SyokDokumen4 halamanDehidrasi Dan SyokBilly Shan LastKagerooboro0% (1)
- Peserta PPCP 72Dokumen2 halamanPeserta PPCP 72ocktoperryphBelum ada peringkat
- Post Op Appendectomy AssessmentDokumen11 halamanPost Op Appendectomy AssessmentFiny FaradisaBelum ada peringkat
- POMR: Problem Oriented Medical RecordDokumen1 halamanPOMR: Problem Oriented Medical RecordFiny FaradisaBelum ada peringkat
- Rubik Clock Solution 1Dokumen2 halamanRubik Clock Solution 1Ionel PaunBelum ada peringkat
- War, Rivalry An State Building in Latin AmericaDokumen16 halamanWar, Rivalry An State Building in Latin AmericaPablo Andrés Garrido GonzálezBelum ada peringkat
- Horizontal Vertical MarketDokumen4 halamanHorizontal Vertical MarketVikasBelum ada peringkat
- Product Manual 82434 (Revision C) : Generator Loading ControlDokumen26 halamanProduct Manual 82434 (Revision C) : Generator Loading ControlAUGUSTA WIBI ARDIKTABelum ada peringkat
- L P 10Dokumen13 halamanL P 10Bình Minh HoàngBelum ada peringkat
- Rethinking Classification and Localization For Object DetectionDokumen13 halamanRethinking Classification and Localization For Object DetectionShah Nawaz KhanBelum ada peringkat
- S 212 Pre Course WorkDokumen5 halamanS 212 Pre Course Workafiwierot100% (2)
- Your Results For: "Multiple-Choice Questions: B": DelayDokumen4 halamanYour Results For: "Multiple-Choice Questions: B": DelayawairmalikBelum ada peringkat
- Fictional Narrative: The Case of Alan and His FamilyDokumen4 halamanFictional Narrative: The Case of Alan and His Familydominique babisBelum ada peringkat
- APM200 Outdoor Power Supply System User Manual-20060628-B-1.0Dokumen52 halamanAPM200 Outdoor Power Supply System User Manual-20060628-B-1.0Andrés MarroquínBelum ada peringkat
- Filler SlabDokumen4 halamanFiller Slabthusiyanthanp100% (1)
- 4 Exploring Your Personality Q and Scoring Key (Transaction Analysis)Dokumen3 halaman4 Exploring Your Personality Q and Scoring Key (Transaction Analysis)Tarannum Yogesh DobriyalBelum ada peringkat
- Nutritional support through feeding tubesDokumen76 halamanNutritional support through feeding tubesKryzza LeizellBelum ada peringkat
- Loverpreet Chapterv 1Dokumen16 halamanLoverpreet Chapterv 1Sheikh SiddiquiBelum ada peringkat
- Leks Concise Guide To Trademark Law in IndonesiaDokumen16 halamanLeks Concise Guide To Trademark Law in IndonesiaRahmadhini RialiBelum ada peringkat
- Remembrance 23 Names PDFDokumen1 halamanRemembrance 23 Names PDFJennifer ThuncherBelum ada peringkat
- XYZ Company Asset Inventory ReportDokumen1 halamanXYZ Company Asset Inventory ReportNini KitsBelum ada peringkat
- PPM To Percent Conversion Calculator Number ConversionDokumen1 halamanPPM To Percent Conversion Calculator Number ConversionSata ChaimongkolsupBelum ada peringkat
- Litz Wire Termination GuideDokumen5 halamanLitz Wire Termination GuideBenjamin DoverBelum ada peringkat
- Elements of Ayurveda Daily Routine GuideDokumen1 halamanElements of Ayurveda Daily Routine GuideShivani GargBelum ada peringkat
- Turabian Sample PaperDokumen9 halamanTurabian Sample Paperemme_lopez908133% (3)
- IntuitionDokumen10 halamanIntuitionmailsonBelum ada peringkat
- Ifatsea Atsep Brochure 2019 PDFDokumen4 halamanIfatsea Atsep Brochure 2019 PDFCondor GuatonBelum ada peringkat
- Direction: Read The Questions Carefully. Write The Letters of The Correct AnswerDokumen3 halamanDirection: Read The Questions Carefully. Write The Letters of The Correct AnswerRomyross JavierBelum ada peringkat
- Template - Time in ManufacturingDokumen2 halamanTemplate - Time in ManufacturingVero RoaBelum ada peringkat