Sample Chapter PDF
Diunggah oleh
Alma AidhaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Sample Chapter PDF
Diunggah oleh
Alma AidhaHak Cipta:
Format Tersedia
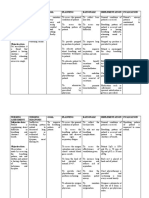
Ineffective breathing pattern 175
Ineffective Breathing Pattern Debra Siela, PhD, RN, CCNS, ACNS-BC, CCRN, CNE, RRT
NANDA-I B
Definition
Inspiration and/or expiration that does not provide adequate ventilation
Defining Characteristics
Alterations in depth of breathing; altered chest excursion; assumption of three-point position; bradypnea;
decreased expiratory pressure; decreased inspiratory pressure; decreased minute ventilation; decreased vital
capacity; dyspnea; increased anterior-posterior diameter; nasal aring; orthopnea; prolonged expiration
phase; pursed-lip breathing; tachypnea; use of accessory muscles to breathe
Related Factors (r/t)
Anxiety; body position; bony deformity; chest wall deformity; cognitive impairment; fatigue; hyperventila-
tion; hypoventilation syndrome; musculoskeletal impairment; neurological immaturity; neuromuscular
dysfunction; obesity; pain; perception impairment; respiratory muscle fatigue; spinal cord injury
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Respiratory Status: Airway Patency, Ventilation; Vital Signs
Example NOC Outcome with Indicators
Respiratory Status as evidenced by the following indicators: Respiratory rate/Respiratory rhythm/Depth of inspiration/Aus-
cultated breath sounds/Airway patency/Oxygen saturation//Ease of breathing/Vital capacity. (Rate each indicator of Respiratory
Status: 1 = severe deviation from normal range, 2 = substantial deviation from normal range, 3 = moderate deviation from
normal range, 4 = mild deviation from normal range, 5 = no deviation from normal range [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Demonstrate a breathing pattern that supports blood gas results within the clients normal parameters
Report ability to breathe comfortably
Demonstrate ability to perform pursed-lip breathing and controlled breathing
Identify and avoid specic factors that exacerbate episodes of ineffective breathing patterns
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Airway Management, Respiratory Monitoring
Example NIC ActivitiesAirway Management
Encourage slow, deep breathing; turning; and coughing; Monitor respiratory and oxygenation status as appropriate
Nursing Interventions and Rationales
Monitor respiratory rate, depth, and ease of respiration. Normal respiratory rate is 10 to 20 breaths/
min in the adult (Jarvis, 2012). EBN: When the respiratory rate exceeds 30 breaths/min, along with other
physiological measures, a study demonstrated that a signicant physiological alteration existed (Hagle,
2008).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
176 Ineffective breathing pattern
Note pattern of respiration. If client is dyspneic, note what seems to cause the dyspnea, the way in which
the client deals with the condition, and how the dyspnea resolves or gets worse.
B Note amount of anxiety associated with the dyspnea. A normal respiratory pattern is regular in a healthy
adult. To assess dyspnea, it is important to consider all of its dimensions, including antecedents, mediators,
reactions, and outcomes.
Attempt to determine if clients dyspnea is physiological or psychological in cause. EB: Maximal respira-
tory work is less unpleasant than moderately intense air hunger, and unpleasantness of dyspnea can vary
independently from perceived intensity, consistent with pain. Separate dimensions should be measured (Ban-
zett et al, 2008). A study found that when the cause was psychological (medically unexplained dyspnea), there
was affective dyspnea, anxiety, and tingling in the extremities, whereas when the dyspnea was physiological,
there was associated wheezing, cough, sputum, and palpitations (Han et al, 2008).
Psychological DyspneaHyperventilation
Monitor for symptoms of hyperventilation including rapid respiratory rate, sighing breaths, lightheadedness,
numbness and tingling of hands and feet, palpitations, and sometimes chest pain (Bickley & Szilagyi, 2009).
Assess cause of hyperventilation by asking client about current emotions and psychological state.
Ask the client to breathe with you to slow down respiratory rate. Maintain eye contact and give reassurance.
By making the client aware of respirations and giving support, the client may gain control of the breathing rate.
Consider having the client breathe in and out of a paper bag as tolerated. This simple treatment helps asso-
ciated symptoms of hyperventilation, including helping to retain carbon dioxide, which will decrease associ-
ated symptoms of hyperventilation (Bickley & Szilagyi, 2009).
If client has chronic problems with hyperventilation, numbness and tingling in extremities, dizziness, and
other signs of panic attacks, refer for counseling.
Physiological Dyspnea
Ensure that client in acute dyspneic state has received any ordered medications, oxygen, and any other
treatment needed.
Determine severity of dyspnea using a rating scale such as the modied Borg scale, rating dyspnea 0 (best)
to 10 (worst) in severity. An alternative scale is the Visual Analogue Scale (VAS) with dyspnea rated as 0
(best) to 100 (worst).
Note use of accessory muscles, nasal aring, retractions, irritability, confusion, or lethargy. These symp-
toms signal increasing respiratory difculty and increasing hypoxia.
Observe color of tongue, oral mucosa, and skin for signs of cyanosis. Cyanosis of the tongue and oral
mucosa is central cyanosis and generally represents a medical emergency. Peripheral cyanosis of nail beds or
lips may or may not be serious (Bickley & Szilagyi, 2009).
Auscultate breath sounds, noting decreased or absent sounds, crackles, or wheezes. These abnormal lung
sounds can indicate a respiratory pathology associated with an altered breathing pattern.
Monitor oxygen saturation continuously using pulse oximetry. Note blood gas results as available. An
oxygen saturation of less than 90% (normal: 95% to 100%) or a partial pressure of oxygen of less than 80 mm
Hg (normal: 80 to 100 mm Hg) indicates signicant oxygenation problems.
Using touch on the shoulder, coach the client to slow respiratory rate, demonstrating slower respirations;
making eye contact with the client; and communicating in a calm, supportive fashion. The nurses pres-
ence, reassurance, and help in controlling the clients breathing can be benecial in decreasing anxiety. CEB:
A study demonstrated that anxiety is an important indicator of severity of clients disease with chronic obstruc-
tive pulmonary disease (COPD) (Bailey, 2004).
Support the client in using pursed-lip and controlled breathing techniques. Pursed-lip breathing results in
increased use of intercostal muscles, decreased respiratory rate, increased tidal volume, and improved oxygen
saturation levels (Faager, Stahle, & Larsen, 2008). EBN: A systematic review found pursed-lip breathing effec-
tive in decreasing dyspnea (Carrieri-Kohlman & Donesky-Cuenco, 2008).
If the client is acutely dyspneic, consider having the client lean forward over a bedside table, resting elbows
on the table if tolerated. Leaning forward can help decrease dyspnea (Brennan & Mazanec, 2011), possibly
because gastric pressure allows better contraction of the diaphragm (Langer et al, 2009). This is called the tri-
pod position and is used during times of distress, including when walking.
Position the client in an upright position (Brennan & Mazanec, 2011). An upright position facilitates lung
expansion. See Nursing Interventions and Rationales for Impaired Gas Exchange for further information
on positioning.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Ineffective breathing pattern 177
Administer oxygen as ordered. Oxygen administration has been shown to correct hypoxemia which causes
dyspnea (Wong & Elliott, 2009).
Increase clients activity to walking three times per day as tolerated. Assist the client to use oxygen during
B
activity as needed. See Nursing Interventions and Rationales for Activity Intolerance. Supervised exercise
has been shown to decrease dyspnea and increase tolerance to activity (Reilly, Silverman, & Shapiro, 2012).
Schedule rest periods before and after activity. Respiratory clients with dyspnea are easily exhausted and
need additional rest.
Evaluate the clients nutritional status. Refer to a dietitian if needed. Use nutritional supplements to
increase nutritional level if needed. Improved nutrition may help increase inspiratory muscle function and
decrease dyspnea. EBN: A study found that almost half of a group of clients with COPD were malnourished,
which can lead to an exacerbation of the disease (Odencrants, Ehnfors, & Ehrenbert, 2008).
Provide small, frequent feedings. Small feedings are given to avoid compromising ventilatory effort and to con-
serve energy. Clients with dyspnea often do not eat sufcient amounts of food because their priority is breathing.
Offer a fan to move the air in the environment. EBN & EB: A systematic review found that the movement of
cool air on the face can be effective in relieving dyspnea in pulmonary clients (Carrieri-Kohlman & Donesky-
Cuenco, 2008). A study found a signicant decrease in dyspnea with use of a fan directed at the nose and
mouth (Galbraith et al, 2010)
Encourage the client to take deep breaths at prescribed intervals and do controlled coughing.
Help the client with chronic respiratory disease to evaluate dyspnea experience to determine if similar to previ-
ous incidences of dyspnea and to recognize that he or she made it through those incidences. Encourage the client
to be self-reliant if possible, use problem-solving skills, and maximize use of social support. The focus of attention
on sensations of breathlessness has an impact on judgment used to determine the intensity of the sensation.
See Ineffective Airway Clearance if client has a problem with increased respiratory secretions.
Refer the COPD client for pulmonary rehabilitation. EB: A Cochrane study found pulmonary rehabilitation
programs highly effective and safe for a client who has an exacerbation of COPD (Puhan et al, 2009).
Geriatric
Encourage ambulation as tolerated. Immobility is harmful to the elderly because it decreases ventilation and
increases stasis of secretions.
Encourage elderly clients to sit upright or stand and to avoid lying down for prolonged periods during the
day. Thoracic aging results in decreased lung expansion; an erect position fosters maximal lung expansion.
Home Care
The above interventions may be adapted for home care use.
Work with the client to determine what strategies are most helpful during times of dyspnea. Educate and
empower the client to self-manage the disease associated with impaired gas exchange. EBN & EB: A study
found that use of oxygen, self use of medication, and getting some fresh air were most helpful in dealing with
dyspnea (Thomas, 2009). Evidence-based reviews have found that self-management offers COPD clients effec-
tive options for managing the illness, leading to more positive outcomes (Kaptein et al, 2008).
Assist the client and family with identifying other factors that precipitate or exacerbate episodes of ineffec-
tive breathing patterns (i.e., stress, allergens, stairs, activities that have high energy requirements). Aware-
ness of precipitating factors helps clients avoid them and decreases risk of ineffective breathing episodes.
Assess client knowledge of and compliance with medication regimen. Client/family may need repetition of
instructions received at hospital discharge and may require reiteration as fear of a recent crisis decreases. Fear
interferes with the ability to assimilate new information.
Refer the client for telemonitoring with a pulmonologist as appropriate, with use of an electronic spirometer,
or an electronic peak owmeter. EB: A systematic review of home telemonitoring for conditions such as COPD,
asthma, and lung transplantation found that use of telemonitoring resulted in early detection of deterioration of
clients respiratory status, and positive client receptiveness to the approach (Jaana, Par, & Sicotte, 2009).
Teach the client and family the importance of maintaining the therapeutic regimen and having PRN drugs
easily accessible at all times. Appropriate and timely use of medications can decrease the risk of exacerbating
ineffective breathing.
Provide the client with emotional support in dealing with symptoms of respiratory difculty. Provide
family with support for care of a client with chronic or terminal illness. Refer to care plan for Anxiety.
Witnessing breathing difculties and facing concerns of dealing with chronic or terminal illness can create fear
in caregiver. Fear inhibits effective coping.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
178 Ineffective breathing pattern
When respiratory procedures (e.g., apneic monitoring for an infant) are being implemented, explain
equipment and procedures to family members, and provide needed emotional support. Family members
assuming responsibility for respiratory monitoring often nd this stressful. They may not have been able to
B assimilate fully any instructions provided by hospital staff.
When electrically based equipment for respiratory support is being implemented, evaluate home environ-
ment for electrical safety, proper grounding, and so forth. Ensure that notication is sent to the local
utility company, the emergency medical team, police and re departments. Notication is important to
provide for priority service.
Refer to GOLD guidelines for management of home care and indications of hospital admission criteria
(GOLD, 2011).
Support clients efforts at self-care. Ensure they have all the information they need to participate in care.
Identify an emergency plan including when to call the physician or 911. Having a ready emergency plan
reassures the client and promotes client safety.
Refer to occupational therapy for evaluation and teaching of energy conservation techniques.
Refer to home health aide services as needed to support energy conservation. Energy conservation decreases
the risk of exacerbating ineffective breathing.
Institute case management of frail elderly to support continued independent living.
Client/Family Teaching and Discharge Planning
Teach pursed-lip and controlled breathing techniques. EB: Studies have demonstrated that pursed-lip
breathing was effective in decreasing breathlessness and improving respiratory function (Faager, Stahle, &
Larsen, 2008).
Teach about dosage, actions, and side effects of medications. Inhaled steroids and bronchodilators can have
undesirable side effects, especially when taken in inappropriate doses.
Using a prerecorded CD, teach client progressive muscle relaxation techniques. EB: Relaxation therapy
can help reduce dyspnea and anxiety (Langer et al, 2009).
Teach the client to identify and avoid specic factors that exacerbate ineffective breathing patterns, such
as exposure to other sources of air pollution, especially smoking. If client smokes, refer to the smoking
cessation section in the Impaired Gas Exchange care plan.
REFERENCES
Bailey PH: The dyspnea-anxiety-dyspnea cycleCOPD patients stories Jaana M, Par G, Sicotte C: Home telemonitoring for respiratory condi-
of breathlessness, Qual Health Res 14(6):760778, 2004. tions: a systematic review, Am J Manage Care 15(5):313320, 2009.
Banzett R, et al: The affective dimension of laboratory dyspnea, Am J Jarvis C: Physical examination and health, ed 6, St. Louis, 2012,
Respir Crit Care Med 177:13841390, 2008. Saunders.
Bickley LS, Szilagyi P: Guide to physical examination, ed 10, Philadel- Kaptein AA, et al: 50 years of psychological research on patients with
phia, 2009, Lippincott. COPDroad to ruin or highway to heaven? Respir Med 103:311,
Brennan C, Mazanec P: Dyspnea management across the palliative care 2008.
continuum, J Hosp Palliat Nurs 13(3):130139, 2011. Langer D, et al: A clinical practice guideline for physiotherapists treating
Carrieri-Kohlman V, Donesky-Cuenco D: Dyspnea management. An patients with chronic obstructive pulmonary disease based on a
EBP guideline. In Ackley B et al, editors: Evidence-based nursing systematic review of available evidence, Clin Rehabil 23(5):445462,
care guidelines: medical-surgical interventions, Philadelphia, 2008, 2009.
Mosby. Odencrants S, Ehnfors M, Ehrenbert A: Nutritional status and patient
Faager G, Stahle A, Larsen FF: Inuence of spontaneous pursed lips characteristics for hospitalized older patients with chronic obstruc-
breathing on walking endurance and oxygen saturation in patients tive pulmonary disease, J Clin Nurs 17(13):17711778, 2008.
with moderate to severe chronic obstructive pulmonary disease, Puhan M, et al: Pulmonary rehabilitation following exacerbations of
Clin Rehabil 22(8):675683, 2008. chronic obstructive pulmonary disease, Cochrane Database Syst
Galbraith S, et al: Does the use of a handheld fan improve chronic Rev(1), CD005305:2009.
dyspnea? A randomized controlled, crossover trial, J Pain Symptom Reilly J, Silverman E, Shapiro S: Chronic obstructive pulmonary disease.
Manage 39(5):831838, 2010. In Longo D et al, editors: Harrisons principles of internal medicine,
GOLD: Global strategy for the diagnosis, management, and prevention of ed 18, New York, 2012, McGraw-Hill.
COPD (revised 2011), 2011, Global Initiative for Chronic Obstruc- Thomas L: Effective dyspnea management strategies identied by elders
tive Lung Disease. with end-stage chronic obstructive pulmonary disease, Appl Nurs
Hagle M: Vital signs monitoring. An EBP guideline. In Ackley B Res 22(2):7985, 2009.
et al, editors: Evidence-based nursing care guidelines: medical-surgical Wong M, Elliott M: The use of medical orders in acute care oxygen
interventions, Philadelphia, 2008, Mosby. therapy, Br J Nurs 18(8):462464, 2009.
Han J, et al: The language of medically unexplained dyspnea, Chest
133(4):961968, 2008.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Decreased cardiac output 179
Decreased Cardiac Output Maryanne Crowther, DNP, APN, CCRN
NANDA-I
Definition
C
Inadequate volume of blood pumped by the heart per minute to meet metabolic demands of the body
Defining Characteristics
Altered Heart Rate/Rhythm
Arrhythmias; bradycardia; electrocardiographic changes; palpitations; tachycardia
Altered Preload
Edema; decreased central venous pressure (CVP); decreased pulmonary artery wedge pressure (PAWP);
fatigue; increased central venous pressure (CVP); increased pulmonary artery wedge pressure (PAWP); jug-
ular vein distention; murmurs; weight gain
Altered Afterload
Clammy skin; dyspnea; decreased peripheral pulses; decreased pulmonary vascular resistance (PVR);
decreased systemic vascular resistance (SVR); increased pulmonary vascular resistance (PVR); increased sys-
temic vascular resistance (SVR); oliguria, prolonged capillary rell; skin color changes; variations in blood
pressure readings
Altered Contractility
Crackles; cough; decreased ejection fraction; decreased left ventricular stroke work index (LVSWI); decreased
stroke volume index (SVI); decreased cardiac index; decreased cardiac output; orthopnea; paroxysmal noc-
turnal dyspnea; S3 sounds; S4 sounds
Behavioral/Emotional
Anxiety; restlessness
Related Factors (r/t)
Altered heart rate; altered heart rhythm; altered stroke volume: altered preload, altered afterload, altered
contractility
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Cardiac Pump Effectiveness, Circulation Status, Tissue Perfusion: Abdominal Organs, Peripheral, Vital Signs
Example NOC Outcome with Indicators
Cardiac Pump Effectiveness as evidenced by the following indicators: Blood pressure/Heart rate/Cardiac index/Ejection
fraction/Activity tolerance/Peripheral pulses/Neck vein distention not present/Heart rhythm/Heart sounds/Angina not present/Periph-
eral edema not present/Pulmonary edema not present. (Rate the outcome and indicators of Cardiac Pump Effectiveness:
1 = severe deviation from normal range, 2 = substantial deviation from normal range, 3 = moderate deviation from normal
range, 4 = mild deviation from normal range, 5 = no deviation from normal range [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Demonstrate adequate cardiac output as evidenced by blood pressure, pulse rate and rhythm within nor-
mal parameters for client; strong peripheral pulses; maintained level of mentation, lack of chest discom-
fort or dyspnea, and adequate urinary output; an ability to tolerate activity without symptoms of dyspnea,
syncope, or chest pain
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
180 Decreased cardiac output
Remain free of side effects from the medications used to achieve adequate cardiac output
Explain actions and precautions to prevent primary or secondary cardiac disease
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
C Cardiac Care, Cardiac Care: Acute
Example NIC ActivitiesCardiac Care
Evaluate chest pain (e.g., intensity, location, radiation, duration, and precipitating and alleviating factors); Document cardiac
dysrhythmias
Nursing Interventions and Rationales
Recognize primary characteristics of decreased cardiac output as fatigue, dyspnea, edema, orthopnea,
paroxysmal nocturnal dyspnea, and increased central venous pressure. Recognize secondary characteris-
tics of decreased cardiac output as weight gain, hepatomegaly, jugular venous distention, palpitations,
lung crackles, oliguria, coughing, clammy skin, and skin color changes. EBN: A nursing study to validate
characteristics of the nursing diagnosis decreased cardiac output in a clinical environment identied and cat-
egorized related client characteristics that were present as primary or secondary (Martins, Alita, & Rabelo,
2010).
Monitor and report presence and degree of symptoms including dyspnea at rest or with reduced exercise
capacity, orthopnea, paroxysmal nocturnal dyspnea, nocturnal cough, distended abdomen, fatigue, or
weakness. Monitor and report signs including jugular vein distention, S3 gallop, rales, positive hepato-
jugular reux, ascites, laterally displaced or pronounced PMI, heart murmurs, narrow pulse pressure,
cool extremities, tachycardia with pulsus alternans, and irregular heartbeat. EB: These are symptoms and
signs consistent with heart failure (HF) and decreased cardiac output (Jessup et al, 2009). In a study of pri-
mary care clients, breathlessness during exercise, limitations in physical activity, and orthopnea were the
three most signicant symptoms most often associated with HF (Devroey & Van Casteren, 2011).
Monitor orthostatic blood pressures and daily weights. EB: These interventions assess for uid volume sta-
tus (Jessup et al, 2009). EB: The extent of volume overload is key to deciding on appropriate treatment for HF
(Lindenfeld et al, 2010).
Recognize that decreased cardiac output that can occur in a number of non-cardiac disorders such as
septic shock and hypovolemia. Expect variation in orders for differential diagnoses related to the etiology
of decreased cardiac output, as orders will be distinct to address primary cause of altered cardiac output.
EB: A study of left ventricular function in patients with septic shock identied that 60% developed reversible
left ventricular dysfunction that could successfully be hemodynamically supported with IV vasoactive medica-
tions (Vieillard-Baron et al, 2008). Obtain a thorough history. EB: It is important to assess for behaviors that
might accelerate the progression of HF symptoms such as high sodium diet, excess uid intake, or missed medi-
cation doses (Jessup et al, 2009).
Administer oxygen as needed per physicians order. Supplemental oxygen increases oxygen availability to
the myocardium. EB: Clinical practice guidelines cite that oxygen should be administered to relieve symptoms
related to hypoxemia. Supplemental oxygen at night or for exercise is not recommended unless there is concur-
rent pulmonary disease. Resting hypoxia or oxygen desaturation may indicate uid overload or concurrent
pulmonary disease (Jessup et al, 2009).
Monitor pulse oximetry regularly, using a forehead sensor if needed. CEB: In a study that compared oxygen
saturation values of arterial blood gases to various sensors, it was found that the forehead sensor was signi-
cantly better than the digit sensor for accuracy in clients with low cardiac output, while being easy to use and
not interfering with client care (Fernandez et al, 2007).
Place client in semi-Fowlers or high Fowlers position with legs down or in a position of comfort. Elevat-
ing the head of the bed and legs in down position may decrease the work of breathing and may also decrease
venous return and preload.
During acute events, ensure client remains on short-term bed rest or maintains activity level that does not
compromise cardiac output. In severe HF, restriction of activity reduces the workload of the heart (Fauci
et al, 2008).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Decreased cardiac output 181
Provide a restful environment by minimizing controllable stressors and unnecessary disturbances. Sched-
ule rest periods after meals and activities. Rest helps lower arterial pressure and reduce the workload of the
myocardium by diminishing the requirements for cardiac output (Fauci et al, 2008).
Apply graduated compression stockings or intermittent sequential pneumatic compression (ISPC) leg
sleeves as ordered. Ensure proper t by measuring accurately. Remove stocking at least twice a day, then
reapply. Assess the condition of the extremities frequently. Graduated compression stockings may be C
contraindicated in clients with peripheral arterial disease (Kahn et al, 2012). EB: A study that assessed
effects of ISPC on healthy adults found that there were signicant increases in cardiac output, stroke volume,
and ejection fraction due to increased preload and decreased afterload (Bickel et al, 2011); EBN: A study that
assessed use of knee-length graduated compression stockings found they are as effective as thigh-length gradu-
ated compression stockings. They are more comfortable for clients, are easier for staff and clients to use, pose
less risk of injury to clients, and are less expensive as recommended in this study (Hilleren-Listerud, 2009). EB:
Graduated compression stockings, alone or used in conjunction with other prevention modalities, help pro-
mote venous return and reduce the risk of deep vein thrombosis in hospitalized clients (Sachdeva et al, 2010).
Check blood pressure, pulse, and condition before administering cardiac medications such as
angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), digoxin, and
beta-blockers such as carvedilol. Notify physician if heart rate or blood pressure is low before holding
medications. It is important that the nurse evaluate how well the client is tolerating current medications
before administering cardiac medications; do not hold medications without physician input. The physician
may decide to have medications administered even though the blood pressure or pulse rate has lowered.
Observe for and report chest pain or discomfort; note location, radiation, severity, quality, duration, asso-
ciated manifestations such as nausea, indigestion, and diaphoresis; also note precipitating and relieving
factors. Chest pain/discomfort may indicate an inadequate blood supply to the heart, which can further com-
promise cardiac output. EB: Clients with decreased cardiac output may present with myocardial ischemia.
Those with myocardial ischemia may present with decreased cardiac output and HF (Jessup et al, 2009; Lin-
denfeld et al, 2010).
If chest pain is present, refer to the interventions in Risk for decreased Cardiac tissue perfusion care
plan.
Recognize the effect of sleep disordered breathing in HF. EB & CEB: A study assessing effects of OSA physi-
ology on left sided cardiac function found that the increase in negative intrathoracic pressure found in OSA led
to a decrease in left ventricular systolic performance (Orban et al, 2008). A study that assessed effectiveness of
nasal cannula oxygen supplement for nocturnal obstructive sleep apnea found that 75% of HF clients had sleep
apnea, and those who exhibited central sleep apnea had signicantly reduced episodes when wearing nasal
oxygen during sleep (Sakakibara et al, 2005). Sleep-disordered breathing, including obstructive sleep apnea
and Cheyne-Stokes with central sleep apnea, are common organic sleep disorders in clients with chronic HF
and are a poor prognostic sign associated with higher mortality (Brostrom et al, 2004).
Closely monitor uid intake, including intravenous lines. Maintain uid restriction if ordered. In clients
with decreased cardiac output, poorly functioning ventricles may not tolerate increased uid volumes.
Monitor intake and output. If client is acutely ill, measure hourly urine output and note decreases in
output. EB: Clinical practice guidelines cite that monitoring I&Os is useful for monitoring effects of diuretic
therapy (Jessup et al, 2009). Decreased cardiac output results in decreased perfusion of the kidneys, with a
resulting decrease in urine output.
Note results of electrocardiography and chest radiography. CEB: Clinical practice guidelines suggest
that chest radiography and electrocardiogram are recommended in the initial assessment of HF (Jessup et al,
2009).
Note results of diagnostic imaging studies such as echocardiogram, radionuclide imaging, or dobuta-
mine-stress echocardiography. EB: Clinical practice guidelines state that the echocardiogram is a key test in
the assessment of HF (Jessup et al, 2009).
Watch laboratory data closely, especially arterial blood gases, CBC, electrolytes including sodium, potas-
sium and magnesium, BUN, creatinine, digoxin level, and B-type natriuretic peptide (BNP assay). Rou-
tine blood work can provide insight into the etiology of HF and extent of decompensation. EB: Clinical practice
guidelines recommend that BNP or NTpro-BNP assay should be measured in clients when the cause of HF is
not known (Jessup et al, 2009). A study assessed hyponatremia as a prognostic indicator in clients with pre-
served left ventricular function and found that hyponatremia at rst hospitalization is a powerful predictor of
long-term mortality in this group (Rusinaru et al, 2009). Serum creatinine levels will elevate in clients with
severe HF because of decreased perfusion to the kidneys. Client may be receiving cardiac glycosides, and the
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
182 Decreased cardiac output
potential for toxicity is greater with hypokalemia; hypokalemia is common in heart clients because of diuretic
use (Fauci et al, 2008).
Gradually increase activity when clients condition is stabilized by encouraging slower paced activities or
shorter periods of activity with frequent rest periods following exercise prescription; observe for symp-
toms of intolerance. Take blood pressure and pulse before and after activity and note changes. Activity of
C
the cardiac client should be closely monitored. See Activity Intolerance.
Serve small, frequent, sodium-restricted, low saturated fat meals. Sodium-restricted diets help decrease
uid volume excess. Low saturated fat diets help decrease atherosclerosis, which causes coronary artery dis-
ease. Clients with cardiac disease tolerate smaller meals better because they require less cardiac output to
digest. EB: A study that compared cardiac event-free survival between clients who ingested more or less than 3
grams of dietary sodium daily found that those who were NYHA class III or IV clients beneted the most from
dietary intake less than 3 grams daily (Lennie et al, 2011); EB: A study that compared HF symptoms with
dietary sodium intake found that those with sodium intakes greater than 3 grams per day had more HF symp-
toms (Son et al, 2011). Emphasis on use of unsaturated fats and less use of saturated fats in the diet is recom-
mended to reduce cardiovascular risk. Polyunsaturates are benecial to vascular endothelial function, while
saturated fats impair vascular endothelial function (Hall et al, 2009; Willett et al, 2011).
Serve only small amounts of coffee or caffeine-containing beverages if requested (no more than four cups
per 24 hours) if no resulting dysrhythmia. CEB: A review of studies on caffeine and cardiac arrhythmias
concluded that moderate caffeine consumption does not increase the frequency or severity of cardiac arrhyth-
mias (Hogan, Hornick, & Bouchoux, 2002; Myers & Harris, 1990; Schneider, 1987).
Monitor bowel function. Provide stool softeners as ordered. Caution client not to strain when defecating.
Decreased activity, pain medication, and diuretics can cause constipation. The Valsalva maneuver which can
be elicited by straining during defecation, cough, lifting self onto the bedpan, or lifting self in bed can be harm-
ful (Moser et al, 2008).
Have clients use a commode or urinal for toileting and avoid use of a bedpan. Getting out of bed to use a
commode or urinal does not stress the heart any more than staying in bed to toilet. In addition, getting the
client out of bed minimizes complications of immobility and is often preferred by the client (Winslow, 1992).
Weigh client at same time daily (after voiding). EB: Clinical practice guidelines state that weighing at the
same time daily is useful to assess effects of diuretic therapy (Jessup et al, 2009). Use the same scale if possible
when weighing clients. Daily weight is also a good indicator of uid balance. Increased weight and severity of
symptoms can signal decreased cardiac function with retention of uids.
Provide inuenza and pneumococcal vaccines prior to discharge for those who have yet to receive them.
EB: Clinical practice guidelines and a Scientic Statement cite that HF hospitalizations are more likely during
inuenza and winter season, and that having the immunization minimizes that risk (Lindenfeld et al, 2010;
Riegel et al, 2009).
Assess for presence of anxiety and refer for treatment if present. See Nursing Interventions and Rationales
for Anxiety to facilitate reduction of anxiety in clients and family. EB: A clinical practice guideline recom-
mends that non-pharmacological techniques for stress reduction are a useful adjunct for reduction of anxiety
in HF clients (Lindenfeld et al, 2010). A study that assessed the relationship between anxiety and incidence of
death, emergency department visits, or hospitalizations found that those with higher anxiety had signicantly
worse outcomes than those with lower anxiety (De Jong et al, 2011).
Refer for treatment when depression is present. EBN: A study on combined depression and level of perceived
social support found that depressive symptoms were an independent predictor of increased morbidity and
mortality, and those with lower perceived social support had 2.1 times higher risk of events than nondepressed
clients with high perceived social support (Chung et al, 2011). A qualitative study that described experiences
of clients living with depressive symptoms found that negative thinking was present in all participants, rein-
forcing depressed mood; multiple stressors worsened depressive symptoms; and depressive symptoms were
reduced by nding activities from which to distract (Dekker et al, 2009). A study that assessed health-related
quality of life found that baseline depression along with perceived control were strongest predictors of physical
symptom status (Heo et al, 2008).
Refer to a cardiac rehabilitation program for education and monitored exercise. EB & CEB: Clients with HF
should be referred for exercise training when deemed safe, to promote exercise expectations, understanding, and
adherence (Lindenfeld et al, 2010). A systematic review of outcomes of exercise based interventions in clients
with systolic HF found that hospitalizations and those for systolic HF were reduced for clients in an exercise
program and quality of life was improved (Davies et al, 2010). In a study to assess effects of exercise in HF cli-
ents, exercise tolerance and left ventricular ejection fraction increased with exercise training (Alves et al, 2012).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Decreased cardiac output 183
Refer to HF program for education, evaluation, and guided support to increase activity and rebuild qual-
ity of life. CEB: A study assessing the 6-month outcomes of a nurse practitionercoordinated HF center found
that readmissions, length of stay, and cost per case were all signicantly reduced, while quality of life was sig-
nicantly improved (Crowther et al, 2002).
Critically Ill
Observe for symptoms of cardiogenic shock, including impaired mentation, hypotension with blood pres-
C
sure lower than 90 mm Hg, decreased peripheral pulses, cold clammy skin, signs of pulmonary conges-
tion, and decreased organ function. If present, notify physician immediately. Cardiogenic shock is a state of
circulatory failure from loss from cardiac function associated with inadequate organ perfusion with a high
mortality rate. CEB: In a study the dening characteristics of decreased cardiac output were best indicated by
decreased peripheral pulses and decreased peripheral perfusion (Oliva & Monteiro da Cruz Dde, 2003).
If shock is present, monitor hemodynamic parameters for an increase in pulmonary wedge pressure, an
increase in systemic vascular resistance, or a decrease in stroke volume, cardiac output, and cardiac index.
Hemodynamic parameters give a good indication of cardiac function (Fauci et al, 2008).
Titrate inotropic and vasoactive medications within dened parameters to maintain contractility, pre-
load, and afterload per physicians order. EB: Clinical practice guidelines recommend that intravenous ino-
tropic drugs might be reasonable for HF clients presenting with low BP and low cardiac output to maintain
systemic perfusion and preserve end-organ performance (Jessup et al, 2009). By following parameters, the
nurse ensures maintenance of a delicate balance of medications that stimulate the heart to increase contractil-
ity, while maintaining adequate perfusion of the body.
When using pulmonary arterial catheter technology, be sure to appropriately level and zero the equip-
ment, use minimal tubing, maintain system patency, perform square wave testing, position the client
appropriately, and consider correlation to respiratory and cardiac cycles when assessing waveforms and
integrating data into client assessment. EB: Clinical practice guidelines recommend that invasive hemody-
namic monitoring can be useful in acute HF with persistent symptoms when therapy is refractory, uid status
is unclear, systolic pressures are low, renal function is worsening, vasoactive agents are required, or when con-
sidering advanced device therapy or transplantation (Jessup et al, 2009).
Observe for worsening signs and symptoms of decreased cardiac output when using positive pressure
ventilation. EB: Positive pressure ventilation and mechanical ventilation are associated with a decrease in
preload and cardiac output (Lukacsovitis, Carlussi, & Hill, 2012; Yucel et al, 2011).
Recognize that clients with cardiogenic pulmonary edema may have noninvasive positive pressure venti-
lation (NPPV) ordered. EB: Clinical practice guidelines for HF state that continuous positive airway pressure
improves daily functional capacity and quality of life for those with HF and obstructive sleep apnea (Linden-
feld et al, 2010) and is reasonable for clients with refractory HF not responding to other medical therapies
(Jessup et al, 2009). A systematic review of NPPV for cardiogenic pulmonary edema found that use of NPPV
signicantly reduced mortality and intubation, while decreasing ICU stay by 1 day (Vital et al, 2009).
Monitor client for signs and symptoms of uid and electrolyte imbalance when clients are receiving ultra-
ltration or continuous renal replacement therapy (CRRT). Clients with refractory HF may have ultral-
tration or CRRT ordered as a mechanical method to remove excess uid volume. EB: Clinical practice
guidelines cite that ultraltration is reasonable for clients with refractory HF not responsive to medical therapy
(Jessup et al, 2009).
Recognize that hypoperfusion from low cardiac output can lead to altered mental status and decreased
cognition. EB & CEB: A study that assessed an association among cardiac index and neuropsychological isch-
emia found that decreased cardiac function, even with normal cardiac index, was associated with accelerated
brain aging (Jefferson et al, 2010). A study that assessed the relationship between hypoperfusion and neuropsy-
chological performance found that among stable geriatric HF clients, executive functions of sequencing and
planning were altered (Jefferson et al, 2007).
Geriatric
Recognize that elderly clients may demonstrate fatigue and depression as signs of HF and decreased car-
diac output (Lindenfeld et al, 2010).
If client has heart disease causing activity intolerance, refer for cardiac rehabilitation. EBN: A study that
assessed clients acceptance of a cardiac rehabilitation program found knowledge and perceived quality of life
had increased signicantly, and anxiety and depression had been reduced at the end of the program and at 6
month follow-up (Muschalla, Glatz, & Karger, 2011).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
184 Decreased cardiac output
Observe for syncope, dizziness, palpitations, or feelings of weakness associated with an irregular heart
rhythm. CEB & EB: Dysrhythmias, particularly atrial brillation and ventricular ectopy, and both non-
sustained and sustained ventricular tachycardia are common in clients with HF (Hunt et al, 2005; Lindenfeld
et al, 2010).
Observe for side effects from cardiac medications. The elderly have difculty with metabolism and excretion
C of medications due to decreased function of the liver and kidneys; therefore toxic side effects are more
common.
Design educational interventions specically for the elderly. EB: Many elderly HF clients have low levels of
knowledge about HF self-care and have limitations in function and cognition, low motivation, and low self-
esteem. They require skilled assessment of educational level and ability to be successful with self-care (Strm-
berg, 2005).
Home Care
Some of the above interventions may be adapted for home care use. Home care agencies may use special-
ized staff and methods to care for chronic HF clients. CEB: A study assessing HF outcomes over a 10-year
period between a multidisciplinary home care intervention and usual care found signicantly improved sur-
vival and prolonged event-free survival and was both cost- and time-effective (Ingles et al, 2006).
Continue to monitor client closely for exacerbation of HF when discharged home. CEB: Home visits and
phone contacts that emphasize client education and recognition of early symptoms of exacerbation can decrease
rehospitalization (Gorski & Johnson, 2003).
After acute hospitalization, the majority of HF clients education is performed, including social support
of others, with each session focused on assessment of current knowledge, client learning priorities, and
barriers to change (Lindenfeld et al, 2010).
Assess for signs/symptoms of cognitive impairment. EBN: Impaired cognitive function can affect 25-50% of
HF clients and is associated with poorer HF self-care. Etiology of this phenomenon may be poorer regional
blood ood to areas of the brain (Riegel et al, 2009).
Assess for fatigue and weakness frequently. Assess home environment for safety, as well as resources/
obstacles to energy conservation. Instruct client and family members on need for behavioral pacing and
energy conservation. EBN: Fatigue and weakness limit activity level and quality of life. Assistive devices and
other techniques of work simplication can help the client participate in and respond to the health care regi-
men more effectively (Quaglietti et al, 2004).
Help family adapt daily living patterns to establish life changes that will maintain improved cardiac func-
tioning in the client. Take the clients perspective into consideration and use a holistic approach in assess-
ing and responding to client planning for the future. Transition to the home setting can cause risk factors
such as inappropriate diet to reemerge.
Assist client to recognize and exercise power in using self-care management to adjust to health change.
EBN: Identied self-care behaviors, barriers to self-care, interventions to promote self-care, and evalua-
tion of effects of self-care are important to maintain the heart failure clients quality of life and functional
status and to reduce mortality from the syndrome (Riegel et al, 2009). Refer to care plan for
Powerlessness.
Explore barriers to medical regimen adherence. Review medications and treatment regularly for needed
modications. Take complaints of side effects seriously and serve as client advocate to address changes as
indicated. The presence of uncomfortable side effects frequently motivates clients to deviate from the medica-
tion regimen.
Refer for cardiac rehabilitation and strengthening exercises if client is not involved in outpatient cardiac
rehabilitation.
Refer to medical social services as necessary for counseling about the impact of severe or chronic cardiac
disease. Social workers can assist the client and family with acceptance of life changes.
Institute case management of frail elderly to support continued independent living.
As the client chooses, refer to palliative care for care, which can begin earlier in the care of the HF client.
Palliative care can be used to increase comfort and quality of life in the HF client before end-of-life care
(Buck & Zambroski, 2012).
If the clients condition warrants, refer to hospice. EB & CEB: End-of-life discussions should occur with
clients and family as end-stage heart failure becomes refractory to therapy (Hunt et al, 2005; Lindenfeld et al,
2010). The multidisciplinary hospice team can reduce hospital readmission, increase functional capacity, and
improve quality of life in end-stage HF (Coviello, Hricz, & Masulli, 2002).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Decreased cardiac output 185
Identify emergency plan in advance, including whether use of cardiopulmonary resuscitation (CPR) is
desired. Encourage family members to become certied in cardiopulmonary resuscitation if the client
desires. EB: A study that assessed the clients perspective on end-of-life care found that the three most impor-
tant issues ranked included avoidance of life support if there was no hope of survival, provider communication
and reduced family burden (Strachan et al, 2009);
Client/Family Teaching and Discharge Planning
C
Begin discharge planning as soon as possible upon admission to the emergency department (ED) with
case manager or social worker to assess home support systems and the need for community or home
health services. Consider referral for advanced practice nurse (APN) follow-up. Support services may be
needed to assist with home care, meal preparations, housekeeping, personal care, transportation to doctor
visits, or emotional support. CEB: A study to assess degree of social support as a predictor of heart failure
readmission demonstrated that those without someone living with them had a greater readmission rate in a
dose-dependent response, but no correlation to death was found (Rodriguez-Artalejo et al, 2006). Clients often
need help on discharge.
Refer to case manager or social worker to evaluate client ability to pay for prescriptions. The cost of drugs
may be a factor in lling prescriptions and adhering to a treatment plan.
Include signicant others in client teaching opportunities. Include all six areas of discharge instructions for
heart failure hospitalizations: Daily weight monitoring/reporting, symptoms recognition/reporting/when
to call for help, smoking cessation, low-sodium diet, medication use and adherence, and regular follow-up
with providers. EB: A scientic statement cites social support from family and friends as being positively associ-
ated with better medication adherence and self-care maintenance, and lower readmission rates (Riegel et al,
2009). Failure to understand and comply with educational instructions is a major cause of HF exacerbation and
hospital readmissions (Jessup et al, 2009). Clinical guidelines recommend that hospitalized heart failure clients
be given basic instructions prior to discharge to facilitate self-care and management at home (Jessup et al, 2009).
Teach importance of performing and recording daily weights upon arising for the day, and to report
weight gain. Ask if client has a scale at home; if not, assist in getting one. EB: Clinical practice guidelines
suggest that daily weight monitoring leads to early recognition of excess uid retention, which, when reported,
can be offset with additional medication to avoid hospitalization from heart failure decompensation (Jessup
et al, 2009). Daily weighing is an essential aspect of self-management. A scale is necessary. Scales vary; the cli-
ent needs to establish a baseline weight on the home scale.
Teach types and progression patterns of heart failure symptoms, when to call the physician for help, and
when to go to the hospital for urgent care. EB: Inability to recognize or adequately interpret symptom wors-
ening heart failure is common among heart failure clients. Early symptom recognition and early self-help
measures or professional evaluation and treatment lead to improved outcomes (Riegel et al, 2009).
Teach importance of smoking cessation and avoidance of alcohol intake. Help clients who smoke stop by
informing them of potential consequences and by helping them nd an effective cessation method. EB:
Smoking has vasoconstrictor and pro-inammatory properties that impede effective cardiac output. Discon-
tinuation of smoking leads to reduced adverse consequences, including decreased mortality in HF (Riegel et al,
2009). Smoking cessation advice and counsel given by nurses can be effective and should be available to clients
to help stop smoking (Rice & Stead, 2008).
Teach the direct benets of a low-sodium diet. EB: A scientic statement and clinical guidelines on heart
failure recommend a 2-3 gram/day sodium diet for most stable heart failure clients, and less when heart failure
severity warrants (Jessup et al, 2009; Lindenfeld et al, 2010; Riege et al, 2009). Sodium retention leading to
uid overload is a common cause of hospital readmission (Fauci et al, 2008).
Teach the client importance of consistently taking cardiovascular medications, and include actions, side
effects to report. EB: A scientic statement cited that adherence to medications ranges from 5% to 90%. In
one study 88% adherence was required in heart failure clients to achieve event-free survival. The study cited
as reasons for non-adherence, depression, cost, attitudes about taking medication, worrying about or feeling
side effects including those on sexual function, receipt of conicting information about medications from dif-
ferent prescribers, and lack of understanding about discharge instructions (Riegel et al, 2009). Evidence-based
guidelines state that taking medication as directed can help prevent HF decompensation, and rehospitaliza-
tion, and decrease morbidity (Jessup et al, 2009).
Instruct client and family on the importance of regular follow up care with providers. EB: Post discharge
support can signicantly reduce hospital readmissions and improve health care outcomes, quality of life, and
costs (Hernandez et al, 2010; Jessup et al, 2009).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
186 Decreased cardiac output
Teach stress reduction (e.g., imagery, controlled breathing, muscle relaxation techniques). CEB: A study
that assessed effects of relaxation or exercise in heart failure clients versus controls found that those who partici-
pated in regular relaxation therapy or exercise training reported greater improvements in psychological out-
comes, with the relaxation group signicantly improving depression and the exercise training group more
improving fatigue (Yu et al, 2007).
C Refer to an outpatient system of care. EB: Systems of care such as disease management, telemonitoring, and
telehealth promote self-care, facilitating transitions across settings (Riegel et al, 2009).
Provide client/family with advance directive information to consider. Allow client to give advance direc-
tions about medical care or designate who should make medical decisions if he or she should lose deci-
sion-making capacity. EB: Heart failure guidelines recommends that clients and families be educated about
end-of-life options prior to client decline, and with a change in clinical status (Jessup et al, 2009).
REFERENCES
Alves AJ, et al: Exercise training improves diastolic function in heart Hunt SA, et al: ACC/AHA 2005 guideline update for the diagnosis and
failure patients, Med Sci Sports Exerc 44(5):776785, 2012. management of chronic heart failure in the adult, J Am Coll Cardiol
Bickel A, et al: The physiological impact of intermittent sequential 46(6):e182, 2005.
pneumatic compression (ISPC) leg sleeves on cardiac activity, Am J Ingles SC, et al: Extending the horizon in chronic heart failure: effects
Surg 202:1522, 2011. of multidisciplinary, home-based intervention relative to usual care,
Brostrom A, et al: Sleep difculties, daytime sleepiness, and health- Circulation 114(23):24662473, 2006.
related quality of life in patients with chronic heart failure, J Cardio- Jefferson AL, et al: Systemic hypoperfusion is associated with executive
vasc Nurs 19(4):234242, 2004. dysfunction in geriatric cardiac patients, Neurobiol Aging 28(3):477
Buck HG, Zambroski CH: Upstreaming palliative care for patients with 483, 2007.
heart failure, J Cardiovasc Nurs 27(2):147153, 2012. Jefferson AL, et al: Cardiac index is associated with brain aging: the
Chung ML, et al: Depressive symptoms and poor social support have a Framingham Heart study, Circulation 122(7):690697, 2010.
synergistic effect on event-free survival in patients with heart failure, Jessup M, et al: 2009 focused update: ACCF/AHA guidelines for the
Heart Lung 40(6):492501, 2011. diagnosis and management of heart failure in adults: a report of
Coviello JS, Hricz L, Masulli PS: Client challenge: accomplishing qual- the American College of Cardiology Foundation/American Heart
ity of life in end-stage heart failure: a hospice multidisciplinary Association Task Force on Practice Guidelines: developed in
approach, Home Healthc Nurse 20:195198, 2002. collaboration with the International Society for Heart and Lung
Crowther M, et al: Evidence-based development of a hospital-based Transplantation, Circulation 119(14):19772016, 2009.
heart failure center, Reect Nurs Leadersh 28(2):3233, 2002. Kahn S, et al: Antithrombotic therapy and prevention of thrombosis, ed
Davies EJ, et al: Exercise based rehabilitation for heart failure, Cochrane 9, American College of Chest Physician Evidence-Based Clinical
Database Syst Rev(4), CD003331:2010. Practice Guidelines Online Only Articles, Chest 141(suppl 2):e195S
De Jong MJ: Linkages between anxiety and outcomes in heart failure, e226S, 2012:doi.10.1378.
Heart Lung 40(5):393404, 2011. Lennie TA, et al: Three gram sodium intake is associated with longer
Dekker RL, et al: Living with depressive symptoms: patients with heart event-free survival only in patients with advanced heart failure,
failure, Am J Crit Care 18(4):310318, 2009. J Card Fail 17(4):325330, 2011.
Devroey D, Van Casteren V: Signs for early diagnosis of heart failure in Lindenfeld J, et al: Executive summary: HFSA comprehensive heart
primary health care, Vasc Health Risk Manag 7:591596, 2011. failure practice guidelines, J Card Fail 16(6):475539, 2010.
Fauci A, et al: Harrisons principles of internal medicine, ed 17, New Lukacsovitis J, Carlussi A, Hill N: Physiological changes during low
York, 2008, McGraw-Hill. and high intensity non-invasive ventilation, Eur Respir J 39(4):869
Fernandez M, et al: Evaluation of a new pulse oximeter sensor, Am J 875, 2012.
Crit Care 16(2):146152, 2007. Martins QC, Alita G, Rabelo ER: Decreased cardiac output: clinical
Gorski LA, Johnson K: A disease management program for heart failure: validation in patients with decompensated heart failure, Int J Nurs
collaboration between a home care agency and a care management Terminol Classif 21(4):156165, 2010.
organization, Home Healthc Nurse 21(11):734, 2003. Moser DK, et al: Cardiac precautions. In Ackley B, et al, editors:
Hall WL: Dietary saturated and unsaturated fats as determinants of Evidence-based nursing care guidelines, Philadelphia, 2008, Mosby.
blood pressure and vascular function, Nutr Res Rev 22(1):1838, Muschalla B, Glatz J, Karger G: Cardiac rehabilitation with a structured
2009. education programme for patients with chronic heart failure
Heo S, et al: Predictors and effect of physical symptom status on health- illness-related knowledge, mental wellbeing and acceptance in
related quality of life in patients with heart failure, Am J Crit Care participants, Rehabilitation 50(2):103110, 2011.
17:124132, 2008. Myers MG, Harris L: High dose caffeine and ventricular arrhythmias,
Hernandez AF, et al: Relationship between early physician follow-up Can J Cardiol 6(3):9598, 1990.
and 30-day readmission among Medicare beneciaries hospitalized Oliva AP: Monteiro da Cruz Dde A: Decreased cardiac output: valida-
for heart failure, JAMA 303(17):17161722, 2010. tion with postoperative heart surgery patients, Dimens Crit Care
Hilleren-Listerud AE: Graduated compression stocking and intermit- Nurs 22(1):3944, 2003.
tent pneumatic compression device length selection, Clin Nurse Spec Orban M, et al: Dynamic changes of left ventricular performance and
23(1):2124, 2009. left atrial volume induced by the Mueller maneuver in healthy
Hogan E, Hornick B, Bouchoux A: Communicating the message: clari- young adults and implications for obstructive sleep apnea, atrial
fying the controversies about caffeine, Nutr Today 37(1):28, 2002. brillation and heart failure, Am J Cardiol 102:15571561, 2008.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Risk for decreased cardiac tissue perfusion 187
Quaglietti S, et al: Management of the patient with congestive heart Son YJ, Lee Y, Song EK: Adherence to a sodium-restricted diet is associ-
failure in the home care and palliative care setting, Ann Long Term ated with lower symptom burden and longer cardiac event-free sur-
Care 12(1):33, 2004. vival in patients with heart failure, J Clin Nurs 20(21/22):30293038,
Rice VH, Stead LF: Nursing interventions for smoking cessation, 2011.
Cochrane Database Syst Rev(2), CD001188:2008. Strachan PH, et al: Mind the gap: opportunities for improving end
Riegel B, et al: State of the science: promoting self-care in persons with of life care for patients with advanced heart failure, Can J Cardiol
heart failure: a scientic statement from the American Heart Asso-
ciation, Circulation 120:11411163, 2009.
25(11):635640, 2009.
Strmberg A: The crucial role of patient education in heart failure, Eur J
C
Rodriguez-Artalejo F, et al: Social network as a predictor of hospital Heart Fail 7(3):363369, 2005.
readmission and mortality among older patients with heart failure, Vital FMR, et al: Non-invasive positive pressure ventilation (CPAP or
J Card Fail 12(8):621627, 2006. bilevel NPPV) for cardiogenic pulmonary edema, Cochrane Data-
Rusinaru D, et al: Relation of serum sodium level to long term outcome base Syst Rev(3), 2009. CD005351.
after a rst hospitalization for heart failure with preserved ejection Willett WC, et al: The Great Fat Debate: a close look at the
fraction, Am J Cardiol 103:405410, 2009. controversyquestioning the validity of age-old dietary guidance,
Sachdeva A, et al: Elastic compression stockings for prevention of deep J Am Dietetic Assoc 11(5):655658, 2011.
vein thrombosis, Cochrane Database Syst Rev(7), CD001484:2010. Winslow EH: Panning bedpans, Am J Nurs 92:16G, 1992.
Sakakibara M, et al: Effectiveness of short-term treatment with noctur- Yu DS, et al: Non-pharmacological interventions in older people with
nal oxygen therapy for central sleep apnea in patients with conges- heart failure: effects of exercise training and relaxation therapy,
tive heart failure, J Cardiol 46(2):5361, 2005. Gerontology 53(2):7481, 2007.
Schneider JR: Effects of caffeine ingestion on heart rate, blood pressure, Yucel S, et al: Nursing diagnoses in patients having mechanical ventila-
myocardial oxygen consumption, and cardiac rhythm in acute myo- tion support in a respiratory intensive care unit in Turkey, Int J Nurs
cardial infarction patients, Heart Lung 16:167, 1987. Pract 17(5):502508, 2011.
Risk for decreased Cardiac tissue perfusion Maryanne Crowther, DNP, APN, CCRN
NANDA-I
Definition
Risk for a decrease in cardiac (coronary) circulation
Risk Factors
Hypertension; hyperlipidemia; cigarette smoking, family history of coronary artery disease; diabetes melli-
tus; alcohol and drug abuse, obesity, cardiac surgery; hypovolemia; hypoxemia; hypoxia; coronary artery
spasm; septic shock, cardiac tamponade; birth control pills, elevated C-reactive protein; lack of knowledge of
modiable risk factors (e.g., smoking, sedentary lifestyle, obesity)
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Cardiac Pump Effectiveness, Circulation Status, Tissue Perfusion: Cardiac, Tissue Perfusion: Cellular, Vital Signs
Example NOC Outcome with Indicators
Tissue Perfusion: Cardiac as evidenced by the following indicators: Angina/Arrhythmia/Tachycardia/Bradycardia/Nausea/
Vomiting/Profuse diaphoresis. (Rate the outcome and indicators of Tissue Perfusion: Cardiac: 1 = severe, 2 = substantial,
3 = moderate, 4 = mild, 5 = none [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Maintain vital signs within normal range
Retain a normal cardiac rhythm (have absence of arrhythmias, tachycardia, or bradycardia)
Be free from chest and radiated discomfort as well as associated symptoms related to acute coronary
syndromes
Deny nausea and be free of vomiting
Have skin that is dry and of normal temperature
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
188 Risk for decreased cardiac tissue perfusion
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Cardiac Care, Cardiac Precautions, Embolus Precautions, Dysrhythmia Management, Vital Signs Monitor-
C ing, Shock Management: Cardiac
Example NIC ActivityCardiac Precautions
Avoid causing intense emotional situations; Avoid overheating or chilling the client; Provide small frequent meals; Substitute artificial
salt and limit sodium intake if appropriate; Promote effective techniques for reducing stress; Restrict smoking
Nursing Interventions and Rationales
Be aware that the most common cause of acute coronary syndromes (ACS) [unstable angina (UA), non-
ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI)] is
reduced myocardial perfusion associated with partially or fully occlusive thrombus development in coro-
nary arteries (Anderson et al, 2011; Antman et al, 2008).
Assess for symptoms of coronary hypoperfusion and possible ACS including chest discomfort (pressure,
tightness, crushing, squeezing, dullness, or achiness), with or without radiation (or originating) in the
back, neck, jaw, shoulder, or arm discomfort or numbness; SOB; associated diaphoresis; dizziness, light-
headedness, loss of consciousness; nausea or vomiting with chest discomfort, heartburn or indigestion;
associated anxiety. EB: These symptoms are signs of decreased cardiac perfusion and acute coronary syndrome
such as UA, NSTEMI, or STEMI. A physical assessment will aid in assessment of the extent, location and pres-
ence of, and complications resulting from a myocardial infarction. It will promote rapid triage and treatment.
It is also important to assess if the client had a prior stroke (American Heart Association, 2011a; Anderson
et al, 2011).
Consider atypical presentations for women, and diabetic clients of ACS. EB & CEB: Women and diabetic
clients may present with atypical ndings. A systematic review of differences showed that women had signi-
cantly less chest discomfort and were more likely to present with fatigue, neck pain, syncope, nausea, right arm
pain, dizziness, and jaw pain (Coventry, Finn, & Bremner, 2011).
Review the clients medical, surgical, and social history. EB: A medical history must be concise and detailed
to determine the possibility of acute coronary syndromes, and to help determine the possible cause of cardiac
symptoms and pathology (Anderson et al, 2011).
Perform physical assessments for both CAD and non-coronary ndings related to decreased coronary
perfusion including vital signs, pulse oximetry, equal blood pressure in both arms, heart rate, respiratory
rate, and pulse oximetry. Check bilateral pulses for quality and regularity. Report tachycardia, bradycar-
dia, hypotension or hypertension, pulsus alternans or pulsus paradoxus, tachypnea, or abnormal pulse
oximetry reading. Assess cardiac rhythm for arrhythmias; skin and mucous membrane color, temperature
and dryness; and capillary rell. Assess neck veins for elevated central venous pressure, cyanosis, and
pericardial or pleural friction rub. Examine client for cardiac S4 gallop, new heart murmur, lung crackles,
altered mentation, pain to abdominal palpation, decreased bowel sounds, or decreased urinary output
EB: These indicators help to assess for cardiac and non-cardiac etiologies of symptoms and differential diagno-
ses (Anderson et al, 2011; Antman et al, 2008).
Administer oxygen as ordered and needed for clients presenting with ACS to maintain a PO2 of at least
90%. EB: Hypoxemia can be under-recognized in the rst 6 hours of ACS treatment. Maintaining a SaO2 level
of 90% or more may decrease the pain associated with myocardial ischemia by increasing the amount of oxy-
gen delivered to the myocardium (Anderson et al, 2011). EB: Advanced Cardiac Life Support guidelines rec-
ommend administering oxygen if the oxygen saturation is less than 94% (OConnor et al, 2012). A Cochrane
review found there was limited evidence to recommend use of oxygen with acute coronary syndrome, more
studies are needed (Cabello et al, 2010).
Use continuous pulse oximetry as ordered. EB: Prevention and treatment of hypoxemia includes maintain-
ing arterial oxygen saturation over 90% (Anderson et al, 2011).
Insert one or more large-bore intravenous catheters to keep the vein open. Routinely assess saline locks
for patency. Clients who come to the hospital with possible decrease in coronary perfusion or ACS may have
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Risk for decreased cardiac tissue perfusion 189
intravenous uids and medications ordered routinely or emergently to maintain or restore adequate cardiac
function and rhythm.
Observe the cardiac monitor for hemodynamically signicant arrhythmias, ST depressions or elevations,
T wave inversions and/or q waves as signs of ischemia or injury. Report abnormal ndings. EB: Arrhyth-
mias and electrocardiogram (ECG) changes indicate myocardial ischemia, injury and/or infarction (Anderson
et al, 2011; Antman et al, 2008). C
Have emergency equipment and debrillation capability nearby and be prepared to debrillate immedi-
ately if ventricular tachycardia with clinical deterioration or ventricular brillation occurs. EB: Life-
threatening ventricular arrhythmias require debrillation (Anderson et al, 2011).
Perform a 12-lead ECG as ordered, to be interpreted within 10 minutes of emergency department arrival
and during episodes of chest discomfort or angina equivalent. EB: A 12-lead ECG should be performed
within 10 minutes of emergency department arrival for all clients who are having chest discomfort. Electrocar-
diograms are used to identify the area of ischemia or injury such as ST depressions or elevations, new left
bundle branch block, T wave inversions, and/or q waves and guide treatment (Anderson et al, 2011; Antman
et al, 2008).
Administer aspirin as ordered. EB: Aspirin has been shown to prevent platelet clumping, aggregation, and
activation that leads to thrombus formation, which in coronary arteries leads to acute coronary syndromes.
Contradictions include active peptic ulcer disease, bleeding disorders, and aspirin allergy (Anderson et al,
2011; Antman et al, 2008).
Administer nitroglycerin tablets sublingually as ordered, every 5 minutes until the chest pain is resolved
while also monitoring the blood pressure for hypotension, for a maximum of three doses as ordered.
Administer nitroglycerin paste or intravenous preparations as ordered. EB: Nitroglycerin causes coronary
arterial and venous dilation, and at higher doses arterial dilation, thus reducing preload and afterload and
decreasing myocardial oxygen demand while increasing oxygen delivery (Anderson et al, 2011).
Do not administer nitroglycerin preparations to clients who have received phosphodiesterase type 5
inhibitors, such as sildenal, tadalal, or vardenal, in the last 24 hours (48 hours for long-acting prepara-
tions). EB: Synergistic effect causes marked exaggerated and prolonged vasodilation/hypotension (Anderson
et al, 2011; Antman et al, 2008).
Administer morphine intravenously as ordered every 5 to 30 minutes while monitoring blood pressure
when nitroglycerin alone does not relieve chest discomfort. EB: Morphine has potent analgesic and anti-
anxiolytic effects and causes mild reductions in blood pressure and heart rate that reduce myocardial oxygen
consumption. It increases venous capacitance in pulmonary edema associated with decreased coronary perfu-
sion and resultant myocardial dysfunction (Anderson et al, 2011; Antman et al, 2008).
Assess and report abnormal lab work results of cardiac enzymes, specically troponin Is, chemistries,
hematology, coagulation studies, arterial blood gases, nger stick blood sugar, elevated C-reactive
protein, or drug screen. Abnormalities can identify the cause of the decreased perfusion and identify
complications related to the decreased perfusion such as anemia, hypovolemia, coagulopathy, drug abuse
or hyperglycemia. Elevated cardiac enzymes are indicative of a myocardial infarction (Anderson et al,
2011).
Assess for individual risk factors for coronary artery disease, such as hypertension, dyslipidemia, cigarette
smoking, diabetes mellitus, or family history of heart disease. Other risk factors including sedentary life
style, obesity, or cocaine or amphetamine use. Note age and gender as risk factors. EB: Certain conditions
place clients at higher risk for decreased cardiac tissue perfusion (Anderson et al, 2011).
Administer additional heart medications as ordered including beta blockers, calcium channel blockers,
ACE inhibitors, aldosterone antagonists, antiplatelet agents, and anticoagulants. Always check the blood
pressure and pulse rate before administering these medications. If the blood pressure or pulse rate is low,
contact the physician to see if the medication should be held. Also check platelet counts and coagulation
studies as ordered to assess proper effects of these agents. EB: These medications are useful to optimize
cardiac function including blood pressure, heart rate, myocardial oxygen demand, intravascular uid volume
and cardiac rhythm (Anderson et al, 2011; Antman et al, 2008).
Administer lipid-lowering therapy as ordered. EB: LDL-C equal to or over 100 mg/dL requires use of LDL
lowering drug therapy to prevent progression and possibly cause regression of coronary artery plaques (Ander-
son et al, 2011). A systematic review of statin use in primary prevention of cardiovascular disease showed
reductions in all-cause mortality, major vascular events, and revascularizations (Taylor et al, 2011).
Prepare client with education, withholding meals and/or medications, and intravenous access for cardiac
catheterization and possible PCI with door to balloon time of under 90 minutes if STEMI is suspected.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
190 Risk for decreased cardiac tissue perfusion
EB & CEB: Door to balloon time of under 90 minutes was associated with improved client outcomes (Antman
et al, 2008; McNamara et al, 2006).
Prepare clients with education, withholding meals and/or medications, and intravenous access for nonin-
vasive cardiac diagnostic procedures such as 2D echocardiogram, exercise or pharmacological stress test,
and cardiac CT scan as ordered. EB: Clients suspected of decreased coronary perfusion should receive these
C diagnostic procedures as appropriate to evaluate for coronary artery disease (Anderson et al, 2011; Antman
et al, 2008).
Maintain bed rest or chair rest as ordered by the physician. EB: Anti-ischemic therapy includes minimizing
myocardial oxygen demand in the early hospital phase (Anderson et al, 2011).
For further medical and nursing interventions used in care of client with an acute coronary event, refer to
the reference by Anderson et al (2011).
Request a referral to a cardiac rehabilitation program. EB: Cardiac rehabilitation programs are designed to
limit the physiological and psychological effects of cardiac disease, reduce the risk for sudden cardiac death and
reinfarction, control symptoms and stabilize or reverse the process of plaque formation, and enhance psycho-
social and vocational status of clients (Anderson et al, 2011; Smith et al, 2011).
Geriatric
Consider atypical presentations for the elderly of possible ACS. CEB: Elderly may present with atypical
signs and symptoms such as weakness, stroke, syncope, or change in mental status (Anderson et al, 2007).
Ask the prescriber about possible reduced dosage of medications for geriatric clients considering weight
and creatinine clearance. EB: Geriatric clients have reduced pharmacokinetics including reduced muscle
mass, renal and hepatic function, and reduced volume of distribution (Anderson et al, 2011).
Consider issues such as quality of life, palliative care, end-of-life care, and differences in sociocultural
aspects for clients and families when supporting them in decisions regarding aggressiveness of care
(Anderson et al, 2011).
Client/Family Teaching and Discharge Planning
Provide information about provider follow-up. EB: Current recommendations suggest that high-risk clients
should be seen within 2 weeks and within 2 to 6 weeks for lower risk clients (Antman et al, 2008).
Teach the client and family to call 911 for symptoms of new angina, existing angina unresponsive to rest
and sublingual nitroglycerin tablets, or heart attack. Do not use friends or family for transportation where
911 is available, unless the delay is expected to be longer than 20 to 30 minutes. EB & CEB: Morbidity and
mortality from myocardial infarction can be reduced signicantly when symptoms are recognized and EMS
activated, shortening time to denitive treatment (Anderson et al, 2011).
Upon discharge, instruct clients on symptoms of ischemia, when to cease activity, when to use sublingual
nitroglycerin, and when to call 911. EB: Degree and extent of myocardial ischemia is related to duration of
time with inadequate supply of oxygen-rich blood (Anderson et al, 2011).
Teach client about any medications prescribed. Medication teaching includes the drug name, its purpose,
administration instructions such as taking it with or without food, and any side effects to be aware of. Instruct
the client to report any adverse side effects to his/her provider.
Upon hospital discharge, educate clients and signicant others about discharge medications, including
nitroglycerin sublingual tablets or spray, with written, easy to understand, culturally sensitive informa-
tion. Clients and signicant others need to be prepared to act quickly and decisively to relieve ischemic discom-
fort (Anderson et al, 2011).
Provide client teaching related to risk factors for decreased cardiac tissue perfusion, such as hypertension,
hypercholesterolemia, diabetes mellitus, tobacco use, advanced age, and gender (female). EB: Those with
two or more risk factors should have a 10-year risk screening for development of symptomatic coronary heart
disease. Client education is a vital part of nursing care for the client. Start with the clients base level of under-
standing and use that as a foundation for further education. It is important to factor in cultural and/or reli-
gious beliefs in the education provided (Anderson et al, 2011).
Instruct the client on antiplatelet and anticoagulation therapy about signs of bleeding, need for ongoing
medication compliance, and INR monitoring. EB: A review of client education literature showed a need to
prioritize education domains, standardize educational content, and deliver that content efciently (Wofford,
Wells, & Singh, 2008.)
After discharge, continue education and support for client blood pressure and diabetes control, weight
management, and resumption of physical activity. EB: Reduction of risk factors aids as secondary prevention
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Caregiver role strain 191
of coronary artery disease (Anderson et al, 2011). ATP III recommends continued efforts to optimize weight
and use of regular physical activity (National Institutes of Health, 2011).
Provide inuenza vaccine prior to discharge (Anderson et al, 2011; Antman et al, 2008).
Stress the importance of ceasing tobacco use. Tobacco use can cause or worsen decreased blood ow in the
coronaries. Effects of nicotine include increasing pulse and blood pressure and constricting of blood vessels.
Tobacco use is a primary factor in heart disease. EBN: Smoking causes vasoconstriction, which can lead to C
atherosclerotic disease (American Heart Association, 2012c; Anderson et al, 201; Smith et al, 2011).
Upon hospital discharge, educate clients about low sodium, low saturated fat diet, with consideration to
client education, literacy and health literacy level. EB: Reduction of risk factors aid as primary and secondary
prevention of coronary artery disease (Anderson et al, 2011). ATP III guidelines recommend that saturated
fats be kept to less than 7% of calories and cholesterol under 200 mg/day when LDL is above goal (http://www.
nhlbi.nih.gov/guidelines/cholesterol/index.htm). A Cochrane review recommended that there be a permanent
reduction in saturated fats and replacement with unsaturated fats to decrease atherosclerosis (Hopper et al,
2012).
Teach the importance of exercise. Exercise helps control blood pressure and weight, which are the most
important controlled risk factors for cardiovascular disease (Smith et al, 2011).
REFERENCES
American Heart Association: Heart attack symptoms and warning signs, Coventry LL, Finn J, Bremner AP: Sex differences in symptom presenta-
2011a. http://www.heart.org/HEARTORG/Conditions/Conditions_ tion in acute myocardial infarction: a systematic review and meta-
UCM_305346_SubHomePage.jsp. analysis, Heart Lung 40(6):477491, 2011.
American Heart Association: Exercise stress test, 2011b. http:// Hooper L, et al: Reduced or modied dietary fat for preventing cardio-
www.heart.org/HEARTORG/Conditions/More/CardiacRehab/ vascular disease, Cochrane Database Syst Rev(7), CD002137:2012.
Exercise-Stress-Test_UCM_307474_Article.jsp. McNamara RL, et al: Effect of door-to-balloon time on mortality in
American Heart Association. Smoking and Cardiovascular Disease patients with ST-segment elevation myocardial infarction, J Am Coll
2012 C. http://www.heart.org/HEARTORG/GettingHealthy/ Cardiol 47(11):21802186, 2006.
QuitSmoking/QuittingResources/Smoking-Cardiovascular- National Institutes of Health. Retrieved November 18, 2011, from http:
Disease_UCM_305187_Article.jsp. Accessed August 29, 2012. //www.nhlbi.nih.gov/guidelines/cholesterol/index.htm.
Anderson JL, et al: ACC/AHA 2007 guidelines for the management of OConnor R, et al: Part 10: Acute Coronary Syndromes: 2010 American
patients with unstable angina/non-ST elevation myocardial infarc- Heart Association guidelines for cardiopulmonary resuscitation and
tion, J Am Coll Cardiol 50(7):e1e157. emergency cardiovascular care, Circulation 122:S787S817, 2010.
Anderson JL, et al: 2011 ACCF/AHA focused update incorporated into Smith SC, et al: AHA/ACCF secondary prevention and risk reduction
the ACC/AHA 2007 guidelines for the management of patients with therapy for patients with coronary and other atherosclerotic vascu-
unstable angina/non-ST-elevation myocardial infarction, J Am Coll lar disease: 2011 update: a guideline from the American Heart Asso-
Cardiol 57(19):e215e330, 2011. ciation and American College of Cardiology Foundation endorsed
Antman EM, et al: 2007 Focused update of the ACC/AHA 2004 guide- by the World Heart Federation and the Preventive Cardiovascular
lines for the management of patients with ST-elevation myocardial Nurses Association, J Am Coll Cardiol 58:24322446, 2011.
infarction, J Am Coll Cardiol 51(2):210247, 2008. Taylor F, et al: Statins for the primary prevention of cardiovascular
Cabello J, et al: Oxygen therapy for acute myocardial infarction, disease, Cochrane Database Syst Rev(1), CD004816:2011.
Cochrane Database Syst Rev(6), CD007160:2010. Wofford JL, Wells MD, Singh S: Best strategies for patient education
with warfarin: a systematic review, BMC Health Serv Res 8:40, 2008.
Caregiver Role Strain Paula Sherwood, RN, PhD, CNRN, FAAN, and Barbara A. Given, PhD, RN, FAAN
NANDA-I
Definition
Difculty in performing family caregiver role
Defining Characteristics
Caregiving Activities
Apprehension about recipients care if caregiver unable to provide care; apprehension about the future
regarding care recipients health; apprehension about the future regarding caregivers ability to provide care;
apprehension about possible institutionalization of care recipient; difculty completing required tasks; dif-
culty performing required tasks; dysfunctional change in caregiving activities; preoccupation with care
routine
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
192 Caregiver role strain
Caregiver Health Status
Physical
Cardiovascular disease; diabetes; fatigue; GI upset; headaches; hypertension; rash; weight change
Behavioral
C Poor self-care behaviors; increased smoking; increased alcohol consumption; sleep disturbances
Emotional
Anger; anxiety; disturbed sleep; feeling depressed; frustration; impaired individual coping; impatience;
increased emotional lability; increased nervousness; lack of time to meet personal needs; somatization;
stress
Socioeconomic
Changes in leisure activities; low work productivity; quitting work or refusing career advancement to pro-
vide care, withdrawing from social life; nancial distress including, but not limited to, poverty and
bankruptcy
CaregiverCare Recipient Relationship
Difculty watching care recipient go through the illness; grief regarding changed relationship with care recip-
ient; uncertainty regarding changed relationship with care recipient
Family Processes
Concerns about family members; family conict; family cohesion; family dysfunction
Related Factors (r/t)
Care Recipient Health Status
Addiction; codependence; cognitive problems; dependency; illness chronicity; illness severity; increasing
care needs; instability of care recipients health; problem behaviors; psychological problems; unpredictability
of illness course
Caregiver Health Status
Addiction; codependency; cognitive problems; inability to fulll ones own expectations; inability to fulll
others expectations; marginal coping patterns; physical problems; psychological problems; unrealistic
expectations of self
CaregiverCare Recipient Relationship
History of poor relationship; mental status of elder inhibiting conversation, presence of abuse or violence;
unrealistic expectations of caregiver by care recipient
Caregiving Activities
24-hour care responsibilities; amount of activities (including number of hours and specic activities that are
distressful); complexity of activities; discharge of family members to home with signicant care needs; ongo-
ing changes in activities; unpredictability of care situation; years of caregiving
Family Processes
History of family dysfunction; history of marginal family coping
Resources
Caregiver is not developmentally ready for caregiver role; decient knowledge about community resources;
difculty accessing community resources; emotional strength; formal assistance; formal support; inadequate
community resources (e.g., respite services, recreational resources); inadequate equipment for providing
care; inadequate physical environment for providing care (e.g., housing, temperature, safety); inadequate
transportation; inexperience with caregiving; informal assistance; informal support; insufcient nances;
insufcient time; lack of caregiver privacy; lack of support; physical energy
Socioeconomic
Alienation from others; competing role commitments; insufcient recreation; isolation from others; nan-
cial distress including potential loss of loss of home and savings
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Caregiver role strain 193
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Caregiver Adaptation to Patient Institutionalization, Caregiver Emotional Health, Caregiver Home Care
Readiness, Caregiver Lifestyle Disruption, Caregiver-Patient Relationship, Caregiver Performance: Direct
Care, Caregiver Performance: Indirect Care, Caregiver Physical Health, Caregiver Role Support, Caregiver
C
Role Endurance, Caregiver Stressors, Caregiver Well-Being
Example NOC Outcome with Indicators
Caregiver Emotional Health with plans for a positive future as evidenced by the following indicators: Satisfaction with
life/Sense of control/Self-esteem/Perceived social connectedness/Perceived spiritual well-being. (Rate the outcome and indicators of
Caregiver Emotional Health: 1 = severely compromised, 2 = substantially compromised, 3 = moderately compromised,
4 = mildly compromised, 5 = not compromised [see Section I].)
Client Outcomes
Throughout the care situation, the caregiver will:
Feel supported by health care professionals, family, and friends
Report reduced or acceptable feelings of burden or distress
Take part in self-care activities to maintain own physical and psychological/emotional health
Identify resources available to help in giving care or to support the caregiver to give care
Verbalize mastery of the care situation; feel condent and competent to provide care
Throughout the care situation, the care recipient will:
Obtain quality and safe care
NIC (Nursing Interventions Classification)
Suggested NIC Intervention
Caregiver Support
Example NIC ActivitiesCaregiver Support
Determine caregivers acceptance of role; Accept expressions of negative emotion
Nursing Interventions and Rationales
Regularly monitor signs of depression, anxiety, burden, and deteriorating physical health in the caregiver
throughout the care situation, especially if the marital relationship is poor, the care recipient has cognitive
or neuropsychiatric symptoms, there is little social support available, the caregiver becomes enmeshed in
the care situation, the caregiver is elderly, female, or has poor preexisting physical or emotional health.
Refer to the care plan for Hopelessness when appropriate. EBN: The incidence of depression in family
caregivers can be higher than that of the patient with chronic illness (Williams & McCorkle, 2011). EB: Care-
giving may weaken the immune system and predispose the caregiver to illness, particularly cardiac illness and
poor response to acquired infections in some situations (Gallagher et al, 2008; Gouin, Hantsoo, & Kiecolt-
Glaser, 2008; Lovell, Moss, & Wetherell, 2012). Particular subgroups have been shown to be at high risk for
becoming distressed as a result of providing care (Schoenmakers, Buntinx, & Delepeleire, 2010).
The impact of providing care on the caregivers emotional health should be assessed at regular intervals
using a reliable and valid instrument such as the Caregiver Strain Index, Caregiver Burden Inventory,
Caregiver Reaction Assessment, Screen for Caregiver Burden, and the Subjective and Objective Burden
Scale (Deeken et al, 2003; Vitaliano et al, 1991). CEB & EBN: Research has validated the effectiveness of
a number of evaluation tools for caregiver stress, including the Caregiver Reaction Assessment (Given et al,
1992), Burden Interview (Zarit et al, 1980), the Caregiver Strain Index (Robinson, 1983), and the
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
194 Caregiver role strain
Caregiver Burden Inventory (Novak & Guest, 1989). Caregiver assessment tools should be multidimen-
sional and evaluate the impact of providing care on multiple aspects of the caregivers life (Hudson &
Hayman-White, 2006).
Identify potential caregiver resources such as mastery, social support, optimism, and positive aspects of
care. EB & EBN: Research has shown that caregivers can have simultaneous positive and negative responses to
C providing care. Positive responses may help to buffer the negative effects of providing care on caregivers emo-
tional health and may also increase the effectiveness of interventions to reduce strain (Kruithof, Visser-Meily, &
Post, 2011).
Screen for caregiver role strain at the onset of the care situation, at regular intervals throughout the care
situation, and with changes in care recipient status and care transitions, including institutionalization.
EB & EBN: Care situations that last for several months or years can cause wear and tear that exhaust caregiv-
ers coping mechanisms and available resources and that may continue after the care recipient has been insti-
tutionalized (Paun & Farran, 2011). In addition, changes in the care recipients health status necessitate new
skills and monitoring from the caregiver and affect the caregivers ability to continue to provide care (Given,
Sherwood, & Given, 2011). Providing caregiver support throughout the care situation may decrease care recip-
ient institutionalization (Matsuzawa, 2011).
Watch for caregivers who become enmeshed in the care situation. EBN: Caregivers are at risk for becoming
overinvolved or unable to disentangle themselves from the caregiver role, particularly in the absence of ade-
quate social support (Hricik et al, 2011).
Arrange for intervals of respite care for the caregiver; encourage use if available. EB & EBN: Respite care
provides time away from the care situation and can help alleviate distress (Beeber, Thorpe, & Clipp, 2008;
Sussman & Regehr, 2009).
Regularly monitor social support for the caregiver and help the caregiver to identify and utilize appropri-
ate support systems for varying times in the care situation. EBN: Lower levels of perceived support can cause
caregivers to feel abandoned and increase their distress (Hwang et al, 2011).
Encourage the caregiver to grieve over changes in the care recipients condition and give the caregiver
permission to share angry feelings in a safe environment. Refer to nursing interventions for Grieving. EB:
Caregivers grieve the loss of personhood of their loved one, especially when dementia is involved (Holland,
Currier, & Gallgher-Thompson, 2009; Kramer et al, 2011).
Help the caregiver nd personal time to meet his or her needs, learn stress management techniques,
schedule regular health screenings, and schedule regular respite time. EB: Due to increased risk for poor
physical health as a result of providing care, caregivers must feel empowered to maintain self-care activities
(Merluzzi et al, 2011). Interventions to provide support for family caregivers have shown improvements in
caregiver health (Elliot, Burgio, & Decoster, 2010).
Encourage the caregiver to talk about feelings, concerns, uncertainties, and fears. Support groups can be
used to gain mutual and educational support. EBN: Support groups can improve depressive symptoms and
burden, particularly for female caregivers (Chien et al, 2011). EB: Social support groups can be effective over
the Internet, using forums such as Facebook (Bender, Jimenez-Marroquin, & Jadad, 2011).
Observe for any evidence of caregiver or care recipient violence or abuse, particularly verbal abuse; if
evidence is present, speak with the caregiver and care recipient separately. EB & CEB: Caregiver violence is
possible, particularly when the caregiver has a history of behavioral, emotional, or family problems; screening
should be done at regular intervals (Cohen et al, 2006; Cooper et al, 2009).
Involve the family in care transitions; use a multidisciplinary team to provide medical and social services
for instruction and planning. EBN: Caregivers who reported involvement in discharge planning, particularly
when discharge planning was done by an interdisciplinary team, occurs well before discharge, and includes
good communication between the family member and the health care team, report better acceptance of the
caregiving role and better health (Bauer et al, 2009).
Encourage regular communication with the care recipient and with the health care team. EB: Caregivers
preferential communication method and communication needs should be addressed at regular intervals to
improve their sense of mastery over the care situation (Moore, 2008). There can be a large discrepancy between
what the health care professional feels s/he has communicated and what the caregiver reports hearing (Molin-
uevo, Hernandez & TRACE, 2011).
Help caregiver assess his or her nancial resources (services reimbursed by insurance, available support
through community and religious organizations) and the impact of providing care on his or her nancial
status. EB & EBN: Low incomes and limited nancial resources can cause strain for the caregiver, particularly
if there are substantial out-of-pocket costs involved in providing care (Siefert et al, 2008). Prolonged
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Caregiver role strain 195
care situations can affect nancial resources; assessment of nancial distress/strain should occur at regular
intervals. Caregivers report needing information regarding nancial assistance during the care situation (Sin-
clair et al, 2010).
Help the caregiver identify competing occupational demands and potential benets to maintaining work
as a way of providing normalcy. Guide caregivers to seek ways to maintain employment through mecha-
nisms such as job sharing or decreasing hours at work. EB: Employed caregivers report that work can pro- C
vide a sense of fulllment, refuge, and satisfaction (Eldh & Carlsson, 2011).
Help the caregiver problem solve to meet the care recipients needs. EBN: Using a psycho-educational or
problem-solving intervention can decrease caregiver feelings of strain, although it has not been shown to help
with caregivers depressive symptoms (Northouse et al, 2010).
Geriatric
Monitor the caregiver for psychological distress and signs of depression, especially if caring for a mentally
impaired elder or if there was an unsatisfactory marital relationship before caregiving. EBN: As the major-
ity of family caregivers are spouses, degree of marital satisfaction is strongly linked with caregiver role strain
(Green & King, 2011).
Assess the health of caregivers, particularly their control over chronic diseases, at regular intervals. CEB:
Caregivers who report feeling burdened have an increased risk of mortality, risk that may be particularly high
in elderly caregivers with comorbid conditions (Beach et al, 2000; Schulz & Beach, 1999).
Assess the presence of and use of social support and encourage the use of secondary caregivers with elderly
caregivers. EBN: Caregivers are at risk for becoming overinvolved or unable to disentangle themselves from the
caregiver role, particularly in the absence of adequate social support (Hricik et al, 2011).
To improve the ability to provide safe care: provide skills training related to direct care, perform complex
monitoring tasks, supervise and interpret client symptoms, assist with decision-making, assist with medi-
cation adherence, provide emotional support and comfort, and coordinate care. CEB: Each task demands
different skills and knowledge, organizational capacities, role demands, and social and psychological strengths
from family members (Schumacher et al, 2000).
Teach symptom management techniques (assessment, potential causes, aggravating factors, potential
alleviating factors, reassessment), particularly for fatigue, constipation, anorexia, and pain. EBN: Caregiv-
ers require training in care recipient monitoring symptom management, and interpretation and can benet
from a problem-solving approach (Sherwood et al, 2012).
Multicultural
Assess for the inuence of cultural beliefs, norms, and values on the clients ability to modify health
behavior. EBN: What the client considers normal and abnormal health behavior may be based on cultural
perceptions (Giger & Davidhizar, 2008). EBN: Each client should be assessed for ability to modify health
behavior based on the phenomenon of communication, time, space, social organization, environmental con-
trol, and biological variations (Giger & Davidhizar, 2008).
Despite the importance of cultural differences in perceptions of caregiver role strain, there are certain
characteristics that are distressing to caregivers across multiple cultures. EBN: Social support and care
recipients behavioral difference have been shown to be an important factor in caregiver distress across multiple
cultures (Chiao & Schepp, 2012; Hwang et al, 2011; Zahid & Ohaeri, 2010).
Persons with different cultural backgrounds may not perceive the provision of care with equal degrees of
distress. EB: A group of caregivers in Belize did not report providing care as negative, although they did exhibit
physical symptoms of distress (Vroman & Morency, 2011).
Recognize that cultures often play a role in identifying who will be recognized as a family caregiver and
form partnerships with those groups. EB: In a study of American Indians, people who attended and partici-
pated in Native events and endorsed traditional healing practices were more likely to be caregivers. The study
also reported that gender played a role in identifying caregivers in some tribes, but not all (Goins, 2011).
Encourage spirituality as a source of support for coping. EBN: Many African Americans and Latinos iden-
tify spirituality, religiousness, prayer, and church-based approaches as coping resources. Socioeconomic status,
geographical location, and risks associated with health-seeking behavior all inuence the likelihood that clients
will seek health care and modify health behavior (Giger & Davidhizar, 2008).
Assess for the presence of conicting values within the culture. EBN: Whereas sharing and caring is part of
the Amish community, females with breast cancer were found to value privacy issues related to their body
image and health status and to prefer this was shared in the closed community (Schwartz, 2008).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
196 Caregiver role strain
Recognize that different cultures value and use caregiving resources in different ways. CEB: When Korean
and Caucasian American caregivers were compared, there was more family support in Korean caregivers while
Caucasian Americans were more likely to use formal support (Kong, 2007).
Home Care
C Assess the client and caregiver at every visit for quality of relationship, and for the quality of caring that
exists. EB: Quality of the caregivercare recipient relationship and the impact of the care situation on that
relationship can be an important source of distress or support for the caregiver (Quinn, Clare, & Woods, 2009).
Chronic illness, especially dementia, can represent a gradual and devastating loss of the marital relationship as
it existed formerly. An understanding of the prior relationship is needed before the couple can be helped to
anticipate continuing care needs or deterioration, as the dyadic relationship can be expected to change over the
care situation (Langer et al, 2010).
Assess preexisting strengths and weaknesses the caregiver brings to the situation, as well as current
responses, depression, and fatigue levels. EB & EBN: Caregivers personality type, mastery, self-efcacy,
optimism, and social support have all been linked to the amount of distress the caregiver will perceive as a
result of providing care (Campbell et al, 2008; Shirai et al, 2009).
Refer the client to home health aide services for assistance with ADLs and light housekeeping. Allow the
caregiver to gain condence in the respite provider. Home health aide services can provide physical relief
and respite for the caregiver. EB: Caregiver burden increases as the care recipients cognitive and functional
ability decline (Ricci et al, 2009).
Client/Family Teaching and Discharge Planning
Identify client and caregiver factors that necessitate the use of formal home care services, that may affect
provision of care, or that need to be addressed before the client can be safely discharged from home care.
EBN: Although home care resources can be useful in decreasing caregiver distress, they are not used with regu-
larity across client populations. Health care practitioners should assess for the need for support resources prior
to discharge and at routine intervals throughout the care situation, tailoring community resources to individ-
ual caregiver needs (Greene et al, 2011). Interventions prior to discharge may include medication manage-
ment, identication of medical red ags, identication of community-based resources, and specic caregiver
concerns about home care (Hendrix et al, 2011).
Collaborate with the caregiver and discuss the care needs of the client, disease processes, medications, and
what to expect; use a variety of instructional techniques (e.g., explanations, demonstrations, visual aids)
until the caregiver is able to express a degree of comfort with care delivery. EB: Knowledge and condence
are separate concepts. Self-assurance in caregiving will decrease the amount of distress the caregiver perceives
as a result of providing care (Giovannetti et al, 2012) and may improve the quality of care provided.
Assess family caregiving skill. The identication of caregiver difculty with any of a core set of processes
highlights areas for intervention. CEB: The ability to engage effectively and smoothly in nine processes has
been identied as constituting family caregiving skill: monitoring client behavior, interpreting changes accu-
rately, making decisions, taking action, making adjustment to care, accessing resources, providing hands-on
care, working together with the ill person, and negotiating the health care system (Schumacher et al, 2000). EB:
Caregiver skills training has been shown to improve caregiver knowledge and skills and may be reimbursable
within governmental health care plans (Gitlin, Jacobs, & Earland, 2010).
Discharge care should be individualized to specic caregiver needs and care situations. EBN: Interventions
implemented by advanced practice nurses have been successful in preventing negative outcomes (Bradway
et al, 2011).
Assess the caregivers need for information such as information on symptom management, disease pro-
gression, specic skills, and available support. EBN: Caregiver interventions should be individualized to
meet specic caregiver needs (Greene et al, 2011; Hendrix et al, 2011).
Teach the caregiver warning signs for burnout, depression, and anxiety. Help them identify a resource in
case they begin to feel overwhelmed.
Teach the caregiver methods for managing disruptive behavioral symptoms if present. Refer to the care
plan for Chronic Confusion. CEB: Multicomponent interventions can be particularly effective in caregivers
of persons with neurologic sequelae (Pinquart & Sorenson, 2007).
Teach the caregiver how to provide the care needed and put a plan in place for monitoring the care
provided.
Provide ongoing support and evaluation of care skills as the care situation and care demands change.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Caregiver role strain 197
Provide information regarding the care recipients diagnosis, treatment regimen, and expected course of
illness.
Refer to counseling or support groups to assist in adjusting to the caregiver role and periodically evaluate
not only the caregivers emotional response to care but the safety of the care delivered to the care
recipient.
C
REFERENCES
Bauer M, et al: Hospital discharge planning for frail older people and Gouin J, Hantsoo L, Kiecolt-Glaser JK: Immune dysregulation and
their family, J Clin Nurs 18(18):25392546, 2009. chronic stress among older adults: a review, Neuroimmunomodula-
Beach SJ, et al: Negative and positive health effects of caring for a dis- tion 15(4-6):251259, 2008.
abled spouse: longitudinal ndings from the caregiver health effects Green TL, King KM: Relationships between biophysical and psy-
study, Psychol Aging 15(2):259271, 2000. chosocial outcomes following minor stroke, Can J Neurosci Nurs
Beeber AS, Thorpe JM, Clipp EC: Community-based service use by 33(2):1523, 2011.
elders with dementia and their caregivers: a latent class analysis, Greene A, et al: Can assessing caregiver needs and activating community
Nurs Res 57(5):312321, 2008. networks improve caregiver-dened outcomes? Palliat Med, Sep 19
Bender JL, Jimenez-Marroquin MC, Jadad AR: Seeking support on 2011 [Epub ahead of print].
Facebook: a content analysis of breast cancer groups, J Med Internet Gullatte M, et al: Religiosity, spirituality, and cancer fatalism beliefs on
Res 13(1):e16, 2011. delay in breast cancer diagnosis in African American women, J Relig
Bradway C, et al: A qualitative analysis of an advanced practice Health, 2009. [Epub ahead of print].
nurse-directed transitional care model intervention, Gerontologist Hendrix CC, et al: Pilot study: individualized training for caregivers of
52(3):394407, 2012. hospitalized older veterans, Nurs Res 60(6):436441, 2011.
Campbell P, et al: Determinants of burden in those who care for Holland JM, Currier JM, Gallagher-Thompson D: Outcomes from the
someone with dementia, Int J Geriatr Psychiatry 23(10):10781085, Resources for Enhancing Alzheimers Caregiver Health (REACH)
2008. program for bereaved caregivers, Psychol Aging 24(1):190202, 2009.
Chien LY, et al: Caregiver support groups in patients with dementia: a Hricik A, et al: Changes in caregiver perceptions over time in response
meta-analysis, Int J Geriatr Psychiatry 26(10):10891098, 2011. to providing care for a loved one with a primary malignant brain
Chiao CY, Schepp KG: The impact of foreign caregiving on depres- tumor, Oncol Nurs Forum 38(2):149155, 2011.
sion among older people in Taiwan: model testing, J Adv Nurs Hudson PL, Hayman-White K: Measuring the psychosocial character-
68(5):10901099, 2012. istics of family caregivers of palliative care patients: psychometric
Cohen M, et al: Development of a screening tool for identifying elderly properties of nine self-report instruments, J Pain Symptom Manage
people at risk of abuse by their caregivers, J Aging Health 18(5):660 31(3):215228, 2006.
685, 2006. Hwang B, et al: Caregiving for patients with heart failure, Am J Crit Care
Cooper C, et al: Abuse of people with dementia by family carers: repre- 20(6):431442, 2011.
sentative cross sectional survey, BMJ 338:b155, 2009. Kong EH: The inuence of culture on the experiences of Korean,
Deeken J, et al: Care for the caregivers: a review of self-report instru- Korean American, and Caucasian-American family caregivers of
ments developed to measure the burden, needs, and quality of life frail older adults: a literature review, Taehan Kanho Hakhoe Chi
of informal caregivers, J Pain Symptom Manage 26(4):922953, 37(2):213220, 2007.
2003. Kramer BJ, et al: Complicated grief symptoms in caregivers of persons
Eldh AC, Carlsson E: Seeking a balance between employment and the with lung cancer, Omega 62(3):201220, 2011.
care of an ageing parent, Scand J Caring Sci 25(2):285293, 2011. Kruithof WJ, Visser-Meily JM, Post MW: Positive caregiving expe-
Elliot AF, Burgio LD, Decoster J: Enhancing caregiver health, J Am riences are associated with life satisfaction in spouses of stroke survi-
Geriatr Soc 58(1):3037, 2010. vors, J Stroke Cerebrovasc Dis, 2011. Jun 1 [Epub ahead of print].
Gallagher S, et al: Caregiving is associated with low secretion rates of Langer SL, et al: Marital adjustment, satisfaction and dissolution
immunoglobulin A in saliva, Brain Behav Immun 22(4):565572, among hematopoietic stem cell transplant patients and spouses:
2008. a prospective, ve-year longitudinal investigation, Psychooncology
Giger J, Davidhizar R: Transcultural nursing: assessment and interven- 19(2):190200, 2010.
tion, St Louis, 2008, Mosby. Lovell B, Moss M, Wetherell M: The psychosocial, endocrine and
Giovannetti ER, et al: Difculty assisting with health care tasks among immune consequences of caring for a child with autism or ADHD,
caregivers of multimorbid older adults, J Gen Intern Med 27(1):37 Psychoneuroendocrinology 37(4):534542, 2012.
44, 2012. Matsuzawa T, et al: Predictive factors for hospitalized and institutional-
Gitlin LN, Jacobs M, Earland TV: Translation of a dementia caregiver ized caregiving of the aged patients with diabetes mellitus in Japan,
intervention for delivery in homecare as a reimbursable Medicare Kobe J Med Sci 56(4):E173E183, 2011.
service: outcomes and lessons learned, Gerontologist 50(6):847854, Merluzzi TV, et al: Assessment of self-efcacy for caregiving: the critical
2010. role of self-care in caregiver stress and burden, Palliat Support Care
Given BA, Sherwood P, Given CW: Support for caregivers of cancer 9(1):1524, 2011.
patients: transition after active treatment, Cancer Epidemiol Bio- Molinuevo JL, Hernandez B, TRACE: Assessment of the information
markers Prev 20(10):20152021, 2011. provided by the medical specialist on Alzheimers disease and that
Given CW, et al: The caregiver reaction assessment (CRA) for caregivers retained by the patient caregivers, Neurologia, 2011, Sep 8 [Epub
to persons with chronic physical and mental impairments, Res Nurs ahead of print].
Health 15(4):271383, 1992. Moore CD: Enhancing health care communication skills: preliminary
Goins RT, et al: Adult caregiving among American Indians: the role of evaluation of a curriculum for family caregivers, Home Health Care
cultural factors, Gerontologist 51(3):310320, 2011. Serv Q 27(1):2135, 2008.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
198 Risk for caregiver role strain
Northouse LL, et al: Interventions with family caregivers of cancer Sherwood PR, et al: The impact of a problem-solving intervention on
patients: meta-analysis of randomized trials, CA Cancer J Clin increasing caregiver assistance and improving caregiver health, Sup-
60(5):317339, 2010. port Care Cancer 20(9):19371947, 2012.
Novak M, Guest C: Application of a multidimensional caregiver burden Shirai Y, et al: Reaping caregiver feelings of gain: the roles of socio-
inventory, Gerontologist 29(6):798803, 1989. emotional support and mastery, Aging Ment Health 13(1):106117,
Paun O, Farran CJ: Chronic grief management for dementia caregivers 2009.
C in transition, J Gerontol Nurs 37(12):2835, 2011.
Pinquart M, Sorensen S: Correlates of physical health of informal care-
Siefert ML, et al: The caregiving experience in a racially diverse sample
of cancer family caregivers, Cancer Nurs 31(5):399407, 2008.
givers: a meta-analysis, J Gerontol B Psychol Sci Soc Sci 62(2):P126 Sinclair AJ, et al: Caring for older adults with diabetes mellitus, Diabet
P137, 2007. Med 27(9):10551059, 2010.
Quinn C, Clare L, Woods B: The impact of the quality of relation- Sussman T, Regehr C: The inuence of community-based services
ship on the experiences and wellbeing of caregivers of people with on the burden of spouses caring for their partners with dementia,
dementia: a systematic review, Aging Ment Health 13(2):143154, Health Soc Work 34(1):2939, 2009.
2009. Vitaliano P, et al: The screen for caregiver burden, Gerontologist
Ricci M, et al: Clinical ndings, functional abilities and caregiver 31(1):7683, 1991.
distress in the early stage of dementia with Lewy bodies (DLB) and Vroman K, Morency J: I do the best I can: caregivers perceptions of
Alzheimers disease (AD), Arch Gerontol Geriatr 49(2):e101e104, informal caregiving for older adults in Belize, Int J Aging Hum Dev
2009. 72(1):125, 2011.
Robinson B: Validation of a Caregiver Strain Index, J Gerontol Williams AL, McCorkle R: Cancer family caregivers during the pallia-
38(3):344348, 1983. tive, hospice, and bereavement phases: a review of the descriptive
Schoenmakers B, Buntinx F, Delepeleire J: Factors determining the psychosocial literature, Palliat Support Care 9(3):315325, 2011.
impact of caregiving on caregivers of elderly patients with dementia, Zahid MA, Ohaeri JU: Relationship of family caregiver burden with
Maturitas 66(2):191200, 2010. quality of care and psychopathology in a sample of Arab subjects
Schulz R, Beach SR: Caregiving as a risk factor for mortality: the Care- with schizophrenia, BMC Psychiatry 10:71, 2010.
giver Health Effects Study, JAMA 282(23):22152219, 1999. Zarit SH, et al: Relatives of the impaired elderly: correlates of feelings of
Schumacher KL, et al: Family caregiving skill: development of the con- burden, Gerontologist 20(6):649655, 1980.
cept, Res Nurs Health 23(3):191203, 2000.
Schwartz K: Breast cancer and health care beliefs, values, and practices
of Amish women, Diss Abstr 29(1):587, 2008.
Risk for Caregiver Role Strain Betty Ackley, MSN, EdS, RN
NANDA-I
Definition
At risk for caregiver vulnerability for felt difculty in performing the family caregiver role
Risk Factors
Amount of caregiving tasks, care receiver exhibits bizarre behavior, care receiver exhibits deviant behavior,
caregiver health impairment, caregiver is female, caregiver is spouse, caregiver isolation, caregiver not devel-
opmentally ready for caregiver role, caregivers competing role commitments, co-dependency, cognitive
problems in care receiver, complexity of caregiving tasks, congenital defect, developmental delay of care-
giver, developmental delay of care receiver, discharge of family member with signicant home care needs,
duration of caregiving required, family dysfunction before the caregiving situation, family isolation, illness
severity of the care receiver, inadequate physical environment for providing care (e.g., housing, transporta-
tion, community services, equipment), inexperience with caregiving, instability in the care receivers health,
lack of recreation for caregiver, lack of respite for caregiver, marginal caregivers coping patterns, marginal
family adaptation, past history of poor relationship between caregiver and care receiver, premature birth,
presence of abuse, presence of situational stressors that normally affect families (e.g., signicant loss, disaster
or crisis, economic vulnerability, major life events), presence of violence, psychological problems in care-
giver, psychological problems in care receiver, substance abuse, unpredictable illness course
NIC, Client Outcomes, Nursing Interventions, Client/Family Teaching, Rationales,
and References
Refer to care plan for Caregiver Role Strain.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Risk for ineffective cerebral tissue perfusion 199
Risk for ineffective Cerebral tissue perfusion Laura Mcilvoy, PhD, RN, CCRN, CNRN
NANDA-I
Definition
C
Risk for decrease in cerebral tissue circulation
Risk Factors
Abnormal partial thromboplastin time; abnormal prothrombin time; akinetic left ventricular segment; aor-
tic atherosclerosis; arterial dissection; atrial brillation; atrial myxoma; brain tumor; carotid stenosis; cere-
bral aneurysm; coagulopathy (e.g., sickle cell anemia); dilated cardiomyopathy; disseminated intravascular
coagulation; embolism; head trauma; hypercholesterolemia; hypertension; infective endocarditis; left atrial
appendage thrombosis; mechanical prosthetic valve; mitral stenosis; recent myocardial infarction; sick sinus
syndrome; substance abuse; thrombolytic therapy; treatment-related side effects (cardiopulmonary bypass,
medications); transient ischemic attack
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Acute Confusion Level, Tissue Perfusion: Cerebral, Agitation Level, Neurological Status, Cognition, Seizure
Control, Motor Strength
Example NOC Outcome with Indicators
Tissue Perfusion: Cerebral as evidenced by the following indicators: Headache/Restlessness/Listlessness/Agitation/Vomiting/
Fever/Impaired Cognition/Decreased level of consciousness/Motor weakness/Dysphagia/Slurred speech. (Rate the outcome and indica-
tors of Tissue Perfusion: Cerebral: 1 = severe, 2 = substantial, 3 = moderate, 4 = mild, 5 = none [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
State absence of headache
Demonstrate appropriate orientation to person, place, time, and situation
Demonstrate ability to follow simple commands
Demonstrate equal bilateral motor strength
Demonstrate adequate swallowing ability
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Medication Management, Neurologic Monitoring, Positioning: Neurologic, Cerebral Perfusion Promotion,
Fall Prevention, Cognitive Stimulation, Environmental Management: Safety
Example NIC ActivitiesNeurologic Monitoring
Monitor pupillary size, shape, symmetry, and reactivity; Monitor level of consciousness; Monitor level of orientation; Monitor trend of
Glasgow Coma Scale; Monitor facial symmetry; Note complaint of headache
Nursing Interventions and Rationales
To decrease risk of reduced cerebral perfusion r/t stroke or transient ischemic attack:
Obtain a family history of hypertension and stroke to identify persons who may be at increased risk of
stroke. EB: A positive family history of stroke increases risk of stroke by approximately 30% (Goldstein et al,
2011).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
200 Risk for ineffective cerebral tissue perfusion
Monitor BP regularly, as hypertension is a major risk factor for both ischemic and hemorrhagic
stroke. EB: Systolic BP should be treated to a goal of less than 140 mm Hg and diastolic BP to less than
90 mm Hg, while clients with diabetes or renal disease have a BP goal of less than 130/80 mm Hg (Gold-
stein et al, 2011).
Teach hypertensive clients the importance of taking their physician-ordered antihypertensive agent to
C prevent stroke. EB: Meta-analysis found thiazide diuretics, ACE inhibitors (ACEI), and calcium channel
blockers (CCB) all reduced the risk of stroke compared with no treatment or placebo (Wright & Musini,
2009).
Stress smoking cessation at every encounter with clients, utilizing multimodal techniques to aid in
quitting, such as counseling, nicotine replacement, and oral smoking cessation medications. EB: Epide-
miological studies show a consistent and overwhelming relationship between smoking and both ischemic
and hemorrhagic stroke (Goldstein et al, 2011).
Teach clients who experience a transient ischemic attack (TIA) that they are at increased risk for a
stroke. CEB: Overall stroke risk in TIA patients is 5.2% at 7 days and 10.3% at 90 days (Giles & Rothwell,
2007; Johnson et al, 2007; Rothwell et al, 2007).
Teach clients with a history of acute coronary syndromes (unstable angina, non-STEMI [non-ST-
elevation myocardial infarction], and STEMI [ST-elevation myocardial infarction]) that they are at risk
for stroke. CEB: Cardiovascular disease and stroke have the same pathophysiology and therefore the same
risk factors. The rate of stroke after a STEMI is markedly increased (Smith et al, 2006; Witt et al 2005).
Screen clients 65 years of age and older for atrial brillation with pulse assessment. EB: Atrial brillation
is associated with a vefold increase in stroke. Systematic pulse assessment in primary care setting resulted
in a 60% increase in the detection of atrial brillation (Goldstein et al, 2011).
Call 911 or activate the rapid response team of a hospital immediately in clients displaying the symptoms
of stroke as determined by the Cincinnati Stroke Scale (F: facial drooping, A: arm drift on one side,
S: speech slurred), being careful to note the time of symptom appearance. Additional symptoms of
stroke include sudden numbness/weakness of face, arm or leg, especially on one side, sudden confusion,
trouble speaking or understanding, sudden difculty seeing in one or both eyes, sudden trouble walking,
dizziness, loss of balance or coordination, or sudden severe headache (National Stroke Association,
2012). CEB: The Cincinnati Stroke Scale (derived from the NIH Stroke Scale) is used to identify patients
having a stroke who may be candidates for thrombolytic therapy (Kothari et al, 1999). EMS activation results
in faster physician assessment, computer tomography, and neurological evaluation, which facilitates admin-
istering thrombolytics to eligible stroke victims in the required 3-hour time period (Adams et al, 2007).
Use clinical practice guidelines for glycemic control and BP targets to guide the care of diabetic patients
that have had a stroke or TIA. CEB: The American Stroke Association recommends that evidence-based
guidelines be used in the care of diabetic clients. Good glycemic control has been associated with decreased
incidence of strokes (Furie et al, 2011; Handelsman et al, 2011).
To decrease risk of reduced cerebral perfusion pressure: Cerebral perfusion pressure = Mean arterial pres-
sure intracranial pressure (CPP = MAP ICP): See care plan for Decreased Intracranial Adaptive
Capacity.
Maintain euvolemia. CEB: Infusing intravenous uids to sustain normal circulating volume helps main-
tain normal cerebral blood ow (Bullock, Chestnut, & Clifton, 2001).
Maintain head of bed at or less than 30 degrees in acute stroke clients. CEB: Both mean blood ow veloc-
ity in the middle cerebral artery and CPP are increased with lowering head position from 30 degrees to 0
degrees in both ischemic and hemorrhagic stroke clients (Schwarz et al, 2002; Wojner-Alexandrov et al, 2005).
REFERENCES
Adams HP, et al: Guidelines for the early management of adults with Goldstein LB, et al: Guidelines for the primary prevention of stroke,
ischemic stroke, Stroke 38:16551711, 2007. Stroke 42:517584, 2011.
Bullock R, Chestnut R, Clifton G: Management and prognosis of severe Handelsman Y, et al: American Association of Clinical Endocrinologist
traumatic brain injury, J Neurotrauma 17(6&7):451627, 2001. medical guidelines for clinical practice for developing a diabetes
Furie KL, et al: Guidelines for the prevention of stroke in patients with mellitus comprehensive care plan, Endocr Pract 17(Suppl 2):153,
stroke or transient ischemic attack, Stroke 42:227276, 2011. 2011.
Giles MF, Rothwell PM: Risk of stroke early after transient ischemic Johnson SC, et al: Validity and refinement of scores to predict early
attack: a systematic review and meta-analysis, Lancet Neurol stroke risk after transient ischemic attack, Lancet 369:283292,
6(12):10631072, 2007. 2007.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Ineffective childbearing process 201
Kothari R, et al: Cincinnati prehospital stroke scale: reproducibility and Smith SC, et al: AHA/ACC guidelines for secondary prevention for
validity, Ann Emerg Med 33(4):373378, 1999. patients with coronary and other atherosclerotic valve disease: 2006
National Stroke Association: Warning signs of a stroke, 2012. http:/ update, Circulation 113:23262372, 2006.
/www.stroke.org/site/PageServer?pagename=symp. accessed August Witt BJ, et al: A community-based study of stroke incidence after myo-
27, 2012. cardial infarction, Ann Intern Med 143:785792, 2005.
Rothwell PM, et al: Effect of urgent treatment of transient ischemic Wojner-Alexandrov A, et al: Heads down: at positioning improves
attack and minor stroke on early recurrent stroke (EXPRESS Study):
a prospective population based sequential comparison, Lancet
blood ow velocity in acute ischemic stroke, Neurology 64:1354
2357, 2005.
C
370:14321442, 2007. Wright JM, Musini VM: First-line drugs for hypertension, Cochrane
Schwarz S, et al: Effects of induced hypertension on intracranial pres- Database Syst Rev(3):CD001841, 2009.
sure and ow velocities of the middle cerebral arteries in patients
with large hemispheric stroke, Stroke 33(4):9981004, 2002.
Ineffective Childbearing Process Kimberly J. Johnson-Crisanti, MSN, CNM
NANDA-I
Definition
Pregnancy and childbirth process and care of newborn that does not match the environmental context,
norms, and expectations
Defining Characteristics
During Pregnancy
Does not access support systems appropriately
Does not report appropriate physical preparations
Does not report appropriate prenatal lifestyle (e.g., diet, elimination, sleep, bodily movement, exercise,
personal hygiene)
Does not report availability of support systems
Does not report managing unpleasant symptoms in pregnancy
Does not report a realistic birth plan
Does not seek necessary knowledge (e.g., of labor and delivery, newborn care)
Failure to prepare necessary newborn care items
Inconsistent prenatal health visits
Lack of prenatal visits
Lack of respect for unborn baby
During Labor and Delivery
Does not demonstrate appropriate baby feeding techniques
Does not demonstrate attachment behavior to the newborn baby
Lacks proactivity during labor and delivery
Does not report lifestyle (e.g., diet, elimination, sleep, bodily movement, personal hygiene) that is appro-
priate for the stage of labor
Does not respond appropriately to onset of labor
Does not report availability of support systems
Does not access support systems appropriately
After Birth
Does not demonstrate appropriate baby feeding techniques
Does not demonstrate appropriate breast care
Does not demonstrate attachment behavior to the baby
Does not demonstrate basic baby care techniques
Does not provide safe environment for the baby
Does not report appropriate postpartum lifestyle (e.g., diet, elimination, sleep, bodily movement, per-
sonal hygiene)
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
202 Ineffective childbearing process
Does not report availability of support systems
Does not access support systems appropriately
Related Factors
Decient knowledge (e.g., of labor and delivery, newborn care)
C Domestic violence
Inconsistent prenatal health visits
Lack of appropriate role models for parenthood
Lack of cognitive readiness for parenthood
Lack of maternal condence
Lack of prenatal health visits
Lack of a realistic birth plan
Lack of sufcient support systems
Maternal powerlessness
Maternal psychological distress
Suboptimal maternal nutrition
Substance abuse
Unsafe environment
Unplanned pregnancy
Unwanted pregnancy
NOC Nursing Outcomes Classification
Suggested NOC Outcomes
Fetal Status: Antepartum, Intrapartum, Maternal Status: Antepartum, Intrapartum, Depression Level, Fam-
ily Resiliency, Knowledge: Substance Use Control, Social Support, Spiritual Support
Example NOC Outcomes with Indicators
Maternal Status: Antepartum as evidenced by the following indicators: Emotional attachment to fetus/Coping with
discomforts of pregnancy/Mood lability/Has realistic birth plan/Has support system. (Rate each indicator of Maternal Status:
Antepartum: 1 = severe deviation from normal range, 2 = substantial deviation from normal range, 3 = moderate deviation
from normal range, 4 = mild deviation from normal range, 5 = no deviation from normal range [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Antepartum
Obtain early prenatal care in the rst trimester and maintain regular visits
Obtain knowledge level needed for appropriate care of oneself during pregnancy including good nutrition
and psychological health
Understand the risks of substance abuse and resources available
Feel empowered to seek social and spiritual support for emotional well-being during pregnancy
Utilize support systems for labor and emotional support
Develop a realistic birth plan taking into account any high risk pregnancy issues
Be able to understand the labor and delivery process and comfort measures to manage labor pain
Postpartum
Utilize a safe environment for self and infant
Obtain knowledge to provide appropriate newborn care and postpartum care of self
Obtain knowledge to develop appropriate bonding and parenting skills
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
High-Risk Pregnancy Care, Intrapartal Care
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Ineffective childbearing process 203
Example NIC ActivitiesHigh-Risk Pregnancy Care
Instruct patient on importance of receiving regular prenatal care and to follow plan of care by taking prescribed medications and
following nutrition guidelines; Encourage identification of psychosocial/psychological issues and substance use and appropriate treat-
ment and referrals as needed
C
Nursing Interventions and Rationales
Encourage early prenatal care and regular prenatal visits. EBN: A study compared outcomes of infants born
to women who received Medicaid and prenatal care coordination (PNCC) services versus women who received
Medicaid but did not receive PNCC. Women who received PNCC services resulted in fewer low-birth-weight
infants, fewer preterm infants, and fewer infants transferred to the neonatal intensive care unit. PNCC is an
effective strategy for preventing adverse birth outcomes (Van Dijk, Anderko, & Stetzer, 2011).
Identify any high-risk factors that may require additional surveillance such as preterm labor, hypertensive
disorders of pregnancy, diabetes, depression, other chronic medical conditions, presence of fetal anoma-
lies, or other high-risk factors. EB: A Cochrane study found that early and regular prenatal care can improve
maternal and fetal outcomes by screening for risk factors and providing appropriate intervention and referrals
(Dowswell et al, 2010).
Assess and screen for signs and symptoms of depression during pregnancy and in postpartal period
including history of depression or postpartum depression, poor prenatal care, poor weight gain, hygiene
issues, sleep problems, substance abuse, and preterm labor. If depression is present, refer for behavioral-
cognitive counseling, and/or medication (postpartum period only). Both counseling and medication are
considered relatively equal to help with depression. EB: Research demonstrates that early screening, treat-
ment, and referral can improve pregnancy outcome by decreasing preterm labor, preterm birth, and low-birth-
weight infants. Psychosocial support can improve bonding between mother and infant and allow the mother
to appropriately care for infant (Yawn, 2011; Yonkers, Vigod & Ross, 2011).
Observe for signs of alcohol use and counsel women to stop drinking during pregnancy. Give appropriate
referral for treatment if needed. EB: Alcohol is teratogenic, and prenatal exposure may result in growth
impairment, facial abnormalities, central nervous system and/or intellectual impairment, and behavioral dis-
orders. Evidence suggests womens past pregnancy, current drinking behavior, and attitude toward alcohol use
in pregnancy were the strongest predictors of alcohol consumption in pregnancy (Barclay, 2011; Peadon et al
2011).
Obtain a smoking history and counsel women to stop smoking for the safety of the baby. Give appropriate
referral to smoking cessation program if needed. EB: Tobacco smoking in pregnancy remains one of the few
preventable factors associated with complications in pregnancy, low birth weight, and preterm birth and has
serious long-term health implications for women and babies. Smoking cessation treatment resulted in reduced
low-birth-weight infants and decreased preterm births, and there was an increase in mean birth weight (Lum-
ley et al, 2009).
Monitor for substance abuse with recreational drugs. Refer to drug treatment program as needed. Refer
opiate-dependent women to methadone clinics to improve maternal and fetal pregnancy outcomes. EB:
Opiate-dependent women experience a sixfold increase in maternal obstetric complications and give birth to
low-weight babies (Minozzi et al, 2008). The newborn may experience narcotic withdrawal (neonatal absti-
nence syndrome) have development problems, increased neonatal mortality, and a 74-fold increased risk of
sudden infant death syndrome. Maintenance treatment with methadone provides a steady concentration of
opiate in the pregnant womans blood preventing the adverse effects on the fetus of repeated withdrawals.
Buprenorphine may also be prescribed. These treatments can reduce illicit drug use, improve compliance with
obstetric care, and improve birth weight but are still associated with neonatal abstinence syndrome (Minozzi
et al, 2008).
Monitor for psychosocial issues including lack of social support system, loneliness, depression, lack of
condence, maternal powerlessness, domestic violence, and socioeconomic problems. EB: A study that
compared psychosocial assessment versus routine care for pregnant women concluded that the providers who
assessed psychosocial factors were more likely to identify psychosocial concerns, including family violence, and
to rate the level of concern as high. In two trials, women identied they did not want to feel so alone, be judged,
be misunderstood and they wanted to feel an increased sense of their own worth (Austin et al, 2008; Gentry
et al, 2010; Small et al, 2011). Social support interventions can improve health. The use of doulas can provide
assistance in addressing social-psychological issues and socioeconomic disparities.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
204 Ineffective childbearing process
Monitor for signs of domestic violence. Refer to a community program for abused women that provides
safe shelter as needed. EB: Fear about judgments about their capacity to provide appropriate care for their
children often holds women back from disclosing depression and intimate partner violence. Psychological vio-
lence during pregnancy by an intimate partner is strongly associated with postnatal depression (Ludermir
et al, 2010; Small et al, 2011).
C Provide antenatal education to increase the womans knowledge needed to make informed choices during
pregnancy, labor, and birth and to promote a healthy lifestyle. EB: The use of doulas and childbirth educa-
tors has been shown to reduce medical interventions and improve maternal and infant outcomes in women
(Gentry et al, 2010). CEB: A Cochrane review found a lack of quality evidence concerning the effects of ante-
natal education (Gagnon & Sandall, 2007).
Encourage expectant parents to prepare a realistic birth plan in order to prepare for the physical and
emotional aspects of the birth process and to plan ahead for how they want various situations handled.
CEB: A Discussion Birth Plan and a Hospital Birth Plan can be used to facilitate communication with the
expectant parents, their care provider and the hospital staff for events that occur during labor and birth. Both
plans can assist expectant parents to make educated and informed decisions (Kaufman, 2007).
Encourage good nutritional intake during pregnancy to facilitate proper growth and development of the
fetus. Women should consume an additional 300 calories per day during pregnancy and achieve a total
weight gain of 25 to 30 lb. EB: Low plasma folate concentrations in pregnancy are associated with preterm
birth. Preconceptual folate supplementation is associated with a 50% to 70% reduction in preterm birth. Stud-
ies revealed that there was little change in dietary patterns in pregnancy, which is of concern because women
were not able to improve their overall diets in pregnancy (Bukowski et al, 2009; Crozier et al, 2009). CEB:
A study of low and middle income countries showed that supplementation with multi-micronutrients showed
a reduction in low birth weight and maternal anemia (Haider & Bhutta, 2006).
Multicultural
Provide depression screening for clients of all ethnicities. EB: Race and ethnicity are important risk factors
for antenatal depression. A study found that non-Hispanic white women, black women, and Asian/Pacic
Islander women had an increased risk for antenatal depression. The prevalence of antenatal depression was
15.3% in black women, 6.9% in Latinas, and 3.6% in non-Hispanic white women (Gavin et al, 2011).
Provide obstetrical care that is culturally diverse to ensure a safe and satisfying childbearing experience.
EBN: Nurses must acknowledge that the maternity health care system has a unique culture that may clash
with the cultures of many of our clients. Women not accustomed to this culture of potential risk in prenatal
care, childbirth, and neonatal care may be frightened, overwhelmed, or made to feel guilty if they are not will-
ing to undergo some of the expected interventions (Lewallen, 2011).
REFERENCES
Austin MP, Priest SR, Sullivan EA: Antenatal psychosocial assessment Haider BA, Bhutta ZA: Multiple-micronutrient supplementa-
for reducing perinatal mental health morbidity, Cochrane Database tion for women during pregnancy, Cochrane Database Syst
Syst Rev(4):CD005124, 2008. Rev(4):CD004905, 2006.
Barclay L: ACOG calls for alcohol screen annually and at prenatal visit, Kaufman T: Evolution of the birth plan, J Perinat Educ 16(3):4752,
Obstet Gynecol 18:383388, 2011. 2007.
Bukowski R, et al: Preconceptual folate supplementation and the risk of Lewallen LP: The importance of culture in childbearing, J Obstet Gyne-
spontaneous preterm birth: a cohort study, PLoS Med 6(5), 2009. col Neonat Nurs 40:48, 2011.
Crozier S, et al: Dietary patterns change little from before to during Ludermir A, et al: Violence against women by their intimate partner
pregnancy, J Nutr 139(10):19561963, 2009. during pregnancy and postnatal depression: a prospective cohort
Dowswell T, et al: Alternative versus standard packages of antenatal care study, Lancet 376(9744):903910, 2010.
for low-risk pregnancy, Cochrane Database Syst Rev(10):CD000934, Lumley J, et al: Interventions for promoting smoking cessation during
2010. pregnancy, Cochrane Database Syst Rev(3):CD001055, 2009.
Gagnon AJ, Sandall J: Individual or group antenatal education Minozzi S, et al: Maintenance agonist treatments for opiate dependent
for childbirth or parenthood, or both, Cochrane Database Syst pregnant women, Cochrane Database Syst Rev(2):CD006318, 2008.
Rev(3):CD002869, 2007. Peadon E, et al: Attitudes and behavior predict womens intention to
Gavin A, et al: Racial differences in the prevalence of antenatal depres- drink alcohol during pregnancy: the challenge for health profession-
sion, Gen Hosp Psychiatry 33(2):8793, 2011. als, BMC Public Health 11:584, 2011.
Gentry Q, et al: Going beyond the call of doula: a grounded theory Small R, et al: The power of social connection and support in improving
analysis for the diverse roles community-based doulas play in the health: lessons from social support interventions with childbearing
lives of pregnant and parenting adolescent mothers, J Perinat Educ women, BMC Public Health 11(Suppl 5):S4, 2011.
19(4):2440, 2010.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Readiness for enhanced childbearing process 205
Van Dijk JW, Anderko L, Stetzer F: The impact of prenatal care coordi- Yonkers KA, Vigod S, Ross LE: Diagnosis, pathophysiology, and man-
nation on birth outcomes, J Obstet Gynecol Neonat Nurs 40:98108, agement of mood disorders in pregnant and postpartum women,
2011. Obstet Gynecol 117(4):961977, 2011.
Yawn B: Recognizing & managing postpartum depression, Am Acad
Fam Physician Sci Assemb, 2011. Retrieved May 29, 2012, from http:
//www.medscape.com/viewarticle/749874.
C
Readiness for enhanced Childbearing Process Gail B. Ladwig, MSN, RN
NANDA-I
Definition
A pattern of preparing for and maintaining a healthy pregnancy, childbirth process, and care of newborn that
is sufcient for ensuring well-being and can be strengthened
Defining Characteristics
During Pregnancy
Attends regular prenatal health visits; demonstrates respect for unborn baby; prepares necessary newborn
care items; reports appropriate physical preparations; reports appropriate prenatal lifestyle (e.g., nutrition,
elimination, sleep, bodily movement, exercise, personal hygiene)
Reports availability of support systems; reports realistic birth plan; reports managing unpleasant symp-
toms in pregnancy; seeks necessary knowledge (e.g., of labor and delivery, newborn care)
During Labor and Delivery
Demonstrates attachment behavior to the newborn baby; is proactive during labor and delivery; reports
lifestyle (e.g., diet, elimination, sleep, bodily movement, personal hygiene) that is appropriate for the stage of
labor; responds appropriately to onset of labor; uses relaxation techniques appropriate for the stage of labor;
utilizes support systems appropriately
After Birth
Demonstrates appropriate baby feeding techniques; demonstrates appropriate breast care; demonstrates
attachment behavior to the baby; demonstrates basic baby care techniques; provides safe environment for
the baby; reports appropriate postpartum lifestyle (e.g., diet, elimination, sleep, bodily movement, exercise,
personal hygiene); utilizes support system appropriately
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Knowledge: Pregnancy, Knowledge: Infant Care, Knowledge: Postpartum Maternal Health
Example NOC Outcome with Indicators
Knowledge: Pregnancy as evidenced by client conveying understanding of the following indicators: Importance of frequent
prenatal care/Importance of prenatal education/Benefits of regular exercise/Healthy nutritional practices/Anatomic and physiological
changes with pregnancy/Psychological changes associated with pregnancy/Birthing options/Effective labor techniques/Signs and symp-
toms of labor. (Rate the outcome and indicators of Knowledge: Pregnancy: 1 = no knowledge, 2 = limited knowledge,
3 = moderate knowledge, 4 = substantial knowledge, 5 = extensive knowledge [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
During Pregnancy
State importance of frequent prenatal care/education
State knowledge of anatomic, physiological, psychological changes with pregnancy
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
206 Readiness for enhanced childbearing process
Report appropriate lifestyle choices prenatal: activity and exercise/healthy nutritional practices
During Labor and Delivery
Report appropriate lifestyle choices during labor
State knowledge of birthing options, signs and symptoms of labor, and effective labor techniques
C After Birth
Report appropriate lifestyle choices postpartum
State normal physical sensations following delivery
State knowledge of recommended nutrient intake, strategies to balance activity and rest, appropriate exer-
cise, time frame for resumption of sexual activity, strategies to manage stress
List strategies to bond with infant
State knowledge of proper handling and positioning of infant/infant safety
State knowledge of feeding technique and bathing of infant
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Prenatal Care, Intrapartal Care, Postpartal Care, Attachment Promotion, Infant Care: Newborn
Example NIC ActivitiesPrenatal Care
Encourage prenatal class attendance; Discuss nutritional needs and concerns (e.g., balanced diet, folic acid, food safety, and supple-
ments); Discuss activity level with patient (e.g., appropriate exercise, activities to avoid, and importance of rest); Discuss importance
of participating in prenatal care throughout entire pregnancy while encouraging involvement of patients partner or other family
member
Nursing Interventions and Rationales
Refer to care plans Risk for impaired Attachment; Readiness for enhanced Breastfeeding; Readiness for
enhanced family Coping; Readiness for enhanced Family Processes; Risk for disproportionate Growth;
Readiness for enhanced Nutrition; Readiness for enhanced Parenting; Ineffective Role Performance
Prenatal Care
Ensure that pregnant clients have an adequate diet and take multimicronutrient supplements during
pregnancy. EB: Nutrition plays an important role in the growth and development of the fetus. Overall, the
diet of pregnant women has been reported to be decient in calories and micronutrients. Prenatal supplemen-
tation with multimicronutrients was associated with a signicantly reduced risk of low-birth-weight infants
and with improved birth weight (Shah et al, 2009).
Encourage pregnant clients to include enriched cereal grain products in their diets. EB: The number of
pregnancies affected by neural tube defects greatly decreased in the United States after the fortication of cereal
grain products with folic acid was mandated (CDC, 2010).
Assess smoking status of pregnant client and offer effective smoking-cessation interventions. EB: Smoking
during pregnancy is associated with delivery of preterm infants, low infant birth weight, and increased infant
mortality. After delivery, exposure to secondhand smoke can increase an infants risk for respiratory tract infec-
tions and for dying of sudden infant death syndrome (Tong et al, 2009). Prenatal smoking prevalence remains
high in the United States. To reduce prenatal smoking prevalence, efforts should focus on delivering evidence-
based cessation interventions to women who are most likely to smoke before pregnancy, younger non-Hispanic
white, Alaska Native, and American Indian women, who were identied in this study (Tong et al, 2011).
Assess for signs of depression and make appropriate referral: inadequate weight gain, underutilization of
prenatal care, increased substance use, and premature birth. Past personal or family history of depression,
single, poor health functioning, and alcohol use. EB: These signs occurring during pregnancy may be associ-
ated with depression treatment. Engagement is important, as untreated depression during pregnancy may
have unfavorable outcomes for both women and children (Sexton et al, 2012).
Intrapartal Care
Encourage psychosocial support during labor. EB: In this study at the University College Hospital Ibadan,
Nigeria, women with anticipated vaginal delivery were recruited and randomized at the antenatal clinic. The
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Readiness for enhanced childbearing process 207
experimental group had companionship in addition to routine care throughout labor until 2 hours after deliv-
ery, while the controls had only routine care. The primary outcome measure was cesarean section rate. Women
with companionship had better labor outcomes compared to those without (Morhason-Bello et al, 2009).
Consider using aromatherapy during labor. EB: Aromatherapy has been used in childbirth to reduce anxiety
and pain (Horowitz, 2011).
Offer immersion bath during labor. EBN: The present ndings of this study suggest that use of an immersion C
bath is a suitable alternative form of pain relief for women during labor (da Silva, de Oliveira, & Nobre, 2009).
Provide massage and relaxation techniques during labor. EB: The ndings in this study suggest that regular
massage with relaxation techniques from late pregnancy to birth is an acceptable coping strategy for pain relief
(Kimber et al, 2008).
Offer the client in labor a light diet and water. EB: In this study consumption of a light diet during labor did
not inuence obstetric or neonatal outcomes in participants, nor did it increase the incidence of vomiting.
Women who are allowed to eat in labor have similar lengths of labor and operative delivery rates to those
allowed water only (OSullivan et al, 2009).
Multicultural
Prenatal
Provide prenatal care for black and white clients. EB: Black-white disparities in infant mortality persist in
the United States. In the years 2001 to 2004, Wisconsin had the highest black infant mortality rate (IMR) in
the 40 states reporting. IMRs have declined in Wisconsin from 2002 to 2007 despite national trends. Prelimi-
nary information suggests contributing factors may include improvement in adequate medical care and pre-
natal care for all (CDC, 2009).
Refer the client to a centering pregnancy group (8 to 10 women of similar gestational age receive group
prenatal care after initial obstetrical visit) or group prenatal care. EBN: African-American women in group
care had signicantly fewer preterm births. Women in Centering Pregnancy groups were more likely to initiate
breastfeeding, more ready for labor and birth and signicantly more satised with their prenatal care (Klima,
2009). The majority of perinatal deaths occur in developing countries. In this article we describe the implemen-
tation and evaluation of group prenatal care in Iran. Birth weight was greater for the infants of women in
group prenatal care compared with those in individual care. We have shown that group prenatal care has
improved birth weight. Low birth weight (LBW), preterm birth, and perinatal death, although not signicant,
were lower in the intervention group (Jafari et al, 2010).
Intrapartal
Consider the clients culture when assisting in labor and delivery. EB: This study demonstrated the need for
a culturally sensitive, reliable, and valid instrument to better understand the self-efcacy of childbirth as a
basis for developing effective interventions to increase normal childbirth among Iranian pregnant women
(Khorsandi et al, 2008).
Postpartal
Provide health and nutrition education for Chinese women after childbirth. Provide information and guid-
ance on contemporary postpartum practices and take away common misconceptions about traditional
dietary and health behaviors (e.g., fruit and vegetables should be restricted because of cold nature). Encour-
age a balanced diet and discourage unhealthy hygiene taboos. EB: Sitting month is the Chinese tradition for
postpartum customs. Available studies indicate that some of the traditional postpartum practices are potentially
harmful for womens health. Chinese women are advised to follow a specic set of food choices and health care
practices. For example, the puerperal women should stay inside and not go outdoors; all windows in the room
should be sealed well to avoid wind. Bathing and hair washing should be restricted to prevent possible headache
and body pain in later years. Foods such as fruits, vegetables, soybean products, and cold drinks that are consid-
ered cold should be avoided. In contrast, foods such as brown sugar, sh, chicken, and pigs trotter, which are
considered hot, should be encouraged. It is believed that if a woman does not observe these restrictions, she may
suffer from poor health later in life. Several studies indicated that the incidences of postpartum health problems
are high and these problems may have relation to traditional and unscientic dietary and behavior practices in
the postpartum period. Available Chinese data also suggested that the incidences of constipation and hemor-
rhoids were associated with lack of exercise and a decreased intake of fruit and vegetables; the risk of oral prob-
lems was associated with no teethbrushing and excessive intake of sugar during the puerperium (Liu et al, 2009).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
208 Readiness for enhanced childbearing process
Health and nutrition education should include the Chinese family (particularly the relative who will be
staying with the new mother) after the woman gives birth. EB: The results of this study found that increased
nutrition and health care knowledge did not lead to parallel dietary and health behavior changes. This lack of
change is attributed to the fact that in China, the tradition to support a newly delivered woman and her baby
C for the rst month after childbirth at home is still common. Most of the women had an elder female of the fam-
ily such as her mother or mother-in-law as the support person. The elder female who takes care of the women
may have hindered the changes due to traditional beliefs. The main problematic aspect of the study was the
education intervention subjects aimed directly to the study of women, yet sitting month was usually recog-
nized as an important event in the family and the postpartum woman has been taken care by her mother or
mother-in-law (Liu et al, 2009).
Home Care
Prenatal
Involve pregnant drug users in drug treatment programs that include coordinated interventions in several
areas: drug use, infectious diseases, mental health, personal and social welfare, and gynecological/obstet-
ric care. EB: This literature search revealed that involving pregnant drug users in drug treatment is likely to
decrease the chances of prenatal and perinatal complications related to drug use and to increase access to pre-
natal care. Timely medical intervention can effectively prevent vertical transmission of human immunode-
ciency virus and hepatitis B virus, as well as certain other sexually transmitted diseases, and would allow
newborns infected with hepatitis C virus during birth to receive immediate treatment (Gyarmathy et al, 2009).
Postpartal
Provide video conferencing to support new parents. EBN: The ndings of this study indicate that VC equip-
ment may be helpful for parents discharged from the hospital early after childbirth (Lindberg, Christensson, &
Ohrling, 2009).
Consider reexology for postpartum women to improve sleep quality. EBN: In this RCT an intervention
involving foot reexology in the postnatal period signicantly improved the quality of sleep in postpartum
women (Liet al, 2011).
Client/Family Teaching and Discharge Planning
Prenatal
Provide dietary and lifestyle counseling as part of prenatal care to pregnant women. EB: In this study an
organized, consistent program of dietary and lifestyle counseling reduced weight gain in pregnancy (Asbee
et al, 2009). Community-level interventions of improved perinatal care practices can bring about a reduction
in maternal mortality (Kidney et al, 2009).
Provide the following information in parenting classes, via DVD and Internet: support mechanisms,
information and antenatal education, breastfeeding, practical baby care, and relationship changes. Include
fathers in the parenting classes. EB: The men felt very involved with their partners pregnancy but excluded
from antenatal appointments and antenatal classes, and by the literature that was available. Parents had been
unaware of, and surprised at, the changes in the relationship with their partners. They would have liked more
information on elements of parenting and baby care, relationship changes, and partners perspectives prior to
becoming parents. Parents suggested that information be provided on a DVD (Deave, Johnson, & Ingram,
2008; St George & Fletcher, 2011).
Provide group prenatal care to families in the military. EBN: Group PNC offers the potential for continuity
of provider, which the women were concerned was lacking. It also offers community with other women. In the
process, women gain knowledge and power as health care consumers (Kennedy et al, 2009).
Postpartal
Encourage physical activity in postpartum women; provide telephone counseling, pedometers, referral to
community PA resources, social support, email advice on PA/pedometer goals, and newsletters. EB: In
this study these interventions were effective in increasing physical activity in postpartum women (Albright,
Maddock, & Nigg, 2009).
Teach mothers of young children principles of a healthy lifestyle: substitute high-fat foods with low-fat
foods such as fruits and vegetables, increase physical activity, consider a community-based
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Risk for ineffective childbearing process 209
self-management intervention to prevent weight gain. EBN: Preventing weight gain rather than treating
established obesity is an important economic and public health response to the rapidly increasing rates of obe-
sity worldwide. In this study both a single health education session and interactive behavioral intervention
resulted in a similar weight loss in the short term, although more participants in the interactive intervention
lost or maintained weight. Self-monitoring appears to enhance weight loss when part of an intervention
(Lombard et al, 2009). C
REFERENCES
Albright CL, Maddock JE, Nigg CR: Increasing physical activity in post- Kimber L, et al: Massage or music for pain relief in labour: a pilot ran-
partum multiethnic women in Hawaii: results from a pilot study, domised placebo controlled trial, Eur J Pain 12(8):961969, 2008.
BMC Womens Health 9:4, 2009. Klima C, Norr K, Vonderheid S, Handler A: Introduction of Centering-
Asbee SM, et al: Preventing excessive weight gain during pregnancy Pregnancy in a public health clinic, Midwifery 54(1):2734, 2009.
through dietary and lifestyle counseling: a randomized controlled Li CY, et al: Randomised controlled trial of the effectiveness of using
trial, Obstet Gynecol 113(2 Pt 1):305312, 2009. foot reexology to improve quality of sleep amongst Taiwanese
Centers for Disease Control and Prevention (CDC): CDC grand rounds: postpartum women, Midwifery 27(2):181186, 2011.
additional opportunities to prevent neural tube defects with folic Lindberg I, Christensson K, Ohrling K: Parents experiences of using
acid fortication, MMWR Morb Mortal Wkly Rep 59(31):980984, videoconferencing as a support in early discharge after childbirth,
2010. Midwifery 25(4):357365, 2009.
Centers for Disease Control and Prevention (CDC): Apparent disap- Liu N, et al: The effect of health and nutrition education intervention
pearance of the black-white infant mortality gap-Dane County, Wis- on womens postpartum beliefs and practices: a randomized con-
consin, 1990-2007, MMWR Morb Mortal Wkly Rep 58(20):561565, trolled trial, BMC Public Health 9:45, 2009.
2009. Lombard CB, et al: Weight, physical activity and dietary behavior
da Silva FM, de Oliveira SM, Nobre MR: A randomised controlled trial change in young mothers: short term results of the HeLP-her cluster
evaluating the effect of immersion bath on labour pain, Midwifery randomized controlled trial, Nutrition J 8:17, 2009.
25(3):286294, 2009. Morhason-Bello IO, et al: Assessment of the effect of psychosocial sup-
Deave T, Johnson D, Ingram J: Transition to parenthood: the needs port during childbirth in Ibadan, south-west Nigeria: a randomised
of parents in pregnancy and early parenthood, BMC Pregnancy controlled trial, Aust N Z J Obstet Gynaecol 49(2):145150, 2009.
Childbirth 8:30, 2008. OSullivan G, et al: Effect of food intake during labour on obstetric
Gyarmathy VA, et al: Drug use and pregnancy-challenges for public outcome: randomised controlled trial, BMJ 338:b784, 2009.
health, Euro Surveill 4(9):3336, 2009. Sexton MB, et al: Predictors of recovery from prenatal depressive
Horowitz S: Aromatherapy: current and emerging applications, Altern symptoms from pregnancy through postpartum, J Womens Health
Complement Ther 17(1):2631, 2011. 21(1):4349, 2012.
Ionescu-Ittu R, et al: Prevalence of severe congenital heart disease after Shah PS, Ohlsson A: Knowledge Synthesis Group on Determinants of
folic acid fortication of grain products: time trend analysis in Low Birth Weight and Preterm Births: Effects of prenatal multimi-
Quebec, Canada, BMJ 338:b1673, 2009. cronutrient supplementation on pregnancy outcomes: a meta-anal-
Jafari F, et al: Comparison of maternal and neonatal outcomes of group ysis, CMAJ 180(12):E99108, 2009.
versus individual prenatal care: a new experience in Iran, Health St George JM, Fletcher RJ: Fathers online: learning about fatherhood
Care Women Int 31(7):571584, 2010. through the Internet, J Perinat Educ 20(3):154162, 2011.
Kennedy HP, et al: I wasnt alonea study of group prenatal care in Tong VT, et al: Trends in smoking before, during, and after pregnancy.
the military, J Midwifery Womens Health 54(3):176183, 2009. Pregnancy Risk Assessment Monitoring System (PRAMS), United
Khorsandi M, et al: Iranian version of childbirth self-efcacy inventory, States, 31 sites, 2000-2005, MMWR Surveill Summ 58(4):129, 2009.
J Clin Nurs 17(21):28462855, 2008. Tong VT, et al: Age and racial/ethnic disparities in prepregnancy
Kidney E, et al: Systematic review of effect of community-level interven- smoking among women who delivered live births, Prev Chron Dis
tions to reduce maternal mortality, BMC Pregnancy Childbirth 9:2, 8(6):A121, 2011.
2009.
Risk for ineffective Childbearing Process Betty Ackley, MSN, EdS, RN
NANDA-I
Definition
Risk for a pregnancy and childbirth process and care of newborn that does not match the environmental
context, norms, and expectations
Risk Factors
Decient knowledge (e.g., of labor and delivery, newborn care), domestic violence, inconsistent prenatal
health visits, lack of appropriate role models for parenthood, lack of cognitive readiness for parenthood, lack
of maternal condence, lack of prenatal health visits, lack of realistic birth plan, lack of sufcient support
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
210 Impaired comfort
systems, maternal powerlessness, maternal psychological distress, suboptimal maternal nutrition, substance
abuse, unplanned pregnancy, unwanted pregnancy
NIC, NOC, Client Outcomes, Nursing Interventions, Client/Family Teaching, Rationales,
and References
C Refer to care plan for Ineffective Childbearing Process.
Impaired Comfort Katharine Kolcaba, PhD, RN
NANDA-I
Definition
Perceived lack of ease, relief, and transcendence in physical, psychospiritual, environmental, and sociocul-
tural dimensions
Defining Characteristics
Anxiety; crying; disturbed sleep pattern; fear; illness-related symptoms; inability to relax; insufcient
resources (e.g., nancial, social support); irritability; moaning; noxious environmental stimuli; reports being
uncomfortable; reports being cold; reports being hot; reports distressing symptoms; reports hunger; reports
itching; reports lack of ease or contentment in situation; restlessness
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Client Satisfaction, Symptom Control, Comfort Status, Coping, Hope, Pain and/or Anxiety Management,
Personal Well-Being, Spiritual Health
Example NOC Outcomes with Indicators
Comfort Status as evidenced by the following indicators: Physical and psychological well-being/Symptom control/Enhanced
comfort. (Rate the outcome and indicators of Comfort Status: 1 = severely compromised, 2 = substantially compromised,
3 = moderately compromised, 4 = mildly compromised, 5 = not compromised [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Provide evidence for improved comfort compared to baseline
Identify strategies, with or without signicant others, to improve and/or maintain acceptable comfort
level
Perform appropriate interventions, with or without signicant others, as needed to improve and/or main-
tain acceptable comfort level
Evaluate the effectiveness of strategies to maintain/and or reach an acceptable comfort level
Maintain an acceptable level of comfort when possible
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Calming Techniques, Massage, Healing Touch, Heat/Cold Application, Hope Inspiration, Humor, Medita-
tion Facilitation, Music Therapy, Pain Management, Presence; Progressive Muscle Relaxation, Spiritual
Growth Facilitation, Distraction
Example NIC ActivitiesHope Inspiration
Assist the client/significant others to identify areas of hope in life; Help to expand spiritual self; Involve the client actively in own care
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Impaired comfort 211
Nursing Interventions and Rationales*
Assess clients current level of comfort. This is the rst step in helping clients achieve improved comfort.
Sources of assessment data to determine level of comfort can be subjective, objective, primary, or secondary
(Kolcaba, 2012; Wilkinson & VanLeuven, 2007).
Comfort is a holistic state under which pain management is included. Management of discomforts, how-
C
ever, can be better managed, and with fewer analgesics, by also addressing other comfort needs such as anxi-
ety, insufcient information, social isolation, or nancial difculties. CEB: One randomized study (N = 53)
found that female breast cancer clients undergoing radiation therapy rated their overall comfort as being greater
than the sum of the hypothesized components of comfort, which provided evidence for the theory of the holistic
nature of comfort (Kolcaba & Steiner, 2000, in Kolcaba, 2012).
Assist clients to understand how to rate their current state of holistic comfort, utilizing institutions pre-
ferred method of documentation. Documentation of comfort prenursing and postnursing interactions is
essential to demonstrating the efcacy of nursing activities (Kolcaba, 2003; Kolcaba, Tilton, & Drouin, 2006,
in Kolcaba, 2012).
Enhance feelings of trust between the client and the health care provider. To attain the highest comfort
level, clients must be able to trust their nurse (Kolcaba, 2003; Kolcaba et al, 2004). CEB: This randomized
design (N = 31) demonstrated the importance of promoting open relationships with clients, which helps to
acknowledge their individuality. Knowing the client/signicant others is essential in the provision of optimum
palliative and terminal care (Kolcaba et al, 2004, in Kolcaba, 2012).
Manipulate the environment as necessary to improve comfort. CEB: In two experimental studies, the pro-
tocol included that all clients be asked about preferences for light, furnishings, body position, television settings,
etc. (Kolcaba et al, 2004; Dowd et al, 2007, in Kolcaba, 2012).
Encourage early mobilization and provide routine position changes to decrease physical discomforts asso-
ciated with bed rest. CEB: An experimental study of 420 individuals following nonemergency cardiac cathe-
terization found consistently lower scores for back discomfort with no increase in bleeding in the intervention
group, when they were turned every hour (Chair et al, 2003). A review comparing the study by Chair et al
found its results to be consistent with other studies that have found that backrest elevation, side lying, and early
ambulation all improved comfort (Benson, 2004).
Provide simple massage. CEB: Two experiments, one with 31 and one with 60 clients, demonstrated that
hand massage was helpful for reducing discomfort and anxiety and promoting relaxation and sleep (Kolcaba
et al, 2004; Kolcaba, Schirm, & Steiner, 2006).
Provide healing touch, which is well-suited for clients who cannot tolerate more stimulating interventions
such as simple massage. EBN: In an experiment (N = 58), college students experienced enhanced comfort
immediately after healing touch, compared to their baseline comfort level (Dowd et al, 2007).
Inform the client of options for control of discomfort such as meditation and guided imagery, and pro-
vide these interventions if appropriate. CEB: A study found that female breast cancer clients (N = 53) treated
with guided imagery while undergoing radiation therapy had signicant improvements in comfort compared
with the control group (Kolcaba, 2003).
Utilize empathy as a response to a clients negative emotions. EBN: An evaluation interaction analysis
found that an accurate empathic response to a clients expressions of negative emotions can contribute to com-
fort (Eide, Sibbern, & Johannessen, 2011).
Encourage clients to use relaxation techniques to reduce pain, anxiety, depression, and fatigue. EBN: In a
systematic review of randomized controlled studies, it was found that relaxation training was effective for
decreasing pain intensity, anxiety, depression, and fatigue in clients with chronic musculoskeletal pain (Pers-
son et al, 2008).
Geriatric
Utilize hand massage for elders because most respond well to touch and the providers presence. EBN: In
an experiment (N = 60), the effects of hand massage on comfort of nursing home residents was found to be
signicant immediately after the massage compared to residents who did not receive hand massage (Kolcaba,
Schirm, & Steiner, 2006, in Kolcaba, 2012).
*In updating these comfort interventions, Dr. Kolcaba wishes to acknowledge the invaluable assistance of Katharine K. Mayer, RN,
MSN, of University Hospitals of Cleveland and Kimberly N. Fiolliett-Vranic, MSN, RN, Coronary Care Unit, Cleveland Clinic Foun-
dation.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
212 Impaired comfort
Discomfort from cold can be treated with warmed blankets. EBN: This study (N = 126) found signicantly
increased comfort and decreased anxiety in clients who used self-controlled warming gowns (Wagner, Byrne, &
Kolcaba, 2006).
Use complementary touch therapies such as reexology on clients with dementia to reduce pain and
stress. EBN: In a study conducted on nursing home residents (N = 21), it was found that reexology was an
C effective treatment of stress and observed pain in residents with mild to moderate dementia (Hodgson &
Andersen, 2008).
Acknowledge any unmet physical, psychological, emotional, spiritual, and environmental needs when
attempting to understand the behavior of an elderly client with dementia. As caregivers, all possible causes
for demented elderly clients behavior must be considered to maximize comfort (Gallaher & Long, 2011).
Provide simple massage. EBN: A prospective study design (N = 52) found that providing massage to nursing
home residents with dementia was effective in controlling agitation (Holliday-Welsh, Gessert, & Renier, 2009).
Multicultural
Identify and clarify cultural language used to describe pain and other discomforts. CEB: Clients may
interchange words meaning discomfort and pain, may refer to minor discomforts as pain, or may not discuss
non-painful discomforts at all (Kolcaba, 2003).
Assess skin for ashy or yellow-brown appearance. Black skin appears ashy and brown skin appears yellow-
brown when clients have pallor sometimes associated with discomfort (Peters, 2007).
Use soap sparingly if the skin is dry. Black skin tends to be dry, and soap will exacerbate this condition.
Encourage and allow clients to practice their own cultural beliefs and recognize the impact different cul-
tures have on a clients belief about health care, suffering, and decision-making. Hindus believe in reincar-
nation, which gives them comfort during the dying process. Hindus also believe that physical suffering can lead
to spiritual growth (Thrane, 2010).
Assess for cultural and religious beliefs when providing care to clients. EBN: In a hermeneutic phenomeno-
logical study conducted in six medical-surgical wards in Iran (N = 22), it was found that family members play
an important role in the comfort of the patient. It was also found that caregivers should allow patients to follow
religious and traditional principles to facilitate comfort despite physical constraints (Youse et al, 2009).
Client/Family Teaching and Discharge Planning
Teach techniques to use when the client is uncomfortable, including relaxation techniques, guided imag-
ery, hypnosis, and music therapy. EBN: Interventions such as progressive muscle relaxation training, guided
imagery, and music therapy can effectively decrease the perception of uncomfortable sensations, including pain
(Kolcaba, 2003). CEB & EBN: Families want to learn how to provide comfort measures to their loved ones who
are uncomfortable. (Kolcaba et al, 2004, in Kolcaba, 2012).
Instruct the client and family on prescribed medications and therapies that improve comfort (Kolcaba, 2003).
Teach the client to follow up with the physician or other practitioner if discomfort persists (Kolcaba,
2003).
Encourage clients to utilize the Internet as a means of providing education to complement medical care
for those who may be homebound or unable to attend face-to-face education. EBN: In a randomized trial
with intervention (N = 41), it was found that the Internet was an effective mode for delivering self-care educa-
tion to older clients with chronic pain (Berman et al, 2009).
Mental Health
Encourage clients to use guided imagery techniques. EBN: A quasi-experimental design (N = 60) found that
patients who listened to a guided imagery compact disk once a day for 10 days had improved comfort and
decreased depression, anxiety, and stress over time (Apstolo & Kolcaba, 2009, in Kolcaba, 2012).
Provide psychospiritual support and a comforting environment in order to enhance comfort. EBN: In a
cross-sectional descriptive study (N = 98), it was found that cancer patients had lower comfort levels relating
to psychospiritual and environmental comfort than to physical and sociocultural comfort. Improvements in
psychospiritual and environmental support will enhance overall comfort (Kim & Kwon, 2007).
Providing music and verbal relaxation therapy can reduce anxiety. EBN: A literature review found that
music and verbal relaxation therapy provided reduced chemotherapy-induced anxiety (Lin et al, 2011).
Caregivers should not hesitate to use humor when caring for their clients. EBN: Analysis of two studies
found that humor can be comforting and can contribute to a positive experience for both patient and caregiver
(Kinsman-Dean & Major, 2008).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Readiness for enhanced comfort 213
REFERENCES
Benson G: Changing patients position in bed after non-emergency Kinsman-Dean RA, Major JE: From critical care to comfort care: the
coronary angiography reduced back pain, Evid Based Nurs 7(1):19, sustaining value of humour, J Clin Nurs 17:10881095, 2008.
2004. Kolcaba K: Comfort theory and practice: a holistic vision for health care,
Berman RLH, et al: The effectiveness of an online mind-body interven- New York, 2003, Springer.
tion for older adults with chronic pain, J Pain 10(1):6879, 2009.
Chair SY, et al: Effect of positioning on back pain after coronary angiog-
Kolcaba K: TheComfortLine.com. Retrieved June 21, 2012, from www.
TheComfortLine.com.
C
raphy, J Adv Nurs 42(5):470478, 2003. Kolcaba K, et al: Efcacy of hand massage for enhancing comfort of
Dowd T, et al: Comparison of healing touch and coaching on stress and hospice patients, J Hospice Palliat Care 6(2):91101, 2004.
comfort in young college students, Holist Nurs Pract 21(4):194202, Kolcaba K, Schirm V, Steiner R: Effects of hand massage on comfort of
2007. nursing home residents, Geriatr Nurs 27(2):8591, 2006.
Eide H, Sibbern T, Johannessen T: Empathic accuracy of nurses Lin MF, et al: A randomized controlled trial of the effect of music
immediate response to bromyalgia patients expressions of nega- therapy and verbal relaxation on chemotherapy-induced anxiety,
tive emotions: an evaluation using interaction analysis, J Adv Nurs J Clin Nurs 20:988999, 2011.
67(6):12421253, 2011. Persson AL, et al: Relaxation as a treatment for chronic musculoskeletal
Gallaher M, Long DO: Demystifying behaviors, addressing pain, and paina systematic review of randomized controlled studies, Phys
maximizing comfort research and practice: partners in care, J Hos- Ther Rev 13(5):355365, 2008.
pice Palliat Nurs 13(2):7178, 2011. Peters J: Examining and describing skin conditions, Pract Nurse
Hodgson N, Andersen S: The clinical efcacy of reexology in nursing 34(8):3940, 43, 45, 2007.
home residents with dementia, J Altern Complement Med 14(3):269 Thrane S: Hindu end of life, J Hospice Palliat Nurs 12(6):337342, 2010.
275, 2008. Wagner D, Byrne M, Kolcaba K: Effect of comfort warming on preop-
Holliday-Welsh D, Gessert C, Renier C: Massage in the management erative patients, AORN J 84(3):113, 2006.
of agitation in nursing home residents with cognitive impairment, Wilkinson J, VanLeuven K: Fundamentals of nursing, Philadelphia,
Geriatr Nurs 30(2):108117, 2009. 2007, FA Davis.
Kim KS, Kwon SH: Comfort and quality of life of cancer patients, Asian Youse H, et al: Comfort as a basic need in hospitalized patients in Iran:
Nurs Res 1:125135, 2007. hermeneutic phenomenology study, J Clin Nurs 65(9):18911898, 2009.
Readiness for enhanced Comfort Natalie Fischetti, PhD, RN
NANDA
Definition
A pattern of ease, relief and transcendence in physical, psychospiritual, environmental, and/or social dimen-
sions that is sufcient for well-being and can be strengthened
Defining Characteristics
Expresses desire to enhance comfort; expresses desire to enhance feelings of contentment; expresses desire to
enhance relaxation; expresses desire to enhance resolution of complaints
NOC Outcomes (Nursing Outcomes Classification)
Suggested NOC Outcomes
Client Satisfaction: Caring, Symptom Control, Comfort Status, Coping, Hope, Motivation, Pain Control,
Participation in Health Care Decisions, Spiritual Health
Example NOC Outcomes with Indicators
Comfort Status as evidenced by the following indicators: Physical well-being/Symptom control/Psychological well-being. (Rate
the outcome and indicators of Comfort Level: 1 = not at all satisfied, 2 = somewhat satisfied, 3 = moderately satisfied,
4 = very satisfied, 5 = completely satisfied.)
Client Outcomes
Client Will (Specify Time Frame):
Assess current level of comfort as acceptable
Express the need to achieve an enhanced level of comfort
Identify strategies to enhance comfort
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
214 Readiness for enhanced comfort
Perform appropriate interventions as needed for increased comfort
Evaluate the effectiveness of interventions at regular intervals
Maintain an enhanced level of comfort when possible
NIC Interventions (Nursing Interventions Classification)
C Suggested NIC Interventions
Calming Technique, Cutaneous Stimulation, Environmental Management, Comfort, Heat/Cold Applica-
tion, Hope Inspiration, Humor, Meditation Facilitation, Music Therapy, Pain Management, Presence, Sim-
ple Guided Imagery, Simple Massage, Simple Relaxation Therapy, Spiritual Growth Facilitation, Therapeutic
Play, Therapeutic Touch, Touch, Distraction
Example NIC ActivitiesSpiritual Growth Facilitation
Assist the patient with identifying barriers and attitudes that hinder growth or self-discovery; Assist the patient to explore beliefs as
related to healing of the body, mind, and spirit; Model healthy relating and reasoning skills
Nursing Interventions and Rationales
Assess clients current level of comfort. This is the rst step in helping clients to achieve enhanced comfort.
Sources of assessment data to determine level of comfort can be subjective, objective, primary, secondary, focused,
or even special needs (Wilkinson & VanLeuven, 2007). While clinicians are assessing pain more frequently, this
has not resulted in widespread pain reduction. A solution may be to establish comfort-function goals for clients,
reminding clients to tell their nurse when pain interferes with function (Pasero & McCaffrey, 2004).
Help clients understand that enhanced comfort is a desirable, positive, and achievable goal. CEB: Human
beings strive to have their basic comfort needs met, but comfort is more than just the absence of pain (Kolcaba,
2003). Comfort is best recognized when a person leaves the state of discomfort and nurses can enhance their
clients comfort in everyday practice (Malinowski & Stamler, 2002).
Enhance feelings of trust between the client and the health care provider. CEB: To attain the highest com-
fort level a client must be able to trust the nurse (Hupcey, Penrod, & Morse, 2000) EBN: Patients had greater
feelings of emotional comfort when they felt secure, informed and valued (Williams, Dawson, & Kristjanson,
2009). EBN: Trust is an essential element in the nurse-patient relationship (Bell & Duffy, 2009).
Use therapeutic massage for enhancement of comfort. CEB: This study determined the effects of hand
massage on clients near the end of life, with clients reporting feeling special and that the massage felt good.
Also, meaningful connectedness was achieved (Kolcaba et al, 2004). Massage is helpful for low back pain
and other orthopedic problems (Dryden, Baskwill, & Preyde, 2004). EBN: Women who received massage in
the latent labor period prior to delivery had less pain perception than women who did not (Yildirim &
Sahin, 2004).
Teach and encourage use of guided imagery. Guided imagery can be helpful on pain level, physical func-
tional status, and self-efcacy on persons with bromyalgia (Menzies, Taylor, & Bourguignon, 2006). Visual
imagery with mind-body relaxation may be used for symptom control in Hispanic persons diagnosed with
bromyalgia (Menzies & Kim, 2008). EBN: Guided imagery was utilized in a study of psychiatric patients and
was found to signicantly improve their comfort level (Apstolo & Kolcaba, 2009). Guided imagery was used
to relieve postoperative pain in elderly orthopedic patients.
Use of heat application to enhance pain relief. EBN: Heat can be helpful with pain management of women
with perineal pain during the second stage of labor; 79.9% of women identied relief of perineal pain with the
use of warm packs during the second stage of labor. Eighty-ve percent of these women found it so effective that
they would use it during subsequent births (Dahlen et al, 2009).
Foster and instill hope in clients whenever possible. EBN: This study was the rst to document the effective-
ness of a brief hope intervention. The intervention produced a signicant effect on pain tolerance. The increase
in pain tolerance was stronger for females than males (Berg, Snyder, & Hamilton, 2008). See the care plan for
Hopelessness.
Provide opportunities for and enhance spiritual care activities. The need for comfort and reassurance may
be perceived as spiritual needs. To meet these needs, nurses engaged in interaction when they comforted and
assured clients. Participants also identied absolution as a spiritual need, and there is evidence that forgiveness
may bring one feelings of joy, peace, elation, and a sense of renewed self-worth (Narayanasomy et al, 2004).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Readiness for enhanced comfort 215
Individuals who practiced spiritual meditation were found to have a greater increase in pain tolerance (Wach-
holtz & Pargament, 2008).
Enhance social support and family involvement. EBN: Methods to help terminally ill clients and their fami-
lies transition from cure to comfort care included spending an increased amount of time with ones family,
appointing one close friend to act as a contact person for other friends, and establishing an email list serve for
updates of a clients status and care (Duggleby & Berry, 2005). C
Encourage mind-body therapies such as meditation as an enhanced comfort activity. EB: The most com-
mon therapies used were meditation, imagery, and yoga. Research demonstrating the connection between the
mind and body has therefore increased interest in the potential use of these therapies (Wolsko et al, 2004).
EBN: Meditation has been shown to reduce anxiety, relieve pain, decrease depression, enhance mood and self-
esteem, decrease stress, and generally improve clinical symptoms (Bonadonna, 2003). A review of clinical trials
for meditation and massage used in end of life found that there was a signicant relationship between medita-
tion and pain reduction in the two studies that assessed pain (Lafferty et al, 2006).
Promote participation in creative arts and activity programs. EBN: A creative arts program for caregivers of
cancer clients was shown to lower anxiety, and positive emotions were expressed (Walsh, Martin, & Schmidt,
2004). The use of an individualized music protocol program by elderly women was shown to promote and
maintain sleep (Johnson, 2003).
Encourage clients to use health information technology (HIT) as needed. Client services can now include
management of medications, symptoms, emotional support, health education, and health information
(Moody, 2005). EBN: Injured car occupants experienced signicantly lower dimensions of pain and discom-
fort with nursing intervention via telephone (Franzen et al, 2009).
Evaluate the effectiveness of all interventions at regular intervals and adjust therapies as necessary. It is
important for nurses to determine comfort and pain management goals because comfort goals will change with
circumstances. Ask questions and ask them frequently, such as How is your comfort? Establish guidelines for
frequency of assessment and document responses noting if goals are being met (Kolcaba, 2003). EB: A compre-
hensive palliative care project was conducted at 11 sites. The interdisciplinary review process built trust,
endorsed creativity, and ultimately resulted in better meeting the needs of clients, families, and the community
(London et al, 2005). Evaluation must be planned for, ongoing, and systematic. Evaluation demonstrates car-
ing and responsibility on the part of the nurse (Wilkinson & VanLeuven, 2007).
Explain all procedures, including sensations likely to be experienced during the procedure. EBN: Patients
undergoing abdominal surgery in an experimental group received routine care and a preoperative nursing
intervention which included explaining the causes of pain that would occur due to the operation, explaining
the inuences of postoperative pain and the importance of early out-of-bed activities, teaching how to reduce
pain using nonpharmacological methods, encouraging requesting pain medications after surgery, encouraging
expression of feelings and concerns, and setting a pain control goal. This group had a signicant decrease in
postoperative anxiety and a statistically signicantly lower postoperative pain intensity 4 hours and 24 hours
after the surgical procedure (Lin & Wang, 2004).
Pediatric
Assess and evaluate childs level of comfort at frequent intervals. Comfort needs should be individually
assessed and planned for. With assessment of pain in children, it is best to use input from the parents or a
primary care provider. Use only accepted scales for standardized pain assessment (Remke & Chrastek,
2007).
Skin-to-skin contact (SSC) and selection of most effective method improves the comfort of newborns
during routine blood draws. EB: Premature infants who received skin-to-skin contact demonstrated a
decrease in pain reaction during heel lancing (Castral et al, 2008).
Adjust the environment as needed to enhance comfort. Environmental comfort measures include maintain-
ing orderliness; quiet; minimizing furniture; special attention to temperature, light and sound, color, and
landscape (Kolcaba & DeMarco, 2005).
Encourage parental presence whenever possible. The same basic principles for managing pain in adults
and children apply to neonates. In addition to other comfort measures, parental presence should be encour-
aged whenever possible (Pasero, 2004). EBN: This study reported the effects of co-residence and caregiving on
the parents of children dying with AIDS. Although parents who did more caregiving did experience anxiety,
insomnia, and fatigue, the caregiving experiences for many parents gave them an opportunity to fulll their
perceived duty as parents before their child died. This in turn resulted in better physical and emotional health
outcomes (Kespichayawattana & VanLandingham, 2003).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
216 Readiness for enhanced comfort
Promote use of alternative comforting strategies such as positioning, presence, massage, spiritual care,
music therapy, art therapy, and story-telling to enhance comfort when needed. In addition to oral sucrose,
other comfort measures should be used to alleviate pain such as swaddling, skin-to-skin contact with
mother, nursing, rocking, and holding (Pasero, 2004). EBN: Building on the belief that parents are the
primary care providers and health care resource for families, the blended infant massageparenting program
C is effective for both mother and infant (Porter & Porter, 2004). EBN: In this study, focus groups were con-
ducted with Moroccan pediatric oncology nurses and physicians to better understand how pain management
was achieved in children with cancer. When no medication was available to relieve pain, other techniques were
used to comfort clients. These included use of cold therapy, presence, holding a childs hand, utilizing distrac-
tion techniques, playing with them, story-telling, and encouraging parental engagement activities (McCarthy
et al, 2004). EB: In a study that examined the effects of music on pain in a pediatric burn unit during nursing
procedures, the use of music during procedures reduced pain (Whitehead-Pleaux et al, 2007). EBN: A Talk
and Touch intervention by the mothers of PICU infants found that 62 percent of the mothers felt that the
intervention made a difference in the pain the infant experienced and 73 percent felt that talk and touch
decreased their infants distress (Rennick et al, 2011).
Support childs spirituality. CEB: Children are born with an intrinsic spiritual essence that can be enhanced.
Spirituality promotes a sense of hope, comfort, and strength and creates a sense of being loved and nurtured by
a higher power (Elkins & Cavendish, 2004).
Multicultural
Identify cultural beliefs, values, lifestyles, practices, and problem-solving strategies when assessing
clients. Cultural sensitivity must always be a component of pain assessment. The nurse must remember
that pain expression will vary among clients and that variation must also be acknowledged within cultures
(Andrews & Boyle, 2003). EBN: In a qualitative study that identied issues in pain management, cultural
beliefs were cited as impediments or barriers to pain management; for example, some Moroccan physicians
felt illness-related pain was inevitable, that suffering was normal, and that it had to be endured, especially
by boys (McCarthy et al, 2004). EBN: In a qualitative study, Muslim patients, particularly Shiites,
expressed feeling more comfortable when they were allowed to practice their religious beliefs (Youse et al,
2009).
Enhance cultural knowledge by actively seeking out information regarding different cultural and ethnic
groups. Cultural knowledge is the process of actively seeking information about different cultural and ethnic
groups such as their world views, health conditions, health practices, use of home remedies or self-medication,
barriers to health care, and risk-taking or health-seeking behaviors (Institute of Medicine, 2002).
Recognize the impact of culture on communication styles and techniques. Communication and culture are
closely intertwined, and communication is the way culture is transmitted and preserved. It inuences how feel-
ings are expressed, decisions are made, and what verbal and nonverbal expressions are acceptable. By the age
of 5, cultural patterns of communication can be identied in children (Giger & Davidhizar, 2004).
Provide culturally competent care to clients from different cultural groups. Cultural competency requires
health care providers to act appropriately in the context of daily interactions with people who are different from
themselves. Providers need to honor and respect the beliefs, interpersonal styles, attitudes, and behaviors of
others. This level of cultural awareness requires providers to refrain from forming stereotypes and judgments
based on ones own cultural framework (Institute of Medicine, 2002). EBN: The ndings from a review of two
studies of Japanese and American women suggest that although there were common ethical concerns between
the two cultures, the cultural context of the underlying values may create very different meanings and result in
different nursing practices (Wros, Doutrich, & Izumi, 2004).
Home Care
The nursing interventions described previously in Readiness for enhanced Comfort may be used with
clients in the home care setting. When needed, adaptations can be made to meet the needs of specic
clients, families, and communities.
Make appropriate referrals to other organizations or providers as needed to enhance comfort. Referrals
should have merit, be practical, timely, individualized, coordinated, and mutually agreed upon by all involved
(Hunt, 2005).
Promote an interdisciplinary approach to home care. Members of the interdisciplinary team who provide
specialized care to enhance comfort can include the physician, physical therapist, occupational therapist,
nutritionist, music therapist, social worker, etc. (Stanhope & Lancaster, 2006).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Readiness for enhanced comfort 217
Evaluate regularly if enhanced comfort is attainable in the home care setting. Home health agencies moni-
tor client outcomes closely. Evaluation is an ongoing process and is essential for the provision of quality care
(Stanhope & Lancaster, 2006).
Use music therapy at home. EBN: The use of music 30 minutes prior to peak agitation in dementia patients
demonstrated that their mean pain levels after listening to music were signicantly lower than before the music
intervention (Park, 2010). C
Client/Family Teaching and Discharge Planning
Teach client how to regularly assess levels of comfort.
Instruct client that a variety of interventions may be needed at any given time to enhance comfort.
Help clients to understand that enhanced comfort is an achievable goal.
Teach techniques to enhance comfort as needed.
When needed, empower clients to seek out other health professionals as members of the interdisciplinary
team to assist with comforting measures and techniques.
Encourage self-care activities and continued self-evaluation of achieved comfort levels to ensure enhanced
comfort will be maintained.
REFERENCES
Andrews M, Boyle J: Transcultural concepts in nursing, ed 4, Philadel- Kolcaba K, DeMarco M: Comfort theory and application to pediatric
phia, 2003, Lippincott Williams & Wilkins. nursing, Pediatr Nurs 31(3):187194, 2005.
Apstolo J, Kolcaba K: The effects of guided imagery on comfort, Kolcaba K, et al: Efcacy of hand massage for enhancing the comfort of
depression, and stress of psychiatric inpatients with depressive hospice patients, Int J Palliat Nurs 6(2):91102, 2004.
disorders, Arch Psychiatr Nurs 23(6):403411, 2009. Lafferty W, et al: Evaluating CAM treatment at the end of life: a review
Bell L, Duffy A: A concept analysis of nurse-patient trust, Br J Nurs of clinical trials for massage and meditation, Complement Ther Med
(BJN) 18(1):4651, 2009. 14(2):100112, 2006.
Berg C, Snyder C, Hamilton N: The effectiveness of a hope interven- Lin L, Wang R: Abdominal surgery, pain and anxiety, J Adv Nurs
tion in coping with cold pressor pain, J Health Psychol 13:804 51(3):252260, 2004.
809, 2008. London M, et al: Evaluation of a comprehensive, adaptable, life-
Bonadonna R: Meditations impact on chronic illness, Holist Nurs Pract afrming, longitudinal palliative care project, J Palliat Med
17(6):309319, 2003. 8(6):12141225, 2005.
Castral T, et al: The effects of skin-to-skin contact during acute pain in Malinowski A, Stamler L: Comfort: exploration of the concept in nurs-
preterm newborns, Eur J Pain 12(4):464471, 2008. ing, J Adv Nurs 39(6):599606, 2002.
Dahlen H, et al: Soothing the ring of re: Australian womens and McCarthy P, et al: Managing childrens cancer pain in Morocco, J Nurs
midwives experiences of using perineal warm packs in the second Scholarsh 36(1):1115, 2004.
stage of labor, Midwifery 25(2):e39e48, 2009. Menzies V, Kim S: Relaxation and guided imagery in Hispanic persons
Dryden T, Baskwill A, Preyde M: Massage therapy for the orthopaedic diagnosed with bromyalgia: a pilot study, Fam Commun Health
patient: a review, Orthop Nurs 23:327332, 2004. 31(3):204212, 2008.
Duggleby W, Berry P: Transitions and shifting goals of care for palliative Menzies V, Taylor A, Bourguignon C: Effects of guided imagery on
patients and their families, Clin J Oncol Nurs 9(4):425428, 2005. outcomes of pain, functional status, and self-efcacy in persons
Elkins M, Cavendish R: Developing a plan for pediatric spiritual care, diagnosed with bromyalgia, J Altern Complement Med 12(1):2330,
Holist Nurs Pract 18(4):179184, 2004. 2006.
Franzen C, et al: Injured road users health-related quality of life after Moody L: E-health web portals: delivering holistic healthcare and mak-
telephone intervention: a randomized controlled trial, J Clin Nurs ing home the point of care, Holist Nurs Pract 19(4):156160, 2005.
18(1):108116, 2009. Narayanasomy A, et al: Responses to the spiritual needs of older people,
Giger J, Davidhizar R: Transcultural nursing: assessment and interven- J Adv Nurs 48(1):616, 2004.
tion, ed 4, St. Louis, 2004, Mosby. Park H: Effects of music on pain for home-dwelling persons with
Hunt R: Introduction to community-based nursing, ed 3, Philadelphia, dementia, Pain Manag Nurs 11(3):141147, 2010.
2005, Lippincott. Pasero C: Pain relief for neonates, Am J Nurs 104(5):4447, 2004.
Hupcey JE, Penrod J, Morse JM: Establishing and maintaining trust Pasero C, McCaffrey M: Comfort-function goals, Am J Nurs 104(9):77
during acute care hospitalizations, including commentary by Robin- 81, 2004.
son CA, Sch Inq Nurs Pract 14(3):227248, 2000. Porter L, Porter B: A blended infant massageparenting enhancement
Institute of Medicine: Speaking of health, Washington, DC, 2002, program for recovering substance abusing mothers, Pediatr Nurs
National Academies Press. 30(5):363401, 2004.
Johnson J: The use of music to promote sleep in older women, J Com- Remke S, Chrastek J: Improving care in the home for children with pal-
munity Health Nurs 20:2735, 2003. liative care needs, Home Healthc Nurse 25(1):4551, 2007.
Kespichayawattana J, VanLandingham M: Effects of coresidence and Rennick J, et al: Mothers experiences of touch and talk nursing inter-
caregiving on health of Thai parents of adult children with AIDS, J vention to optimise pain management in the PICU: a qualitative
Nurs Schol 35(3):217224, 2003. study, Intensive Crit Care Nurs 27(3):151157, 2011.
Kolcaba K: Comfort theory and practice, New York, 2003, Springer. Stanhope M, Lancaster J: Foundation of nursing in the community, ed 2,
St. Louis, 2006, Mosby.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
218 Readiness for enhanced communication
Wachholtz A, Pargament K: Migraines and meditation: does spirituality Wolsko P, et al: Use of mind-body medical therapies, J Gen Intern Med
matter? J Behav Med 31(4):351366, 2008. 19:4350, 2004.
Walsh S, Martin S, Schmidt L: Testing the efcacy of a creative-arts Wros P, Doutrich D, Izumi S: Ethical concerns: comparison of values
intervention with family caregivers of patients with cancer, J Nurs from two cultures, Nurs Health Sci 6(2):131140, 2004.
Scholarsh 36(3):214219, 2004. Yildirim G, Sahin N: The effect of breathing and skin stimulation
Whitehead-Pleaux AM, et al: Exploring the effects of music therapy on techniques on labour pain perception of Turkish women, Pain Res
C pediatric pain: phase 1, J Music Ther 46(3):217241, 2007.
Wilkinson J, VanLeuven K: Fundamentals of nursing, Philadelphia,
Manag 9(4):183187, 2004.
Youse H, et al: Comfort as a basic need in hospitalized patients in Iran:
2007, FA Davis. a hermeneutic phenomenology study, J Adv Nurs 65(9):18911898,
Williams A, Dawson S, Kristjanson L: Patients felt greater personal 2009.
control and emotional comfort in hospital when they felt secure,
informed, and valued, Evid Based Nurs 12(1):29, 2009.
Readiness for enhanced Communication
Stacey M. Carroll, PhD, ANP-BC, and Suzanne White, MSN, RN, PHCNS-BC
NANDA-I
Definition
A pattern of exchanging information and ideas with others that is sufcient for meeting ones needs and lifes
goals and can be strengthened
Defining Characteristics
Able to speak a language; able to write a language; expresses feelings; expresses satisfaction with ability to
share ideas with others; expresses satisfaction with ability to share information with others; expresses
thoughts; expresses willingness to enhance communication; forms phrases; forms sentences; forms words;
interprets nonverbal cues appropriately; uses nonverbal cues appropriately
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Communication, Communication: Expressive, Receptive
Example NOC Outcome with Indicators
Communication as evidenced by the following indicators: Use of spoken language/Use of written language/Acknowledgment
of messages received/Exchanges messages accurately with others. (Rate the outcome and indicators of Communication: 1 =
severely compromised, 2 = substantially compromised, 3 = moderately compromised, mildly compromised, 5 = not compromised
[see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Express willingness to enhance communication
Demonstrate ability to speak or write a language
Form words, phrases, and language
Express thoughts and feelings
Use and interpret nonverbal cues appropriately
Express satisfaction with ability to share information and ideas with others
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Active Listening, Communication Enhancement: Hearing Decit, Communication Enhancement: Speech
Decit
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Readiness for enhanced communication 219
Example NIC ActivityCommunication Enhancement: Hearing Deficit
Listen attentively; allowing patient adequate time to process communication and respond; Verify what was said or written using
patients response before continuing
Nursing Interventions and Rationales C
Establish a therapeutic nurse-client relationship: provide appropriate education for the client, demon-
strate caring by being present to the client. CEB: Clients who were nonvocal and ventilated appreciated
nursing care that was delivered in an individualized, caring manner (Carroll, 2007).
Assess the clients readiness to communicate, using an individualized approach. Avoid making assump-
tions regarding the clients preferred communication method. EBN: Using varied communication
approaches improved communication efciency and client engagement (Radtke et al, 2011).
Assess the clients literacy level. Screening clients literacy levels upon assessment using REALM (Rapid Esti-
mate of Adult Literacy in Medicine) allows providers to tailor information accordingly (Rajda & George, 2009).
Listen attentively and provide a comfortable environment for communicating; use these practical guide-
lines to assist in communication: Slow down and listen to the clients story; use augmentative and alterna-
tive communication methods (such as lip-reading, communication boards, writing, body language, and
computer/electronic communication devices) as appropriate; repeat instructions if necessary; limit the
amount of information given; have the client teach back to conrm understanding; avoid asking, Do
you understand?; be respectful, caring, and sensitive. EB: Multiple augmentative and alternative commu-
nication methods, applied with an individualized and creative approach, aid in facilitating communication
(Radtke et al, 2011).
Provide communication with specialty nurses such as clinical nurse specialists or nurse practitioners who
have knowledge about the clients situation. CEB: Clients report being well informed and having high satis-
faction with nurse practitioner communication (Hayes, 2007).
Refer couples in maladjusted relationships for psychosocial intervention and social support to strengthen
communication; consider nurse specialists. EB: Being part of a strong dyad may serve as a buffering factor
regarding post-traumatic stress related to a cancer diagnosis (Brosseau, McDonald, & Stephen, 2011).
Consider using music to enhance communication between client who is dying and his/her family. EB: In
clients with communication difculties, music therapy resulted in improvement in communication (Leow,
Drury, & Hong, 2010).
See care plan for Impaired verbal Communication.
Pediatric
All individuals involved in the care and everyday life of children with learning difculties need to have a
collaborate approach to communication. EB: Effective collaborative implementation can meet a wide range
of communication and learning needs (Greenstock & Wright, 2010).
See care plan for Impaired verbal Communication.
Geriatric
Assess for hearing and vision impairments and make appropriate referrals for hearing aids. Healthy People
2020 encourages early identication of people with hearing and vision loss (Healthy People 2020, 2011).
Use touch if culturally acceptable when communicating with older clients and their families. Touch has a calm-
ing effect on a client who may be frightened due to difculty with communication (Grossbach, Stranberg, &
Chan, 2011).
Consider singing during caregiving of clients with dementia. EB: When professional caregivers sang to cli-
ents with dementia during care, enhanced communication and cooperation resulted (Hammar et al, 2011).
See care plan for Impaired verbal Communication.
Multicultural
See care plan for Impaired verbal Communication.
Home Care
The interventions described previously may be used in home care.
See care plan for Impaired verbal Communication.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
220 Impaired verbal communication
Client/Family Teaching and Discharge Planning
See care plan for Impaired verbal Communication.
REFERENCES
C See Impaired verbal Communication for additional references.
Brosseau DC, McDonald MJ, Stephen JE: The moderating effect of Hammar LM, et al: Communicating through caregiver singing dur-
relationship quality in partner secondary traumatic stress among ing morning care situations in dementia care, Scand J Caring Sci
couples coping with cancer, Fam Syst Health 29(2):114126, 2011. 25:160168, 2011.
Carroll SM: Silent, slow lifeworld: the communication experiences of Hayes E: Nurse practitioners and managed care: patient satisfaction and
nonvocal ventilated patients, Qual Health Res 17(9):11651177, intention to adhere to nurse practitioner plan of care, J Am Acad
2007. Nurse Pract 19(8):418426, 2007.
Greenstock L, Wright J: Collaborative implementation: working Leow M, Drury V, Hong P: The experience and expectations of termi-
together when using graphic symbols, Child Lang Teach Ther nally ill patients receiving music therapy in the palliative setting: a
27(3):331343, 2010. systematic review, JBI Lib Syst Rev 8(27):10881111, 2010.
Grossbach I, Stranberg S, Chan L: Promoting effective communica- Rajda C, George NM: The effect of education and literacy levels on
tion for patients receiving mechanical ventilation, Crit Care Nurse health outcomes, JNP 5(2):115119, 2009.
31(3):4661, 2011.
Impaired verbal Communication
Stacey M. Carroll, PhD, ANP-BC, and Suzanne White, MSN, RN, PHCNS-BC
NANDA-I
Definition
Decreased, delayed, or absent ability to receive, process, transmit, and/or use a system of symbols
Defining Characteristics
Absence of eye contact; cannot speak; difculty expressing thoughts verbally (e.g., aphasia, dysphasia,
apraxia, dyslexia); difculty forming sentences; difculty forming words (e.g., aphonia, dyslalia, dysarthria);
difculty in comprehending usual communication pattern; difculty in maintaining usual communication
pattern; difculty in selective attending; difculty in use of body expressions; difculty in use of facial expres-
sions; disorientation to person; disorientation to space; disorientation to time; does not speak; dyspnea;
inability to speak language of caregiver; inability to use body expressions; inability to use facial expressions;
inappropriate verbalization; partial visual decit; slurring; speaks with difculty; stuttering; total visual de-
cit; verbalizes with difculty; willful refusal to speak
Related Factors (r/t)
Absence of signicant others; alteration in self-concept; alteration of central nervous system; altered percep-
tions; anatomic defect (e.g., cleft palate, alteration of the neuromuscular visual system, auditory system,
phonatory apparatus); brain tumor; chronic low self-esteem; cultural differences; decreased circulation to
brain; differences related to developmental; emotional conditions; environmental barriers; lack of informa-
tion; physical barrier (e.g., tracheostomy, intubation); physiological conditions; psychological barriers (e.g.,
psychosis, lack of stimuli); situational low self-esteem; stress; treatment-related side effects (e.g., pharmaceu-
tical agents); weakened musculoskeletal system
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Communication, Communication: Expressive, Receptive
Example NOC Outcome with Indicators
Communication as evidenced by the following indicators: Use of spoken and written language/Acknowledgment of messages
received/Exchanges messages accurately with others. (Rate the outcome and indicators of Communication: 1 = severely compro-
mised, 2 = substantially compromised, 3 = moderately compromised, 4 = mildly compromised, 5 = not compromised [see Section I].)
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Impaired verbal communication 221
Client Outcomes
Client Will (Specify Time Frame):
Use effective communication techniques
Use alternative methods of communication effectively
Demonstrate congruency of verbal and nonverbal behavior
Demonstrate understanding even if not able to speak
C
Express desire for social interactions
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Active Listening, Communication Enhancement: Hearing Decit, Communication Enhancement: Speech
Decit
Example NIC ActivitiesCommunication Enhancement: Hearing Deficit
Listen attentively; Allow client adequate time to process communication and respond; Verify what was said or written using clients
response before continuing
Nursing Interventions and Rationales
Assess the language spoken, cultural considerations, literacy level, cognitive level, and use of glasses and/
or hearing aids. A comprehensive nursing assessment assists in understanding any communication difculties
(Patak et al, 2009).
Determine clients own perception of communication difculties and potential solutions when possible.
EB: The Communication Condence Rating Scale for Aphasia (CCRSA) was found to be an effective tool for
assessment of the self-report of communication condence among clients with aphasia (Babbitt et al, 2011).
Involve a familiar person when attempting to communicate with a client who has difculty with com-
munication, if accepted by the client. EBN: Family members recognized clients cues and had a deeper under-
standing of clients needs (Dreyer & Nortvedt, 2008).
Listen carefully. Validate verbal and nonverbal expressions particularly when dealing with pain and utilize
nonverbal scales for pain when appropriate. EBN: The revised nonverbal pain scale (NVPS) was found to be
superior to the original NVPS in assessing pain in sedated clients receiving mechanical ventilation in the ICU
(Kabes, Graves, & Norris, 2009).
Use therapeutic communication techniques: speak in a well-modulated voice, use simple communica-
tion, maintain eye contact at the clients level, get the clients attention before speaking, and show concern
for the client. EB: Effective communication between clients and health care professionals facilitates positive
relations (Wain, Kneebone, & Billings, 2008).
Avoid ignoring the client with verbal impairment; be engaged and provide meaningful responses to client con-
cerns. EBN: Meaningful responses and emotional support by nurses facilitated organized behavior and initiative in
adults with communication impairments as a result of intellectual disabilities and autism (Bakken et al, 2008).
Use touch as appropriate. Touch has a calming effect on a client who may be frightened due to difculty with
communication (Grossbach, Stranberg, & Chan, 2011).
Use presence. Spend time with the client, allow time for responses, and make the call light readily avail-
able. Relationship-centered care involves the art of nursing, presence, and caring (Finfgeld-Connett, 2008).
Explain all health care procedures. CEB: Clients who were nonvocal and ventilated were attuned to every-
thing occurring around them, and they appreciated explanations from the nurse (Carroll, 2007). EB: Being
understood was described as important by those who were ventilated (Laasko, Hartelius, & Idvall, 2009) and
those who were deaf (Andrade et al, 2010).
Be persistent in deciphering what the client is saying, and do not pretend to understand when the message is
unclear. CEB: Persons who were nonvocal and ventilated appreciated persistence on the nurses part with respect
to being understood, and found it bothersome when others pretended to understand them (Carroll, 2007).
Utilize an individualized and creative multidisciplinary approach to augmentative and alternative com-
munication assistance and other interventions. EB: A combination of high-technology (with voice output)
and low-technology options improved communication efciency (Radtke et al, 2011). EBN: A story-telling
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
222 Impaired verbal communication
intervention with clients with dementia resulted in improved communication skills and social interaction
(Phillips, Reid-Arndt, & Pak, 2010).
Use consistent nursing stafng for those with communication impairments. CEB: Consistent nursing care
increased client-nurse communication and decreased client powerlessness (Carroll, 2007).
Consult communication specialists as appropriate. Speech language pathologists, audiologists, and inter-
C preters provide more comprehensive communication assistance for those with impaired communication
(Patak et al, 2009). LRTs are procient lipreaders who determine what a nonvocal client is mouthing and then
verbalize the clients words verbatim to others, in order to facilitate communication (Carroll, 2003; Grossbach,
Stranberg, & Chan, 2011).
When the client is having difculty communicating, assess and refer for audiology consultation for hear-
ing loss. Suspect hearing loss when:
Client frequently complains that people mumble, claims that others speech is not clear, or client hears
only parts of conversations.
Client often asks people to repeat what they said.
Clients friends or relatives state that client doesnt seem to hear very well, or plays the television or
radio too loudly.
Client does not laugh at jokes due to missing too much of the story.
Client needs to ask others about the details of a meeting that the client attended.
Client cannot hear the doorbell or the telephone.
Client nds it easier to understand others when facing them, especially in a noisy environment.
People with hearing loss do not hear sounds clearly. The loss may range from hearing speech sounds faintly or
in a distorted way to profound deafness (American Academy of Audiology, 2011).
When communicating with a client with a hearing loss:
Obtain clients attention before speaking and face toward his or her unaffected side or better ear while
allowing client to see speakers face at a reasonably close distance. Correct positioning increases the clients
awareness of the interaction and enhances the clients ability to communicate (Alexander Graham Bell
Association for the Deaf and Hard of Hearing, 2011).
Provide sufcient light and do not stand in front of window. Light illuminates the speakers face, making
expressions and lip movements clearer. Standing in front of a window causes glare, which impedes the clients
ability to clearly see the speaker (Alexander Graham Bell Association for the Deaf and Hard of Hearing, 2011).
Remove masks if safe to do so, or use see-through masks and reduce background noise whenever pos-
sible. Information on see-through masks: www.amphl.org. EB: Noise reduction reduced listening effort,
even in those who are hearing (Sarampalis et al, 2009).
Do not raise voice or overenunciate. This practice distorts the voice and lips, inhibiting effective lip-reading
(Middleton et al, 2010).
Avoid making assumptions about the communication choice of those with hearing loss or voice impair-
ments. EBN: After seeking client input, communication rounds or communication care plans can be com-
pleted (Happ et al, 2010).
Pediatric
Observe behavioral communication cues in infants. EB: Because they are preverbal, infants are completely
reliant on a caregiver in their immediate environment to be sensitive and recognize their distress (Riddle &
Racine, 2009).
Identify and dene at least two new forms of socially acceptable communication alternatives that may be
used by children with signicant disabilities. EB: Children with severe intellectual disabilities and little or no
spoken language may benet from the use of augmentative and alternative communication (AAC) strategies
such as the use of graphic symbols (Stephenson, 2009). EB: If distal gestures can be elicited, students with lim-
ited symbolic and intentional communication may show more communication independence, choice making,
and actions that affect daily routines (McLaughlin & Cascella, 2008).
Teach children with severe disabilities functional communication skills. EB: Students can develop func-
tional communication skills if they are given intensive, consistent communication interventions and a mecha-
nism for expressing themselves (Parker, Grimmett, & Summers, 2008).
Refer children with primary speech and language delay/disorder for speech and language therapy inter-
ventions. EB: Speech and language therapy services often target resources toward parents in order to address
issues of delay/difculty in children that could impact on school learning (Burns & Radford, 2008). EB: The
use of integrated treatment models that simultaneously target speech, phonological awareness, and reading is
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Impaired verbal communication 223
critical to ensure treatment is efcient and effective in improving these childrens oral and written language
development (McNeill, Gillon, & Dodd, 2009).
Geriatric
Carefully assess all clients for hearing difculty using an audiometer. Healthy People 2020 encourages early
identication of people with hearing loss (Healthy People 2020, 2011). C
Avoid use of elderspeak. EB: Using elderspeak, a speech style similar to baby talk that fails to communicate
appropriate respect, increases resistiveness to care in clients with dementia (Williams et al, 2009).
Initiate communication with the client with dementia, and give client time to respond. The responsibility
to use a creative approach and take the time to listen and understand clients who have dementia lies with the
clinician (Jootun & McGhee, 2011).
Encourage the client to wear hearing aids, if appropriate. EB: Hearing aid usage is low among older adults
with hearing loss, despite the benets of hearing aids (Golding et al, 2010; Gopinath et al, 2011). Older women
with poor hearing acuity had poorer balance and higher risk of falls in addition to communication difculties
(Viljanen et al, 2009).
Facilitate communication and reminiscing with memory boxes that contain objects, photographs, and writ-
ings that have meaning for the client. EB: Collage creation as a means of reminiscence facilitated the conveying
of information by older adults with dementia who had difculty communicating verbally (Stallings, 2010).
Continue to nd means to communicate even with those who are nonverbal. EB: Communication between
those with advanced dementia and their caregivers was enhanced using Adaptive-Interaction, a system that
recognizes nonverbal cues (Ellis & Astell, 2010).
Multicultural
Nurses should become more sensitive to the meaning of a cultures nonverbal communication modes, such
as eye contact, facial expression, touching, and body language. EBN: All cultural groups have rules regarding
patterns of social interaction. Culture inuences not only the manner in which feelings are expressed, but also
which verbal and nonverbal expressions of communication are considered appropriate (Ball, Bindler, &
Cowen, 2010).
Assess for the inuence of cultural beliefs, norms, and values on the clients communication process.
EBN: The nurse must be aware of personal beliefs about communication and control personal reactions by a
broadened understanding of the beliefs and behaviors of others (Giger & Davidhizar, 2008). EBN: Cultural
imposition may result when a health care provider is unaware of another persons beliefs and plans and imple-
ments care without taking into account the cultural beliefs of the client (Lewis et al, 2011).
Assess personal space needs, acceptable communication styles, acceptable body language, interpretation
of eye contact, perception of touch, and use of paraverbal modes when communicating with the client.
EBN: Nurses need to consider multiple factors when interpreting verbal and nonverbal messages (Giger &
Davidhizar, 2008).
Assess for how language barriers contribute to health disparities among ethnic and racial minorities. EBN:
Attending to linguistic differences is important not only because it can enhance the respectful treatment of typi-
cally vulnerable populations, but because it can help to prevent serious adverse outcomes (Carnevale et al, 2009).
EBN: Communication difculties are a major obstacle for immigrant clients and can lead to insufcient infor-
mation and poor quality nursing care in contrast to the majority population (Jirwe, Gerrish, & Emami, 2010).
Although touch is generally benecial, there may be certain instances where it may not be advisable due
to cultural considerations. CEB & EBN: Touch is largely culturally dened and conveys various meanings
depending on the clients culture (Leininger & McFarland, 2002; Lewis et al, 2011).
Modify and tailor the communication approach in keeping with the clients particular culture. EBN:
Along with having the knowledge, consideration, understanding, and respect for an individual, a tailoring or
adaptation must take place in an attempt to meet ones needs and demonstrate cultural sensitivity (Foronda,
2008).
Use reminiscence therapy as a language intervention. EB: Issues of culture, language, and aging are chal-
lenging. Less engaged residents and clients who are nonverbal, immobile, or who have other occupational per-
formance issues may become engaged in occupations of reminiscence that are rich in personal meaning and
relevance (Hodges & Schmidt, 2009).
The Ofce of Minority Health (OMH) of the U.S. Department of Health and Human Services (DHHS)
standards on culturally and linguistically appropriate services (CLAS) in health care should be used as
needed. EB: The recommended standards cover three broad areas of competence requirements for health care
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
224 Impaired verbal communication
for racial or ethnic minorities: (1) culturally competent care, (2) language access services, and (3) organiza-
tional support for cultural competence (CLAS, 2011).
Home Care
The interventions described previously may be adapted for home care use.
C Client/Family Teaching and Discharge Planning
Teach the client and family techniques to increase communication, including the use of communication
devices and tactile touch. Incorporate multidisciplinary recommendations. EB: Recommendations by SLPs
were omitted from discharge summaries at a high rate, placing clients at risk for lack of continuity of care
(Kind et al, 2011).
Refer the client to a speech-language pathologist (SLP) or audiologist. Audiological assessment quanties
and qualies hearing in terms of the degree of hearing loss, the type of hearing loss, and the conguration of
the hearing loss. Once a particular hearing loss has been identied, a treatment and management plan can be
put into place by an SLP (Baumgartner, Bewyer, & Bruner, 2008).
REFERENCES
Alexander Graham Bell Association for the Deaf and Hard of Hearing: Golding M, et al: Use of hearing aids and assistive listening devices in an
Communicating with people who have a hearing loss. Retrieved July older Australian population, J Am Acad Audiol 21(10):642653, 2010.
13, 2011, from http://agbell.org/NetCommunity/Document.Doc Gopinath B, et al: Incidence and predictors of hearing aid use and
?id=343. ownership among older adults with hearing loss, Ann Epidemiol
American Academy of Audiology: Hows your hearing? Retrieved July 21(7):497506, 2011.
13, 2011, from http://www.howsyourhearing.org. Grossbach I, Stranberg S, Chan L: Promoting effective communica-
Andrade PC, et al: Communication and information barriers to health tion for patients receiving mechanical ventilation, Crit Care Nurse
assistance for deaf patients, Am Ann Deaf 155(1):3137, 2010. 31(3):4661, 2011.
Babbitt EM, et al: Psychometric properties of the Communication Happ MB, et al: SPEACS-2: Intensive care unit communication
Condence Rating Scale for Aphasia (CCRSA): Phase 2, Aphasiology rounds with speech language pathology, Geriatr Nurs 31(3):170
25(6/7):727735, 2011. 177, 2010.
Bakken TL, et al: Effective communication related to psychotic disorga- Healthy People 2020: Hearing and other sensory or communication disor-
nized behavior in adults with intellectual disability and autism, Nord ders. Retrieved July 31, 2011, from www.healthypeople.gov/2020/top
J Nurs Res Clin Stud 28(2):913, 2008. icsobjectives2020/overviewaspx?topicid=20.
Ball JW, Bindler RC, Cowen KJ: Child health nursing: parenting with Hodges C, Schmidt R: An exploration of reminiscence and post-war
children and families, ed 2, Upper Saddle River, NJ, 2010, Pearson. European immigrants living in a multicultural aged-care setting in
Baumgartner CA, Bewyer E, Bruner D: Management of communication Australia, Occup Ther Int 16(2):154168, 2009.
and swallowing in intensive care: the role of the speech pathologist, Jirwe M, Gerrish K, Emami A: Student nurses experiences of com-
AACN Adv Crit Care 19(4):433443, 2008. munication in cross-cultural care encounters, Scand J Caring Sci
Burns A, Radford J: Parent-child interaction in Nigerian families: 24(3):436444, 2010.
conversation analysis, context and culture, Child Lang Teach Ther Jootun D, McGhee G: Effective communication with people who have
24(2):193209, 2008. dementia, Nurs Stand 25(25):4046, 2011.
Carroll SM: Lip-reading translating for non-vocal ventilated patients, Kabes AM, Graves JK, Norris J: Further validation of the nonverbal pain
JAMPHL Online 1(2), 2003. Retrieved November 26, 2006, from scale in intensive care patients, Crit Care Nurse 29(1):5966, 2009.
www.amphl.org. Kind A, et al: Omission of dysphagia therapies in hospital discharge
Carroll SM: Silent, slow lifeworld: the communication experiences of communications, Dysphagia 26(1):4961, 2011.
nonvocal ventilated patients, Qual Health Res 17(9):11651177, Laasko K, Hartelius L, Idvall M: Ventilator-supported communication:
2007. a case study of patient and staff experiences, J Med Speech Lang
Carnevale F, et al: Ethical considerations in cross-linguistic nursing, Pathol 17(4):153164, 2009.
Nurs Ethics 16(6):813826, 2009. Leininger MM, McFarland MR: Transcultural nursing: concepts, theories,
CLAS (Culturally and Linguistically Appropriate Services). Retrieved research and practices, ed 3, New York, 2002, McGraw-Hill.
December 2, 2011, from http://www.minorityhealth.hhs.gov/temp Lewis SL, et al: Medical surgical nursing: assessment and management of
lates/browse.aspx?lvl=2&lvlID=15. clinical problems, ed 8, St Louis, 2011, Elsevier.
Dreyer A, Nortvedt P: Sedation of ventilated patients in intensive care McLaughlin K, Cascella P: Eliciting a distal gesture via dynamic assess-
units: Relatives experiences, J Adv Nurs 61(5):549556, 2008. ment among students with moderate to severe intellectual disability,
Ellis M, Astell A: Communication and personhood in advanced demen- Commun Disord Q 29(2):7581, 2008.
tia, Healthc Couns Psychother J 10(3):3235, 2010. McNeill B, Gillon G, Dodd B: Phonological awareness and early reading
Finfgeld-Connett D: Qualitative convergence of three nursing con- development in childhood apraxia of speech (CAS), Int J Lang Com-
cepts: art of nursing, presence and caring, J Adv Nurs 63(5):527 mun Disord 44(2):175192, 2009.
534, 2008. Middleton A, et al: Communicating in a healthcare setting with people
Foronda C: A concept analysis of cultural sensitivity, J Transcult Nurs who have hearing loss, BMJ 341:c4672, 2010.
19(207):207212, 2008. Parker AT, Grimmett ES, Summers S: Evidence-based communica-
Giger J, Davidhizar R: Communication. In Giger J, Davidhizar R, edi- tion practices for children with visual impairments and additional
tors: Transcultural nursing: assessment and intervention, St Louis, disabilities: an examination of single-subject design studies, J Vis
2008, Mosby. Impair Blind 102(9):540552, 2008.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Acute confusion 225
Patak L, et al: Spotlight on improving patient-provider communication: Stephenson J: Picture-book reading as an intervention to teach the use
a call to action, J Nurs Admin 39(9):372376, 2009. of line drawings for communication with students with severe intel-
Phillips LJ, Reid-Arndt SI, Pak Y: Effects of a creative expression inter- lectual disabilities, AAC Augment Altern Commun 25(3):202214,
vention on emotions, communication, and quality of life in persons 2009.
with dementia, Nurs Res 59(6):417425, 2010. Viljanen A, et al: Hearing acuity as a predictor of walking difculties in
Radtke JV, et al: Listening to the voiceless patient: case reports in older women, J Am Geriatr Soc 57(12):22822286, 2009.
assisted communication in the intensive care unit, J Palliat Med
14(6):791795, 2011.
Wain HR, Kneebone II, Billings J: Patient experience of neurologic
rehabilitation: a qualitative investigation, Arch Phys Med Rehabil
C
Riddle RP, Racine N: Assessing pain in infancy: the caregiver context, 63(5):527534, 2008.
Pain Res Manage 14(1):2732, 2009. Williams KN, et al: Elderspeak communication: Impact on dementia
Sarampalis A, et al: Objective measures of listening effort: effects of care, Am J Alzheimers Dis Other Dement 24(1):1120, 2009.
background noise and noise reduction, J Speech Lang Hear Res
52:12301240, 2009.
Stallings JW: Collage as a therapeutic modality for reminiscence in
patients with dementia, Art Ther 37(3):136140, 2010.
Acute Confusion Mila W. Grady, MSN, RN
NANDA-I
Definition
Abrupt onset of reversible disturbances of consciousness attention, cognition, and perception that develop
over a short period of time
Defining Characteristics
Fluctuation in cognition, level of consciousness, psychomotor activity; hallucinations; increased agitation;
increased restlessness; lack of motivation to follow through with goal-directed behavior or purposeful behav-
ior; lack of motivation to initiate goal-directed behavior or purposeful behavior; misperceptions
Related Factors (r/t)
Alcohol abuse; delirium; dementia; drug abuse, uctuation in sleep-wake cycle, over 60 years of age,
polypharmacy
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Cognition, Distorted Thought Self-Control, Information Processing, Memory
Example NOC Outcome with Indicators
Cognition as evidenced by the following indicators: Communication clear for age/Comprehension of the meaning of situations/
Attentiveness/Concentration/Cognitive orientation. (Rate the outcome and indicators of Cognition: 1 = severely compromised,
2 = substantially compromised, 3 = moderately compromised, 4 = mildly compromised, 5 = not compromised [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Demonstrate restoration of cognitive status to baseline
Be oriented to time, place, and person
Demonstrate appropriate motor behavior
Maintain functional capacity
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Delirium Management, Delusion Management
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
226 Acute confusion
Example NIC ActivitiesDelirium Management
Inform client of time, place, and person as needed; Provide information slowly and in small doses, with frequent rest periods
C Nursing Interventions and Rationales
Assess the clients behavior and cognition systematically and continually throughout the day and night, as
appropriate. Utilize a validated tool to assess presence of delirium such as the Confusion Assessment
Method (CAM) or Delirium Observation Screening Scale. EB: The best evidence in a review of the literature
supports the use of the CAM (Wong et al, 2010). Delirium is often underrecognized and underdiagnosed
(OMahoney et al, 2011). EBN: Nurses are missing key symptoms of delirium; use of an objective instrument
is essential in guiding assessment and documentation (Steis & Fick, 2008).
Recognize that delirium may be superimposed on dementia; the nurse must be aware of the clients base-
line cognitive function. EB: Dementia increases the risk and severity of delirium (Voyer et al, 2011b).
Recognize that there are three distinct types of delirium based on either arousal or motor disturbances
(Breitbart & Alici, 2008):
Hyperactive: delirium characterized by restlessness, agitation, hypervigilance, hallucinations and delu-
sions; may be combative
Hypoactive: delirium characterized by psychomotor retardation, lethargy, sedation, reduced awareness
of surroundings and confusion
Mixture of both hyper- and hypodelirium: the client uctuates between periods of hyperactivity and
agitation and hypoactivity and sedation. EB: The hypoactive form of delirium was most often unrecognized
by physicians in a study of clients in a mixed ICU (van Eijk et al, 2009). Many older adults in the emergency
department present with the hypoactive subtype, which is missed the majority of the time (Han et al, 2009);
these clients have worse outcomes (Flinn et al, 2009).
Identify clients who are at high risk for delirium. EB: Predisposing factors leading to increased vulnerability
for delirium include: cognitive impairment, severity of illness, older age, depression, vision and/or hearing
impairment, and functional impairment (Sendelbach & Guthrie, 2009) and clients with advanced cancer
(Bush & Bruera, et al, 2009), often due to the anticholinergic effects of opioids. Dementia increases the risk and
severity of delirium (Voyer et al, 2011b). EBN: There was a signicant reduction in delirium in hospitalized
elders when a delirium prevention protocol was implemented (Robinson et al, 2008).
Identify precipitating factors that may precede the development of delirium: use of restraints, indwelling
bladder catheter, metabolic disturbances, polypharmacy, pain, infection, dehydration, constipation, elec-
trolyte imbalances, immobility, general anesthesia, hospital admission for fractures or hip surgery, anti-
cholinergic medications, anxiety, sleep deprivation, and environmental factors. Prevention of delirium
must be a high priority in light of frequency of occurrence, high treatment costs, longer hospital length of stay,
higher rates of functional decline and institutional care, and higher mortality. Delirium may persist and may
lead to long-term cognitive decline (OMahoney et al, 2011). EB: Recognize that clients who are highly vulner-
able for developing delirium require relatively fewer precipitating factors to develop delirium (Sendelbach &
Guthrie, 2009). Clients who might benet from a proactive geriatrics consultation include those over 65 or 70,
with baseline cognitive dysfunction, multiple comorbidities, chronic use of psychotropic medications, drug or
alcohol dependence, sensory impairment, immobility or functional decline, surgery, prolonged hospital stay,
ICU stay, recurrent hospitalizations within the past year, and poor social support (Flinn et al, 2009).
Perform an accurate mental status examination that includes the following:
Overall appearance, manner, and attitude
Behavior characteristics and level of psychomotor behavior (activity may be increased or decreased and
may include spastic movements or tremors with delirium)
Mood and affect (may be paranoid or fearful with delirium; may have rapid mood swings)
Insight and judgment
Cognition as evidenced by level of consciousness, orientation to time, place, and person, thought pro-
cess (thinking may be disorganized, distorted, fragmented, slow or accelerated with delirium), and con-
tent (perceptual disturbances such as visual, auditory or tactile delusions or hallucinations)
Level of attention (may be decreased with delirium; may be unable to focus, maintain attention or shift
attention, or may be hypervigilant)
Memory (recent and immediate memory is impaired with delirium; unable to register new information)
Arousal (may uctuate with delirium; sleep-wake cycle may be disturbed)
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Acute confusion 227
Language (may have rapid, rambling, slurred, incoherent speech) (Breitbart & Alici, 2008; Sendelbach
& Guthrie, 2009)
Assess for and report possible physiological alterations (e.g., sepsis, hypoglycemia, hypoxia, hypotension,
infection, changes in temperature, uid and electrolyte imbalance, and use of medications with known
cognitive and psychotropic side effects). Delirium is often unrecognized, inappropriately treated, or
untreated, especially in terminally ill clients (Breitbart & Alici, 2008). EB: Avoid unnecessary catheterization; C
utilize infection control protocols to prevent infection, and maintain usual sleep schedule (OMahoney et al,
2011).
Treat the underlying risk factors or the causes of delirium in collaboration with the health care team:
establish/maintain normal uid and electrolyte balance; normal body temperature, normal oxygenation
(if the client experiences low oxygen saturation, deliver supplemental oxygen), normal blood glucose
levels, normal blood pressure. EB: These factors are common contributors to delirium in the older adult
(Flinn et al, 2009).
Conduct a medication review and eliminate unnecessary medications. Medications that should be mini-
mized or discontinued include anticholinergics, antihistamines, and benzodiazepines; cholinesterase
inhibitors should be continued, as should carbidopa and levodopa for clients with parkinsonism (Flinn
et al, 2009).
Communicate client status, cognition, and behavioral manifestations to all necessary providers.
Monitor for any trends occurring in these manifestations, including laboratory tests.
EB: Careful monitoring is needed to identify the potential etiologic factors for delirium (Sendelbach &
Guthrie, 2009).
Identify, evaluate and treat pain quickly and adequately (see care plans for Acute Pain or Chronic Pain).
Around the clock acetaminophen may result in less opioid use (Bourne, 2008). EB: There was an associa-
tion between low doses of analgesia and the development of delirium in hospitalized clients experiencing pain
(Robinson & Vollmer, 2010). Untreated pain is a potential cause of delirium, as is excessive opioid adminis-
tration (Clegg & Young, 2011). Delirium can interfere with pain recognition (Breitbart & Alici, 2008).
Promote regulation of bowel and bladder function. EB: Constipation may precipitate delirium (OMahoney
et al, 2011). Catheters should be removed by postoperative day 2 to decrease infection risk (Flinn et al, 2009);
urinary retention may precipitate delirium (Waardenburg, 2008).
Ensure adequate nutritional and uid intake. Dehydration often precipitates delirium (Thomas et al, 2008).
EB: BMI less than 20 is an important risk factor for the development of delirium in postoperative older adult
hip fracture clients (Juliebo et al, 2009).
Promote early mobilization and rehabilitation. EB: Impaired mobility is a risk factor for developing delirium
(Brouquet et al, 2010).
Promote continuity of care; avoid frequent changes in staff and surroundings. EB: Changes may contribute
to feelings of disorientation and confusion (OMahoney et al, 2011).
Plan care that allows for an appropriate sleep-wake cycle. Please refer to the care plan for Sleep depriva-
tion. Both delirium and sleep deprivation are associated with disrupted neurotransmitters. It is sometimes
difcult to tell which came rst. It is known that benzodiazepines deplete melatonin in the body which is
needed for normal sleep (Figueroa-Ramos et al, 2009). EB: Sleep deprivation may potentially be a modiable
risk factor for the development of delirium (Weinhouse et al, 2009).
Facilitate appropriate sensory input by having clients use aids (e.g., glasses, hearing aids) as needed; check
for impacted ear wax. Sensory impairment is a predisposing factor for the development of delirium (Voyer
et al, 2009). EBN: Clients with hearing loss receive lower doses of pain medication and have a higher incidence
of delirium (Robinson et al, 2008).
Modulate sensory exposure and establish a calm environment. Environments with too much or too little
stimulation may precipitate delirium; noise reduction, appropriate lighting based on time of day, reduced clut-
ter, and quiet music are strategies that may impact delirium (Schreier, 2010).
Provide reality orientation, including identifying self by name at each contact with the client, calling the
client by their preferred name, using orientation techniques, providing familiar objects from home such
as an afghan, providing clocks and calendars, and gently correcting misperceptions. Facilitate regular
visits from family and friends. EB: Persons at risk for delirium should be provided clocks and calendars that
are easily visible; family and friends may help with reorientation (OMahoney et al, 2011).
Use gentle, caring communication; provide reassurance of safety; give simple explanations of procedures
(Bourne, 2008). Clients with delirium often respond to caring even though they may not understand the ver-
bal message.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
228 Acute confusion
Provide supportive nursing care, including meeting basic needs such as feeding, toileting, and hydration.
Delirious clients are unable to care for themselves due to their confusion (Rubin et al, 2011).
Recognize that delirium is frequently treated with an antipsychotic medication. Administer cautiously as
ordered, if there is no other way to keep the client safe. Watch for side effects of the medications. Be aware of
paradoxical effects and side effects such as extrapyramidal symptoms, agitation, sedation, and arrhythmias; these
C may exacerbate the delirium (Bourne, 2008). EB: Haloperidol is recommended as the rst-line agent for delirium at
the end of life (NCCN Clinical Practice Guidelines in Oncology, 2011); atypical antipsychotics such as risperidone,
olanzapine, and quetiapine have been utilized with comparable response (Fong, Tulebaev, & Inouye, 2009).
Critical Care
Recognize admission risk factors for delirium. EB: Risk factors related to ICU clients include daily alcohol
use of greater than 3 units, living at home alone, smoking more than 10 cigarettes per day, and cognitive
impairment; precipitating risk factors included more than three infusions, presence of an endotracheal tube or
tracheotomy, internal medicine admission, and factors such as isolation, no visible daylight, and a lack of visi-
tors (Van Rompaey et al, 2009).
Monitor for delirium in each client in critical care daily. Utilize the Confusion Assessment Method for the
ICU (CAM-ICU) or the Intensive Care Delirium Screening Checklist (ICDSC). Delirium is extremely com-
mon in critically ill clients (Sona, 2009) but often remains undiagnosed due to lack of assessment (Guenther
et al, 2010) or because of the presence of hypoactive delirium (Girard, Pandharipande, & Ely, 2008). EB: The
use of reliable, validated tools such as the CAM-ICU should be a routine part of daily critical care due to the
underdetection of delirium and impact on morbidity (Spronk et al, 2009).
Sedate critical care clients carefully; monitor sedation, analgesia, and delirium scores. EB: Sedatives and
analgesics prescribed to improve patient-ventilator dyssynchrony and treat anxiety and pain may precipitate
delirium (Banerjee, Girard, &Pandharipande, 2011). Individualized titration of sedation, analgesia, and
delirium therapies, utilizing management protocols and initiating nonpharmacologic measures are associated
with improved outcomes (Skrobik et al, 2010).
Awaken the client daily. This has been associated with decreased incidence of ventilator-associated pneumo-
nia; also monitoring the client for continued need for intubation is needed since intubation itself is associated
with increased incidence of delirium. NOTE: A sedation vacation may not be appropriate for all clients, such
as those receiving neuromuscular blockade (Bourne, 2008). EB: Benzodiazepines increase the risk of delirium
in a dose-dependent manner (Pandharipande et al, 2008).
Bundle awakening and breathing coordination, choosing the appropriate sedative, monitoring for delir-
ium, and promotion of exercise and early mobility. EB: Bundling these activities was found to improve
functional and cognitive outcomes for critically ill clients (Banerjee, Girard, & Pandharipande, 2011).
Initiate mobilization, physical therapy, and occupational therapy early in the ICU stay. EB: Clients who
experienced daily interruption of sedation with early mobilization had more ventilator-free days and an
improved functional status at discharge, as well as a 50% decrease in the duration of delirium (Schweikert
et al, 2009).
Encourage visits from families. EB: Clients in the intensive care who did not receive visits were at greater risk
of developing delirium (Van Rompaey et al, 2009).
Geriatric
Assess older adults upon hospital admission and routinely for risk factors, precipitating factors, and the
presence of delirium. Predisposing factors include advanced age, sensory impairment, functional impairment,
dementia, malnutrition, dehydration and previous history of depression. EBN: Older adults who undergo
cardiac surgery are at an increased risk for developing delirium (Koster et al, 2011). CEB: Delirium affects one
third of hospitalized older adults (Inouye, 2006) and is the most prevalent complication in hospitalized older
adults (Young & Inouye, 2007).
Avoid the use of restraints. EBN: In a study of long-term care residents with dementia, the use of physical
restraints was the factor most associated with delirium; initiate alternative interventions (Voyer et al,
2011a).
Evaluate all medications for potential to cause or exacerbate delirium. Review the Beers Criteria for
Potentially Inappropriate Medication Use in Elderly. Elderly are very prone to medication side effects that
can include confusion; drug interactions contribute to the development of delirium (Flinn et al, 2009). EB:
Avoid or reduce benzodiazepines; prescribe with caution opioids, dihydropyridines, and antihistamine H1
antagonists (Clegg & Young, 2011).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Acute confusion 229
Establish or maintain elimination patterns of urination and defecation. EB & EBN: Urinary retention or a
urinary tract infection resulting in urosepsis, as well as constipation, may lead to delirium in the elderly
(Faezah, Zhang, & Yin, 2008; Waardenburg, 2008).
Determine if the client is nourished; watch for protein-calorie malnutrition. Consult with physician or
dietitian as needed. EBN: A study found increased delirium in a group of extended care clients who had
decreased body weight, possibly because of protein-binding from polypharmacy of medications (Culp & C
Cacchione, 2008).
Explain hospital routines and procedures slowly and in simple terms; repeat information as necessary.
Provide continuity of care when possible, avoid room changes, and encourage visits from family members
or signicant others. EB: Frequent changes may contribute to confusion (OMahoney et al, 2011).
If clients know that they are not thinking clearly, acknowledge the concern. Fear is frequently experienced
by people with delirium. EB: Confusion is frightening; the memory of the delirium can be moderately to
severely distressing (Bruera et al, 2009).
Keep the clients sleep-wake cycle as normal as possible (e.g., avoid letting the client take daytime naps,
avoid waking the client at night, give sedatives but not diuretics at bedtime, provide pain relief and back
rubs). The relationship between delirium and sleep deprivation is reciprocal (Figueroa-Ramos et al, 2009).
Home Care
Some of the interventions described previously may be adapted for home care use.
Assess and monitor for acute changes in cognition and behavior. An acute change in cognition and behavior
is the classic presentation of delirium and should be considered a medical emergency (Bond, 2009).
Delirium is reversible but can become chronic if untreated. The client may be discharged from the hospi-
tal to home care in a state of undiagnosed delirium. EB: Delirium may occur in approximately 20% of cli-
ents 6 months after hospital discharge (Cole et al, 2009).
Avoid preconceptions about the source of acute confusion; assess each occurrence on the basis of available
evidence.
Institute case management of frail elderly clients to support continued independent living if possible once
delirium has resolved.
Client/Family Teaching and Discharge Planning
Teach the family to recognize signs of early confusion and seek medical help.
Counsel the client and family regarding the management of delirium and its sequelae. EB: Families experi-
ence a high degree of distress when observing a loved one in delirium (Arend & Christensen, 2009); the major-
ity of clients with advanced cancer were able to remember their delirium episode which caused moderate to
severe distress to themselves as well as to their family caregivers (Bruera et al, 2009). Families should be told
that symptoms of delirium may persist for months; clients may need ongoing assistance (Cole et al, 2009).
REFERENCES
Arend E, Christensen M: Delirium in the intensive care unit: a review, Bush SH, Bruera E: The assessment and management of delirium in
Br Assoc Crit Care Nurses 14(3):145154, 2009. cancer patients, Oncologist 14(10):10391049, 2009.
Banerjee A, Girard TD, Pandharipande P: The complex interplay Clegg A, Young JB: Which medications to avoid in people at risk of
between delirium, sedation, and early mobility during criti- delirium: a systematic review, Age Ageing 41(1):2329, 2011.
cal illness: applications in the trauma unit, Curr Opinion Anesth Cole MG, et al: Persistent delirium in older hospital patients: a system-
24(2):195201, 2011. atic review of frequency and prognosis, Age Ageing 38(1):1926,
Bond SM: Delirium at home: strategies for home health clinicians, 2009.
Home Healthc Nurse 27(1):2434, 2009. Culp KR, Cacchione PZ: Nutritional status and delirium in long-term
Bourne RS: Delirium and use of sedation agents in intensive care, Crit care elderly individuals, Appl Nurs Res 21(2):6674, 2008.
Care Nurs 13(4):195202, 2008. Faezah S, Zhang D, Yin LF: The prevalence and risk factors of delirium
Breitbart W, Alici Y: Agitation and delirium at the end of life: We amongst the elderly in acute hospital, Singapore Nurs J 35(1):1114,
couldnt manage him, JAMA 300(24):28982910, 2008. 2008.
Brouquet A, et al: Impaired mobility, ASA status and administration Figueroa-Ramos MI, et al: Sleep and delirium in ICU patients: a review
of tramadol are risk factors for postoperative delirium in patients of mechanisms and manifestations, Intensive Care Med 35(5):781
aged 75 years or more after major abdominal surgery, Ann Surg 795, 2009.
251(4):759765, 2010. Flinn DR, et al: Prevention, diagnosis, and management of postopera-
Bruera E, et al: Impact of delirium and recall on the level of distress in tive delirium in older adults, J Am Coll Surg 209(2):261268, 2009.
patients with advanced cancer and their family caregivers, Cancer Fong TG, Tulebaev SR, Inouye SK: Delirium in elderly adults: diagnosis,
115(9):20042012, 2009. prevention and treatment, Nat Rev Neurol 5(4):210220, 2009.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
230 Chronic confusion
Girard TD, Pandharipande PP, Ely EW: Review: Delirium in the inten- Sendelbach S, Guthrie PF: Acute confusion/delirium evidence-based
sive care unit, Crit Care 12(Suppl 3):S3, 2008. guideline, Ames, IA, 2009, John A. Hartford Foundation Center of
Guenther U, et al: Validity and reliability of the CAM-ICU owsheet to Geriatric Nursing Excellence, University of Iowa.
diagnose delirium in surgical ICU patients, J Crit Care 25(1):144 Skrobik Y, et al: Protocolized intensive care unit management of anal-
151, 2010. gesia, sedation, and delirium improves analgesia and subsyndromal
Han JH, et al: Delirium in older emergency department patients: rec- delirium rates, Anesth Analg 111(2):451463, 2010.
C ognition, risk factors, and psychomotor subtypes, Acad Emerg Med
16(3):193200, 2009.
Sona C: Assessing delirium in the intensive care unit, Crit Care Nurs
29(2):103104, 2009.
Inouye SK: Current concepts: delirium in older persons, N Engl J Med Spronk PE, et al: Occurrence of delirium is severely underestimated
354(11):11571165, 12171220:2006. in the ICU during daily care, Intensive Care Med 35(7):12761280,
Juliebo V, et al: Risk factors for preoperative and postoperative delirium 2009.
in elderly patients with hip fracture, J Am Geriatr Soc 57(8):1354 Steis MR, Fick DM: Are nurses recognizing delirium? A systematic
1361, 2009. review, J Gerontol Nurs 34(9):4048, 2008.
Koster S, et al: Risk factors for delirium after cardiac surgery: a system- Thomas DR, et al: Understanding clinical dehydration and its treat-
atic review, Eur J Cardiovasc Nurs 10(4):197204, 2011. ment, J Am Med Dir Assoc 9(5):292301, 2008.
National Comprehensive Cancer Network: Clinical practice guidelines Van Eijk MM, et al: Comparison of delirium assessment tools in a
in oncology, version 2.2011, palliative care. Retrieved November 1, mixed intensive care unit, Crit Care Med 37(6):18811885, 2009.
2011, from http://www.nccn.org/professionals/physician_gls/pdf/ Van Rompaey B, et al: Risk factors for delirium in intensive care
palliative.pdf. patients: a prospective cohort study, Crit Care 13(3):R77, 2009.
OMahoney R, et al: Synopsis of the National Institute for Health and Voyer P, et al: Predisposing factors associated with delirium among
Clinical Excellence guideline for prevention of delirium, Ann Intern demented long-term care residents, Clin Nurs Res 18(2):153171,
Med 154(11):746751, 2011. 2009.
Pandharipande P, et al: Prevalence and risk factors for development Voyer P, et al: Precipitating factors associated with delirium among
of delirium in surgical and trauma intensive care unit patients, long-term care residents with dementia, Appl Nurs Res 24(3):171
J Trauma 65(1):3441, 2008. 178, 2011a.
Robinson S, et al: Delirium prevention for cognitive, sensory and mobil- Voyer P, et al: Factors associated with delirium severity among older
ity impairments, Res Theory Nursing Pract 22(2):103113, 2008. persons with dementia, J Neurosci Nurs 43(2):6269, 2011b.
Robinson S, Vollmer C: Undermedication for pain and precipitation of Waardenburg IE: Delirium caused by urinary retention in elderly
delirium, Medsurg Nurs 19(2):7983, 2010. people: a case report and literature review on the cystocerebral
Rubin FH, et al: Sustainability and scalability of the hospital elder life syndrome, J Am Geriatr Soc 56(12):23712372, 2008.
program at a community hospital, J Am Geriatr Soc 59(2):359365, Weinhouse GL, et al: Bench-to bedside review: delirium in ICU
2011. patientsimportance of sleep deprivation, Crit Care 13(6):234,
Schreier AM: Nursing care, delirium, and pain management for the 2009.
hospitalized older adult, Pain Manage Nurs 11(3):177185, 2010. Wong C, et al: Does this patient have delirium? Value of bedside instru-
Schweikert W, et al: Early physical and occupational therapy in mechan- ments, JAMA 304(7):779786, 2010.
ically ventilated, critically ill patients: a randomized control trial, Young J, Inouye SK: Delirium in older people, BMJ 334(7598):842846,
Lancet 373(9678):18741882, 2009. 2007.
Chronic Confusion Mila W. Grady, MSN, RN
NANDA-I
Definition
Irreversible, long-standing, and/or progressive deterioration of intellect and personality characterized by
decreased ability to interpret environmental stimuli; decreased capacity for intellectual thought processes;
and manifested by disturbances of memory, orientation, and behavior
Defining Characteristics
Altered interpretation; altered personality; altered response to stimuli; clinical evidence of organic impair-
ment; impaired long-term memory; impaired short-term memory; impaired socialization; long-standing
cognitive impairment; no change in level of consciousness; progressive cognitive impairment
Related Factors (r/t)
Alzheimers disease; cerebrovascular attack; head injury; Korsakoffs psychosis; multi-infarct dementia
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Cognition, Cognitive Orientation, Distorted Thought Self-Control
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Chronic confusion 231
Example NOC Outcome with Indicators
Cognition as evidenced by the following indicators: Cognitive orientation/Communicates clearly for age/Comprehends the meaning
of situations/Attentiveness/Concentration. (Rate the outcome and indicators of Cognition: 1 = severely compromised, 2 =
substantially compromised, 3 = moderately compromised, 4 = mildly compromised, 5 = not compromised [see Section I].)
C
Client Outcomes
Client Will (Specify Time Frame):
Remain content and free from harm
Function at maximal cognitive level
Participate in activities of daily living at the maximum of functional ability
Have minimal episodes of agitation (as agitation occurs in up to 70% of clients with dementia)
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Dementia Management, Environmental Management, Surveillance: Safety
Example NIC ActivitiesDementia Management
Use distraction rather than confrontation to manage behavior; Give one simple direction at a time
Nursing Interventions and Rationales
Determine the clients cognitive level using a screening tool such as the Mini-Mental State Exam (MMSE),
Mini-Cog (includes a three-item recall and clock drawing test), or Montreal Cognitive Assessment. Age,
education, and literacy must be taken into account when interpreting results of the MMSE (Mitchell, 2009) as
well as culture and ethnicity (Struble & Sullivan, 2011); an abnormal score necessitates further evaluation. For
older adults with mild cognitive impairment, the Short Test of Mental Status and Montreal Cognitive Assess-
ment are more sensitive diagnostic tools than the MMSE (Petersen, 2011). EB: The clock drawing test is useful
for detecting moderate to severe dementia; its usefulness in detecting early cases of dementia is limited (Pinto &
Peters, 2009).
In clients who are complaining of memory loss, assess for depression, alcohol use, medication use, sleep,
and nutrition. These factors may be implicated in memory loss (Struble & Sullivan, 2011).
Recognize that pharmacological treatment to slow the progression of Alzheimers disease is most effective
when used early in the course of the disease. The U.S. Food and Drug Administration has approved ve
drugs that slow the progression of symptoms for approximately 6 to 12 months; over 75 experimental therapies
are being clinically tested in humans (Alzheimers Association, 2011).
If hospitalized, gather information about the clients pre-admission cognitive functioning, daily routines
and care, and decision-making capacity. Establishing continuity of care lessens risk for hospitalized clients.
Informed consent may create a dilemma; decision-making capacity will vary depending on the degree of cogni-
tive impairment (Weitzel et al, 2011). EBN & EB: Individuals with a history of cognitive dysfunction are at
higher risk for acute confusion during acute illness (Voyer et al, 2011a). Clients with mild cognitive impair-
ment may be able to make decisions regarding their care (Okonkwo et al, 2008).
Assess the client for signs of depression: anxiety, sadness, irritability, agitation, somatic complaints, ten-
sion, loss of concentration, insomnia, poor appetite, apathy, at affect, and withdrawn behavior. EB: Up
to 95% of individuals with dementia have some neuropsychiatric problems (Gauthier et al, 2010), with the
most common being apathy, depression, and anxiety; others include aggression, agitation, delusions, and hal-
lucinations (Jalbert, Daiello, & Lapane, 2008). The Cornell Scale is a reliable and valid tool to assess for
depression in dementia (Leontjevas, van Hooren, & Mulders, 2009). Approximately 20% of older adults may
be affected by signicant depressive symptoms (Thielke, Diehr, & Unutzer, 2010).
Assess the client for anxiety if he or she reports worry regarding physical or cognitive health, reports feelings
of being anxious, shortness of breath, dizziness, or exhibit behaviors such as restlessness, irritability, noise
sensitivity, motor tension, fatigue, or sleep disturbances. The Rating Anxiety in Dementia (RAID) Scale
may be utilized; this may require caregiver input. Recognize that anxiety is common in dementia, is often
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
232 Chronic confusion
undiagnosed, and may signicantly impact quality of life. CEB: Symptoms of anxiety may progress to more
challenging behaviors which negatively impact function and may contribute to discharge from assisted living
to nursing home care (Aud, 2004). CEB: The RAID scale is a reliable and valid tool for identifying and mea-
suring anxiety in dementia (Shankar et al, 1999).
Recognize that clients with Alzheimers disease may experience apathy, anxiety and depression, psycho-
C motor agitation, and psychotic or manic syndromes; nonpharmacological interventions for management
should be attempted rst. EB: More than 75% of clients with Alzheimers disease presented with one or more
neuropsychiatric syndromes; therapeutic strategies must be planned accordingly (Spaletta et al, 2010). Best
practice guidelines recommend psychological interventions as the rst approach to treatment (Ballard et al,
2009). Medication for neuropsychiatric symptoms should be prescribed after nonpharmacological interven-
tions have been tried and should be administered at the lowest possible dose and chosen with regard to side
effects and adverse reactions (Gauthier et al, 2010).
Determine clients normal routines and attempt to maintain them. CEB: Activities that are designed to be
consistent with past routines were effective at providing engagement and interest and enhancing quality of life
(Cohen-Manseld & Jensen, 2006).
Obtain information about the clients life history from the family; collaborate with family members to
provide optimal care. EBN: Knowing the history, interests, needs, and preferences of the individual is essential
to person-centered care and helpful when initiating conversation, activities, and routines; the familys unique
knowledge should be incorporated into the plan of care (Edvardsson, Fetherstonhaugh, & Nay, 2010).
Begin each interaction with the client by gaining and maintaining eye contact, identifying yourself and call-
ing the client by name. Approach the client with a caring, loving, and an accepting attitude, and speak calmly
and slowly. EB: Dementia causes a loss of the ability to learn new things and remember people and places (epi-
sodic memory); clients will need reassurance and frequent reminding of the identity of caregivers (Yu et al, 2009).
enhance communication, use a calm approach, avoid distractions, show interest, keep communication
To
simple, give clear choices, give the client time with word nding, use repetition and rephrasing, and utilize
gestures, prompts, and cues or visual aids. Listen attentively to understand nonverbal messages, and
engage in topics of interest to the client. EB: These communication techniques assist in focusing attention,
incorporate nonverbal means of communication, simplify memory demands, compensate for cognitive slow-
ing, and assist with retrieval and comprehension (Smith et al, 2011).
Engage the client in scheduled activities that relate to past interests, experiences, and hobbies and are
matched to current preferences and abilities. EB: Activities that were once meaningful to the client in terms
of self-identity are more likely to result in engagement, even for those with severe cognitive impairment. Resi-
dents with current interests in art, music, and pets were more engaged in stimuli that reected those current
interests (Cohen-Manseld et al, 2010a).
Promote regular exercise. EB: Exercising regularly may signicantly slow the rate of functional decline in
individuals with Alzheimers disease (Littbrand et al, 2009); a small study demonstrated that a specic walk-
ing program for individuals in the later stages of dementia can reduce functional and cognitive decline (Ven-
terelli, Scarsini, & Schena, 2011).
Provide opportunities for contact with nature or nature-based stimuli, such as facilitating time spent
outdoors or indoor gardening. EB: Horticultural-based therapy programs provide positive engagement and
may be benecial for difcult to engage clients with dementia (Jarrott & Gigliotti, 2010). EBN: Individuals
with dementia experience more barriers to experiencing nature, which may be an untapped source of pleasure
for them (Bossen, 2010).
Provide animal-assisted therapy. EB: This activity can successfully engage residents with dementia, promot-
ing communication and social interaction regardless of the level of cognitive function (Marx et al, 2010). In a
study of animal-assisted therapy with a group of clients with severe Alzheimers disease, animal-assisted ther-
apy was associated with a decrease in sadness and anxiety and an increase in motor activity and positive emo-
tions (Mossello et al, 2011).
Break down self-care tasks into simple steps (e.g., instead of saying, Take a shower, say to the client,
Please follow me. Sit down on the bed. Take off your shoes. Now take off your socks.). Utilize gestures
when giving directions; allow for adequate time and model the desired action if needed or possible. EB:
Assistance in focusing attention, modeling behavior, and using prompts and cues maximizes communication
with individuals with dementia (Smith et al, 2011).
Promote routines and facilitate success by keeping frequently used items in a visible and consistent loca-
tion. Consistently practicing routines in an unchanged environment will assist the client in successful mainte-
nance and performance of skills (Bourgeois & Hickey, 2009).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Chronic confusion 233
Use reminiscence and life review therapeutic interventions for clients in the early to middle stages of
dementia; ask questions about the clients past activities, important events and experiences from the past
while utilizing photographs, videos, artifacts, music or newspaper clippings or multimedia technology to
stimulate memories. EB: In a small preliminary study utilizing YouTube videos, it was found that reminis-
cence and life review may improve well-being and social engagement (ORourke et al, 2011). Memories from
childhood or young adulthood are generally intact in the early and middle stages of Alzheimers (Smith et al, C
2011).
For clients in the middle to late stages of dementia, engage them in creative expression through the
use of TimeSlips story-telling groups. EB: In a study of residents in long-term care settings who were
involved in TimeSlips groups, the residents were more alert, socially engaged, had more interactions with
staff and others, and staff had more positive views of residents than facilities without the TimeSlips
groups (Fritsch, 2009).
If the client is verbally agitated (repetitive verbalizations, complaints, moaning, muttering, threats,
screaming), assess for and address unsatised basic needs or environmental factors that may be addressed.
EB: Disruptive vocalizations may be an indication that the client with dementia has the need for comfort,
attention, or more or less stimulation (Beedard et al, 2011). Behaviors are not solely due to cognitive impair-
ment and may be due to an unmet need or environmental factors that may be overwhelming or understimulat-
ing (Gitlin et al, 2009).
Utilize music as a nonpharmacological approach to managing anxiety. Identify music preferences of the
client; interview family members if necessary. For anxious clients who are having problems relaxing
enough to eat, try having them listen to music during meals. EBN: Preferred music listening is an effective
intervention to decrease anxiety in older adults with dementia (Sung, Chang, & Lee, 2010); utilizing percus-
sion instruments with familiar music was found to be a cost effective method for decreasing anxiety and
improving psychological well-being (Sung et al, 2012).
Assist clients in waynding, monitoring them so that they do not get lost in unfamiliar settings. EB:
Dementia and some related disorders cause impaired spatial learning; security measures should be unobtru-
sive, personal surroundings should include familiar objects, and facilities should be designed to have a home-
like appearance (Fleming & Purandare, 2010).
For clients who wander, utilize technologies that monitor but do not restrict. Direct the client who is
wandering to a more soothing location with lower light levels and less variation in noise if necessary. EB:
Motion detectors may improve quality of life by allowing clients to wander safely without restriction (Wigg,
2010). Modify the environment to reduce wandering if that is the therapeutic goal (Algase et al, 2010).
Promote sleep by promoting daytime activity, creating a restful sleep environment, decreasing waking, and
promoting quiet. EB: Sleep disorders are very common in those with dementia; individuals with Lewy body demen-
tia experience disturbed sleep twice as often (Bliwise et al, 2011). Promoting a dark and quiet nighttime environ-
ment, a comfortable sleeping temperature for the client, encouraging physical activity, especially in the afternoon,
maintaining a consistent schedule of meals and activities, maintaining a bright daytime environment, and facilitat-
ing outdoor activity are all methods of improving sleep (Neikrug & Ancoli-Israel, 2010).
Provide structured social and physical activities that are individualized for the client. EB: Combined weekly
live music and occupational therapy sessions resulted in an improvement in disruptive behavior and depressive
symptoms in adults with dementia (Han et al, 2010).
Provide activities for the client, such as folding washcloths and sorting or stacking activities or other hob-
bies the individual enjoyed prior to the onset of dementia. EB: The purposeful use of activities tailored to an
individuals abilities may allow the individual to maintain social roles and feelings of connectedness, express
themself in a positive way, enhance self-identity, reduce frustration, and prevent boredom, resulting in less
agitation (Gitlin et al, 2009).
Use cues, such as picture boards denoting day, time, and location, to help client with orientation. EBN:
Reality orientation, used not when clients are agitated, but as overall reminders of orientation, can help some
clients remain more oriented (Yu et al, 2009).
If the client becomes increasingly confused and/or agitated, perform the following steps:
Assess the client for physiological causes, including acute hypoxia, pain, medication effects, malnutri-
tion, and infections such as urinary tract infection, fatigue, electrolyte disturbances, and constipation.
Dementia increases the risk and severity of delirium, which may be precipitated by several factors (Voyer
et al, 2011b).
Assess for psychological causes, including changes in the environment, caregiver, routine, demands to
perform beyond capacity, or multiple competing stimuli, including discomfort. CEB: Agitated behaviors
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
234 Chronic confusion
can be an expression of a need that is not being met (Kolanowski, Litaker, & Buettner, 2005; Kovach et al,
2005).
In clients with agitated behaviors, rather than confronting the client, decrease stimuli in the environ-
ment or provide diversional activities such as quiet music, looking through a photo album, or providing
the client with textured items to handle. EB: Music may reduce aggressive behaviors during bathing,
C reduce agitation at mealtime or in general; structured activities that include manipulating, nurturing, sort-
ing or using the tactile sense may reduce agitation (Cohen-Manseld, Dakheel-Ali, & Marx, 2009).
If clients with dementia become more agitated, assess for pain. EBN: Pain assessment should begin with
eliciting a self-report using a valid and reliable tool. For the client with cognitive impairment, identify poten-
tial causes of pain, physiologic indicators, and assess behaviors that might indicate pain, elicit information
from family or signicant others regarding behaviors that are a change from baseline that could indicate
pain, and initiate an analgesic trial if indicated (Pasero, 2009).
Avoid using restraints if at all possible. EB: The use of trunk restraints is associated with higher fall risk for
clients with dementia (Luo, Lin, & Castle, 2011).
Use PRN or low-dose regular dosing of psychotropic or antianxiety drugs only as a last resort; start with the
lowest possible dose. They can be effective in managing symptoms of psychosis and aggressive behavior, but
have undesirable side effects. EB: Psychotropic medications can cause sedation, orthostatic hypotension and dizzi-
ness; use is associated with an increased risk of hospitalization from hip fracture (Jalbert et al, 2010).
Avoid the use of anticholinergic medications such as diphenhydramine. Anticholinergic medications have
a high side-effect prole that includes disorientation, urinary retention, and excessive drowsiness, especially in
those with decreased cognition; the anticholinergic side effects outweigh the antihistaminic effects (Artero et al,
2008; Uusvaara et al, 2009).
For predictable difcult times, such as during bathing and grooming, try the following:
Massage the clients hands or back to relax the client. EBN: Hand and back massage have been shown to
induce physiological and psychological relaxation (Harris & Richards, 2010).
Approach the client in a client-centered framework: utilize respectful, positive statements, give direc-
tions one step at a time, provide short and clear cues, utilize verbal praise for successful task completion.
EB: Modifying activity demands on an individual basis will result in skill retention and maximum indepen-
dence (Padilla, 2011).
Involve the family in care of the client. EBN: Establishing a partnership of shared responsibility, transpar-
ency, and trust is essential to family caregivers (Legault & Ducharme, 2009).
care of early dementia clients with primarily symptoms of memory loss, see the care plan for Impaired
For
Memory.
For clients nearing the end of life, consider a hospice referral. EB: Family members of individuals with
dementia reported higher perceptions of the quality of care and quality of dying experience with hospice care
(Teno et al, 2011).
For care of clients with self-care decits, see the appropriate care plan (Feeding Self-Care decit; Dress-
ing Self-Care decit; and Toileting Self-Care decit).
Geriatric
Note: All interventions are appropriate with geriatric clients.
Multicultural
Assess for the inuence of cultural beliefs, norms, and values on the familys or caregivers understanding
of chronic confusion or dementia. EBN: What the family considers normal and abnormal health behavior
may be based on cultural perceptions (Giger & Davidhizar, 2008). Hispanic and Chinese caregivers were more
likely to believe that Alzheimers can be diagnosed with a blood test and is a normal part of aging, which may
delay seeking help with management (Gray et al, 2009). Korean American immigrants may have a strong
stigma regarding the diagnosis of Alzheimers disease, may consider memory loss as part of the normal aging
process, and lack knowledge regarding cause, diagnosis, and treatment (Lee, Lee, & Diwan, 2010).
Inform the clients family or caregiver of the meaning of and reasons for common behavior observed in
clients with dementia. EB: An understanding of behavior will enable the clients family or caregiver to provide
the client with a safe environment. Disease expression may vary in different ethnoracial groups; Latinos were
found in one study to have more depressive symptoms (Livney et al, 2011).
Assist the family or caregiver in identifying barriers that would prevent the use of social services or other
supportive services that could help reduce the impact of caregiving; refer to social services or other
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Chronic confusion 235
supportive services. EB: Knowledge about the disease, common concerns, beliefs about risks and treatment
have been identied as important areas to discuss in Alzheimers outreach efforts for racial and ethnic minori-
ties (Connell et al, 2009). Barriers to services do exist; Hispanic individuals reported a longer history of mem-
ory loss at the time of referral, African Americans were 30% less likely to be prescribed cholinesterase inhibitors,
and minority ethnic groups were less likely to receive 24-hour care or be enrolled in research trials (Cooper
et al, 2010). Asian cultures have a great sense of respect and responsibility for older adults; interdependence is C
valued; coping strategies and strength from religion and spirituality should be supported (Lim et al, 2010).
Home Care
Note: Keeping the client as independent as possible is important. Because community-based care is usually
less structured than institutional care, in the home setting the goal of maintaining safety for the client takes
on primary importance.
The interventions described previously may be adapted for home care use.
Provide information to the family and home care client regarding advance directives. This is a legal
requirement of the Consolidated Omnibus Budget Reconciliation Act (COBRA). Encouraging advance care
planning, identifying goals for end-of-life care, and providing information to make treatment decisions in
accordance with the clients wishes are important interventions for health care providers (Black et al, 2009).
Assess the clients memory and executive function decits before assuming the inability to make any
medical decisions; driving capacity and nancial capacity should be assessed for clients with mild cogni-
tive impairment. Decisional capacities for informed consent include: understanding and demonstrating com-
prehension of diagnosis and treatment-related information, appreciation of the signicance of the information,
reasoning regarding alternatives and consequences, and expressing a choice (Weitzel et al, 2011). EB: Clients
with mild cognitive impairment should be proactive in engaging in nancial and legal planning in light of the
risk of developing dementia (Marson et al, 2009).
Assess the home for safety features and client needs for assistive devices. Refer to the interventions for
Feeding Self-Care decit, Dressing Self-Care decit, Bathing Self-Care decit as needed.
Promote cognitive stimulation (conversation, singing, dancing, creative activities, games) and memory
training exercises for individuals in the early stages of dementia. EBN: Cognitive training interventions may
improve cognition, learning, memory, problem-solving abilities as well as ability to carry out ADLs; cognitive
training is most effective when combined with medication (Yu et al, 2009).
Provide education and support to the family regarding effective communication and ways to manage
cognitive and behavioral changes; be prepared to offer support and information to family members who
live at a distance as well. EB: Family members desired education regarding communication and management
of behavioral changes (Rosa et al, 2010). Changes in symptoms and behavioral challenges were associated with
higher caregiver burden and depression; psychosocial and pharmacologic interventions to manage neuropsy-
chiatric symptoms may alleviate the suffering of the client and promote the well-being of the caregiver
(Mohamed et al, 2010).
Use familiar aspects of the environment (smells, music, foods, pictures) to cue the client, capitalizing on
habit to remind the client of activities in which the client can participate. EBN: While clients with dementia
are probably unable to learn new activities because of deteriorated explicit memory, preserved implicit memory
or habit may be useful in maximizing functional ability (Hong & Song, 2009).
Instruct the caregiver to provide a balanced activity schedule that does not stress the client or deprive him
or her of stimulation; avoid sustained low- or high-stimulation activity. EB: Planned, individualized struc-
tured activities can prevent agitation (Gitlin et al, 2009).
Encourage the use of preferred music listening to evoke memories and promote relaxation. EB: In a small
study of caregiver-administered music, caregivers and care recipients reported increased relaxation, comfort
and happiness, with caregivers showing the most benet, citing enjoyment in reminiscence and participation
in musical activities with their loved ones (Hanser et al, 2011).
If the client will require extensive supervision on an ongoing basis, evaluate the client for day care
programs. Refer the family to medical social services to assist with this process if necessary. Day care
programs provide safe, structured care for the client and respite for the family, cost a great deal less than
nursing home care, and provide stress relief and respite for the caregiver (Alzheimers Association, 2009).
CEB: Adult day care programs have been shown to reduce stress associated with work, leisure, and family
needs (Schacke & Zank, 2006). For younger individuals with early onset dementia who are in the early
stages, assisting staff with responsibilities in adult day care centers may promote self-esteem (Silverstein,
Wong, & Brueck, 2010).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
236 Chronic confusion
Encourage the family to include the client in family activities when possible. Reinforce the use of thera-
peutic communication guidelines (see Client/Family Teaching and Discharge Planning) and sensitivity to
the number of people present. These steps help the client maintain dignity and lead to familial socialization
of the client.
Assess family caregivers for caregiver stress, loneliness, and depression. Caregivers experience physical and
C emotional health challenges, with $7.9 billion in additional health care costs in 2010 (Alzheimers Association,
2011). Anxiety, depression, exhaustion, and grief are common in caregivers of chronically ill family members
(Hanser et al, 2011).
Refer to the care plan for Caregiver Role Strain.
Refer the client to medical social services as necessary to evaluate nancial resources and initiate benets
or access to providers. EBN: Limited resources serve as barriers to effective use of community services (Beeber,
Thorpe, & Clipp, 2008).
Institute case management for frail elderly clients to support continued independent living.
Client/Family Teaching and Discharge Planning
In the early stages of dementia, provide the caregiver with information on illness processes, needed care,
available services, role changes, and the importance of advance directives discussion; facilitate family
cohesion. EB: Provide information to caregivers gradually, introduce change slowly, facilitate legal changes,
and provide continuous support to caregivers (Livingston, 2010).
Teach the family how to converse with a memory-impaired person and strategies for handling challenging
behaviors. EB: Educational needs of caregivers mainly relate to communication skills as well as management
of difcult behaviors (Rosa et al, 2010).
Teach the family how to provide physical care for the client (bathing, feeding, and ADLs) as well as coping
strategies to deal with the burden of caregiving. EB: Interventions that improve competence in care and cop-
ing may lessen caregiver stress (Williams et al, 2010).
Discuss with the family what to expect as the dementia progresses.
Counsel the family about resources available regarding end-of-life decisions and legal concerns. EB: Fam-
ily members report distress regarding decision making throughout the course of dementia, having insufcient
information, lack of support in having these discussions with family members in the early stages of dementia,
role conict, maintaining the dignity of their family member, family conict; supporting caregivers throughout
the process and assisting them in advocacy is essential (Livingston et al, 2010).
Inform the family that as dementia progresses, hospice care may be available in the home or nursing
home in the terminal stages to help the caregiver. EB: 70% of individuals with dementia in the United States
die in the nursing home (Fulton et al, 2011). Clients who have hospice are more likely to die in the location of
their choice and have improved caregiver satisfaction (Shega et al, 2008).
Note: The nursing diagnoses Impaired Environmental Interpretation Syndrome and Chronic Confusion
are very similar in denition and interventions. Impaired Environmental Interpretation Syndrome must
be interpreted as a syndrome when other nursing diagnoses would also apply. Chronic Confusion may be
interpreted as the human response to a situation or situations that require a level of cognition of which the
individual is no longer capable.
REFERENCES
Algase DL, et al: Wandering and the physical environment, Am J Ballard C, et al: Management of agitation and aggression associated
Alzheimers Dis Other Demen 25(4):340346, 2010. with Alzheimers disease: controversies and possible solutions, Curr
Alzheimers Association: 2009 Alzheimers disease facts and gures. Opinion Psych 22(6):532540, 2009.
Retrieved October 8, 2011, from http://www.alz.org/national/ Beeber AS, Thorpe JM, Clipp EC: Community-based service use by
documents/report_alzfactsgures2009.pdf. elders with dementia and their caregivers: a latent class analysis,
Alzheimers Association: Alzheimers Association report: 2011 Nurs Res 57(5):312, 2008.
Alzheimers disease facts and figures, Alzheimers Dement Beedard A, et al: Reducing verbal agitation in people with dementia:
7(2):208244, 2011. evaluation of an intervention based on the satisfaction of basic
Artero S, et al: Risk proles for mild cognitive impairment and progres- needs, Aging Ment Health 15(7):855865, 2011.
sion to dementia are gender specic, J Neurol Neurosurg Psychiatry Black BS, et al: Surrogate decision makers understanding of dementia
79(9):979984, 2008. patients prior wishes for end-of-life care, J Aging Health 21(4):627
Aud MA: Residents with dementia in assisted living facilities: 650, 2009.
the role of behavior in discharge decisions, J Gerontol Nurs Bliwise DL, et al: Sleep disturbance in dementia with Lewy bodies and
30(6):1626, 2004. Alzheimers disease: a multicenter analysis, Dement Geriatr Cogn
Disord 31(3):239246, 2011.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Chronic confusion 237
Bossen A: The importance of getting back to nature for people with Kolanowski AM, Litaker M, Buettner L: Efcacy of theory-based activi-
dementia, J Gerontol Nurs 36(2):1722, 2010. ties for behavioral symptoms of dementia, Nurs Res 54(4):219228,
Bourgeois MS, Hickey EM: Dementia: from diagnosis to management: a 2005.
functional approach, New York, 2009, Psychology Press. Kovach C, et al: A model of consequences of need-driven, dementia-
Cohen-Manseld J, Jensen B: Do interventions bringing current self- compromised behavior, J Nurs Scholarsh 37(2):134140, 2005.
care practices into greater correspondence with those performed Lee SE, Lee HY, Diwan S: What do Korean American immigrants know
premorbidly benet the person with dementia? A pilot study, Am J
Alzheimers Dis Other Demen 21(5):312317, 2006.
about Alzheimers disease (AD)? The impact of acculturation and
exposure to the disease on AD knowledge, Int J Geriatr Psychiatry
C
Cohen-Manseld J, Dakheel-Ali M, Marx MS: Engagement in persons 25(1):6673, 2010.
with dementia: the concept and its measurement, Am J Geriatr Psych Legault A, Ducharme F: Advocating for a parent with dementia in a
17(4):299307, 2009. long-term care facility: the process experienced by daughters, J Fam-
Cohen-Manseld J, et al: The impact of past and present preferences ily Nurs 15(2):198219, 2009.
on stimulus engagement in nursing home residents with dementia, Leontjevas R, van Hooren S, Mulders A: The Montgomery-Asberg
Aging Ment Health 14(1):6773, 2010a. Depression Rating Scale and the Cornell Scale for Depression in
Cohen-Manseld J, et al: The underlying meaning of stimuli: impact on Dementia: a validation study with patients exhibiting early-onset
engagement of persons with dementia, Psychiatry Res 177(1-2): dementia, Am J Geriatr Psychiatry 17(1):5664, 2009.
216222, 2010b. Lim JB, et al: Coping strategies inuence caregiver outcomes among
Connell CM, et al: Racial differences in knowledge and beliefs about Asian family caregivers of persons with dementia in Singapore,
Alzheimer disease, Alzheimer Dis Assoc Disord 23(2):110116, 2009. Alzheimer Dis Assoc Disord 25(1):3441, 2011.
Cooper C, et al: A systematic review and meta-analysis of ethnic differ- Littbrand H, et al: The effect of a high-intensity functional exercise
ences in use of dementia treatment, care, and research, Am J Geriatr program on activities of daily living: a randomized controlled
Psychiatry 18(3):193203, 2010. trial in residential care facilities, J Am Geriatr Soc 57(10):1741
Edvardsson D, Fetherstonhaugh D, Nay R: Promoting a continuation 1749, 2009.
of self and normality: person-centred care as described by people Livingston G, et al: Making decisions for people with dementia who
with dementia, their family members and aged care staff, J Clin Nurs lack capacity: qualitative study of family carers in UK, Brit Med J
19(17-18):26112618, 2010. 341:c4184, 2010.
Fleming R, Purandare N: Long-term care for people with dementia: Livney MG, et al: Ethnoracial differences in the clinical characteristics
environmental design guidelines, Int Psychogeriatr 22(7):10841096, of Alzheimer disease at initial presentation at an urban Alzheimers
2010. disease center, Am J Geriatr Psychiatry 19(5):430439, 2011.
Fritsch T, et al: Impact of TimeSlips, a creative expression interven- Luo H, Lin M, Castle N: Physical restraint use and falls in nursing
tion program, on nursing home residents with dementia and their homes: a comparison between residents with and without dementia,
caregivers, Gerontologist 49(1):117127, 2009. Am J Alzheimers Dis Other Demen 26(1):4450, 2011.
Fulton AT, et al: Palliative care for patients with dementia in long-term Marson DC, et al: Clinical interview assessment of nancial capacity
care, Clin Geriatr Med 27(2):153170, 2011. in older adults with mild cognitive impairment and Alzheimers
Gauthier S, et al: Management of behavioral problems in Alzheimers disease, J Am Geriatr Soc 57(5):806814, 2009.
disease, Int Psychogeriatr 22(3):346372, 2010. Marx MS, et al: The impact of different dog-related stimuli on engage-
Giger J, Davidhizar R: Transcultural nursing: assessment and interven- ment of persons with dementia, Am J Alzheimers Dis Other Demen
tion, St Louis, 2008, Mosby. 25(1):3745, 2010.
Gitlin LN, et al: The tailored activity program to reduce behavioral Mitchell AJ: A meta-analysis of the accuracy of the mini-mental state
symptoms in individuals with dementia: feasibility, acceptability, examination in the detection of dementia and mild cognitive
and replication potential, Gerontologist 49(3):428439, 2009. impairment, J Psych Res 43(4):411431, 2009.
Gray HL, et al: Ethnic differences in beliefs regarding Alzheimer disease Mohamed S, et al: Caregiver burden in Alzheimer disease: cross-
among dementia family caregivers, Am J Geriatr Psych 17(11):925 sectional and longitudinal correlates, Am J Geriatr Psychiatry
933, 2009. 18(10):917927, 2010.
Han P, et al: A controlled naturalistic study on a weekly music therapy Mossello E, et al: Animal-assisted activity and emotional status of
and activity program on disruptive and depressive behaviors in patients with Alzheimers disease in day care, Int Psychogeriatr
dementia, Dement Geriatr Cogn Disord 30(6):540546, 2010. 23(6):899905, 2011.
Hanser SB, et al: Home-based music strategies with individuals who Neikrug AB, Ancoli-Israel: Sleep disturbances in nursing homes, J Nutr
have dementia and their family caregivers, J Music Ther 48(1):227, Health Aging 14(3):207211, 2010.
2011. Okonkwo OC, et al: Medical decision-making capacity in mild cognitive
Harris M, Richards KC: The physiological and psychological effects of impairment: a 3-year longitudinal study, Neurology 71(19):1474
slow-stroke back massage and hand massage on relaxation in older 1480, 2008.
people, J Clin Nurs 19(7-8):917926, 2010. ORourke J, et al: YouTube: a useful tool for reminiscence therapy in
Hong GR, Song JA: Relationship between familiar environment and dementia? Age Ageing 40(6):742744, 2011.
wandering behaviour among Korean elders with dementia, J Clin Padilla R: Effectiveness of interventions designed to modify the activ-
Nurs 18(9):13651373, 2009. ity demands of the occupations of self-care and leisure for people
Jalbert JJ, Daiello LA, Lapane K: Dementia of the Alzheimer type, Epide- with Alzheimers disease and related dementia, Am J Occup Ther
miol Rev 30:1534, 2008. 65(5):523531, 2011.
Jalbert JJ, et al: Antipsychotic use and the risk of hip fracture among Pasero C: Challenges in pain assessment, J PeriAnesthesia Nurs
older adults aficted with dementia, J Am Med Dir Assoc 11(2):120 24(1):5054, 2009.
127, 2010. Petersen RC: Mild cognitive impairment, N Engl J Med 364(23):2227
Jarrott SE, Gigliotti CM: Comparing responses to horticultural-based 2234, 2011.
and traditional activities in dementia care programs, Am J Alzheimer Pinto E, Peters R: Literature review of the clock drawing test as a tool
Dis Other Demen 25(8):657665, 2010. for cognitive screening, Dement Geriatr Cogn Disord 27(3):201213,
2009.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
238 Constipation
Rosa E, et al: Needs of caregivers of the patients with dementia, Arch Teno JM, et al: Does hospice improve quality of care for persons dying
Gerontol Geriatr 51(1):5458, 2010. from dementia? J Am Geriatr Soc 58(8):15311536, 2011.
Schacke C, Zank S: Measuring the effectiveness of adult day care as a Thielke S, Diehr P, Unutzer J: Prevalence, incidence, and persistence
facility to support family caregivers of dementia patients, J Appl of major depressive symptoms in the cardiovascular health study,
Gerontol 25:6581, 2006. Aging Ment Health 14(2):168176, 2010.
Shankar KK, et al: The development of a valid and reliable scale for Uusvaara J, et al: Association between anticholinergic drugs and apoli-
C rating anxiety in dementia (RAID), Aging Ment Health 3(1):3949,
1999.
poprotein E epsilon4 allele and poorer cognitive function in older
cardiovascular patients: a cross-sectional study, J Am Geriatr Soc
Shega JW, et al: Patients dying with dementia: experience at the end of 57(3):427431, 2009.
life and impact of hospice care, J Pain Symptom Manag 35(5):499 Venterelli M, Scarsini R, Schena F: Six-month walking program changes
507, 2008. cognitive and ADL performance in patients with Alzheimer, Am J
Silverstein NM, Wong CM, Brueck KE: Adult day health care for Alzheimers Dis Other Demen 26(5):381388, 2011.
participants with Alzheimers disease, Am J Alzheimers Dis Other Voyer P, et al: Factors associated with delirium severity among older
Demen 25(3):276283, 2010. persons with dementia, J Neurosci Nurs 43(2):6269, 2011a.
Smith E, et al: Memory and communication support in dementia: Voyer P, et al: Precipitating factors associated with delirium among
research-based strategies for caregivers, Int Psychogeriatr 23(2):256 long-term care residents with dementia, Appl Nurs Res 24(3):171
263, 2011. 178, 2011b.
Spaletta G, et al: Neuropsychiatric symptoms and syndromes in a large Weitzel T, et al: The special needs of the hospitalized patient with
cohort of newly diagnosed, untreated patients with Alzheimer dis- dementia, MedSurg Nurs 20(1):1318, 2011.
ease, Am J Geriatr Psychiatry 18(11):10261035, 2010. Wigg JM: Liberating the wanderers: using technology to unlock doors
Struble LM, Sullivan B-J: Cognitive health in older adults, Nurse Pract for those living with dementia, Sociol Health Illn 32(2):288303,
36(4):2434, 2011. 2010.
Sung HC, Chang AM, Lee WL: A preferred music listening intervention Williams VP, et al: Video-based coping skills to reduce health risk and
to reduce anxiety in older adults with dementia in nursing homes, improve psychological and physical well-being in Alzheimers dis-
J Clin Nurs 19(7-8):10561064, 2010. ease family caregivers, Psychosomatic Med 72(9):897904, 2010.
Sung HC, et al: A group music intervention using percussion instru- Yu F, et al: Cognitive training for early-stage Alzheimers disease and
ments with familiar music to reduce anxiety and agitation of dementia, J Gerontol Nurs 35(3):2329, 2009.
institutionalized older adults with dementia, Int J Geriatr Psychiatry
27(6):621627, 2012.
Risk for acute Confusion Betty Ackley, MSN, EdS, RN
NANDA-I
Definition
At risk for reversible disturbances of consciousness, attention, cognition, and perception that develop over a
short period of time
Risk Factors
Decreased mobility, decreased restraints, dementia, uctuation in sleep-wake cycle, history of stroke,
impaired cognition, infection, male gender, metabolic abnormalities: azotemia, decreased hemoglobin,
dehydration, electrolyte imbalances, increased BUN/creatinine, malnutrition, over 60 years of age, pain,
pharmaceutical agents: anesthesia, anticholinergics, diphenhydramine, multiple medications, opioids, psy-
choactive drugs, sensory deprivation, substance abuse, urinary retention
NIC, NOC, Client Outcomes, Nursing Interventions, Client/Family Teaching, Rationales,
and References
Refer to care plan for Acute Confusion.
Constipation Marilee Schmelzer, PhD, RN
NANDA-I
Definition
Decrease in normal frequency of defecation, accompanied by difcult or incomplete passage of stool and/or
passage of excessively hard, dry stool
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Constipation 239
Defining Characteristics
Feeling of rectal fullness; feeling of rectal pressure; straining with defecation; unable to pass stool; abdominal
pain; abdominal tenderness; anorexia; atypical presentations in older adults (e.g., change in mental status,
urinary incontinence, unexplained falls, elevated body temperature); borborygmi; change in bowel pattern;
decreased frequency; decreased volume of stool; distended abdomen; generalized fatigue; hard, formed stool;
headache; hyperactive bowel sounds; hypoactive bowel sounds; increased abdominal pressure; indigestion;
C
nausea; oozing liquid stool; palpable abdominal or rectal mass; percussed abdominal dullness; pain with
defecation; severe atus; vomiting
Related Factors (r/t)
Functional
Abdominal muscle weakness; habitual denial; habitual ignoring of urge to defecate; inadequate toileting
(e.g., timeliness, positioning for defecation, privacy); irregular defecation habits; insufcient physical activ-
ity; recent environmental changes
Psychological
Depression, emotional stress, mental confusion
Pharmacological
Aluminum-containing antacids; anticholinergics, anticonvulsants; antidiarrheal agents, antidepressants,
antilipemic agents, bismuth salts, calcium carbonate, calcium channel blockers, diuretics, iron salts, laxative
overdose, nonsteroidal antiinammatory drugs (NSAIDs), opioids, phenothiazines, sedatives, and
sympathomimetics
Mechanical
Neurological impairment, electrolyte imbalance, hemorrhoids, Hirschsprungs disease, obesity, postsurgical
obstruction, pregnancy, prostate enlargement, rectal abscess, rectal anal ssures, rectal anal stricture, rectal
prolapse, rectal ulcer, rectocele, tumors
Physiological
Change in eating patterns, change in usual foods, decreased motility of gastrointestinal tract, defecation dis-
order, dehydration, inadequate dentition, inadequate oral hygiene, insufcient ber intake, insufcient uid
intake, poor eating habits
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Bowel Elimination, Hydration
Example NOC Outcome with Indicators
Bowel Elimination as evidenced by the following indicators: Elimination pattern/Stool soft and formed/Passage of stool
without aids/Ease of stool passage. (Rate each indicator of Bowel Elimination: 1 = severely compromised, 2 = substantially
compromised, 3 = moderately compromised, 4 = mildly compromised, 5 = not compromised [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Maintain passage of soft, formed stool every 1 to 3 days without straining
State relief from discomfort of constipation
Identify measures that prevent or treat constipation
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
240 Constipation
NIC (Nursing Interventions Classification)
Suggested NIC Intervention
Constipation/Impaction Management
C Example NIC ActivitiesConstipation/Impaction Management
Identify factors (e.g., medications, bed rest, and diet) that may cause or contribute to constipation/impaction; Institute a toileting
schedule, as appropriate
Nursing Interventions and Rationales
Assess usual pattern of defecation, including time of day, amount and frequency of stool, consistency of
stool; history of bowel habits or laxative use; diet, including ber and uid intake; exercise patterns; per-
sonal remedies for constipation; obstetrical/gynecological history; surgeries; diseases that affect bowel
motility; alterations in perianal sensation; present bowel regimen. Individual bowel habits vary and clients
with constipation experience a variety of symptoms (Spinzi et al, 2009).
Consider emotional inuences (e.g., depression and anxiety) on defecation. Emotions inuence gastroin-
testinal function, possibly because control of both emotions and gastrointestinal function is located in the
limbic system of the brain. Difculties with defecation often begin in childhood (e.g., during toilet training),
and constipation is also associated with sexual and physical abuse, depression, and anxiety (Whitehead et al,
2009). EBN: In a study, clients with functional constipation were compared to normal controls; subjects with
functional constipation had signicantly higher anxiety and depression scores (Zhou et al, 2010).
Have the client or family keep a 7-day diary of bowel habits, including information such as time of day;
usual stimulus; consistency, amount, and frequency of stool; difculty defecating; uid consumption; and
use of any aids to defecation. Health care providers dene constipation mainly in terms of frequency, but
those affected are more concerned about hard stool and discomfort and straining when attempting to defecate
(Wald et al, 2008). CEB: A diary of bowel habits is valuable in treatment of constipation; the use of a diary has
proven to be more accurate than client recall in determining the presence of constipation (Andersen et al,
2006).
Use the Bristol Stool Scale to assess stool consistency. The Bristol Stool scale is widely used as a more objec-
tive measure to describe stool consistency (Tack et al, 2011).
Review the clients current medications. EB: Many medications are associated with chronic constipation
including opioids, anticholinergics, antidepressants, antihypertensives (e.g., clonidine, calcium channel block-
ers), antispasmodics, diuretics, anticonvulsants, and psychotropics (Eoff & Lembo, 2008; Spinzi et al, 2009).
If clients are suffering from constipation and are taking constipating medications, consult with the health
care provider (with prescriptive powers) about the possibilities of decreasing the medication dosages or
nding an alternative medication that is less constipating (Gallagher, OMahony, & Quigley, 2008).
Recognize that opioids cause constipation. If the client is receiving temporary opioids (e.g., for acute
postoperative pain), request an order for routine stool softeners from the primary care practitioner, mon-
itor bowel movements, and request a laxative if the client develops constipation. If the client is receiving
around-the-clock opiates (e.g., for palliative care), request an order for Senokot-S and institute a bowel
regimen. Opioids cause constipation because they decrease propulsive movement in the colon and enhance
sphincter tone, making it difcult to defecate. Senokot-S is recommended to prevent constipation when opioids
are given around the clock (Kyle, 2007). EB: In a study of hip fracture clients who received opioids following
surgery, clients who received prophylactic laxatives were less likely to develop constipation than those who did
not (Davies et al, 2008).
If the client is terminally ill and is receiving around-the-clock opioids for palliative care, speak with the
prescribing provider about ordering methylnaltrexone, a drug that blocks opioid effects on the gastroin-
testinal tract without interfering with analgesia. Methylnaltrexone is FDA approved for clients in palliative
care when other laxatives are ineffective (Greenwood-Van Meerveld & Standifer, 2008). Methylnaltrexone
does not replace, but is given in addition to, the usual laxative regimen (Kyle, 2009). EB: In an RCT with
subjects with opioid-induced constipation, a signicantly greater percentage of those who received methylnal-
trexone had a bowel movement within 4 hours (without other laxatives) than those who received placebo
(Thomas et al, 2008). In a randomized study of clients who took opioids for chronic, nonmalignant pain, those
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Constipation 241
who received subcutaneous methylnaltrexone daily or every other day had signicantly more bowel move-
ments than subjects who received the placebo (Michna et al, 2011).
If new onset of constipation, determine if the client has recently stopped smoking. Constipation is com-
mon, but usually transient, when people stop smoking (Wilcox et al, 2010). CEB: In a survey about perceived
effects of various foods and beverages on constipation, cigarettes was the item that was most often perceived to
have a laxative effect among smokers in all three groups (Mller-Lissner et al, 2005). C
Palpate for abdominal distention, percuss for dullness, and auscultate bowel sounds. In clients with consti-
pation the abdomen is often distended and tender, and stool in the colon produces a dull percussion sound.
Bowel sounds will be present.
Check for impaction; if present, perform digital removal of stool per providers order. An impaction is
hard stool that is too large to move through the sphincter and must be removed manually. Clients with neuro-
genic bowel dysfunction (e.g., spinal cord injury) commonly require manual evacuation of stool (Coggrave &
Norton, 2009).
Encourage ber intake of 20 g/day (for adults) ensuring that the ber is palatable to the individual and
that uid intake is adequate. Add ber gradually to decrease bloating and atus. Larger stools move through
the colon faster than smaller stools, and dietary ber make stools bigger because it is undigested in the upper
intestinal tract. Fiber fermentation by bacteria in the colon produces gas. The effectiveness of water-insoluble
bers (e.g., wheat bran) on bowel function is well supported by research, and there is growing evidence that
water-soluble bers (e.g., psyllium) also promote laxation (Vuksan et al, 2008). CEB: The Nurses Health
Study found that women with a median ber intake of 20 g/day were less likely to experience constipation than
those with a median intake of 7 g/day (Dukas, Willett, & Giovannucci, 2003). In a study of subjects receiving
each of 5 treatments in a randomized design, the 5 treatments included: (1) bran cereal, (2) bran with corn
cereal, (3) bran with psyllium cereal, (4) a cereal blend of 70% glucomannan and 30% xanthan, and (5) the
low-ber control diet. All four cereals produced signicantly greater bowel movement than the low-ber control
diet and all were well tolerated (Vuksan et al, 2008). Researchers found that rye bread shortened intestinal
transit time, softened the feces, and eased defecation of women with constipation, and that yogurt lessened the
bloating and atulence resulting from rye bread (Hongisto et al, 2006).
Use a mixture of bran cereal, applesauce, and prune juice; begin administration in small amounts and
gradually increase amount. Keep refrigerated. Always check with the primary care provider before initiat-
ing this intervention. It is important that the client also ingest sufcient uids. CEB: This bran mixture has
been shown to be effective even with short-term use in elderly clients recovering from acute conditions; how-
ever, it has not been tested with an RCT (Joanna Briggs Institute, 2008). NOTE: Giving ber without sufcient
uid may result in worsening of constipation. Additional dietary ber and bulk-forming laxatives are inap-
propriate for those who have difculty ingesting adequate uids, such as clients in palliative care (Kyle, 2007).
Provide prune or prune juice daily. Each 100 g of prunes contain about 6 g of ber, 15 g of sorbitol, and 184
mg of polyphenol; all have laxative effects (Attaluri et al, 2011). CEB: In a study about the perceived effects of
various foods and beverages on stool consistency, over half of subjects surveyed reported that prunes had a
softening effect on their stools (Mller-Lissner et al, 2005). In a randomized study, dried prunes produced
signicantly more complete spontaneous bowel movements (CSBMs) per week than psyllium, and both treat-
ments produced signicantly more CSBMs than at baseline (Attaluri et al, 2011).
Encourage a uid intake of 1.5 to 2 L/day (6 to 8 glasses of liquids per day), unless contraindicated because
of other health concerns such as renal or heart disease. Cereal bers such as wheat bran add additional bulk
by attracting water to the ber, so adequate uid intake is essential. CEB: When dehydrated, the body absorbs
additional water from stools, resulting in dry, hard stools that are difcult to pass (Sykes, 2006). Increasing
uid intake is not helpful if the person is already well hydrated.
If the client is uncomfortable or in pain due to constipation or has acute or chronic constipation that does
not respond to increased ber, uid, activity, and appropriate toileting, refer the client to the primary care
provider for an evaluation of bowel function and health status. There can be multiple causes of constipation,
such as endocrine disorders (e.g., hypothyroidism), depression, neurological conditions (e.g., multiple sclerosis
and Parkinsons disease), anorectal disorders, and Hirschsprungs disease (Eoff & Lembo, 2008).
Encourage clients to resume walking and activities of daily living as soon as possible if their mobility has
been restricted. Encourage turning and changing positions in bed, lifting the hips off the bed, performing
range-of-motion exercises, alternately lifting each knee to the chest, doing wheelchair lifts, doing waist
twists, stretching the arms away from the body, and pulling in the abdomen while taking deep breaths.
Bed rest and decreased mobility lead to constipation, but additional exercise does not help the constipated
person who is already mobile. When the client has diminished mobility, even minimal activity increases
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
242 Constipation
peristalsis, which is necessary to prevent constipation (Joanna Briggs Institute, 2008). CEB: Twelve weeks of
physical activity signicantly decreased symptoms of constipation and difculty defecating in sedentary clients
with chronic constipation, but transit time decreased only in subjects who had abnormally long transit time
before starting the exercise program (DeSchryver et al, 2005). In a study of 192 hospitalized clients which
included daily recording of activity levels, being bedridden for 2 to 3 weeks accounted for a sixfold increase in
C dissatisfaction with bowel emptying (Cardin et al, 2010).
Ask clients when they normally have a bowel movement and assist them to the bathroom at that same
time every day to establish regular elimination. An optimal time for many individuals is 30 minutes after
breakfast because of the gastrocolic reex (Godfrey & Rose, 2007). CEB: When clients followed a bowel pro-
gram that included adequate hydration, dietary ber and regular toileting, most resumed normal bowel elimi-
nation patterns without laxatives (Benton et al, 1997). When subjects who had suffered a stroke were randomly
scheduled for morning or evening defecation, those defecating in the morning after breakfast returned to regu-
lar elimination patterns signicantly faster. Subjects whose defecation was scheduled for the same time of day
as their normal, pre-stroke patterns also resumed normal elimination patterns signicantly faster (Venn,
1992).
Provide privacy for defecation. If not contraindicated, help the client to the bathroom and close the door.
Bowel elimination is a private act in Western cultures, and a lack of privacy can hinder the defecation urge,
thus contributing to constipation (Kyle, 2011).
Help clients onto a bedside commode or toilet so they can either squat or lean forward while sitting. Rec-
ognize that it is difcult to impossible to defecate in the lying supine position. Sitting upright allows gravity
to aid defecation. CEB: A study of men found that exing the hip to 90 degrees or more straightens the angle
between the anus and the rectum and pulls the anal canal open, to decrease the resistance to the movement of
feces from the rectum and the amount of pressure needed to empty the rectum. Hip exion is greatest when
squatting or when leaning forward while sitting (Tagart, 1966). In a study involving volunteers, defecation
required signicantly less time and was signicantly easier when squatting than when sitting (Sikirov, 2003).
In another study, researchers found a signicant decrease in the ability of subjects to defecate both a water-
lled balloon and a silicone device in the lying position versus the sitting position (Rao, Kavolic, & Rao, 2006).
Teach clients to respond promptly to the defecation urge. CEB: A study of male volunteers determined that
the defecation urge can be delayed and that delaying defecation decreased bowel movement frequency, stool
weight, and transit time (Klauser et al, 1990).
Provide laxatives, suppositories, and enemas only as needed if other more natural interventions are not
effective, and as ordered only; establish a client goal of eliminating their use. EB & CEB: Moderate evidence
exists for the efcacy of lactulose, laxatives containing polyethylene glycol, and bulking agents (e.g., psyllium
and bran) for the treatment of constipation in the elderly (Joanna Briggs Institute, 2008). Use of stimulant
laxatives should be avoided because they result in laxative dependence and loss of normal bowel function.
Laxatives (e.g., bisacodyl) and enemas also damage the surface epithelium of the colon (Schmelzer et al, 2004).
When giving large volume enema solutions (e.g., soap-suds or tap-water enemas), measure the amount
of uid given and the amount expelled, especially when giving repeated enemas. Use a low concentration
of Castile soap in the soap-suds enema. Enema uid can be retained, and this retained uid can be harmful
for the client prone to uid overload. CEB: In studies comparing the effectiveness of soap-suds enemas in pre-
operative liver transplant clients (Schmelzer et al, 2000) and in healthy subjects (Schmelzer et al, 2004), the
amount of enema solution given was often larger than the amount of returns, and some subjects retained large
amounts of solution. Biopsies taken immediately after soap-suds and tap-water enemas demonstrated damage
to the surface epithelium of the colon (Schmelzer et al, 2004).
Geriatric
Assess older adults for the presence of factors that contribute to constipation, including dietary ber and
uid intake (less than 1.5 L/day), physical activity, use of constipating medications, and diseases that are
associated with constipation.
Explain the importance of adequate ber intake, uid intake, activity, and established toileting routines to
ensure soft, formed stool. EB: Strong evidence exists for the efcacy of adequate hydration and dietary ber
in the prevention of constipation in older adults; moderate evidence exists for the effectiveness of increased
activity for those restricted to bed rest (Joanna Briggs Institute, 2008). In an RCT of elderly nursing home resi-
dents who were chronically ill and regularly used laxatives, those who received an additional 5.1 g of oat bran
with their usual diets had signicant reductions in laxative use when compared to those who did not (Sturtzel
& Elmadfa, 2008). CEB: A study involving institutionalized elderly men with chronic constipation
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Constipation 243
demonstrated that, with use of a bran mixture, clients were able to discontinue use of oral laxatives (Howard,
West, & Ossip-Klein, 2000).
Determine the clients perception of normal bowel elimination and laxative use; promote adherence to a
regular schedule. EB: In a survey in the United States, United Kingdom, Germany, France, Italy, Brazil, and
South Korea, elderly subjects reported more constipation and used laxatives more often than younger subjects
(Wald et al, 2008). C
Explain why straining (Valsalva maneuver) should be avoided. Excessive straining can cause syncope or
cardiac dysrhythmias in susceptible people (Gallagher, OMahony, & Quigley, 2008).
Respond quickly to the clients call for assistance with toileting.
Offer food, uids, activity and toileting opportunities to elderly clients who are cognitively impaired. Even
cognitively impaired individuals who are unable to initiate a request for food, uids, and so forth may respond
when opportunities are offered (Gallagher, OMahony, & Quigley, 2008). EB: In an RCT study involving
nursing home residents, subjects who received the treatment protocol (offering of food, uid, activity, and toi-
leting opportunities) had signicantly more bowel movements than the control group. Both cognitively intact
and cognitively impaired subjects beneted from the treatment (Schnelle et al, 2010).
Avoid regular use of enemas in the elderly. Enemas can cause uid and electrolyte imbalances (Gallagher,
OMahony, & Quigley, 2008) and damage to the colonic mucosa (Schmelzer et al, 2004). However, judicious
enema use may help prevent impactions (Gallagher, OMahony, & Quigley, 2008).
Use opioids cautiously. Opioids cause constipation (Davies et al, 2008).
Position the client on the toilet or commode and place a small footstool under the feet. Placing a small
footstool helps the client assume a squatting posture to facilitate defecation.
Home Care
The interventions described previously may be adapted for home care use.
Take complaints seriously and evaluate claims of constipation in a matter-of-fact manner. Continued
constipation can lead to bowel obstruction, a medical emergency. Use of a matter-of-fact manner will limit
positive reinforcement of the behavior if actual constipation does not exist. Refer to the care plan for Per-
ceived Constipation.
Assess the self-care management activities the client is already using. CEB: Many older adults seek solutions
to constipation, with laxative use a frequent remedy that creates its own problems (Annells & Koch, 2002).
The following treatment recommendations have been offered):
Acknowledge the clients life-long experience of bowel function; respect beliefs, attitudes, and prefer-
ences, and avoid patronizing responses.
Make available comprehensive, useful written information about constipation and possible
solutions.
Make available empathetic and accessible professional care to provide treatment and advice; a multi-
disciplinary approach (including physician, nurse, and pharmacist) should be used.
Institute a bowel management program.
Consider affordability when suggesting solutions to constipation; discuss cost-effective strategies.
Discuss a range of solutions to constipation and allow the client to choose the preferred options.
Have orders in place for a suppository and enema as the need may occur. As part of a bowel manage-
ment program, suppositories or enemas may become necessary.
Although the use of a bedside commode may be necessitated by the clients condition, allow the client to
use the toilet in the bathroom when possible and provide assistance. Bowel elimination is a very private act,
and a lack of privacy can contribute to constipation.
In older clients, routinely advise consumption of uids, fruits, and vegetables as part of the diet, and
ambulation if the client is able. Introduce a bowel management program at the rst sign of constipation.
Constipation is a major problem for terminally ill or hospice clients, who may need very high doses of opioids
for pain management (Sykes, 2006).
Refer for consideration of the use of polyethylene glycol 3350 (PEG-3350) for constipation. CEB: In a
study of PEG-3350 use for idiopathic constipation, researchers concluded that it appeared to be safe and efca-
cious when dietary and lifestyle changes were ineffective. Clients reported increased perceived bowel control,
with reduced complaints of straining, stool hardness, bloating, and gas (Stoltz et al, 2001). There is good evi-
dence to support the use of PEG for chronic constipation (Ramkumar & Rao, 2005).
Advise the client against attempting to remove impacted feces on his or her own. Older or confused clients
in particular may attempt to remove feces and cause rectal damage.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
244 Constipation
When using a bowel program, establish a pattern that is very regular and allows the client to be part of the
family unit. Regularity of the program promotes psychological and/or physiological readiness to evacuate stool.
Families of home care clients often cannot proceed with normal daily activities until bowel programs are complete.
Client/Family Teaching and Discharge Planning
C Instruct the client on normal bowel function and the need for adequate uid and ber intake, activity, and
a dened toileting pattern in a bowel program.
Encourage the client to heed defecation warning signs and develop a regular schedule of defecation by
using a stimulus such as a warm drink or prune juice. Most cases of constipation are mechanical and result
from habitual neglect of impulses that signal the appropriate time for defecation.
Encourage the client to avoid long-term use of laxatives and enemas and to gradually withdraw from their
use if they are used regularly. Use of stimulant laxatives should be avoided; long-term use can result in depen-
dence on laxative for defecation (Roerig et al, 2010).
If not contraindicated, teach the client how to do bent-leg sit-ups to increase abdominal tone; also encour-
age the client to contract the abdominal muscles frequently throughout the day. Help the client develop a
daily exercise program to increase peristalsis.
REFERENCES
Andersen C, et al: The effect of a multidimensional exercise programme Joanna Briggs Institute: Management of constipation in older adults,
on symptoms and side-effects in cancer patient undergoing Aust Nurs J 16(5):3235, 2008.
chemotherapythe use of semi-structured diaries, Eur J Oncol Nurs Jones MP, et al: Brain-gut connections in functional GI disorders:
10:247262, 2006. anatomic and physiologic relationships, Neurogastrointest Motil
Annells M, Koch T: Older people seeking solutions to constipation: the 18:91103, 2006.
laxative mire, J Clin Nurs 11:603, 2002. Klauser AG, et al: Behavioral modication of colonic function. Can
Attaluri A, et al: Randomised clinical trial: dried plums (prunes) vs psyl- constipation be learned? Dig Dis Sci 35(10):12711275, 1990.
lium for constipation, Aliment Pharmacol Ther 33:822828, 2011. Kyle G: Constipation and palliative carewhere are we now? Int J Pal-
Benton JM, et al: Changing bowel hygiene practice successfully: a pro- liat Nurs 13(1):616, 2007.
gram to reduce laxative use in a chronic care hospital, Geriatr Nurs Kyle G: Methylnaltrexone: a subcutaneous treatment for opioid-
18(1):1217, 1997. induced constipation in palliative care patients, Int J Palliat Nurs
Cardin F, et al: Constipation in the acutely hospitalized older patients, 15(11):533540, 2009.
Arch Gerontol Geriatr 50:277281, 2010. Kyle G: Risk assessment and management tools for constipation, Br J
Coggrave MJ, Norton C: The need for manual evacuation and oral Community Nurs 16(5):224230, 2011.
laxatives in the management of neurogenic bowel dysfunction after Michna E, et al: Subcutaneous methylnaltrexone for treatment of
spinal cord injury: a randomized controlled trial of a stepwise proto- opioid-induced constipation in patients with chronic, nonmalignant
col, Spinal Cord 48:504510, 2010. pain: a randomized controlled study, J Pain 12(5):554562, 2011.
Davies EC, et al: The use of opioids and laxatives, and incidence of Mller-Lissner SA, et al: The perceived effect of various foods and bev-
constipation, in patients requiring neck-of-femur (NOF) surgery: a erages on stool consistency, Eur J Gastroenterol Hepatol 17:109112,
pilot study, J Clin Pharm Ther 33:561566, 2008. 2005.
DeSchryver AM, et al: Effects of regular physical activity on defecation Rao SSC, Kavolic R, Rao S: Inuence of body position and stool
pattern in middle-aged patients complaining of chronic constipa- characteristics on defecation in humans, Am J Gastroenterol
tion, Scand J Gastroenterol 40:422429, 2005. 206(101):27902796, 2006.
Dukas L, Willett WC, Giovannucci EL: Association between physical Ramkumar D, Rao SS: Efcacy and safety of traditional medical thera-
activity, ber intake, and other lifestyle variables and constipation in pies for chronic constipation: systematic review, Am J Gastroenterol
a study of women, Am J Gastroenterol 98(8):17901796, 2003. 100(4):936971, 2005.
Eoff JC, Lembo AG: Optimal treatment of chronic constipation in man- Roerig JL, et al: Laxative abuse: epidemiology, diagnosis and management,
aged care: review and roundtable discussion, J Managed Care Pharm Drugs 70(12):14871503, 2010. doi; 10.2165/11898640-000000000-
(Suppl) 14(9-a):S1S17, 2008. 00000.
Gallagher PF, OMahony D, Quigley MM: Management of chronic Schmelzer M, et al: Colonic cleansing, uid absorption, and discomfort
constipation in the elderly, Drugs Aging 25(10):807821, 2008. following tap water and soapsuds enemas, Appl Nurs Res 13(2):83,
Godfrey JR, Rose S: Conversations with the experts: toward optimal 2000.
health: Suzanne Rose, MD, MSEd, discusses management of consti- Schmelzer M, et al: Safety and effectiveness of large-volume enema solu-
pation in women, J Womens Health 16(9):12521257, 2007. tions, Appl Nurs Res 17(4):265274, 2004.
Greenwood-Van Meerveld B, Standifer KM: Methylnaltrexone in the Schnelle JF, et al: A controlled trial of an intervention to improve
treatment of opioid-induced constipation, Clin Exp Gastroenterol urinary and fecal incontinence and constipation, J Am Geriatr Soc
49-58:2008, 2008. 58(8):15041511, 2010.
Hongisto S-M, et al: A combination of bre-rich rye bread and yoghurt Sikirov D: Comparison of straining during defecation in three positions:
containing Lactobacillus GG improves bowel function in women results and implications for human health, Dig Dis Sci 48(7):1201
with self-reported constipation, Eur J Clin Nutr 60:319324, 2006. 1205, 2003.
Howard LV, West D, Ossip-Klein DJ: Chronic constipation manage- Spinzi G, et al: Constipation in the elderly, Drugs Aging 26(6):469474,
ment for institutionalized older adults, Geriatr Nurs 21(2):78, 2000. 2009.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Perceived constipation 245
Stolz R, et al: An efcacy and consumer preference study of polyethyl- Vuksan V, et al: Using cereal to increase dietary ber intake to the
ene glycol 3350 for the treatment of constipation in regular laxative recommended level and the effect of ber on bowel function in
users, Home Health Consult 8(2):21, 2001. healthy persons consuming North American diets, Am J Clin Nutr
Sturtzel B, Elmadfa I: Intervention with dietary ber to treat constipa- 88:12561262, 2008.
tion and reduce laxative use in residents of nursing homes, Ann Wald A, et al: A multinational survey of prevalence and patterns of
Nutr Metab 52(suppl 1):5456, 2008. laxative use among adults with self-dened constipation, Aliment
Sykes NP: The pathogenesis of constipation, J Support Oncol 4(5):213
218, 2006.
Pharmacol Ther 28:917930, 2008.
Whitehead WE, et al: Conservative and behavioural management of
C
Tack J, et al: Diagnosis and treatment of chronic constipationa Euro- constipation, Neurogastroenterol Motil 2(21(Suppl):5561, 2009.
pean perspective, Neurogastroenterol Motil 23:697710, 2011. Wilcox CS, et al: An open-label study of naltrexone and bupropion
Tagart REB: The anal canal and rectum: their varying relationship and combination therapy for smoking cessation in overweight and obese
its effect on anal continence, Dis Colon Rectum 9(6):449452, 1966. subjects, Addict Behav 35(3):229234, 2010.
Thomas J, et al: Methylnaltrexone for opioid-induced constipation in Zhou L, et al: Functional constipation: implications for nursing inter-
advanced illness, N Engl J Med 358(22):23322343, 2008. ventions, J Clin Nurs 19:18381843, 2010.
Venn MR: The inuence of timing and suppository use on efciency
and effectiveness of bowel training after a stroke, Rehabil Nurs
17(3):116121, 1992.
Perceived Constipation Betty Ackley, MSN, EdS, RN, and Marilee Schmelzer, PhD, RN
NANDA-I
Definition
Self-diagnosis of constipation and abuse of laxatives, enemas, and suppositories to ensure a daily bowel
movement
Defining Characteristics
Expectation of a daily bowel movement that results in overuse of laxatives, enemas, and suppositories; expec-
tation of a passage of stool at same time every day
Related Factors (r/t)
Cultural or family health beliefs, faulty appraisals (long-term expectations/habits), impaired thought
processes
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Bowel Elimination, Health Beliefs, Health Beliefs: Perceived Threat
Example NOC Outcome with Indicators
Bowel Elimination as evidenced by the following indicators: Elimination pattern/Stool soft and formed/ Passage of stool
without aids/Ease of stool passage. (Rate each indicator of Bowel Elimination: 1 = severely compromised, 2 = substantially
compromised, 3 = moderately compromised, 4 = mildly compromised, 5 = not compromised [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Regularly defecate soft, formed stool without use of aids
Explain the need to decrease or eliminate the use of stimulant laxatives, suppositories, and enemas
Identify alternatives to stimulant laxatives, enemas, and suppositories for ensuring defecation
Explain that defecation does not have to occur every day
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Bowel Management; Medication Management
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
246 Perceived constipation
Example NIC ActivitiesBowel Management
Note preexistent bowel problems, bowel routine, and use of laxatives; Initiate a bowel training program, as appropriate
C Nursing Interventions and Rationales
Have the client keep a 7-day diary of bowel habits, including information such as time of day; usual stimu-
lus; consistency, amount, and frequency of stool; difculty defecating; uid consumption; and use of any
aids to defecation. Health care providers dene constipation mainly in terms of frequency, but those affected
are more concerned about hard stool and discomfort and straining when attempting to defecate (Wald et al,
2008). CEB & EB: A diary of bowel habits is valuable in treatment of constipation; the use of a diary has proven
to be more accurate than client recall in determining the presence of constipation (Andersen et al, 2006). A
bowel diary was shown to be helpful for clients with opioid-induced constipation (Camilleri et al, 2010).
Determine the clients perception of an appropriate defecation pattern. The client may need to be taught
that one bowel movement every 1 to 3 days is normal (Mayo Foundation for Medical Education and Research,
2011a).
Recognize the emotional inuences (e.g., depression and anxiety) on defecation. The relationship between
emotions and bowel function can be explained as stress-mediated brain-gut dysfunction and can range from
altered stress-induced mucosal immune function to impaired ability of the central nervous system to down-
regulate incoming gut or body afferent signals (Drossman, 2011). Difculties with defecation often begin in
childhood (e.g. during toilet training) (van Dijk et al, 2007), and constipation is also associated with sexual
and physical abuse, depression, and anxiety (Whitehead et al, 2009). EBN: In a study, clients with functional
constipation were compared to normal controls; subjects with functional constipation had signicantly higher
anxiety and depression scores (Zhou et al, 2010).
Monitor the use of laxatives, suppositories, or enemas and suggest replacing them with increased ber
intake along with increased uids to 2 L/day. Use of stimulant laxatives should be avoided; long-term use can
result in dependence on laxative for defecation. In elderly clients with heart failure, use of laxatives containing
magnesium can lead to hypermagnesemia and possibly result in increased mortality (Corbi et al, 2008) An
increase in ber intake to 20 to 30 g/day along with an increase in uid intake can help clients with chronic
constipation (Sturtzel & Elmadfa, 2008).
Encourage ber intake of 20 g/day (for adults) ensuring that the ber is palatable to the individual and that
uid intake is adequate. Add ber gradually to decrease bloating and atus. Some people with eating disorders
do not eat enough ber to produce stools. Larger stools move through the colon faster than smaller stools, and dietary
ber makes stools bigger because it is undigested in the upper intestinal tract. Fiber fermentation by bacteria in the
colon produces gas. The effectiveness of water-insoluble bers (e.g., wheat bran) on bowel function is well supported
by research, and there is growing evidence that water-soluble bers (e.g., glucomannan and psyllium) also promote
laxation (Vuksan et al., 2008). For further information on use of ber, please refer to care plan Constipation.
Use a mixture of bran cereal, applesauce, and prune juice; begin administration in small amounts and
gradually increase amount. Keep refrigerated. Always check with the primary care practitioner before
initiating this intervention. It is important that the client also ingest sufcient uids. EBN & CEB: This
bran mixture has been shown to be effective even with short-term use in elderly clients recovering from acute
conditions; however, it has not been tested with an RCT (Joanna Briggs Institute, 2008). NOTE: Giving ber
without sufcient uid has resulted in worsening of constipation (Mller-Lissner et al, 2005).
Teach clients to respond promptly to the defecation urge. CEB: A study of male volunteers determined that the
defecation urge can be delayed and that delaying defecation decreased bowel movement frequency, stool weight, and
transit time (Klauser et al, 1990). The reex that causes the urge to defecate diminishes after a few minutes and may
remain quiet for several hours; as a result, the stool becomes hardened and more difcult to expel.
Obtain a referral to a dietitian for analysis of the clients diet and input on how to improve the diet to
ensure adequate ber intake and nutrition.
Assess for signs of depression, other psychological disorders, and a history of physical or sexual abuse.
Often, people with functional constipation have experienced physical or sexual abuse, and symptoms of con-
stipation may arise from psychological problems (OBrien et al, 2009). EB: A study found that somatic com-
plaints of constipation were common in people with depression (Afridi, Siddiqi, & Ansari, 2009).
Encourage the client to increase activity, walking for at least 30 minutes at least 5 days a week as tolerated.
Decreased mobility leads to constipation, but additional exercise does not help the constipated person who is
already mobile. When the client has diminished mobility, even minimal activity increases peristalsis, which is
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Perceived constipation 247
necessary to prevent constipation (Joanna Briggs Institute, 2008). EB: A program of increased toileting assis-
tance, increased exercise, and choice of food and uid snacks every 2 hours for 8 hours per day over 3 months
resulted in increased number of stools for nursing home residents (Schnelle et al, 2010).
Observe for the presence of an eating disorder, the use of laxatives to control or decrease weight; refer for
counseling if needed. People with eating disorders suffer from constipation and other gastrointestinal symp-
toms, or use laxatives as part of inducing weight loss (Roerig et al, 2010). CEB: Laxative abuse is found in C
clients with both anorexia and bulimia nervosa and may be associated with worsening of the eating disorder
as a form of self-harm (Tozzi et al, 2006).
Home Care
The interventions described previously may be adapted for home care use.
Take complaints seriously and evaluate claims of constipation in a matter-of-fact manner. Continued
constipation can lead to bowel obstruction, a medical emergency. Presence of a pattern of perceived constipa-
tion does not mean actual constipation cannot occur. However, use of a matter-of-fact manner will limit posi-
tive reinforcement of the behavior.
Obtain family and client histories of bowel or other patterned behavior problems. History may reveal a
psychological cause for the constipation (e.g., withholding) (van Dijk et al, 2007).
Observe family cultural patterns related to eating and bowel habits. Cultural patterns may control bowel
habits.
Encourage a mindset and program of self-care management. Elicit from the client the self-talk he or she
uses to describe body perceptions; correct fatalistic interpretations.
Instruct the client in a healthy lifestyle that supports normal bowel function (e.g., activity, uid intake,
diet) and encourage progressive inclusion of these elements into daily activities.
Discuss the clients self-image. Help the client to reframe the self-concept as capable. Developing the ability
to see themself as capable of self-care management may take time, as will making lifestyle changes.
Instruct the client and family in appropriate expectations for having bowel movements.
Offer instruction and reassurance regarding explanations for variation from the previous pattern of bowel
movements. The client may have unrealistic expectations regarding the frequency or type of bowel movements
and may assume that constipation exists when there is a reasonable explanation for deviation from the past
pattern. The client may resort to the use of laxatives inappropriately.
Contract with the client and/or a responsible family member regarding the use of laxatives. Have the cli-
ent maintain a bowel pattern diary. Observe for diarrhea or frequent evacuation. Intermittent care does not
allow for 24-hour supervision. Contracting allows guided control of care by the client in partnership with the
nurse, and the diary promotes more accurate reporting.
Teach the family to carry out the bowel program per the physicians orders.
Refer for home health aide services to assist with personal care, including the bowel program, if
appropriate.
Identify a contingency plan for bowel care if the client is dependent on outside persons for such care.
Client/Family Teaching and Discharge Planning
Explain normal bowel function and the necessary ingredients for a regular bowel regimen (e.g., uid,
ber, activity, and regular schedule for defecation).
Work with the client and family to develop a diet that ts the clients lifestyle and includes increased ber.
Teach the client that it is not necessary to have daily bowel movements and that the passage of anywhere
from three stools each day to three stools each week is considered normal. Explain to the client the harm-
ful effects of the continual use of defecation aids such laxatives and enemas. Lazy bowel syndrome may
occur if laxatives are used too frequently, causing the bowels to become dependent on laxatives to stimulate a
bowel movement. Overuse of laxatives can also lead to poor absorption of vitamins and other nutrients and
damage to the gastrointestinal tract (Mayo Foundation for Medical Education and Research, 2011b). Fre-
quent use of enemas can result in harm including absorption of bacteria and toxins (Seow-Choen, 2009).
Encourage the client to gradually decrease the use of the usual laxatives and or enemas, and recognize it
may take months for the process to do it gradually.
Determine a method of increasing the clients uid intake and t this practice into clients lifestyle.
Explain what Valsalva maneuver is and why it should be avoided.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
248 Risk for constipation
Work with the client and family to design a bowel training routine that is based on previous patterns
(before laxative or enema abuse) and incorporates the consumption of warm uids, increased ber, and
increased uids; privacy; and a predictable routine.
Refer care plan for Constipation for additional Nursing Interventions, Rationales, and Client/Family
Teaching and Discharge Planning.
C
REFERENCES
Afridi MI, Siddiqui MA, Ansari A: Gastrointestinal somatization OBrien S, et al: Sexual abuse: a strong predictor of outcomes after
in males and females with depressive disorder, J Pak Med Assoc colectomy for slow-transit constipation, Dis Colon Rectum
59(10):675679, 2009. 52(11):18441847, 2009.
Andersen C, et al: The effect of a multidimensional exercise programme Roerig JS, et al: Laxative abuse: epidemiology, diagnosis and manage-
on symptoms and side-effects in cancer patient undergoing ment, Drugs 70(12):14871503, 2010.
chemotherapythe use of semi-structured diaries, Eur J Oncol Nurs Schnelle JF, et al: A controlled trial of an intervention to improve
10:247262, 2006. urinary and fecal incontinence and constipation, J Am Geriatr Soc
Camilleri M, et al: Validation of a bowel function diary for assessing 58(8):15041511, 2010.
opioid-induced constipation, Am J Gastroenterol 106(3):497506, 2011. Seow-Choen F: The physiology of colonic hydrotherapy, Colorectal Dis
Corbi G, et al: Hypermagnesemia predicts mortality in elderly with 11(7):686688, 2009.
congestive heart disease: relationship with laxative and antacid use, Sturtzel B, Elmadfa I: Intervention with dietary ber to treat constipa-
Rejuv Res 11(1):129138, 2008. tion and reduce laxative use in residents of nursing homes, Ann
Drossman DA: Abuse, trauma, and GI illness: is there a link? Am J Nutr Metab 52(Suppl 1):5456, 2008.
Gastroenterol 106(1):1425, 2011. Tozzi F, et al: Features associated with laxative abuse in individuals with
Eoff JC, Lembo AJ: Optimal treatment of chronic constipation in man- eating disorders, Psychosomat Med 68(3):470477, 2006.
aged care: review and roundtable discussion, J Manage Care Pharm van Dijk M, et al: Chronic childhood constipation: a review of the lit-
(Suppl) 14(9a):S1S17, 2008. erature and the introduction of a protocolized behavioral interven-
Joanna Briggs Institute: Management of constipation in older adults, tion program, Patient Educ Couns 67:6377, 2007.
Aust Nurs J 16(5):3235, 2008. Vuksan V, et al: Using cereal to increase dietary ber intake to the
Klauser AG, et al: Behavioral modication of colonic function. Can recommended level and the effect of ber on bowel function in
constipation be learned? Dig Dis Sci 35(10):12711275, 1990. healthy persons consuming North American diets, Am J Clin Nutr
Mayo Foundation for Medical Education and Research: Constipation: 88:12561262, 2008.
diseases and conditions, 2011a. Retrieved October 30, 2011, from Wald A, et al: A multinational survey of prevalence and patterns of
http://www.mayoclinic.com/health/constipation/DS00063/ laxative use among adults with self-dened constipation, Aliment
DSECTION=symptoms. Pharmacol Ther 28:917930, 2008.
Mayo Foundation for Medical Education and Research: Constipation. Whitehead WE, et al: Conservative and behavioural management of
Complications, diseases, and condition, 2011b. Retrieved October 30, constipation, Neurogastroenterol Motil 21(Suppl 2):5561, 2009.
2011, from http://www.mayoclinic.com/health/constipation/ Zhou L, et al: Functional constipation: implications for nursing inter-
DS00063/DSECTION=complications. ventions, J Clin Nurs 19:18381843, 2010.
Mller-Lissner SA, et al: Myths and misconceptions about constipation,
Am J Gastroenterol 100(1):232242, 2005.
Risk for Constipation Betty Ackley, MSN, EdS, RN
NANDA-I
Definition
At risk for a decrease in normal frequency of defecation accompanied by difcult or incomplete passage of
stool and/or passage of excessively hard, dry stool
Risk Factors
Functional
Abdominal weakness; habitual denial/ignoring of urge to defecate; recent environmental changes; inade-
quate toileting (e.g., timeliness, positioning for defecation, privacy); irregular defecation habits; insufcient
physical activity
Psychological
Depression; emotional stress; mental confusion
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Contamination 249
Physiological
Change in usual eating patterns, change in usual foods, decreased motility of gastrointestinal tract, dehydra-
tion, inadequate dentition, inadequate oral hygiene, insufcient ber intake, insufcient uid intake, poor
eating habits
Pharmacological C
Aluminum-containing antacids, anticholinergics, anticonvulsants, antidepressants, antilipemic agents, bis-
muth salts, calcium carbonate, calcium channel blockers, diuretics, iron salts, laxative overuse, nonsteroidal
antiinammatory drugs, opioids, phenothiazines, sedatives, and sympathomimetics
Mechanical
Electrolyte imbalance, hemorrhoids, Hirschsprungs disease, neurological impairment, obesity, postsurgical
obstruction, pregnancy, prostate enlargement, rectal abscess, rectal anal ssures, rectal anal stricture, rectal
prolapse, rectal ulcer, rectocele, tumors
NIC, NOC, Client Outcomes, Nursing Interventions, Client/Family Teaching, Rationales,
and References
Refer to care plans for Constipation.
Contamination Laura V. Polk, PhD, RN, and Pauline M. Green, PhD, RN, CNE
NANDA-I
Definition
Exposure to environmental contaminants in doses sufcient to cause adverse health effects
Defining Characteristics
Pesticides
Dermatological effects of pesticide exposure; gastrointestinal effects of pesticide exposure; neurological
effects of pesticide exposure; pulmonary effects of pesticide exposure; renal effects of pesticide exposure;
major categories of pesticides: insecticides, herbicides, fungicides, antimicrobials, rodenticides; major pesti-
cides: organophosphates, carbamates, organochlorines, pyrethrum, arsenic, glycophosphates, bipyridyls,
chlorophenoxy
Chemicals
Dermatological effects of chemical exposure; gastrointestinal effects of chemical exposure; immunologic
effects of chemical exposure; neurological effects of chemical exposure; pulmonary effects of chemical expo-
sure; renal effects of chemical exposure; major chemical agents: petroleum-based agents, anticholinesterases
type I agents act on proximal tracheobronchial portion of the respiratory tract, type II agents act on alveoli;
type III agents produce systemic effects
Biologicals
Dermatological effects of exposure to biologics; gastrointestinal effects of exposure to biologics; pulmonary
effects of exposure to biologics; neurological effects of exposure to biologics; renal effects of exposure to
biologics (toxins from organisms [bacteria, viruses, fungi])
Pollution
Neurological effects of pollution exposure; pulmonary effects of pollution exposure (major locations: air,
water, soil; major agents: asbestos, radon, tobacco, heavy metal, lead, noise, exhaust)
Waste
Dermatological effects of waste exposure; gastrointestinal effects of waste exposure; hepatic effects of waste
exposure; pulmonary effects of waste exposure (categories of waste: trash, raw sewage, industrial waste)
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
250 Contamination
Radiation
External exposure through direct contact with radioactive material; genetic effects of radiation exposure;
immunologic effects of radiation exposure; neurological effects of radiation exposure; oncological effects of
radiation exposure
C Related Factors (r/t)
External
Chemical contamination of food; chemical contamination of water; exposure to bioterrorism; exposure to
disasters (natural or human-made); exposure to radiation (occupation in radiology; employment in nuclear
industries and electrical generating plants; living near nuclear industries and/or electrical generating plants);
exposure through ingestion of radioactive material (e.g., food/water contamination); aking, peeling paint
in presence of young children; aking, peeling plaster in presence of young children; oor surface (carpeted
surfaces hold contaminant residue more than hard oor surfaces); geographic area (living in area where high
level of contaminants exist); household hygiene practices; inadequate municipal services (trash removal,
sewage treatment facilities); inappropriate use of protective clothing; lack of breakdown of contaminants
once indoors (breakdown is inhibited without sun and rain exposure); lack of protective clothing; lacquer in
poorly ventilated areas; lacquer without effective protection; living in poverty (increases potential for mul-
tiple exposure, lack of access to health care, poor diet); paint in poorly ventilated areas; paint without effec-
tive protection; personal hygiene practices; playing in outdoor areas where environmental contaminants are
used; presence of atmospheric pollutants; use of environmental contaminants in the home (e.g., pesticides,
chemicals, environmental tobacco smoke); unprotected contact with chemicals (e.g., arsenic); unprotected
contact with heavy metals (e.g., chromium, lead)
Internal
Age (children <5 years, older adults); concomitant exposures; developmental characteristics of children;
female gender; gestational age during exposure; nutritional factors (e.g., obesity, vitamin and mineral de-
ciencies); preexisting disease states; pregnancy; previous exposures; smoking
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Community Health Status, Family Physical Environment, Anxiety Level, Fear Level
Example NOC Outcome with Indicators
Community Health Status as evidenced by the following indicators: Evidence of health protection measures/Compliance
with environmental health standards/Health status of population. (Rate the outcome and indicators of Community Health
Status: 1 = poor, 2 = fair, 3 = good, 4 = very good, 5 = excellent [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Have minimal health effects associated with contamination
Cooperate with appropriate decontamination protocol
Participate in appropriate isolation precautions
Community Will (Specify Time Frame):
Utilize health surveillance data system to monitor for contamination incidents
Utilize disaster plan to evacuate and triage affected members
Have minimal health effects associated with contamination
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Triage: Disaster, Infection Control, Anxiety Reduction, Crisis Intervention, Health Education
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Contamination 251
Example NIC ActivitiesTriage: Disaster
Initiate appropriate emergency measures, as indicated; Monitor for and treat life-threatening injuries or acute needs
Nursing Interventions and Rationales
Help individuals cope with contamination incident by doing the following:
C
Use groups that have survived terrorist attacks as useful resource for victims
Provide accurate information on risks involved, preventive measures, use of antibiotics, and vaccines
Assist to deal with feelings of fear, vulnerability, and grief
Encourage individuals to talk to others about their fears
Assist victims to think positively and to move toward the future
CEB: A crisis situation follows a predictable course in which individuals progress in response to a precipitating
stressor and that culminate in a state of acute crisis. Interventions aimed at supporting an individuals coping
help the person deal with feelings of fear, helplessness, and loss of control that are normal reactions in a crisis
situation (Boscarino et al, 2006; Caplan, 1964).
Triage, stabilize, transport, and treat affected community members. CEB: Accurate triage and early treat-
ment provide the best chance of survival to affected persons (Murdoch & Cymet, 2006; Veenema, 2007).
Utilize approved procedures for decontamination of persons, clothing, and equipment. Victims may rst
require decontamination prior to entering health facility to receive care in order to prevent the spread of con-
tamination (U.S. Army Medical Research Institute of Infectious Diseases, 2005).
Utilize appropriate isolation precautions: universal, airborne, droplet, and contact isolation. Proper use of
isolation precautions prevents cross-contamination by contaminating agents (U.S. Army Medical Research
Institute of Infectious Diseases, 2005).
Monitor individual for therapeutic effects, side effects, and compliance with postexposure drug therapy.
Drug therapy may extend over a long period of time and will require monitoring for compliance as well as
therapeutic and side effects (Veenema, 2007).
Collaborate with other agencies (local health department, emergency medical service [EMS], state and
federal agencies). Communication among agencies increases ability to handle crisis efciently and correctly
(CDC, 2009; Veenema, 2007).
Geriatric
Help the client identify age-related factors that may affect response to contamination incidents.
Encourage family members to acknowledge and validate the clients concerns. Validation alleviates anxiety
and increases clients ability to cope (Boscarino et al, 2006).
Advise the elderly to follow public notices related to drinking water. Contaminated water can harm the
health of older persons and those with chronic conditions (EPA, 2009).
Encourage older adults to receive inuenza vaccination when it is available beginning as early as late
August and continuing through the end of February. This administration schedule is cost effective, and
comorbidities increase a persons risk of inuenza and inuenza-related complications (Lee et al, 2009).
Pediatric
Provide environmental health hazard information. Developing children are more vulnerable to environ-
mental toxicants due to greater and longer exposure and particular susceptibility windows (Childrens Envi-
ronmental Health Network, 2006).
Caution families to avoid having children play in streams following heavy rainfall. Exposure to microbial
water contamination after periods of heavy rainfall is linked to an increase in acute gastrointestinal illnesses in
children (Drayna et al, 2010).
Multicultural
Ask about use of imported or culture-specic products. Immigrant children are at increased risk of con-
tamination, particularly from lead, related to exposure to imported culture-specic products (Lin et al,
2010).
Assess exposure to multiple pollutants, pre-existing disease, poor nutrition, substandard housing, and
limited access to health care. These factors related to lower socioeconomic status increase Latino childrens
susceptibility to environmental contaminants (Carter-Pokras et al, 2007).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
252 Risk for contamination
Nurses need to consider the cultural and social factors that impact access to and understanding of the
health care system, particularly for groups such as migrant workers who do not have consistent care pro-
viders EB: Subtle cultural biases in how nurses approach care can affect outcomes (Holmes, 2006).
Home Care
C Assess current environmental stressors and identify community resources. Accessing resources decreases
stress and increases ability to cope (Boscarino et al, 2006).
Residential settings may present household related hazards that impact health such as spread of nosoco-
mial infections and unsanitary, unsafe conditions (Gershon et al, 2008).
Client/Family Teaching and Discharge Planning
Provide truthful information to the person or family affected.
Discuss signs and symptoms of contamination.
Explain decontamination protocols.
Explain need for isolation procedures.
Well-managed efforts at communication of contamination information ensure that messages are correctly
formulated, transmitted, and received and that they result in meaningful actions (ATSDR, 2006).
Emphasize the importance of pre- and postexposure treatment of contamination. Early treatment will
decrease associated complications related to contamination (ATSDR, 2010).
REFERENCES
Agency for Toxic Substances and Disease Registry (ATSDR): A primer Environmental Protection Agency (EPA): Fact sheet: Water works:
on health risk communication: principles and practices. Overview of information for older adults and family caregivers (publication no.
issues and guiding principles, 2006. Retrieved April 1, 2009, from EPA-100-F-09044), 2009.
http://www.atsdr.cdc.gov/risk/-riskprimer/vision.html. Gershon R, et al: Home health care patients and safety hazards in the
Agency for Toxic Substances and Disease Registry (ATSDR): Medical home: preliminary ndings, Rockville, MD, 2008, Agency for Health-
management guideline for parathion, 2010. Retrieved August 2, 2011, care Research and Quality (AHRQ).
from http://www.atsdr.cdc.gov/MMG/MMG.asp?id=1140&tid=246. Holmes SM: An ethnographic study of the social context of migrant
Boscarino J, et al: Fear of terrorism and preparedness in New York health in the United States, PLoS Med 3(10):e448, 2006.
City 2 years after the attacks: implications for disaster planning and Lee BY, et al: The timing of inuenza vaccination for older adults
research, J Public Health Manag Pract 12(6):505513, 2006. (65 years and older), Vaccine 27(50):71107115, 2009.
Caplan G: Principles of preventive psychiatry, New York, 1964, Basic Books. Lin CG, et al: Pediatric lead exposure from imported Indian spices and
Carter-Pokras O, et al: The environmental health of Latino children, cultural powders, Pediatrics 125(4):e828e835, 2010.
J Pediatr Healthc 21(5):307314, 2007. Murdoch S, Cymet TC: Treating victims after disaster: physical and
Centers for Disease Control and Prevention (CDC): Emergency pre- psychological effects, Compr Ther 32(1):3942, 2006.
paredness & response, 2009. Retrieved March 19, 2009, from http:// U.S. Army Medical Research Institute of Infectious Diseases: USAM-
www.bt.cdc.gov. RIIDs medical management of biological casualties handbook, ed 6,
Childrens Environmental Health Network: Resource guide on childrens Fort Detrick, MD, 2005, Author.
environmental health, 2006, Retrieved March 19, 2009, from Veenema TG: Disaster nursing and emergency preparedness for chemical,
http://www.cehn.org/cehn/-resourceguide/rgtoc.html. biological and radiological terrorism and other hazards, ed 2, New
Drayna P, et al: Association between rainfall and pediatric emergency York, 2007, Springer.
department visits for acute gastrointestinal illness, Environ Health
Perspect 118:14391443, 2010.
Risk for Contamination Laura V. Polk, PhD, RN, and Pauline M. Green, PhD, RN, CNE
NANDA-I
Definition
Accentuated risk of exposure to environmental contaminants in doses sufcient to cause adverse health
effects
Risk Factors
See Related Factors in Contamination care plan.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Risk for contamination 253
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Risk Control, Health Beliefs: Perceived Threat, Knowledge: Health Resources, Knowledge: Health Behavior,
Community Disaster Readiness, Community Health Status. See Contamination for other possible NOC
outcomes.
C
Example NOC Outcome with Indicators
Risk Control as evidenced by the following indicators: Monitors environmental risk factors/Avoids exposure to health threats/Fol-
lows selected risk control strategies. (Rate the outcome and indicators of Risk Control: 1 = never demonstrated, 2 = rarely
demonstrated, 3 = sometimes demonstrated, 4 = often demonstrated, 5 = consistently demonstrated [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Remain free of adverse effects of contamination
Community Will (Specify Time Frame):
Utilize health surveillance data system to monitor for contamination incidents
Participate in mass casualty and disaster readiness drills
Remain free of contamination-related health effects
Minimize exposure to contaminants
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Environmental Risk Protection, Bioterrorism Preparedness, Environmental Management: Safety, Health
Education, Health Screening, Immunization/Vaccination Management, Risk Identication, Surveillance:
Safety, Community, Communicable Disease Management, Community Disaster Preparedness, Health Pol-
icy Monitoring
Example NIC ActivitiesEnvironmental Risk Protection
Assess environment for potential and actual risk; Monitor incidents of illness and injury related to environmental hazards
Nursing Interventions and Rationales
Conduct surveillance for environmental contamination. Notify agencies authorized to protect the envi-
ronment of contaminants in the area. Early surveillance and detection are critical components of preparation
(Murdoch & Cymet, 2006; Veenema, 2007)
Assist individuals to modify the environment to minimize risk or assist in relocating to safer environment.
Modication of the environment will decrease the risk of actual contamination occurring (Veenema & Toke,
2006).
Schedule mass casualty and disaster readiness drills. Practice in handling contamination occurrences will
decrease the risk of exposure during actual contamination events (Chung & Shannon, 2005).
Provide accurate information on risks involved, preventive measures, use of antibiotics, and vaccines.
Well-managed efforts at communication of contamination information ensure that messages are correctly
formulated, transmitted, and received, and that they result in meaningful actions (ATSDR, 2006).
Assist to deal with feelings of fear and vulnerability. EB: Interventions aimed at supporting an individuals
coping help the person deal with feelings of fear, helplessness, and loss of control that are normal reactions in a
crisis situation (Boscarino et al, 2006).
For more interventions including Pediatric, Geriatric, Multicultural, and Home Care, see the Contamina-
tion care plan.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
254 Risk for adverse reaction to iodinated contrast media
REFERENCES
Agency for Toxic Substances and Disease Registry (ATSDR): Medical Murdoch S, Cymet TC: Treating victims after disaster: physical and
management guideline for parathion, 2012. Retrieved August 2, 2011, psychological effects, Compr Ther 32(1):3942, 2006.
from http://www.atsdr.cdc.gov/MMG/MMG.asp?id=1140&tid=246. Veenema TG: Disaster nursing and emergency preparedness for chemical,
Boscarino J, et al: Fear of terrorism and preparedness in New York biological and radiological terrorism and other hazards, ed 2, New
C City 2 years after the attacks: implications for disaster planning and
research, J Public Health Manag Pract 12(6):505513, 2006.
York, 2007, Springer.
Veenema T, Toke J: Early detection and surveillance for bioprepared-
Chung S, Shannon M: Hospital planning for acts of terrorism and ness and emerging infectious diseases, Online J Issues Nurs 11(1):3,
other public health emergencies involving children, Arch Dis Child 2006.
90(12):13001307, 2005.
Risk for adverse reaction to iodinated Contrast media
Betty Ackley, MSN, EdS, RN
NANDA-I
Definition
At risk for any noxious or unintended reaction associated with the use of iodinated contrast media that can
occur within 7 days after contrast agent injection
Risk Factors
Anxiety; concurrent use of medications (e.g., beta-blockers, interleukin-2, metformin, nephrotoxic medica-
tions); dehydration; extremes of age; fragile veins (e.g., prior or actual chemotherapy treatment or radiation
in the limb to be injected, multiple attempts to obtain intravenous access, indwelling intravenous lines in
place for more than 24 hours, previous axillary lymph node dissection in the limb to be injected, distal intra-
venous access sites: hand, wrist, foot, ankle); generalized debilitation; history of allergies; history of previous
adverse effect from iodinated contrast media; physical and chemical properties of the contrast media (e.g.,
iodine concentration, viscosity, high osmolality, ion toxicity); unconsciousness; underlying disease (e.g.,
heart disease, pulmonary disease, blood dyscrasias, endocrine disease, renal disease, pheochromocytoma,
autoimmune disease)
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Tissue Perfusion: Renal, Kidney Function
Example NOC Outcome with Indicators
Kidney Function as evidenced by: 24-hour intake and output balance/Blood urea nitrogen/Serum creatinine/Urine color/Serum
electrolytes. (Rate the outcome and indicators of Kidney Function: 1 = severely compromised, 2 = substantially compro-
mised, 3 = moderately compromised, 4 = mildly compromised, 5 = not compromised [see section I].)
Client Outcomes
Client Will (Specify Time Frame):
Maintain normal blood urea nitrogen and serum creatinine levels
Maintain urine output of 0.5 mL/kg/hr
Maintain serum electrolytes (K+, PO4, Na+) within normal limits
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Fluid/Electrolyte Management, Laboratory Data Interpretation
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Risk for adverse reaction to iodinated contrast media 255
Example NIC ActivitiesFluid/Electrolyte Management
Monitor for serum electrolytes levels, as available; Weigh daily and monitor trends; Monitor vital signs, as appropriate. Recognize that
iodinated contrast media can be harmful to clients in a number of ways including onset of contrast-induced nephropathy, allergic
reactions to the dye, and damage to veins and vascular access devices.
C
Nursing Interventions and Rationales
Contrast-Induced Nephropathy (CIN)
Protect clients from contrast mediainduced nephropathy by taking the following actions:
Watching for closely spaced studies using contrast media and consulting with provider for change in
scheduling of studies if needed (Cheung, Ponnusamy & Anderton, 2008). Multiple administration of con-
trast within 72 hours is considered a risk factor for CIN (ODonovan, 2010).
Notifying the provider and the radiology staff if the client has preexisting renal disease. Clients with
preexisting impaired renal function are prone to develop acute contrast media induced nephropathy (CIN)
(Schilcher et al, 2011; Wong et al, 2011).
Ensuring that clients having diagnostic testing with contrast are well hydrated with IV saline as ordered
before and after the examination. EB: Hydration with crystalloids has been shown to prevent renal insuf-
ciency by diluting the IV contrast. Fluids without salt have been shown to increase acute kidney injury
(Rudnick, Goldfarb, & Tumlin, 2008).
Recognize that many clients with decreased renal function are not aware of their health status, and that
a questionnaire checklist administered before testing may not be satisfactory to nd clients with
impaired renal function that should receive contrast media carefully or who are not a candidate for test-
ing utilizing contrast media because of possible increased renal dysfunction. EB: A study found that use
of a pre-procedure checklist was not effective in identifying all the clients with a history of chronic kidney
disease to protect them from further kidney damage; instead point-of-care creatine testing was recommended
(Kalisz et al, 2011).
Recognizing that cancer clients are often very vulnerable to contrast induced nephropathy due to fre-
quent imaging examinations. Cancer clients have frequent examinations requiring contrast for tumor stag-
ing and assessment of treatment response. In addition the risk is compounded by advancing age,
co-administration of nephrotoxic chemotherapy drugs, and dehydration from gastrointestinal complications
from drugs and radiation (Heiken, 2008).
Monitor the client carefully for symptoms of hypovolemia following use of contrast media including
intake and output, blood pressure measurements, and new onset of postural hypotension with dizziness.
Hypovolemia can happen following contrast media administration due to the increased osmolarity of the
contrast media, resulting in postprocedure diuresis (ODonovan, 2011).
Monitor the client carefully for symptoms of acute failure following use of contrast media including
decreased or normal urinary output, and increased creatinine levels. Contrast media is thought to be
harmful to the kidneys in several ways, through being cytotoxic to the kidney itself, through ischemia of
the kidneys, and renal cell necrosis. Damage to the kidney results in acute renal failure (ODonovan,
2010). See Risk for ineffective Renal Perfusion if CIN is present for further interventions regarding
kidney function.
Allergic Reaction to Contrast Media
Recognize that both allergic and anaphylactoid reactions can occur. Anaphylaxis occurs rapidly, often
within 20 minutes of injection, versus a less serious anaphylactoid reaction, which can occur later after an
hour. Hypersensitivity reactions can be divided into immediate occurring less than 1 hour of administration
and less immediate occurring more than 1 hour after injection (Brockow & Ring, 2010).
Watch carefully for symptoms of a reaction, which can be either mild, moderate, or severe. Report all
symptoms to primary care physician because symptoms can advance from mild to severe rapidly.
Mild Reactions: Urticaria, pruritus, rhinorrhea, nausea, emesis, diaphoresis, coughing, dizziness
Moderate Reactions: Persistent emesis, widespread urticaria, headache, edema of the face, laryngeal
edema, mild dyspnea, palpitations, tachycardia/bradycardia, hypertension, abdominal cramps
Severe Reactions: Severe bronchospasm, severe arrhythmias, severe hypotension, pulmonary edema,
laryngeal edema, seizures, syncope, death (Wilson, 2011)
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
256 Readiness for enhanced community coping
Vein Damage and Damage to Vascular Access Devices
After diagnostic testing using contrast media given IV, inspect the IV site used for administration for pos-
sible problems such as extravasation, or development of compartment syndrome with excessive amounts
of contrast pushed into the tissues under pressure. The incidence of serious complications associated with the
C media has increased since advent of use of power or pressure mechanical injectors. Unfortunately compartment
syndrome though rare can result in infection, loss of use of the affected extremity, necrosis, skin sloughing,
amputation, need for skin grafting, paralysis, and death (Wilson, 2011).
Recognize that a vascular access device utilized for administration of contrast media can rupture
from the high pressures utilized to administer the contrast media. The Food and Drug Administration
(FDA) has received more than 250 adverse event reports in which vascular access devices have ruptured
when used with power injectors. The adverse events include rupture and device fragmentation (Earhart &
McMahon, 2011).
Geriatric
Screen the elderly client thoroughly before diagnostic testing utilizing contrast media. The elderly are more
likely to have pre-existing renal failure, along with other comorbidities and are more vulnerable to develop
renal damage (Cheung et al, 2008; ODonovan, 2011).
REFERENCES
Brockow K, Ring J: Anaphylaxis to radiographic contrast media, Curr ODonovan K: Preventing contrast-induced nephropathy part 2: pre-
Opin Allergy Clin Immunol 11(4):326331, 2010. ventive strategies, BJCN 6(1):610, 2011.
Cheung C, Ponnusamy A, Anderton J: Management of acute renal Rudnick MR, Goldfarb S, Tumlin J: Contrast induced nephropathy: is
failure in the elderly patient, Drugs Aging 25(6):455476, 2008. the picture any clearer? Clin J Am Soc Nephrol 3(1):261262, 2008.
Earhart A, McMahon P: Vascular access and contrast media, J Infusion Schilcher G, et al: Early detection and intervention using neutrophil
Nurs 34(2):97105, 2011. gelatinase-associated lipocalin (NGAL) may improve renal outcome
Heiken JP: Contrast safety in the cancer patient: preventing contrast- of acute contrast media induced nephropathy: a randomized
induced nephropathy, Cancer Imaging 8(Suppl A):S124S127, 2008. controlled trial in patients undergoing intra-arterial angiography
Kalisz KR, et al: Detection of renal dysfunction by point-of-care creati- (ANTI-CIN Study), BMC Nephrol 17:1239, 2011.
nine testing in patients undergoing peripheral MR angiography, AJR Wilson B: Contrast media-induced compartment syndrome, Radiol
197(2):430435, 2011. Technol 83(1):6377, 2011.
ODonovan K: Preventing contrast-induced nephropathy part 1: what is Wong PC, et al: Pathophysiology of contrast-induced nephropathy, Int J
CIN? BJCN 5(12):576581, 2010. Cardiol 158(2):186192, 2011.
Readiness for enhanced community Coping Dawn Fairlie, ANP, FNP, GNP, DNS(c)
NANDA-I
Definition
Pattern of community activities for adaptation and problem solving that is satisfactory for meeting the
demands or needs of the community but that can be improved for management of current and future
problems/stressors
Defining Characteristics
One or more characteristics that indicate effective coping:
Active planning by community for predicted stressors; active problem solving by community when faced
with issues; agreement that community is responsible for stress management; positive communication
among community members; positive communication between community/aggregates and larger commu-
nity; programs available for recreation; programs available for relaxation; resources sufcient for managing
stressors
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Community Competence, Community Health Status
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Readiness for enhanced community coping 257
Example NOC Outcome with Indicators
Community Health Status as evidenced by the following indicators: Prevalence of health promotion programs/Health
status of infants, children, adolescents, adults, elders/Participation rates in community health programs. (Rate the outcome and
indicators of Community Health Status: 1 = poor, 2 = fair, 3 = good, 4 = very good, 5 = excellent [see Section I].)
C
Community Outcomes
Community Will (Specify Time Frame):
Develop enhanced coping strategies
Maintain effective coping strategies for management of stress
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Environmental Management: Community, Health Policy Monitoring: Program Development
Example NIC ActivitiesProgram Development
Assist the group or community in identifying significant health needs or problems; Identify alternative approaches to address the
need(s) or problem(s)
Nursing Interventions and Rationales
Note: Interventions depend on the specic aspects of community coping that can be enhanced (e.g., planning
for stress management, communication, development of community power, community perceptions of stress,
community coping strategies). Nursing interventions are conducted in collaboration with key members of the
community, community/public health nurses, and members of other disciplines (Anderson & McFarlane, 2011).
Describe the roles of community/public health nurses in working with healthy communities. EBN: Nurses
at general and specialists levels (bachelors and masters degrees) have signicant roles in helping communities
to achieve optimum health, including coping with stress (Chinn, 2012; Stanhope & Lancaster, 2009).
Help the community to obtain funds for additional programs. EBN: Healthy communities may need
additional funding sources to strengthen community resources (Anderson & McFarlane, 2011; Chinn, 2012).
Encourage positive attitudes toward the community through the media and other sources. EB: Negative
attitudes or stigmas create additional stress and decits in social support (Anderson & McFarlane, 2011;
Chinn, 2012; Stanhope & Lancaster, 2009).
Help community members to collaborate with one another for power enhancement and coping skills.
EBN: Community members may not have sufcient skills to collaborate for enhanced coping. Health care
providers can promote effective collaboration skills (Anderson & McFarlane, 2011; Chinn, 2012).
Assist community members with cognitive skills and habits of mind for problem solving. EBN: The cog-
nitive skills and habits of mind of critical thinking support problem-solving ability (Rubenfeld & Scheffer,
2010).
Demonstrate optimum use of power resources. EBN: Optimum use of power resources and working for
community empowerment supports coping (Chinn, 2012).
Reduce poverty whenever possible. EB: Poverty is a major determinant of poor health, and people living on
low income consistently have higher rates of morbidity and mortality due to chronic and acute illness. There-
fore, primary health care providers should consider and address income as a distinct risk to health, and
researchers should explore these issues with a broader group of primary care providers and people who live in
poverty (Bloch, Rozmovits, & Giambrone, 2011).
Collaborate with community members to improve educational levels within the community. EB: Patient
safety, self-care behaviors, adherence to treatment plans, knowledge of ones medical condition, health care
quality, and positive health outcomes are compromised by low health literacy. There is also compromised physi-
cal and mental health, as well as greater risk of hospitalization, and increased mortality (Evangelista et al, 2010).
Multicultural
Refer to care plan Ineffective community Coping.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
258 Defensive coping
Client/family Teaching and Discharge Planning
Review coping skills, power for coping, and the use of power resources.
C REFERENCES
Refer to Ineffective community Coping for additional references.
Bloch G, Rozmovits L, Giambrone B: Barriers to primary care respon- Rubenfeld MG, Scheffer BK: Critical thinking tactics for nurses: achieving
siveness to poverty as a risk factor for health, BMC Fam Pract 12:62, IOM competencies, ed 2, Boston, 2010, Jones and Bartlett.
2011. Stanhope M, Lancaster J: Foundations of nursing in the community:
Evangelista LS, et al: Health literacy and the patient with heart failure community-oriented approach, ed 3, St Louis, 2009, Mosby.
implications for patient care and research: a consensus statement of
the Heart Failure Society of America, J Card Fail 16(1):916, 2010.
Defensive Coping Patricia Ferreira, RN, MSN, Michelangelo Juvenak, Biologist/Immunologist, MSc, Phd,
and Gail B. Ladwig, MSN, RN
NANDA-I
Definition
Repeated projection of falsely positive self-evaluation based on a self-protective pattern that defends against
underlying perceived threats to positive self-regard
Defining Characteristics
Denial of obvious problems; denial of obvious weaknesses; difculty establishing relationships; difculty in
perception of reality testing; difculty maintaining relationships; grandiosity; hostile laughter; hypersensitivity
to criticism; hypersensitivity to slight; lack of follow-through in therapy; lack of follow-through in treatment;
lack of participation in therapy; lack of participation in treatment; projection of blame; projection of respon-
sibility; rationalization of failures; reality distortion; ridicule of others; superior attitude toward others
Related Factors (r/t)
Conict between self-perception and value system; decient support system; fear of failure; fear of humilia-
tion; fear of repercussions; lack of resilience; low level of condence in others; low level of self-condence;
uncertainty; unrealistic expectations of self
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Coping, Decision Making, Impulse Self-Control, Information Processing
Example NOC Outcome with Indicators
Coping as evidenced by the following indicators: Identifies effective and ineffective coping patterns/Modifies lifestyle to reduce
stress. (Rate the outcome and indicators of Coping: 1 = never demonstrated, 2 = rarely demonstrated, 3 = sometimes
demonstrated, 4 = often demonstrated, 5 = consistently demonstrated [see Section I].)
Client Outcomes
Client Will (Specify Time Frame):
Acknowledge need for change in coping style
Accept responsibility for own behavior
Establish realistic goals with validation from caregivers
Solicit caregiver validation in decision-making
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Defensive coping 259
NIC (Nursing Interventions Classification)
Suggested Nursing Interventions
Body Image Enhancement, Complex Relationship Building, Coping Enhancement, Patient Contracting,
Self-Awareness Enhancement, Self-Esteem Enhancement, Socialization Enhancement, Surveillance C
Example NIC ActivitiesSelf-Awareness Enhancement
Encourage patient to recognize and discuss thoughts and feelings; Assist patient in identifying behaviors that are self-destructive
Nursing Interventions and Rationales
Assess for possible symptoms associated with defensive coping: depressive symptoms, excessive self-
focused attention, negativism and anxiety, hypertension, post-traumatic stress disorder (PTSD) (e.g.,
exposure to terrorism), unjust world beliefs. Depression is often associated with use of defensive coping
(Hobfoll, Canetti-Nisim, & Johnson, 2006). CEB: The heightened self-focused attention might result from auto-
matically instigated states of self-focused attention and paradoxical effects of defensive efforts to avoid self-
focus. This study demonstrated, in group comparisons, that negative affect group obtained higher scores on the
Self-reectiveness scale than the control group (p < 0.03) (Hping, de Jong-Meyer, & Abrams, 2006).
Repressive (or defensive) coping has been associated with elevated blood pressure levels, essential hypertension,
and paroxysmal hypertension. Cardiovascular clients who use a repressive style have shown mixed results dur-
ing recuperation (Gleiberman, 2007). In this study, authors related that exposure to terrorism was signi-
cantly related to greater loss and gain of psychosocial resources and to greater posttraumatic stress disorder
(PTSD) and depressive symptoms (Hobfoll, Canetti-Nisim, & Johnson, 2006). In two studies, the Unjust
World Views Scale (UJWVS) was developed. Belief in an unjust world was related to defensive coping, anger,
and perceived future risk. These ndings contribute to theory development and suggest that a belief in an
unjust world may serve a self-protective function. Clinical implications are discussed as unjust world views also
were found to be potentially maladaptive (Lench & Chang, 2007).
Stimulate cognitive behavioral stress management (CBSM). CEB: Although denial may be an effective means
of distress reduction in the short term, reliance on this coping strategy may result in a decreased capacity to
effectively manage a variety of disease-related stressors in the long term. CBSM addresses this potentially det-
rimental pattern by teaching stress reduction skills that may decrease depressed mood via reduced reliance on
denial coping (Carrico et al, 2006).
Ask appropriate questions to assess whether denial (defensive coping) is being used in association with
alcoholism. CEB: Alcohol abuse is a major problem in the United States, but individuals are not getting treat-
ment. In this survey, denial or refusal to admit severity and fear of social embarrassment were the top two
reasons for not seeking help (To & Vega, 2006).
Promote interventions with multisensory stimulation environments. EB: Multisensory stimulation envi-
ronments (MSEs) are a popular space for intervention in the numerous forms of disability, with occupational,
therapeutic, or educational objectives (Castelhano & Roque, 2009).
Empower the client/caregivers self-knowledge. EB: Theory of therapist resilience: the theory that was constructed
included a central category (Integration of Self with Practice), a paradigm (Trust in Self), and two main categories
(Career Development and Practice of Therapy). The process involved an initial calling, a positive agency experi-
ence, career corrections, the inuence of relationships, and a move to a more exible environment (Clark, 2009).
Geriatric
Identify problems with alcohol in the elderly with the appropriate tools and make suitable referrals. Tools
such as the Alcohol Use Disorders Identication Test (AUDIT), Michigan Alcohol Screening Test-Geriatric
Version (MAST-G), and the Alcohol-Related Problems Survey (ARPS) may have additional use in this popu-
lation. Brief interventions have been shown to be effective in producing sustained abstinence or reducing levels
of consumption, thereby decreasing hazardous and harmful drinking (Culberson, 2006).
Encourage exercise for positive coping. CEB: After a 10-week period, the elderly participants in this exercise
group reported signicant improvements in stress, mood, and several quality-of-life indices (Starkweather,
2007).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
260 Defensive coping
Stimulate individual reminiscence therapy. EB: After eight sessions, an elderly woman had a happier expres-
sion on her face, was willing to express herself more verbally, had more interaction with others, and required
medication less frequently to help her sleep (Chou, Lan, & Chao, 2008).
Stimulate group reminiscence therapy. CEB: Participation in reminiscence activities can be a positive and
valuable experience for demented older persons. Consequently, the development of a structured care program
C for elderly persons with cognitive impairment and the need for long-term care is essential. Thus, health provid-
ers in long-term care facilities should be trained in reminiscence group therapy and to be able to deliver such a
program to the targeted group (Wang, 2007).
Multicultural
Acknowledge racial/ethnic differences at the onset of care. CEB: Acknowledgment of race/ethnicity issues
will enhance communication, establish rapport, and promote treatment outcomes (DAvanzo et al, 2001).
African American parents who denied experiences of racism reported higher rates of behavior problems in their
children, in contrast to African American parents who actively coped with racism and reported lower levels of
behavior problems in their children (Caughy, OCampo, & Muntaner, 2004).
Assess an individuals sociocultural backgrounds in teaching self-management and self-regulation as a
means of supporting hope and coping with a diagnosis of type 2 diabetes. EBN: Findings obtained from the
themes of this study illustrated that self-management of clients with diabetes is highly related to their own
sociocultural environment and experiences (Lin et al, 2008).
Encourage the client to use spiritual coping mechanisms such as faith and prayer. CEB & EBN: Prayer is a
powerful way of coping and is practiced by all Western religions and several Eastern traditions (Mohr, 2006).
Spirituality inspired hope among caregivers of stroke clients (Pierce et al, 2008). This study indicates that black
American young adult college students may utilize religious coping methods for psychological stress (Kohn-
Wood et al, 2012)
Encourage spirituality as a source of support for coping. EB: The association among spirituality/religiosity,
positive appraisals, and internal adaptive coping strategies indicates that the utilization of spirituality/religios-
ity goes far beyond fatalistic acceptance, but can be regarded as an active coping process (Bssing et al, 2009).
Home Care
Refer the client for a behavioral program that teaches coping skills via Lifeskills workshop and/or video.
CEB: Commercially available, facilitator- or self-administered behavioral training products can have signi-
cant benecial effects on psychosocial well-being in a healthy community sample (Kirby et al, 2006).
Client/Family Teaching and Discharge Planning
Teach coping skills to family caregivers of cancer clients. CEB: A coping skills intervention was effective in
improving caregiver quality of life, reducing burden related to clients symptoms, and caregiving tasks com-
pared with hospice care alone or hospice plus emotional support (McMillan et al, 2006).
Teach caregivers the COPE intervention (creativity, optimism, planning, expert information) to assist
with symptom management. CEB: Symptom distress, a measure that encompasses client suffering along with
intensity, was signicantly decreased in the group in which caregivers were trained to better manage client
symptoms (McMillan & Small, 2007).
Family-based intervention may prevent anxiety disorders in the offspring of parents with anxiety disorders.
EB: Parental satisfaction with the intervention was high. Findings suggest that a family-based intervention may
prevent the onset of anxiety disorders in the offspring of parents with anxiety disorders (Ginsburg, 2009).
REFERENCES
Refer to Ineffective Coping for additional references.
Bssing A, et al: Are spirituality and religiosity resources for patients Caughy MO, OCampo PJ, Muntaner C: Experiences of racism
with chronic pain conditions? Pain Med 10(2):327339, 2009. among African American parents and the mental health of their
Carrico AW, et al: Reductions in depressed mood and denial coping preschool-aged children, Am J Public Health 94(12):21182124,
during cognitive behavioral stress management with HIV-positive 2004.
gay men treated with HAART, Ann Behav Med 31(2):155164, 2006. Chou YC, Lan YH, Chao SY: Application of individual reminiscence
Castelhano, N, Roque L: The integration of the Computer-mediated Ludic therapy to decrease anxiety in an elderly woman with dementia,
Experience in Multisensory Environments, in Proc. of the DiGRA Hu Li Za Zhi 55(4):105110, 2008.
(Digital Conference on Information Systems) 2009-Breaking New Clark P: Resiliency in the practicing marriage and family therapist,
Ground: Innovation in Games, Play, Practice and Theory, Newport, J Marital Fam Ther 35(2):231247, 2009.
UK, September 2009
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Ineffective coping 261
Culberson JW: Alcohol use in the elderly: beyond the CAGE. Part 2: Lench HC, Chang ES: Belief in an unjust world: when beliefs in a just
Screening instruments and treatment strategies, Geriatrics world fail, J Pers Assess 89(2):126135, 2007.
61(11):2026, 2006. Lin CC, et al: Diabetes self-management experience: a focus group study
DAvanzo CE, et al: Developing culturally informed strategies for of Taiwanese patients with type 2 diabetes, J Clin Nurs 17(5a):3442,
substance-related interventions. In Naegle MA, DAvanzo CE, edi- 2008.
tors: Addictions and substance abuse: strategies for advanced practice McMillan SC, et al: Impact of coping skills intervention with family
nursing, St Louis, 2001, Mosby.
Ginsburg GS: The Child Anxiety Prevention Study: intervention model
caregivers of hospice patients with cancer: a randomized clinical
trial, Cancer 106(1):214222, 2006.
C
and primary outcomes, J Consult Clin Psychol 77(3):580587, 2009. McMillan SC, Small BJ: Using the COPE intervention for family care-
Gleiberman L: Repressive/defensive coping, blood pressure, and cardio- givers to improve symptoms of hospice homecare patients: a clinical
vascular rehabilitation, Curr Hypertens Rep 9(1):712, 2007. trial, Oncol Nurs Forum 34(2):313321, 2007.
Hobfoll SE, Canetti-Nisim D, Johnson RJ: Exposure to terrorism, stress- Mohr WK: Spiritual issues in psychiatric care, Perspect Psychiatr Care
related mental health symptoms, and defensive coping among Jews 42(3):174183, 2006.
and Arabs in Israel, J Consult Clin Psychol 74(2):207218, 2006. Pierce LL, et al: Spirituality expressed by caregivers of stroke survivors,
Hping W, de Jong-Meyer R, Abrams D: Excessive self-focused atten- West J Nurs Res 30(5):606619, 2008.
tion and defensiveness among psychiatric patients: a vicious cycle? Starkweather AR: The effects of exercise on perceived stress and IL-6
Psychol Rep 98(2):307317, 2006. levels among older adults, Biol Res Nurs 8(3):186194, 2007.
Kirby ED, et al: Psychosocial benets of three formats of a standardized To SE, Vega CP: Alcoholism and pathways to recovery: new survey
behavioral stress management program, Psychosom Med 68(6): results on views and treatment options, MedGenMed 8(1):2, 2006.
816823, 2006. Wang JJ: Group reminiscence therapy for cognitive and affective
Kohn-Wood L, et al: Coping styles, depressive symptoms and race dur- function of demented elderly in Taiwan, Int J Geriatr Psychiatry
ing the transition to adulthood, Ment Health Relig Cult 15(4): 22(12):12351240, 2007.
363372, 2012.
Ineffective Coping Arlene T. Farren, RN, PhD, AOCN, CTN-A
NANDA-I
Definition
Inability to form a valid appraisal of the stressors, inadequate choices of practiced responses, and/or inability
to use available resources
Defining Characteristics
Change in usual communication patterns; decreased use of social support; destructive behavior toward
others; destructive behavior toward self; difculty organizing information; fatigue; high illness rate; inability
to attend to information; inability to meet basic needs; inability to meet role expectations; inadequate
problem solving; lack of goal-directed behavior; lack of resolution of problem; poor concentration; reports
inability to ask for help; reports inability to cope; risk taking; sleep pattern disturbance; substance abuse; use
of forms of coping that impede adaptive behavior
Related Factors (r/t)
Disturbance in pattern of appraisal of threat; disturbance in pattern of tension release; gender differences in
coping strategies; high degree of threat; inability to conserve adaptive energies; inadequate level of condence
in ability to cope; inadequate level of perception of control; inadequate opportunity to prepare for stressor;
inadequate resources available; inadequate social support created by characteristics of relationships; matura-
tional crisis; situational crisis; uncertainty
NOC (Nursing Outcomes Classification)
Suggested NOC Outcomes
Coping, Decision-Making, Impulse Self-Control, Information Processing
Example NOC Outcome with Indicators
Coping as evidenced by the following indicators: Identifies effective and ineffective coping patterns/Modifies lifestyle to reduce
stress. (Rate the outcome and indicators of Coping: 1 = never demonstrated, 2 = rarely demonstrated, 3 = sometimes demon-
strated, 4 = often demonstrated, 5 = consistently demonstrated [see Section I].)
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
262 Ineffective coping
Client Outcomes
Client Will (Specify Time Frame):
Use effective coping strategies
Use behaviors to decrease stress
C Remain free of destructive behavior toward self or others
Report decrease in physical symptoms of stress
Report increase in psychological comfort
Seek help from a health care professional as appropriate
NIC (Nursing Interventions Classification)
Suggested NIC Interventions
Coping Enhancement, Decision-Making Support
Example NIC ActivitiesCoping Enhancement
Assist the patient in developing an objective appraisal of the event; Explore with the client previous methods of dealing with life
problems
Nursing Interventions and Rationales
Observe for contributing factors of ineffective coping such as poor self-concept, grief, lack of problem-
solving skills, lack of support, recent change in life situation, maturational or situational crises. EB: In a
large sample (n =758) of people living with HIV, the top three life stressors identied were taking on too many
things at once, not having enough money for what is needed, and having a scary experience in childhood that
one continues to think about (Gibson et al, 2011).
Use verbal and nonverbal therapeutic communication approaches including empathy, active listening,
and confrontation to encourage the client and family to express emotions such as sadness, guilt, and
anger (within appropriate limits); verbalize fears and concerns; and set goals. EBN: Clinicians commu-
nication skills contribute to the well-being of clients and minimize psychosocial problems (Duff et al, 2009).
EB: Solution-focused communication with clients helps to focus on goals and helps nd solutions (Ruddick,
2011).
Collaborate with the client to identify strengths such as the ability to relate the facts and to recognize the
source of stressors. EBN: Hart and Grindel (2010) examined coping and self-care behavior in individuals
with type 2 diabetes and found that coping efcacy was associated with self-care behaviors. The researchers
recommended that nurses collaborate with patients to identify successful coping strategies. EB: Ruddick
(2011) describes solution-focused communications as enhancing the identication of strengths and resources
for coping.
Encourage the client to describe previous stressors and the coping mechanisms used. EBN: A psychoedu-
cation intervention that included clients identication of symptoms, types of coping strategies used before and
after the event, and ways to select alternative strategies was accompanied by medication intervention for par-
ticipants with post-traumatic stress disorder (PTSD) and statistically signicantly improved PTSD and
depression were found (Oaz, Haitpoglu, & Ayan, 2008).
Be supportive of coping behaviors; allow the client time to relax. EBN: Solari-Twadell (2010) found a selec-
tion of nursing interventions used by parish nurses (n = 1,161) to provide coping assistance to women includ-
ing presence, touch, emotional support, and coping enhancement.
Provide opportunities for the client to discuss the meaning the situation might have for the client. EBN: Parish
nurses (n = 1,161) identied frequent use of values clarication, spiritual growth facilitation, and hope instil-
lation in their work with women (Solari-Twadell PA, 2010). In a systematic review examining the character-
istics of coping in adults with advanced cancer, seven factors were identied, which included creating meaning
(Thomsen, Rydahl-Hansen, & Wagner, 2010).
Assist the client to set realistic goals and identify personal skills and knowledge. EBN: Researchers found
that participants who were 4 months after myocardial infarction experiencing fatigue described fumbling cop-
ing strategies. The researchers concluded that nursing interventions to assist clients to identify and reduce
stressors and increase clients ability to cope with stressors would be useful (Alsen, Brink, & Persson, 2008). EB:
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Ineffective coping 263
In one correlational study, adjusting goals was found to be an effective coping strategy in childless people
(Kraaij, Garnefski, & Schroevers, 2009).
Provide information regarding care before care is given. EBN: One systematic review examining coping
interventions for parents included the importance of informing parents of what to expect in their children and
in relation to their own responses (Peek & Melnyk, 2010). EB: In a clinical trial of families responsible for tak-
ing care of a relative with mental illness, a family-led education intervention resulted in signicant differences
C
in coping and decreased information needs between the intervention and control group (Pickett-Schenk et al,
2008).
Discuss changes with the client before making them. EBN: When dealing with adults with cancer, the
authors assert the importance of informing patients of treatment related symptoms and toxicities to help
patients prepare for the treatment course; furthermore, nurses should discuss additional coping strategies to
help with managing treatment-related problems (Boucher, Olson, & Piperdi, 2011).
Provide mental and physical activities within the clients ability (e.g., reading, television, radio, crafts, out-
ings, movies, dinners out, social gatherings, exercise, sports, games). EBN: In a pilot study of a nurse-based,
in-home transitional care intervention for seriously mentally ill persons, researchers found that one of the fac-
tors of importance to community transition was involvement in daily activities (Rose, Gerson, & Carbo, 2007).
Discuss the clients and familys power to change a situation or the need to accept a situation. EBN:
Researchers conducted a controlled trial of a nursing intervention to facilitate older adults (n = 89) access to
community resources to assist them to remain at home. Researchers found the older adults accepted the inter-
vention and had improved health empowerment, purposeful participation in goal attainment, and well-being
(Shearer, Fleury, & Belyea, 2010). EB: Acceptance of illness and acceptance through coping strategies have
been found to be associated with subjective health in a sample (n = 106) of cardiac patients (Karademas &
Hondronikola, 2010).
Offer instruction regarding alternative coping strategies. EBN: Mindfulness meditation intervention assisted
coping with unpleasant symptoms for hospitalized clients receiving hematopoietic stem cell transplantation
(Bauer-Wu, Sullivan, & Rosenbaum, 2008).
Encourage use of spiritual resources as desired. EBN: Spiritual activities such as prayer, meditation, and
doing good deeds played a major role in coping with living with HIV in a sample of Thai women practicing
Buddhism (Ross, Sawatphanit, & Suwansujarid, 2007). In a small qualitative study of Mexican American
cancer survivors (n = 5), three themes were uncovered, one of which was the use of spiritual resources to cope
with cancer (Campesino, 2009).
Encourage use of social support resources. EB: Authors of a systematic review of interventions for supporting
informal caregivers of terminal patients concluded the ndings suggest practitioners should consider that infor-
mal caregivers may need additional support (Candy et al, 2011). Low social support predicted maladaptive
coping in cancer survivors (Zucca et al, 2010).
Refer for additional or more intensive therapies as needed. EBN: More complex interventions are avail-
able to assist with coping, for example, a nurse-delivered intervention for depression in clients with cancer
(Forchuk, 2009). Victims of crime need the assistance of a multidisciplinary team to cope and achieve a posi-
tive recovery (Green, Choi, & Kane, 2010).
Pediatric
Monitor the clients risk of harming self or others and intervene appropriately. See care plan for Risk for
Suicide. CEB: Adolescents may use self-harming behaviors as a means of communication or way of coping
(Murray & Wright, 2006).
Support adolescent and childrens individual coping styles. EBN: Researchers found that a connection to
school could be protective against ineffective coping patterns in a sample of 166 fourth graders (Rice et al,
2008). In a study of coping of 4- to 6-year-olds who were hospitalized, researchers concluded that it was essen-
tial to support childrens individual coping strategies with information, guidance, and participation in deci-
sions (Salmela, Salanter, & Aronen, 2010). EB: In one study of youth with type 1 diabetes, the following
coping skills were observed: Younger children used more coping that involved choosing an alternate activity,
helping others, and an emotional response (taking personal responsibility), whereas adolescents used more
coping that involved persistence, alternate thinking, and talking things over (taking personal responsibility)
(Hema, Roper, & Nehring, 2009).
Encourage moderate aerobic exercise (as appropriate). CEB: Exercise was found to decrease the likelihood of
depressive feelings when used as a positive coping strategy for school-age children with angry feelings (Goodwin, 2006).
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
264 Ineffective coping
Geriatric
Assess and report possible physiological alterations (e.g., sepsis, hypoglycemia, hypotension, infection,
changes in temperature, uid and electrolyte imbalances, and use of medications with known cognitive
and psychotropic side effects). EB: A reversible pathophysiological process may be causing symptoms (Roc-
C chiccioli & Sanford, 2009).
Screen for elder neglect or other forms of elder mistreatment. CEB & EB: Abuse of older people is a serious
and growing social problem (Wang, Tseng, & Chen, 2007). In one study of 86 persons with Alzheimers disease
and their caregivers, researchers found predictors of caregiver abuse behaviors included caregivers who were
male, had greater burden, and whose care recipient had greater irritability and cognitive impairment (with less
functional impairment)(Cooper et al, 2008).
Encourage the client to make choices (as appropriate) and participate in planning care and scheduled activi-
ties. CEB & EBN: Older persons with heart failure transitioning to home from the hospital made choices about
participation in the therapeutic regimen based on their individual goals for community living during a nursing
intervention study, which resulted in positive client outcomes and cost savings (McCauley, Bixby, & Naylor, 2006).
In a pilot study examining depression care preferences of older home care clients, researchers concluded client prefer-
ences during care planning may improve participation in geriatric depression care management (Fyffe et al, 2008).
Target selected coping mechanisms for older persons based on client features, use, and preferences. CEB:
Elders with arthritis reported cognitive efforts, diversional activities, and assertive actions were useful in deal-
ing with daily stress (Tak, 2006). EB: Data from 37 interviews in one study of African American older adults
with mild symptoms of depression revealed culturally based coping strategies, which included self-reliance
strategies, keeping depressive symptoms from family and friends, denial, use of less stigmatizing emotional
expressions, and prayer and relationship with God (Conner et al, 2010).
Increase and mobilize support available to older persons by encouraging a variety of mechanisms involv-
ing family, friends, peers, and health care providers. EBN: Researchers conducted a controlled trial of a
nursing intervention to facilitate older adults (n = 89) access to community resources to assist them to remain
at home. Researchers found the older adults accepted the intervention and had improved health empower-
ment, purposeful participation in goal attainment, and well-being (Shearer, Fleury, & Belyea, 2010).
Actively listen to complaints and concerns. EBN: One of the most frequently used strategies by nurses in
end-of-life care and communication was active and passive listening (Boyd et al, 2011).
Engage the client in reminiscence. EBN: In a review of the literature, one author found that while more
research is needed, reminiscence was a promising intervention for older adults and proposes a protocol for a
structured group reminiscence intervention (Stinson, 2009).
Multicultural
Assess for the inuence of cultural beliefs, norms, and values on the clients perceptions of effective cop-
ing. EBN: The representation of strength inuences African American womens conceptualization of depres-
sion and coping strategies (Porter & Pacquiao, 2011).
Assess the inuence of fatalism on the clients coping behavior. EB: While fatalism has been a culturally
associated concept, recent studies of Latinos experiencing post-traumatic symptoms and African American
women diagnosed with cancer have found no signicant ndings related to fatalism and traumatic symptoms
or fatalism and delay in seeking treatment for breast cancer (Gullatte et al, 2010). More research is needed.
Assess the inuence of cultural conicts that may affect coping abilities. EBN: In one ethnographic study,
the researcher concluded that in the United States, there are differences between nurses cultures and those of
Syrian Muslims and suggested that improved cultural knowledge can lessen cultural pain and conicts
(Wehbe-Alamah, 2011).
Assess for intergenerational family problems that can overwhelm coping abilities. EB: While generalization
is not possible, in one qualitative case study of intergenerational dynamics in a Euro-American family experi-
encing the suicide of a father and daughter, areas for assessment were illuminated and included the role of
ways of dealing with the initial death, presence of incarceration of family members, and the perceptions of
family survivors of suicide (Sandage, 2010).
Encourage spirituality as a source of support for coping. EBN: In a small qualitative study of Mexican
American cancer survivors (n = 5), three themes were uncovered, one of which was the use of spiritual resources
to cope with cancer (Campesino, 2009).
Negotiate with the client with regard to the aspects of coping behavior that will need to be modied. EBN:
The use of self-mutilation as a coping behavior or communication of strength has been found in many cultures.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Ineffective coping 265
One case study reports the care of a Pakistani woman who began self-cutting when she rst arrived in the
United States. The author identies the importance of open communication with individualized care, refer-
rals, and support for more effective coping patterns (Williams & Hamilton, 2009).
Encourage moderate aerobic exercise (as appropriate). CEB: In a group of African American elders with
chronic health conditions, exercise was used as a coping strategy for effectively managing chronic health condi-
tions (Loeb, 2006). C
Identify which family members the client can count on for support. EBN: In a study of sources of social
support for adults living with HIV (n = 150), researchers found that spouses, friends, siblings, and mothers
provided appraisal, belonging, and tangible support (Grant et al, 2009).
Support the inner resources that clients use for coping. EB: In a qualitative study of 23 Sudanese refugees,
participants used a number of coping strategies to deal with pre-immigration, transition, and post-immigration
difculties including reliance on religious beliefs, relying on inner resources, and focus on the future (Khawaja
et al, 2008).
Use an empowerment framework to redene coping strategies. EBN: In an intervention study of an
empowerment intervention in a group (n = 18) of Norwegian women undergoing or recovering from treat-
ment for breast cancer, researchers used empowerment strategies such as reection on strengths and resources
and afrmation of strengths and abilities contributing to the empowerment of the participants (Stang & Mit-
telmark, 2010). EB: In a qualitative study of deaf people in the United States, researchers found that many
participants self-identied as members of an ethno-linguistic minority. Both individual and community
empowerment strategies were uncovered in the Internet weblog format, such as the value of using American
Sign Language, use of humor, and advocating for social justice (Hamill & Stein, 2011).
Home Care
The interventions described previously may be adapted for home care use.
Assess for suicidal tendencies. Refer for mental health care immediately if indicated.
Identify an emergency plan should the client become suicidal. Ineffective coping can occur in a crisis situa-
tion and can lead to suicidal ideation if the client sees no hope for a solution. A suicidal client is not safe in the
home environment unless supported by professional help. Refer to the care plan for Risk for Suicide.
Observe the family for coping behavior patterns. Obtain family and client history as possible. CEB: Family
assessment is necessary to guide interventions and activate appropriate resources (Ellenwood & Jenkins, 2007).
Assess for effective symptoms after cerebrovascular accident (CVA) in the elderly, particularly emotional
lability and depression. Refer for evaluation and treatment as indicated. CEB: In a study of older persons
poststroke, researchers found a range of physical and psychological concerns, with some clients expressing fears
of getting worse while others expressed hope for recovery. In either case, nurses can assist with the needs and
promote the use of effective coping (Popovich, Fox, & Bandagi, 2007).
Encourage the client to use self-care management to increase the experience of personal control. Identify
with the client all available supports and sense of attachment to others. Refer to the care plan for
Powerlessness. EBN: In a study of coping strategies of Latino women spouses of stroke survivors, women
maintained a sense of spousal obligation to care and used emotion-focused coping to preserve their own
physical and psychological health (Arabit, 2008). In a qualitative study of African American women (n = 46)
with low incomes trying to lose weight, the women, who were generally had low weight loss self-efcacy, did not
set goals regarding weight loss and exercise, and did not have sufcient support from family and friends to
make the necessary changes (Mastin, Campo, & Askelson, 2012).
Refer the client and family to support groups. CEB: Predictors of participation in support groups by cancer
clients include trusted others views of support groups, support received from special others, and the persons
own beliefs about support groups (Grande, Myers, & Sutton, 2006).
If monitoring medication use, contract with the client or solicit assistance from a responsible caregiver.
Elders with arthritis identied taking medications as an assertive action coping strategy (Tak, 2006).
Institute case management for frail elderly clients to support continued independent living. EBN: Case
management provides home-based care of frail elderly using a process of assessment and medication review
leading to new diagnoses, coordination of care, and tailoring of services that match individual needs
(Elwyn et al, 2008).
If the client is homebound, refer for psychiatric home health care services for client reassurance and
implementation of a therapeutic regimen. CEB: Researchers found a therapeutic life review intervention
delivered by home care workers enhanced mood in women participants (Symes et al, 2007). CEB: An interven-
tion study of a peer-based and regular case management for community-dwelling adults with severe mental
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
266 Ineffective coping
illness demonstrated that improved positive regard at 6 months predicted and sustained treatment motivation
for psychiatric, alcohol, and drug use problems and attendance at Alcoholics and Narcotics Anonymous
meetings (Sells et al, 2006).
Client/Family Teaching and Discharge Planning
C Teach the client to problem solve. Have the client dene the problem and cause, and list the advantages
and disadvantages of the options. CEB: A systematic review regarding healthy coping in diabetes manage-
ment suggested there is evidence from well-controlled intervention studies about coping/problem solving inter-
ventions, which support their use (Fisher et al, 2007).
Provide the seriously ill client and his or her family with needed information regarding the condition and
treatment. CEB: Researchers concluded that seriously ill hospitalized clients have poor knowledge of CPR and
would benet from improved understanding of CPR and their role (clients and family) in the decision-making
process (Heyland et al, 2006).
Teach relaxation techniques. EBN: Mindfulness meditation (MBSR) was taught to community-dwelling
adults who found the intervention promoted health awareness, personal self-care, and overall well-being
(Matchim, Armer, & Stewart, 2008).
Work closely with the client to develop appropriate educational tools that address individualized needs.
EB: Researchers developed a purpose-based information assessment (PIA) tool to evaluate how effective the
information met the clients individual needs; ndings included estimates supporting the validity, reliability,
and sensitivity of the PIA. Researchers concluded that the PIA can be used to identify strengths and limitations
in meeting an individuals information needs (Feldman-Stewart, Brennestuhl, & Brundage, 2007).
Teach the client about available community resources (e.g., therapists, ministers, counselors, self-help groups).
EBN: Researchers concluded from a review of the literature regarding couples surviving prostate cancer that in
addition to meeting educational needs, nurses must assess for potential concerns and make recommendations and
referrals to assist couples with nding appropriate resources for coping with issues related to their relationship
(Galbraith, Fink, & Wilkins, 2011). EB: While research suggests that persons needing community services are inter-
ested in using them, not all who need services use them, due in part to the need for more information about resources,
how to use them more effectively, or availability of services (Janda et al, 2008).
REFERENCES
Alsen P, Brink E, Persson L: Living with incomprehensible fatigue after Ellenwood AE, Jenkins JE: Unbalancing the effects of chronic ill-
recent myocardial infarction, J Adv Nurs 64(5):459468, 2008. ness: non-traditional family therapy assessment and intervention
Arabit LD: Coping strategies of Latino women caring for a spouse approach, Am J Fam Ther 35(3):265277, 2007.
recovering from stroke: a grounded theory, J Theory Construct Elwyn G, et al: Case management by nurses in primary care: analysis of
12(2):4249, 2008. 73 success stories, Qual Prim Care 16(2):7582, 2008.
Bauer-Wu S, Sullivan AM, Rosenbaum E: Facing the challenges of Feldman-Stewart D, Brennestuhl S, Brundage MD: A purpose-based
hematopoietic stem cell transplantation with mindfulness medita- evaluation of information for patients: an approach to measuring
tion: a pilot study, Integr Cancer Ther 7(2):6269, 2008. effectiveness, Patient Educ Couns 65(3):311319, 2007.
Boucher J, Olson L, Piperdi B: Preemptive management of dermatologic Fisher EB, et al: Healthy coping, negative emotions, and diabetes man-
toxicities associated with epidermal growth factor receptor inhibi- agement: a systematic review, Diabetes Educ 33(6):10801103, 2007.
tors, Clin J Oncol Nurs 15(5):501508, 2011. Forchuk C: A nurse-delivered intervention was effective for depression
Boyd D, et al: Nurses perceptions and experiences with end-of-life in patients with cancer, Evid Based Nurs 12(1):17, 2009.
communication and care, Oncol Nurs Forum 38(3):E229E239, Fyffe DC, et al: Older home care patients preferred approaches to
2011. depression care: a pilot study, J Gerontol Nurs 34(8):1722, 2008.
Campesino M: Exploring perceptions of cancer care delivery among Galbraith ME, Fink R, Wilkins GG: Couples surviving prostate cancer:
older Mexican American adults, Oncol Nurs Forum 36(4):413420, challenges in their lives and relationships, Semin Oncol Nurs
2009. 27(4):300308, 2011.
Candy B, et al: Interventions for supporting informal caregivers of Gibson K, et al: Mastery and coping moderate the negative effect of
patients in the terminal phase of a disease, Cochrane Database Syst acute and chronic stressors on mental health-related quality of life
Rev(6), CD007617:2011. in HIV, AIDS Patient Care STDs 25(6):371381, 2011.
Conner KO, et al: Barriers to treatment and culturally endorsed coping Goodwin RD: Association between coping with anger and feelings of
strategies among depressed African American older adults, Aging depression among youths, AM J Publ Health 96(4):664669, 2006.
Ment Health 14(8):971983, 2010. Grande GE, Myers LB, Sutton SR: How do patients who participate in
Cooper C, et al: Screening for elder abuse in dementia in the LASER-AD cancer support groups differ from those who do not? Psychol Oncol
study: prevalence, correlates, and validation of instruments, Int J 15(4):321334, 2006.
Geriatr Psychiatry 23(3):283288, 2008. Grant JS, et al: Sources of social support provided to people living with
Duff E, et al: A follow-up study of oncology nurses after communica- HIV, J Nurs Healthc Chronic Illn 1(4):331338, 2009.
tion skills training, Cancer Nurs Pract 8(1):2731, 2009.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Ineffective coping 267
Green DL, Choi JJ, Kane MN: Coping strategies for victims of crime: Popovich JM, Fox PG, Bandagi R: Coping with stroke: psychologi-
effects of the use of emotion-focused, problem-focused, and cal and social dimensions in U.S. patients, Int J Psychiatr Nurs Res
avoidance-oriented coping, J Hum Behav Soc Environ 20(6):732 12(3):14741487, 2007.
743, 2010. Porter SN, Pacquiao DF: Social and cultural construction of depres-
Gullatte MM, et al: Religiosity, spirituality, and cancer fatalism on delay sion among African American women, UPNAAI Nurs J 7(1):1315,
in breast cancer diagnosis in African American women, J Religion 1719, 2011.
Health 49(1):6272, 2010.
Hamill AC, Stein CH: Culture and empowerment in the deaf commu-
Rice M, et al: Relationship of anger, stress and coping with school con-
nectedness in fourth-grade children, J Sch Health 78:149156, 2008.
C
nity: an analysis of internet weblogs, J Community Appl Soc Psychol Rocchiccioli JT, Sanford JT: Revisiting geriatric failure to thrive: a com-
21(5):388406, 2011. plex and compelling clinical condition, J Gerontol Nurs 35(1):1824,
Hart PL, Grindel CG: Illness representations, emotional distress, coping 2009.
strategies, and coping efcacy as predictors of patient outcomes in Rose LE, Gerson L, Carbo C: Transitional care for seriously mentally ill
type 2 diabetes, J Nurs Healthc Chronic Illn 2(3):225240, 2010. persons: a pilot study, Arch Psychiatr Nurs 21(6):297308, 2007.
Hema DA, Roper SO, Nehring JW, et al: Daily stressors and coping Ross R, Sawatphanit W, Suwansujarid T: Finding peace (Kwam Sa-
responses of children and adolescents with type 1 diabetes, Child ngob): a Buddhist way to live with HIV, J Holistic Nurs 25(4):228
Care Health Dev 35(3):330339, 2009. 235, 2007.
Heyland DK, et al: Understanding cardiopulmonary resuscitation deci- Ruddick F: Coping with problems by focusing on solutions, Ment
sion making: perspectives of seriously ill hospitalized patients and Health Pract 14(8):2830, 2011.
family members, Chest 130(2):419428, 2006. Salmela M, Salanter S, Aronen ET: Coping with hospital related fears:
Janda M, et al: Unmet supportive care needs and interest in services experiences of pre-school-aged children, J Adv Nurs 66(6):1222
among patients with a brain tumor and their carers, Patient Educ 1231, 2010.
Couns 71(2):251258, 2008. Sandage SJ: Intergenerational suicide and family dynamics: a hermeneu-
Karademas EC, Hondronikola I: The impact of illness acceptance and tic phenomenological case study, Contemp Fam Ther 32(2):209227,
helplessness to subjective health and their stability over time: a pro- 2010.
spective study in a sample of cardiac patients, Psychol Health Med Sells D, et al: The treatment relationship in peer-based and regular case
15(3):336346, 2010. management for clients with severe mental illness, Psychiatr Serv
Khawaja NG, et al: Difculties and coping strategies of Sudanese 57(8):11791184, 2006.
refugees: a qualitative approach, Transcult Psychiatry 45(3):489512, Shearer BC, Fleury JD, Belyea M: Randomized control trial of the
2008. health empowerment intervention: feasibility and impact, Nurs Res
Kraaij V, Garnefski N, Schroevers MJ: Coping, goal adjustment, and 59(3):203211, 2010.
positive and negative effect in denitive infertility, J Health Psychol Solari-Twadell PA: Providing coping assistance for women with behav-
14(1):1826, 2009. ioral interventions, JOGNN 39(2):205211, 2010.
Loeb SJ: African American older adults coping with chronic health Stang J, Mittelmark MB: Intervention to enhance empowerment in a
conditions, J Transcult Nurs 17(2):139147, 2006. breast cancer self-help group, Nurs Inquiry 17(1):4656, 2010.
Mastin T, Campo S, Askelson NM: African American women and Stinson CK: Structured group reminiscence: an intervention for older
weight loss: disregarding environmental challenges, J Transcult Nurs adults, J Contin Educ Nurs 40(1):521528, 2009.
23(1):3845, 2012. Symes L, et al: The feasibility of home care workers delivering an inter-
Matchim Y, Armer JM, Stewart BR: IOS new scholar paper: a qualitative vention to decrease depression among home-dwelling older women,
study of participants perceptions of the effect of mindfulness medi- Issues Ment Health Nurs 28(7):799810, 2007.
tation practice on self care and overall well-being, Self Care Depend Tak SH: An insider perspective of daily stress and coping in elders with
Care Nurs 16(2):4653, 2008. arthritis, Orthop Nurs 25(2):2732, 2006.
McCauley KM, Bixby MB, Naylor MD: Advanced practice nurses Thomsen TG, Rydahl-Hansen S, Wagner L: A review of potential fac-
strategies to improve outcomes and reduce costs in elders with heart tors relevant to coping in patients with advanced cancer, J Clin Nurs
failure, Dis Manag 9(5):302310, 2006. 19(23/24):34103426, 2010.
Murray BL, Wright K: Integration of a suicide risk assessment and inter- Wang J, Tseng H, Chen K: Development and testing of screening indi-
vention approach: the perspective of youth, J Psychiatr Ment Health cators for psychological abuse of older people, Arch Psychiatr Nurs
Nurs 13(2):157164, 2006. 21(1):4047, 2007.
Oaz F, Haitpoglu S, Ayan H: Effectiveness of psychoeducation Wehbe-Alamah H: The use of Culture Care Theory with Syrian Mus-
intervention on post-traumatic stress disorder and coping styles of lims in the mid-western United States, Online J Cult Competence
earthquake survivors, J Clin Nurs 17(5):677687, 2008. Nurs Healthc 1(3):112, 2011.
Peek G, Melnyk BM: Coping interventions for parents of children newly Williams KA, Hamilton K: Culturally competent assessment of care of
diagnosed with cancer: an evidence review with implications for self-mutilation in urologic nursing, Urol Nurs 29(3):191194, 2009.
clinical practice and future research, Pediatr Nurs 36(6):306313, Zucca AC, et al: Life is precious and Im making the best of it: coping
2010. strategies of long-term cancer survivors, Psycho Oncol 19(12):1268
Pickett-Schenk SA, et al: Improving knowledge about mental illness 1276, 2010.
through family-led education: the journey of hope, Psychiatr Serv
59(1):4956, 2008.
= Independent CEB = Classic Research = Collaborative EBN = Evidence-Based Nursing EB = Evidence-Based
Anda mungkin juga menyukai
- Discharge Medical ReportDokumen3 halamanDischarge Medical ReportTeuku Arie HidayatBelum ada peringkat
- Amanda AquiliniDokumen2 halamanAmanda AquilinineoclintBelum ada peringkat
- Fetal Growth RestrictionDokumen13 halamanFetal Growth Restrictionantoniovilmo100% (2)
- Nursing Care Plans of PneumoniaDokumen16 halamanNursing Care Plans of Pneumoniaha,hr12480% (5)
- Ineffective Breathing PatternDokumen185 halamanIneffective Breathing PatternSusi LambiyantiBelum ada peringkat
- Plan of Care For Ineffective Air Way 1Dokumen6 halamanPlan of Care For Ineffective Air Way 1LisaBelum ada peringkat
- AssesmentDokumen9 halamanAssesmentmizrypBelum ada peringkat
- TUGAS Bahasa InggrisDokumen8 halamanTUGAS Bahasa InggrissantiBelum ada peringkat
- Weaning IndicesDokumen28 halamanWeaning IndicesSri HarshaBelum ada peringkat
- Below Are 8 Pneumonia Nursing Care Plans (NCP)Dokumen16 halamanBelow Are 8 Pneumonia Nursing Care Plans (NCP)Diana CarinoBelum ada peringkat
- Dyspnea and CoughDokumen70 halamanDyspnea and CoughLatha SukumarBelum ada peringkat
- DX Resp Failure PDFDokumen5 halamanDX Resp Failure PDFSherree HayesBelum ada peringkat
- Copd - NCPDokumen6 halamanCopd - NCPMonique Sacherow BacherBelum ada peringkat
- Nursing Diagnosis Impaired Gas ExchangeDokumen7 halamanNursing Diagnosis Impaired Gas ExchangeZycon Rodney Ae'zecquel Gachallan50% (2)
- Respiratory Assessment OHT Branding EditsDokumen25 halamanRespiratory Assessment OHT Branding EditsDeepika LingamBelum ada peringkat
- Bronchitis Nursing Care PlanDokumen8 halamanBronchitis Nursing Care PlanBryan NguyenBelum ada peringkat
- Group 2 DyspneaDokumen13 halamanGroup 2 DyspneaEmira CadizBelum ada peringkat
- Patient AssessmentDokumen2 halamanPatient AssessmentHopelet BieraBelum ada peringkat
- Nursing Management of Patients WithDokumen8 halamanNursing Management of Patients Withfunky goodBelum ada peringkat
- NCPDokumen9 halamanNCPEjie Boy Isaga67% (3)
- Oxygenation Lesson 3Dokumen78 halamanOxygenation Lesson 3Yjah Cheimira ASEBOBelum ada peringkat
- Respiratory RateDokumen15 halamanRespiratory RatekierchyBelum ada peringkat
- RespirationDokumen29 halamanRespirationbemina jaBelum ada peringkat
- Essential Parameters of Airway Evaluation Lecture 6Dokumen27 halamanEssential Parameters of Airway Evaluation Lecture 69yqgmkvyzdBelum ada peringkat
- Bronchitis: Kelompok IDokumen14 halamanBronchitis: Kelompok ILinda Permata Sari100% (1)
- Shortness of Breath Nursing Diagnosis and Nursing Care PlansDokumen13 halamanShortness of Breath Nursing Diagnosis and Nursing Care PlansRuffy AbdulazisBelum ada peringkat
- Diagnostic Studies: The Forced Expiratory Volume Over 1 Second (FEVDokumen7 halamanDiagnostic Studies: The Forced Expiratory Volume Over 1 Second (FEVKushan SenanayakaBelum ada peringkat
- Funda Notes Nca MidtermDokumen9 halamanFunda Notes Nca MidtermAICEL A. ABILBelum ada peringkat
- Chest Physical TherapyDokumen42 halamanChest Physical TherapySalman KhanBelum ada peringkat
- TriageDokumen20 halamanTriage39 femina pcBelum ada peringkat
- Triage 2Dokumen21 halamanTriage 239 femina pcBelum ada peringkat
- The Power of Breath: Diaphragmatic Breathing Clinical Tool: Whole Health: Change The ConversationDokumen11 halamanThe Power of Breath: Diaphragmatic Breathing Clinical Tool: Whole Health: Change The ConversationN onlyBelum ada peringkat
- Nursing Assessment Nursing Diagnosis Goal Planning Rationale Implementation Evaluation Subjective DataDokumen5 halamanNursing Assessment Nursing Diagnosis Goal Planning Rationale Implementation Evaluation Subjective DataDimpal Choudhary100% (1)
- NCP2Dokumen2 halamanNCP2Aura Salve Ildefonso AllasBelum ada peringkat
- Nursing DiagnosisDokumen16 halamanNursing DiagnosisSi Bunga JonquilleBelum ada peringkat
- Hronic Bstructive Ulmonary Isease: C O P DDokumen17 halamanHronic Bstructive Ulmonary Isease: C O P DĂhlă ZădjăĹỉăBelum ada peringkat
- Chapter 027Dokumen7 halamanChapter 027Diamonique95Belum ada peringkat
- Respiratory PresentationDokumen137 halamanRespiratory Presentationakoeljames8543Belum ada peringkat
- NS118 RLE: Click To Edit Master Title StyleDokumen12 halamanNS118 RLE: Click To Edit Master Title StyleAhmad BaolayyanBelum ada peringkat
- Oxygen Advantage Class 1Dokumen105 halamanOxygen Advantage Class 1Charles MitchellBelum ada peringkat
- Askep TBC Bahasa InggrisDokumen5 halamanAskep TBC Bahasa InggrisZaiful AhmadBelum ada peringkat
- Management of DysarthriaDokumen12 halamanManagement of DysarthriaSherin Manoj100% (1)
- Ch50 NCP IneffAirClear 1395-1396Dokumen2 halamanCh50 NCP IneffAirClear 1395-1396Caress Mae Gubaton CabudoyBelum ada peringkat
- Ineffective Breathing PatternDokumen2 halamanIneffective Breathing PatternPaolo Anthony GonzalesBelum ada peringkat
- Sir Tonette ICuDokumen3 halamanSir Tonette ICuDylle Lorenzo ClaudioBelum ada peringkat
- Emphysema Case Study AnalysisDokumen10 halamanEmphysema Case Study AnalysisEfren VisteBelum ada peringkat
- The Power of Breath Diaphragmatic BreathingDokumen13 halamanThe Power of Breath Diaphragmatic BreathingDrose BackBelum ada peringkat
- NCPDokumen11 halamanNCPRyan Dela CruzBelum ada peringkat
- Nursing Care PlanDokumen22 halamanNursing Care Planaln00550% (2)
- Ineffective Airway ClearanceDokumen9 halamanIneffective Airway ClearanceFatiha Sri Utami TamadBelum ada peringkat
- Nursing Care Plans For Activity IntoleranceDokumen4 halamanNursing Care Plans For Activity IntolerancethebigtwirpBelum ada peringkat
- Teaching Care PlanDokumen2 halamanTeaching Care Planapi-544206685Belum ada peringkat
- Effects of Buteyko Breathing Technique and Conventional Physical Therapy in Adult Bronchial Asthma: A Randomized Control TrailDokumen3 halamanEffects of Buteyko Breathing Technique and Conventional Physical Therapy in Adult Bronchial Asthma: A Randomized Control TrailMuhammad YozaBelum ada peringkat
- Alaa Abozeid ThesisDokumen133 halamanAlaa Abozeid Thesismostafa younisBelum ada peringkat
- COPDDokumen47 halamanCOPDMegha VadanereBelum ada peringkat
- Impaired Gas ExchangeDokumen4 halamanImpaired Gas ExchangeNuraini Hamzah100% (1)
- PneumoniaDokumen17 halamanPneumoniajustin_saneBelum ada peringkat
- What Is COPD? Chronic Obstructive Pulmonary Disease (COPD) : Signs and SymptomsDokumen11 halamanWhat Is COPD? Chronic Obstructive Pulmonary Disease (COPD) : Signs and SymptomsCecil Bhang-i Cacay - PabloBelum ada peringkat
- NCPDokumen9 halamanNCPLeolene Grace BautistaBelum ada peringkat
- Respiratory DisordersDokumen8 halamanRespiratory DisordersCezanne CruzBelum ada peringkat
- Sighing, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDari EverandSighing, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsBelum ada peringkat
- Snoring, A Simple Guide To The Condition, Treatment And Related ConditionsDari EverandSnoring, A Simple Guide To The Condition, Treatment And Related ConditionsBelum ada peringkat
- ArticleDokumen7 halamanArticleAlma AidhaBelum ada peringkat
- Pediatrics 2007 Spear S254 88Dokumen35 halamanPediatrics 2007 Spear S254 88arthoclaseBelum ada peringkat
- 14 Male Sexual Dysfunction LRDokumen54 halaman14 Male Sexual Dysfunction LRSammy FilipeBelum ada peringkat
- 1 SMDokumen6 halaman1 SMAlma AidhaBelum ada peringkat
- Telur Rebus Luka Perineum PDFDokumen6 halamanTelur Rebus Luka Perineum PDFAlma AidhaBelum ada peringkat
- Open Close CPR ResucitationDokumen9 halamanOpen Close CPR ResucitationAlma AidhaBelum ada peringkat
- Cig Smoking ComponentsDokumen17 halamanCig Smoking ComponentsIsmaira Moslem IsmaelBelum ada peringkat
- Materi Sertifikasi TI UBDokumen138 halamanMateri Sertifikasi TI UBMaika100% (2)
- NIH Public Access: The Nurse's Role in Preventing Cervical Cancer: A Cultural FrameworkDokumen10 halamanNIH Public Access: The Nurse's Role in Preventing Cervical Cancer: A Cultural FrameworkAlma AidhaBelum ada peringkat
- JNC 8Dokumen2 halamanJNC 8ririnrahayumsBelum ada peringkat
- Drug and Alcohol Dependence: Lisa Dierker, Donald Hedeker, Jennifer Rose, Arielle Selya, Robin MermelsteinDokumen5 halamanDrug and Alcohol Dependence: Lisa Dierker, Donald Hedeker, Jennifer Rose, Arielle Selya, Robin MermelsteinAlma AidhaBelum ada peringkat
- Laos-Health Professional ResearchDokumen94 halamanLaos-Health Professional ResearchAlma AidhaBelum ada peringkat
- 13r Newsletter Hypertension in Children and AdolescentsDokumen2 halaman13r Newsletter Hypertension in Children and AdolescentsAlma AidhaBelum ada peringkat
- International Journal of CardiologyDokumen6 halamanInternational Journal of CardiologyAlma AidhaBelum ada peringkat
- The Importance of Smoking Definitions For The Study of Adolescent Smoking BehaviorDokumen9 halamanThe Importance of Smoking Definitions For The Study of Adolescent Smoking BehaviorAlma AidhaBelum ada peringkat
- 13r Newsletter Hypertension in Children and AdolescentsDokumen2 halaman13r Newsletter Hypertension in Children and AdolescentsAlma AidhaBelum ada peringkat
- Unit 6: Resistance of The Body To Infection: II. Immunity and AllergyDokumen34 halamanUnit 6: Resistance of The Body To Infection: II. Immunity and AllergyEsteban Tabares GonzalezBelum ada peringkat
- Pharma NotesDokumen69 halamanPharma NotesJawad Ahmad100% (1)
- 1 s2.0 S1526054219300235 MainDokumen4 halaman1 s2.0 S1526054219300235 MainBruno SantosBelum ada peringkat
- Efficacy and Safety of Twice Vs Once Daily ALAADokumen11 halamanEfficacy and Safety of Twice Vs Once Daily ALAAOmar AyashBelum ada peringkat
- Why Your Muscles Get SoreDokumen11 halamanWhy Your Muscles Get SoreanaluieBelum ada peringkat
- Regulation of RespirationDokumen21 halamanRegulation of RespirationSheeraz ShahzadBelum ada peringkat
- TIFF X DAN 6 Week Shred III Workout Program Schedule v2Dokumen9 halamanTIFF X DAN 6 Week Shred III Workout Program Schedule v2808ricksmithBelum ada peringkat
- Clinical GuideDokumen13 halamanClinical GuideFatima NaeemBelum ada peringkat
- Cardiac Changes Associated With Vascular Aging: Narayana Sarma V. Singam - Christopher Fine - Jerome L. FlegDokumen7 halamanCardiac Changes Associated With Vascular Aging: Narayana Sarma V. Singam - Christopher Fine - Jerome L. Flegabraham rumayaraBelum ada peringkat
- DR - Monobina Sarker (Moic, Ccu) : Howrah District HospitalDokumen56 halamanDR - Monobina Sarker (Moic, Ccu) : Howrah District HospitalDeepa BhattacharjeeBelum ada peringkat
- PricelistDokumen71 halamanPricelistBugar Wahyu PBelum ada peringkat
- First Aid For BurnsDokumen21 halamanFirst Aid For Burnsgashbin MahdyBelum ada peringkat
- Precautions - Isolation Precautions - Guidelines Library - Infection Control - CDCDokumen6 halamanPrecautions - Isolation Precautions - Guidelines Library - Infection Control - CDCKomite PPI RSUDPCBelum ada peringkat
- Schistosomiasis JournalDokumen3 halamanSchistosomiasis JournalDez TabiosBelum ada peringkat
- SeizureDokumen10 halamanSeizureRomeo ReyesBelum ada peringkat
- Donating Corneas: Emma Hart and Alyssa NovelliDokumen12 halamanDonating Corneas: Emma Hart and Alyssa NovellisueiannacciBelum ada peringkat
- Above Knee AmputationDokumen8 halamanAbove Knee AmputationAbdul Ghafoor SajjadBelum ada peringkat
- High Salivary Soluble L-Selectin and Interleukin-7 Levels in Asian Indian Patients With Primary Sjögren's SyndromeDokumen5 halamanHigh Salivary Soluble L-Selectin and Interleukin-7 Levels in Asian Indian Patients With Primary Sjögren's SyndromeMaite Fernanda CuturrufoBelum ada peringkat
- Giraffe Blood CirculationDokumen9 halamanGiraffe Blood Circulationthalita asriandinaBelum ada peringkat
- GDS Scale PDFDokumen2 halamanGDS Scale PDFDiyah RahmawatiBelum ada peringkat
- Chromium Picolinate Side Effects What Are The Side Effects of Chromium Picolinate?Dokumen5 halamanChromium Picolinate Side Effects What Are The Side Effects of Chromium Picolinate?Jun JoniBelum ada peringkat
- Urostomy Guide - American Cancer SocietyDokumen19 halamanUrostomy Guide - American Cancer SocietyDipa HandraBelum ada peringkat
- Computational Fluid Dynamics and Trigeminal Sensory Examinations of Empty Nose Syndrome PatientsDokumen60 halamanComputational Fluid Dynamics and Trigeminal Sensory Examinations of Empty Nose Syndrome Patientsmadhumitha srinivasBelum ada peringkat
- Apollo Fertility IUI IVF Clinic and Dr. Lakshmi Krishna Leela GynecologistDokumen6 halamanApollo Fertility IUI IVF Clinic and Dr. Lakshmi Krishna Leela GynecologistPrabha SharmaBelum ada peringkat
- Atlas of Emergency Medicine 5Th Edition Kevin J Knoop Full ChapterDokumen67 halamanAtlas of Emergency Medicine 5Th Edition Kevin J Knoop Full Chaptergreg.vasquez490100% (8)
- Brugada SyndromeDokumen5 halamanBrugada SyndromevitriaBelum ada peringkat
- Laboratory Tests of Renal FunctionDokumen5 halamanLaboratory Tests of Renal Functiongiselle155204Belum ada peringkat
- Pregnancy PlannerDokumen75 halamanPregnancy PlannerDaniza LanyonBelum ada peringkat