734 Full PDF
Diunggah oleh
amraovcinaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
734 Full PDF
Diunggah oleh
amraovcinaHak Cipta:
Format Tersedia
Original Article
Journal of Child Neurology
26(6) 734-737
Primary Adenosine Monophosphate (AMP) The Author(s) 2011
Reprints and permission:
sagepub.com/journalsPermissions.nav
Deaminase Deficiency in a Hypotonic DOI: 10.1177/0883073810390367
http://jcn.sagepub.com
Infant
Manuel Castro-Gago, MD1, Carmen Gomez-Lado, MD1,
Laura Perez-Gay, MD1, Jesus Eirs-Punal, MD1,
Elena Pintos Martnez, MD2, Ines Garca-Consuegra, BSc3, and
Miguel Angel Martn, PhD3
Abstract
The spectrum of the adenosine monophosphate (AMP) deaminase deficiency ranges from asymptomatic carriers to patients who
manifest exercise-induced muscle pain, occasionally rhabdomyolysis, and idiopathic hyperCKemia. However, previous to the
introduction of molecular techniques, rare cases with congenital weakness and hypotonia have also been reported. We report
a 6-month-old girl with the association of congenital muscle weakness and hypotonia, muscle deficiency of adenosine monopho-
sphate deaminase, and the homozygous C to T mutation at nucleotide 34 of the adenosine monophosphate deaminase-1 gene.
This observation indicates the possible existence of a primary adenosine monophosphate deaminase deficiency manifested by
congenital muscle weakness and hypotonia.
Keywords
adenosine monophosphate deaminase deficiency, congenital muscle weakness, hyperCKemia, muscle pain, rhabdomyolysis
Received September 9, 2010. Received revised October 14, 2010. Accepted for publication October 20, 2010.
Adenosine monophosphate (AMP) deaminase deficiency, form was genetically defined as a homozygous mutant allele.
described by Fishbein et al in 1978,1 is the most common The acquired or secondary form is defined by a single muta-
metabolic muscle disorder, with a prevalence rate of 1% to tion in 1 allele and a decrease in enzymatic activity, probably
2% in white populations.2-4 Adenosine monophosphate dea- because of its association with other diseases.2,12 A third form
minase, the most active enzyme of the purine nucleotide of adenosine monophosphate deaminase deficiency is defined
cycle, deaminates adenosine-5-monophosphate, thereby as double trouble, or coincident adenosine monophosphate
maintaining the high adenosine-5-triphosphate/-dipho- deaminase deficiency, in which genetically proven adenosine
sphate/-monophoshate ratios necessary for a high adenylate monophosphate deaminase deficiency coexists with another
charge or a high energy yield on adenosine-5-triphosphate disorder, generally a metabolic myopathy (glycogenosis V,
hydrolysis, respectively. Inosine-5-monophosphate and glycogenosis VII, partial mitochondrial enzyme defect, or
ammonia, formed by adenosine monophosphate deaminase mitochondrial DNA mutations).13-17
(AMPD), activate glycogenolysis and glycolysis. In addition,
conversion of inosine-5-monophosphate to adenosine-
5-monophosphate increases Krebs cycle mediator production 1
Servicio de Neuropediatra, Hospital Clnico Universitario, Facultad de
in active muscle. These mechanisms cannot function in ade- Medicina, Universidad de Santiago de Compostela, Santiago de Compostela,
nosine monophosphate deaminase deficiency, leading to a Spain
2
defective energy supply during work.5,6 The spectrum of this Servicio de Anatoma Patologica, Hospital Clnico Universitario, Facultad de
Medicina, Universidad de Santiago de Compostela, Santiago de Compostela,
condition ranges from asymptomatic carriers to patients who Spain
manifest exercise-induced muscle pain and occasionally rhab- 3
Laboratorio de Enfermedades Mitocondriales, Centro de Investigacion,
domyolysis,7-10 but a few cases with congenital muscle weak- Instituto de Investigacion Hospital 12 de Octubre (i + 12), Madrid. Centro
ness and hypotonia have also been reported.8,11 de Investigacion Biomedica en Red de Enfermedades Raras (CIBERER), Spain
The adenosine monophosphate deaminase gene (adenosine
Corresponding Author:
monophosphate deaminase-1) has been cloned, sequenced, Manuel Castro-Gago, MD, Servicio de Neuropediatra, Hospital Clnico
and assigned to chromosome 1p13-p21.2,4 After the introduc- Universitario, La Choupana s/n, 15706 Santiago de Compostela, Spain
tion of molecular techniques, the inherited or primary Email: manuel.castro.gago@usc.es
Downloaded from jcn.sagepub.com at Hoffmann-La Roche on September 20, 2016
Castro-Gago et al 735
Here we report an additional case, a 6-month-old girl with
clinical association of the primary form of adenosine monopho-
sphate deaminase deficiency, weakness, and hypotonia.
Case Report
A 6-month-old girl, without relevant family or personal history,
was referred for weakness and hypotonia. She was born to a
37-year-old gravida 1, following a normal pregnancy by in
vitro fertilization with sperm donation. Birth weight was
3.80 kg, and delivery was by cesarean section. Apgar scores
at 1 and 5 minutes were 6 and 10, respectively. Neonatal
screening for congenital metabolic diseases, including blood
acyl-carnitines was normal. Hypotonia was detected by the
mother during the first month of life. Clinical examination
showed macrocephaly (45.5 cm > 2 SD), severe muscle weak-
ness and hypotonia of trunk and upper limbs, and tendency to
slip through the hands when held, without muscle atrophy, and
with absence of deep tendon reflexes. Ocular movements were
normal.
Blood biochemistry, including creatine kinase, carnitine,
basal lactic acid, and pyruvic acid levels, was normal. Electro-
myogram recorded from biceps brachii, deltoids, gluteus, quad-
riceps, and anterior tibialis was myopathic with a full
recruitment pattern of reduced amplitude and polyphasic
potentials. Motor nerve conduction velocity and brain magnetic
resonance were normal. Histological examination (optic and
electron microscope) of the deltoid muscle and immunohisto-
chemistry for dystrophin, sarcoglycans (a, , g, d), a and
dytroglycans, dysferlin, utrophin, merosin, caveolin-3, col-
lagen VI, desmin, emerin, lamin A/C, myotilin, titin, teletho-
nin, and calpain-3 were normal. Histoenzymatic staining for
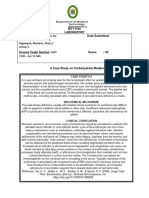
adenosine monophosphate deaminase showed loss of enzy-
Figure 1. Loss of histoenzymatic staining for adenosine
matic activity in comparison with normal muscle control monophosphate deaminase (top) in comparison with normal muscle
(Figure 1), and histoenzymatic staining for myophosphory- control (bottom).
lase, phosphofructokinase, and lactate dehydrogenase were
normal. Staining with the oxidative enzymes reduced nicoti-
namide adenine dinucleotide-tetrazolium reductase, succinate
dehydrogenase, and cytochrome oxidase was normal. The introduction, adenosine monophosphate deaminase deficiency
mitochondrial respiratory chain complexes in muscle homo- has also been noted in patients with other neuromuscular
genate and the relation in muscle of mtDNA/nDNA were nor- diseases and appears to be secondary or coincident double trou-
mal. Genetic testing showed a homozygous C to T mutation at ble, but whether it contributes to these patients symptoms is
nucleotide 34 of the adenosine monophosphate deaminase-1 not clear.2,12-17 Myalgia upon exertion was the main clinical
gene, and her mother was heterozygous for this particular symptom in 93% of primary adenosine monophosphate deami-
mutation (Figure 2). nase deficiency cases reported. Other manifestations include
At this time, 12 months after the initial clinical exploration myoglobinuria, which has been reported in a small fraction of
and diagnosis (18 months of life), she was unable to sit and patients, and occasional idiopathic hyperCKemia.9,18
muscular weakness and hypotonia of trunk and upper limbs In almost 80% of patients, the onset of the symptoms is
persist, with absence of deep tendon reflexes. noted in late childhood to the early adult years; the median age
at the time of diagnosis is 37 years, with onset as early as 12
years and as late as 76 years.18 The symptoms are usually non-
Discussion progressive and approximately one-half experience their initial
Primary adenosine monophosphate deaminase deficiency is difficulties in childhood.19
characterized by dynamic symptoms related to exertion, con- The presenting complaints in children with primary adeno-
sisting primarily of muscle aches and cramps that are some- sine monophosphate deaminase deficiency include stiffness,
times very mild and poorly defined.18 As discussed in the muscle cramps, and postexercise myalgia and weakness.18,19
Downloaded from jcn.sagepub.com at Hoffmann-La Roche on September 20, 2016
736 Journal of Child Neurology 26(6)
deaminase deficiency is not always the primary cause of
1 2 3 G symptoms in symptomatic patients.18
AATACTCACATA TCTC TTC In conclusion, our observations indicate the possible exis-
226 bp a)
200 bp tence of a primary adenosine monophosphate deaminase defi-
ciency manifested by congenital weakness and hypotonia, and
that routine histochemical analysis of adenosine monophosphate
b) deaminase should be performed in all muscle biopsies, followed
26 bp by molecular analysis in each adenosine monophosphate
deaminase-negative case.
c)
Author Contributions
MC-G, CG-L, LP-G and JE-P were responsible for the clinical diag-
Figure 2. Molecular analysis of c.34C>T (p.Q12X) mutation in the nosis and collaborated on the writing of the text. EP-M was responsible
adenosine monophosphate deaminase-1 gene. Left panel: polymerase for the histological examination of the deltoid muscle and collaborated
chain reaction (PCR) and restriction length polymorphism. Lane 1, on the writing of the text. IG-C and MAM were responsible for the
healthy control; lane 2, proband homozygous for the mutation; lane determination of the mitochondrial respiratory chain complexes in mus-
3, heterozygous probands mother. Right panel: direct sequencing in cle homogenate, the ratio in muscle of mtDNA/nDNA, and the genetic
the reverse direction of exon 2 in the adenosine monophosphate testing of the adenosine monophosphate deaminase-1 gene and collabo-
deaminase-1 genes showing (a) homozygous proband, (b) heterozy- rated on the writing of the text. MC-G was the director of the investiga-
gous patients mother, and (c) wild-type control. Electropherogram tion and was responsible for the final version of the text.
shows the mutated nucleotide position (G >A in reverse) and a mis-
matched nucleotide belonging to the forward primer (underlined).
Declaration of Conflicting Interests
The authors declared no potential conflicts of interests with respect to
Cardiomyopathy has also been described, but most of these the authorship and/or publication of this article.
patients probably have an acquired or coincidental form
of adenosine monophosphate deaminase deficiency, because Financial Disclosure/Funding
the adenosine monophosphate deaminase deficiency was pri-
The authors disclosed receipt of the following financial support for the
mary in only 1 patient with this association.6,18 The severe research and/or authorship of this article: This work was supported by
congenital muscle weakness and hypotonia observed in our a Grant from Instituto de Salud Carlos III (ISCIII), Ministry of Science
patient is an uncommon finding, reported in some rare cases and Innovation, Spain (Number PS 09-1359). IG-C is supported by a
prior to the introduction of molecular techniques.8,11,19 In this research contract from ISCIII.
sense, because the patient was homozygous for the most com-
mon mutation and other known myopathies were excluded, Ethical Approval
we think that our observation probably represents a primary
No ethical approval was necessary.
deficiency in adenosine monophosphate deaminase, without
excluding the possibility of a coincidental form of adenosine
monophosphate deaminase deficiency with an uncharacter- References
ized associated disease. 1. Fishbein WN, Armbrustmacher VM, Griffin JL. Myoadenylate
The absence of symptoms in many individuals with inher- deaminase deficiency: A new disease of muscle. Science. 1978;
ited adenosine monophosphate deaminase deficiency sug- 200:545-548.
gests a biochemical or genetic compensatory mechanism, 2. Morisaki T, Gross M, Morisaki H, Pongratz D, Zollner N,
although it is not reflected in the expression of adenosine Holmes EW. Molecular basis of AMP deaminase deficiency in ske-
monophosphate deaminase in muscle, in which a total letal muscle. Proc Natl Acad Sci U S A. 1992;89:6457-6461.
absence of the enzyme was invariably demonstrated.9,10 The 3. Norman B, Glenmark B, Jansson E. Muscle AMP deaminase defi-
hypothesis that compensatory overexpression of 2 nonmus- ciency in 2% of healthy population. Muscle Nerve. 1995;18:
cle isoforms (adenosine monophosphate deaminase-2 and 239-241.
adenosine monophosphate deaminase-3) leads to asymp- 4. Norman B, Mahnke-Zizelman DK, Vallis A, Sabina RL. Genetic
tomatic cases has been discarded, because increases in and other determinants of AMP deaminase activity in healthy adult
expression of these genes has not been demonstrated.9,18 skeletal muscle. J Appl Physiol. 1998;85:1273-1278.
Alternative splicing of exon 2 has been proposed as a possi- 5. Zollner N, Reiter S, Gross M, et al. Myoadenylate deaminase defi-
ble explanation for the absence of clinical manifestations. ciency: Successful symptomatic therapy by high dose oral admin-
However, the absence of enzyme activity in muscle biopsies istration of ribose. Klin Wochenschr. 1986;64:1281-1290.
argues against this possibility.9 Other authors have stated 6. Skyllouriotis MI, Marx M, Bittner RE, Skyllouriotis P, Gross M,
that adenosine monophosphate deaminase deficiency is not Wimmer M. Myoadenylate deaminase deficiency, hypertrophic
a disease but instead represents a harmless polymorphism,20 cardiomyopathy and gigantism syndrome. Pediatr Neurol. 1997;
and perhaps an inherited adenosine monophosphate 17:61-66.
Downloaded from jcn.sagepub.com at Hoffmann-La Roche on September 20, 2016
Castro-Gago et al 737
7. DiMauro S, Miranda AF, Hays AP, et al. Myoadenylate deaminase 14. Rubio JC, Martn MA, Bautista J, Campos Y, Segura D, Arenas J.
deficiency. Muscle biopsy and muscle culture in a patient with Association of genetically proven deficiencias of myophosphory-
gout. J Neurol Sci. 1980;47:191-202. lase and AMP deaminase: a second case of double trouble.
8. Kelemen J, Rice DR, Bradley WG, Munsat TL, DiMauro S, Neuromuscul Disord. 1997;7:387-389.
Hogan EL. Familial myoadenylate deaminase deficiency and 15. Bruno C, Minetti C, Shanske S, et al. Combined defects of muscle
exertional mylagia. Neurology. 1982;32:857-863. phosphofructokinase and AMP deaminase in a child with myoglo-
9. Teijeira S, San Millan B, Fernandez JM, et al. Myoadenylate dea- binuria. Neurology. 1998;50:296-298.
minase deficiency: clinico-pathological and molecular study of a 16. Rubio JC, Martn MA, Del Hoyo P, et al. Molecular analysis of
series of 27 Spanish cases. Clin Neuropathol. 2009;28:136-142. Spanish patients with AMP deaminase deficiency. Muscle Nerve.
10. Hanish F, Joshi P, Zierz S. AMP deaminase deficiency in skeletal 2000;23:1175-1178.
muscle is unlikely to be of clinical relevance. J Neurol. 2008;255: 17. Tsao CY, McCombo RD. Myalgia with parcial defects of mito-
318-322. chondrial enzyme and myoadenylate deaminase. Pediatr Neurol.
11. Shumate JB, Kaiser KK, Carrol JE, Brooke MH. Adenylate dea- 1999;6:65.
minase deficiency in a hypotonic infant. J Pediatr. 1980;96: 18. Darras BT. Myoadenylate deaminase deficiency. In: Jones HR Jr,
885-887. De Vivo DC, Darras BT, eds. Neuromuscular Disorders of Infancy,
12. Fishbein WN. Primary, secondary, and coincidental types of Childhood, and Adolescence. A Clinicans Approach. Amsterdam:
myoadenylate deaminase deficiency. Ann Neurol. 1999;45: Butterwordth Heinemann; 2003:861-866.
547-548. 19. Ashwal S, Peckham N. Myoadenylate deaminase deficiency in
13. Tsujino S, Shanske S, Carroll JE, Sabina RL, DiMauro S. Double children. Pediatr Neurol. 1985;1:185-191.
trouble: combined myophosphorylase and AMP deaminase defi- 20. Verzijl HT, van Engelen BG, Luyten JA, et al. Genetic character-
ciency in a child homozygous for nonsense mutations at both loci. istics of myoadenylate deaminase deficiency. Ann Neurol. 1998;
Neuromuscul Disord. 1995;5:263-266. 44:140-143.
Downloaded from jcn.sagepub.com at Hoffmann-La Roche on September 20, 2016
Anda mungkin juga menyukai
- Primary Adenosine Monophosphate (AMP) Deaminase Deficiency in A Hypotonic InfantDokumen4 halamanPrimary Adenosine Monophosphate (AMP) Deaminase Deficiency in A Hypotonic InfantamraovcinaBelum ada peringkat
- A Case of A Patient With Mucopolysaccharidosis Type IIDokumen4 halamanA Case of A Patient With Mucopolysaccharidosis Type IIAdaya HernándezBelum ada peringkat
- ParkinsonDokumen9 halamanParkinsonSOCIETE S.T.HBelum ada peringkat
- Neuroprotective Effects of Omega-3 Polyunsaturated Fatty Acids in A Rat Model of Anterior Ischemic Optic NeuropathyDokumen9 halamanNeuroprotective Effects of Omega-3 Polyunsaturated Fatty Acids in A Rat Model of Anterior Ischemic Optic NeuropathyGading AuroraBelum ada peringkat
- Neuronal Bioenergetics and Acute Mitochondrial Dysfunction A Clue To Understanding The Central Nervous System Side Effects of Efavirenz.Dokumen11 halamanNeuronal Bioenergetics and Acute Mitochondrial Dysfunction A Clue To Understanding The Central Nervous System Side Effects of Efavirenz.Roman_1988Belum ada peringkat
- Treatment and Prophylaxis of Ifosfamide-Induced Encephalopathy With Intravenous Methylene BlueDokumen2 halamanTreatment and Prophylaxis of Ifosfamide-Induced Encephalopathy With Intravenous Methylene BlueNurkholis Amin0% (1)
- Boss Ola 2009Dokumen8 halamanBoss Ola 2009nettoxsBelum ada peringkat
- Diabetes Insipida. Tratamiento NeurohipofisiarioDokumen10 halamanDiabetes Insipida. Tratamiento NeurohipofisiarioJesus OsorioBelum ada peringkat
- Pharmacogenomics Cases 1Dokumen23 halamanPharmacogenomics Cases 1Pranita BhatBelum ada peringkat
- Menzies 2015Dokumen13 halamanMenzies 2015kosikevinonuBelum ada peringkat
- Pharmacogenetics and Pharmacogenomics in Moderate-to-Severe PsoriasisDokumen14 halamanPharmacogenetics and Pharmacogenomics in Moderate-to-Severe PsoriasisDian Arief PutraBelum ada peringkat
- Treatment of Neurohypophyseal Diabetes Insipidus - Oiso YDokumen10 halamanTreatment of Neurohypophyseal Diabetes Insipidus - Oiso Yshintia novotnaBelum ada peringkat
- Involvement of MnSOD Ala16Val Polymorphism in Epilepsy A Relationship With Seizure TypeDokumen6 halamanInvolvement of MnSOD Ala16Val Polymorphism in Epilepsy A Relationship With Seizure TypeDetector BotsBelum ada peringkat
- Perspective Is Therapeutic Plasma Exchange A Viable Option For TreatingDokumen11 halamanPerspective Is Therapeutic Plasma Exchange A Viable Option For TreatingRaul Rios RitterBelum ada peringkat
- Epilepsia - 2020 - Contel - High ConcordanceDokumen16 halamanEpilepsia - 2020 - Contel - High Concordanceloherjulian6Belum ada peringkat
- Hypercalcitoninaemia in Pseudohypo-ParathyroidismDokumen5 halamanHypercalcitoninaemia in Pseudohypo-Parathyroidismradu nicolaeBelum ada peringkat
- Lysosomal Impairment in Parkinson's Disease: ReviewDokumen8 halamanLysosomal Impairment in Parkinson's Disease: ReviewRara Aulia IIBelum ada peringkat
- Advocating For Demonstration of Disease Modification - Have We Been Approaching Clinical Trials in Early Alzheimer Disease Incorrectly?Dokumen2 halamanAdvocating For Demonstration of Disease Modification - Have We Been Approaching Clinical Trials in Early Alzheimer Disease Incorrectly?Lorrane NevesBelum ada peringkat
- Spektro Uv VisDokumen7 halamanSpektro Uv VisNadaBelum ada peringkat
- A A-Degrading Enzymes: Potential For Treatment of Alzheimer DiseaseDokumen16 halamanA A-Degrading Enzymes: Potential For Treatment of Alzheimer DiseaseMinikBelum ada peringkat
- Arthritis Rheumatism - June 1987 - ValenDokumen8 halamanArthritis Rheumatism - June 1987 - ValenghfkhgfjhfgBelum ada peringkat
- Combinatorial Treatment For Spinal Muscular AtrophyDokumen4 halamanCombinatorial Treatment For Spinal Muscular AtrophymaleticjBelum ada peringkat
- The GLP-1 Analogue Lixisenatide Decreases Atherosclerosis... Diabetologia, 2017Dokumen12 halamanThe GLP-1 Analogue Lixisenatide Decreases Atherosclerosis... Diabetologia, 2017m.angela.vinueBelum ada peringkat
- Children 10 00553 v2Dokumen18 halamanChildren 10 00553 v2ilonaskorinBelum ada peringkat
- De La Rosa 2015Dokumen12 halamanDe La Rosa 2015yasmin matterBelum ada peringkat
- Not All RashesDokumen2 halamanNot All RashesDivyesh AmarsedaBelum ada peringkat
- SegawaDokumen4 halamanSegawaIngrid GomesBelum ada peringkat
- 2020 Article 80954Dokumen9 halaman2020 Article 80954Chintya Redina HapsariBelum ada peringkat
- A Homozygous Mutation in The PSMB8 Gene in A Case With Proteasome-Associated Autoinflammatory SyndromeDokumen5 halamanA Homozygous Mutation in The PSMB8 Gene in A Case With Proteasome-Associated Autoinflammatory SyndromeNidhiDesaiBelum ada peringkat
- Derosa 2010 InfDokumen5 halamanDerosa 2010 InfJuan Carlos FloresBelum ada peringkat
- Zheng 2013Dokumen10 halamanZheng 2013Aldo ValenzuelaBelum ada peringkat
- BPA 32 E13036Dokumen18 halamanBPA 32 E13036Valentina MartinezBelum ada peringkat
- 2484 FullDokumen2 halaman2484 FullRuby KumarBelum ada peringkat
- Artificially Cultivated Ophiocordyceps Sinensis AlleviatesDokumen17 halamanArtificially Cultivated Ophiocordyceps Sinensis AlleviatesHoang IceBelum ada peringkat
- Parkinson19 PDFDokumen6 halamanParkinson19 PDFLorenaBelum ada peringkat
- gft021 PDFDokumen8 halamangft021 PDFحيدر كاملBelum ada peringkat
- GFT 021Dokumen8 halamanGFT 021حيدر كاملBelum ada peringkat
- Emerging Alternative Proteinases in APP Metabolism and Alzheimer Disease Pathogenesis-A Focus On MT1-MMP and MT5-MMPDokumen19 halamanEmerging Alternative Proteinases in APP Metabolism and Alzheimer Disease Pathogenesis-A Focus On MT1-MMP and MT5-MMPRaynBelum ada peringkat
- Diabetes Insipidus - A ReviewDokumen11 halamanDiabetes Insipidus - A ReviewKelly Moreno SánchezBelum ada peringkat
- AJTR1001004Dokumen9 halamanAJTR1001004Rajesh KumarBelum ada peringkat
- Review: Irina Bancos, Stefanie Hahner, Jeremy Tomlinson, Wiebke ArltDokumen11 halamanReview: Irina Bancos, Stefanie Hahner, Jeremy Tomlinson, Wiebke Arltinterna MANADOBelum ada peringkat
- PKD BiochemistryDokumen7 halamanPKD BiochemistryHyun Jae WonBelum ada peringkat
- Fang Dietary Polyphenols Comt 2007Dokumen6 halamanFang Dietary Polyphenols Comt 2007Nufitbell NufitbellBelum ada peringkat
- AnandDokumen12 halamanAnandre septian IlhamsyahBelum ada peringkat
- Role of Matrix Metalloproteinase-9 in The Development of Diabetic Retinopathy and Its Regulation by H-RasDokumen7 halamanRole of Matrix Metalloproteinase-9 in The Development of Diabetic Retinopathy and Its Regulation by H-RasmeyvitasBelum ada peringkat
- Respuesta de Proteinas-0216Dokumen8 halamanRespuesta de Proteinas-0216Daniela HBelum ada peringkat
- Chronic Arthritis. Decreased Fibrinolytic Activity in JuvenileDokumen4 halamanChronic Arthritis. Decreased Fibrinolytic Activity in JuvenileKadek Nopy AriantyBelum ada peringkat
- Poppers-Associated Retinal Toxicity: Frank M. Sacks, M.D. Hannia Campos, PH.DDokumen3 halamanPoppers-Associated Retinal Toxicity: Frank M. Sacks, M.D. Hannia Campos, PH.DAnonymous aCbEaeDWsBelum ada peringkat
- Hypoxic Ischemic Encephalopathy: Pathophysiology and Experimental TreatmentsDokumen9 halamanHypoxic Ischemic Encephalopathy: Pathophysiology and Experimental TreatmentsAndreiMunteanuBelum ada peringkat
- "Hook Effect" in Prolactinomas Case Report and Review of LiteratureDokumen8 halaman"Hook Effect" in Prolactinomas Case Report and Review of LiteratureLinlin LiBelum ada peringkat
- Camargo 2018 (Pathology, Pathophysio, Diagnosis, Symptomps, Treatment)Dokumen6 halamanCamargo 2018 (Pathology, Pathophysio, Diagnosis, Symptomps, Treatment)Rizki Muhammad RanandaBelum ada peringkat
- KetogenikDokumen7 halamanKetogeniksari rezekiBelum ada peringkat
- Del Toro 2006Dokumen5 halamanDel Toro 2006NATALIA MARTINEZ CORDOBABelum ada peringkat
- NAP ZNDokumen9 halamanNAP ZNancuta.lupaescuBelum ada peringkat
- Alves Et Al - 2016 - Gene Therapy Strategies For Alzheimer's DiseaseDokumen8 halamanAlves Et Al - 2016 - Gene Therapy Strategies For Alzheimer's DiseaseMaria ChenBelum ada peringkat
- D-Penicillamine-induced Pemphigus Vulgaris in A Patient With Scleroderma-Rheumatoid Arthritis Overlap SyndromeDokumen2 halamanD-Penicillamine-induced Pemphigus Vulgaris in A Patient With Scleroderma-Rheumatoid Arthritis Overlap SyndromeNiken Tri HapsariBelum ada peringkat
- SMFM Abstracts: American Journal of Obstetrics & Gynecology Supplement To DECEMBER 2008Dokumen1 halamanSMFM Abstracts: American Journal of Obstetrics & Gynecology Supplement To DECEMBER 2008Pradhika Perdana SaktiBelum ada peringkat
- Kong Lee Final 1Dokumen10 halamanKong Lee Final 1api-557190611Belum ada peringkat
- Jurnal Anita HuraeraDokumen3 halamanJurnal Anita HuraeraRachmi AvillianiBelum ada peringkat
- Risgaard Et Al-2013-Clinical GeneticsDokumen7 halamanRisgaard Et Al-2013-Clinical GeneticsamraovcinaBelum ada peringkat
- Queille Et Al 2001#11710928Dokumen9 halamanQueille Et Al 2001#11710928amraovcinaBelum ada peringkat
- 5200674a PDFDokumen3 halaman5200674a PDFamraovcinaBelum ada peringkat
- JHG 200038 ADokumen2 halamanJHG 200038 AamraovcinaBelum ada peringkat
- Expanding The Phenotype of GMPPB Mutations: Doi:10.1093/brain/awv013 BRAIN 2015: 138 836-844 836Dokumen9 halamanExpanding The Phenotype of GMPPB Mutations: Doi:10.1093/brain/awv013 BRAIN 2015: 138 836-844 836amraovcinaBelum ada peringkat
- Yang - Et - Al - 2015 #26727668Dokumen8 halamanYang - Et - Al - 2015 #26727668amraovcinaBelum ada peringkat
- 734 Full PDFDokumen4 halaman734 Full PDFamraovcinaBelum ada peringkat
- Hum. Mol. Genet. 2003 Suriano 575 82Dokumen8 halamanHum. Mol. Genet. 2003 Suriano 575 82amraovcinaBelum ada peringkat
- Nihms 182954 PDFDokumen14 halamanNihms 182954 PDFamraovcinaBelum ada peringkat
- v040p00242 PDFDokumen7 halamanv040p00242 PDFamraovcinaBelum ada peringkat
- Effects of Variation at The ALDH2 Locus On Alcohol Metabolism, Sensitivity, Consumption, and Dependence in EuropeansDokumen8 halamanEffects of Variation at The ALDH2 Locus On Alcohol Metabolism, Sensitivity, Consumption, and Dependence in EuropeansamraovcinaBelum ada peringkat
- Oliveira-Et-Al-2004 #15735979Dokumen4 halamanOliveira-Et-Al-2004 #15735979amraovcinaBelum ada peringkat
- Research ArticleDokumen11 halamanResearch ArticleamraovcinaBelum ada peringkat
- Michalski - Et - Al - 2012 #22226667Dokumen8 halamanMichalski - Et - Al - 2012 #22226667amraovcinaBelum ada peringkat
- Molecular Characterization of Melanoma Cases in Denmark Suspected of Genetic PredispositionDokumen16 halamanMolecular Characterization of Melanoma Cases in Denmark Suspected of Genetic PredispositionamraovcinaBelum ada peringkat
- CDH1-related Hereditary Diffuse Gastric Cancer Syndrome: Clinical Variations and Implications For CounselingDokumen10 halamanCDH1-related Hereditary Diffuse Gastric Cancer Syndrome: Clinical Variations and Implications For CounselingamraovcinaBelum ada peringkat
- Pnas01088 0240 PDFDokumen5 halamanPnas01088 0240 PDFamraovcinaBelum ada peringkat
- NIHMS317778 Supplement Supp Figure S1 S2 Table S1 S2Dokumen6 halamanNIHMS317778 Supplement Supp Figure S1 S2 Table S1 S2amraovcinaBelum ada peringkat
- JHG 200038 ADokumen2 halamanJHG 200038 AamraovcinaBelum ada peringkat
- Nihms317778 PDFDokumen10 halamanNihms317778 PDFamraovcinaBelum ada peringkat
- Palomba 2009Dokumen10 halamanPalomba 2009amraovcinaBelum ada peringkat
- 1589 FullDokumen12 halaman1589 FullamraovcinaBelum ada peringkat
- Brain 2015 01890 File006Dokumen1 halamanBrain 2015 01890 File006amraovcinaBelum ada peringkat
- Data Supplement JCO.2014.57.8088Dokumen5 halamanData Supplement JCO.2014.57.8088amraovcinaBelum ada peringkat
- Complete OATP1B1 and OATP1B3 Deficiency Causes Human Rotor Syndrome by Interrupting Conjugated Bilirubin Reuptake Into The LiverDokumen18 halamanComplete OATP1B1 and OATP1B3 Deficiency Causes Human Rotor Syndrome by Interrupting Conjugated Bilirubin Reuptake Into The LiveramraovcinaBelum ada peringkat
- Effects of Variation at The ALDH2 Locus On Alcohol Metabolism, Sensitivity, Consumption, and Dependence in EuropeansDokumen8 halamanEffects of Variation at The ALDH2 Locus On Alcohol Metabolism, Sensitivity, Consumption, and Dependence in EuropeansamraovcinaBelum ada peringkat
- Michalski - Et - Al - 2012 #22226667Dokumen8 halamanMichalski - Et - Al - 2012 #22226667amraovcinaBelum ada peringkat
- Desmond A Et Al. - 2015 - CLinical Actionability of Multigene Panel TestingDokumen9 halamanDesmond A Et Al. - 2015 - CLinical Actionability of Multigene Panel TestingamraovcinaBelum ada peringkat
- Free Radicals and Human Health: July 2015Dokumen7 halamanFree Radicals and Human Health: July 2015mabel yapuraBelum ada peringkat
- Biocatalysis Questions and AnswersDokumen9 halamanBiocatalysis Questions and Answerskumara guruparanBelum ada peringkat
- Quality Control of Fish and Fishery ProductsDokumen35 halamanQuality Control of Fish and Fishery ProductsAndres Borrre100% (7)
- Pinho e Melo T. Heterocycles. Synthesis, Catalysis,... 2022Dokumen544 halamanPinho e Melo T. Heterocycles. Synthesis, Catalysis,... 2022YananBelum ada peringkat
- Biochem Exam4practiceCHE242summer2011Dokumen12 halamanBiochem Exam4practiceCHE242summer2011Praveen TekkaliBelum ada peringkat
- Multiple Choice Questions (MCQ) Topic Quiz Enzymes: Instructions and Answers For TeachersDokumen19 halamanMultiple Choice Questions (MCQ) Topic Quiz Enzymes: Instructions and Answers For TeachersRed VicenteBelum ada peringkat
- Ascorbic Acid in Plant Growth, Development and Stress Tolerance PDFDokumen514 halamanAscorbic Acid in Plant Growth, Development and Stress Tolerance PDFmalin.oloier100% (1)
- Enzyme Classification and Nomenclature: Sinead Boyce, Keith F TiptonDokumen11 halamanEnzyme Classification and Nomenclature: Sinead Boyce, Keith F TiptonmiminBelum ada peringkat
- 6 Microbial Production of ButanolDokumen40 halaman6 Microbial Production of Butanolhuynhthiensach100% (1)
- Biochemistry Ii Midterm ReviewDokumen4 halamanBiochemistry Ii Midterm ReviewBiology BảoBelum ada peringkat
- Babs2244 Metabolic BiochemistryDokumen24 halamanBabs2244 Metabolic BiochemistryKhAi En33% (3)
- 8 Steps Krebs+ETCDokumen3 halaman8 Steps Krebs+ETCRhianne Grace CastroBelum ada peringkat
- EAMCET Sample Paper-6 (AP Eamcet 2015 - Medical Question Paper)Dokumen30 halamanEAMCET Sample Paper-6 (AP Eamcet 2015 - Medical Question Paper)Firdosh KhanBelum ada peringkat
- CHAPTER 23 Fatty Acid CatabolismDokumen9 halamanCHAPTER 23 Fatty Acid Catabolism楊畯凱Belum ada peringkat
- Ec 1Dokumen443 halamanEc 1Chaitanya KumarBelum ada peringkat
- Biological Oxidation by SatishDokumen12 halamanBiological Oxidation by SatishBiochemistry DenBelum ada peringkat
- How Cells Harvest Chemical Energy: Biology: Concepts & ConnectionsDokumen74 halamanHow Cells Harvest Chemical Energy: Biology: Concepts & Connectionscyberbat2008Belum ada peringkat
- Classes of EnzymesDokumen33 halamanClasses of EnzymesZzeba KhanBelum ada peringkat
- Vitamin A Vitamin B1, B2, B3, B5, B6, B7, B9, B12 Vitamin C Vitamin E Vitamin D Vitamin KDokumen28 halamanVitamin A Vitamin B1, B2, B3, B5, B6, B7, B9, B12 Vitamin C Vitamin E Vitamin D Vitamin KSajanMaharjanBelum ada peringkat
- Microbial Metabolism Lecture Part ADokumen16 halamanMicrobial Metabolism Lecture Part AKashif IqbalBelum ada peringkat
- 14 Dehydrogenase in YeastDokumen4 halaman14 Dehydrogenase in Yeastsung_kei_pin100% (1)
- Chemical BiologyDokumen14 halamanChemical BiologyVaibhav MardeBelum ada peringkat
- Examination of Succinic DehydrogenationDokumen6 halamanExamination of Succinic DehydrogenationVictor Nyarugwe83% (6)
- 19 Pasos Lanosterol A ColesterolDokumen8 halaman19 Pasos Lanosterol A ColesterolmonicaBelum ada peringkat
- CC 2 Lab LU1. Introduction To EnzymologyDokumen13 halamanCC 2 Lab LU1. Introduction To EnzymologySophia Gail ChingBelum ada peringkat
- (G. Gordon Gibson, Paul Skett) Introduction To DruDokumen265 halaman(G. Gordon Gibson, Paul Skett) Introduction To DruIvone Loretta100% (1)
- Niacin: DR. Beenish Zafar BiochemistryDokumen32 halamanNiacin: DR. Beenish Zafar BiochemistryShehryar AbbasBelum ada peringkat
- Bifidobacterium Asteroides PRL2011 Genome Analysis Reveals Clues For Colonization of The Insect GutDokumen14 halamanBifidobacterium Asteroides PRL2011 Genome Analysis Reveals Clues For Colonization of The Insect Guttissue88Belum ada peringkat
- Bot 20 Ex 6Dokumen30 halamanBot 20 Ex 6Kath Valad-onBelum ada peringkat
- Acetic Acid Bacteria and Vinegar 2019Dokumen39 halamanAcetic Acid Bacteria and Vinegar 2019gustavopsoBelum ada peringkat
- The Obesity Code: Unlocking the Secrets of Weight LossDari EverandThe Obesity Code: Unlocking the Secrets of Weight LossPenilaian: 4 dari 5 bintang4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDari EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsBelum ada peringkat
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePenilaian: 2 dari 5 bintang2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDari EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDPenilaian: 5 dari 5 bintang5/5 (2)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDari EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionPenilaian: 4 dari 5 bintang4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDari EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsPenilaian: 5 dari 5 bintang5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDari EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisPenilaian: 4.5 dari 5 bintang4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 5 dari 5 bintang5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDari EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDari EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisPenilaian: 4 dari 5 bintang4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDari EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityPenilaian: 4 dari 5 bintang4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDari EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Comfort of Crows: A Backyard YearDari EverandThe Comfort of Crows: A Backyard YearPenilaian: 4.5 dari 5 bintang4.5/5 (23)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDari EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningPenilaian: 4 dari 5 bintang4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Dari EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Belum ada peringkat
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDari EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisPenilaian: 3.5 dari 5 bintang3.5/5 (2)
- Gut: the new and revised Sunday Times bestsellerDari EverandGut: the new and revised Sunday Times bestsellerPenilaian: 4 dari 5 bintang4/5 (392)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDari EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryPenilaian: 4 dari 5 bintang4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Dari EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Penilaian: 4.5 dari 5 bintang4.5/5 (110)
- The Marshmallow Test: Mastering Self-ControlDari EverandThe Marshmallow Test: Mastering Self-ControlPenilaian: 4.5 dari 5 bintang4.5/5 (58)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDari EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessPenilaian: 4.5 dari 5 bintang4.5/5 (328)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDari EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingPenilaian: 4 dari 5 bintang4/5 (1138)
- Troubled: A Memoir of Foster Care, Family, and Social ClassDari EverandTroubled: A Memoir of Foster Care, Family, and Social ClassPenilaian: 4.5 dari 5 bintang4.5/5 (27)