Aki Poor4
Diunggah oleh
Pratita Jati PermatasariJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Aki Poor4
Diunggah oleh
Pratita Jati PermatasariHak Cipta:
Format Tersedia
Am J Physiol Renal Physiol 307: F939F948, 2014.
First published August 20, 2014; doi:10.1152/ajprenal.00025.2013.
Comparison of serum creatinine and serum cystatin C as biomarkers to detect
sepsis-induced acute kidney injury and to predict mortality in CD-1 mice
Asada Leelahavanichkul,1,2,4* Ana Carolina P. Souza,1,2* Jonathan M. Street,1,2 Victor Hsu,1,2
Takayuki Tsuji,1,2 Kent Doi,1,2 Lingli Li,2 Xuzhen Hu,1,2 Hua Zhou,1,2 Parag Kumar,3
Jrgen Schnermann,2 Robert A. Star,1,2 and Peter S. T. Yuen1,2
1
Renal Diagnostics and Therapeutics Unit, National Institute of Diabetes and Digestive and Kidney Diseases, National
Institutes of Health, Bethesda, Maryland; 2Kidney Disease Branch, National Institute of Diabetes and Digestive and Kidney
Diseases, National Institutes of Health, Bethesda, Maryland, and 3Pharmacy Department, Clinical Center, National Institutes
of Health, Bethesda, Maryland; and 4Department of Microbiology, Faculty of Medicine, Chulalongkorn University, Bangkok,
Thailand
Submitted 14 January 2013; accepted in final form 14 August 2014
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
Leelahavanichkul A, Souza AC, Street JM, Hsu V, Tsuji T, freely filtered through the glomerulus, also secreted but not
Doi K, Li L, Hu X, Zhou H, Kumar P, Schnermann J, Star RA, absorbed by renal tubules. Whereas SCr is predominantly
Yuen PS. Comparison of serum creatinine and serum cystatin determined by glomerular filtration rate (GFR), SCr is also
C as biomarkers to detect sepsis-induced acute kidney injury influenced by nonrenal factors that alter creatinine generation
and to predict mortality in CD-1 mice. Am J Physiol Renal Physiol
(muscle mass, dietary creatine intake, and liver function) and
307: F939 F948, 2014. First published August 20, 2014;
doi:10.1152/ajprenal.00025.2013.Acute kidney injury (AKI) dra- elimination (gastrointestinal excretion) (3). We previously
matically increases sepsis mortality, but AKI diagnosis is delayed demonstrated that creatinine production is reduced in sepsis,
when based on serum creatinine (SCr) changes, due in part, to which limits the ability of SCr to detect and stage sepsis-
decreased creatinine production. During experimental sepsis, we com- induced AKI (sepsis-AKI) (5). An endogenous molecule with
pared serum cystatin C (sCysC), SCr, and blood urea nitrogen (BUN) different properties could overcome these limitations, such as
to inulin glomerular filtration rate (iGFR) before or 318 h after cecal serum cystatin C (sCysC; molecular mass: 13.3 kDa) (1) a
ligation and puncture (CLP)-induced sepsis in CD-1 mice. sCysC had proteinase inhibitor that 1) prevents connective tissue destruc-
a faster increase and reached peak levels more rapidly than SCr in tion (24), 2) is constantly produced by most nucleated cells in
both sepsis and bilateral nephrectomy (BiNx) models. sCysC was a the body, 3) is freely filtered by the glomerulus, and 4) is then
better surrogate of iGFR than SCr during sepsis. Combining sCysC
entirely reabsorbed and catabolized in the proximal tubule (28,
with SCr values into a composite biomarker improved correlation
with iGFR better than any biomarker alone or any other combination.
31). sCysC has been proposed by some as a more ideal
We determined the renal contribution to sCysC handling with BiNx. endogenous biomarker of chronic kidney function (4, 12, 21,
sCysC and SCr were lower post-BiNx/CLP than post-BiNx alone, 28), although it is also affected by age, sex, muscle mass,
despite increased inflammatory and nonrenal organ damage biomark- smoking, thyroid function, and malignancies (2).
ers. Sepsis decreased CysC production in nephrectomized mice with- Whether sCysC is a better biomarker of kidney injury is a
out changing body weight or CysC space. Sepsis decreased sCysC matter of controversy, and it may depend on the context of use
production and increased nonrenal clearance, similar to effects of (14, 15). Within the context of chronic kidney disease, a
sepsis on SCr. sCysC, SCr, and BUN were measured 6 h postsepsis to combined creatinine-CysC estimated GFR (eGFR) equation
link AKI with mortality. Mice with above-median sCysC, BUN, or can perform somewhat better than equations based on either
SCr values 6 h postsepsis died earlier than mice with below-median biomarker alone (15).
values, corresponding to a substantial AKI association with sepsis
mortality in this model. sCysC performs similarly to SCr in classify-
In the setting of human AKI, urinary CysC predicts AKI
ing mice at risk for early mortality. We conclude that sCysC detects 48 72 h before SCr, whereas sCysC may detect AKI 12 days
AKI early and better reflects iGFR in CLP-induced sepsis. This study earlier than SCr in intensive care unit patients who developed
shows that renal biomarkers need to be evaluated in specific contexts. AKI and were classified according to RIFLE criteria (13).
sCysC also outperforms SCr as an early biomarker of AKI in
bilateral nephrectomy; glomerular filtration rate; survival; Kaplan- the emergency room setting (29) and after cardiopulmonary
Meier; receiver-operating characteristic curve
bypass in children (17).
But while some studies have shown the superiority of sCysC
SERUM CREATININE (SCr) is currently used to detect and stage as an early biomarker of AKI, other studies have shown that
acute kidney injury (AKI) and chronic kidney injury despite sCysC performs as well as, or even worse, than SCr. In a study
well-known limitations. Creatine is synthesized primarily in by Wald et al. (32), serial measurements of sCysC in adult
the liver and then transported to skeletal muscle for use in patients undergoing cardiopulmonary bypass correlated with
storing ATP (3). Creatinine (molecular mass: 113 Da), a the development of AKI, but the discriminatory capacity of
metabolic end product of creatine, is released into plasma, sCysC as an early biomarker of AKI was very limited. In the
postoperative period after cardiac surgery in elderly patients,
sCysC and SCr detected AKI similarly (25), and in a multi-
* A. Leelahavanichkul and A. C. P. Souza contributed equally to this work. center prospective observational cohort study involving a het-
Address for reprint requests and other correspondence: P. Yuen, National
Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of
erogeneous adult population admitted to an intensive care unit,
Health, Bldg. 10, Rm. 3N108, 10 Center Drive, MSC 1268, Bethesda, MD both urinary CysC and sCysC were poor early predictors of
20892-1268 (e-mail: py@nih.gov). AKI and the need for renal replacement therapy (26).
http://www.ajprenal.org F939
F940 SERUM CysC AS A BIOMARKER OF SEPSIS-INDUCED ACUTE KIDNEY INJURY
For sCysC to be considered a better biomarker of AKI than Survival experiments. Six hours after the induction of CLP-induced
SCr in some settings but not in others, rational criteria are sepsis, 50 l of blood were collected by the retroorbital sinus
needed for each setting (context of use). Early detection bio- approach under avertin anesthesia. Blood collection from younger
markers are especially difficult to establish in patients, as the (6 8 wk old) mice after sepsis resulted in rapid mortality (data not
shown); hence, the use of older (1216 wk old) mice for survival
timing of the initial renal injury is often difficult to discern. experiments. Animals were monitored for survival every 4 8 h after
Therefore, we compared the ability of SCr and sCysC to detect surgery, and the time to death was recorded for each animal. SCr,
kidney injury caused by sepsis (sepsis-AKI) under more con- sCysC, and BUN were measured as described above. Mice were given
trolled circumstances using an experimental model of sepsis in fluids and buprenorphine immediately after CLP; fluids, antibiotic,
mice. and buprenorphine were given starting at 6 h after sepsis and then
given every 12 h until the time to death. Morbidly ill mice were
METHODS euthanized per protocol.
Production and kinetics of sCysC. Production and kinetics of
Animals and animal models. We followed National Institutes of sCysC were performed in BiNx and BiNx CLP groups only. We
Health (NIH) criteria for the use and treatment of laboratory animals. took advantage of the otherwise stable sCysC level 12 h after BiNx or
All experiments were conducted on 6- to 8-wk-old male CD-1 mice BiNx CLP to measure the pharmacokinetics of injected recombi-
nant CysC. At 12 h after BiNx or BiNx CLP, 25 l of capillary
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
(Charles River Laboratories) except that 12- to 16-wk-old male CD-1
mice were used for blood collections at 6 h after the induction of blood were collected via the retroorbital sinus, and recombinant CysC
sepsis and subsequent survival analysis. All animals had free access to
water and chow and were monitored postoperatively for symptoms
including piloerection, spontaneous activity, response to stimuli, la- A
bored breathing, and eye grooming. All procedures were performed
under isoflurane anesthesia (including the euthanasia of morbidly ill
mice, per protocol).
Cecal ligation and puncture (CLP) was performed to induce sepsis
as previously described (18, 20, 33). In brief, the cecum was ligated
12 mm from its tip and then punctured twice with a 21-gauge needle.
Bilateral nephrectomy (BiNx) was performed as previously described
(5); briefly, both kidneys were decapsulated to avoid adrenal damage
and then removed via flank incisions. BiNx was performed at the same
time as CLP in the BiNx CLP group. For sham surgery, the cecum
and/or kidneys were identified via simultaneous incisions. Normal
saline (15 ml/kg) was given intraperitoneally immediately after all
surgeries and then either antibiotic (imipenem-cilastatin, 14 mg/kg in
1 ml normal saline) for CLP or normal saline for BiNx was given
subcutaneously at 6 h. All mice subjected to any surgical procedure
also received buprenorphine solution (0.05 mg/kg ip) immediately
after and at 6 h after surgery. When we measured GFR 6 h after CLP,
we delayed fluid administration so that it would not dilute inulin
before blood sampling.
GFR measurements in conscious mice. GFR was measured at 0, 3,
6, 12, or 18 h after CLP by FITC-labeled inulin clearance (7). Each B
mouse was studied only once at a single time point (n 5 6
mice/time point). One microcapillary tube of blood (50 l) was
collected via a tail vein for the measurement of SCr, blood urea
nitrogen (BUN), and sCysC at the specified time point post-CLP. A
single dose of FITC-inulin (3.74 l/g body wt) was injected into the
retroorbital plexus, and 5-l blood samples were collected from the
tail vein 10, 15, 35, 55, and 75 min afterward. Plasma fluorescence
was measured by a Nanodrop-ND-3300 fluorescence spectrometer
(Nanodrop Technologies, Wilmington, DE). GFR was then calculated
using a two-compartment model, as previously described (7). The
correlation between SCr, sCysC, and BUN at the specified time
post-CLP and inulin GFR (iGFR) in the individual mice was calcu-
lated (SigmaStat 3.1, Systat Software, Point Richmond, CA).
Blood chemistries. Fifty microliters of blood were collected by the
retroorbital approach before surgery (0 h) and at 3, 6, 12, and 18 h
after surgery (n 5 6 mice/time point), and body weight was
recorded. SCr was measured by HPLC (34), BUN by colorimetric
assay (QuantiChrom Urea assay kit DIUR-500, Hayward, CA), and Fig. 1. Fold changes of biomarkers over baseline values (0 h) at different time
mouse sCysC by ELISA (BioVendor, Candler, NC). Under anesthesia points after cecal ligation and puncture (CLP). A: at 3 h after CLP, serum
at 18 h after surgery, blood was collected after cardiac puncture, and cystatin C (sCysC) was 3-fold higher than baseline, whereas serum creatinine
(SCr) was unchanged (1.16-fold) and blood urea nitrogen (BUN) was slightly
mice were euthanized. Serum aspartate transaminase, alanine changed (1.74-fold). SCr was not different from BUN at all time points. There
transaminase, and lactate dehydrogenase were measured by an auto- were no differences among biomarkers at 6 h. sCysC represents the earliest
analyzer (Hitachi 917, Boehringer Mannheim, Indianapolis, IN), and and highest relative change among all biomarkers. *P 0.05. **P 0.01.
serum TNF-, IL-6, and IL-10 were measured by ELISA (R&D ***P 0.001. B: changes in inunlin glomerular filtration rate (iGFR) at the
Systems, Minneapolis, MN). various time points after CLP. #P 0.001 relative to baseline.
AJP-Renal Physiol doi:10.1152/ajprenal.00025.2013 www.ajprenal.org
SERUM CysC AS A BIOMARKER OF SEPSIS-INDUCED ACUTE KIDNEY INJURY F941
A 500 E 500
400 400
iGFR (l/min)
iGFR (l/min)
300 300
200 200
100 100
R 2 = 0 .924
p < 0.001
0 0
0 2 4 6 8 10 0 100 200 300 400 500 600
sCysC (g/ml) 220.7564
eGFR ( 3.3411 + ) (l/min)
sCysC
B 500 F 500
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
400 400
iGFR (l/min)
iGFR (l/min)
300 300
200 200
100 100
R 2 = 0 .743
p < 0.001
0 0
0.0 0.2 0.4 0.6 0.8 1.0 1.2 0 50 100 150 200 250 300 350 400 450
Scr (mg/dl) 36.7066
eGFR ( 28.3925 + ) (l/min)
Scr
C 600 G 600
500 500
iGFR (l/min)
iGFR (l/min)
400 400
300 300
200 200
100 100 R 2 = 0 .813
p < 0.001
0 0
20 40 60 80 100 0 100 200 300 400 500
BUN (mg/dl) 8080.9724
eGFR ( 62.7609 + ) (l/min)
BU N
D 500 H 500
400 400
iGFR (l/min)
iGFR (l/min)
300 300
200 200
100 100
R 2 = 0 .944
p < 0.001
0 0
0.000 0.005 0.010 0.015 0.020 0.025 0.030 0.035 0.040 0 100 200 300 400 500
10.5599 174.2714 1 10.5599 174.2714
Composite ( + ) eGFR ( 22.7981 + + ) (l/min)
Scr sCysC Scr sCysC
0h 3h 6h 12h 18h
Fig. 2. Time course of kidney dysfunction during sepsis-induced acute kidney injury (AKI) and cross correlation with renal function biomarkers. After
sepsis-induced AKI, sCysC (A; R2 0.924), SCr (B; R2 0.743), and BUN (C; R2 0.813) all increased, and their reciprocals were correlated with iGFR,
which decreased. A linear regression analysis of the relationship between each biomarkers reciprocal and iGFR was performed. iGFR and estimated GFR (eGFR)
values based on sCysC (E), SCr (F), and BUN (G) values were plotted against each other. A multiple regression model was created combining SCr and sCysC
(R2 0.944). The relationship between a weighted composite value of SCr and sCysC generated based on the coefficients of the multiple regression model is
shown (D), together with iGFR plotted against composite eGFR (H).
AJP-Renal Physiol doi:10.1152/ajprenal.00025.2013 www.ajprenal.org
F942 SERUM CysC AS A BIOMARKER OF SEPSIS-INDUCED ACUTE KIDNEY INJURY
distribution (Vd) was calculated as follows: Vd injected dose/
A [sCysCpeak postinjection(12 h 5 min) sCysCpreinjection(12 h)], and the
sCysC net production was calculated as follows: net production
(sCysC12 h sCysC0 h) Vd, as nonrenal clearance cannot be distin-
guished from production. An alternative noncompartmental method of
calculating Vd (Phoenix WinNonlin software, version 6.02, Pharsight,
Mountain View, CA) yielded similar results for Vd estimates.
Statistical analysis. All data are expressed as means SE.
ANOVA with Bonferronis multiple comparison correction was per-
formed using Prism 4.0 (Graphpad Software). We compared survival
curves using a log-rank test (Prism 4.0, Graphpad Software). The area
under the receiver-operating characteristic curve was calculated for
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
B
Fig. 3. Time course of sCysC, SCr, and BUN after CLP-induced sepsis alone
or after bilateral nephrectomy (BiNx). AC: time courses of sCysC (A), SCr
(B), and BUN (C) in CLP and BiNx (n 5 6 mice/group). Two-way ANOVA
was performed with Bonferroni post hoc analysis. *P 0.05, **P 0.01, and
#P 0.001, BiNx vs. CLP at each time point.
(5 g, R&D Systems) was injected by the tail vein. Additional
samples were taken at 5, 15, 30, 60, 120, and 180 min to determine
peak levels, and these limited time points enabled us to qualitatively Fig. 4. AC: time courses of sCysC (A), SCr (B), and BUN (C) in BiNx with
confirm a single compartment with no substantial distributive phase. and without CLP (n 5 6 mice/group). Two-way ANOVA was performed
sCysC levels after CysC administration at 12 h were adjusted for with Bonferroni post hoc analysis. *P 0.05 and #P 0.001, CLP vs.
an extrapolated production rate from 0 to 12 h. The volume of BiNx CLP at each time point. ns, Not significant.
AJP-Renal Physiol doi:10.1152/ajprenal.00025.2013 www.ajprenal.org
SERUM CysC AS A BIOMARKER OF SEPSIS-INDUCED ACUTE KIDNEY INJURY F943
each biomarker for each time point during the survival study (Prism in SCr and BUN (Fig. 1A). At 12 and 18 h, sCysC also had
4.0, Graphpad Software). We used the Statsmodels software package significantly higher increases over baseline compared with SCr
(python programming language, http://statsmodels.sourceforge.net/) and BUN, whereas at 6 h, the increased biomarker levels were
to perform a linear regression analysis on the reciprocal value of the
biomarkers. A weighted regression analysis was used to validate
not statistically different (Fig. 1A). At 3 h after CLP, GFR
results, with weights based on inverse variances, when visual inspec- dramatically decreased 50% (Fig. 1B); this was associated
tion of residual plots indicated a possible deviation from homosce- with a 3.2-fold increase in sCysC and a 1.7-fold increase in
dasticity. Models were compared using the Akaike information crite- BUN but no change in SCr (1.16-fold; Fig. 1A). Accordingly,
rion. P values of 0.05 were accepted as statistically significant. both sCysC and BUN outperformed SCr as early biomarkers of
sepsis-AKI, with sCysC being the best early biomarker. At
RESULTS
18 h after sepsis, GFR was reduced by 90% (from 428 to 5
sCysC outperforms SCr and BUN as a renal function bio- l/min; Fig. 1B), which was associated with 12.7-, 4.8-, and
marker early in the course of sepsis-AKI. We simultaneously 8.2-fold increases in sCysC, BUN, and SCr, respectively (Fig.
measured SCr, BUN, sCysC, and FITC-iGFR in conscious 1A). In addition to detecting changes in GFR early in the
mice at 0, 3, 6, 12, and 18 h after CLP using 5 6 mice/time progression of disease, accurate assessment of GFR is also
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
point. At 3 h after CLP, sCysC was increased threefold over important. The level of each biomarker was correlated to iGFR
baseline (0 h) sCysC. At this time point, both SCr and BUN by including all time points. Because there is a reciprocal
less than doubled their values over baseline, and the sCysC relationship between GFR and net accumulation of each cir-
increase over baseline was significantly higher than increases culating biomarker, we used 1/biomarker values to avoid an
Fig. 5. Effect of CLP-induced sepsis after BiNx on inflammation and nonrenal injury biomarkers. sCysC (A), SCr (B), BUN (C), aspartate transaminase (AST;
D), alanine transaminase (ALT; E), lactate dehydrogenase (LDH; F), TNF- (G), IL-6 (H), and IL-10 (I) were measured at 18 h after surgery (n 5 6
mice/group). One-way ANOVA was performed with Bonferroni post hoc analysis. *P 0.05, **P 0.01, and #P 0.001 between the indicated groups.
AJP-Renal Physiol doi:10.1152/ajprenal.00025.2013 www.ajprenal.org
F944 SERUM CysC AS A BIOMARKER OF SEPSIS-INDUCED ACUTE KIDNEY INJURY
A B C
Fig. 6. Effect of sepsis on CysC volume of
distribution (Vd), production, and elimina-
tion. A: Vd of CysC was measured at 5 min
(as baseline) and at 12 h after surgery. B:
estimated CysC production was measured at
0 12 h after CLP surgery (n 5 6 mice/
group). C: clearance was measured at 12 h
after CLP surgery (n 5 6 mice/group).
*P 0.05 vs. baseline.
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
asymptotic curve, which would visually and computationally not blunt BUN increases (Fig. 4, AC). In contrast, BiNx
compress the differences at the low GFR/high biomarker end combined with sepsis significantly increased other inflamma-
of the curve. With this transformation, the relationship was tory and organ damage parameters (inflammatory cytokines,
analyzed by linear regression. Although BUN changed quickly aspartate transaminase, alanine transaminase, and lactate de-
(at 3 h after sepsis), it underperformed sCysC in reflecting hydrogenase) compared with BiNx alone (Fig. 5). Hence,
iGFR (R2 0.813 vs. R2 0.924, P 0.001; Fig. 2). Both consistent with our previous study with SCr (5), we now
sCysC- and BUN-based eGFR equations were superior to SCr demonstrate that within the context of BiNx, sCysC also
(R2 0.743) in correlating to iGFR (P 0.001 and P 0.01, decreases after sepsis, in contrast to other circulating biomark-
respectively; Fig. 2). Next, we considered whether a combina- ers, which do not decrease.
tion of biomarkers would more accurately reflect iGFR than Sepsis decreases sCysC production and may increase non-
any individual biomarker. The combination of sCysC with renal sCysC elimination after BiNx without changing Vd. We
SCr, but not BUN, improved on the correlation of sCysC next determined whether changes in sCysC kinetics (i.e., in-
alone to iGFR (P 0.02 and P 0.6, respectively). sCysC creased Vd, production, metabolism, or elimination) could
alone was superior to the combination of SCr and BUN (P account for the reduction of sCysC after sepsis. Exogenous
0.001). The combination of all three biomarkers was not recombinant CysC was injected, and blood was sampled fre-
better than the combination of sCysC and SCr (P 0.83). quently (see METHODS). Vd of sCysC was not different between
Using the coefficients from the linear regression analysis, a BiNx sham and BiNx CLP groups (Fig. 6A), similar to
weighted composite mouse eGFR equation was created from our previous data on the FITC-inulin space (5). Additionally,
SCr and sCysC, and the relationship with GFR was visual- there were no differences in body weights between BiNx
ized (Fig. 2, D and H). sham and BiNx CLP groups (data not shown), as previously
Time courses of sCysC, SCr, and BUN accumulation after reported (5). Next, we found that sepsis reduced estimated net
CLP differ from those after BiNx. To determine the kinetic sCysC production (Fig. 6B); from this, we can infer that it may
response of these biomarkers to a sudden change in GFR, we have increased nonrenal elimination (see METHODS) (Fig. 6C).
measured the time course of sCysC, SCr, and BUN after BiNx. Serum CysC does not outperform SCr on predicting mortal-
We found that sCysC stabilized 12 h after BiNx and CLP, ity in the setting of sepsis. SCr, sCysC, and BUN were
whereas SCr and BUN were still increasing at 18 h (Fig. 3, measured at 6 h after CLP surgery, and the time to death was
AC). The increases in all biomarkers were diminished after measured. Post hoc assignment of mice to low and high
CLP compared with BiNx. This difference was statistically biomarker groups, using the median as a threshold, demon-
significant starting at 3 h for SCr (Fig. 3B), 6 h for sCysC (Fig. strated statistically significant differences in the Kaplan-Meier
3A), and 12 h for BUN (Fig. 3C). Therefore, CLP caused an survival curves for SCr, sCysC, and BUN (Fig. 7A). All mice
accumulation of each circulating biomarker over time that was died within 52 h. SCr, sCysC, and BUN were each able to
distinct from that caused by complete (BiNx) loss of renal predict the time to death (Fig. 7B), and higher biomarker
function. median values were associated with decreased survival (Fig.
Sepsis blunts BiNx-induced increases in sCysC and SCr. We 7A). Both SCr (P 0.001) and sCysC (P 0.001) were
(5) have previously demonstrated that sepsis decreases creati- superior to BUN, and SCr was stronger than sCysC (P
nine production. To determine if sepsis also affects sCysC 0.015) in predicting the time to death. Combining multiple
kinetics, CLP was performed simultaneously with BiNx. Loss biomarkers in the analysis did not improve on SCr alone. In
of kidney function by BiNx increased sCysC, SCr, and BUN, contrast, there was no difference in the ability of SCr and
as expected (Fig. 4, AC); BiNx combined with sepsis blunted sCysC to classify animals to earlier and later mortality groups.
these increases in sCysC at 18 h and SCr at 12 and 18 h but did Receiver-operating characteristic curves constructed compar-
Fig. 7. AKI biomarkers and mortality. Mice were grouped into above and below median (high vs. low, respectively) groups. Median/cutoff values were 1.186
mg/ml for sCysC, 0.241 mg/dl for SCr, and 54.57 mg/dl for BUN. A: mice with higher levels of sCysC, SCr, or BUN had a higher mortality rate. B: sCysC and
SCr correlated equivalently with the time to death, whereas BUN did not correlate with the time to death. C: there were no differences between areas under the
curves for both sCysC and SCr at different time points.
AJP-Renal Physiol doi:10.1152/ajprenal.00025.2013 www.ajprenal.org
SERUM CysC AS A BIOMARKER OF SEPSIS-INDUCED ACUTE KIDNEY INJURY F945
A B 2.5
2.0
sCysC (g/ml)
1.5
1.0
0.5
15 20 25 30 35 40 45 50 55
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
0.9
0.8
0.7
Scr (mg/dl)
0.6
0.5
0.4
0.3
0.2
0.1
15 20 25 30 35 40 45 50 55
120
110
100
BUN (mg/dl)
90
80
70
60
50
40
30
15 20 25 30 35 40 45 50 55
AJP-Renal Physiol doi:10.1152/ajprenal.00025.2013 www.ajprenal.org
F946 SERUM CysC AS A BIOMARKER OF SEPSIS-INDUCED ACUTE KIDNEY INJURY
ing mortality at earlier and later time points demonstrated no even before systemic sepsis symptoms, such as lethargy, di-
difference between SCr and sCysC (Fig. 7C). minished response to stimulus, or piloerection, developed at
6 h. Despite these large and rapid changes in iGFR, SCr was
DISCUSSION slow to react; sCysC and BUN had much faster kinetics: both
increased rapidly and achieved a steady state approximately
An ideal serum kidney filtration biomarker should be con- within 12 h (Fig. 1A).
stantly produced, freely filtered, neither secreted nor reab- Influence of sepsis on sCysC production and metabolism.
sorbed by the renal tubule, and lack nonrenal elimination We have recently found that sepsis blunted the increase in SCr
pathways (27). The biomarker might either have fast kinetics to after sepsis in BiNx mice and that creatinine production was
rapidly track minute changes in GFR or slower kinetics that reduced by sepsis (5). In the present study, we found that sepsis
integrate changes in GFR over a long time interval (similar to similarly blunted the increase in sCysC after sepsis in BiNx
glucose vs. HbA1C). Unfortunately, the production rate of mice.
creatinine is influenced by many extrarenal factors (muscle The effect of sepsis on sCysC was complicated, as sepsis
mass, age, sex, and reduced production in sepsis-AKI) and both reduced sCysC production and may have also enhanced
tubular secretion (3). Similarly, BUN is influenced by noncon- nonrenal clearance. The latter could be due to increased clear-
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
stant production and significant tubular reabsorption, espe- ance by the reticuloendothelial system (31). Both of these
cially during volume depletion (6). In contrast, sCysC produc- could conspire to reduce the ability of sCysC to function as an
tion is more predictable, although it is modestly influenced by early detection biomarker, even though sCysC did increase
smoking, obesity, hyperthyroidism, and low-grade chronic in- earlier (at 3 h) than SCr and BUN in the same mice. Although
flammation (10, 11, 16), but it is largely unaffected by acute BUN did not correspond to iGFR as well as sCysC, it also
inflammation, including sepsis-induced inflammation (19, 23, increased rapidly after BiNx or CLP, and CLP did not blunt the
28). Thus, sCysC could meet most of the ideal filtration increase observed after BiNx. As such, although BUN is not
biomarker criteria with less interindividual variation (9). the best biomarker for GFR, it may still be useful for detecting
At least two classes of AKI biomarkers are needed, each early changes in GFR. The usefulness of this early rise may be
with a different context of use or role in clinical decision somewhat diminished by 6 h when systemic symptoms of
making: an early detection biomarker that is tightly coupled to sepsis begin to manifest, as both sCr and sCysC outperformed
GFR, enabling rapid detection after the insult with an oppor- BUN as predictors of mortality.
tunity to identify patients that may be at a higher risk, and a AKI biomarkers and mortality. In this study, although sCysC
prognosis biomarker that can predict severity and/or mortality. was increased more than SCr early after CLP, it did not
We demonstrated in an animal model of sepsis that sCysC outperform SCr in predicting mortality. The areas under the
changes rapidly after injury and that a sCysC-based eGFR receiver-operating characteristic curves of sCysC and SCr with
equation better reflects iGFR throughout the course of sepsis- the outcome of mortality were comparable. Our result is
AKI. In comparison, BUN increased rapidly, but a BUN-based consistent with previous work by Perianayagam et al. (22),
eGFR equation only moderately correlated with iGFR; SCr which demonstrated that a single measurement of sCysC at the
increased slowly, and a SCr-based eGFR equation only poorly time of nephrology consultation did not surpass SCr on pre-
reflected GFR. The combination of sCysC with SCr, but not dicting in-hospital mortality among critically ill patients diag-
BUN, further improved eGFR equations when correlated to nosed with AKI. To date, very few clinical studies have
iGFR. However, sCysC is still not an ideal biomarker because analyzed sCysC as a predictor of mortality or early AKI
sepsis decreases the production and potentially increases the biomarker among septic patients. Recently, in a large multi-
nonrenal clearance of sCysC. Furthermore, sCysC did not center study (30), it was found that sCysC was less sensitive
outperform the widely used SCr to predict mortality. The for AKI detection than SCr among postcardiac surgery pa-
combination of SCr with sCysC also did not improve the tients.
performance of either individual biomarker with respect to For the mouse survival experiments, we chose to measure
sepsis mortality. sCysC, SCr, and BUN at 6 h after the induction of sepsis
sCysC outperforms creatinine early after AKI. GFR cannot because this is when the animals become clinically sick and,
be calculated in patients from SCr during AKI until a steady hence, in this model, mimics the time needed to diagnose
state is reached days after injury; this period is prolonged sepsis in a clinical setting. Both sCysC and SCr did not show
because of the slow creatinine kinetics and decreased produc- a very strong correlation with the time to death (with R2 0.7
tion (8). Therefore, we measured iGFR by the best available for both), as AKI is not expected to be the primary cause of
method of plasma disappearance of FITC-inulin, which uses a sepsis mortality, and dysfunction of other organs/systems also
two-compartment model of two-phase compartment decay, to contributes to mortality during sepsis.
approximate how quickly GFR falls during sepsis. This iGFR Conclusions. We evaluated the ability of sCysC to monitor
measurement has limitations during sepsis because 1) the the progression of sepsis-AKI in the clinically relevant mouse
calculation is based on an assumption that GFR does not model of polymicrobial sepsis in CD-1 mice. Among the three
change appreciably during the 75-min sampling window and 2) studied filtration biomarkers (sCysC, SCr, and BUN), sCysC
the number of samples that can be collected is limited by showed a more robust increase early after sepsis. The blunted
potential artifacts introduced by multiple blood draws. A more increase in sCysC after sepsis in BiNx, despite the increase in
sophisticated model could be developed, but there are limits to other nonrenal injury biomarkers, was caused by a sepsis-
how many time points can be collected before the collection induced reduction of sCysC production and possibly the in-
itself can cause its own artifacts. Nevertheless, sepsis rapidly crease in sCysC nonrenal elimination. Thus, sCysC is a better
reduced iGFR by 50% as early as 3 h after CLP (Fig. 1B), early detection biomarker than SCr in sepsis but is still influ-
AJP-Renal Physiol doi:10.1152/ajprenal.00025.2013 www.ajprenal.org
SERUM CysC AS A BIOMARKER OF SEPSIS-INDUCED ACUTE KIDNEY INJURY F947
enced by nonrenal factors that conspire to limit the accurate 9. Filler G, Bokenkamp A, Hofmann W, Le Bricon T, Martinez-Bru C,
prediction of GFR during the evolution of sepsis-AKI. BUN Grubb A. Cystatin C as a marker of GFR history, indications, and future
research. Clin Biochem 38: 18, 2005.
levels after BiNx were not affected by sepsis but corresponded 10. Fricker M, Wiesli P, Brandle M, Schwegler B, Schmid C. Impact of
poorly to iGFR. thyroid dysfunction on serum cystatin C. Kidney Int 63: 1944 1947, 2003.
sCysC did not outperform SCr in identifying mice at risk of 11. Galteau MM, Guyon M, Gueguen R, Siest G. Determination of serum
early or late mortality in this model of sepsis. sCysC can be cystatin C: biological variation and reference values. Clin Chem Lab Med
39: 850 857, 2001.
used interchangeably with SCr for mortality risk stratification,
12. Grubb AO. Cystatin Cproperties and use as diagnostic marker. Adv Clin
and it increases more, early after the insult, and correlates Chem 35: 6399, 2000.
better with iGFR than SCr. 13. Herget-Rosenthal S, Marggraf G, Husing J, Goring F, Pietruck F,
sCysC may not be an ideal biomarker for sepsis-AKI, but Janssen O, Philipp T, Kribben A. Early detection of acute renal failure
because an early biomarker may enhance risk stratification and by serum cystatin C. Kidney Int 66: 11151122, 2004.
14. Inker LA, Okparavero A. Cystatin C as a marker of glomerular filtration
facilitate early diagnosis, sCysC may be, indeed, a better rate: prospects and limitations. Curr Opin Nephrol Hypertens 20: 631
biomarker of sepsis-AKI than SCr. Although BUN also in- 639, 2011.
creased early after CLP, it did not correlate well with iGFR and 15. Inker LA, Schmid CH, Tighiouart H, Eckfeldt JH, Feldman HI,
was inferior to sCysC and SCr for classification of mortality Greene T, Kusek JW, Manzi J, Van Lente F, Zhang YL, Coresh J,
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
risk. Levey AS. Estimating glomerular filtration rate from serum creatinine and
cystatin C. N Engl J Med 367: 20 29, 2012.
16. Knight EL, Verhave JC, Spiegelman D, Hillege HL, de Zeeuw D,
ACKNOWLEDGMENTS Curhan GC, de Jong PE. Factors influencing serum cystatin C levels
The authors thank our late colleague Richard Chen for his invaluable other than renal function and the impact on renal function measurement.
contribution to statistical analysis and interpretation. The authors thank Chris- Kidney Int 65: 1416 1421, 2004.
toph Eisner for iGFR measurements. 17. Krawczeski CD, Vandevoorde RG, Kathman T, Bennett MR, Woo
JG, Wang Y, Griffiths RE, Devarajan P. Serum cystatin C is an early
predictive biomarker of acute kidney injury after pediatric cardiopulmo-
GRANTS nary bypass. Clin J Am Soc Nephrol 5: 15521557, 2010.
This research was supported by the Intramural Research Program of the 18. Leelahavanichkul A, Yasuda H, Doi K, Hu X, Zhou H, Yuen PS, Star
National Institutes of Health (National Institute of Diabetes and Digestive and RA. Methyl-2-acetamidoacrylate, an ethyl pyruvate analog, decreases
Kidney Diseases). sepsis-induced acute kidney injury in mice. Am J Physiol Renal Physiol
295: F1825F1835, 2008.
19. Martensson J, Martling CR, Oldner A, Bell M. Impact of sepsis on
DISCLOSURES levels of plasma cystatin C in AKI and non-AKI patients. Nephrol Dial
No conflicts of interest, financial or otherwise, are declared by the author(s). Transplant 27: 576 581, 2012.
20. Nemeth K, Leelahavanichkul A, Yuen PS, Mayer B, Parmelee A, Doi
K, Robey PG, Leelahavanichkul K, Koller BH, Brown JM, Hu X,
AUTHOR CONTRIBUTIONS
Jelinek I, Star RA, Mezey E. Bone marrow stromal cells attenuate sepsis
Author contributions: A.L., A.C.P.S., K.D., J.B.S., R.A.S., and P.S.Y. via prostaglandin E(2)-dependent reprogramming of host macrophages to
conception and design of research; A.L., A.C.P.S., V.H., L.L., X.H., and increase their interleukin-10 production. Nat Med 15: 4249, 2009.
P.S.Y. performed experiments; A.L., A.C.P.S., J.M.S., V.H., L.L., X.H., H.Z., 21. Newman DJ, Thakkar H, Edwards RG, Wilkie M, White T, Grubb
P.K., J.B.S., and P.S.Y. analyzed data; A.L., A.C.P.S., J.M.S., V.H., T.T., AO, Price CP. Serum cystatin C: a replacement for creatinine as a
K.D., H.Z., P.K., J.B.S., R.A.S., and P.S.Y. interpreted results of experiments; biochemical marker of GFR. Kidney Int Suppl 47: S20 S21, 1994.
A.L., A.C.P.S., J.M.S., and P.S.Y. prepared figures; A.L. and A.C.P.S drafted 22. Perianayagam MC, Seabra VF, Tighiouart H, Liangos O, Jaber BL.
manuscript; A.L., A.C.P.S., J.M.S., V.H., T.T., K.D., L.L., X.H., H.Z., P.K., Serum cystatin C for prediction of dialysis requirement or death in acute
J.B.S., R.A.S., and P.S.Y. approved final version of manuscript; A.C.P.S., kidney injury: a comparative study. Am J Kidney Dis 54: 10251033,
J.M.S., V.H., T.T., K.D., L.L., X.H., P.K., J.B.S., R.A.S., and P.S.Y. edited and 2009.
revised manuscript. 23. Randers E, Kornerup K, Erlandsen EJ, Hasling C, Danielsen H.
Cystatin C levels in sera of patients with acute infectious diseases with
REFERENCES high C-reactive protein levels. Scand J Clin Lab Invest 61: 333335, 2001.
24. Reed CH. Diagnostic applications of cystatin C. Br J Biomed Sci 57:
1. Baas MC, Bouman CS, Hoek FJ, Krediet RT, Schultz MJ. Cystatin C 323329, 2000.
in critically ill patients treated with continuous venovenous hemofiltration. 25. Ristikankare A, Poyhia R, Kuitunen A, Skrifvars M, Hammainen P,
Hemodial Int 10, Suppl 2: S33S37, 2006. Salmenpera M, Suojaranta-Ylinen R. Serum cystatin C in elderly
2. Bagshaw SM, Bellomo R. Cystatin C in acute kidney injury. Curr Opin cardiac surgery patients. Ann Thorac Surg 89: 689 694, 2010.
Crit Care 6: 533539, 2010. 26. Royakkers AA, Korevaar JC, van Suijlen JD, Hofstra LS, Kuiper
3. Bjornsson TD. Use of serum creatinine concentrations to determine renal MA, Spronk PE, Schultz MJ, Bouman CS. Serum and urine cystatin C
function. Clin Pharmacokinet 4: 200 222, 1979. are poor biomarkers for acute kidney injury and renal replacement therapy.
4. Christensson A, Ekberg J, Grubb A, Ekberg H, Lindstrom V, Lilja H. Intensive Care Med 37: 493501, 2011.
Serum cystatin C is a more sensitive and more accurate marker of 27. Shemesh O, Golbetz H, Kriss JP, Myers BD. Limitations of creatinine
glomerular filtration rate than enzymatic measurements of creatinine in as a filtration marker in glomerulopathic patients. Kidney Int 28: 830 838,
renal transplantation. Nephron Physiol 94: p19 p27, 2003. 1985.
5. Doi K, Yuen PS, Eisner C, Hu X, Leelahavanichkul A, Schnermann J, 28. Simonsen O, Grubb A, Thysell H. The blood serum concentration of
Star RA. Reduced production of creatinine limits its use as marker of cystatin C (gamma-trace) as a measure of the glomerular filtration rate.
kidney injury in sepsis. J Am Soc Nephrol 20: 12171221, 2009. Scand J Clin Lab Invest 45: 97101, 1985.
6. Dossetor JB. Creatininemia versus uremia. The relative significance of 29. Soto K, Coelho S, Rodrigues B, Martins H, Frade F, Lopes S, Cunha
blood urea nitrogen and serum creatinine concentrations in azotemia. Ann L, Papoila AL, Devarajan P. Cystatin C as a marker of acute kidney
Intern Med 65: 12871299, 1966. injury in the emergency department. Clin J Am Soc Nephrol 5: 17451754,
7. Eisner C, Faulhaber-Walter R, Wang Y, Leelahavanichkul A, Yuen 2010.
PS, Mizel D, Star RA, Briggs JP, Levine M, Schnermann J. Major 30. Spahillari A, Parikh CR, Sint K, Koyner JL, Patel UD, Edelstein CL,
contribution of tubular secretion to creatinine clearance in mice. Kidney Passik CS, Thiessen-Philbrook H, Swaminathan M, Shlipak MG.
Int 77: 519 526, 2010. Serum cystatin C- versus creatinine-based definitions of acute kidney
8. Endre ZH, Westhuyzen J. Early detection of acute kidney injury: injury following cardiac surgery: a prospective cohort study. Am J Kidney
emerging new biomarkers. Nephrology (Carlton) 13: 9198, 2008. Dis 60: 922929, 2012.
AJP-Renal Physiol doi:10.1152/ajprenal.00025.2013 www.ajprenal.org
F948 SERUM CysC AS A BIOMARKER OF SEPSIS-INDUCED ACUTE KIDNEY INJURY
31. Tenstad O, Roald AB, Grubb A, Aukland K. Renal handling of 33. Yasuda H, Leelahavanichkul A, Tsunoda S, Dear JW, Takahashi Y, Ito S,
radiolabelled human cystatin C in the rat. Scand J Clin Lab Invest 56: Hu X, Zhou H, Doi K, Childs R, Klinman DM, Yuen PS, Star RA.
409 414, 1996. Chloroquine and inhibition of Toll-like receptor 9 protect from sepsis-induced
32. Wald R, Liangos O, Perianayagam MC, Kolyada A, Herget- acute kidney injury. Am J Physiol Renal Physiol 294: F1050 F1058, 2008.
Rosenthal S, Mazer CD, Jaber BL. Plasma cystatin C and acute 34. Yuen PS, Dunn SR, Miyaji T, Yasuda H, Sharma K, Star RA. A
kidney injury after cardiopulmonary bypass. Clin J Am Soc Nephrol 5: simplified method for HPLC determination of creatinine in mouse serum.
13731379, 2010. Am J Physiol Renal Physiol 286: F1116 F1119, 2004.
Downloaded from http://ajprenal.physiology.org/ by 10.220.33.3 on July 11, 2017
AJP-Renal Physiol doi:10.1152/ajprenal.00025.2013 www.ajprenal.org
Anda mungkin juga menyukai
- Recent Advances of Sarcopenia and Frailty in CKDDari EverandRecent Advances of Sarcopenia and Frailty in CKDAkihiko KatoBelum ada peringkat
- Urine NGAL Predicts Severity of Acute Kidney Injury After Cardiac Surgery: A Prospective StudyDokumen9 halamanUrine NGAL Predicts Severity of Acute Kidney Injury After Cardiac Surgery: A Prospective StudyCa Nd RaBelum ada peringkat
- Diagnostik 1Dokumen6 halamanDiagnostik 1Roberto SoehartonoBelum ada peringkat
- Ascitic Lactate in SBPDokumen13 halamanAscitic Lactate in SBPtahayaseenfcpsgastroBelum ada peringkat
- Biomarcadores Post Aki A ErcDokumen12 halamanBiomarcadores Post Aki A ErcGiss UrizarBelum ada peringkat
- Predicting Pregnancy AKI with Multiple BiomarkersDokumen7 halamanPredicting Pregnancy AKI with Multiple BiomarkerscecilliacynthiaBelum ada peringkat
- Circulating miRNAs as Early Biomarkers for Contrast-Induced Acute Kidney InjuryDokumen21 halamanCirculating miRNAs as Early Biomarkers for Contrast-Induced Acute Kidney Injurytiger KeysBelum ada peringkat
- Biomarcadores en AKIDokumen14 halamanBiomarcadores en AKIhemer hadyn calderon alvitesBelum ada peringkat
- Ultrasound Spleen Morphology, But Not Vascular Liver Doppler MeasuresDokumen1 halamanUltrasound Spleen Morphology, But Not Vascular Liver Doppler MeasuresdenisegmeloBelum ada peringkat
- Evaluasi Prospektif Kadar Neutrophil Gelatinase-: Associated Lipocalin Urin Dan Kreatinin SerumDokumen7 halamanEvaluasi Prospektif Kadar Neutrophil Gelatinase-: Associated Lipocalin Urin Dan Kreatinin SerumJack Eugene LiowBelum ada peringkat
- An Update On Hepatorenal SyndromeDokumen10 halamanAn Update On Hepatorenal SyndromeWildaBelum ada peringkat
- CK and LBMDokumen8 halamanCK and LBMSarathBelum ada peringkat
- Urine Sediment Exam Provides More Diagnostic Information in AKI-1Dokumen4 halamanUrine Sediment Exam Provides More Diagnostic Information in AKI-1Ingrid González EfronBelum ada peringkat
- Acute Kidney Injury From Sepsis Current ConceptsDokumen33 halamanAcute Kidney Injury From Sepsis Current ConceptsUntuk DownloadBelum ada peringkat
- Acute Kidney Injury After Cardiac Surgery Chew2018Dokumen54 halamanAcute Kidney Injury After Cardiac Surgery Chew2018Oğuz KayıkçıBelum ada peringkat
- Bagshaw 2007Dokumen7 halamanBagshaw 2007Oğuz KayıkçıBelum ada peringkat
- Non-Onvasive Diagnosis of Acrd Current OpinionDokumen9 halamanNon-Onvasive Diagnosis of Acrd Current Opinionnathalialusman98Belum ada peringkat
- Derivation and Validation of The Renal Angina Index To Improve The Prediction of Acute Kidney Injury in Critically Ill ChildrenDokumen19 halamanDerivation and Validation of The Renal Angina Index To Improve The Prediction of Acute Kidney Injury in Critically Ill ChildrendoctoramanphalswalBelum ada peringkat
- Hepatorenal SyndromeDokumen14 halamanHepatorenal SyndromeVerónica Duménez JofréBelum ada peringkat
- Sharawey2011 PDFDokumen7 halamanSharawey2011 PDFIkram DibBelum ada peringkat
- Comparison of Scores in AclfDokumen9 halamanComparison of Scores in AclftahayaseenfcpsgastroBelum ada peringkat
- JCM 09 00619 v2Dokumen14 halamanJCM 09 00619 v2Medicina FamiliarBelum ada peringkat
- Lokesh Rana Laboratory MarksDokumen8 halamanLokesh Rana Laboratory MarksOlga GoryachevaBelum ada peringkat
- Acute Kidney Injury: Current Concepts and New Insights: Key WordsDokumen5 halamanAcute Kidney Injury: Current Concepts and New Insights: Key WordsIHBelum ada peringkat
- Screening Tests For Cushing's Syndrome: Urinary Free Cortisol Role Measured by LC-MS/MSDokumen6 halamanScreening Tests For Cushing's Syndrome: Urinary Free Cortisol Role Measured by LC-MS/MSAirene ZulfikarBelum ada peringkat
- Article AcuteKidneyInjuryInTheCriticalDokumen16 halamanArticle AcuteKidneyInjuryInTheCriticalJoão João MendesBelum ada peringkat
- Acute Kidney Injury Narrative 2021Dokumen16 halamanAcute Kidney Injury Narrative 2021Sanjith SaseedharanBelum ada peringkat
- Paper 2Dokumen15 halamanPaper 2constanzanazarethBelum ada peringkat
- Evaluation of NK Cells in HCV Patients on HemodialysisDokumen13 halamanEvaluation of NK Cells in HCV Patients on HemodialysisMaged SaadBelum ada peringkat
- Urine Interleukin-18 in Prediction of Acute Kidney InjuryDokumen10 halamanUrine Interleukin-18 in Prediction of Acute Kidney InjuryDianLumintoBelum ada peringkat
- 402 FullDokumen7 halaman402 FullFearless AngelBelum ada peringkat
- Evaluation of Specific Cytomorphologic Features and CA19-9 LevelsDokumen6 halamanEvaluation of Specific Cytomorphologic Features and CA19-9 LevelsТетяна МагасьBelum ada peringkat
- Risk Factors For Mortality in Acute Kidney InjuryDokumen6 halamanRisk Factors For Mortality in Acute Kidney Injuryredouane bennaiBelum ada peringkat
- The Association Between Urine Output, Creatinine Elevation, and DeathDokumen9 halamanThe Association Between Urine Output, Creatinine Elevation, and DeathTrahmono SrBelum ada peringkat
- A Comparative Study of Platelet Indices in Acute Coronary SyndromeDokumen4 halamanA Comparative Study of Platelet Indices in Acute Coronary SyndromeMarcellia AngelinaBelum ada peringkat
- Acute-On-Chronic Liver Failure Is A Distinct Syndrome That Develops in Patients With Acute Decompensation of CirrhosisDokumen21 halamanAcute-On-Chronic Liver Failure Is A Distinct Syndrome That Develops in Patients With Acute Decompensation of CirrhosisRubia Moresi Vianna De OliveiraBelum ada peringkat
- Urologi Jurnal InternasionalDokumen9 halamanUrologi Jurnal InternasionalMyisha UfairaBelum ada peringkat
- Left Ventricular Hypertrophy Is Associated With Inflammation in Sodium Loaded Subtotal Nephrectomized RatsDokumen8 halamanLeft Ventricular Hypertrophy Is Associated With Inflammation in Sodium Loaded Subtotal Nephrectomized RatsLuis Marcas VilaBelum ada peringkat
- Falla Renal en UCI Chest-2012Dokumen13 halamanFalla Renal en UCI Chest-2012Alexander CasillaBelum ada peringkat
- 530 FullDokumen9 halaman530 FullJackson MwaiBelum ada peringkat
- Fmed 07 617786Dokumen5 halamanFmed 07 617786Ashifa AshfaBelum ada peringkat
- Fmed 07 617786Dokumen5 halamanFmed 07 617786Ashifa AshfaBelum ada peringkat
- Irnf 45 2166531Dokumen9 halamanIrnf 45 2166531Romina Belen Mendez PerezBelum ada peringkat
- 1615 FullDokumen5 halaman1615 FullFearless AngelBelum ada peringkat
- Jurnal AkiDokumen8 halamanJurnal Akinelly muslimahBelum ada peringkat
- A Study of Serum Calcium and Serum Albumin Levels in Predicting Severity of Acute PancreatitisDokumen11 halamanA Study of Serum Calcium and Serum Albumin Levels in Predicting Severity of Acute PancreatitisIJAR JOURNALBelum ada peringkat
- 1994 - A Yeast System For Expression of Human Cystathionine F3-SynthaseDokumen5 halaman1994 - A Yeast System For Expression of Human Cystathionine F3-Synthasedo258Belum ada peringkat
- WalkerDokumen10 halamanWalkerPatty GracinoBelum ada peringkat
- The Cardiorenal Syndrome in Heart Failure 2022Dokumen17 halamanThe Cardiorenal Syndrome in Heart Failure 2022Raul FernandoBelum ada peringkat
- ACKD in DogsDokumen9 halamanACKD in DogsGreomary Cristina MalaverBelum ada peringkat
- Art:10.1007/s10140 015 1327 4Dokumen6 halamanArt:10.1007/s10140 015 1327 4Kumail KhandwalaBelum ada peringkat
- SX Hepatorrenal 2020Dokumen14 halamanSX Hepatorrenal 2020AlexisBallénBelum ada peringkat
- Clinical Risk Factors for Organ Involvement in Systemic SclerosisDokumen11 halamanClinical Risk Factors for Organ Involvement in Systemic Sclerosisnermal93Belum ada peringkat
- Cancers 15 00565Dokumen12 halamanCancers 15 00565Sediki ZakariaBelum ada peringkat
- 2012 Cistatina Cambios AgudosDokumen12 halaman2012 Cistatina Cambios Agudosisette.landerosBelum ada peringkat
- Paper 017Dokumen6 halamanPaper 017made dediBelum ada peringkat
- Cerebral Blood Flow in Acute and Chronic Ischemic Stroke Using Xenon-Inhalation TomographyDokumen13 halamanCerebral Blood Flow in Acute and Chronic Ischemic Stroke Using Xenon-Inhalation TomographygunawanBelum ada peringkat
- anan2020Dokumen7 halamananan2020Mohamed MohammedBelum ada peringkat
- Circulating Procalcitonin and Cleavage Products in Septicaemia Compared With Medullary Thyroid CarcinomaDokumen5 halamanCirculating Procalcitonin and Cleavage Products in Septicaemia Compared With Medullary Thyroid Carcinomamr_curiousityBelum ada peringkat
- Liver Transplantation - 2012 - Plotkin - Coronary Artery Disease and Liver Transplantation The State of The Art PDFDokumen4 halamanLiver Transplantation - 2012 - Plotkin - Coronary Artery Disease and Liver Transplantation The State of The Art PDFphonex xoxBelum ada peringkat
- Assess Child Growth and Causes of Failure to ThriveDokumen49 halamanAssess Child Growth and Causes of Failure to ThrivePratita Jati PermatasariBelum ada peringkat
- Chapter 5: Electrolyte and Acid - Base Disorders in MalignancyDokumen7 halamanChapter 5: Electrolyte and Acid - Base Disorders in MalignancyPratita Jati PermatasariBelum ada peringkat
- Hearing Loss9Dokumen12 halamanHearing Loss9Pratita Jati PermatasariBelum ada peringkat
- FTT 8Dokumen59 halamanFTT 8Pratita Jati PermatasariBelum ada peringkat
- (From J.N. Medical College, Aligarh) : Pulmonary Tuberculosis and LeukemiaDokumen3 halaman(From J.N. Medical College, Aligarh) : Pulmonary Tuberculosis and LeukemiaPratita Jati PermatasariBelum ada peringkat
- The Cognitive Phenotype in Klinefelter Syndrome: A Review of The Literature Including Genetic and Hormonal FactorsDokumen21 halamanThe Cognitive Phenotype in Klinefelter Syndrome: A Review of The Literature Including Genetic and Hormonal FactorsPratita Jati PermatasariBelum ada peringkat
- Klinefelter 8Dokumen13 halamanKlinefelter 8Pratita Jati PermatasariBelum ada peringkat
- Failure To Thrive: American Family Physician October 2003Dokumen7 halamanFailure To Thrive: American Family Physician October 2003Pratita Jati PermatasariBelum ada peringkat
- Klinefelter 29Dokumen4 halamanKlinefelter 29Pratita Jati PermatasariBelum ada peringkat
- Klinefelter 3Dokumen12 halamanKlinefelter 3Pratita Jati PermatasariBelum ada peringkat
- Klinefelter 6Dokumen5 halamanKlinefelter 6Pratita Jati PermatasariBelum ada peringkat
- Tuberculosis in Acute Leukemia: A Clinico-Hematological ProfileDokumen7 halamanTuberculosis in Acute Leukemia: A Clinico-Hematological ProfilePratita Jati PermatasariBelum ada peringkat
- Klinefelter 7 PDFDokumen44 halamanKlinefelter 7 PDFPratita Jati PermatasariBelum ada peringkat
- Klinefelter 5Dokumen7 halamanKlinefelter 5Pratita Jati PermatasariBelum ada peringkat
- Klinefelter 2Dokumen18 halamanKlinefelter 2Pratita Jati PermatasariBelum ada peringkat
- Klinefelter 1Dokumen2 halamanKlinefelter 1Pratita Jati PermatasariBelum ada peringkat
- ALL FeverDokumen5 halamanALL FeverPratita Jati PermatasariBelum ada peringkat
- Klinefelter ChildhoodDokumen9 halamanKlinefelter ChildhoodPratita Jati PermatasariBelum ada peringkat
- ALL GizburDokumen3 halamanALL GizburPratita Jati PermatasariBelum ada peringkat
- ALL+infiltrasi IntrakranialDokumen8 halamanALL+infiltrasi IntrakranialPratita Jati PermatasariBelum ada peringkat
- ICU Rounds: Pulmonary Leukostasis as a Complication of LeukemiaDokumen6 halamanICU Rounds: Pulmonary Leukostasis as a Complication of LeukemiaPratita Jati PermatasariBelum ada peringkat
- ALL CND p8Dokumen7 halamanALL CND p8Pratita Jati PermatasariBelum ada peringkat
- ALL Infiltrasi N XIIDokumen1 halamanALL Infiltrasi N XIIPratita Jati PermatasariBelum ada peringkat
- ALL+gizbur 9Dokumen8 halamanALL+gizbur 9Pratita Jati PermatasariBelum ada peringkat
- ALL Infiltrasi ParuDokumen5 halamanALL Infiltrasi ParuPratita Jati PermatasariBelum ada peringkat
- ALL+gizbur 6Dokumen8 halamanALL+gizbur 6Pratita Jati PermatasariBelum ada peringkat
- ALL+gizbur 2Dokumen4 halamanALL+gizbur 2Pratita Jati PermatasariBelum ada peringkat
- 2864Dokumen5 halaman2864kemalmiaBelum ada peringkat
- ALL Parese Nervus 3Dokumen4 halamanALL Parese Nervus 3Pratita Jati PermatasariBelum ada peringkat
- ALL CnsDokumen29 halamanALL CnsPratita Jati PermatasariBelum ada peringkat
- Meeting The Physical Therapy Needs of Children - Effgen, Susan K. (SRG)Dokumen797 halamanMeeting The Physical Therapy Needs of Children - Effgen, Susan K. (SRG)bizcocho4100% (7)
- Versed dosing guideDokumen4 halamanVersed dosing guideintrovert ikonBelum ada peringkat
- RLE Manual EditedDokumen68 halamanRLE Manual EditedReymondBelum ada peringkat
- Gout N C P BY BHERU LALDokumen1 halamanGout N C P BY BHERU LALBheru LalBelum ada peringkat
- SWOT AnalysisDokumen3 halamanSWOT Analysisdadedidopyaaang100% (2)
- Veinuino RiceDokumen10 halamanVeinuino RiceAshley NacarBelum ada peringkat
- Nursing Fundamentals Exam ReviewDokumen10 halamanNursing Fundamentals Exam ReviewAlain CheryBelum ada peringkat
- Discharge Planning FinalDokumen3 halamanDischarge Planning FinalRae Marie AquinoBelum ada peringkat
- Patient Scenario, Chapter 19, Nutritional Needs of A NewbornDokumen3 halamanPatient Scenario, Chapter 19, Nutritional Needs of A NewbornNobiliary ortizBelum ada peringkat
- Writing OETDokumen4 halamanWriting OETfernanda1rondelliBelum ada peringkat
- Mod 3 Guidelines in Giving Emergency CAreDokumen5 halamanMod 3 Guidelines in Giving Emergency CArerez1987100% (2)
- The Asthma, COPD & Allergic Rhinitis Market Outlook To 2011: HealthcareDokumen163 halamanThe Asthma, COPD & Allergic Rhinitis Market Outlook To 2011: HealthcareYuva VikazBelum ada peringkat
- Callo, Dimple C. (Case Scenario 2)Dokumen4 halamanCallo, Dimple C. (Case Scenario 2)Dimple Castañeto CalloBelum ada peringkat
- Protocols Sepsis Treatment Stony BrookDokumen6 halamanProtocols Sepsis Treatment Stony BrookVicky Chrystine SianiparBelum ada peringkat
- 125.6 (Medicine) DISCHARGE PLANDokumen1 halaman125.6 (Medicine) DISCHARGE PLANNadja Jamilah100% (1)
- Nursing Process PsychiatricDokumen13 halamanNursing Process PsychiatricamitBelum ada peringkat
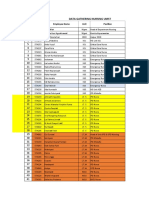
- Data Peserta Gartheting LT 3aumst Final 2022Dokumen11 halamanData Peserta Gartheting LT 3aumst Final 2022Doni IrawanBelum ada peringkat
- Ehaq 4TH Cycle Protocol Must PreparedDokumen3 halamanEhaq 4TH Cycle Protocol Must PreparedMiraf Mesfin100% (2)
- Preterm Its ProblemsDokumen30 halamanPreterm Its ProblemsEnlighten usBelum ada peringkat
- Ear MedicationDokumen15 halamanEar MedicationPascalina Monts'onyaneBelum ada peringkat
- Reading Sample Test 1 Question Paper Part A PDFDokumen4 halamanReading Sample Test 1 Question Paper Part A PDFnavroop bajwaBelum ada peringkat
- Pancreatic Cancer Therapeutics in Major Developed Markets To 2021Dokumen7 halamanPancreatic Cancer Therapeutics in Major Developed Markets To 2021Kanchan JagtaniBelum ada peringkat
- Extraoral Examination 1Dokumen58 halamanExtraoral Examination 1SyaZuWaN JaMiLBelum ada peringkat
- The Vision, Mission and Core Values of The Institution: - o o o - o oDokumen23 halamanThe Vision, Mission and Core Values of The Institution: - o o o - o oYvonne de ChavezBelum ada peringkat
- Module 1 To 5 QM Training For Blood Transfusion Services WHO PDFDokumen182 halamanModule 1 To 5 QM Training For Blood Transfusion Services WHO PDFRose jane Tambasen100% (1)
- Dog Parvo Virus Guide: Symptoms, Diagnosis & TreatmentDokumen39 halamanDog Parvo Virus Guide: Symptoms, Diagnosis & TreatmentKundan Kumar Panda100% (1)
- October 2023 PRC PLE Schedule and Reminders 2Dokumen4 halamanOctober 2023 PRC PLE Schedule and Reminders 2TrisBelum ada peringkat
- GERD DR Hegar Dec2015Dokumen52 halamanGERD DR Hegar Dec2015nur_betaBelum ada peringkat
- Emergency Department Case Management: Second EditionDokumen39 halamanEmergency Department Case Management: Second EditionsadikinBelum ada peringkat
- Ritin Kumar Srivastava Block No. 31/4, Kabeer Nagar Colony: TH THDokumen3 halamanRitin Kumar Srivastava Block No. 31/4, Kabeer Nagar Colony: TH THswapnilkhadke89Belum ada peringkat
- The Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthDari EverandThe Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthPenilaian: 5 dari 5 bintang5/5 (37)
- The Raw Food Detox Diet: The Five-Step Plan for Vibrant Health and Maximum Weight LossDari EverandThe Raw Food Detox Diet: The Five-Step Plan for Vibrant Health and Maximum Weight LossPenilaian: 4 dari 5 bintang4/5 (22)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyDari EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyPenilaian: 5 dari 5 bintang5/5 (1)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisDari EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisPenilaian: 3 dari 5 bintang3/5 (2)
- Power Souping: 3-Day Detox, 3-Week Weight-Loss PlanDari EverandPower Souping: 3-Day Detox, 3-Week Weight-Loss PlanPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- Summary of Mary Claire Haver's The Galveston DietDari EverandSummary of Mary Claire Haver's The Galveston DietPenilaian: 5 dari 5 bintang5/5 (1)
- Glucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingDari EverandGlucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingPenilaian: 5 dari 5 bintang5/5 (59)
- Forever Strong: A New, Science-Based Strategy for Aging WellDari EverandForever Strong: A New, Science-Based Strategy for Aging WellBelum ada peringkat
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouDari EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouBelum ada peringkat
- Happy Gut: The Cleansing Program to Help You Lose Weight, Gain Energy, and Eliminate PainDari EverandHappy Gut: The Cleansing Program to Help You Lose Weight, Gain Energy, and Eliminate PainPenilaian: 3.5 dari 5 bintang3.5/5 (6)
- Keto Friendly Recipes: Easy Keto For Busy PeopleDari EverandKeto Friendly Recipes: Easy Keto For Busy PeoplePenilaian: 2 dari 5 bintang2/5 (1)
- Allen Carr's Easy Way for Women to Lose Weight: The original Easyway methodDari EverandAllen Carr's Easy Way for Women to Lose Weight: The original Easyway methodPenilaian: 4.5 dari 5 bintang4.5/5 (18)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsDari EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsPenilaian: 4 dari 5 bintang4/5 (49)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeDari EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeBelum ada peringkat
- Proteinaholic: How Our Obsession with Meat Is Killing Us and What We Can Do About ItDari EverandProteinaholic: How Our Obsession with Meat Is Killing Us and What We Can Do About ItPenilaian: 4.5 dari 5 bintang4.5/5 (19)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeDari EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifePenilaian: 4 dari 5 bintang4/5 (3)
- Lose Weight by Eating: 130 Amazing Clean-Eating Makeovers for Guilt-Free Comfort FoodDari EverandLose Weight by Eating: 130 Amazing Clean-Eating Makeovers for Guilt-Free Comfort FoodPenilaian: 2 dari 5 bintang2/5 (1)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreDari EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MorePenilaian: 5 dari 5 bintang5/5 (17)
- The Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthDari EverandThe Candida Cure: The 90-Day Program to Balance Your Gut, Beat Candida, and Restore Vibrant HealthBelum ada peringkat
- How to Be Well: The 6 Keys to a Happy and Healthy LifeDari EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifePenilaian: 5 dari 5 bintang5/5 (1)
- The Longevity Plan: Seven Life-Transforming Lessons from Ancient ChinaDari EverandThe Longevity Plan: Seven Life-Transforming Lessons from Ancient ChinaBelum ada peringkat
- The Ultimate Volumetrics Diet: Smart, Simple, Science-Based Strategies for Losing Weight and Keeping It OffDari EverandThe Ultimate Volumetrics Diet: Smart, Simple, Science-Based Strategies for Losing Weight and Keeping It OffBelum ada peringkat
- Ultrametabolism: The Simple Plan for Automatic Weight LossDari EverandUltrametabolism: The Simple Plan for Automatic Weight LossPenilaian: 4.5 dari 5 bintang4.5/5 (28)
- The Toxin Solution: How Hidden Poisons in the Air, Water, Food, and Products We Use Are Destroying Our Health—AND WHAT WE CAN DO TO FIX ITDari EverandThe Toxin Solution: How Hidden Poisons in the Air, Water, Food, and Products We Use Are Destroying Our Health—AND WHAT WE CAN DO TO FIX ITPenilaian: 5 dari 5 bintang5/5 (1)
- Celiac Disease: A Hidden EpidemicDari EverandCeliac Disease: A Hidden EpidemicPenilaian: 4.5 dari 5 bintang4.5/5 (17)
- Brain Body Diet: 40 Days to a Lean, Calm, Energized, and Happy SelfDari EverandBrain Body Diet: 40 Days to a Lean, Calm, Energized, and Happy SelfPenilaian: 5 dari 5 bintang5/5 (2)
- Think Yourself Thin: A 30-Day Guide to Permanent Weight LossDari EverandThink Yourself Thin: A 30-Day Guide to Permanent Weight LossPenilaian: 4.5 dari 5 bintang4.5/5 (22)
- Kintsugi Wellness: The Japanese Art of Nourishing Mind, Body, and SpiritDari EverandKintsugi Wellness: The Japanese Art of Nourishing Mind, Body, and SpiritPenilaian: 4.5 dari 5 bintang4.5/5 (3)