In-Hospital Outcomes of Methylprednisolone Pulse Therapy in The Treatment of
Diunggah oleh
Ma Azalea V LaquiJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
In-Hospital Outcomes of Methylprednisolone Pulse Therapy in The Treatment of
Diunggah oleh
Ma Azalea V LaquiHak Cipta:
Format Tersedia
Philippine Journal of Internal Medicine Original Paper
In-Hospital Outcomes of Methylprednisolone Pulse Therapy in the
Treatment of Systemic Lupus Erythematosus
Angeline-Therese D. Magbitang M.D.*; Anna Kristina Gutierrez Rubio, M.D.*; Evelyn Osio Salido, M.D.*
Abstract
Background: Methylprednisolone Pulse Therapy (MPPT) of MPPT with a mean Mex-SLEDAI score of 14.69.
is standard of care in the management of severe Infection (83%) is the most common comorbidity.
systemic lupus erythematosus (SLE). This treatment, Anemia, hypoalbuminemia and significant proteinuria
though, is considered a double-edged sword due are the most common laboratory abnormalities. The
to its life-threatening adverse effects. Renal disease, top indication for MPPT is nephritis (83.3%). The dose
liver disease and high dose of the drug are factors received by the majority (66.7%) is one gram/day
proposed to adversely affect outcomes of patients for three days, which is a high dose.
treated with MPPT. Despite the widely accepted Improvement rate is 76% but the in-hospital
use of MPPT, there are no reports describing the complication rate is 64% and mortality rate is
outcomes from its use among Filipinos with SLE. 21%. Patients with in-hospital complications have
significantly lower absolute lymphocyte count
Objective: To determine the in-hospital outcomes of (p=0.013), serum albumin (p=0.04) and greater 24-hour
patients with SLE treated with MPPT and to identify proteinuria (p=0.04) at baseline. High-dose MPPT is
factors associated with adverse outcomes. significantly associated with in-hospital complications
(p=0.04) but not mortality. Nephritis (p= 0.04) and low
General Study Design: Retrospective platelet counts at baseline (p=0.01) are associated
with mortality.
Population: Adult patients with SLE who were admitted
in Philippine General Hospital and underwent MPPT Conclusion: In this population, there is a high rate
from January 2008 to December 2012. of improvement of lupus disease activity when MPPT
is used but there is a corresponding high rate of
Methods: Patient demographics, disease characteristics in-hospital complications and mortality. High dose
on admission, indications for MPPT and in-hospital of MPPT seems to be associated with increased in-
outcomes were extracted. hospital complication, while nephritis and low platelet
count showed a probable association with mortality.
Analysis: Chi-square test and Fishers exact test were Further studies on a larger cohort are needed. For
used to elicit association of population characteristics now, the findings of this study may be helpful in
to outcomes. developing guidelines on the use of MPPT among
Filipino patients with SLE.
Results: Forty-two patients with SLE who underwent
MPPT were included. Majority are females (98%) and Keywords: methylprednisolone pulse therapy, Systemic
most (60%) underwent MPPT within one year of SLE Lupus Erythematosus, pulse steroid treatment,
diagnosis. High disease activity is seen at the time outcomes, Asian, Filipino
is believed to have an immediate profound anti-
inflammatory effect, leading to faster clinical recovery.
I ntroduction The clinical improvement is seen within 24 hours of
Methylprednisolone Pulse Therapy (MPPT) was first treatment and lasts up to around three weeks after
used in the treatment of lupus nephritis in 1976. Since one pulse. There is no prolonged suppressive effect
then, it has become essential in the management on the hypothalamic pituitary axis, which implicates
of systemic lupus erythematosus (SLE). Pulse high-dose a favorable risk/benefit ratio.1,2
steroids, paradoxically, are utilized for their steroid- Methylprednisolone Pulse Therapy has been used
sparing effect. Methylprednisolone Pulse Therapy successfully in the renal and non-renal manifestations
of lupus. Response to treatment has been favorable,
although differences in response due to racial and
*Section of Rheumatology, Department of Medicine, University of the ethnic factors have been proposed.3,4 This treatment,
Philippines-Philippine General Hospital
though, has been considered a double-edged sword
Volume 52 Number 1 January-March, 2014 1
Magbitang A, et al In-Hospital Outcomes of Methylprednisolone Pulse Therapy
due to the development of adverse effects such MPPT, and mortality. Definitions of SLE disease activity
as acute blood pressure elevations, stroke, seizures, improvement are contained in Appendix B.
arrhythmia and acute coronary events, which may We used means and proportions to describe the
be life-threatening. 5-8 Several factors have been population characteristics and outcomes. We determined
postulated to predict the occurrence of poor outcome, association between population characteristics and
such as renal disease and presence of laboratory outcomes using, chi-square test and Fishers exact
abnormalities. 9,10 The dose of MPPT has also been test. The differences in baseline Mex-SLEDAI score and
proposed to influence the outcomes of treatment. The laboratory values between those who did and did
dosing regimen of MPPT in SLE is not clearly defined. not develop complications and between those who
MPPT is usually administered at a dose of 500 to died and those who improved were reported using
1000 mg/day; the arbitrary definition of pulse steroid T-test.
therapy being any dose greater than or equal to
250 mg prednisone equivalent given in discontinuous
intravenous (IV) infusions. 1
R esults
Despite the widely accepted use of MPPT in the Patient characteristics
treatment of SLE, the experience and outcomes of There were 42 SLE patients, treated with MPPT
Filipino SLE patients treated with methylprednisolone anytime during the period January 2008 to December
pulse therapy have not been clearly documented. 2012, who were included in the study. Table I
There are no guidelines, about how it should be summarizes the demographics of this population.
administered, that are tailored for our patient The majority of the patients were females with
population. Given the observed differences in treatment no smoking or alcohol history. The mean BMI was
responses that are attributed to race and ethnicity, 20.8 kg/m2 (SD 11.42). Almost all had concomitant
we deem it worthwhile to report our experience with conditions at the time of MPPT; the most common
this mode of therapy. The objectives, therefore, of this were infections (83.3%), hypertension (31%), transaminitis
study are to determine the in-hospital outcomes of (14.3%), antiphospholipid antibody syndrome (11.9%),
patients with SLE treated with MPPT and to identify and hypothyroidism (9.5%)
factors associated with adverse outcomes.
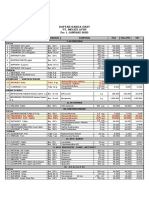
Table I: Patient demographics
M ethods Demographics n=42 Frequency(%)
Female 41 (98)
We conducted a retrospective study of charts of
Smoker (n=34) 3 (9)
patients diagnosed with SLE, who fulfilled the 1982 With alcohol intake (n=34) 2 (6)
American College of Rheumatology (ACR) criteria for With comorbid conditions 39 (93)
SLE diagnosis, aged 19 years and above, who were Infection 35 (83)
admitted at the Philippine General Hospital (PGH), Hypertension 13 (31)
Transaminitis 6 (14)
which is the largest tertiary government hospital in
Anti-phospholipid antibody syndrome 5 (12)
the country, anytime during the period January 2008 Hypothyroidism 4 (10)
to December 2012 and completed MPPT. We defined Pregnancy 3 (7)
MPPT as treatment with either 500 mg or one gram Chronic kidney disease 2 (5)
of methylprednisolone given intravenously once daily Cerebrovascular disease 2 (5)
Heart disease 2 (5)
for three days. We utilized non-probability sampling.
Diabetes 2 (5)
Using the outcomes of mortality and any adverse Other conditions 6 (14)
event, we computed a sample size of 44 to achieve
90% power and to detect an effect size of 0.4898 There was high SLE disease activity prior to MPPT;
using one degree of freedom. the mean Mex-SLEDAI score was 14.7 +5.35. Lupus
Only 42 out of the 51 charts identified for disease activity was most evidently renal, hematologic
retrieval could be obtained due to loss of charts. (leukopenia/lymphopenia), mucocutaneous, and
We extracted the following data: demographics, SLE neuropsychiatric (Table II). There was hypoalbuminemia,
disease activity score at the time of MPPT using anemia, proteinuria of > 500 mg/24 hours, lymphopenia,
the Mexican Modification of the Systemic Lupus transaminitis, and azotemia in more than half of the
Erythematosus Disease Activity Index (Mex-SLEDAI, population at baseline (Figure 1).
Appendix A), disease characteristics at the time
of MPPT (Appendix B), indications for and dose of Administration of methylprednisolone pulse
MPPT. We identified patient outcomes in terms of: In most (64%) patients, MPPT occured during the
improvement in SLE disease activity, the occurrence first year of illness. The majority (67%) received the
of adverse events or complications during and after standard dose of intravenous MPPT, which is one
gram per day for three consecutive days (Table III).
2 Volume 52 Number 1 January-March, 2014
In-Hospital Outcomes of Methylprednisolone Pulse Therapy Magbitang A, et al
The average time of administration of treatment with
Table IV: Indications for MPPT
pulse methylprednisolone was six days from the date
Indication (n=42) Frequency (%)
of admission.
Nephritis 35 (83.33)
Acute confusional state 11 (26.19)
Table II: SLE Disease activity present at the time of MPPT Myocarditits 10 (23.81)
Disease Activity (n=42) Frequency (%) Thrombocytopenia 10 (23.81)
Vasculitis 8 (19.05)
Nephritis 37 (88.1) Seizures 5 (11.90)
Leukopenia/lymphopenia 29 (69.04) Myelopathy 2 (4.76)
Mucocutaneous 25 (59.52)
Neuropsychiatric 21 (50) Others 2 (4.76)
Serositis 18 (42.86) Hemolytic anemia 1
Arthritis/Arthralgia 15 (35.71) Myositis 1
Vasculitis 13 (30.95)
Fever/fatigue 10 (23.81) Outcomes
The average duration of hospital stay was between
two to three weeks (Mean 18.6 days, SD 11.9).
Improvement was seen in 76% (32/42) of the patients
but post-treatment complication rate was 64% (27/42).
The most common in-hospital complication was
infection (30%), usually pneumonia, majority of which
were considered as hospital-acquired. Neuropsychiatric
symptoms such as headache, depressed mood,
irritability and insomnia were frequent (23%). Other
central nervous system complications seen post
treatment were seizures (16%) and cerebrovascular
disease (7%). There was blood pressure increase in 19%.
Gastrointestinal (GI) adverse events such as vomiting
and GI bleeding were observed in 9% of patients.
Figure 1: Laboratory abnormalities present at baseline Table V: In-hospital Complications
Complication Frequency(%)
New infection
Table III: Timing and Dose of MPPT Neuropsychiatric symptoms 13 (30.95)
Timing of MPPT from SLE diagnosis, in years (n=42) Frequency(%)
other than CVD or seizures 10 (23.81)
BP elevation 8 (19.05)
<1 27 (64.28) Seizures 7 (16.67)
1-3 7 (16.67) Cerebrovascular disease 3 (7.1)
Arrhythmia 2 (4.76)
>3 8 (19.05)
Others 12 (28.57)
Dose of MPPT Freuency (%)
High dose (1 g/day) 28 (66.67) A high overall-mortality rate of 21% was noted
Low dose (500 mg/day) 14 (33.33) post MPPT. If one patient who went home against
medical advice is added to the known mortalities,
Table IV shows the indications for MPPT. Nephritis the mortality rate is further increased to 23.8%.
was the most common reason for pulse steroid therapy. The use of high dose (1 gram/day) MPPT was
Other common indications were neuropsychiatric significantly associated with the development of in-
SLE, manifesting as severe acute confusional state, hospital complications (p=0.04). The patients with post-
thrombocytopenia, and myocarditis. Most of the MPPT complications had lower absolute lymphocyte
patients (64%) had more than one indication for count (p=0.01), serum albumin (p=0.04), and greater
receiving MPPT. 24-hour proteinuria (p=0.04) at baseline than those who
The diagnosis of myocarditis was based on the do not have in-hospital complications. There was a
clinical presentation of hypotension or shock at trend towards occurrence of in-hospital complications
baseline and low ejection fraction on two-dimensional among those with vasculitis, hemolytic anemia,
echocardiogram. The average platelet count of azotemia, and a low absolute lymphocyte count at
thrombocytopenic patients was 32,140 (SD 21.56) and the time of MPPT. There was, however, no difference
90% of patients had platelet counts below 50,000. in disease activity (Mex-SLEDAI) and other laboratory
parameters at baseline (Table VI). Other factors, such
as smoking and alcohol history, timing of MPPT, co-
Volume 52 Number 1 January-March, 2014 3
Magbitang A, et al In-Hospital Outcomes of Methylprednisolone Pulse Therapy
morbidity, and individual organ involvement were not High dose MPPT 0.60 (0.13-2.71) 0.50
significantly associated with complications (Table VII). Timing of MPPT 2.89 (0.52-15.91) 0.21
Smoking History 1.6(0.14-20.94) 0.70
Alcohol history 3.29 (0.18-59.60) 0.40
Table VI: Comparison of baseline disease activity and Presence of any comorbidity 0.62 (0.05-7.670 0.71
laboratory parameters among patients with and without NPSLE 1.60 (0.38-6.87) 0.52
complications post- MPPT Nephritis 0.16 (0.02-1.15) 0.05*
Vasculitis 0.52 (0.11-2.39) 0.40
Baseline Values Developed Did not develop P value Serositis 2.88 (0.66-12.60) 0.15
Complications Complications Hemolytic anemia 2.22 (0.43-11.68) 0.34
n=27 n=15 Mucocutaneous 1.92 (0.42-8.84) 0.39
Mean(SD) Mean (SD) Arthritis 1.40 (0.32-6.10) 0.65
Leukopenia/lymphopenia 2.20 (0.40-12.23) 0.36
MEX SLEDAI 14.67 (34.62) 14.73 (5.08) 0.48
anemia 3.57(0.17-72.19) 0.22
Hemoglobin mg/dL 84.81 (23.41) 98.93 (27.76) 0.13
Leukopenia 0.74 (0.16-3.46) 0.70
WBC count X109 7.76 (4.44) 8.10 (4.66) 0.41
Low ALC 3.43 (0.37-31.59) 0.26
Absolute Lymphocyte
Thrombocytopenia 3.00 (0.68-13.12) 0.14
Count 933.71 (1654.73) 2111.75 (2481.40) 0.01*
azotemia 1.17 (0.26-5.24) 0.84
Platelet Count 205.577 (150.41) 161.53 (106.52) 0.19
Low albumin 0.33 (0.02-5.97) 0.44
Creatinine umol/L 182.42 (266.88) 219.071 (292.61) 0.34
Albuminuria >500 mg/24h 1.44 (0.06-34.02) 0.46
Albumin mg/dL 17.521734 (7.76) 22.33 (8.70) 0.04*
Any infection 2.16 (0.23-20.49) 0.49
ALT mg/dL 60.4 (44.33) 48 (24.56) 0.28
AST mg/dL 173.5 (324.91) 182.57 (317.32) 0.48 *Statistically significant
24 hour Proteinuria
mg/24 hr 4886.71 (4055.21) 2086 (1917.34) 0.04*
*Statistically significant
Table IX: Comparison of baseline disease activity and
laboratory parameters between patients who died and
patients who did not die post MPPT.
Table VII: Association of factors with occurrence of Baseline Factor Died Survived p
in-hospital complications Mean(SD) Mean(SD) value
Factors Odds Ratio (95% CI) P value MEX SLEDAI 16.5 (5.74) 14.13 (5.19) 0.11
Hemoglobin mg/dL 84.9 (17.82) 96.19 (24.56) 0.09
High dose MPPT 4.00 (1.03- 15.60) 0.04*
WBC (count x 109) 7.63 (4.76) 7.98 (4.42) 0.42
Timing of MPPT 1.33 (0.36-4.93) 0.67
Absolute Lymphocyte
Smoking History 0.95 (0.08-11.79) 0.97
Count 761.76 (535.32) 1553.65 (1826.83) 0.11
Alcohol history 0.45 (0.04-8.02) 0.58
Platelet count 97,600 (59,563) 219,096 (159, 304) 0.01*
Presence of any comorbidity 4.00 (0.33-48.30) 0.25
Creatinine in umol/L 116.22 (39.94) 219.39 (300.58) 0.16
NPSLE 0.53 (0.15-1.92) 0.33
Albuming mg/dL 19.89 (8.82) 18.92 (7.54) 0.38
Nephritis 1.23 (0.18-8.33) 0.83
ALT mg/dL 37.83 (16.59) 63.44 (49.69) 0.12
Vasculitis 4.47 (0.84-23.86) 0.07
AST mg/L 77.83 (35.03) 216.00 (380.17) 0.20
Serositis 0.79 (0.22-2.80) 0.71
24 hour urine
Myocarditis 0.55 (0.14-2.24) 0.40
protein(mg/24hr) 4850.71 (4904.23) 3801.74(3853.47) 0.28
Hemolytic anemia 5.89 (0.66-52.70) 0.08
Mucocutaneous activity 1.48 (0.41-5.35) 0.54 *Statistically significant
Arthritis 0.48 (0.13-1.78) 0.27
Leukopenia/lymphopenia 1.90 (0.50-7.31) 0.34
Anemia
Leukopenia
6.25 (0.59-66.56)
1.06 (0.28-4.06)
0.09
0.93
D iscussion
Low ALC 3.50 (0.79-15.48) 0.09
Thrombocytopenia 1.18 (0.32-4.33) 0.80 Methylprednisolone pulse therapy, together with
Azotemia 3.20 (0.82-12.52) 0.09
Low albumin 2.00 (0.11-35.09) 0.63
immunosuppressive medications, remains a cornerstone
Transaminitis 0.56 (0.08-3.69) 0.54 in the management of life or organ-threatening
Albuminuria >500 mg/24h 0.25 (0.01-5.36) 0.21 complications of SLE. Evidence for the use of MPPT
*Statistically significant is particularly robust in lupus nephritis.11-15 The efficacy
of MPPT in the management of the non-renal
Table VIII shows the association of factors with manifestations of SLE has also been demonstrated but
mortality. Among the factors analyzed, nephritis at is less conclusive, with some studies, demonstrating
the time of admission was seen to be significantly non-sustained improvement and increased incidence
associated with mortality. Despite its association with of infection. 2,16,17 At present, the representative
increased in-hospital complications, use of high dose indications of MPPT in SLE are rapidly progressive
methylprednisolone was not associated with the glomerulonephritis, diffuse proliferative glomerulonephritis,
outcome of death. Comparing the population of severe focal proliferative glomerulonephritis, severe
patients who died versus those who are discharged acute confusional state, alveolar hemorrhage, vasculitis,
improved, baseline platelet count was significantly lower optic neuritis and high dose glucocorticoid refractory
in the former (p=0.01). Other baseline parameters were disease. 18
similar between the two groups (Table IX). Our study shows that MPPT exerts a favorable
response among lupus patients with various organ
Table VIII: Association of factors with increased mortality system involvements. Although thrombocytopenia and
Factor OR (95% CI) p value myocarditis are not considered representative indications
4 Volume 52 Number 1 January-March, 2014
In-Hospital Outcomes of Methylprednisolone Pulse Therapy Magbitang A, et al
for MPPT in lupus, these are the indications for use of still no consensus as to the optimal dosing of MPPT.
the drug in some of our patients. Methylprednisolone Our data suggests that a lower dose may be just
pulse therapy has also been evaluated for use in acute as effective with fewer complications. In terms of
rheumatic carditis19, but it has not been evaluated in mortality, our data detected a significant association
clinical trials for lupus myocarditis. Its use in lupus with the presence of nephritis.
myocarditis, thus, remains anecdotal. We accept the various limitations of our study.
Several case reports show good outcomes after Firstly, this is a retrospective studydata may be
MPPT use in conditions which present with refractory missed during the review of charts. Our limited sample
thrombocytopenia such as thrombotic thrombocytopenic size may underestimate the results and associations
purpura (TTP) and idiopathic thrombocytopenic purpura derived. Also, the high dose group comprised 67%
(ITP).20,21 Nevertheless, evidence for efficacy of MPPT versus the 33% of the low dose group which may
in lupus thrombocytopenia is lacking. Whether MPPT skew the data versus the high dose group in relation
is efficacious in lupus thrombocytopenia is not to the complications. Moreover, the review of data
answered conclusively by our data. It is, however, was limited to the time of admission and did not
seen that patients who died post treatment had take into consideration the possible long-term efficacy
significantly lower platelet counts compared to those and adverse effects of treatment. This data are also
who were successfully discharged. The presence of derived from the experience of a tertiary hospital in
thrombocytopenia per se did not show a significant an urban setting. The types of patients encountered
association with mortality. In SLE, treatment of may be different from those in the general population
thrombocytopenia is considered warranted if bleeding of patients with lupus. These considerations must be
is present or the platelet count is below 50,000. High taken into account when interpreting our results.
dose steroids are indicated if the platelet count is
below 20,000. 22 Our data, however, implies that this Conclusion
level may be too low to expect a favorable outcome
and may put the patient at increased risk of death. We observed the usefulness of MPPT in the
This study validates findings in other studies that treatment of high SLE disease activity, but is associated
infection is common post-MPPT. Pneumonia, tuberculosis with high rates of in-hospital complication, prolonged
and urinary tract infection are the most common hospital stay and mortality. The standard dose of one
infections documented. Other complications that gram per day for three consecutive days seems to
may arise include cognitive dysfunction, hypertension, be associated with increased in-hospital complication,
transient increase in creatinine, cerebrovascular disease, while the presence of nephritis and low platelet count
acute symptomatic seizures and arrhythmias. 2,3,23-25 showed a probable association with mortality. Further
These adverse events were seen in our patient. studies on a larger cohort are suggested, however
Neuopsychiatric manifestations such as insomnia, these findings may help in developing guidelines on
behavioral changes, and irritability occurred in some. the use of MPPT in SLE patients that are tailored to
We also noted gastrointestinal manifestations such as our setting. Treatment modifications, such as the use
nausea, vomiting and GI bleeding post treatment, of a lower MPPT dose of 500 mg/day and a more
which were not reported in previous data. aggressive treatment of nephritis and thrombocytopenia
Methylprednisolone pulse therapy has also been may be reasonable approaches to achieve an optimal
linked to increased mortality in SLE. Our data showed short-term outcome.
a high cumulative in-hospital complication rate and
mortality rate. Literature have identified factors that References
may be associated with poor outcomes such as
1. Sinha A,Bagga A: Pulse Steroid Therapy. Indian Journal
worsening of renal disease, hypoalbuminemia and
of Pediatrics 2008; 75:1057-64.
liver disease. 9,10 Some of these factors were also 2. Howe HS, Boey ML, Feng PH: Methylprednisolone In
seen in our data. Patients who developed in-hospital Systemic Lupus Erythematosus. Singapore Med Journal
complications had significantly lower levels of albumin, 1990; 31:18-21.
absolute lymphocyte count and greater degree of 3. K o n g K , B a d s h a H , L i a n T: L o w - d o s e p u l s e
methylprednisolone is an effective therapy for severe SLE
proteinuria. We also detected an association between flares. Lupus 2004; 13: 212213.
the standard MPPT dose of 1000 mg per day for 4. Badsha H, Kong KO, Lian TY, Chan SP, Edwards
three consecutive days and the presence of in-hospital CJ, Chng HH: Low dose pulse methylprednisolone for
complications. This finding is similar to the results of systemic lupus erythematosus flares is efficacious and has
a decreased risk of infectious complications. Lupus 2002;
a retrospective study done by Badsha, et al in 2002
11:
which suggested that a lower MPPT dose of 500 mg 508513.
per day may be just as useful and associated with 5. Mackworth-Young C, David J, Morgan S et al.: A
fewer infectious complications. 4 At present, there is double-blind placebo controlled trial of intravenous
methylprednisolone in systemic lupus erythematosus. Ann
Volume 52 Number 1 January-March, 2014 5
Magbitang A, et al In-Hospital Outcomes of Methylprednisolone Pulse Therapy
Rheum Dis 1988; 47: 496502.
23. Zonana-Nacach A, Barr S, Magder L et al.: Damage
6. Isenberg D, Morrow W, Snaith M: Methylprednisolone pulse in systemic lupus erythematosus and its association with
therapy in the treatment of systemic lupus erythematosus. corticosteroids. Arthritis Rheum 2000; 43: 18011808.
Ann Rheum Dis 1982; 4: 347351.
24. Moses RE, McCormick A, Nickey W: Fatal Arrhythmia
7. Ballou S, Khan M, Kushner I: Intravenous pulse After Pulse Methylprednisolone Therapy Ann Intern
methylprednisolone followed by alternate day corticosteroid Med.1981;95(6):781-782.
therapy in lupus erythematosus: a prospective evaluation.
25. Wysenbeek AJ, Leibovici L, Zoldan J: Acute central
J Rheumatology 1985; 12:944948. nervous system complications after pulse steroid therapy in
8. Parker BJ, Bruce IN: High dose methylprednisolone patients with systemic lupus Erythematosus. J Rheumatol.
pulse therapy for the treatment of severe systemic lupus 1990 Dec;17(12):1695-6.
erythematosus. Lupus 2001;16: 387-93.
9. Harisdangkul V, Rockhold L, Myers A, Jackson M. APPENDIX
Lupus Nephritis: Efficacy of monthly pulse therapy with
intravenous methylprednisolone. Southern Medical Journal Appendix A. Mexican Systemic Lupus Erythematosus
1989; 82 (3): 321-27. Disease Activity Index (Mex-SLEDAI)
10. B a d s h a H , E d w a r d s C J : I n t r a v e n o u s p u l s e s o f
methylprednisolone for systemic lupus erythematosus. Weight Descriptor Definition
Seminars in Arthritis and Rheumatism 2003; 32(6): 370-77.
11. Cathcart ES, Idelson BA, Scheinberg MA, Couser WG. 8 NEUROLOGIC MANIFESTATIONS
Beneficial Effects of Methylprednisolone Pulse Therapy Seizure Recent onset. Exclude metabolic,
in diffuse proliferative lupus nephritis. Lancet 1976; 1: infectious drug related causes
163-166. Psychosis Altered ability to function in normal
12. Dosa S, Cairns SA, Lawler W, Mallick NP, Slotki IN: activity due to severe disturbance
The treatment of lupus nephritis by methylprednisolone in perception to reality. Includes
pulse therapy. Postgrad Med J 1978; 54: 628-32. hallucinations, incoherence,
13. Makino H, Yamasaki Y, Hayashi Y, Haramoto T, Shikata loose association, poor thought
K, Kumagai I, Taniai K, Takahashi K, Ota Z: Effect content, , illogical thinking, bizarre,
disorganized or catatonic behavior
of methylprednisolone pulse therapy in patients with lupus
. Exclude presence of uremia and
nephritis assessed by WHO morphologic classification. offending drugs.
NihonJinzoGakkai Shi 1990 Jul;32(7):791-9.
14. Barile-Fabris L, Ariza-Andraca R, Olgun-Ortega L, Jara Organic Brain Syndrome Altered mental function with
impaired orientation or impaired
LJ, Fraga-Mouret A, Miranda-Limon LM, Fuentes de
memory or other intellectual
la Mata J, Clark P, Vargas P, Alcocer-Varela J: function, with rapid onset and fluc-
Controlled clinical trial of IV cyclophosphamide versus IV tuating clinical features. Includes
methylprednisolone in severe neurological manifestations in clouding of consciousness with
systemic lupus erythematosus. Ann Rheum Dis 2005;64:620 a reduced capacity to focus and
625. inability to sustain attention on en-
15. Houssiau FA, Vasconcelos C, DCruz D, Sebastiani vironment, and at least two of the
following; perceptual disturbance,
GD, Garrido ER, DanieliMG,et al.: Immunosuppressive
incoherent speech, insomnia or
Therapy in Lupus Nephritis The Euro-Lupus Nephritis daytime drowsiness, increased or
Trial, a Randomized Trial of Low-Dose Versus High-Dose decreased psychomotor activity.
IntravenousCyclophosphamide.Arthritis & Rheumatism Vol. Exclude metabolic, infectious and
46, No. 8, August 2002, pp 21212131. drug related causes.
16. Eyanson S, Passo MH, Marlene A, Aldo-Benson, Benson Visual Retinal changes form SLE: Cytoid
MD: Methylprednisolone pulse therapy in non-renal lupus bodies, retinal hemorrhages, seri-
erythematosus. Annals of the Rheumatic Diseases 1980; ous exudates or hemorrhages in
39:377-80. the choroids, optic neuritis.
17. I s e n b e r g D A , J o h n W, M o r ro w W, S n a i t h M : Cranial Nerve New onset of sensory or motor
Methylprednisolone pulse therapy in the treatment of neuropathy involving a CN.
systemic lupus erythematosus. Annals of Rheumatic Diseases
Lupus Headache Severe persistent HA; may be
1982; 41: 347-51. migrainous; unresponsive to nar-
18. Wallace DJ and Hahn BH.Dubois Lupus Erythematosus. cotics analgesia
7th ed.
19. Cmara EJ, Braga JC, Alves-Silva LS, Cmara GF, da CVA New syndrome. Exclude arterio-
sclerosis
Silva Lopes AA.Cardiol Young. 2002 Mar;12(2):119-24.
20. Winiewski P, Szarejko-Kaska M, Sworczak K, Hellmann 6 RENAL MANIFESTATIONS
A: Thrombotic thrombocytopenic purpura in a patient Casts Heme, granular or erythrocyte
with systemic lupus erythematosus successfully treated
Hematuria >5/hpf. Exclude other causes
with plasma exchange and corticosteroids. Pol Arch Med
(Stone infection)
Wewn. 2007 Aug;117(8):375-8.
21. Honma M, Ichikawa Y, Akizuki M, Kashiwazaki S, Proteinuria More than 0.5 g/24h. New onset or
Kondo H, Hashimoto H, Sugawara M, Hanaoka K: recent increase of more than 0.5 g.
Double blind trial of pulse methylprednisolone versus Pyuria >5/hpf. Exclude infection
conventional oral prednisolone in lupus nephritis. Ryumachi.
4 VASCULITIS Ulceration, gangrene, tender finger
1994 Jun;34(3):616-27. nodules, peri-ungal infarction,
22. Hepburn AL, Narat S and Mason JC: The management of splinter hemorrhages. Vasculitis
peripheral blood cytopenias in systemic lupus erythematosus. confirmed by biopsy or angiogram
Rheumatology 2010;49:22432254
6 Volume 52 Number 1 January-March, 2014
In-Hospital Outcomes of Methylprednisolone Pulse Therapy Magbitang A, et al
3 HEMOLYSIS Presence of hemolytic anemia complete resolution of malar rash, discoid rash, and oral
documented either with positive ulcers.
Coombs test, elevated bilirubins Improved vasculitis disease activity- partial or complete
or LDH resolution of signs of vasculitis post treatment.
3 MYOSITIS Proximal muscle aching or weak- Fever and fatigue, which are deemed due to systemic
ness associated with elevated lupus activity, that resolved partially or completely post
CPL/ aldolase, EMG or biopsy treatment will also be considered as improved.
showing myositis
2 ARTHRITIS More than two joints with pain and
signs of inflammation
2 MUCOCUTANEOUS Alopecia, malar rash, discoid rash
or nasopharyngeal ulcers
2 SEROSITIS
Pleurisy Pleuritic CP with pleural rub or ef-
fusion, or pleural thickening
Pericarditis Pericardial pain with at least one or
friction rub or effusion. Confirma-
tion by ECG or Echo
1 FEVER OR FATIGUE More than 38 or after exclusion of
infection
1 LEUKOPENIA or WBC<3000/mm3 or ALC < 1500/
LYMOPHOPENIA mm3
Appendix B. Definition of Significant Laboratory
Abnormalities and In-hospital Outcomes.
Anemia: Hemoglobin <12.5g/dL
Hypoalbuminemia: Serum albumin(< 34 mg/dL)
Thrombocytopenia: Platelet count<150 x 109/L
Leukopenia: WBC <5.0 x109/L
Low ALC: Absolute Lymphocyte Count <500
Elevated liver enzymes: AST and/or ALT 3x the upper
limit of normal
Azotemia: Serum creatinine >115 umol/L
Hospital discharge with improvementcomplete or partial
resolution of initial symptoms that warranted treatment
with MPPT, and the absence of worsening of disease
manifestation/s, with eventual discharge from hospital
admission as deemed prudent by the attending physician.
Improved neurologic disease activity- complete or
partial resolution of seizure, confusional state, myelopathy,
and other presenting neuropsychiatric manifestations. The
presence of a known primary neuropsychiatric illness will
be noted and considered.
Improved renal disease activity- Post-treatment urine
output, serum creatinine, urinalysis and/or hour urine total
protein will be the parameters used to evaluate renal
disease activity. Improvement in at least one or all of
these parameters, defined as an increase in urine output,
non-worsening or a decrease in serum creatinine and
non-worsening or a decrease in proteinuria compared to
baseline, with the absence of worsening in any of the
parameters, will be considered as improved renal disease
activity.
Improved hematologic disease activity- Hemoglobin,
platelet count, white blood cell count and absolute
lymphocyte count will be the parameters used to evaluate
hematologic disease activity. Improvement is defined as
increase in hemoglobin, platelet count, white blood cell
count and absolute lymphocyte count in patients with
baseline anemia and/or thrombocytopenia and leukopenia,
with the absence of worsening in any of the parameters.
Improved musculoskeletal disease activity- partial or
complete resolution of myalgia, arthralgia and arthritis.
Improved mucocutaneousdiease activity- partial or
Volume 52 Number 1 January-March, 2014 7
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- HESI Qbank From QuizletDokumen11 halamanHESI Qbank From Quizletnana100% (4)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Drug StudyDokumen4 halamanDrug Studyw dBelum ada peringkat
- FLCCC Protocols - A Guide To The Management of COVID 19Dokumen58 halamanFLCCC Protocols - A Guide To The Management of COVID 19L E100% (1)
- Asthma and COPDDokumen79 halamanAsthma and COPDDawit g/kidanBelum ada peringkat
- Acute Multiple Sclerosis RelapseDokumen16 halamanAcute Multiple Sclerosis RelapseHabib G. Moutran BarrosoBelum ada peringkat
- Steroids in Dengue Systematic ReviewDokumen15 halamanSteroids in Dengue Systematic Reviewlakshminivas PingaliBelum ada peringkat
- 22PG MATH-plus-Rationale-Journal-of-Intensive-Care-Medicine-Dec2020Dokumen22 halaman22PG MATH-plus-Rationale-Journal-of-Intensive-Care-Medicine-Dec2020Barbara RoweBelum ada peringkat
- Rational Use of SteroidsDokumen15 halamanRational Use of SteroidsPrayoga SiraitBelum ada peringkat
- 2023 - Hydrocortisone in Severe CommunityDokumen11 halaman2023 - Hydrocortisone in Severe CommunitygiseladlrBelum ada peringkat
- 2013 - Contrast - Media - ACR v.9Dokumen128 halaman2013 - Contrast - Media - ACR v.9aegysabetterwayBelum ada peringkat
- Bursitis TrocanterDokumen18 halamanBursitis TrocanterAngie Paola RodriguezBelum ada peringkat
- Corticosteroids: Ghadi Mahmoud Elbarghathi Roll Number: 1950 5 Year 2021-2022Dokumen26 halamanCorticosteroids: Ghadi Mahmoud Elbarghathi Roll Number: 1950 5 Year 2021-2022Ghadi ElbarghathiBelum ada peringkat
- Emergency Drugs / Orthodontic Courses by Indian Dental AcademyDokumen74 halamanEmergency Drugs / Orthodontic Courses by Indian Dental Academyindian dental academyBelum ada peringkat
- Daftar Harga Obat - Pt. Molex Ayus - Januari 2023Dokumen4 halamanDaftar Harga Obat - Pt. Molex Ayus - Januari 2023Muhammad AdninBelum ada peringkat
- Acute Exacerbation of AsthmaDokumen31 halamanAcute Exacerbation of AsthmaMuneeb YounisBelum ada peringkat
- SOLU-MEDROL Sterile Powder IsDokumen3 halamanSOLU-MEDROL Sterile Powder IsMARIAM A JAJIBelum ada peringkat
- Soal Acak Orthobullets 2019Dokumen131 halamanSoal Acak Orthobullets 2019kristinaBelum ada peringkat
- Ann Rheum Dis 2015 Dejaco 1799 807Dokumen11 halamanAnn Rheum Dis 2015 Dejaco 1799 807Retno ManggalihBelum ada peringkat
- Secondary HLH Case Report: Highlighting Clinical ChallengesDokumen11 halamanSecondary HLH Case Report: Highlighting Clinical ChallengesDr. Surya Abadi KristyoadiBelum ada peringkat
- KDIGO Glomerular Diseases Guideline 2021 English 200 281Dokumen82 halamanKDIGO Glomerular Diseases Guideline 2021 English 200 281khongquantam101010Belum ada peringkat
- CorticosteroidsDokumen8 halamanCorticosteroidsAkuMrW100% (1)
- Ponticelli Treatment V 1.1 11.2019 WebDokumen12 halamanPonticelli Treatment V 1.1 11.2019 WebDiddi SkittlessBelum ada peringkat
- Steroids in Dentistry: Presented By-Shibani Sarangi Postgraduate Iind Year (Dept of Oral & Maxillofacial Surgery)Dokumen67 halamanSteroids in Dentistry: Presented By-Shibani Sarangi Postgraduate Iind Year (Dept of Oral & Maxillofacial Surgery)Max FaxBelum ada peringkat
- Steroid Pulse Therapies in DermatologyDokumen4 halamanSteroid Pulse Therapies in DermatologyWelly WijayantiBelum ada peringkat
- Methylprednisolone (Solu-Medrol) : Emergency MedicationsDokumen3 halamanMethylprednisolone (Solu-Medrol) : Emergency MedicationsKdamnzBelum ada peringkat
- Final Exam Study GuideDokumen40 halamanFinal Exam Study GuideLillabinBelum ada peringkat
- Clinical Alert A Quick Reference To Adverse Clinical EventsDokumen272 halamanClinical Alert A Quick Reference To Adverse Clinical EventsOmasNers100% (1)
- DM & DI ExamsDokumen11 halamanDM & DI ExamsTomzki CornelioBelum ada peringkat
- Exam Cram CardDokumen2 halamanExam Cram CardVietnam Vo100% (1)
- An Assignment On Routinely Use Drugs in Our Clinic: Submitted To: Submitted byDokumen48 halamanAn Assignment On Routinely Use Drugs in Our Clinic: Submitted To: Submitted byIbad Ur Rahman100% (1)