Causes of Indirect Hyperbilirubinemia in Neonates
Diunggah oleh
Rahmah WantiDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Causes of Indirect Hyperbilirubinemia in Neonates
Diunggah oleh
Rahmah WantiHak Cipta:
Format Tersedia
ORIGINAL ARTICLE
A Study of Various Causes of Indirect Hyperbilirubinemia in
Neonates
1 2 3
SAEED AHMAD MALIK , MUHAMMAD AURANGZEB MALIK , SAADIA AURANGZEB MALIK
ABSTRACT
Background: Neonatal jaundice is a fairly common cause of morbidity in Pakistan and accounts for
(1
almost 25% of all newborn admissions . This may also account for the wide variation in the etiology of
jaundice from various reports in Pakistan.
Aim: To describe the etiology hemolytic jaundice in the region of Bahawalpur, Pakistan and to identify
factors determining the severity of hyperbilirubinemia.
Methods: sixty cases of jaundice were ad mitted in various units of BV Hospital/QAMC Bahawalpur
referred from various DHQ hospitals of Bahawalpur Division. They were examined clinically and were
investigated hematologically to be differentiated from other groups of jaundice by various routine and
special tests like blood count, enzyme assay, RBC fragility and coombs test etc
Results: Sixty neonates referred to various units of Bahwal Victoria Hospital, Bahawalpur during the
period of 1 year were investigated for this purpose. 22(36.6%) out of 60 cases of hemolytic jaundice
were found to showed exaggerated physiological jaundice, 2(3.3%) from G6PD enzyme deficiency, 4
(6.6%) were diagnosed as a case of hereditary spherocytosis, 8(13%) were of ABO incompatibility,
10(16.6%) infections 5(8.3%) of drug induced hemolytic anemia.
Conclusion: It is observed that indirect hyperbilirubinemia may be associated with a wide variety of
disease states like cardiac, GI disorders, infections and due to increased pigment production.
Incidence of hemolytic anemia due to G6PD deficiency needs further probing to evaluate the incidence
of this disorder in the population of Bahawalpur Division initially and then in population of Pakistan
after collecting data from other areas of the country.
Keywords: Indirect hyperbilirubinemia, Jaundice, G6PD, Infections. NH: neonatal hyperbilirubinemia
INTRODUCTION
trauma in circulation or infectious agents). It can be
Increase rate of hemoglobin degradation in hemolytic seen in all age groups. Causes also vary in various
anemia, congenital and acquired, will lead to age groups. Most cases of neonatal
increased bilirubin concentration in blood stream. hyperbilirubinemia are due to physiological jaundice
Liver may not be able to properly excrete the greater and go without have serious consequences. The
load of pigment present, and this increased bilirubin important challenge clinically is to identify those
level will result in the clinical condition of jaundice newborns that may develop severe neonatal
(hemolytic or prehepatic). It is important to determine 1
hyperbilirubinemia . There are many factors involved
the cause of indirect hyperbilirubinemia so proper in the development of pathological jaundice, which
treatment can be directed. Hemolysis is of two types; may include perinatal factors (e.g., birth trauma or
1) Intravascular , caused by rupture of red cells within infections), maternal factors(e.g., Rh or ABO
the blood stream. 2) Extravascular, removal of red incompatibility), neonatal factors (e.g., prematurity or
cells from the blood stream by cells of polycythemia), and genetic factors (e.g., Crigler-
reticuloendothelial system. Most hemolysis occurs 2
Najjars or Gilberts syndrome) . The administrations
extravascularly i.e. by the phagocytic cells in spleen, of drugs like cephalosporins and glucose-6-
liver and bone marrow. Hemolysis is usually due to 1. phosphate dehydrogenase (G6PD) enzyme
Abnormalities within RBCs (Hemoglobin or deficiency have been implicated in pathological
metabolism); 2) abnormalities of RBC membrane 2
jaundice . The mechanism of hyperbilirubinemia is
(permeability, structure, or lipid content) or 3) through either increased production of bilirubin
abnormalities extrinsic to RBC (serum antibodies, (resulting from hemolysis, sepsis, blood extravasation
----------------------------------------------------------------------- or polycythemia) or increased enterohepatic
Professor of Hematology, Quaid-e- Azam Medical College,
Bahawalpur circulation (resulting from prematurity, pyloric
Demonstrator Pathology Quaid-e- Azam Medical College, stenosis, delayed bacterial gut colonization,
Bahawalpur gastrointestinal tract immobility or obstruction), or a
Correspondence to Dr. Saadia Aurangzeb Malik Email: decrease in bilirubin elimination which occurs in
saadiazeb@hotmail.com Crigler-Najjars and Gilberts syndromes
2
874 P J M H S Vol. 10, NO. 3, JUL SEP 2016
Saeed Ahmad Malik, M Aurangzeb Malik, Saadia Aurangzeb Malik
ABO incompatibility is usually found in the 65% and have neonatal hyperbilirubinemia as a
8
offsprings of women with blood type O and on common clinical feature .
occasions in mothers with both type A blood and Hyperbilirubinemia may also be a result of
3
having high anti-B IgG levels . ABO incompatibility increased oxidative stress. It is reported that bilirubin
may exist in approximately 1525% of all also functions as a scavenger of reactive oxygen
9
maternal/fetal pairs. However, ABO hemolytic species . Malondialdehyde (MDA) is a reactive
disease of the newborn is found in approximately 1% metabolic product that results from the effects of
of group O mothers who carry a high antenatal IgG reactive oxygen species on tissues and from a series
4 10
antibody titers . At present, with the use of of reactions that occur during lipid peroxidation .
prophylactic anti-D immunoglobulin has greatly
reduced the incidence of hemolytic disease of the MATERIALS AND METHODS
5
newborn resulting from Rh incompatibility .
G6PD deficiency is an X-linked recessive Investigations were carried out in all cases of
disease resulting in clinical manifestations such as significant jaundice, which included maternal and
neonatal jaundice, chronic nonspherocytic anemia, neonatal blood groups, serial levels of total serum
infections and drug-induced hemolysis . G6PD
6 bilirubin, direct bilirubin, Coombs test, hemoglobin
deficiency has been reported to be involved in the and hematocrit, reticulocyte count, and peripheral
7
genesis of neonatal hyperbilirubinemia . One of the blood smear. G6PD deficiency was screened in red
most serious complication of G6PD deficiency seen cells by a qualitative, visual colorimetric method using
in newborns is kernicterus resulting from severe dichlorophenol as dye. An 'Infection' being a cause
neonatal hyperbilirubinemia. Those infants who suffer of jaundice in newborn infants was ascribed to those
from chronic or acute fetal hypoxia have a higher risk with positive blood cultures and/or features of
of polycythemia, with hematocrit levels greater than infection necessitating antibiotics for 7 days, in the
absence of any other attributable cause for jaundice.
Data was analyzed using SPSS version 6.1.
RESULTS
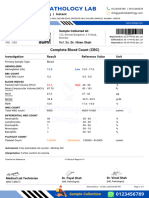
Table 1: Clinical and laboratory data
G6PD DEF Exaggerated Abo Hereditary Rh Drug Bacterial
Physio- Incompatbility Spherpcytosis Incompati- induced toxins
logical bility
Anemia + + ++ ++ ++ +++ +++
--
Jaundice + ++ + + +++ + ++
Splenomegaly + -- ++ ++ ++ + +
--
Hepatomegaly -- -- + + ++ -- +
-- --
Fever + -- -- + + +++
-- --
Coombs test - -- - - - ++ -
Reticulocytosis 5-10 % -- 10-12% 4-8% 15-20% 5-8% 15-20%
Abnormal Anisopoikilocyto Anisopoikilo- Anisopoikilo- Spherocytes Sphero- Anisopoikil Anisopoikil
morphology sis like broken cytosis cytosis cytes ocytosis ocytosis
egg shells ++
Urobilinogen Increased + Increased Increased Increased Increased Increased
Enzyme G6pd def N N N N N N
Table 2: Gender distribution of hemolytic anemia
Gender n %age
Male 38 63.3
Female 22 46.6
Table 3 : Causes of hemolyitic anemia in neonates
Cause of hemolytic anemia n %age Male %age Female %age
G6pd deficiency 2 3.3 2 100 0 0
Hereditary spherocytosis 4 6.6 4 100 0 0%
Rh incompatibility 9 15 5 55.5 4 44.4
Abo incompatibility 8 13 3 37.5 5 62.5
Infections 10 16.6 4 40 6 60
Drug induced 5 8.3 4 85.7 1 14.2
Exaggerated physiological 22 36.6 18 81 4 18.8
P J M H S Vol. 10, NO. 3, JUL SEP 2016 875
A Study of Various Causes of Indirect Hyperbilirubinemia in Neonates
DISCUSSION previously reported case series. While the rate of
17
infection is much lower than in Africa and
Neonatal hyperbilirubinemia is associated with a comparable to data from the Middle East and
variety of conditions. Severe NH poses a direct risk 18,19
India. . It still remains much higher than developed
of permanent neurological sequelae. Therefore, early countries, where sepsis accounts for less than 5% of
recognition of neonates who are at a higher risk of 20,21
significant hyperbilirubinemia . This indicates the
developing severe neonatal hyperbilirubinemia is of need for aggressively treating infection associated
17
paramount importance to preventing brain damage . with jaundice.
In our study, physiological jaundice is found to be Hemolytic jaundice accounted for almost 20% of
the most frequent cause of neonatal jaundice 36%. all significant jaundice, with ABO and Rh
These findings are comparable to various national incompatibility contribute to two thirds of the total.
18,19
and international studies . Physiological aspects ABO incompatibility is usually reported as a milder
that can lead to neonatal hyperbilirubinemia include 22
disease in comparison to Rh disease, However
increased bilirubin production, less efficient hepatic newborns with ABO incompatibility in our series had
conjugation, and increased bilirubin absorption by more severe hemolysis with significantly higher
20
the enterohepatic circulation . Bilirubin has been an bilirubin and lower hemoglobin levels which is similar
effective antioxidant, and modest elevations of 12 23
21
to previous Pakistani reports and support the
bilirubin may be beneficial in neonates . contention that ABO incompatibility is a severe
ABO incompatibility and G6PD deficiency were 24
disease in South Asia . While studies from northern
found to be frequent causes of neonatal Pakistan (predominantly Pathan ethnicity) reports a
hyperbilirubinemia in our study, as well as in other 13,25
7-8% prevalence of G6PD, deficiency . Our results
studies. The deficiency of G6PD is the one of most from Bahawalpur, a multiethnic city in the Southern
common human genetic enzymopathy, affecting over Punjab region of Pakistan reveal a figure of 3%. This
200 million individuals worldwide. It has been is comparable to reports from Singapore, and
associated with neonatal jaundice, chronic 26,27
Malaysia although less than reports from the
nonspherocytic hemolytic anemia, favism and food- 28 29
22
Middle East and India However, all cases of
or drug-induced acute hemolytic anemia . G6PD deficiency had evidence of severe hemolysis.
In majority of cases, ABO hemolytic disease of Despite this low prevalence, given that G6PD
newborns causes hyperbilirubinemia without severe deficiency has hemolytic jaundice with comparable
neonatal anemia, which is due to few group A or B severity to ABO and Rh incompatibility, we would
antigens on neonatal red blood cells and the recommend a qualitative G6PD deficiency test in all
presence of A and B antigens on other tissues and in Pakistani newborns with suspected hemolysis.
24
body fluids . This fact is also revealed in our study,
as most ABO incompatible cases had normal CONCLUSION
hemoglobin levels. In the indirect hyperbilirubinemia
group, Rh hemolytic disease of the newborns is in In summary, our data from this study done in
agreement with previous studies, that depicted that Bahawalpur reveals prevalence of significant
Rh hemolytic disease of the newborn is less common jaundice of which a fifth were attributable to hemolytic
than previously due to the administration of Rh Ig, causes. Infection accounted for a large proportion
which results in a greater than 90% reduction in the (16%) of all cases and in 36% labeled as
30,31
alloimmunization rate among treated women .Our exaggerated physiological jaundice. ABO and Rh
data highlight the importance of drugs, infection and isoimmunization, G6PD deficiency and sepsis were
ABO and Rh incompatibility in newborns with independent risk factors for severe jaundice.
significant jaundice in Bahawalpur and also of G6PD
deficiency in this study. Due to lack of sophisticated REFERENCES
laboratory facilities, we were unable to further
1. Maisels, M. J. et al. Hyperbilirubinemia in the Newborn
analyze the subcategory of miscellaneous hemolyses Infant $35 Weeks Gestation: An Update With
to determine specific etiologies. Multiple etiologies Clarifications. Pediatrics 124, 1193
are found to operate in several newborns, e.g., 1198,doi:10.1542/peds.2009-0329 (2009).
infection and prematurity whereas we primarily 2. Dennery, P. A., Seidman, D. S. & Stevenson, D. K.
ascribed physiological jaundice as the dominant Neonatal Hyperbilirubinemia. N Engl J Med 344, 581
etiology in our analysis. Infection (16%) was the 590, doi:10.1056/NEJM200102223440807 (2001).
second most common etiology, it was still less than a 3. Wang, M., Hays, T., Ambruso, D. R., Silliman, C. C. &
1 Dickey, W. C. Hemolytic disease of the newborn
figure of 53% previously reported from Pakistan .
This is probably because of the selective nature of caused by a high titer anti-group B IgG from a group A
876 P J M H S Vol. 10, NO. 3, JUL SEP 2016
Saeed Ahmad Malik, M Aurangzeb Malik, Saadia Aurangzeb Malik
mother. Pediatr Blood Cancer 45, 861862, 18. AI-Magamci MSF, Khan A, Bhat BA, Nadroo AM, Itoo
doi:10.1002/pbc.20503 (2005). B A. Neonatal jaundice: An etiological survey in the
4. Chen, J. Y. & Ling, U. P. Prediction of the development Madinah region. Ann Saudi Med 1996; 16: 221-223.
of neonatal hyperbilirubinemia in ABO incompatibility. 19. Singh M, Deorari AK, Khajuria RC, Paul VK. A four
Zhonghua Yi Xue Za Zhi 53, 1318 (1994). year study on neonatal morbidity in a New Delhi
5. Roberts, I. A. G. The changing face of haemolytic hospital. Indian J Med Res 1991; 94: 186-]92.
disease of the newborn. Early Hum Dev 84, 515523 20. Guaran RL, Drew JH, Watkins AM. Jaundice: Clinical
(2008). practice in 88,000 liveborn infants. Aust NZ J Qbstet
6. Singhi, S. C. Does nimesulide induce haemolysis in Gynecol 1992; 32: 186-192.
glucose-6-phosphate dehydrogenase deficiency? Acta 21. Maisels MJ, Kring E. Risk of sepsis in newborns with
Paediatr. 92, 637638, doi:10.1111/j.1651- severe hyperbilirubinemia. Pediatrics 1992; 90: 741-
2227.2003.tb02524.x (2003). 743.
7. Kaplan, M., Herschel, M., Hammerman, C., Hoyer, J. 22. Clarke CA. Scientific basis of clinical practice:
D. & Stevenson, D. K. Hyperbilirubinemia Among Practical effects of blood group incompatibility between
African American, Glucose-6-Phosphate mother and fetus. Br Med J 1972; 2: 90-95.
Dehydrogenase-Deficient Neonates. Pediatrics 114, 23. ArifMA. Neonatal jaundice due to Rhesus and AB
e213e219 (2004). isoimmunization and frequency of these antigens in
8. Sarkar, S. & Rosenkrantz, T. S. Neonatal polycythemia Pakistani mothers. J Pak Med Assoc 1982; 2: 165-167.
and hyperviscosity. Semin Fetal Neonatal Med. 13, 24. Lucas GN. Neonatal jaundice due to ABO in-
248255 (2008). compatibility in Sri Lanka. Indian J Pediatr 1996; 63:
9. Saugstad, O. D. Free Radicals in Neonatal Intensive 381-384.
Care. In Tibboel, D. & Voort, E. (Eds.), Intensive Care 25. Bouma MJ, Goris M, Akhtar T, Khan E, Kita E.
in Childhood. Update in Intensive Care and Prevalence and clinical presentation of glu- cose-6-
Emergency Medicine Vol. 25:3652 (Springer Berlin phosphate dehydrogenase deficiency in Pakistani Path
Heidelberg, 1996). an and Afghan refugee communities in Pakistan:
10. Weinberger, B. et al. Association of Lipid Peroxidation Implications for the use of primaquine in regional
with Antenatal Betamethasone and Oxygen Radical malaria control pro- grams. Trans Royal Soc Trop Med
Disorders in Preterm Infants. Biol Neonate 85, 121 Hyg 1995; 89: 62-64.
127 (2004). 26. Tan KL. Phototherapy for neonatal jaundice in
11. Molina EG, Reddy KR. Postoperative jaundice. Clin erythrocyte. glucose-6-phosphate dehydrogenase
Liver Dis. 1999;3:47788.11. Sackey K. Hemolytic deficient infants. Pediatrics 1977; 59: 1023-1026.
anemia: part 1. Pediatr Rev. 1999;20:1528. 27. Singh H. Glucose-6-phosphate dehydrogenase
12. ArifMA. Neonatal jaundice in Pakistan. J Trop Pediatr deficiency: A preventable cause of mental re-
1984; 30: 213-216. tardation. Br Med J 1986; 295: 297-298.
13. Rehman H, Khan MA, Hameed A, Roghani MT, 28. Yaish HM, Niazi GA, Al Shalaan M, Khan S, Ahmed
Ahmad A. Erythrocyte G6PD deficiency and neonatal GS: Increased incidence of hyperbilirubinemia in
jaundice. J Pak Med Assoc 1995; 45: 259-260. 'unchallenged' glucose-6-phosphate dehydrogenase
14. Haneef SM. Pattern of neonatal disease. Paki- stan deficiency in term Saudi newborns. Ann Trop Paediatr
Paediatr J 1985; 9: 42-48. 1991; 11: 259-266.
15. AI-Magamci MSF, Khan A, Bhat BA, Nadroo AM, Itoo 29. Singhal PK, Singh M, Paul VK, Deorari AK, Ghorpade
B A. Neonatal jaundice: An etiological survey in the MG. Spectrum of neonatal hyperbilirubinemia: An
Madinah region. Ann Saudi Med 1996; 16: 221-223. analysis of 454 cases. Indian Pediatr 1992; 29: 319-
16. Kuruvilla KA, Sakumar ST, Jana AK. Glucose-6- 325.
phosphate dehydrogenase deficiency in neonatal 30. Garratty, G. Hemolytic disease of the newborn.
hyper-bilirubinemia in a south Indian referral hospital. (American Association of Blood Banks, 1984).
Indian Pediatr 1998; 35: 52- 55. 31. Irshad, M. et al. Prevalence of Rhesus type and ABO
17. Ahmed H, Yukubu AM, Hendrickse RG. Neonatal incompatibility in jaundiced neonates. Vol. 25 (2011).
jaundice in Zaria, Nigeria-A second prospective study.
West Afr J Med. 1995; 14: 15- 23
P J M H S Vol. 10, NO. 3, JUL SEP 2016 877
Anda mungkin juga menyukai
- CBC Test Report Format Example Sample Template Drlogy Lab ReportDokumen1 halamanCBC Test Report Format Example Sample Template Drlogy Lab ReportThota charanBelum ada peringkat
- Nelson JaundiceDokumen7 halamanNelson JaundiceJesly CharliesBelum ada peringkat
- Lovenox (Enoxaparin)Dokumen1 halamanLovenox (Enoxaparin)E100% (1)
- Forward and ReverseDokumen11 halamanForward and ReversecyrhenmieBelum ada peringkat
- Neonatal Jaundice - StatPearls - NCBI BookshelfDokumen14 halamanNeonatal Jaundice - StatPearls - NCBI BookshelfDhany karubuyBelum ada peringkat
- Neonatal Jaundice Assignment BCH 806Dokumen11 halamanNeonatal Jaundice Assignment BCH 806ukosam10Belum ada peringkat
- Ijph 45 558 PDFDokumen11 halamanIjph 45 558 PDFArifah Azizah ArifinBelum ada peringkat
- Hemolytic DiseaseDokumen10 halamanHemolytic DiseaseChino Paolo SamsonBelum ada peringkat
- Neonatal Anemia: Revisiting The Enigmatic PyknocyteDokumen5 halamanNeonatal Anemia: Revisiting The Enigmatic PyknocyteDavid MerchánBelum ada peringkat
- Neonatal Jaundice DR - MaslianiDokumen58 halamanNeonatal Jaundice DR - MaslianiHengky HanggaraBelum ada peringkat
- 2007 28 259 M. Catherine Driscoll: Pediatrics in ReviewDokumen12 halaman2007 28 259 M. Catherine Driscoll: Pediatrics in ReviewcharlesBelum ada peringkat
- HyperbilirubinemiaDokumen11 halamanHyperbilirubinemianursereview100% (12)
- NN HyperbilirubinemiaDokumen35 halamanNN Hyperbilirubinemiaanwar jabariBelum ada peringkat
- Jaundice Clinical Manifestation and Pathophysiology A Review ArticleDokumen3 halamanJaundice Clinical Manifestation and Pathophysiology A Review ArticleHany ZutanBelum ada peringkat
- Jaundice: Newborn To Age 2 Months: Education GapDokumen14 halamanJaundice: Newborn To Age 2 Months: Education GapRaul VillacresBelum ada peringkat
- ) Jaundice PDFDokumen4 halaman) Jaundice PDFAzzBelum ada peringkat
- Rhesus Type and Abo Incompatibility in Jaundiced NeonatesDokumen7 halamanRhesus Type and Abo Incompatibility in Jaundiced Neonatesdaniel_iosif_glBelum ada peringkat
- HEMOLYTIC DISEASE OF THE NEWBORN - Docx PrintDokumen6 halamanHEMOLYTIC DISEASE OF THE NEWBORN - Docx PrintJudy HandlyBelum ada peringkat
- Neonatal Hyperbilirubinemia - Risk Assessment and ManagementDokumen65 halamanNeonatal Hyperbilirubinemia - Risk Assessment and Managementchamarauw91Belum ada peringkat
- Neonatal Jaundice: AuthorsDokumen9 halamanNeonatal Jaundice: AuthorsRam Kumar ShresthaBelum ada peringkat
- Maternal and Neonatal Risk Factors of Hyperbilirubinemia Among Term and Preterm Newborns A Comparative StudyDokumen6 halamanMaternal and Neonatal Risk Factors of Hyperbilirubinemia Among Term and Preterm Newborns A Comparative StudyEditor IJTSRDBelum ada peringkat
- Neonatal JaundiceDokumen12 halamanNeonatal JaundiceGiska T PutriBelum ada peringkat
- 113 Shruti Kadam Sem 6 Biochem P1 U3 AssignmentDokumen4 halaman113 Shruti Kadam Sem 6 Biochem P1 U3 AssignmentRomil DaghaBelum ada peringkat
- Neonatal Jaundice Assessment and ManagementDokumen10 halamanNeonatal Jaundice Assessment and ManagementibanggBelum ada peringkat
- Neonatal Jaundice and Liver DiseaseDokumen1 halamanNeonatal Jaundice and Liver DiseaseVillapaoBelum ada peringkat
- Jaundice Newborn - 2Dokumen15 halamanJaundice Newborn - 2Miratunnisa AzzahrahBelum ada peringkat
- BB OriginalDokumen14 halamanBB Originalstone siehBelum ada peringkat
- Neonatal JaundiceDokumen48 halamanNeonatal JaundiceRemy MartinsBelum ada peringkat
- Newborn jaundice causes, pathophysiology and managementDokumen32 halamanNewborn jaundice causes, pathophysiology and managementviyolaazzahraBelum ada peringkat
- Prevalence and Causes of Neonatal Jaundice in Nepali HospitalDokumen4 halamanPrevalence and Causes of Neonatal Jaundice in Nepali HospitalkattysarkBelum ada peringkat
- Newborn Jaundice: Causes, Symptoms and TreatmentDokumen6 halamanNewborn Jaundice: Causes, Symptoms and TreatmentGeo ClimBelum ada peringkat
- UNIT HyperbilirubinemiaDokumen17 halamanUNIT Hyperbilirubinemiaurmila dewanBelum ada peringkat
- 2506-Article Text-13783-1-10-20201214Dokumen4 halaman2506-Article Text-13783-1-10-20201214Venus PlanetBelum ada peringkat
- Gomella's Neonatology, 8th Edition 2020, EdithDokumen62 halamanGomella's Neonatology, 8th Edition 2020, Edithmaryano 0015Belum ada peringkat
- Neonatal JaundiceDokumen3 halamanNeonatal JaundicevorezBelum ada peringkat
- 8 Th. Lec. Hemolytic Disease of The Newborn and FetusDokumen32 halaman8 Th. Lec. Hemolytic Disease of The Newborn and Fetusda202263357026Belum ada peringkat
- Original Article: Prevalence of Glucose-6-Phosphate Dehydrogenase Deficiency in Neonates in EgyptDokumen4 halamanOriginal Article: Prevalence of Glucose-6-Phosphate Dehydrogenase Deficiency in Neonates in EgyptSriarbiatiBelum ada peringkat
- Manuscript 2Dokumen5 halamanManuscript 2maryBelum ada peringkat
- Neonatal Jaundice: Causes and TreatmentsDokumen18 halamanNeonatal Jaundice: Causes and TreatmentsArinaManaSikanaBelum ada peringkat
- Neonatal HandbookDokumen11 halamanNeonatal HandbookJanua NavaretteBelum ada peringkat
- Anemia FetalDokumen9 halamanAnemia FetalCarolina Cabrera CernaBelum ada peringkat
- Jaundice in The NewbornDokumen18 halamanJaundice in The NewbornSuardimanAchoBelum ada peringkat
- Jaundice: Nccu Clinical Guidelines S: 10Dokumen3 halamanJaundice: Nccu Clinical Guidelines S: 10Gomathi Sankara Narayanan VenkataramanBelum ada peringkat
- Bili Blanket For Neonatal JaundiceDokumen9 halamanBili Blanket For Neonatal JaundicehamidhaBelum ada peringkat
- Hemolitic AutoimunDokumen3 halamanHemolitic Autoimun08- Ridho Nur CahyoBelum ada peringkat
- Recurrent Non-Immune Fetal Hydrops: A Case ReportDokumen3 halamanRecurrent Non-Immune Fetal Hydrops: A Case ReportHervi LaksariBelum ada peringkat
- HrtuyftdtyujytygujfDokumen52 halamanHrtuyftdtyujytygujfNichole Audrey SaavedraBelum ada peringkat
- Angelic - Doc - Neonatal JaundiceDokumen16 halamanAngelic - Doc - Neonatal JaundiceAngy100% (5)
- A Comparative Clinical Investigation of Hyper Bilirubinemia in Babies With Low and Normal Birth WeightsDokumen14 halamanA Comparative Clinical Investigation of Hyper Bilirubinemia in Babies With Low and Normal Birth WeightsInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- T15 - Neonatal JaundiceDokumen38 halamanT15 - Neonatal JaundiceMawuliBelum ada peringkat
- NIH Public Access: Neonatal CholestasisDokumen21 halamanNIH Public Access: Neonatal CholestasismkafabillahBelum ada peringkat
- p599 PDFDokumen8 halamanp599 PDFMiftakhul HudaBelum ada peringkat
- Red Blood Cell Enzyme DisordersDokumen17 halamanRed Blood Cell Enzyme DisordersGustavo GCBelum ada peringkat
- Presentation and Duration of Neonatal JaundiceDokumen5 halamanPresentation and Duration of Neonatal JaundiceRizki DaulayBelum ada peringkat
- New Diagnosis Criteria For Common Variable Immunodeficiency Exploration Systematic Review and Current PerspectivesDokumen8 halamanNew Diagnosis Criteria For Common Variable Immunodeficiency Exploration Systematic Review and Current PerspectivesInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Conjugated Bilirubin Direct Bilirubin Unconjugated Bilirubin Indirect BilirubinDokumen12 halamanConjugated Bilirubin Direct Bilirubin Unconjugated Bilirubin Indirect BilirubinTanviBelum ada peringkat
- Neonatal JaundiceDokumen4 halamanNeonatal JaundiceChristian Eduard de DiosBelum ada peringkat
- Research questions on blood typing procedures and hemolytic disease of the newborn (HDNDokumen3 halamanResearch questions on blood typing procedures and hemolytic disease of the newborn (HDNBrielleBelum ada peringkat
- Hemoglobinopathy Screening in Reproductive Age Women Using HPLCDokumen6 halamanHemoglobinopathy Screening in Reproductive Age Women Using HPLCNavtej kumarBelum ada peringkat
- A Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaDari EverandA Model for Gene Therapy: Gene Replacement in the Treatment of Sickle Cell Anemia and ThalassemiaBelum ada peringkat
- Orbital Trauma: The Radiology ofDokumen34 halamanOrbital Trauma: The Radiology ofRahmah Wanti100% (1)
- Chart Gizi WhoDokumen2 halamanChart Gizi WhoRahmah WantiBelum ada peringkat
- Age and Sex Identification Using Multislice Computed Tomography Ofthe Last Thoracic Vertebrae of An Egyptian Sample 2157 7145 1000386 PDFDokumen6 halamanAge and Sex Identification Using Multislice Computed Tomography Ofthe Last Thoracic Vertebrae of An Egyptian Sample 2157 7145 1000386 PDFRahmah WantiBelum ada peringkat
- Effect of Phototherapy On Serum Calcium Level in Neonatal JaundiceDokumen5 halamanEffect of Phototherapy On Serum Calcium Level in Neonatal JaundiceRahmah WantiBelum ada peringkat
- Jurnal Foren 5Dokumen6 halamanJurnal Foren 5Rahmah WantiBelum ada peringkat
- 853 3845 1 PBDokumen5 halaman853 3845 1 PBRahmah WantiBelum ada peringkat
- Dna 1Dokumen4 halamanDna 1Rahmah WantiBelum ada peringkat
- EtioDokumen6 halamanEtioRahmah WantiBelum ada peringkat
- 853 3845 1 PBDokumen5 halaman853 3845 1 PBRahmah WantiBelum ada peringkat
- Jurnal 1 Mata Globe 2017Dokumen4 halamanJurnal 1 Mata Globe 2017Rahmah WantiBelum ada peringkat
- Spasmodic Dysphonia A Laryngeal Control Disorder Specific PDFDokumen5 halamanSpasmodic Dysphonia A Laryngeal Control Disorder Specific PDFRahmah WantiBelum ada peringkat
- Update in Trauma Anesthesiology Perioperative.12Dokumen8 halamanUpdate in Trauma Anesthesiology Perioperative.12ramaBelum ada peringkat
- 084-Feat.-Hoarseness (Goldstein) PDFDokumen5 halaman084-Feat.-Hoarseness (Goldstein) PDFRahmah WantiBelum ada peringkat
- Kjim 2015 137Dokumen9 halamanKjim 2015 137Rahmah WantiBelum ada peringkat
- Circulatory ShockDokumen9 halamanCirculatory ShockTri UtomoBelum ada peringkat
- Hematuria - 2 PDFDokumen10 halamanHematuria - 2 PDFRahmah WantiBelum ada peringkat
- Beta-Thalassemia Intermedia: An IntroductionDokumen4 halamanBeta-Thalassemia Intermedia: An IntroductionMaLik ZaKwan IwAnBelum ada peringkat
- Principles in Medical Laboratory Science 2: Phlebotomy Kit and AnticoagulantsDokumen5 halamanPrinciples in Medical Laboratory Science 2: Phlebotomy Kit and AnticoagulantsDio Aura NobleBelum ada peringkat
- Coombs TestDokumen11 halamanCoombs TestunilabreynosaBelum ada peringkat
- Protoporphyrin Screening: DeficiencyDokumen7 halamanProtoporphyrin Screening: DeficiencyFanny Trestanita BahtiarBelum ada peringkat
- Thrombocytopenia in Pregnancy Web FriendlyDokumen8 halamanThrombocytopenia in Pregnancy Web FriendlyAthishPanchpersadhBelum ada peringkat
- Practical 3: Blood Grouping Test ObjectiveDokumen2 halamanPractical 3: Blood Grouping Test ObjectiveTHASVIN OFFICIAL NETWORKBelum ada peringkat
- Genetics in Blood BankingDokumen47 halamanGenetics in Blood BankingMandy A. Delfin100% (3)
- Blood Case 6Dokumen12 halamanBlood Case 6إنعام الحفيانBelum ada peringkat
- Clotting Time Macromethod: Utilized Larger Amount of BloodDokumen4 halamanClotting Time Macromethod: Utilized Larger Amount of BloodGerly MaglangitBelum ada peringkat
- 10 2 Neonatal TransfusionDokumen6 halaman10 2 Neonatal TransfusionfatmaBelum ada peringkat
- Physio 2.05 Bloodphysiology2 HemostasisDokumen9 halamanPhysio 2.05 Bloodphysiology2 HemostasisSimon Peter Familara100% (1)
- Red Blood Cell Indices: DR KatekDokumen10 halamanRed Blood Cell Indices: DR KatekNathan Lupiya100% (1)
- Difficult Crossmatch1Dokumen13 halamanDifficult Crossmatch1Devie MaraBelum ada peringkat
- Antithrombotic DrugsDokumen11 halamanAntithrombotic DrugsKatyBrnBelum ada peringkat
- #081121 JBMTCT Ed07 Consenso PediatricoDokumen231 halaman#081121 JBMTCT Ed07 Consenso Pediatricobach75Belum ada peringkat
- Diagrammatic Description of Blood Preparation ProcessesDokumen17 halamanDiagrammatic Description of Blood Preparation ProcessesJes CmtBelum ada peringkat
- Eurton Electric Co., Inc.: AbbottDokumen16 halamanEurton Electric Co., Inc.: Abbottjose navaBelum ada peringkat
- 1-4 Hemostasis, Surgical Bleeding and TransfusionDokumen17 halaman1-4 Hemostasis, Surgical Bleeding and TransfusionRobin Tolentino100% (3)
- Blood Group: Made By:-Vedant PatelDokumen18 halamanBlood Group: Made By:-Vedant PatelVedant PatelBelum ada peringkat
- (S.C. Rastogi) Essentials of Animal Physiology, 4t (BookSee - Org) 246Dokumen1 halaman(S.C. Rastogi) Essentials of Animal Physiology, 4t (BookSee - Org) 246Indah Rizka AprilianiBelum ada peringkat
- Experiment No.6 Blood Grouping and Blood Typing Objective: Materials: ProcedureDokumen3 halamanExperiment No.6 Blood Grouping and Blood Typing Objective: Materials: ProcedureClaveria Jeric FernandezBelum ada peringkat
- Disorders of Red Blood CellsDokumen27 halamanDisorders of Red Blood Cellskirti sharmaBelum ada peringkat
- Understanding Thrombophilia Risk FactorsDokumen9 halamanUnderstanding Thrombophilia Risk FactorsSeraj Abed ElmoatiBelum ada peringkat
- Biochemistry Report: Test Is Carried Out by Dimension EXL 200Dokumen1 halamanBiochemistry Report: Test Is Carried Out by Dimension EXL 200KH. A. H. M. SAYEF 1706024Belum ada peringkat
- BIOCHEMISTRY TEST LOINC CODESDokumen15 halamanBIOCHEMISTRY TEST LOINC CODESSowji PBelum ada peringkat
- Coagulation Factor DisordersDokumen35 halamanCoagulation Factor DisordersMelesBelum ada peringkat
- Neonatal Jaundice: Causes, Symptoms, and TreatmentDokumen8 halamanNeonatal Jaundice: Causes, Symptoms, and TreatmentNatosha MendozaBelum ada peringkat