2
Diunggah oleh
dark0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
11 tayangan3 halaman123
Hak Cipta
© © All Rights Reserved
Format Tersedia
TXT, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen Ini123
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai TXT, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
11 tayangan3 halaman2
Diunggah oleh
dark123
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai TXT, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 3
Current cardiopulmonary problem Evidence for each problem based on clinical
features Most likely pathophysiological basis for each problem Treatment
Impaired airway clearance ? Ausc: inspiratory crackles in LL
? Known infection + difficulty expectorating
? Febrile
? Change of colour/ consistency of sputum
? Increased WCC/CRP suggesting inflammation (pneumonia)
? Moist cough
? CXR: consolidation Impaired Cough d/t pain ? decreased exp flow ?
impaired airway clearance Supported huff/cough
Analgesia to decrease pain
Impaired MCC caused by infection / smoking
Pneumonia = infection & sputum retention ? decreased cilia function ? inability to
clear secretions ? impaired airway clearance ABx to decrease infection
ACBT / TEE ? increase VT ? increase expiratory flow rate ? shear secretions
from CW
Ambulate/SOOB ? Increase VT ? increase expiratory flow rate ? shear
secretions from CW
Humidification
Nebulisation
VHI/MHI (improved alveolar ventilation by collateral ventilation & lung
interdependence
Impaired gas exchange ? Oxygen supply
? Decreased SpO2
? ABGs Respiratory acidosis (high CO2, low pH, low O2)
? Hypoxaemia
? CXR: hyperinflation / low, flat diaphragm Surg = Atelectasis ? decreased
ventilation ? V/Q mismatch ?
Hypoxaemia ? impaired gas
exchange Mobilise = natural deep
breaths ? increase exp force
? shear secretions
Sit upright = increase FRC ? increase alveolar ventilation
? increase gas exchange
SMI = increases FRC by
breath hold via
collateral ventilation/lung interdependence
Oxygen supply
COPD = Destruction of alveoli
walls ? decrease
SA ? V/Q mismatch ?
hypoxaemia ? impaired gas
exchange
Pneumonia = shunt ? V/Q
mismatch ? hypoxaemia ?
impaired gas exchange
Diffusion limitation
(emphysema)
Hypoventilation (neuro)
Airflow limitation ? COPD
? Decreased FEV1/FVC
? Decreased CE
? CXR: hyperinflation horizontal ribs, low flat diaphragm, barrel chest
? Increased FRC, TLC
? Ausc: wheeze on expiration
? Tight cough
? Adaptive breathing pattern: PLB, prolonged expiration time, increased
abdominal effort COPD = loss radial traction ? floppy airways ? early airway
closure ? obstruction of airways on exp ? increase resistance to exp flow ? airflow
limitation PLB = supplies PEEP ? splints airways open ? increases exp time ?
increases quantity of CO2 expelled ? decreases gas trapping ? decrease WOB
Forward lean = diaphragm is at a mechanical advantage ? pushes up on
abdominal contents ? increases LV ability to expand
UL fixation = fixes
accessory m/s ? switches O/I ? allows accessory m/s to assist with breathing ?
decreases dyspnoea
Bronchodilator
Asthma ? bronchoconstriction
Reduced lung volume ? Surgery
? Recumbent positioning / bed rest
? Atelectasis
? Increased RR / rapid shallow breathing d/t pain
? CXR: atelectasis / consolidation
? Ausc: decreased BS / insp crackles (late-fine) indicates atelectasis
? Reduced CE Pain ? rapid shallow breathing Sit upright increases
FRC ? increase alveolar inflation
CPAP = increases FRC
SMI = increases FRC by
breath hold via collateral ventilation/lung interdependence
Surgery / recumbent / anaesthesia ? Decreased surface area of alveoli ?
atelectasis ? reduced FRC ? reduced LV
Dyspnoea ? Borg scale
? Subjective
? Increase RR COPD = loss radial traction ? floppy airways ? early airway
closure ? gas trapping ? static hyperinflation ? horizontal ribs/low flat diaphragm
= mechanical disadvantage ? increase use of accessory m/s ? increased O2
requirement ? weakness ? increase lactic acidosis ? increase WOB ? increase RR ?
dynamic hyperinflation ? dyspnoea PLB = supplies PEEP ? splints airways
open ? increases exp time ? increases quantity of CO2 expelled ? decreases gas
trapping ? decrease WOB ? decrease dyspnoea
Forward lean = diaphragm is at a mechanical advantage ? pushes up on
abdominal contents ? increases LV ability to expand
UL fixation = fixes
accessory m/s ? switches O/I ? allows accessory m/s to assist with breathing ?
decreases dyspnoea
Pneumonia = lungs inflamed and infected and filled with fluid ? shunt ?
V/Q mismatch ? hypoxaemia ? impaired gas exchange ? inability to meet ventilatory
demands ? dyspnoea
Decreased exercise tolerance ? Subjective COPD = loss radial traction ?
floppy airways ? early airway closure ? gas trapping ? static hyperinflation ?
horizontal ribs/low flat diaphragm = mechanical disadvantage ? increase use of
accessory m/s ? increased O2 requirement ? weakness ? increase lactic acidosis ?
increase WOB ? increase RR ? dynamic hyperinflation ? dyspnoea ? decreased ex
tolerance Education that ex when breathless is not harmful
Spiral of disability deconditioned if dont exercise then become breathless
with less activity
Pneumonia = Pneumonia = lungs inflamed and infected and filled with
fluid ? shunt ? V/Q mismatch ? hypoxaemia ? impaired gas exchange ? inability to
meet ventilatory demands ? dyspnoea ? fatigue ? decreased ex tol
Pain ? Subjective Pleura = sharp, stabbing pain
Cardiac = severe pressure, ache, squeezing, tightness left of sternum, jaw, L
arm, neck Analgesia
Respiratory muscle dysfunction ? Abnormal breathing pattern paradoxical
? Resp muscle weakness
? Neurological complications
? Dyspnoea Increasing resp muscle strength
Musculoskeletal dysfunction COPD = stiff CW / kyphosis Muscle
strengthening and stretching
Neuromuscular = abnormal postures ? increase CW stiffness
Dysfunctional breathing pattern ? Abnormal breathing pattern paradoxical
? Resp muscle weakness
? Neurological complications
? Dyspnoea
? Airflow limitation Decrease WOB by relaxed breathing
Ventilation for SCI
Short term goals ? increase mobilisation / weaning O2 / 6MWT / increase ADL /
Improve Ausc, CXR, ABGs
Long term goals ? pulmonary rehab program / (PFT) Spiro / decreased admissions /
increase QOL / CRDQ
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Goasj 1Dokumen2 halamanGoasj 1darkBelum ada peringkat
- Goasj 1Dokumen2 halamanGoasj 1darkBelum ada peringkat
- Goasj 1Dokumen2 halamanGoasj 1darkBelum ada peringkat
- Goasj 1Dokumen2 halamanGoasj 1darkBelum ada peringkat
- Goasj 1Dokumen2 halamanGoasj 1darkBelum ada peringkat
- Goasj 1Dokumen2 halamanGoasj 1darkBelum ada peringkat
- Goasj 1Dokumen2 halamanGoasj 1darkBelum ada peringkat
- Goasj 1Dokumen2 halamanGoasj 1darkBelum ada peringkat
- GoasjDokumen2 halamanGoasjdarkBelum ada peringkat
- 2Dokumen3 halaman2darkBelum ada peringkat
- GoasjDokumen3 halamanGoasjdarkBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Practical Research 2: "Correlation of Anxiety To Students' Achievement"Dokumen4 halamanPractical Research 2: "Correlation of Anxiety To Students' Achievement"Marie LargoBelum ada peringkat
- CCRN Cert Review Neuro 2Dokumen15 halamanCCRN Cert Review Neuro 2Giovanni MictilBelum ada peringkat
- Genetics Practice NCLEX Questions HandoutDokumen6 halamanGenetics Practice NCLEX Questions HandoutAlvin L. Rozier100% (3)
- Lived Experience Leading The Way: Peer Support in Mental HealthDokumen4 halamanLived Experience Leading The Way: Peer Support in Mental HealthCarolyn AndersonBelum ada peringkat
- Jambi Cardiology Update WorkshopDokumen3 halamanJambi Cardiology Update WorkshopFahrurrozi SyarifBelum ada peringkat
- Suicide Risk Assessment FormDokumen2 halamanSuicide Risk Assessment Formadrucker100% (1)
- RP18-EE-427 Mujahid HussainDokumen6 halamanRP18-EE-427 Mujahid HussainIjaz AhmadBelum ada peringkat
- National Tuberculosis Program OverviewDokumen21 halamanNational Tuberculosis Program OverviewJames RiedBelum ada peringkat
- Orthopaedic Connection: Hip DislocationDokumen2 halamanOrthopaedic Connection: Hip DislocationTeuku FennyBelum ada peringkat
- CBR AhmedRefatDokumen71 halamanCBR AhmedRefatAhmed-Refat RefatBelum ada peringkat
- 7.2 IV InjectionDokumen4 halaman7.2 IV InjectionManisa ParidaBelum ada peringkat
- Overactive BladderDokumen4 halamanOveractive BladderRanda Hayudha SBelum ada peringkat
- BCS: An Account of the Biopharmaceutical Classification SystemDokumen10 halamanBCS: An Account of the Biopharmaceutical Classification Systemruchit_darjiBelum ada peringkat
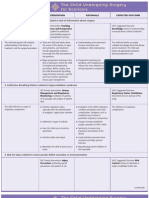
- NURSING CARE PLAN The Child Undergoing Surgery For ScoliosisDokumen3 halamanNURSING CARE PLAN The Child Undergoing Surgery For ScoliosisscrewdriverBelum ada peringkat
- Formulation and Evaluation of An Injectable Soluti PDFDokumen7 halamanFormulation and Evaluation of An Injectable Soluti PDFdhirazhrBelum ada peringkat
- ChemoDokumen32 halamanChemoJehannah Dayanara HayudiniBelum ada peringkat
- Circular Questioning As A Therapeutic ToDokumen13 halamanCircular Questioning As A Therapeutic ToNicole Prat CoghlanBelum ada peringkat
- Arabic TerminologiesDokumen5 halamanArabic TerminologiesPearly Angelique Boco-MalateBelum ada peringkat
- Specimen InformationDokumen4 halamanSpecimen Informationapi-26135524Belum ada peringkat
- l01.Htn .CaseDokumen29 halamanl01.Htn .CaseFaith Castillo100% (2)
- Chapter 48 - Drugs Affecting Blood CoagulationDokumen12 halamanChapter 48 - Drugs Affecting Blood CoagulationJonathon100% (1)
- Clinical Pharmacology in Healthcare, Teaching and ResearchDokumen80 halamanClinical Pharmacology in Healthcare, Teaching and ResearchVNcomer100% (1)
- 360 Comprehensive Exam: Assessment Form Completion Guide 2018Dokumen1 halaman360 Comprehensive Exam: Assessment Form Completion Guide 2018Altus GoldenBelum ada peringkat
- Milga ReferencesDokumen23 halamanMilga Referencessherif_awadBelum ada peringkat
- Hipertensi DM PDFDokumen32 halamanHipertensi DM PDFRian HutabaratBelum ada peringkat
- Drugs ReviewedDokumen7 halamanDrugs ReviewedJamil LorcaBelum ada peringkat
- Drug classification, action, and nursing responsibilities for Celecoxib and CloxacillinDokumen3 halamanDrug classification, action, and nursing responsibilities for Celecoxib and Cloxacillinervin_agena394Belum ada peringkat
- Quality and Safety Synthesis PaperDokumen6 halamanQuality and Safety Synthesis Paperapi-260053520Belum ada peringkat
- Ce Booklet Fall 14Dokumen28 halamanCe Booklet Fall 14api-279863771Belum ada peringkat
- Physiotherapy Course PDFDokumen156 halamanPhysiotherapy Course PDFMamta100% (1)