Management of Newly Diagnosed HIV Infection
Diunggah oleh
Roberto López MataHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Management of Newly Diagnosed HIV Infection
Diunggah oleh
Roberto López MataHak Cipta:
Format Tersedia
Annals of Internal Medicine
In the Clinic
Management
of Newly
Diagnosed
HIV Infection Screening and Prevention
N
o eld in medicine has moved as swiftly
as HIV/AIDS over the past 35 years. Be- Diagnosis and Evaluation
cause of the rapid turnover of key infor-
mation, this In the Clinic focuses on essential
principles of care for newly diagnosed adults Treatment
with HIV-1 infection and how to prevent infec-
tion in persons at risk. To ensure continued use-
fulness, future directions in therapy and how to
access updated information on a continuous
Practice Improvement
basis are emphasized.
CME/MOC activity available at Annals.org.
Physician Writers doi:10.7326/AITC201707040
Judith Feinberg, MD
Susana Keeshin, MD CME Objective: To review current evidence for screening and prevention, diagnosis and
From West Virginia University, evaluation, treatment, and practice improvement of management of newly diagnosed HIV
Morgantown, West Virginia, infection.
and the University of Utah, Funding Source: American College of Physicians.
Salt Lake City, Utah.
Disclosures: Drs. Feinberg and Keeshin, ACP Contributing Authors. Disclosures can also be
viewed at www.acponline.org/authors/icmje/ConictOfInterestForms.do?msNum=M17
-0709.
With the assistance of additional physician writers, the editors of Annals of Internal
Medicine develop In the Clinic using MKSAP and other resources of the American
College of Physicians.
In the Clinic does not necessarily represent ofcial ACP clinical policy. For ACP clinical
guidelines, please go to https://www.acponline.org/clinical_information/guidelines/.
2017 American College of Physicians
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
Studies have shown that positive cine, family medicine, pharmacy,
clinical outcomes for HIV-infected and advanced-practice nursing.
persons are a function of the cli- Thus, it is important to identify
nician's experience (1, 2). Thus, experts available in a given com-
nonspecialists are urged to seek munity. It is especially important
1. Kitahata MM, Koepsell TD, expert advice and consultation to seek input from experienced
Deyo RA, Maxwell CL,
Dodge WT, Wagner EH. from experienced HIV care pro- practitioners in the setting of
Physicians' experience viders whenever possible. HIV antiretroviral treatment failure and
with the acquired immu-
nodeciency syndrome as specialists come from many in cases of advanced HIV disease
a factor in patients' sur-
vival. N Engl J Med. 1996; backgrounds, including infec- (AIDS) when patients are vulnera-
334:701-6. [PMID: tious diseases, hematology/on- ble to multiple, often simultaneous
8594430]
2. Kitahata MM, Van Rom- cology, general internal medi- opportunistic infections (OIs).
paey SE, Shields AW.
Physician experience in
the care of HIV-infected
persons is associated with
earlier adoption of new Screening and Prevention
antiretroviral therapy. J
Acquir Immune Dec Who should be screened for or who received a blood transfu-
Syndr. 2000;24:106-14. HIV infection? sion between 1978 and 1985.
[PMID: 10935685]
3. Palella FJ Jr, Delaney KM, Despite a sharp decline in AIDS Persons who request an HIV test
Moorman AC, Loveless
MO, Fuhrer J, Satten GA, cases and deaths since the ad- despite reporting no individual
et al. Declining morbidity vent of highly active antiretroviral risk factors may also be consid-
and mortality among
patients with advanced therapy (ART) (3), the Centers for ered at increased risk because it
human immunodeciency is likely that they have risk factors
virus infection. HIV Outpa- Disease Control and Prevention
tient Study Investigators. (CDC) estimates that more than that they are unwilling or unable
N Engl J Med. 1998;338:
853-60. [PMID: 9516219] 1.2 million adults and adoles- to disclose. Anyone who asks for
4. Centers for Disease Con- cents in the United States are liv- an HIV test should receive one.
trol and Prevention. HIV
Surveillance Report, 2015. ing with HIV, including 14% (1 in
Accessed at www.cdc.gov In 2006, the CDC recommended that everyone
/hiv/pdf/library/reports 7) who are unaware of their infec-
between the ages of 13 and 64 years should be
/surveillance/cdc-hiv tion (4). The U.S. epidemic con-
-surveillance-report-2015 tested for HIV on an opt-out basis at least once as
-vol-27.pdf on 16 March tinues to disproportionately af- part of routine health care, unless the local prev-
2017.
5. Branson BM, Handseld
fect racial and ethnic minorities, alence rate of HIV infection is below 0.1%. Be-
HH, Lampe MA, Janssen and especially young men who cause clinicians may not know this rate, the CDC
RS, Taylor AW, Lyss SB,
et al; Centers for Disease have sex with men (MSM). Per- recommends routine voluntary HIV screening for
Control and Prevention sons with undiagnosed HIV tend
(CDC). Revised recommen-
all patients aged 13 to 64 years in any health care
dations for HIV testing of to be younger (1329 years) MSM setting until the diagnostic yield in a given local-
adults, adolescents, and
pregnant women in and males with high-risk hetero- ity has been shown to be less than 1 per 1000
health-care settings. sexual contact (4). patients screened (5).
MMWR Recomm Rep.
2006;55:1-17. [PMID:
16988643] People at known increased risk Opt-out means that permission
6. Nebraska Revised Statute
for HIV infection include MSM; for HIV testing is included in the
71-531. Accessed at http:
//nebraskalegislature.gov men and women having unpro- general informed consent for
/laws/statutes.php?statute
=71-531 on 16 March tected sex with multiple partners; medical care unless, after being
2017. persons who inject drugs notied of this fact, the patient
7. New York State Public
Health Law Article 27F, (PWIDs) currently or have done explicitly declines. Written con-
Section 2781. Accessed at sent and prevention counseling
www.health.ny.gov so in the past; men and women
/diseases/aids/providers who exchange sex for money, as required elements of HIV test-
/regulations/testing
/section_2781.htm on 16 drugs, or other commodities or ing were eliminated from the
March 2017.
who have sex partners who do; 2006 recommendations. Only
8. Centers for Disease Con-
trol and Prevention (CDC). persons with past or present sex Nebraska and New York have
Diagnoses of HIV infection
among adults aged 50 partners who are HIV-infected, laws that differ from CDC recom-
years and older in the bisexual, or PWIDs; persons who mendations (6, 7). Also, because
United States and depen-
dent areas, 2010 2014. engage in receptive anal sex re- many adults continue sexual ac-
HIV Surveillance Supple-
ment 1al Report. 2016.
gardless of sexual orientation; tivity past age 64 years and 45%
Accessed at www.cdc.gov persons treated for sexually of HIV-infected persons are aged
/hiv/pdf/library/reports
/surveillance/cdc-hiv transmitted diseases (STDs); and, 50 years or older (8), testing all
-surveillance-supplemen- although now few in number, sexually active adults, regardless
tal-report-vol-21-2.pdf on
16 March 2017. persons treated for hemophilia of age, is clinically appropriate.
2017 American College of Physicians ITC2 In the Clinic Annals of Internal Medicine 4 July 2017
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
These recommendations are those who may have serocon-
based partially on the fact that verted during pregnancy. The
risk-based testing has not been CDC recommends that all per-
effective: Providers seldom ade- sons and their prospective sex
quately assess risk, approxi- partners be tested before enter- 9. Chou R, Huffman L. U.S.
mately 10%25% of persons with ing into a new sexual relation- Preventive Services Task
Force Evidence Syntheses,
undiagnosed HIV are unaware of ship. Rescreening patients who formerly Systematic Evi-
any risk factors or are uncomfort- dence Reviews. Screening
are not likely to be at high risk is for human immunode-
able with disclosing them, and left to clinical judgment. Clini- ciency virus: focused up-
date of a 2005 systematic
almost half of patients are identi- cians should generally maintain a evidence review for the
ed late in the course of disease low threshold for both screening U.S. Preventive Services
Task Force. Rockville:
when they can no longer receive and rescreening. Agency for Healthcare
the maximum benet from ART Research and Quality;
2007. [PMID: 20722143]
(4). Many persons, especially MSM 10. Chou R, Korthuis PT, Huff-
man LH, Smits AK. U.S.
who seek preventive services for Preventive Services Task
All persons at risk as well as HIV, face stigma, homophobia, Force Evidence Syntheses,
those in the following subgroups and discriminatory behavior;
formerly Systematic Evi-
dence Reviews. Screening
should routinely be screened for black MSM have substantially for human immunode-
ciency virus in adolescents
HIV infection: those who have sex more challenges. The CDC esti- and adults. Rockville:
with a person of unknown HIV mates the lifetime risk for HIV as Agency for Healthcare
Research and Quality;
status; those diagnosed with and 1 in 2 among black MSM. Young 2005. [PMID: 20722134]
initiating treatment for tuberculo- black MSM are more likely not to
11. Centers for Disease Control
and Prevention (CDC).
sis, hepatitis B, or hepatitis C; know their HIV status, face strong Updated guidelines for
antiretroviral postexposure
those seeking treatment for socioeconomic barriers, and prophylaxis after sexual,
STDs; victims of sexual assault; all injection drug use, or
have smaller sexual networks other nonoccupational
pregnant women as part of rou- exposure to HIVUnited
(14, 15).
tine prenatal care on an opt-out States, 2016. 2016. Ac-
cessed at www.cdc.gov/hiv
basis; all women of unknown HIV Daily PrEP with a single, xed- /pdf/programresources/cdc
-hiv-npep-guidelines.pdf
serostatus who present in labor dose, antiviral combination tablet on 16 March 2017.
(9, 10); infants exposed to HIV in (emtricitabine/tenofovir) has 12. Kuhar DT, Henderson DK,
Struble KA, Heneine W,
utero; persons initiating and tak- been shown to reduce HIV acqui- Thomas V, Cheever LW,
ing HIV pre- or post-exposure sition by 92% or greater in cer- et al; US Public Health
Service Working Group.
prophylaxis (PrEP, PEP); and any- tain at-risk populations, is consid- Updated US Public Health
Service guidelines for the
one who requests testing (9). Per- ered safe, and is approved by the management of occupa-
sons whose blood or body uid U.S. Food and Drug Administra- tional exposures to human
immunodeciency virus
is the source of an occupational tion for this purpose (16). An esti- and recommendations for
or a nonoccupational exposure mated 1.2 million people in the
postexposure prophylaxis.
Infect Control Hosp Epide-
should be informed of the inci- United States are eligible for miol. 2013;34:875-92.
[PMID: 23917901]
dent, and a request to be tested PrEP, specically 1 in 4 MSM, 1 in 13. Centers for Disease Control
for HIV should be made at the 5 PWIDs, and 1 in 200 heterosex- and Prevention (CDC).
Prevalence and awareness
time of exposure. Assessment of uals (17). In May 2014, the U.S. of HIV infection among
potential occupational exposure Public Health Service released
men who have sex with
men21 cities, United
to HIV should follow the U.S. Pub- States, 2008. MMWR
clinical practice guidelines as Morb Mortal Wkly Rep.
lic Health Service guidelines, in-
well as a clinical providers' sup- 2010;59:1201-7. [PMID:
cluding PrEP provision as indi- 20864920]
plement that highlights certain 14. Ford CL, Whetten KD, Hall
cated (11, 12). SA, Kaufman JS, Thrasher
behavioral risk factors that are AD. Black sexuality, social
How frequently should persons clear indications for prescribing construction, and research
targeting The Down Low
at risk be tested? PrEP. Although PrEP is a powerful (The DL). Ann Epidemiol.
All potentially high-risk persons prevention tool, 1 in 3 primary 2007;17:209-16. [PMID:
17320787]
should be retested at least annu- care physicians and nurses are 15. Millett GA, Peterson JL,
Flores SA, Hart TA, Jeffries
ally per the 2006 recommenda- unaware of it (17). Current stud- WL 4th, Wilson PA, et al.
tions. In sexually active MSM, rou- ies are investigating products Comparisons of disparities
and risks of HIV infection
tine testing every 3 6 months and delivery methods other than in black and other men
who have sex with men in
should be considered (13). Re- pills, including vaginal rings, vag- Canada, UK, and USA: a
testing at-risk pregnant women in inal and rectal gels, vaginal lms, meta-analysis. Lancet.
2012;380:341-8. [PMID:
the third trimester will identify and long-acting injectables. 22819656]
4 July 2017 Annals of Internal Medicine In the Clinic ITC3 2017 American College of Physicians
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
Screening and Prevention... All sexually active persons aged 13 years
or older should be offered screening for HIV on an opt-out basis at least
once; high-risk persons should be retested annually. Sexually active
MSM can be retested as frequently as every 3 6 months. Persons re-
ceiving PrEP should be tested every 3 months. All pregnant women
should be offered opt-out HIV testing and receive immediate treatment
if results are positive to prevent vertical transmission.
CLINICAL BOTTOM LINE
Diagnosis and Evaluation
Which tests should be used, and decreases the window pe-
and what is the appropriate riod before antibody conversion
sequence of tests to conrm a to as little as 10 days (19). This
diagnosis of HIV infection? allows earlier initiation of ART,
According to the 2014 CDC decreasing both morbidity and
guidelines on laboratory testing the likelihood of transmission to
for HIV infection, screening starts others, which is especially high in
with the fourth-generation HIV- the setting of acute infection.
1/2 antigen/antibody combina- Positive results are followed by
tion (HIV Ag/Ab) test (Figure 1) an HIV-1/2 differentiation test.
(18). The dening benets of this The fourth-generation HIV Ag/Ab
test are that it eliminates the con- test is the most accurate in medi-
rmatory Western blot, allows cal use (>99.7% sensitivity and
detection sooner after infection, >99.3% specicity) and can iden-
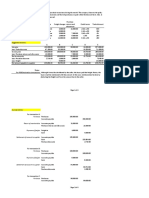
Figure 1. Centers for Disease Control and Prevention laboratory testing for HIV diagnosis from serum or plasma.*
Fourth-generation HIV-1/HIV-2 immunoassay
(+) ()
Negative for HIV-1 and HIV-2
antibodies and p24 antigen
HIV-1/HIV-2 antibody-differentiation immunoassay
HIV-1 (+) HIV-1 () HIV-1 (+) HIV-1 () or indeterminate
HIV-2 () HIV-2 (+) HIV-2 (+) HIV-2 ()
HIV-1 antibodies HIV-2 antibodies HIV antibodies
detected detected detected
RNA
RNA (+) RNA ()
Acute HIV-1 Negative for
infection HIV-1
* Updated in 2014.
Additional testing required to rule out HIV-1 and HIV-2 co-infection.
2017 American College of Physicians ITC4 In the Clinic Annals of Internal Medicine 4 July 2017
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
tify most (>80%) acute infections mononucleosis-like presentation
that would otherwise require (particularly those with a negative
RNA polymerase chain reaction result on a Monospot test) should
(PCR) conrmation (19, 20). How- be evaluated for acute HIV infec-
16. Grant RM, Lama JR,
ever, as with all screening tests, tion with a quantitative RNA PCR Anderson PL, McMahan
the predictive value of individual assay (23). Proof of seroconver- V, Liu AY, Vargas L, et al;
iPrEx Study Team. Preex-
positive or negative results de- sion typically occurs 2 6 weeks posure chemoprophy-
pends on local seroprevalence after exposure, and 99.9% of HIV- laxis for HIV prevention
in men who have sex
(21, 22). Chronic HIV infection infected patients have a positive with men. N Engl J Med.
2010;363:2587-99.
should not be diagnosed by an combination Ag/Ab test result by [PMID: 21091279]
HIV quantitative RNA PCR assay 12 weeks (18). Because risk for 17. Smith DK, Van Handel
M, Wolitski RJ, Stryker
because of the possibility of transmission is directly related to JE, Hall HI, Prejean J,
false-positive results at low viral viral load, patients with negative et al. Vital Signs: Esti-
mated Percentages and
loads (<5000 copies/mL). The results on the fourth-generation Numbers of Adults with
Indications for Preexpo-
PCR assay should only be used Ag/Ab test who may still be sure Prophylaxis to Pre-
for diagnostic purposes in the acutely infected should avoid sex vent HIV Acquisition
United States, 2015.
setting of acute infection. A spe- until they are retested. Pregnant MMWR Morb Mortal
cialist should be consulted women who develop acute HIV Wkly Rep. 2015;64:
1291-5. [PMID:
when serologic results are infection should be rapidly re- 26606148]
18. Centers for Disease Con-
inconsistent. ferred to an HIV specialist and trol and Prevention
an obstetrician experienced in (CDC). Laboratory testing
Several rapid tests have been HIV disease for immediate ART
for the diagnosis of HIV
infection: updated rec-
approved for detection of HIV (24, 25). ommendations. 27 June
2014. Accessed at http:
antibodies that can be per- //dx.doi.org/10.15620
formed on plasma and variably What symptoms and signs /cdc.23447 on 16 March
2017.
on whole blood, serum, or saliva, should prompt clinicians to 19. Chavez P, Wesolowski L,
including a new rapid HIV-1/2 consider acute or chronic HIV Patel P, Delaney K, Owen
SM. Evaluation of the
Ag/Ab test (21). Although the infection? performance of the Ab-
bott ARCHITECT HIV
sensitivity and specicity of these Acute HIV infection (also termed Ag/Ab Combo Assay. J
tests are excellent, all rapid tests acute seroconversion syn- Clin Virol. 2011;52
Suppl 1:S51-5. [PMID:
must be conrmed with the stan- drome) is a nonspecic viral syn- 21983253]
dard fourth-generation test (18). drome similar to mononucleosis, 20. Nasrullah M, Wesolowski
LG, Meyer WA 3rd, Owen
Data are currently insufcient to inuenza, and hepatitis and in- SM, Masciotra S, Vorwald
C, et al. Performance of a
recommend a single rapid HIV- cludes the common features of fourth-generation HIV
1/2 Ag/Ab test as the initial fever, fatigue, myalgia and ar- screening assay and an
alternative HIV diagnos-
assay. thralgia, lymphadenopathy, phar- tic testing algorithm.
AIDS. 2013;27:731-7.
What should clinicians do yngitis, and rash. However, the [PMID: 23135170]
range of possible presentations 21. Centers for Disease Con-
if they suspect acute HIV trol and Prevention
is wide and encompasses neuro- (CDC). False-positive oral
infection but test results
logic syndromes (meningitis, uid rapid HIV tests
are negative? encephalitis, radiculopathy),
New York City, 2005
2008. MMWR Morb
The fourth-generation HIV-1/2 hepatitis, and gastrointestinal Mortal Wkly Rep. 2008;
57:660-5. [PMID:
Ag/Ab tests can be indetermi- symptoms. If the patient's CD4 18566566]
nate or negative during serocon- count drops precipitously below
22. Kleinman S, Busch MP,
Hall L, Thomson R, Glynn
version (window period). How- 200 cells/mL, he or she may pres- S, Gallahan D, et al.
ever, in acute infection the False-positive HIV-1 test
ent with an OI that is the hallmark results in a low-risk
quantity of HIV virions in the of AIDS. screening setting of
voluntary blood dona-
blood (viral load) is extraordi- tion. Retrovirus Epidemi-
narily high often in the millions; Approximately 40%90% of per- ology Donor Study.
JAMA. 1998;280:
thus, HIV infection can be diag- sons who have seroconverted 1080-5. [PMID:
nosed by a quantitative RNA PCR have symptoms (26), but not all 9757856]
23. Vidrih JA, Walensky RP,
assay that measures the number seek medical care. Acute HIV in- Sax PE, Freedberg KA.
Positive Epstein-Barr
of copies of the virus in plasma. fection is often not recognized by virus heterophile anti-
Because acute infection often primary care and emergency body tests in patients
with primary human
mimics mononucleosis or other physicians because the symp- immunodeciency virus
acute viral illnesses, sexually ac- toms mimic those of other com- infection. Am J Med.
2001;111:192-4. [PMID:
tive or persons at risk with a mon viral illnesses (27). One 11530029]
4 July 2017 Annals of Internal Medicine In the Clinic ITC5 2017 American College of Physicians
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
study estimated the prevalence occurrence of one or more OIs or
24. Panel on Antiretroviral
Guidelines for Adults and of acute HIV infection among pa- severe immune depletion de-
Adolescents. Guidelines ned by a CD4 count less than
for the use of antiretrovi-
tients seeking care for fever or
ral agents in HIV-1- rash as 0.5% 0.7% (28). Because 200 cells/mL.
infected adults and ado-
lescents. Department of viral load in plasma and genital
Health and Human Ser- secretions is very high, acute se- Many patients tolerate waning
vices. Accessed at http: immunity fairly well until they
//aidsinfo.nih.gov roconverters have a high rate of
/contentles/lvguidelines
transmission to others and thus present emergently with a seri-
/AdultandAdolescentGL
.pdf on 16 March 2017. play a disproportionate role in ous complication that signals an
25. Panel on Treatment of AIDS diagnosis. Typically, viral
HIV-Infected Pregnant maintaining the epidemic. Thus,
Women and Prevention
there is a signicant public health loads are high in advanced dis-
of Perinatal Transmis-
sion. Recommendations benet to identifying and treat- ease, and CD4 counts are gener-
for use of antiretroviral
drugs in pregnant HIV-1- ing these individuals as soon as ally far less than 200 cells/mL.
infected women for ma- possible (29). Late diagnosis is still the rule
ternal health and inter-
ventions to reduce rather than the exception; in
perinatal HIV transmis- Chronic HIV infection has a pro- 2014, 23% of persons who tested
sion in the United States.
Accessed at https://aids tean range of presentations, with positive for HIV in the United
info.nih.gov/contentles some dependence on the stage States were concurrently diag-
/lvguidelines/perinatalgl
.pdf on 16 March 2017. of disease. Throughout the nosed with AIDS (29).
26. Kahn JO, Walker BD.
Acute human immuno-
course of HIV infection, lymph-
deciency virus type 1 adenopathy waxes and wanes The most common OIs include
infection. N Engl J Med.
1998;339:33-9. [PMID: and thus is not an accurate clini- Pneumocystis pneumonia,
9647878]
27. Weintrob AC, Giner J,
cal marker of disease stage. In esophageal candidiasis, crypto-
Menezes P, Patrick E, fact, many patients are diag- coccal meningitis, and toxo-
Benjamin DK Jr, Lennox
J, et al. Infrequent diag- nosed with HIV when lymph plasma encephalitis. Most pa-
nosis of primary human node biopsies for possible lym- tients with AIDS and an acute OI
immunodeciency virus
infection: missed oppor- phoma are read as reactive. are sick enough to warrant hospi-
tunities in acute care
settings. Arch Intern
Many have minor, nonspecic talization. Interestingly, Kaposi
Med. 2003;163:2097- skin problems, such as folliculitis sarcoma, the opportunistic can-
100. [PMID: 14504125]
28. Coco A, Kleinhans E. or seborrhea; recurrent episodes cer that was one of the original
Prevalence of primary of candida vaginitis are fre-
HIV infection in symp- hallmarks of AIDS in the early
tomatic ambulatory pa- quently the rst manifestation of 1980s, has for unknown reasons
tients. Ann Fam Med.
2005;3:400-4. [PMID: HIV disease in women (30). Obvi- become relatively rare. However,
16189055] ously, these conditions also occur other types of cancer, including
29. Centers for Disease Con-
trol and Prevention in HIV-negative persons, but it is B-cell lymphoma, Hodgkin dis-
(CDC). Late versus early
testing of HIV16 Sites,
important to consider HIV infec- ease, and central nervous system
United States, 2000 tion in the differential diagnosis lymphoma, do occur in patients
2003. MMWR Morb
Mortal Wkly Rep. 2003; and recommend testing. Some with AIDS.
52:581-6. [PMID: laboratory abnormalities, such as
12836626]
30. Aberg JA, Kaplan JE, an unexplained low platelet Which laboratory tests and
Libman H, Emmanuel P, evaluations are indicated in a
Anderson JR, Stone VE, count or low lymphocyte fraction,
et al; HIV Medicine Asso- should trigger an HIV test. Ill- patient with newly diagnosed
ciation of the Infectious
Diseases Society of Amer- nesses that cause disease in HIV- disease?
ica. Primary care guide-
lines for the manage-
negative persons with intact im- As measures of immune function
ment of persons infected mune responses may occur in and viral activity, respectively,
with human immunode-
ciency virus: 2009 HIV-positive persons at relatively CD4 cell count and HIV viral load
update by the HIV Medi- well-preserved CD4 (T-helper)
cine Association of the
are surrogate markers of disease
Infectious Diseases Soci- cell counts, including tuberculo- with proven value for determin-
ety of America. Clin In-
fect Dis. 2009;49:651- sis and bacterial pneumonia (es- ing prognosis, clinical staging,
81. [PMID: 19640227] pecially pneumococcal disease). and monitoring response to
31. Mellors JW, Munoz A,
Giorgi JV, Margolick JB, Oral thrush is frequently present treatment (31, 32). These tests
Tassoni CJ, Gupta P,
et al. Plasma viral load
as CD4 counts drop below 350 are done at the start of care and
and CD4+ lymphocytes cells/mL. Unexplained weight repeated at regular intervals
as prognostic markers of
HIV-1 infection. Ann loss, fever, and night sweats are throughout follow-up. An HIV-
Intern Med. 1997;126: common nonspecic symptoms resistance test should be done at
946-54. [PMID:
9182471] of AIDS, which is dened by the diagnosis because the overall
2017 American College of Physicians ITC6 In the Clinic Annals of Internal Medicine 4 July 2017
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
Recommended Laboratory Tests for Newly Diagnosed HIV Infection*
HIV tests: HIV serology; CD4 cell percentage and absolute number (requires con-
comitant CBC and differential); plasma HIV RNA level; HIV genotype (resistance test)
Possible additional HIV tests: HLA-B*5701 if considering abacavir; coreceptor tro-
pism assay if considering CCR5 entry inhibitor
Other key tests: CBC with differential; serum chemistries to include measurement of
electrolytes, renal and hepatic function, fasting blood glucose or hemoglobin A1c
level, fasting lipid level, and vitamin D level and complete urinalysis
Co-infection and comorbidity tests: Screening for tuberculosis by puried protein
derivative or interferon-release assays (QuantiFERON [Qiagen] or T-SPOT [Oxford
Immunotec]) and, if positive, chest radiography; screening for syphilis, chlamydia, and
gonorrhea; screening for viral hepatitis (hepatitis B surface antigen and antibody,
hepatitis B core antibody, hepatitis A IgG, hepatitis C antibody); cervical Papanicolaou
(Pap) test, and anal Pap test if indicated
Possible additional co-infection and comorbidity tests: Pregnancy test in women
of childbearing age before starting or changing antiretroviral therapy; total and free
testosterone in men with fatigue, weight loss, depression, loss of libido, absence or
diminished frequency of erection on awakening, erectile dysfunction, or evidence of
reduced bone mineral density; testosterone level in women with loss of libido;
glucose-6-phosphate dehydrogenase for persons of Mediterranean ancestry who
may have absolute enzyme deciency; toxoplasma IgG; cytomegalovirus IgG,
varicella-zoster IgG in persons without a history of chickenpox or shingles;
dual-energy x-ray absorptiometry for bone mineral density, as indicated
Women should receive a Pap smear twice in the rst year of care and then annually if initial
results are negative. Although there is increased risk for anal dysplasia and carcinoma
among MSM with human papillomavirus infection, anal cytologic screening is not yet
the standard of care.
CBC = complete blood count; MSM = men who have sex with men.
* Adapted from reference 40.
rate of resistant infection is 10% offer such testing. Testing for a
17% (33). Risk for anal dysplasia variety of co-infections and other
and carcinoma is increased causes of comorbidity is also indi-
among MSM with human papillo- cated (see the Box: Recom-
mavirus infection. Although anal mended Laboratory Tests for
cytologic screening is not yet the Newly Diagnosed HIV Infection)
standard of care, many HIV clinics (24).
Diagnosis and Evaluation... Diagnosis of established (chronic) infec-
tion by HIV-1/2 Ag/Ab screening is highly sensitive and specic, and
this test is among the most reliable in medical practice. If acute HIV in-
fection is suspected but results are negative or indeterminate, HIV
quantitative RNA PCR assay should be used for diagnosis because sero-
conversion has not yet occurred; on retesting 4 12 weeks later, results
of the standard serologic test will be positive. Patients often present late
in the course of HIV disease (AIDS), and careful evaluation for OIs and
cancer is important in this setting.
32. Mellors JW, Rinaldo CR
Jr, Gupta P, White RM,
Todd JA, Kingsley LA.
CLINICAL BOTTOM LINE Prognosis in HIV-1 infec-
tion predicted by the
quantity of virus in
plasma. Science. 1996;
272:1167-70. [PMID:
8638160]
Treatment 33. World Health Organiza-
tion. WHO HIV Drug
Resistance Report 2012.
What are the goals of ART and reduce morbidity and prolong Geneva: World Health
Organization. Accessed at
the principles of treatment? length and quality of life. This is www.who.int/hiv/pub
Because HIV cannot be cured, accomplished by maximally and /drugresistance
/report2012 on 16
the primary goal of therapy is to durably suppressing the HIV load March 2017.
4 July 2017 Annals of Internal Medicine In the Clinic ITC7 2017 American College of Physicians
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
Figure 2. Care continuum for the 1.2 million persons in the United States
who live with HIV.
86%
62%
40%
37%
30%
Diagnosed Linked to Care Engaged in Care Prescribed ART Virally Suppressed
Adapted from reference 36. ART = antiretroviral therapy.
below the limit of detection (cur- crease the effectiveness of treat-
rently <20 copies/mL, or unde- ment and prevent or delay emer-
tectable in common parlance) gence of resistance mutations.
and improving immune function Typically, this is a combination of
by increasing the CD4 cell count. 3 drugs from at least 2 of 6 cur-
This goal was once limited to rent drug classes. Maximum sup-
previously untreated patients but pression of virus replication to
now also applies to treatment- undetectable levels (virologic
experienced patients with drug success) in a treatment-naive
resistance and/or intolerance. patient usually occurs in the rst
Increasingly better-tolerated 4 24 weeks of treatment. Predic-
drugs that are highly active tors of virologic success include
against multidrug-resistant HIV regimen potency, lower baseline
are available. Achieving these viral load, higher baseline CD4 cell
goals requires individualization count, rapid response of viremia to
of therapy and encouragement treatment, and adherence to ther-
of patients to adhere to treat- apy (24). The vast majority of pa-
34. Castilla J, Del Romero J,
Hernando V, Marincovich ment; it also has the public health tients can achieve this goal, al-
B, Garca S, Rodrguez C.
Effectiveness of highly
benet of preventing transmis- though success rates in clinical
active antiretroviral ther- sion to sex partners and neo-
apy in reducing hetero- practice tend to be lower than the
nates (vertical transmission) (34,
sexual transmission of approximate 85%90% seen in
HIV. J Acquir Immune 35). The care continuum for peo-
Dec Syndr. 2005;40:96- clinical trials. Virologic failure is
101. [PMID: 16123689] ple living with HIV in the United
dened as repeated measures of
35. Cohen M, HPTN 052 States is shown in Figure 2 (36).
Study Team. Antiretrovi- viral load greater than 200 copies/
ral treatment prevents
HIV transmission: nal The START (Strategic Timing of Antiretroviral mL; repeated measures are key in
results from the HPTN Treatment) study was the rst large, interna- determining treatment failure be-
052 randomized con-
trolled trial. Presented at tional, randomized clinical trial showing that cause some patients may have
the 8th IAS Conference earlier treatment can decrease serious AIDS transient viral load increases,
on HIV Pathogenesis,
Treatment, and Preven- events (tuberculosis, Pneumocystis pneumo- known as blips. These individuals
tion, Vancouver, Canada, nia, and AIDS-related cancer) as well as serious may then resuppress without any
2015.
36. Lundgren JD, Babiker nonAIDS-dening events (other types of can-
clinical consequences, resistance
AG, Gordin F, Emery S, cer, cardiovascular disease, and renal and liver
Grund B, Sharma S, et al;
disease) and death (36). development, or change in ART.
INSIGHT START Study
Group. Initiation of Anti- Most blips are small (50 100 cop-
retroviral Therapy in Early The cornerstone of HIV treatment ies/mL), and multiple studies have
Asymptomatic HIV Infec-
tion. N Engl J Med. is the use of multiple agents di- reported that they are relatively
2015;373:795-807. rected against different steps in common, occurring in 20% 60%
[PMID: 26192873] doi:10
.1056/NEJMoa1506816 the HIV life cycle, to both in- of patients (37, 38).
2017 American College of Physicians ITC8 In the Clinic Annals of Internal Medicine 4 July 2017
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
Drug drug interactions are a com- ommended, alternative, and
mon clinical issue that is often un- other for nonpregnant adoles-
derrecognized by nonHIV special- cents and adults and preferred
ists. As infected persons age and and alternative for pregnant
those with well-suppressed dis- women (24). Choosing among
ease visit HIV specialists less fre- them is a matter of balancing
quently, they may begin to receive drug susceptibility, convenience
drugs that are contraindicated or (pill burden, dosing frequency,
signicantly interact with ART. The food requirements, use of acid
most common and critical of these suppressants), potential adverse
are statins or topical steroids with effects and drug interactions, ad-
regimens that contain a protease herence potential, and patient
inhibitor (such as ritonavir or cobi- desire (see the Box: Treatment
cistat) and the use of metformin for Adults and Pregnant Women)
with dolutegravir. (24). Other factors to consider
during selection of an initial regi-
Treatment is lifelong, and inter-
men include pregnancy or the
ruptions should be assiduously
potential to become pregnant
avoided. Both randomized and
and comorbid conditions (cardio-
cohort studies have shown that
vascular disease, drug depen-
interrupting therapy not only por-
dence, liver or renal disease, psy-
tends a poorer outcome for HIV
disease but also increases risk for chiatric condition, hepatitis B or
nonHIV-associated end organ C, tuberculosis). Alternative regi-
disease (cardiac, renal, hepatic) mens are chosen on the same
and cancer (33). This morbidity basis when the preferred ap-
may be due in part to inamma- proaches are not effective, when
tion that results from chronic, low- they have limitations for certain
level viremia even when infection populations, or when there are
is well-controlled. fewer supporting data than for
the recommended regimens.
Prevention of transmission is an- Other regimens, when com-
other goal of treatment: By decreas- pared with recommended or al-
ing the viral load in blood and gen- ternative regimens, have de-
ital secretions, treatment reduces creased virologic activity, limited
infectiousness to others (35). supporting data in large compar-
ative trials, poorer tolerance and
The HPTN 052 trial demonstrated a 93% reduc-
tion in HIV transmission among serodiscordant
more toxicity, higher pill burden,
couples when the HIV-infected partner received increased potential for drug in-
ART and was virologically suppressed (35). This teraction, or limitations in certain
study established the concept of treatment-as- populations.
preventionthe goal of improving the cascade
of care so that as many HIV-infected persons as All antiretrovirals have the poten-
possible are virologically suppressed to greatly re- tial for short- and long-term ad-
duce the likelihood of infecting others. verse effects; the rst few weeks
are generally the most difcult.
Treatment-as-prevention is criti- Subjective adverse effects usually 37. Lee PK, Kieffer TL, Sili-
cal to containing the HIV epi- improve with time. With current ciano RF, Nettles RE.
HIV-1 viral load blips are
demic because an effective vac- well-tolerated regimens, many of limited clinical signi-
cine remains elusive after more patients do not have any adverse cance. J Antimicrob Che-
mother. 2006;57:803-5.
than 30 years of investigation. effects. [PMID: 16533823]
38. Nettles RE, Kieffer TL,
What should guide the How should clinicians monitor Kwon P, Monie D, Han Y,
Parsons T, et al. Intermit-
selection of ART? patients receiving ART? tent HIV-1 viremia (blips)
and drug resistance in
The U.S. Public Health Service The frequency of evaluation patients receiving
treatment guidelines classify should be driven by disease HAART. JAMA. 2005;
293:817-29. [PMID:
combination regimens as rec- stage and response to therapy. 15713771]
4 July 2017 Annals of Internal Medicine In the Clinic ITC9 2017 American College of Physicians
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
CD4+ cell counts are both impor-
Treatment for Adults and tant prognostic indicators and
Pregnant Women* key means of monitoring health.
Recommended for nonpregnant They disclose different aspects
adults of the patient's health status and
INSTI-based: thus have complementary value.
The viral load measures how well
DTG/ABC/3TC
DTG + TDF/FTC or TAF/ HIV replication is being sup-
FTC pressed, but it is important for
EVG/c/TAF/FTC patients to understand that un-
EVG/c/TDF/FTC detectable (viral load below the
RAL + TDF/FTC or TAF/ assay's limit of detection) does
FTC not mean cured. The CD4+ cell
PI-based: DRV/r (once daily) + count and percentage reect the
TDF/FTC or TAF/FTC restoration of immune function
as measured by recovery of
Preferred for pregnant women
T-helper cells, but an increase
PI-based:
in CD4+ cells even to normal
ATV/r + ABC/3TC or TDF/ levels does not indicate com-
FTC or TDF/3TC plete restoration of immunocom-
DRV/r (twice daily) = petence because there are other
ABC/3TC or TDF/FTC or
HIV-associated immune defects
TDF/3TC
that are not measured routinely.
INSTI-based: RAL + ABC/3TC The CD4 percentage is a better
or TDF/FTC or TDF/3TC tool to monitor long-term re-
3TC = lamivudine; ABC = aba- sponse because it is measured
cavir; ATV = atazanavir; c = directly, whereas the total CD4
with cobicistat for pharmacoki- cell count is derived from the
netic boosting; DRV = daruna- concurrent complete blood
vir; DTG = dolutegravir; EVG = count and differential and
elvitegravir; FTC = emtricit- thus can vary widely, even on the
abine; INSTI = integrase same day.
strand transfer inhibitor; PI =
protease inhibitor; r = with In general, asymptomatic per-
ritonavir for pharmacokinetic sons should have interval testing
boosting; RAL = raltegravir; of markers (CD4 cell count, viral
TAF = tenofovir alafenamide; load) every 3 6 months (30).
TDF = tenofovir disoproxil However, after 2 years of therapy
fumarate. with consistently suppressed viral
* Adapted from reference 24. loads and clinical stability, testing
Italics indicate coformulation
and visits every 6 months and
of 2 or 3 drugs as a single
tablet. ABC must not be used annual checks of the CD4 cell
in patients with positive count are usually adequate.
results on HLA-B*5701 Standard laboratory tests (uri-
testing because it indicates nalysis, renal and hepatic func-
potential for hypersensitivity
tion, and lipid and glucose lev-
reaction. Results should be
reviewed before the drug is els) should be repeated at
started. similar intervals, depending on
baseline values, drug regimen,
and comorbidities.
Viral load should be measured In patients who are symptomatic
2 8 weeks after therapy is initi- at entry to care, monitoring cer-
ated to reassure both the physi- tain clinical variables is useful to
cian and patient that the infection reassure both the patient and the
is responding and that the pa- physician. These include weight
tient is adherent. Viral load and gain, increased energy level, res-
2017 American College of Physicians ITC10 In the Clinic Annals of Internal Medicine 4 July 2017
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
olution of minor skin problems decrease below 200 cells/mL. As
and thrush, and improvement in the CD4 count decreases below
other signs and symptoms. 75 cells/mL, the risk extends to
include OIs associated with end-
What other management
stage AIDS, such as disseminated
strategies should be
Mycobacterium avium complex
incorporated into care?
and cytomegalovirus retinitis.
With prolonged survival now the
Conversely, once a patient's CD4
expectation (39), all routine pre-
count is sustained above 200
ventive and health maintenance
cells/mL for at least
strategies for adults and adoles-
3 months, primary prophylaxis as
cents are warranted. These in-
well as long-term maintenance
clude appropriate immunizations
therapy for various OIs (second-
(with special limitations on live
ary prophylaxis) can safely be
vaccines based on CD4 cell
discontinued (30).
count); smoking cessation; con-
trol of hypertension and hyperlip- Which immunizations are
idemia; minimizing cardiovascu- indicated?
lar risk factors by regular exercise Persons with HIV should receive
and a nutritious diet; preventing vaccination for pneumococcal
obesity; evaluating at-risk pa- disease when they are initially
tients for decreased bone min- diagnosed. They should also re-
eral density; and screening for ceive the routine vaccinations
cancer (cervical, anal, breast, co-
recommended for all adults;
lon, prostate) as well as screen-
however, some vaccines should
ing for infectious diseases as ap-
not be given when the CD4 39. Lewden C, Chene G,
propriate, including tuberculosis, Morlat P, Raf F, Dupon
count is below 200 cells/mL, and M, Dellamonica P, et al;
hepatitis B, and hepatitis C. Agence Nationale de
some need to be repeated (see Recherches sur le Sida et
There are no formal recommen-
the Box: Recommended Immuni- les Hepatites Virales
dations for yearly anal Pap (ANRS) CO8 APROCO-
zations for HIV-Infected Adults) COPILOTE Study Group.
screening; however, the CDC HIV-infected adults with
(24).
and the HIV Medicine Associa- a CD4 cell count greater
than 500 cells/mm3 on
tion state that anal cytologic How should clinicians counsel long-term combination
antiretroviral therapy
screening in HIV-infected MSM patients to decrease risk for reach same mortality
may become a useful preventive transmission? rates as the general
population. J Acquir
measure and anal Pap tests At the initial visit and subsequent Immune Dec Syndr.
should be considered (40). The 2007;46:72-7. [PMID:
intervals, plans for conception 17621240]
AIDS Institute of the New York 40. Panel on Opportunistic
must be discussed with both men Infections in HIV-Infected
State Department of Health has Adults and Adolescents.
and women. HIV-infected per-
published guidelines for yearly Guidelines for preven-
sons who plan to have children tion and treatment of
screening for MSM, women with opportunistic infections
should be counseled about safe in HIV-infected adults
a history of cervical cancer, and and adolescents. Centers
conception and prevention of
persons with a history of ano- for Disease Control and
vertical transmission. All HIV- Prevention, the National
genital warts (41). Institutes of Health, and
infected persons should use the HIV Medicine Associ-
Aside from ART, what male or female condoms as ap- ation of the Infectious
Diseases Society of Amer-
approaches are appropriate for propriate for barrier protection; ica. Accessed at http:
//aidsinfo.nih.gov
prevention and treatment of abstinence may be an option for /contentles/lvguidelines
some. Seronegative partners of /adult_oi.pdf on 16
OIs and other infections? March 2017.
Initiation of prophylaxis for OIs is infected persons should be rou- 41. New York State Depart-
ment of Health. HIV
determined by the absolute CD4 tinely tested for HIV every 6 12 clinical resource: human
cell count. As discussed, HIV- months and counseled to seek papillomavirus (HPV).
Accessed at www.health
infected patients are vulnerable immediate care if they develop .ny.gov/diseases/aids
/providers/standards
to AIDS-dening OIs, such as symptoms of acute seroconver- /support_services
Pneumocystis pneumonia, as sion, such as a mononucleosis- or _providers/docs/primary
_care.pdf on 17 March
their CD4 counts approach and u-like illness (23). 2017.
4 July 2017 Annals of Internal Medicine In the Clinic ITC11 2017 American College of Physicians
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
Pregnant HIV-positive women
Recommended Immuniza- should be given combination
tions for HIV-Infected Adults* ART at the time of HIV diagnosis
Streptococcus pneumoniae: and during pregnancy, with intra-
13-valent conjugate venous zidovudine administra-
(PCV13)all patients at entry
to care; when CD4 count
tion during labor and delivery
>200 cells/mL, then and prophylactic medication
23-valent polysaccharide given to the neonate for the rst
(PPV23) at least 8 weeks after 4 6 weeks. Currently recom-
receiving PCV13; then single mended ART for pregnant
PPV23 in 5 years and again at
age 65 years, not to exceed 3 women is summarized in the Box
lifetime doses (Treatment for Adults and Preg-
Inuenza vaccine (inactivated): nant Women). In the United
All patients, annually States, breastfeeding should be
Hepatitis A vaccine series: All avoided because formula is read-
MSM; patients with or at risk ily available and breast milk can
for chronic hepatitis B and/or transmit HIV. Vaginal delivery is
C infection, such as those
who inject drugs; and safe for women with a prenatal
patients with chronic liver viral load less than 1000 copies/
disease mL; women with higher viral
Hepatitis B vaccine series: All loads should have a cesarean
susceptible patients. Check section. This approach has de-
hepatitis B surface antigen
creased vertical transmission of
6 months after third dose
and revaccinate as needed HIV to fewer than 1% of babies
(consider using double dose born to infected mothers in the
for repeated vaccination) United States (25, 42). The rate of
Human papillomavirus series: congenital malformations as cap-
All patients through age 26 tured by the Antiretroviral Preg-
years; 3 doses
nancy Registry does not differ
Varicella vaccine series: All
from that of the background
susceptible patients with
CD4 count >200 cells/mL population rate; however, some
Tetanus/diphtheria/pertussis women may prefer to delay ART
vaccine: All patients; then until the second trimester.
boost with tetanus/diphtheria
vaccine every 10 years At every visit, the physician
Meningococcus: All MSM. If never should ask about symptoms of
vaccinated, use 2-dose primary STDs and discuss risk-reduction
series of MenACWY conjugate behaviors and strategies. PWIDs
vaccine at an interval of at least
should be counseled never to
2 months, and revaccinate
every 5 years reuse or share syringes, needles,
Other vaccines: Other vaccines other equipment, or water used
should be administered for drug preparation. Equipment
according to ACIP guide- that is planned to be shared
lines. Live viral vaccines should be cleaned with 10%
should not be given to
HIV-infected patients with
bleach. Use of sterile water or
CD4 count <200 cells/mL water from a reliable source is
ACIP = Advisory Committee on preferred for drug preparation.
Immunization Practices; PWIDs should clean the injection
MSM = men who have sex site with a new alcohol swab and
42. Thea DM, Steketee RW, with men. not lick the needle. PWIDs
Pliner V, Bornschlegel K,
Brown T, Orloff S, et al.
* Adapted from reference 40. The should be referred to syringe ser-
The effect of maternal most up-to-date information
viral load on the risk of can be found at the ACIP's
vices programs, if available.
perinatal transmission of
Web site: www.cdc.gov
HIV-1. New York City
/vaccines/hcp/acip-recs
The CDC recommends adminis-
Perinatal HIV Transmis-
sion Collaborative Study /vacc-specic/index.html. tration of triple-drug therapy for
Group. AIDS. 1997;11: 4 weeks to health care and labo-
437-44. [PMID:
9084790] ratory workers and all other per-
2017 American College of Physicians ITC12 In the Clinic Annals of Internal Medicine 4 July 2017
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
sons who have had penetrating and prevent, diagnose, and
injury, such as a needlestick from manage OIs and opportunistic
an HIV-positive patient or a pa- cancers; a baseline genotype
tient of unknown serostatus (12). indicating drug-resistant HIV;
persistently elevated viral loads
What are the special
indicating virologic failure; clini-
gynecologic and obstetric
cal deterioration regardless of
considerations for women
virologic response; the potential
diagnosed with HIV? for antiretroviral toxicity that af-
Because gynecologic problems fects health, quality of life, and
are common and cervical carci- functioning and/or adherence;
noma is an AIDS-dening condi- potential drug drug interactions
tion, complete gynecologic and necessitating a change in ther-
obstetric history, comprehensive apy; and ART begun during treat-
gynecologic assessment at entry ment of an acute OI or other ill-
to care, interval examination, and ness requiring hospitalization. A
Pap smears are indicated. Preg-
specialist should also be con-
nancy does not accelerate the
sulted if the primary provider is
course of HIV disease, and verti-
not comfortable with the pa-
cal transmission can be pre-
tient's management for any rea-
vented. All pregnant women
son. Although a recent study has
should ideally be comanaged
shown benet to starting ART
with an obstetrician experienced
during therapy for most acute
in HIV disease and have viral load
OIs, experience managing multi-
testing at regular intervals
ple potential drug interactions
throughout the pregnancy to
and toxicities is required in this
guide the choice of delivery
setting as well as to determine
method (25).
the optimal timing of ART initia-
When should an HIV specialist tion to avoid immune reconstitu-
be consulted? tion syndrome, indicated by
An HIV specialist should be con- acute symptoms or frank illness
sulted for persons with a late pre- due to the rapid return of im-
sentation in order to start ART mune competence (24, 43).
Treatment... ART is the cornerstone of HIV care and should be initiated
at or near diagnosis and as soon as the patient understands what is in-
volved and indicates readiness. There are 6 preferred therapeutic op-
tions and several alternatives, which allows individualization of treat-
ment. Short- and long-term adverse effects and drug drug interactions
should be anticipated and managed proactively. Prophylaxis and treat-
ment of OIs are integral to HIV care and are determined by the absolute
CD4 cell count. With increased life expectancy, health care mainte-
nance and prevention of common age-related illnesses, such as cardio-
vascular disease, have become important. Immunization to prevent
other infections is essential. HIV-infected women should not be discour-
aged from having children; with ART, healthy pregnancies and preven-
tion of vertical transmission are possible.
CLINICAL BOTTOM LINE 43. Zolopa A, Andersen J,
Powderly W, Sanchez A,
Sanne I, Suckow C, et al.
Early antiretroviral ther-
apy reduces AIDS pro-
gression/death in indi-
viduals with acute
opportunistic infections:
a multicenter random-
ized strategy trial. PLoS
One. 2009;4:e5575.
[PMID: 19440326]
4 July 2017 Annals of Internal Medicine In the Clinic ITC13 2017 American College of Physicians
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
Practice Improvement
What measures do U.S. What do professional
stakeholders use to evaluate organizations recommend
the quality of care for regarding the care of
HIV-infected patients? HIV-infected patients?
The National HIV/AIDS Strategy There is a wealth of resources
has dened the following goals: from professional organizations,
1) to reduce the number of per- such as the HIV Medicine Associ-
sons who become infected, 2) to ation of the Infectious Diseases
increase access to care and opti- Society of America (which last
mize health outcomes for per- updated its evidence-based pri-
sons living with HIV, and 3) to mary care guidelines for HIV-
reduce HIV-related health dispar- infected persons in 2013) (45)
ities (39). The Health Resources and the American Academy of
and Services Administration has HIV Medicine, which periodically
developed the HIVQUAL-US updates its Fundamentals of HIV
program to facilitate quality im- Medicine (46). Several guidelines
provement through measure- from the U.S. Public Health Ser-
ment of key quality indicators vice are listed in the Tool Kit. The
described for the entire range recommendations contained in
of HIV care (44). this overview largely reect these
guidelines, with some amend-
ments by the authors based on
clinical experience.
44. HIVQUAL_US. Accessed
at http://hivqualus.org
on 17 March 2017.
45. Aberg JA, Gallant JE,
Ghanem KG, Emmanuel
P, Zingman BS, Horberg
MA; Infectious Diseases
Society of America. Pri-
mary care guidelines for
the management of
persons infected with
HIV: 2013 update by the
HIV Medicine Association
of the Infectious Diseases
Society of America. Clin
Infect Dis. 2014;58:1-10.
[PMID: 24343580]
46. Hardy WD, ed. Funda-
mentals of HIV Medicine.
New York: Oxford Univ
Pr; 2017.
2017 American College of Physicians ITC14 Annals of Internal Medicine 4 July 2017
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
In the Clinic Guidelines
https://www.cdc.gov/vaccines/hcp/acip-recs/vacc
Tool Kit
-specic/index.html
Vaccine guidelines from the Advisory Committee on
Immunization Practices.
https://www.cdc.gov/hiv/guidelines/testing.html
Centers for Disease Control and Prevention (CDC)
recommendations for HIV testing of adolescents,
adults, and pregnant women.
Management https://www.cdc.gov/hiv/risk/pep/index.html
of Newly 2016 guidelines on pre- and posteexposure prophylaxis
from the CDC.
Diagnosed https://aidsinfo.nih.gov/guidelines/html/1/adult-and
-adolescent-treatment-guidelines/0/
HIV Infection Guidelines for adults and adolescents from the National
Institutes of Health (NIH).
https://aidsinfo.nih.gov/guidelines/html/3/perinatal
-guidelines/0/#
Guidelines for perinatal care and prevention of vertical
IntheClinic
transmission from the NIH.
https://aids.nlm.nih.gov/
HIV-related topics from the NIH.
www.who.int/hiv/pub/guidelines/en/
Guidelines from the World Health Organization,
including self-testing and partner notication.
Patient Information
https://www.cdc.gov/hiv/basics/index.html
HIV basics from the CDC.
https://www.aids.gov/hiv-aids-basics/
Information on federal HIV programs, funding, and
services for newly diagnosed patients.
https://www.cdc.gov/hiv/pdf/prep_gl_patient
_factsheet_acute_hiv_infection_english.pdf
Information from the CDC.
www.mayoclinic.org/diseases-conditions/hiv-aids
/basics/denition/con-20013732
Many useful pages from the Mayo Clinic for the patient or
health care provider concerning HIV.
http://hivinsite.ucsf.edu/InSite?page=li-04-22
Comprehensive information from the University of
California, San Francisco.
www.aidsmap.com/translations/es/Folletos-Booklets
/page/1412531/
Booklets to help patients with HIV in several languages.
4 July 2017 Annals of Internal Medicine ITC15 2017 American College of Physicians
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
WHAT YOU SHOULD In the Clinic
Annals of Internal Medicine
KNOW ABOUT NEWLY
DIAGNOSED HIV INFECTION
What Is HIV?
HIV (human immunodeciency virus) makes it dif-
cult for your body to ght infection. When the
immune system becomes badly damaged, HIV
develops into AIDS (acquired immunodeciency
syndrome). There is no cure for HIV or AIDS, but
highly effective treatment is available and, if
used regularly, can permit people of all ages
with HIV infection to live a normal lifespan.
Treatment of a pregnant woman with HIV infec-
tion prevents her baby from becoming infected.
HIV is passed through bodily uids, such as blood,
semen, and breast milk, in the following ways:
By having anal and/or vaginal sex with an HIV-
infected person, especially without using a condom
By sharing needles with an HIV-infected person
By being stuck by a needle or sharp object
contaminated with HIV
From mother to child during pregnancy, birth, the United States or in countries where donated
or breastfeeding. blood has not been screened for HIV
People with high-risk sex partners.
What Are the Warning Signs? You should talk to your doctor about taking HIV
Acute HIV occurs 2 to 4 weeks after you become preexposure prophylaxis (PrEP) if you are not
infected. Symptoms may be mild, and you may infected with HIV but are at high risk. PrEP in-
not even notice them. Common symptoms are volves taking HIV medicines every day and is
similar to the u and may include fatigue (tired- highly effective. Whether to use postexposure
ness); sore throat; swollen glands in the neck, prophylaxis (PEP) should be discussed with your
armpits, and groin; fever; and rash. doctor if a high-risk exposure occurs, such as a
Chronic HIV infection is the second stage, during condom breaking during sex.
which symptoms may not appear again for many
years. When they do, they may include swollen How Is It Diagnosed?
Patient Information
lymph nodes, shingles, and anemia or low plate- HIV can be diagnosed through blood and saliva
lets. Vaginal yeast infections may keep coming tests, most of which can detect HIV between 2
back. However, these problems also occur in peo- and 12 weeks after infection.
ple who do not have HIV infection.
Who Should Be Tested? How Is It Treated?
HIV is controlled by a combination of at least 3 drugs,
Health care professionals should offer HIV testing to known as antiretroviral therapy (ART). You must take
anyone who requests it, and everyone should be them for the rest of your life to stay healthy.
tested at least once. All pregnant women should Talk to your doctor about other things you can do to
also be offered testing, usually twice during the help stay healthy, such as eating nutritious foods
pregnancy. If you are at high risk for HIV infection, and getting all recommended immunizations.
you should be offered testing at least once a year.
People who are at high risk for getting HIV are: Questions for My Doctor
Men who have sex with men
Men and women who have unprotected sex How will HIV affect my day-to-day life?
with many people What is the best treatment for me?
Persons who currently or in the past have used Does the treatment have side effects?
injection drugs How can I avoid spreading HIV to others?
Men and women who pay or receive money for sex How active can I be?
Men or women who receive anal sex Can I have sex despite the infection?
People being treated for other sexually How often should I see my doctor?
transmitted diseases (STDs) Can HIV be prevented?
People who were treated for hemophilia or had If I think I've been exposed to HIV, what
blood transfusions between 1978 and 1985 in should I do?
For More Information
MedlinePlus
https://medlineplus.gov/hivaids.html
Centers for Disease Control and Prevention
www.cdc.gov/actagainstaids/basics
U.S. Department of Health and Human Services
www.aids.gov/hiv-aids-basics
Downloaded From: https://annals.org/pdfaccess.ashx?url=/data/journals/aim/936340/ by a Columbia University User on 07/03/2017
Anda mungkin juga menyukai
- VIH Diagnóstico Reciente in The Clinic PDFDokumen16 halamanVIH Diagnóstico Reciente in The Clinic PDFFernando ArancibiaBelum ada peringkat
- Lo Más NuevoDokumen16 halamanLo Más Nuevorqr5rsnhq6Belum ada peringkat
- Hepatitis C Virus: Annals of Internal MedicineDokumen17 halamanHepatitis C Virus: Annals of Internal MedicineMax CamargoBelum ada peringkat
- Rapid Routine Hiv Testing For Psychiatric Inpatients 2155 6113 1000555Dokumen5 halamanRapid Routine Hiv Testing For Psychiatric Inpatients 2155 6113 1000555Elisa BaronBelum ada peringkat
- J Annemergmed 2017 01 018Dokumen14 halamanJ Annemergmed 2017 01 018Jorge BarriosBelum ada peringkat
- Vih Ingreso Al Cuidado VihDokumen15 halamanVih Ingreso Al Cuidado Vihsamuro625Belum ada peringkat
- Vih GuidlineDokumen21 halamanVih GuidlineDavid MonroyBelum ada peringkat
- Goldschmidt Final AfpDokumen10 halamanGoldschmidt Final AfpDiego Fernando Escobar GarciaBelum ada peringkat
- Recommendations For Human Immunodeficiency Virus Screening, Prophylaxis, and Treatment For Pregnant Women in The United StatesDokumen14 halamanRecommendations For Human Immunodeficiency Virus Screening, Prophylaxis, and Treatment For Pregnant Women in The United StateselaBelum ada peringkat
- Khawcharoenporn2014 PDFDokumen10 halamanKhawcharoenporn2014 PDFsinta belaBelum ada peringkat
- Prevention of Infection in Patients With Cancer Evidence Based Nursing InterventionsDokumen10 halamanPrevention of Infection in Patients With Cancer Evidence Based Nursing InterventionsAkshayBelum ada peringkat
- Recommendations For Human Immunodeficiency Virus Screening, Prophylaxis, and Treatment For Pregnant Women in The United StatesDokumen14 halamanRecommendations For Human Immunodeficiency Virus Screening, Prophylaxis, and Treatment For Pregnant Women in The United StateselaBelum ada peringkat
- New Guidelines On HIV Prevention in Teens and AdultsDokumen1 halamanNew Guidelines On HIV Prevention in Teens and AdultsFadhilah M. YanuarBelum ada peringkat
- Tuberculosis Internal MedicineDokumen16 halamanTuberculosis Internal MedicineAdamary MerinoBelum ada peringkat
- Predicting Adherence To Antiretroviral Therapy Among Pregnant Women in Guyana: Utility of The Health Belief ModelDokumen10 halamanPredicting Adherence To Antiretroviral Therapy Among Pregnant Women in Guyana: Utility of The Health Belief ModelRiska Resty WasitaBelum ada peringkat
- Neumonia 2022Dokumen18 halamanNeumonia 2022Lele0407Belum ada peringkat
- Jorgensen 2017Dokumen6 halamanJorgensen 2017jessicapxeBelum ada peringkat
- VIHDokumen34 halamanVIHAndres Felipe Iglesias RealesBelum ada peringkat
- Sociodemographic Characteristics of Patients With Advanced HIV Disease in Enugu, South-East Nigeria: A Retrospective Analysis of Program DataDokumen6 halamanSociodemographic Characteristics of Patients With Advanced HIV Disease in Enugu, South-East Nigeria: A Retrospective Analysis of Program DataInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- 2016 Antifungal Agent Full PDFDokumen16 halaman2016 Antifungal Agent Full PDFyeni novi yantiBelum ada peringkat
- Arv 2010 UsDokumen14 halamanArv 2010 UsGuide LPBelum ada peringkat
- Diarrea InfecciosaDokumen36 halamanDiarrea InfecciosaIsabel VegaBelum ada peringkat
- BundleDokumen1 halamanBundleNicen SuherlinBelum ada peringkat
- Idsa Infectious DiarrheaDokumen36 halamanIdsa Infectious DiarrheastephaniesugihartoBelum ada peringkat
- Paediatrica IndonesianaDokumen9 halamanPaediatrica IndonesianaFika FebrianaBelum ada peringkat
- Effects of Adherence To Antiretroviral Therapy On Body Mass Index, Immunological and Virological Status of Nigerians Living With HIV/AIDSDokumen4 halamanEffects of Adherence To Antiretroviral Therapy On Body Mass Index, Immunological and Virological Status of Nigerians Living With HIV/AIDSDavidBelum ada peringkat
- Public Health - Vol 2 - Issue 4 - Article 5Dokumen44 halamanPublic Health - Vol 2 - Issue 4 - Article 5kaisamerno2003Belum ada peringkat
- Hiv 09 58Dokumen13 halamanHiv 09 58dewiBelum ada peringkat
- Discontinuation From Antiretroviral Therapy: A Continuing Challenge Among Adults in HIV Care in Ethiopia: A Systematic Review and Meta-AnalysisDokumen20 halamanDiscontinuation From Antiretroviral Therapy: A Continuing Challenge Among Adults in HIV Care in Ethiopia: A Systematic Review and Meta-AnalysisMamanya Fadhil HaniBelum ada peringkat
- Guidance On The Management of HIV-infected Healthcare Workers in The Philippines 2017Dokumen21 halamanGuidance On The Management of HIV-infected Healthcare Workers in The Philippines 2017psmid-webBelum ada peringkat
- Rapid AdviceDokumen44 halamanRapid AdviceJuhu NakaBelum ada peringkat
- Sample PresentationDokumen36 halamanSample Presentationmuhammed essaBelum ada peringkat
- Tropical Med Int Health - 2023 - Daltro - Virological Failure and Adherence To Antiretroviral Therapy in Adolescents andDokumen13 halamanTropical Med Int Health - 2023 - Daltro - Virological Failure and Adherence To Antiretroviral Therapy in Adolescents andCliff Daniel DIANZOLE MOUNKANABelum ada peringkat
- New England Journal Medicine: The ofDokumen13 halamanNew England Journal Medicine: The ofIndah RahmaBelum ada peringkat
- HIV Prevention in Primary Care Practice: A PrEP PrimerDari EverandHIV Prevention in Primary Care Practice: A PrEP PrimerBelum ada peringkat
- Recommendations and Reports OI - HIVDokumen323 halamanRecommendations and Reports OI - HIVJevie KairupanBelum ada peringkat
- The Role of a Pharmacist in the Analysis of Adherence Rates and Associated Factors in HIV-Patients Registered on Centralized Chronic Medicines Dispensing and Distribution (CCMDD) Programme in the Public Sector in South AfricaDokumen11 halamanThe Role of a Pharmacist in the Analysis of Adherence Rates and Associated Factors in HIV-Patients Registered on Centralized Chronic Medicines Dispensing and Distribution (CCMDD) Programme in the Public Sector in South AfricaSabrina JonesBelum ada peringkat
- BIDMC HIV Manual 2019Dokumen97 halamanBIDMC HIV Manual 2019oluBelum ada peringkat
- DMFT Study (Decayed, Missing, and Filled Teeth) in HIV Seropositive Patients: Case-ControlDokumen3 halamanDMFT Study (Decayed, Missing, and Filled Teeth) in HIV Seropositive Patients: Case-ControlEduardo J. S. HonoratoBelum ada peringkat
- HIV Screening USPTFDokumen21 halamanHIV Screening USPTFhivpolicyyesBelum ada peringkat
- Addressing Cancer Survivorship Care Under COVID 19 P - 2021 - American JournalDokumen5 halamanAddressing Cancer Survivorship Care Under COVID 19 P - 2021 - American JournalEstreLLA ValenciaBelum ada peringkat
- Lester 2010Dokumen8 halamanLester 2010Riska Resty WasitaBelum ada peringkat
- Civ 028Dokumen9 halamanCiv 028Deah RisbaBelum ada peringkat
- HIV Care Cascade Among Cisgender MenDokumen11 halamanHIV Care Cascade Among Cisgender MenAnonymousPlatypusBelum ada peringkat
- Journal of Clinical Tuberculosis and Other Mycobacterial DiseasesDokumen16 halamanJournal of Clinical Tuberculosis and Other Mycobacterial DiseasesIlna RamadhaniBelum ada peringkat
- Rubin2013 ImunisasiDokumen57 halamanRubin2013 ImunisasiIma SoniaBelum ada peringkat
- 6371 Measuring Stigma and Discrimination Towards People Living With Hiv Among Health Care Workers in A Tertiary Government Teaching Hospital in The PhilippinesDokumen9 halaman6371 Measuring Stigma and Discrimination Towards People Living With Hiv Among Health Care Workers in A Tertiary Government Teaching Hospital in The PhilippinesCamia SinagdaBelum ada peringkat
- PMTCT Service Uptake Among Pregnant Women in 3 Internally Displace Persons Camps in Borno State Northeast NigeriaDokumen6 halamanPMTCT Service Uptake Among Pregnant Women in 3 Internally Displace Persons Camps in Borno State Northeast NigeriaSunkanmi FadojuBelum ada peringkat
- International Journal of Infectious Diseases: SciencedirectDokumen5 halamanInternational Journal of Infectious Diseases: SciencedirectMuh Syukriadi AnsarBelum ada peringkat
- Risk FactorDokumen5 halamanRisk FactorBima AryaputraBelum ada peringkat
- 10.1016@j.ijhydene. - 2017Dokumen1 halaman10.1016@j.ijhydene. - 2017Mr Mathavan SBelum ada peringkat
- 655 FullDokumen8 halaman655 FullDonny ArdyanBelum ada peringkat
- Perceptions Dynamics About Antiretroviral Treatment Among HIV Patients in BaliDokumen8 halamanPerceptions Dynamics About Antiretroviral Treatment Among HIV Patients in BaliIJPHSBelum ada peringkat
- Whittaker Et Al-2022-Scientific ReportsDokumen22 halamanWhittaker Et Al-2022-Scientific ReportsAlex WhittakerBelum ada peringkat
- Actualizacion en El Manejo de Pctes Vih en Anestesia y UciDokumen9 halamanActualizacion en El Manejo de Pctes Vih en Anestesia y UciPierina VeramatosBelum ada peringkat
- NIH Public Access: Author ManuscriptDokumen8 halamanNIH Public Access: Author ManuscriptMona HelouBelum ada peringkat
- Preventive Medicine Reports: Samuel R. Bunting, Brian A. Feinstein, Aniruddha Hazra, Neeral K. Sheth, Sarah S. GarberDokumen9 halamanPreventive Medicine Reports: Samuel R. Bunting, Brian A. Feinstein, Aniruddha Hazra, Neeral K. Sheth, Sarah S. GarberKnowledge PepalaBelum ada peringkat
- Media Release - Inaugural Global Scientific Strategy Towards An HIV Cure Launched Ahead of The XIX International AIDS Conference in Washington DCDokumen7 halamanMedia Release - Inaugural Global Scientific Strategy Towards An HIV Cure Launched Ahead of The XIX International AIDS Conference in Washington DCLaura Lopez GonzalezBelum ada peringkat
- Understanding The Gaps in DR TB Care Casc - 2020 - Journal of Clinical TuberculoDokumen16 halamanUnderstanding The Gaps in DR TB Care Casc - 2020 - Journal of Clinical TuberculoKarina ChristantoBelum ada peringkat
- The Vaccine Handbook: A Practical Guide for Clinicians, Twelfth EditionDari EverandThe Vaccine Handbook: A Practical Guide for Clinicians, Twelfth EditionBelum ada peringkat
- Top 10 Myths Regarding The Diagnosis and Treatment of CellulitisDokumen8 halamanTop 10 Myths Regarding The Diagnosis and Treatment of CellulitisRoberto López MataBelum ada peringkat
- 2017 ACC Expert Consensus Decision Pathway For Optimization of Heart Failure TreatmentDokumen30 halaman2017 ACC Expert Consensus Decision Pathway For Optimization of Heart Failure TreatmentRoberto López MataBelum ada peringkat
- Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of The 2017 American College of Cardiology:American Heart Association Hypertension GuidelineDokumen10 halamanPrevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Synopsis of The 2017 American College of Cardiology:American Heart Association Hypertension GuidelineRoberto López MataBelum ada peringkat
- Hyperglycemic CrisisDokumen9 halamanHyperglycemic CrisisRoberto López MataBelum ada peringkat
- HTN Emergencies and UrgenciesDokumen14 halamanHTN Emergencies and UrgenciesRoberto López MataBelum ada peringkat
- Best Clinical Practice: AnaphylaxisDokumen6 halamanBest Clinical Practice: AnaphylaxisputriBelum ada peringkat
- ADA 2018 Diabetes CareDokumen150 halamanADA 2018 Diabetes CareRoberto López Mata100% (1)
- The Use of Cephalosporins in Penicillin-Allergic Patients - A Literature ReviewDokumen9 halamanThe Use of Cephalosporins in Penicillin-Allergic Patients - A Literature ReviewRoberto López MataBelum ada peringkat
- The Role of Nitroglycerin and Other Nitrogen Oxides in Cardiovascular TherapeuticsDokumen18 halamanThe Role of Nitroglycerin and Other Nitrogen Oxides in Cardiovascular TherapeuticsRoberto López MataBelum ada peringkat
- Uric Acid Is A Strong Risk Marker For Developing Hypertension From PrehypertensionDokumen16 halamanUric Acid Is A Strong Risk Marker For Developing Hypertension From PrehypertensionRoberto López MataBelum ada peringkat
- Update On The Management of Venous ThromboembolismDokumen8 halamanUpdate On The Management of Venous ThromboembolismRoberto López MataBelum ada peringkat
- Diagnosis and Treatment of HyperkalemiaDokumen9 halamanDiagnosis and Treatment of HyperkalemiaRoberto López MataBelum ada peringkat
- Necrotizing Soft-Tissue InfectionsDokumen13 halamanNecrotizing Soft-Tissue InfectionsRoberto López MataBelum ada peringkat
- Pathophysiology of Septic ShockDokumen19 halamanPathophysiology of Septic ShockRoberto López MataBelum ada peringkat
- Fluid Therapy Options and Rational SelectionDokumen13 halamanFluid Therapy Options and Rational SelectionRoberto López MataBelum ada peringkat
- Atrial Fibrillation and HypertensionDokumen17 halamanAtrial Fibrillation and HypertensionRoberto López MataBelum ada peringkat
- Hepatitis B Vaccination, Screening, and Linkage To Care - Best Practice Advice From The American College of Physicians and The Centers For Disease Control and PreventionDokumen12 halamanHepatitis B Vaccination, Screening, and Linkage To Care - Best Practice Advice From The American College of Physicians and The Centers For Disease Control and PreventionRoberto López MataBelum ada peringkat
- The Dark Sides of Fuid Administration in The Critically Ill PatientDokumen3 halamanThe Dark Sides of Fuid Administration in The Critically Ill PatientRoberto López MataBelum ada peringkat
- Sudden Cardiac Arrest During Participation in Competitive SportsDokumen11 halamanSudden Cardiac Arrest During Participation in Competitive SportsRoberto López MataBelum ada peringkat
- 2015 ESC Guidelines For The Diagnosis and Management of Pericardial DiseasesDokumen44 halaman2015 ESC Guidelines For The Diagnosis and Management of Pericardial DiseasesRoberto López MataBelum ada peringkat
- A Test in Context - D-DimerDokumen10 halamanA Test in Context - D-DimerRoberto López MataBelum ada peringkat
- Diuretic Treatment in Heart FailureDokumen12 halamanDiuretic Treatment in Heart FailureRoberto López Mata100% (1)
- Rivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeDokumen10 halamanRivaroxaban Vs Warfarin Sodium in The Ultra-Early Period After Atrial Fibrillation-Related Mild Ischemic StrokeRoberto López MataBelum ada peringkat
- Acute Monocular Vision LossDokumen9 halamanAcute Monocular Vision LossRoberto López MataBelum ada peringkat
- Evaluation and Management of Lower-Extremity UlcersDokumen9 halamanEvaluation and Management of Lower-Extremity UlcersRoberto López MataBelum ada peringkat
- Effects of Acarbose On Cardiovascular and Diabetes Outcomes in Patients With Coronary Heart Disease and Impaired Glucose Tolerance (ACE) - A Randomised, Double-Blind, Placebo-Controlled TrialDokumen10 halamanEffects of Acarbose On Cardiovascular and Diabetes Outcomes in Patients With Coronary Heart Disease and Impaired Glucose Tolerance (ACE) - A Randomised, Double-Blind, Placebo-Controlled TrialRoberto López MataBelum ada peringkat
- Effects on the Incidence of Cardiovascular Events of the Addition of Pioglitazone Versus Sulfonylureas in Patients With Type 2 Diabetes Inadequately Controlled With Metformin (TOSCA.it)- A Randomised, Multicentre TrialDokumen11 halamanEffects on the Incidence of Cardiovascular Events of the Addition of Pioglitazone Versus Sulfonylureas in Patients With Type 2 Diabetes Inadequately Controlled With Metformin (TOSCA.it)- A Randomised, Multicentre TrialRoberto López MataBelum ada peringkat
- Synopsis of The 2017 U.S. Department of Veterans Affairs: Management of Type 2 Diabetes MellitusDokumen10 halamanSynopsis of The 2017 U.S. Department of Veterans Affairs: Management of Type 2 Diabetes MellitusRoberto López MataBelum ada peringkat
- Dual Antithrombotic Therapy With Dabigatran After PCI in Atrial FibrillationDokumen12 halamanDual Antithrombotic Therapy With Dabigatran After PCI in Atrial FibrillationRoberto López MataBelum ada peringkat
- Xiaopan OS: DescriptionDokumen1 halamanXiaopan OS: DescriptionMan SavliBelum ada peringkat
- D904 - D906 - D914 - D916 - D924 - D926 - 8718458 - 04092008 - v02 - enDokumen218 halamanD904 - D906 - D914 - D916 - D924 - D926 - 8718458 - 04092008 - v02 - enАлексей89% (18)
- E-Catalog 2021 Jan JMI Dan KimDokumen52 halamanE-Catalog 2021 Jan JMI Dan KimbobBelum ada peringkat
- Bleeding Disorders in Pregnancy: Table 1Dokumen7 halamanBleeding Disorders in Pregnancy: Table 1KharismaNisaBelum ada peringkat
- A Single-Stage Asymmetrical Half-Bridge Flyback CoDokumen16 halamanA Single-Stage Asymmetrical Half-Bridge Flyback CoSantosh KumarBelum ada peringkat
- Three Moment Equation For BeamsDokumen12 halamanThree Moment Equation For BeamsRico EstevaBelum ada peringkat
- Itf EssayDokumen18 halamanItf EssayTharshiBelum ada peringkat
- Competency #14 Ay 2022-2023 Social StudiesDokumen22 halamanCompetency #14 Ay 2022-2023 Social StudiesCharis RebanalBelum ada peringkat
- 5 Waves AnswersDokumen2 halaman5 Waves AnswersNoor Ulain NabeelaBelum ada peringkat
- 1 Kane Equations - Example 1Dokumen8 halaman1 Kane Equations - Example 1Khisbullah HudhaBelum ada peringkat
- Healthy Body CompositionDokumen18 halamanHealthy Body CompositionSDasdaDsadsaBelum ada peringkat
- Ringleman Chart FlareDokumen12 halamanRingleman Chart FlareguhadebasisBelum ada peringkat
- Symantec Endpoint Protection 14.3 RU3 Release NotesDokumen28 halamanSymantec Endpoint Protection 14.3 RU3 Release NotesMilind KuleBelum ada peringkat
- Handout No. 03 - Purchase TransactionsDokumen4 halamanHandout No. 03 - Purchase TransactionsApril SasamBelum ada peringkat
- Selling AIESEC To Your TargetsDokumen7 halamanSelling AIESEC To Your TargetspijoowiseBelum ada peringkat
- Body LanguageDokumen17 halamanBody LanguageAR PiZaBelum ada peringkat
- State Partnership Program 101 Brief (Jan 2022)Dokumen7 halamanState Partnership Program 101 Brief (Jan 2022)Paulo FranciscoBelum ada peringkat
- Case 07-53: #REF! #REF! #REF! #REF! #REF!Dokumen6 halamanCase 07-53: #REF! #REF! #REF! #REF! #REF!saad bin sadaqatBelum ada peringkat
- Negotiation SimulationDokumen11 halamanNegotiation SimulationJade Arbee BarbosaBelum ada peringkat
- FPA 03-A.01 Permohonan Akreditasi LP LK LI LM PUP PBADokumen595 halamanFPA 03-A.01 Permohonan Akreditasi LP LK LI LM PUP PBAabimanyubawonoBelum ada peringkat
- IGCSE Religious Studies (Edexcel - 2009 - Be Careful Not To Choose The New' IGCSE)Dokumen8 halamanIGCSE Religious Studies (Edexcel - 2009 - Be Careful Not To Choose The New' IGCSE)Robbie TurnerBelum ada peringkat
- Sekonic L 758Dokumen68 halamanSekonic L 758mariosapereiraBelum ada peringkat
- How Do I Predict Event Timing Saturn Nakshatra PDFDokumen5 halamanHow Do I Predict Event Timing Saturn Nakshatra PDFpiyushBelum ada peringkat
- Global Title Format: ITU-T Recommendation Q.713Dokumen4 halamanGlobal Title Format: ITU-T Recommendation Q.713Pravesh Kumar ThakurBelum ada peringkat
- Doyennés Et Granges de L'abbaye de Cluny (A. Guerreau)Dokumen45 halamanDoyennés Et Granges de L'abbaye de Cluny (A. Guerreau)theseus11Belum ada peringkat
- Cracking Passwords GuideDokumen45 halamanCracking Passwords GuideKorben100% (6)
- Nur Syamimi - Noor Nasruddin - Presentation - 1002 - 1010 - 1024Dokumen14 halamanNur Syamimi - Noor Nasruddin - Presentation - 1002 - 1010 - 1024abdulhasnalBelum ada peringkat
- Unpriced Proposed Renovation of Bugolobi Flat, Block C For Uganda Coffee Development AuthorityDokumen39 halamanUnpriced Proposed Renovation of Bugolobi Flat, Block C For Uganda Coffee Development AuthoritynicolasBelum ada peringkat
- Thetford c250 InstallationDokumen19 halamanThetford c250 InstallationCatalin Bejan100% (1)
- Final Project Report by Himanshu Yadav Student of Fostiima Business SchoolDokumen55 halamanFinal Project Report by Himanshu Yadav Student of Fostiima Business Schoolak88901Belum ada peringkat