17 Questions
Diunggah oleh
muzammil21_adHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
17 Questions
Diunggah oleh
muzammil21_adHak Cipta:
Format Tersedia
How to Validate an Autoclave 1
Introduction
There is an array of qualification tests that can be conducted to validate
an autoclave. Many laboratories validate autoclaves by simply using
biological indicators (BIs). For some labs, however, a simple validation
with BIs is not enough and a more elaborate validation process must
be followed. These labs typically require installation, operation, and
performance qualifications (IQ/OQ/PQ) to help comply with the current
USA and International Standard for steam sterilization as set forth in
ISO 17665.
In this eBook, we will explain a variety of validation tests you may need
to perform in order to properly and effectively validate your autoclave.
How to Validate an Autoclave 2
Table of Contents
4 / Calibration
8 / Cycle Development
10 / Installation Qualification
13 / Operational Qualification
17 / Performance Qualification
21 / Steam Quality Testing
27 / Factory Acceptance Testing
31 / Simple Validation Procedure
How to Validate an Autoclave 3
1. Calibration
Calibration is a word that is frequently used in the steam sterilization industry.
At its very basic premise, calibration is bringing the response of a sensor (e.g.
transducer, thermocouple, etc.) to within a specified range relative to a primary
reference standard. For example, an autoclaves chamber temperature probes
response can be compared to a previously calibrated device, or standard,
whose response is traceable to a national reference standard, maintained in
the United States by the National Institute of Standards and Technology (NIST).
How to Validate an Autoclave 4
Why Calibrate?
The short answer is calibration ensures consistent results from a process. Steam sterilization
efficacy is highly dependent upon actual temperature. For example, if a steam autoclave is running
at 120C for 15 minutes, the theoretical lethality of that cycle is only 82% of a cycle running at
122C for the same amount of exposure time.
Since most laboratory autoclaves do not require temperature to be accurate to better than 1C,
this variability can be more common than one would think. If your temperature transducers are
calibrated, this problem will diminish.
Equipment Required to Calibrate
The proper way to calibrate an autoclave is with the use of a NIST-traceable device (standard) such
as a dry block, oil bath, or temperature probe. If using a dry block or an oil bath (pricing starts at
approximately $1,250) make sure it is designed to control to a constant temperature (0.1C). If the
dry block or oil bath is not NIST-traceable, or its calibration has expired, then use a NIST-traceable
temperature probe (cost is approximately $500) with 0.1C minimum accuracy.
Note: As a rule of thumb, the standard should be five times as
5x accurate as the device being calibrated. Therefore, when calibrating
a temperature probe with a desired accuracy of 0.5C, the
calibration standard should be accurate to 0.1C.
If the above-recommended equipment is not available, you can use boiling water to help cali-
brate the autoclaves temperature sensors. Boiling water can act as a constant-temperature (i.e.
100C/212F) bath that is somewhat near sterilization temperature. However, if the facility isnt
exactly at sea level then boiling water isnt necessarily going to be 100C/212F. Check the atmo-
spheric pressure in your area (obtained online at www.weather.gov) or use an absolute pressure
manometer (mercury column or electronic) to obtain the exact pressure reading, then calculate the
actual pressure corrected boiling temperature of water by using this steam table: (http://www.
efunda.com/materials/water/steamtable_sat.cfm). If you place your sensor into boiling water (not
in contact with the bottom of the vessel holding the water) and it isnt within 1C of the theoretical
temperature then you will need to carry out a calibration.
How to Validate an Autoclave 5
Calibration Methods
Calibration instructions can vary by the number of calibration points measured (i.e. 1-point, 2-point,
or 3-point). What is the difference?
Single Point Calibration
A single point calibration is valid only within the accuracy at that specific point. When steriliz-
ing at only one temperature, say 121C/250F, this is not too much of a problem, although you
have no idea what is happening in any process excursions to higher or lower temperatures.
Two Point Calibration
Some calibration instructions recommend taking two measurements and calculating the
slope (gain) and y-intercept (zero offset). Using two points for calibration is relatively fast and
convenient; however, two points define a straight line and reveal nothing about any non-lin-
earity in the probes reading. Also, any errors in the two measurements are not going to be
evident.
Multipoint Calibration
A multipoint (more than two point) calibration will indicate if the probe is behaving in a nonlin-
ear manner, which could be a good reason to replace it, and allows any measurement errors
to be averaged out over the greater number of points. These instructions suggest taking three
or more measurements and performing a linear regression to get the slope and y-intercept.
Any multipoint calibration should be done with points both outside the working range of the
sterilization cycle(s) you will use. For example, a lab running at 121C (and only 121C) should
calibrate at 116, 121, and 126C or at 116 and 126C for a two-point calibration. This allows
the response of the measurement and control system to be considered. If the lab is running
cycles over a greater range, calibration should start and finish 5C below the minimum tem-
perature and 5C above the maximum temperature used. A good rule of thumb is to calibrate
against at least the number of degrees in C plus one. So, if you run cycles at three different
temperatures (e.g. 115C, 121C, and 134C), you would make calibration measurements at
four points (e.g. 110C, 120C, 130C, and 140C.
How to Validate an Autoclave 6
Sample Calibration Procedure for an Autoclave
1. Record the as-found calibration data (zero and gain) for each sensor to be calibrated.
2. Using appropriate caution (shut the steam off and wait for the pressure to go to
zero!),remove the sensors to be calibrated from the sterilizer, leaving their cables
connected to the control system.
3. Set the zero and gain to 0 and 1, respectively.
4. If using a NIST-traceable dry block or oil bath place the sensor in the dry block or
oil bath.
5. If using a NIST-traceable temperature probe, place the temperature probe into a
central position in the dry block or oil bath and the sensors as close to it as possible.
6. Measure at the selected temperatures and record the standard and transducer data
You should wait for at least one minute at each temperature to allow the
measurement to stabilize. Dont rush this step.
7. Do a linear regression of the data collected. This is straightforward in Microsoft Excel
[intercept() and slope() functions] with the standards data on the y-axis and the
sensors data on the x-axis.
8. Do a correlation as well [correl() function]. It should be at least 0.999999 (i.e. a
very straight line).
9. Enter the zero and gain values to the sterilizer controller to enter the calibration.
10. Verify the calibration using at least one point like your process temperature. If more than one
process temperature, then verify at each one. Then you will have an exact statement of the
accuracy of the sensors.
11. Re-install the sensors in the sterilizer.
How to Validate an Autoclave 7
2. Cycle Development
Cycle development is performed to provide you with a sterilization process (i.e. cycle
type, sterilization temperature, sterilization time, etc.) that can be validated. Ideally,
cycle development should begin before the sterilizer is purchased, since the cycle types
will affect the type of autoclave you need, and changes in the field after installation are
generally difficult and expensive. At the very least, cycles should be developed prior to
performing a full validation of the autoclave and, more specifically, before Performance
Qualification (PQ) validation.
Its worth pointing out that in most laboratories cycle development isnt required or has
already been performed by others in the lab. Cycle development is most commonly used
for biotechnology, pharmaceutical, or medical device companies that are regularly validat-
ing their autoclaves and/or sterilizing new or unique loads.
How to Validate an Autoclave 8
Selecting a Sterilization Cycle
Refer to the flow-chart below to determine which cycle type is best for your load.
Unsterile Load
Can air be removed
Is it liquid or does easily/are there no
No No Use Prevacuum
it contain a liquid? restrictions on air
Cycle
removal?
Yes
Yes
Is the container Does the liquid have a
flexible with residual No tendency to boil No Use Liquid Use Gravity
over easily? Cycle Cycle
air inside?
Yes Yes
Use Steam-Air Mixture Use Air Overpressure
Once the cycle type is determined you must decide on the key cycle parameters:
sterilization temperature and sterilizer time.
The vast majority of loads sterilized in the laboratory setting are sterilized at 121.1C/250F for
30-90 minutes. For loads that are sensitive to heat, contact your autoclave validation expert for
advice on calculating your sterilization time using the F0 relationship.
Once you have determined your cycle type and parameter, you must validate the cycle to ensure
the load will be sterile. These test cycles should be loaded in a way that is representative of the
actual load to be sterilized. It is recommended to run your test cycles at half of the desired steriliza-
tion time (this is referred to as the half-cycle method).
Sterility testing is confirmed with the use of biological indicators (BIs). The most common test
organism for steam sterilization is Geobacillus stearothermophilus. BIs are placed in intimate
contact with the load and are placed throughout the chamber. Typically, at least 10 BIs are used per
cycle. If all BIs show no growth (i.e. all the bacteria are destroyed) in three successive cycles, you
have validated the cycle.
How to Validate an Autoclave 9
3. Installation Qualification (IQ)
Installation Qualification (IQ) provides documentary evidence that the equipment has
been built and installed to specification, and that all supporting services (i.e., utilities such
as electricity, water, and steam) are available and connected properly. The IQ process
methodically documents all aspects of the installation, the machine components, and any
testing equipment used to provide a complete, closed-loop assessment. In addition, IQ
includes NIST traceable calibration (see above) verification of the units critical
components.
How to Validate an Autoclave 10
Equipment Procurement
IQ begins before you issue the purchase order for the autoclave. Completing a successful IQ is the
result of careful planning and there should be no surprises when the unit arrives at your facility.
Naturally, what you ordered and what you receive should match.
IQ is typically carried out concurrently with installation or soon after installation at the users facility.
The IQ is performed by following a specific IQ protocol tailored for each piece of equipment.
Equipment Installation
Installation has requirements that are unique to each machine, or at least should be treated that
way. As part of IQ, these requirements must be verified. They include:
Utilities
Electrical: voltages, current, fusing, correct number of phases, and three-phase configuration
Compressed air: pressure (static AND dynamic), flow
Water: pressure (static AND dynamic), flow, temperature(s), purity(ies), dissolved gas content
Steam: pressure, purity, pipe insulation, pipe size and peak flow rate
Drain: capacity, temperature tolerance
Installation Area
Dimensions: including space to allow service
Free-standing or through-wall mounting
Biosafety barrier
Seismic anchoring
Leveling: for sterilizer performance and to align with delivery cart for removable load carriages
An IQ should list the requirements and provide documentation of the presence and adequacy of
each utility and feature listed above (if so furnished).
How to Validate an Autoclave 11
Calibration
Calibration requires standards that are traceable to the standards maintained by the United States
National Institute of Standards and Technology (NIST). In other countries, traceability is to be to that
countrys national equivalent of NIST.
Transducers and Sensors
For autoclaves, this means that a pressure standard and a temperature standard should be
available, as well as a means of providing stable pressure for calibrating the pressure
transducer(s) and a dry block or oil bath for calibrating the temperature transducers.
Optimally, a calibration standard should be five times as accurate as the device being cal-
ibrated needs to be. For a 0.5C accuracy on the sterilizer, the standard should have an
accuracy of 0.1C. Details of the calibration depend upon the sterilizers controls system
and how it handles calibrations. Generally, at least a three-point calibration is required,
with more points providing a better indication of the linearity of the system. The golden
rule of calibration is, If you do it fast, you get to do it twice. So waiting for a stable value
is key in a successful calibration.
Time
Another aspect of calibration is that of the internal clock of the sterilizer. The standards
related to steam sterilizers generally have accuracy requirements for the process control
clock(s) in the controller. Testing is straightforward, since NIST has a dial-in phone number
(303-499-7111) that tells you the national standard time on a one-minute interval, providing
you with 1 second accuracy. This level of accuracy is adequate for any laboratory auto-
clave. Measurements at either end of a 24-hour period would be acceptable to any audit.
A thorough IQ will enable you to have confidence in your autoclave, and more importantly,
documented proof of its ability to carry out the task at hand, not just because the
manufacturer tells you so, but also because it has been demonstrated in place.
IQ is a critical part of the process for fully commissioning an autoclave and
putting it into its appointed use.
How to Validate an Autoclave 12
4. Operational Qualification (OQ)
Operational Qualification (OQ) verifies that the autoclave meets the desired and intended
performance standards of the lab. OQ testing examines the autoclaves ability to run the
sterilization process correctly and repeatedly while also responding appropriately to error
conditions. OQ testing typically includes the following tests:
Empty chamber temperature mapping
Simulated load chamber temperature mapping and, if required, verification
of sterilization efficacy using biological indicators (BI)
Alarm conditions and expected results
How to Validate an Autoclave 13
Equipment Capabilities and Specifications
In general, the operational requirements for a sterilizer are detailed in a User Requirement Spec-
ification (URS). The URS defines the required performance, parameter limits, accuracy, ancillary
functions, and standards to which the equipments performance must meet. It is the basis of
OQ and can be written by the customer or may be the manufacturers specification that the user
accepts.
Autoclaves have specific critical process parameters:
Temperature set point range and control
Temperature uniformity throughout the chamber and load
Pressure range and control
For prevacuum sterilizers: air evacuation capability, including depth and control of vacuum
setpoints
For any sterilizer: the capability to achieve saturated steam pressures given the
temperature setpoint and control range
It may also include evacuation and pressurization rate control
Exposure time (and other dwell phase) control
Successful cycle execution requires that these parameters are achieved repeatedly and with pre-
defined precision. If the machine must comply with a specific standard (ISO 17665, PDA Technical
Report 1, PDA Technical Report 48, EN 285), the accuracy and precision of the process parameters
will be specified in the standard.
Equipment Testing
OQ validation generally includes both empty chamber and loaded chamber temperature mapping
for all cycle types that the facility runs (e.g., gravity, liquid, pre-vacuum, etc.). If an autoclave has
the capability to run a cycle but it is not currently used, the facility does not have to test it since the
validation for that cycle can always be run at a later date.
How to Validate an Autoclave 14
Empty Chamber Testing
Empty chamber temperature mapping is performed to verify and document that the temperature
range delivered throughout the empty autoclave is within required specifications. Interestingly,
temperature mapping an empty chamber can create more of a challenge than testing a fully-loaded
chamber because the loads thermal mass aids in providing temperature homogeneity and limiting
overshoot.
Empty-chamber testing is done with temperature datalogging probes. Temperatures should be
measured at a minimum of five locations in the chamber (plus at a point adjacent to the controlling
temperature sensor in chambers up to 800 liters). More sensors provide a more-detailed analysis of
temperature profile.
Examples of acceptance criteria are:
Chamber temperature -0/+3C relative to setpoint
Chamber temperature range over all dataloggers at any given time 2C
Pressure datalogging should also be performed only if pressure is a controlled parameter.
Simulated Load Testing
OQ validation must also test simulated loads that mimic the real loads a laboratory plans to run.
These loads may be solid, liquids, glassware, medical devices, in short, anything that would
normally be sterilized. For simulated load testing, ensure that at least three of the items in each
load are being monitored for temperature and biological indicator (i.e. place the probe and BI right
next to or on top of the load).
Diverse items processed in a specific cycle type may be tested together, however, their tempera-
ture and indicator (see below) data should be evaluated independently. Therefore, if mixed loads
are to be tested, at least three of each item type should be included, and arrayed throughout the
sterilizer chamber, not all adjacent to one another.
Simulated load testing may also include biological and/or chemical indicator testing. For overkill
cycles, half-cycle testing (the cycle has exposure duration of half the normal exposure time)
should be carried out for these cases. Biological indicators must have a 106 population of G.
stearothermophilus spores for validation testing of steam sterilization. If chemical indicators are
used, a Class 4 or 5 indicator is required. Class 6 indicators are only suitable for full-cycle testing,
since they are not expected to show a complete cycle in less exposure time.
How to Validate an Autoclave 15
Alarm Testing
Here is sample list of alarms that should be tested during an OQ validation:
Method & Actual
Alarm/Interlock Action Expected Results
Results
Simulate recycle
alarm (Alarm occurs
Buzzer sounds,
when temperature
alarm message
falls below steril-
printed, and steam
Recycle Alarm ization temperature
supply to chamber
setpoint for 1 min-
is shut off and
ute or more during
chamber exhausts
the sterilize phase
of a cycle)
Simulate over Buzzer sounds,
temperature alarm alarm message
(Alarm occurs when printed, steam
Over Temperature Alarm
chamber tem- supply to chamber
perature exceeds is shut off and
setpoint by xC) chamber exhausts
Buzzer sounds,
Simulate time limit
alarm message
alarm (Alarm occurs
printed, steam
when temperature
Time Limit Alarm supply to chamber
is not achieved
is shut off
within 1 hour of
and chamber
cycle start)
exhausts
The method used to activate the alarm must be documented and should simulate the process error
that would cause it to take place. The actual result must be identical to the expected result in order
for it to pass the OQ validation.
Ancillary Items to Test
Other unit-specific items that should be tested include, but are not limited, to:
Switches to prevent steam from being admitted to the chamber with the door unsealed
Interlocks to ensure that, in a double-door unit, both doors cannot be opened at the same time
in normal operation
For units with dual transducers, the transducers must read within a specified amount of one
another during exposure phase
Operational Qualification provides documented proof that the autoclave can execute the required
processes and that its safety and ancillary features work properly. These capabilities must be
demonstrated in the units final location of
How to Validate an Autoclave 16
5. Performance Qualification (PQ)
Performance Qualification demonstrates that the autoclave not only runs the required
cycles, but provides the required result: sterility. The PQ process involves testing the
loads that must be successfully sterilized in the autoclave. The prerequisites for PQ
are successful IQ and OQ tests.
How to Validate an Autoclave 17
Sample Test Protocol
PQ is comprised of at least three repeated tests for each defined load. The critical aspect of the
tests is to validate sterility in each of the loads. Each load type will have its own challenges so its
important that each is specified with information such as: number and type of objects being steril-
ized, sterile barrier material used, and in certain cases, orientation of the objects being sterilized in
the autoclave.
Here is a sample PQ test protocol:
1. Objective
The Objective is to prove sterilization of the specified load. The sterility assurance level may derive
from a standard, from a client SOP or specification, or from a manufacturers specification. Specific
citations to any of these should be made in this section.
2. Procedure or Setup
The Procedure or Setup explains how to setup and execute the test. The following
specifications should be noted here:
The type of cycle (vacuum, gravity, liquids, air-overpressure, low temperature, etc.)
including all critical parameters
Any equipment needed for the test
The number and location of each item in the load
If a mixed load is to be run, the number of each item and the items locations should
be specified
Locations of the indicators and datalogger probes these should be placed in
worst-case locations in the load to provide assurance that the entire load is sterilized
Sterile barrier materials or vessel covers (like aluminum foil for flasks), as well as
their application to the items closed by them
A step-by-step listing of how to carry out the test
3. Acceptance Criteria
The Acceptance Criteria section lists the required result or range of results. Examples of accep-
tance criteria for Performance Qualification involve sterility and temperature. For example, if the
acceptable criteria for the temperature range within the chamber during sterilization is -0/+3C
relative to the actual set point, then the chamber temperature at all measured points must be
within that range for a successful outcome to be recorded.
How to Validate an Autoclave 18
4. Result Record
The Result Record is where all of the test data is recorded. At least three iterations are typically run
for process tests. Any failure to comply with the acceptance criteria makes an iteration a failed
test. The required number of iterations must be run successively with successful outcomes for the
test to be considered a pass. The record must include:
Sterilizer cycle tape or electronic record
Biological (and chemical, if used) indicator results
Datalogger results and their compliance with the Acceptance Criteria
Analysis of the datalogger (thermocouple) records for accumulated lethality (Fo)
and compliance with allowable load temperature ranges in the exposure phase
5. Verification
After the testing is done, the results are typically reviewed for compliance with the acceptance
criteria. The review is finalized in this section with signatures from the person who ran the test and,
preferably, with countersignature of a second person or manager.
Sterility Testing & Record Keeping
Sterilization cycles are to be run sequentially and the load setup should follow the Procedure or
Setup section of the test. Indicators and data logger probes are to be placed as specified. Sterile
barrier or closure materials are to be applied as specified. If sample loads are to be reused, they
should be allowed to cool to a specified temperature (optimally room temperature) between cycles
to provide a real-world thermal load for the sterilizer and a real-world exposure for the indicators.
In all tests, record keeping is essential to the integrity of the test. Records may include cycle tape
printout from the sterilizer, data logger data files, photos, sketched diagrams, etc. These must
be attached or provided with the report, with each identified by the section of the PQ protocol to
which it applies. Any electronic data records should be provided in a non-volatile form with the final
report, i.e., as a CDROM or DVDROM, or via cloud storage.
How to Validate an Autoclave 19
A more extensive list of the required records is listed here:
A catalog of who carried out the testing, the verification of results, and approvals
with initials and signatures
A listing of reference or other test equipment, manufacturer, model, serial number,
and calibration due date, if applicable
A listing of biological indicators and chemical indicators (if used), including manufacturer
model number, lot number, D-value, and nominal population
If inoculum is used, a recovery study shall be done to ascertain the actual recoverable
population of the indicators; also, a growth promotion study shall be done to ensure that
the item upon which the inoculum is deposited does not have a negative effect on out
growth of the indicator organism
A calibration record for test equipment (e.g. thermocouples) if done at the work-site,
both before and after a series of tests and/or after the entire test protocol is performed
A well-executed PQ will enable you to demonstrate and document that
the autoclave can execute the desired processes and provide the sterility
assurance level that is required for your application.
PQ is generally the final step in qualification. This testing creates an unassailable baseline
level of proof of the autoclaves ability to do the specified job, and is the basis for
requalification at periodic intervals.
How to Validate an Autoclave 20
6. Steam Quality Testing
The quality of the steam feeding an autoclave is an important factor in steam steriliza-
tion. Liketime, temperature,andpressure, steam is a critical variable in the success and
repeatability of the sterilization process. As such, steam quality should be part of the
validation of any steam sterilizer.
How to Validate an Autoclave 21
Steam quality is defined as the measurable physical aspects of steam used for sterilization. These
physical aspects include temperature (superheat), dryness (liquid water content), and non-condens-
able gas content. (Steam quality is not a measure of the impurity content of the steam.) Deviations
from established ranges of these aspects of the steam can result in the following issues:
Wet loads
Damaged loads
Unsterile loads
Sterilization (biological and chemical) indicator failures
Staining and corrosion of instruments and containers
Each of these issues has a specific cause or causes and can usually be remedied.
What to Know About Steam Quality
Almost every sterilizer manufacturer recommends 97% pure steam. In general, this is not
defined, rarely measured, and, if discussed at all, is relegated to the mythology of sterilizer arcana.
The good news is that essentially all laboratory autoclaves on the market today can provide sterile,
dry, and intact sterilization loads if provided good quality steam from the steam supply. The bad
news is that any autoclave can experience the above problems, and the cause is not always some-
thing that can be predicted.
With careful design, following well-established principles, and proper maintenance, the system
(steam supply and sterilizer) can be engineered to provide a large margin of security against steam
quality noncompliance. For a production or GMP environment, steam quality testing should be part
of annual preventative maintenance and qualification testing.
When steam quality testing is performed, three parameters are measured:
The amount of the steam by weight that is steam and not
Steam Dryness
liquid water
The amount of the steam by volume that is not steam
Non-condensable gases or water, but is air or other gas that does not contribute
meaningfully to sterility of the load
The temperature of the steam above the temperature of
Superheat
saturated steam for a given moisture content
How to Validate an Autoclave 22
EN 285, the European Large Steam Sterilizer standard[1], is the worlds baseline authority for
steam quality acceptance criteria. It is referenced in most national standards and in ISO 17665[2].
With the release of EN 285:2015, the bar has been raised. The acceptance criteria are shown in the
following table.
Steam Dryness Non-condensable gases Superheat
>0.95 w/w* 3.5% v/v 25K
*For laboratory autoclaves, >0.90 w/w is considered acceptable.
Steam Dryness
Steam dryness is calculated by measuring the temperature change in a known amount of water
in relation to the mass of steam that is required to cause that temperature change. Ideally, the
temperature rise is exactly proportional to the amount of steam delivered to the water to heat it,
resulting in a dryness value of 1.0 (i.e. perfectly dry steam with no liquid water content.) Normally,
the dryness value is less than 1.0, as there are thermal losses in any piping system even if it is well
insulated. Because the dryness value of the steam at the chamber entry point can be quite a bit
lower than the dryness value in the sterilizer, measurements of steam dryness should be made at
both locations.
The acceptance criterion for steam dryness (the fraction of steam relative to water 1.0 = all
steam, no water) is at least 0.95, or 95% by weight. A dryness level down to 90% is considered
acceptable for laboratory autoclaves, however, steam below this value is considered to be wet
steam.
Wet steam does not deliver as much energy to the load as >90% saturated steam and can cause
what is known as wet packs. If the steam is wet, or if the saturation level has decreased since
the last validation, the expected Sterility Assurance Level is probably not being achieved. This is
especially important for bioburden-based validations, since overkill cycles have more of a safety
margin by their very nature.
How to Validate an Autoclave 23
Non-condensable gases
Non-condensable gases are generally air and air is a poor sterilant compared to steam. As an exam-
ple, a typical dry-heat sterilization exposure phase lasts upwards of two hours at a temperature of
at least 160C/320F. Steam sterilization typically is done with exposure phases of 15 minutes at
121C/250F or 3.5 minutes at 134C. The efficacy difference is notable. For a comparison, consider
a contact lens manufacturer that must sterilize contact lens blisters to a 10-6sterility assurance
level. Sterilization can be performed using a steam/air mix cycle that runs at 122C/252F for 45
minutes with a steam/air mix of approximately 48% steam (using absolute pressures for the calcu-
lation). The same result can be achieved in 15 minutes with saturated steam alone.
In short, non-condensable gases decrease sterilization efficacy. As with wet steam, the Sterility
Assurance Level will be less than expected if non-condensable gas content has increased since
product sterility validation. The percentage of non-condensable gases in the steam should be less
than or equal to 3.5% by volume.
Superheat
The steam is sampled in free expansion into ambient air. The maximum temperature measured at
a precise location in the jet is the temperature upon which the superheat analysis is based. When
the temperature and moisture content do not match up, two things can happen:
1. If the moisture content is higher than saturation for the temperature, wet loads occur, as dis-
cussed previously.
2. When the moisture content is lower than saturation for the temperature, the condition is called
superheat. In superheat, the steam is too dry and its energy content is too high. When the steam
condenses on the load, the energy released is enough to melt plastic packaging and actually char
paper packaging. Neither is a good outcome.
The amount of superheat present in the steam should be no more than 25 degrees Celsius above
the temperature in free expansion into atmosphere at the current atmospheric pressure. For all
intents and purposes, this corresponds to an upper limit of 125C in the measurement.
The amount of superheat present in the
steam should be no more than
25 degrees Celsius.
How to Validate an Autoclave 24
What causes non-compliant results?
Wet steam
Inadequate insulation around the sterilizer or steam piping, allowing energy loss
and condensation
Poorly controlled steam boiler chemistry (especially a deficiency of sulfites)
Low sections of piping between the boiler and the sterilizer, allowing condensate to pool and be
carried over with the steam entering the chamber
Too great a pressure drop across a regulator or between the jacket and chamber, which causes
the extra water in the steam at the higher pressure to fall out as condensate
No/clogged steam filters, either letting condensate pass if no filter, or causing a pressure drop
that causes condensate to fall out
No/clogged steam traps/separators, in either case, condensate in the steam line is not removed
Steam trap/filter too far from the sterilizer, allowing condensate to be generated between the
trap or filter and the sterilizer
Inadequate number of steam traps for the distance that steam must travel from its source to
the sterilizer
Bad steam system design (vertical drops of steam direct to the sterilizer, no traps,
no header, etc.)
Load too dense/too cold when placed in sterilizer
Foaming of the water in the boiler
How to Validate an Autoclave 25
What causes non-compliant results, Cont.
Non-condensable gases
These are brought into the steam primarily via two sources:
Leaks/cracks in the steam plumbing, filters, separators, etc.
Inadequate deaeration of the boiler feed water
Superheat
Superheat can result from the following sources:
Jacket temperature/pressure too high
Steam pressure/temperature too high entering the sterilizer
Steam flowing through a small orifice or tight-radiused direction change between its
source and the chamber causing a large pressure reduction/steam velocity increase
The temperature shown on the sterilizer controls generally will not show superheat values, even
if superheat is present. Since the temperature is measured in the drain of the sterilizer chamber,
superheat will have been dissipated into the load, chamber wall, door and backhead long before it
reaches that sensor.
Solutions
Each of the steam quality parameters can be measured and, if issues arise, addressed. The first
step is to measure, even if there are no problems. This should be done on a regular basis at
initial installation, and after preventative maintenance to establish a baseline for the system.
Measurements made when there are no problems can also provide an indication if the sterilizer is
close to having a problem. Measurements should also be made when changes are made to supply
plumbing.
Persons experienced in steam quality analysis
can usually make cost-effective suggestions
to fix the problems, and of course measure to
see if the problem is, in fact, fixed.
How to Validate an Autoclave 26
7. Factory Acceptance Testing (FAT)
A steam sterilizer, whether used for pharmaceutical or laboratory sterilizing applications,
is designed to use steam under pressure as the sterilizing agent. When constructed,
installed and operated correctly, a steam sterilizer should function properly and sterilize
your load. But, how does a sterilizer manufacturer ensure the unit theyve built is assem-
bled properly and is in good working condition prior to being shipped? Furthermore, how
does the end-user know that the sterilizer they are buying is up to spec? The answer:
Factory Acceptance Testing (FAT).
How to Validate an Autoclave 27
What is Factory Acceptance Testing?
Factory Acceptance Testing (FAT) is a process that evaluates the sterilizer during and after the
assembly process by verifying that it is built and operating in accordance with design specifica-
tions. FAT ensures that the sterilizers components and controls are working properly vis-a-vis the
functionality of the sterilizer itself. As the name suggests, this testing is performed at the factory.
FAT is typically conducted in order to assess any discrepancies and non-conformities, as well as
develop a process for how they are to be handled. Deviations or abnormalities observed during
testing are documented in a problem report and corrected prior to shipment. While the end goal for
a manufacturer is to ship a sterilizer as soon as possible, FAT must be conducted in a thorough and
forthright manner. A poor or rushed FAT can lead to missed non conformities, which can only then
be corrected after the equipment is installedwhich in turn can wreak havoc on a project schedule.
In short, the purpose of FAT is to document the results of the sterilizer testing at the factory prior
to shipment.
The Factory Acceptance Testing Process
There are several components that make up FAT. The product must be assembled, prepared, and
connected to utilities for testing. Documentation such as drawings, ASME certificates, and test
procedures must be gathered. And finally, testing must be conducted in the factory that follows
specific test procedures.
Preparation
Before the FAT begins, the manufacturer should present the FAT procedure to the client for review
and approval. The procedure should include testing of as much functionality as is practical in the
factory and, where possible, should show pass/fail criteria or desired results for each item tested.
Once the procedure is approved, the manufacturer should test the equipment before the FAT
begins. Keep in mind that some clients like to visit the factory during FAT, so this pre-test
will confirm that the sterilizer is set up with the correct options, ensure a smoother FAT process
and minimize down-time during the FAT.
How to Validate an Autoclave 28
Documentation
There is much documentation to be gathered and checked during FAT (see Table 1 below for a
sample list of key documents). These documents are provided by the manufacturer before, during,
and after the testing phase.
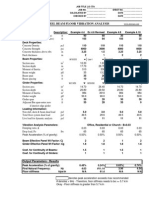
Table 1
Sample List of Required Documents for FAT
Dimensioned Outline Drawings
Assembly Drawings
Schematic Piping Drawings
Schematic Wiring Drawings
Installation, Operation and Maintenance Manuals
Piping and Instrumentation Diagram(s)
Maintenance Procedures
Detailed Parts List and Materials of Construction
Instrument Index including Tag, Location, Specifications, Ranges and Tolerances
NIST Traceable Calibration Data Sheets for Monitoring Instruments
Software and/or Controls Parameters, PID Constants
Pressure Test Reports
Manufacturer/Vendor Certificates (Materials, ASME, etc.)
Supplier SOPs for Setting up the Sterilizer with Adjustments using Manual Needle Valve
How to Validate an Autoclave 29
Testing
Next comes the critical testing involved in FAT. Each critical system of the sterilizer is tested and
referred to as a Test Case (see Table 2). In order to confirm that the autoclave is operating correctly
you must then settest objectivesfor each Test Case and developacceptance criteriain accordance
with your pre-test procedures. The actual results of each test will be documented and indicated
as either passed or failed. The initials of the tester are provided for each test as well as a signature
sheet. Some FAT forms also include an area for commentsin case there are any discrepancies or
non-conformities, as well as suggested remedies.
Table 2
Test Cases Objective Test Procedure Acceptance Criteria
Dimensioned Outline Drawings
Assembly Drawings
Schematic Piping Drawings
Schematic Wiring Drawings
Installation, Operation and
Maintenance Manuals
FAT may be a necessary step in the validation process, especially for pharmaceutical clients where
special one-off features may be ordered. In some instances, FAT can actually be conducted during
Installation Qualification (IQ). It is best to review your project and validation requirements to deter-
mine if this is possible for your situation.
Interestingly, most laboratory clients and general purpose applications do not require FAT. Where
FAT is not a requirement, any reputable manufacturer will still follow a testing process to ensure
the autoclave is functioning properly prior to shipping.
How to Validate an Autoclave 30
8. Simple Validation Process
If the budget isnt available to perform periodic validation then the easiest and most
inexpensive way to ensure the autoclave is sterilizing properly is to run cycles with
biological indicators (BIs). See below for a step-by-step protocol for simple validation.
How to Validate an Autoclave 31
1. Calibrate sterilizer temperature probe
Use NIST traceable thermocouple and meter (or bath)
2. Run an empty chamber cycle (5-10min)
3. Load the autoclave with a typical load (e.g. bottles, cages, liquids, etc.)
Load should be worst case scenario
4. Place BIs in the load and near drain
Minimum of 3-5 BIs per test cycle
5. Run cycle
6. Repeat steps 3-5 for each autoclave load or cycle type
7. Check and record results after 48-hour incubation
The frequency at which you perform this type of simple validation is your choice: once per week,
once per month, once every six months. Whatever it is that you decide, try to be consistent and if
any tests fail (i.e. the BIs show growth) then contact your local service representative to
investigate and resolve the problem.
The procedures mentioned throughout this eBook allow researchers, technicians,
facility managers, and consultants to gain a better understanding of laboratory
autoclave validation.
The validation requirements for each lab will be different, some requiring more documentation and testing
than others. Whatever procedures that are executed will add a layer of comfort to the users that the
autoclave is functioning properly.
Consolidated Sterilizer Systems manufactures top-quality steam sterilizers for leading universities, hospitals
and biotechnology facilities worldwide. Our autoclave validation specialists are available to answer all your
questions.
Reference: ANSI/AAMI/ISO 17665-1: 2006/(R)2013 Sterilization of health care productsMoist heatPart 1:
Requirements for the development, validation, and routine control of a sterilization process for medical devices,
definition 3.17.
How to Validate an Autoclave 32
How to Validate an Autoclave 33
Please contact us for more information on
autoclave validation services.
www.consteril.com
617.782.6072
Consolidated Sterilizer Systems
All Rights Reserved
How to Validate an Autoclave 34
Anda mungkin juga menyukai
- Autoclave (Steam Sterlizer) Validation - Pharmaceutical GuidelinesDokumen3 halamanAutoclave (Steam Sterlizer) Validation - Pharmaceutical GuidelinesASHOK KUMAR LENKABelum ada peringkat
- Pharmaceutical Industry Documents: 90 Pharmaceutical Quality Assurance Interview Questions & AnswersDari EverandPharmaceutical Industry Documents: 90 Pharmaceutical Quality Assurance Interview Questions & AnswersBelum ada peringkat
- Autoclave Validation MSPDADokumen35 halamanAutoclave Validation MSPDAYessine Mrabet100% (1)
- TocDokumen7 halamanTocIlayaraja Boopathy0% (1)
- PQ Sterile TunnelDokumen10 halamanPQ Sterile TunnelReza JafariBelum ada peringkat
- F0 What It Means - How To Calculate It - How To Use Itv3 PDFDokumen34 halamanF0 What It Means - How To Calculate It - How To Use Itv3 PDFJosé Manuel Pais-Chanfrau100% (1)
- Autoclave ValidationDokumen7 halamanAutoclave ValidationMohanad Alashkar100% (1)
- Validation of Terminal Sterilization PDFDokumen14 halamanValidation of Terminal Sterilization PDFjpabloqf100% (1)
- Validation Protocall For AutoclaveDokumen7 halamanValidation Protocall For AutoclaveBalakrishnan S NadarBelum ada peringkat
- Chapter 14Dokumen85 halamanChapter 14Michael A SalvatoreBelum ada peringkat
- Qualification Procedure For Vial Washing Machine - Pharmaceutical GuidelinesDokumen1 halamanQualification Procedure For Vial Washing Machine - Pharmaceutical GuidelinesAli Goutas50% (2)
- How To Validate An AutoclaveDokumen3 halamanHow To Validate An AutoclaveqhpuongBelum ada peringkat
- ASTM Standard E 2500 for Risk-Based Verification of Pharma Manufacturing SystemsDokumen30 halamanASTM Standard E 2500 for Risk-Based Verification of Pharma Manufacturing SystemsMohsinShaikh100% (2)
- Media Fill ChecklistDokumen11 halamanMedia Fill ChecklistSilke Igemann100% (1)
- Air SamplerDokumen42 halamanAir SamplerKuldeepBelum ada peringkat
- Validation of Lab Incubators & OvensDokumen4 halamanValidation of Lab Incubators & Ovensltrevino100Belum ada peringkat
- HTM2010 Parts1-6 PDFDokumen724 halamanHTM2010 Parts1-6 PDFJUAN CARLOS RiveraBelum ada peringkat
- PDA TR Nº40 Sterilizing Filtration of Gases PDFDokumen45 halamanPDA TR Nº40 Sterilizing Filtration of Gases PDFehsan050628Belum ada peringkat
- Media Fills and Environment Atl Monitoring 26 July 2011 Presentation OneDokumen18 halamanMedia Fills and Environment Atl Monitoring 26 July 2011 Presentation OneRiccardo TorelliBelum ada peringkat
- S. No. SOP Title Room No. Responsibility StatusDokumen1 halamanS. No. SOP Title Room No. Responsibility Statusjpmaurya77Belum ada peringkat
- PQ - Autoclave (HPHV Steam Sterilizer)Dokumen26 halamanPQ - Autoclave (HPHV Steam Sterilizer)hbhatt88100% (5)
- ECA Task Force CCS Guideline Vers2Dokumen53 halamanECA Task Force CCS Guideline Vers2elisabetta ghilardi100% (2)
- Pda Technical Report 48 Moist Heat Sterilizer SystemsDokumen70 halamanPda Technical Report 48 Moist Heat Sterilizer SystemsDuc100% (2)
- Autoclave Validation EssentialsDokumen17 halamanAutoclave Validation EssentialsprakhyaatBelum ada peringkat
- Checklist of Validation of Dy Heat SterilizerDokumen8 halamanChecklist of Validation of Dy Heat Sterilizersami2210Belum ada peringkat
- Aseptic Processing Risk Assessment The Simplified Akers Agalloco MethodDokumen55 halamanAseptic Processing Risk Assessment The Simplified Akers Agalloco MethodDoan Chi ThienBelum ada peringkat
- Protocol For Disinfectant Validation Disinfectant Validation ProtocolDokumen13 halamanProtocol For Disinfectant Validation Disinfectant Validation ProtocolMax PainBelum ada peringkat
- Media Fill FDA 483 ObservationsDokumen22 halamanMedia Fill FDA 483 Observationsvijayns_250355172Belum ada peringkat
- Disinfectant ValidationDokumen7 halamanDisinfectant Validationrose itaBelum ada peringkat
- Cross Contamination Prevention in HVACDokumen8 halamanCross Contamination Prevention in HVAChuynhhaichauchauBelum ada peringkat
- Microbiological Enviromental MonitoringDokumen34 halamanMicrobiological Enviromental MonitoringAna Dulce100% (1)
- Media Fill ReadingDokumen6 halamanMedia Fill ReadingMina Maher MikhailBelum ada peringkat
- 7.5 Steam in Place (SIP)Dokumen32 halaman7.5 Steam in Place (SIP)Cg Ida Home Tuition100% (1)
- PDART59 12 Statistical MethodsDokumen74 halamanPDART59 12 Statistical MethodsJorge Martinez Quezada100% (1)
- TR57 Toc PDFDokumen6 halamanTR57 Toc PDFnsk79in@gmail.comBelum ada peringkat
- PQ of AutoclaveDokumen23 halamanPQ of Autoclavedinesh000786100% (7)
- Autoclave Validation ProtocolDokumen4 halamanAutoclave Validation Protocolsalluraj100% (2)
- Autoclaves - Proper Operation and ValidationDokumen7 halamanAutoclaves - Proper Operation and Validationgrace holmBelum ada peringkat
- Qualification of AutoclavesDokumen39 halamanQualification of Autoclavesjermac17100% (1)
- Simulating Aseptic ProcessesDokumen13 halamanSimulating Aseptic ProcessesraghuBelum ada peringkat
- Fo ValueDokumen1 halamanFo Valuej.k.kumar100% (12)
- Parenteral Process Validation 1Dokumen30 halamanParenteral Process Validation 1BALU LTD BALU PHARMACEUTICALBelum ada peringkat
- PQ of Vial Washer Ensures Removal of ContaminantsDokumen25 halamanPQ of Vial Washer Ensures Removal of ContaminantsJuan DanielBelum ada peringkat
- USP 1229.8 Dry Heat SterilizationDokumen3 halamanUSP 1229.8 Dry Heat SterilizationDoan Chi ThienBelum ada peringkat
- A Risk Matrix Approach For Media Simulation TrialsDokumen11 halamanA Risk Matrix Approach For Media Simulation Trialsschumon100% (2)
- Autoclave Validation PresentationDokumen17 halamanAutoclave Validation PresentationAnkur Bhatia100% (1)
- IVT Network - Microbiological Assessment of Compressed Gases in Pharmaceutical Facilities - 2015-08-17Dokumen7 halamanIVT Network - Microbiological Assessment of Compressed Gases in Pharmaceutical Facilities - 2015-08-17Youstina PhillipeBelum ada peringkat
- Steam SterilizerDokumen24 halamanSteam Sterilizerj.k.kumar83% (6)
- Auoclave Validation ProtocolDokumen20 halamanAuoclave Validation Protocolyogendra67% (3)
- Autoclave Validation: Presented by Paul Yeatman Bsc. MicrobiologistDokumen17 halamanAutoclave Validation: Presented by Paul Yeatman Bsc. Microbiologistzfo302Belum ada peringkat
- ECA Cleaning ValidationDokumen4 halamanECA Cleaning ValidationschumonBelum ada peringkat
- HVAC, Water and Critical Utility QualificationsDokumen51 halamanHVAC, Water and Critical Utility Qualificationsvijaysirsat2007100% (1)
- Biocontamination Control for Pharmaceuticals and HealthcareDari EverandBiocontamination Control for Pharmaceuticals and HealthcarePenilaian: 5 dari 5 bintang5/5 (1)
- Cleanroom Technology: Fundamentals of Design, Testing and OperationDari EverandCleanroom Technology: Fundamentals of Design, Testing and OperationBelum ada peringkat
- Validation Master Plan A Complete Guide - 2020 EditionDari EverandValidation Master Plan A Complete Guide - 2020 EditionBelum ada peringkat
- Gamma IrradiationDokumen27 halamanGamma Irradiationmuzammil21_adBelum ada peringkat
- DCVMN Heat Sterilisation v3 1 PDFDokumen94 halamanDCVMN Heat Sterilisation v3 1 PDFmuzammil21_adBelum ada peringkat
- Gamma IrradiationDokumen27 halamanGamma Irradiationmuzammil21_adBelum ada peringkat
- Standard Update ISO 11140 UpdateDokumen2 halamanStandard Update ISO 11140 Updatemuzammil21_adBelum ada peringkat
- Risk Benefit Analysis EmergoDokumen9 halamanRisk Benefit Analysis Emergomuzammil21_adBelum ada peringkat
- Guidance for Nebulizers, Metered Dose Inhalers, Spacers and ActuatorsDokumen15 halamanGuidance for Nebulizers, Metered Dose Inhalers, Spacers and Actuatorsmuzammil21_adBelum ada peringkat
- Guidance On Biological Safety.02.11Dokumen10 halamanGuidance On Biological Safety.02.11muzammil21_adBelum ada peringkat
- ISO 13485 Certification RVP 6-12-2013Dokumen30 halamanISO 13485 Certification RVP 6-12-2013muzammil21_adBelum ada peringkat
- Usp29nf24s0 c71Dokumen11 halamanUsp29nf24s0 c71muzammil21_adBelum ada peringkat
- Revision To Cleanroom Standard ISO 14644Dokumen4 halamanRevision To Cleanroom Standard ISO 14644TueBelum ada peringkat
- 17 Questions PDFDokumen19 halaman17 Questions PDFmuzammil21_adBelum ada peringkat
- Sterile Packaging Sample SizeDokumen5 halamanSterile Packaging Sample Sizemuzammil21_adBelum ada peringkat
- 2-77-1392292485-10. Eng-A Review On Properties of Surgical-Srinivasulu K PDFDokumen12 halaman2-77-1392292485-10. Eng-A Review On Properties of Surgical-Srinivasulu K PDFmuzammil21_adBelum ada peringkat
- HPLC Method ValidationDokumen11 halamanHPLC Method ValidationexecBelum ada peringkat
- Deviation Report TemplateDokumen1 halamanDeviation Report Templatemuzammil21_ad100% (2)
- Effect of Sterilization Silk SuturesDokumen6 halamanEffect of Sterilization Silk Suturesmuzammil21_adBelum ada peringkat
- Surgical Sutures - An OverviewDokumen5 halamanSurgical Sutures - An OverviewGorila JuliBelum ada peringkat
- Guidelines For Mapping LinksDokumen2 halamanGuidelines For Mapping Linksmuzammil21_adBelum ada peringkat
- FastVal Design Specification TemplateDokumen16 halamanFastVal Design Specification Templaterobert.ragland4819Belum ada peringkat
- Stainless Steel Needle0316Dokumen2 halamanStainless Steel Needle0316muzammil21_adBelum ada peringkat
- Ann Occup Hyg 1999 Hwang 275 81Dokumen7 halamanAnn Occup Hyg 1999 Hwang 275 81muzammil21_adBelum ada peringkat
- Tools For Quality ImprovementDokumen64 halamanTools For Quality Improvementmuzammil21_adBelum ada peringkat
- Testing Compressed Air Lines For Microbiological ContaminationDokumen8 halamanTesting Compressed Air Lines For Microbiological Contaminationmuzammil21_adBelum ada peringkat
- Cal Water BathDokumen6 halamanCal Water Bathmuzammil21_adBelum ada peringkat
- Medical DevicecasestudiesDokumen55 halamanMedical DevicecasestudiesKshitij GuptaBelum ada peringkat
- Classification IdentificationDokumen42 halamanClassification Identificationmuzammil21_adBelum ada peringkat
- APG AuditingElectronicBasedMSDokumen5 halamanAPG AuditingElectronicBasedMSmuzammil21_adBelum ada peringkat
- PublishedDokumen9 halamanPublishedmuzammil21_adBelum ada peringkat
- LF Solar Panels Datasheet - July 2022 - Preview FileDokumen9 halamanLF Solar Panels Datasheet - July 2022 - Preview FileMayur HiwarkarBelum ada peringkat
- Nishimura Sh. Handbook of Heterogeneous Catalytic Hydrogenation For Organic Synthesis (Wiley, 2001) (ISBN 0471396982) (747s) PDFDokumen747 halamanNishimura Sh. Handbook of Heterogeneous Catalytic Hydrogenation For Organic Synthesis (Wiley, 2001) (ISBN 0471396982) (747s) PDFindiomajadero100% (2)
- States of Matter ExplainedDokumen13 halamanStates of Matter ExplainedSatish KumarBelum ada peringkat
- Submarine Cable Installation ContractorsDokumen19 halamanSubmarine Cable Installation Contractorswiji_thukulBelum ada peringkat
- Introduction To Physical ScienceDokumen31 halamanIntroduction To Physical ScienceVeronica MedranoBelum ada peringkat
- CFM and Capacity Calcs 4.5Dokumen9 halamanCFM and Capacity Calcs 4.5hvacrmedicBelum ada peringkat
- Ashby Jones - Engineering Materials - Vol.1 - NeckingDokumen5 halamanAshby Jones - Engineering Materials - Vol.1 - NeckingpippaBelum ada peringkat
- Technical Data Sheet Chryso Cim 5376 115Dokumen3 halamanTechnical Data Sheet Chryso Cim 5376 115clangatBelum ada peringkat
- A 289 - A 289M - 97 R03 Qti4os9bmjg5tqDokumen3 halamanA 289 - A 289M - 97 R03 Qti4os9bmjg5tqRudiyansah RudiyansahBelum ada peringkat
- Crain'S Simplified Rules: Log Response Chart PDFDokumen8 halamanCrain'S Simplified Rules: Log Response Chart PDFKaiysse YoukéBelum ada peringkat
- Physics Syllabus in 40 CharactersDokumen3 halamanPhysics Syllabus in 40 CharactersAmit YadavBelum ada peringkat
- Piezoelectric MaterialsDokumen15 halamanPiezoelectric Materialsmahmoud ahmed0% (1)
- Siemens Rayos X Multix Swing Datasheet 1 PDFDokumen8 halamanSiemens Rayos X Multix Swing Datasheet 1 PDFAlejandro FaveroBelum ada peringkat
- 1-Universal Vibrational Spectrum - Online CoursesDokumen9 halaman1-Universal Vibrational Spectrum - Online CoursesPanther Panther25% (4)
- Static Electrification: Standard Test Method ForDokumen10 halamanStatic Electrification: Standard Test Method Forastewayb_964354182Belum ada peringkat
- Lihardo Rotua Sinaga. Maulidatul Fadhilah. Maria Angel Aftritesia. BilPhys19. Thermodynamics. Mini ResearchDokumen14 halamanLihardo Rotua Sinaga. Maulidatul Fadhilah. Maria Angel Aftritesia. BilPhys19. Thermodynamics. Mini ResearchFitri handayaniBelum ada peringkat
- CHAPTER 2 PV Tech PDFDokumen35 halamanCHAPTER 2 PV Tech PDFPal KycBelum ada peringkat
- Building Hot Air Balloon ModelsDokumen11 halamanBuilding Hot Air Balloon ModelsOkotie-Eboh ToritsejuBelum ada peringkat
- Architectural Acoustics ExplainedDokumen10 halamanArchitectural Acoustics Explainedproject jadeBelum ada peringkat
- Phaser3428 Service PDFDokumen206 halamanPhaser3428 Service PDFRobert GreenBelum ada peringkat
- AISC DG11 ExamplesDokumen7 halamanAISC DG11 ExamplesMarcel Toruño MendezBelum ada peringkat
- Binary Offset Carrier (BOC)Dokumen18 halamanBinary Offset Carrier (BOC)ninnnnnnimoBelum ada peringkat
- Tolc I Sinavi Ornek SorulariDokumen50 halamanTolc I Sinavi Ornek SorulariborabasmaciBelum ada peringkat
- Mat3002 Applied-Linear-Algebra LT 1.0 1 Mat3002Dokumen2 halamanMat3002 Applied-Linear-Algebra LT 1.0 1 Mat3002Tanmay BohraBelum ada peringkat
- Nissin Di700 ManualDokumen24 halamanNissin Di700 ManualVladimir TodorovićBelum ada peringkat
- Eagle Color SeriesDokumen2 halamanEagle Color SeriestrumukyBelum ada peringkat
- Master Thesis S BuysseDokumen141 halamanMaster Thesis S Buyssemichael KetselaBelum ada peringkat
- Connected Array AntennasDokumen234 halamanConnected Array Antennasmarchelo_cheloBelum ada peringkat
- Design Manual for Ethiopia's Low-Volume Rural RoadsDokumen45 halamanDesign Manual for Ethiopia's Low-Volume Rural RoadsMichael Kazi100% (1)
- Class 6 Assignment 15 2022-23Dokumen27 halamanClass 6 Assignment 15 2022-23Debaprasad MukherjeeBelum ada peringkat