Queti A Pine
Diunggah oleh
Herry HendrayadiJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Queti A Pine
Diunggah oleh
Herry HendrayadiHak Cipta:
Format Tersedia
CLINICAL CONSULTATION Quetiapine
C L I N I C A L C O N S U LTAT I O N
Quetiapine for insomnia: A review of the literature
Sarah L. Anderson and Joseph P. Vande Griend
P
opulation-based estimates have
indicated that as many as 30% Purpose. The safety and efficacy of que- active control (e.g., zolpidem); the data that
of adults have symptoms of in- tiapine for the treatment of insomnia in exist compare quetiapine to a placebo or
adults are reviewed. there is no comparison and all patients are
somnia, and 10% experience daytime
Summary. Quetiapine was developed for treated with quetiapine. Very few studies
impairment or stress due to their the treatment of psychiatric disorders, but have evaluated quetiapines efficacy in the
insomnia.1 Insomnia can result in its antagonism of histamine H1- and sero- treatment of insomnia using sleep objective
decreased quality of life, decreased tonin type 2A receptors has the added effect testing, another limitation of the available
work productivity, increased risk of of causing sedation. As such, quetiapine data on quetiapine.
accidents (e.g., motor vehicle acci- is widely used off-label as a treatment for Conclusion. Robust studies evaluating the
dents, work-related accidents), and insomnia. Due to quetiapines potential safety and efficacy of quetiapine for the
adverse effects, guidelines for the treatment treatment of insomnia are lacking. Given its
increased health care utilization.1,2
of insomnia have recommended the drugs limited efficacy data, its adverse-effect pro-
People with insomnia are more likely use only in patients with specific comorbid file, and the availability of agents approved
to be absent from work and to use psychiatric disorders. The use of quetiapine by the Food and Drug Administration for
more health care resources com- for the treatment of insomnia in the absence the treatment of insomnia, quetiapines
pared with people without insomnia, of comorbid conditions has been evaluated benefit in the treatment of insomnia has
resulting in increased costs to both in only two clinical trials of 31 patients in not been proven to outweigh potential
patients and society.3,4 total, and very few studies have evaluated risks, even in patients with a comorbid
quetiapine use in patients with insomnia labeled indication for quetiapine.
Insomnia is often chronic in na-
and other comorbidities. No trials have been Am J Health-Syst Pharm. 2014; 71:394-
ture. In a population-based study conducted comparing quetiapine with an 402
of 388 adults with insomnia, 74%
reported having insomnia for at
least one year, and 46% continued to
have insomnia after three years.5 The
chronic nature of insomnia implies concomitant psychiatric disorder.1 as such, insomnia in the presence
the potential for long-term drug The comorbid psychiatric disorder of a psychiatric disorder should be
therapy, particularly with sedative most commonly associated with in- considered a comorbid condition.7
hypnotics, a controversial topic be- somnia is depression, but insomnia Common mechanisms are thought
yond the scope of this article.6 has also been associated with anxiety, to underlie insomnia and psychiatric
Insomnia is frequently associ- substance abuse, and posttraumatic disorders, suggesting that, while a
ated with psychiatric disorders. Es- stress disorder.1-4,7-9 Insomnia can be person may be predisposed to both, it
timates report that as many as 40% either a cause or a consequence of might be possible to treat both con-
of patients with insomnia have a an underlying psychiatric disorder; ditions with the same treatment.1-4,8,9
Sarah L. Anderson, Pharm.D., BCPS, is Assistant Professor, Skaggs The authors have declared no potential conflicts of interest.
School of Pharmacy and Pharmaceutical Sciences, University of
Colorado, Aurora, and Clinical Pharmacy Specialist, Denver Health Copyright 2014, American Society of Health-System Pharma-
Medical Center, Denver, CO. Joseph P. Vande Griend, Pharm.D., cists, Inc. All rights reserved. 1079-2082/14/0301-0394$06.00.
BCPS, CGP, is Assistant Professor, Skaggs School of Pharmacy and DOI 10.2146/ajhp130221
Pharmaceutical Sciences, University of Colorado.
Address correspondence to Dr. Anderson (sarah.anderson@
ucdenver.edu).
394 Am J Health-Syst PharmVol 71 Mar 1, 2014
CLINICAL CONSULTATION Quetiapine
The Clinical Consultation section features the treatment of insomnia, particu- search was limited to clinical trials,
articles that provide brief advice on how to larly in prison and military popula- human studies, and studies written
handle specific drug therapy problems. All tions, with significant cost implica- in English. Of the 25 studies identi-
articles are based on a systematic review tions. A recent study of low-dose fied using these criteria, 13 were in-
of the literature. The assistance of ASHPs quetiapine use (<100 mg daily) in cluded in this review. Twelve studies
Section of Clinical Specialists and Scientists the New Jersey prison population were excluded because the enrolled
in soliciting Clinical Consultation submis- highlighted the frequency of the participants did not have a diagnosis
sions is acknowledged. Unsolicited submis- drugs use for insomnia as well as of insomnia at baseline.
sions are also welcome. the expense of brand-name que- Outpatient insomnia manage-
tiapine (Seroquel, AstraZeneca).16 ment. Cohrs et al.21 performed a
At the beginning of the study, as randomized, double-blind, placebo-
many as 12 patients per psychiatrist controlled crossover study to exam-
Rationale for and prevalence of were taking low-dose quetiapine ine the effects of quetiapine on the
quetiapine use for insomnia for insomnia. The average whole- polysomnographic sleep structure
Quetiapine is a dibenzothiaz- sale price was $4.50 per tablet of and subjective sleep quality of 14
epine derivative with Food and Drug quetiapine (50 or 100 mg) com- healthy men (mean age, 27 years old).
Administration (FDA)-approved pared with $0.05 per tablet of hy- Each participant was studied three
labeling for the treatment of schizo- droxyzine hydrochloride (100 mg), times for three consecutive nights
phrenia and acute manic, depres- making quetiapine 90 times more four days apart. No treatment was
sive, or mixed episodes of bipolar expensive than hydroxyzine, anoth- administered on night 0. On nights 1
I disorder; maintenance treatment er agent used to treat insomnia.16 and 2, participants received placebo,
of bipolar I disorder in combina- A retrospective chart review of quetiapine 25 mg, or quetiapine 100
tion with lithium or divalproex; 692 soldiers treated with quetiapine mg orally one hour before sleep.
and adjunctive treatment of major at Madigan Army Medical Center in Participants slept in standard sleep
depressive disorder.10,11 Quetiapine Tacoma, Washington, revealed that laboratory conditions on night 1; on
has also been used for the off-label the most common indications for night 2, acoustic stress was applied.
treatment of anxiety disorders, de- quetiapine use were insomnia (57%) Compared with placebo, quetiapine
mentia, autism, refractory obsessive- and anxiety (20%).17 Further, only improved sleep latency, total sleep
compulsive disorder, delirium, and 9.4% of soldiers were prescribed time, and sleep efficiency (p < 0.01,
insomnia. 12,13 It exhibits a strong quetiapine for an FDA-approved p < 0.001, and p < 0.001, respective-
affinity for antagonism at hista- indication. According to the Associ- ly) compared with placebo. Specific
mine H1-receptors, similar to that ated Press, the Pentagon and the polysomnographic data are provided
of diphenhydramine, amitriptyline, Department of Veterans Affairs spent in Table 1. Similar findings were
mirtazapine, and doxepin, and has a $8.6 million and $125.4 million on noted in the subjective sleep quality
moderate affinity for serotonin type quetiapine in 2009, respectively.18 scores and time scores on the visual
2A (5-HT2A) receptors.14 Antagonism Information on the use of quetiapine analog scale and sleep question-
at these receptor sites is thought to be in the general population is more naires. The number of awakenings
the primary mechanism behind que- elusive; however, off-label use is fre- experienced was fewer in participants
tiapines sedative properties.14 Due to quent. In 2002, quetiapine was sixth randomized to quetiapine versus
quetiapines potential adverse effects on the list of the top 16 drugs used to placebo but was not significantly dif-
(e.g., orthostatic hypotension, weight treat insomnia.19 Quetiapine became ferent (p = 0.10). Overall, quetiapine
gain, hyperlipidemia, hyperglyce- available in generic form in March was well tolerated. Two volunteers
mia), guidelines for the treatment 2012 but is still considerably costly, withdrew from the study after ex-
of insomnia have recommended the approximately $6$7 per tablet for periencing orthostatic hypotension
drugs use only in patients who have 50- and 100-mg tablets.20 after receiving 100 mg of quetiapine;
a comorbid psychiatric disorder and This article examines the safety these participants were not included
in those who may benefit from the and efficacy of quetiapine use for the in the data analysis. The other ad-
primary action of [the drug] as well treatment of insomnia. verse effect of note was periodic leg
as from the sedating effect.15 movement, which was most preva-
Despite the recommendation Literature review lent in the individuals who received
to limit its use to individuals with A literature search was performed quetiapine 100 mg. This study was
a comorbid psychiatric disorder, using PubMed and MEDLINE limited by its small sample size and
the medical literature has reported (1950April 2013) with the search the fact that subjects took quetiapine
widespread use of quetiapine for terms quetiapine and insomnia. The for only two nights.
Am J Health-Syst PharmVol 71 Mar 1, 2014 395
CLINICAL CONSULTATION Quetiapine
Insomnia disorder. To date, two based on both objective and subjec- used for the treatment of psychiatric
published studies have evaluated tive data (Tables 1 and 2). Total sleep disorders.
the use of quetiapine specifically for time and sleep efficiency evaluated by Tassniyom et al.23 conducted a
the treatment of insomnia. In an polysomnography were significantly small, randomized, double-blind,
open-label pilot study by Wiegand et improved at weeks 2 and 6 (p = 0.05). placebo-controlled trial in 16 Thai
al.,22 18 adults with insomnia (demo- Similarly, the Pittsburgh Sleep Qual- adults with a diagnosis of insomnia
graphics not reported) were treated ity Index (PSQI) score and subscores based on criteria established by the
with quetiapine 25 mg orally at bed- were statistically improved at both Diagnostic and Statistical Manual, 4th
time. The dosage of quetiapine was weeks 2 and 6 (Table 1). The most edition, Text Revision (DSM-IV-TR).
increased to 50 mg in 7 patients and frequently reported adverse effects Participants mean age was 46 years,
to 75 mg in 1 patient. Patients experi- were dry mouth and transient morn- and the majority were women.
enced improvement in sleep param- ing hangover effects. Importantly, Patients were excluded if they had
eters after two weeks and continued quetiapine promoted sleep in these comorbid psychiatric conditions or
to show improvements at six weeks patients at dosages well below those were already receiving medications
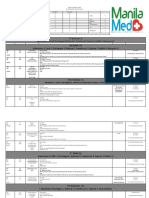
Table 1.
Subjective Evaluations of Quetiapine for Insomniaa
Ref. Intervention Evaluation Findings
22 Quetiapine 2575 mg daily PSQI Quetiapine showed statistical improvement (p = 0.00) on
the total score and subscale scores of sleep quality, total
sleep time, and sleep efficiency at weeks 2 and 6.
23 Quetiapine 25 mg daily VAS Sleep satisfaction scores improved for both groups and
were not statistically different (p = 0.505).
24 Quetiapine 315 109 mg daily HAM-D Insomnia Subscale Quetiapine significantly (p < 0.001) improved items 46
compared to placebo.
25 Quetiapine 25100 mg daily MADRS Insomnia Quetiapine plus fluoxetine improved the mean insomnia
score sooner (p 0.01 for the first, second, and third
follow-up visits) compared with the fluoxetine plus
placebo group.
26 Quetiapine 300 or 600 mg PSQI Both doses of quetiapine showed statistical improvement
daily (p < 0.001) at days 29 and 57 compared to placebo.
27 Quetiapine 300 or 600 mg MADRS Insomnia Both doses of quetiapine showed statistical improvement
daily vs. paroxetine 20 mg (p < 0.05) on item 4 (reduced sleep) compared to
daily paroxetine.
28 Quetiapine 12.550 mg daily PSQI PSQI improved in 11 patients and was reduced by 3.9 3.8
points (p < 0.01).
29 Quetiapine 25100 mg daily ISI For 5 of 6 patients, the ISI score moved from moderate
insomnia to absence of insomnia at week 1 and was
maintained through week 6.
30 Quetiapine 25225 mg daily SSQ 75% improvement in global score; greatest improvements
in overall quality of sleep and sleep latency.
31 Quetiapine 50750 mg daily PSQI A significant time effect for total score occurred after
vs. olanzapine 2.520 mg 8 weeks in both middle-aged and elderly patients,
daily, risperidone 112 mg regardless of drug (p = 0.008).
daily, and perospirone 448
mgb daily
33 Quetiapine 340 mg (mean) PSQI Most improved quality of sleep occurred in the patients
daily in the upper quetiapine quartile (>360-mg mean daily
dose). The strongest reduction in daytime sedation was
observed in patients receiving the highest quetiapine
doses.
a
PSQI = Pittsburgh Sleep Quality Index, VAS = visual analog scale, HAM-D = Hamilton Rating Scale for Depression, MADRS = Montgomery-sberg Depression Rating
Scale, ISI = Insomnia Severity Index scale, SSQ = Spiegel Sleep Questionnaire.
b
Not available in the United States.
396 Am J Health-Syst PharmVol 71 Mar 1, 2014
CLINICAL CONSULTATION Quetiapine
known to cause sedation. Patients of the study may have been too short ficacy outcome was improvement
received either placebo or quetiapine to determine if there was a difference in the Hamilton Rating Scale for
25 mg orally nightly for two weeks. between quetiapine and placebo with Depression (HAM-D) score, which
A total of 13 participants (6 in the regard to improvement in sleep. included an evaluation of the sub-
placebo group, 7 in the quetiapine None of the aforementioned stud- scale for insomnia (items 46). The
group) completed the study. One ies reported on changes in metabolic insomnia subscale scores improved
person in the quetiapine group variables (e.g., weight, waist circum- over baseline by week 2, and this ef-
withdrew after being diagnosed with ference, fasting glucose concentra- fect was maintained through week 20
vertigo, and 2 participants in the tion, lipid profile). This was likely (Table 1). Of the 14 patients studied,
placebo group withdrew citing lack not done due to the small sample 3 experienced hypotension and 2 had
of efficacy; all 3 individuals withdrew sizes, short durations, and relatively daytime sedation, all of which were
before receiving the intervention. healthy populations evaluated. noted to be mild and transient in
Both the quetiapine and placebo Major depressive disorder. agud et nature. Four patients were noted to
groups experienced increased total al.24 conducted a prospective, open- have hyperlipidemia at baseline, but
sleep time (by 125 and 72 minutes, label, noncomparative, flexible-dose no metabolic outcomes (e.g., change
respectively), decreased sleep latency study to evaluate the efficacy of in lipid values) were reported. The
(by 96 and 24 minutes, respectively), quetiapine add-on therapy in 14 authors concluded that quetiapine
and improved sleep satisfaction patients with major depressive disor- alleviated insomnia, a common and
based on visual analog scale scores, der (defined using DSM-IV criteria) severe symptom of depression, in pa-
but none of the differences between who were refractory to previous tients enrolled in this study and this
groups were significant (p > 0.05) therapy. The mean age of patients was perceived as a beneficial effect.
(Tables 1 and 2). Adverse effects was 53 years, and the majority were Garakani et al.25 evaluated the
were observed only in the quetiap- men. Quetiapine 50 mg was added to ability of quetiapine to augment
ine group and included dry lips, dry patients current antidepressant regi- fluoxetine therapy over eight weeks
tongue, and daytime drowsiness. men at bedtime, with dosage increas- in 114 patients with major depres-
The authors acknowledged that the es in increments of 50 mg; the mean sive disorder, as defined by DSM-IV
small sample size rendered the study S.D. bedtime dose in study patients criteria. A total of 51 men (mean
underpowered and that the duration was 315 109 mg. The primary ef- age, 41 years) and 64 women (mean
Table 2.
Objective Evaluations of Quetiapine for Insomnia via Polysomnography or Actigraphy
Mean S.D. No. Occurences S.D.
Sleep Total Sleep Sleep Periodic Leg
Ref. and Intervention Latency, min Time, min Efficiency, % Awakenings Movements
21
Quetiapine 25 mg daily 12.2 6.1a,b 439.9 20.5c 91.8 4.2c 27 7.7 62.2 78.1
Quetiapine 100 mg daily 13.3 8.5 a,b 441.4 23.4c 92.0 4.8c 24.9 10.1 138.4 153.8c
Placebo 22.8 18.4b 411.4 37.7 85.8 7.9 30.0 11.3 41.2 63.2
22
Quetiapine 2575 mg daily 24.2 19.0 395.6 62.3d 89.9 8.2d . . .e ...
23
Quetiapine 25 mg daily 66.5 51.2 347.5 100.9 ... ... ...
Placebo 47.4 30.4 361.9 85.4 ... ... ...
32
Quetiapine 340 mg (mean) 15.6 18.1f 432 66 82.7 9.1f ... ...
daily
No therapy (control) 24.5 30.2 390 54 77.0 7.9 ... ...
a
p < 0.005 compared with placebo.
b
Sleep stage 2.
c
p < 0.001 compared with placebo.
d
p < 0.05 compared with baseline.
e
Not evaluated.
f
p < 0.05 at week 4 compared with control.
Am J Health-Syst PharmVol 71 Mar 1, 2014 397
CLINICAL CONSULTATION Quetiapine
age, 42 years) participated in this studies that randomized 1051 pa- majority of patients were women,
randomized, double-blind, placebo- tients who were experiencing a major and the mean age was approximately
controlled trial. The study allowed for depressive episode of bipolar I or 39 years. Both dosages of quetiapine
flexible dosing of quetiapine (start- II disorder (as defined by DSM-IV produced significant improvements
ing dosage of 25 mg daily adjusted criteria) to monotherapy with fixed- in sleep compared with placebo;
in 25-mg increments every third dose quetiapine 300 or 600 mg daily the same was not true of paroxetine
day to a maximum of 100 mg daily); or placebo for eight weeks. The ma- (Table 1). As in the BOLDER I study,
the mean dosage was 47.3 mg daily. jority of patients were women, and the most common patient-reported
Quetiapine and placebo were admin- the mean age was approximately 38 adverse effects of quetiapine were
istered in the evening. All patients years. Data on the quality of sleep dry mouth, somnolence, and seda-
received concurrent fluoxetine 2040 from the BOLDER I trial (n = 511) tion. In the EMBOLDEN II study,
mg daily. The main outcome mea- were analyzed. Improvements in 911.3% of patients in the quetiapine
sure was the Montgomery-sberg PSQI scores for both dosages of groups experienced clinically signifi-
Depression Rating Scale (MADRS) quetiapine at days 29 and 57 were cant weight gain (greater than 7% of
score, with a focus on the sleep item. significant compared with placebo their baseline weight) compared with
Patients were defined as having in- (p < 0.001) (Table 1). Although those receiving paroxetine (3.3%) or
somnia at baseline if they scored 4 quantitative data were not reported, placebo (4.1%). The only statistically
or greater on the reduced sleep ques- the most substantial benefits appear significant change in weight from
tion of the MADRS. Overall, there to have been in sleep quality and baseline compared with placebo
was no difference in response on the total sleep time. The improvements occurred in the quetiapine 600-mg
MADRS or a difference in remission in PSQI scores correlated with im- group (mean S.D. weight change
rates between groups; however, pa- provements in depression and anxi- from baseline of 1.7 0.23 kg, p <
tients who had insomnia at baseline ety symptoms, measured using the 0.001). More patients in the que-
in the quetiapine plus fluoxetine MADRS, HAM-D, Hamilton Rating tiapine groups experienced clinically
group experienced improvements Scale for Anxiety, and the Clinical relevant increases in cholesterol val-
in sleep and anxiety. The insomnia Global Impression scale. The most ues, with 14.214.7% of quetiapine-
scores of patients in the quetiapine common adverse events in the que- treated patients having a triglyceride
plus fluoxetine group improved tiapine groups included dry mouth, concentration of 200 mg/dL at the
quicker than those in the placebo sedation, and somnolence. Fewer end of the study; however, 13% of pa-
plus fluoxetine group (Table 1). The than 4% of patients in each quetia- tients in the placebo group also had
mean S.D. weight change from pine group reported insomnia as an significant increases in cholesterol
baseline to weeks 8 and 9 of treat- adverse event. Patients in the que- values. A small percentage of patients
ment was not statistically different tiapine groups were more likely to re- in the quetiapine groups (35.6%)
between groups (0.853 2.79 kg in port weight gain as an adverse effect and in the paroxetine group (4.3%)
the placebo group and 0.204 2.404 (2.9% in the 300-mg group, 5.7% in had clinically significant increases
kg in the quetiapine plus fluoxetine the 600-mg group) compared with in fasting blood glucose (concentra-
group, p not reported). The most placebo (1.2%). It should be noted tions of 126 mg/dL).
common patient-reported adverse that patients in the quetiapine groups Although the use of quetiapine
effects in both groups were gastro- weighed more at baseline than those in these populations with insomnia
intestinal symptoms (nausea, diar- in the placebo group (mean weights and concurrent unipolar or bipolar
rhea, constipation), dizziness, and of 87.0, 85.6, and 83.4 kg in the 300- depression was shown to be effective
sedation; sedation was significantly mg, 600-mg, and placebo groups, for improving sleep, it is unknown
more common in the quetiapine plus respectively). whether the insomnia improved
fluoxetine group (p = 0.006). Similar to the BOLDER I and because the depression improved or
Bipolar depression. Endicott et II studies, the EMBOLDEN II (Ef- if the insomnia improved indepen-
al.26 performed a secondary analy- ficacy of Monotherapy Seroquel in dently of the depression.
sis on data from the BOLDER BipOLar DepressioN II) trial con- Parkinsons disease. Juri et al.28 stud-
(BipOLar DEpRession) I and II trials ducted by McElroy et al.27 random- ied 14 patients (11 men and 3 women)
to evaluate the effects of quetiapine ized 740 patients with bipolar I or II with nonpsychotic Parkinsons dis-
monotherapy on quality of life and disorder and a major depressive epi- ease who received quetiapine for 12
sleep in patients with bipolar I and sode (as defined by DSM-IV criteria) weeks for the treatment of insomnia.
II depressive episodes. The BOLDER to quetiapine 300 mg daily, quetiap- This was an open-label study that al-
I and II trials were randomized, ine 600 mg daily, paroxetine 20 mg lowed for dosage adjustments based
double-blind, placebo-controlled daily, or placebo for eight weeks. The on response; at the end of 12 weeks,
398 Am J Health-Syst PharmVol 71 Mar 1, 2014
CLINICAL CONSULTATION Quetiapine
the mean daily quetiapine dose on response. At the end of 60 days, antidepressant therapy on daytime
was 31.9 mg (range, 12.550 mg). the mean dosage was 62.35 mg daily sleepiness and quality of sleep were
Total PSQI and its subscale scores (range, 25225 mg) at bedtime. Pa- evaluated over four weeks in 27 adult
improved significantly over baseline tients were assessed using the Spiegel patients admitted for the treatment
(p < 0.01), with the largest improve- Sleep Questionnaire and demon- of a major depressive episode.32,33
ment seen in sleep latency (reduced strated a 75% improvement in the During the treatment period, the
from a mean S.D. time of 82 65.4 global score over baseline (p < 0.001). mean daily quetiapine dose was 340
minutes to 28.6 22.7 minutes). Two The greatest improvements occurred mg. Actigraphy data from the first
patients with restless legs syndrome in overall quality of sleep and sleep and last seven nights (10:00 p.m. to
at baseline discontinued treatment latency. Benzodiazepine use was also 6:00 a.m.) were used to objectively
with quetiapine due to worsening of evaluated and had decreased from assess sleep quality. There were no
these symptoms. 83% at baseline to 22.6% at 60 days. significant differences found in the
Breast cancer. Pasquini et al. 29 No patients discontinued therapy patients between weeks 1 and 4. Ac-
studied 6 women with localized due to adverse effects, the most tigraphic data were also collected for
breast cancer (TNM Stage IIIIA) common of which was dry mouth 27 matched controls due to a lack of
who were receiving tamoxifen 20 (34.6%). Metabolic effects were not normative actigraphic data. Com-
mg daily and had a diagnosis of reported. pared with study patients, patients
substance-induced sleep disorder. Inpatient management of insom- in the control group at week 4 had
At baseline, the 6 participants had nia. Schizophrenia. Yamashita et al.31 significantly longer sleep latency
been taking daily tamoxifen for at stratified 86 inpatient adults into two (p = 0.03), lower sleep efficiency
least three months. Quetiapine treat- groups, elderly (older than 65 years) (p = 0.01), and shorter sleep time
ment for insomnia was started at 25 and middle-aged (4364 years), and (p = 0.02).32 A PSQI score was col-
mg nightly and could be increased randomized these patients to switch lected at baseline and weekly for
in 25-mg increments to a maximum from their baseline antipsychotic to study patients. Both the total PSQI
daily dose of 100 mg. Five of the 6 one of four atypical antipsychotics, score and the PSQI daytime sleepi-
women showed improvements in which included quetiapine (13 in the ness subscore showed significant
insomnia at week 1 that persisted to elderly group, 12 in the middle-aged improvement over baseline for all
week 6 based on the Insomnia Sever- group). These patients were admitted four weeks (p < 0.001). The largest
ity Index scale. Two women reported to an inpatient psychiatric hospital improvement in sleep quality oc-
weight gain (not quantified), and 1 in Japan. Antipsychotic dosages were curred in the patients receiving the
reported dizziness at the six-week allowed to vary; the mean quetiapine highest dose of quetiapine (>364
follow-up visit. Interestingly, 2 of dosages at the end of the study were mg daily).33 There were no recorded
the 6 women had previously taken a 409.6 mg daily in the elderly group instances of adverse metabolic or
benzodiazepine and 1 had taken mir- and 541.7 mg daily in the middle-aged clinical effects or significant weight
tazapine for insomnia. Although the group. Sleep was assessed via the PSQI gain (10% of baseline weight) over
conclusions regarding the efficacy of at baseline and at eight weeks after the the four-week study.33
quetiapine for insomnia were posi- medication switch. PSQI scores were Similar to the studies that evalu-
tive, it is difficult to draw generalized reported for all patients (not strati- ated quetiapine for the treatment of
conclusions from a small study with fied by antipsychotic) and showed insomnia in outpatient adults with
such a specific patient population. a significantly improved time effect unipolar or bipolar depression, it
Addictive conditions. Tern et al.30 for total PSQI score and number of is unknown whether the insomnia
reviewed the charts of 52 patients minutes spent in bed (p < 0.05). A improved because the psychiatric
with polysubstance abuse who had logistic regression analysis found that disorder improved or the insomnia
insomnia as their primary with- the use of quetiapine (as well as the improved independent of the psychi-
drawal symptom and were treated use of olanzapine and risperidone) atric disorder.
with quetiapine for insomnia. The was a predictor of improvement on
majority of patients (n = 31) were the PSQI. The authors noted that 1 Safety of quetiapine for insomnia
started on quetiapine in the inpatient patient in the elderly group who was The two studies that evaluated the
setting; the remaining patients (n = treated with quetiapine dropped out use of quetiapine specifically for the
21) started quetiapine as outpatients. because of a hip fracture; otherwise, treatment of insomnia in the absence
All had been followed for 60 days in safety concerns regarding quetiapine of comorbid conditions found that
the outpatient setting. Quetiapine were not reported. the drug was generally well tolerated
was initiated at 50100 mg daily, Major depressive disorder. The ef- at a dosage of 2575 mg nightly for
and the dosage was adjusted based fects of quetiapine as an adjunct to two to six weeks.22,23 In each study,
Am J Health-Syst PharmVol 71 Mar 1, 2014 399
CLINICAL CONSULTATION Quetiapine
the adverse effects most commonly reports have also demonstrated the and sleep outcomes were statistically
cited by patients in the quetiapine tendency for quetiapine to induce analyzed in healthy volunteers and
groups were dry mouth and daytime Q-Tc-interval prolongation, particu- patients with primary insomnia,
sedation, which are consistent with larly in patients taking concomitant respectively, in two studies21,22; such
the common adverse effects noted drugs known to prolong the Q-T in- testing and analysis were not con-
in the drugs prescribing informa- terval (e.g., amiodarone, methadone) ducted in the four studies evaluating
tion.10,11,22,23 Adverse-effect data from and in patients with underlying con- the use of quetiapine for insomnia
the small, short-duration trials of ditions known to predispose some- in patients with unipolar or bipolar
quetiapine for insomnia showed the one to Q-Tc-interval prolongation depression.24-27 In addition, no trials
drug to be well tolerated, but it is (e.g., electrolyte imbalance, heart comparing quetiapine with an active
unknown if this would hold true for failure).10,11,13 The obvious adverse control (e.g., zolpidem) have been
longer durations of use in a larger effect of sedation exists with quetia- conducted; the data that exist com-
number of patients. Recent safety pine use, but, in the case of insomnia pare quetiapine to a placebo or there
reviews of quetiapine dosages of less treatment, sedation is a desired effect. is no comparison and all patients are
than 300 mg per day have noted treated with quetiapine. This type of
that the drug can cause harmful Discussion comparative data would be helpful to
adverse effects.34-36 Low-dose quetia- Quetiapine was developed for the determine the true efficacy of que-
pine ( 200 mg) at bedtime used for treatment of psychiatric disorders, tiapine in treating insomnia, particu-
insomnia has been shown to cause but its antagonism of the H1- and larly in patients with a psychiatric
significant increases in weight (p = 5-HT2A receptors has the added ef- comorbidity. The limited number
0.037) and body mass index (p = fect of causing sedation. As such, of trials combined with small sam-
0.048). 34 The American Diabetes quetiapine is widely used as a treat- ple sizes, short durations, variable
Association consensus development ment for insomnia. However, before populations (e.g., Parkinson disease,
conference cautions that any medica- a practitioner recommends or pre- breast cancer), and predominantly
tion that causes substantial weight scribes quetiapine for the treatment subjective evaluations (e.g., ques-
gain could put a person at risk for de- of insomnia, several issues should be tionnaires) do not lend confidence
veloping diabetes mellitus.37 The data considered. to the concept that quetiapine is a
are mixed on whether diabetes or First, robust studies evaluating proven safe and effective treatment
dyslipidemia is caused by quetiapine the safety and efficacy of quetiapine modality for insomnia.
use, but the same consensus position for the treatment of insomnia are Second, quetiapine has gained a
statement recommends that patients lacking. There are a limited number reputation as a drug of misuse and
treated with second-generation anti- of studies, some of which evaluated abuse. Quetiapine has been referred
psychotics, such as quetiapine, have niche populations whose data would to as several street names, includ-
their weight, waist circumference, not be generalizable to the general ing quell, Susie Q, and baby
blood pressure, fasting glucose con- population. The use of quetiapine heroin.39 Case reports of quetiapine
centration, and fasting lipid panel for the treatment of insomnia in the abuse have described patients who
routinely monitored.37 absence of comorbid conditions has have misused the drug orally, intra-
Although the causality is ques- been evaluated in only two clini- nasally, and intravenously (achieved
tionable, nonmetabolic adverse ef- cal trials of 31 patients in total.22,23 by crushing quetiapine tablets).40
fects that have been associated with Quetiapine studies in patients with Quetiapine has also been mixed
low-dose quetiapine include restless insomnia and other comorbidities with illicit drugs, such as cocaine
legs syndrome and periodic limb are not much more prevalent; the (Q-ball) or marijuana (Maq-ball).40
movements in sleep, daytime se- four trials included in this review It should be noted, however, that
dation, dry mouth, akathisia, and that included patients with unipolar most reports of quetiapine abuse
fatal hepatotoxicity. 21-23,36 Tardive or bipolar depression evaluated just have occurred among prison inmates
dyskinesia has also been associated 1379 patients.24-27 This is not a large or in inpatient psychiatric settings in
with quetiapine use. While the risk number of patients, given the high patients with a history of substance
of developing tardive dyskinesia is prevalence of insomnia and the high abuse, so the abuse potential may
typically associated with increasing prevalence of quetiapine prescrib- not be generalizable to the overall
dosages and longer treatment dura- ing.1,38 Very few of the studies evalu- population of people with insom-
tions of therapy, it can occur with ated sleep using objective testing, nia.41 The implications for abuse by
low dosages and during short treat- which is another limitation of the people using the drug for insomnia
ment courses, such as those used to available data on quetiapine. Poly- are unknown. Quetiapine is not a
treat insomnia.10,11,13 Postmarketing somnographic testing was performed controlled substance but, based on
400 Am J Health-Syst PharmVol 71 Mar 1, 2014
CLINICAL CONSULTATION Quetiapine
reports of abuse, may have the poten- 5. Morin CM, Blanger L, LeBlanc M et pilot study. Psychopharmacology. 2008;
al. The natural history of insomnia: a 196:337-8. Letter.
tial to be misused in a patient desper- population-based 3-year longitudinal 23. Tassniyom K, Paholpak S, Tassniyom S
ate for sleep. study. Arch Intern Med. 2009; 169:447-53. et al. Quetiapine for primary insomnia:
Finally, off-label use of quetiapine 6. Shahid A, Chung SA, Phillipson R, Shapiro a double blind, randomized controlled
CM. An approach to long-term sedative trial. J Med Assoc Thai. 2010; 93:729-34.
for the treatment of insomnia has hypnotic use. Nat Sci Sleep. 2012; 4:53-61. 24. agud M, Mihaljevi-Pele A, Mck-eler
medicallegal implications. Based on 7. American Psychiatric Association. High- D et al. Quetiapine augmentation in
its known H1-receptor antagonistic lights to changes from DSM-IV-TR to treatment-resistant depression: a natu-
DSM-5. www.psychiatry.org/File%20 ralistic study. Psychopharmacology. 2006;
properties, the use of quetiapine Library/Practice/DSM/DSM-5/Changes- 187:511-4.
for insomnia could be considered f ro m - D S M - I V- T R t o - D S M - 5 . p d f 25. Garakani A, Martinez JM, Marcus S et
evidence-based off-label use; none- (accessed 2013 Jun 11). al. A randomized, double-blind, and
8. Riemann D. Insomnia and comorbid placebo-controlled trial of quetiapine
theless, such use is not supported by psychiatric disorders. Sleep Med. 2007; augmentation of fluoxetine in major de-
the FDA-approved labeling for the 8(suppl 4):S15-20. pressive disorder. Int Clin Psychopharm.
drug.42 Because quetiapine has the 9. Sateia MJ. Update on sleep and psychiat- 2008; 23:269-75.
ric disorders. Chest. 2009; 135:1370-9. 26. Endicott J, Paulsson B, Gustafsson U et
potential to cause serious adverse 10. Seroquel (quetiapine fumarate) package al. Quetiapine monotherapy in the treat-
effects, including increased risk of insert. Wilmington, DE: AstraZeneca; ment of depressive episodes of bipolar I
death in elderly patients; increased 2012. and II disorder: improvements in quality
11. Seroquel XR (quetiapine fumarate) pack- of life and quality of sleep. J Affect Disord.
risk of suicidal thinking and behavior age insert. Wilmington, DE: AstraZeneca; 2008; 111:306-19.
in children, adolescents, and young 2012. 27. McElroy SL, Weisler RH, Chang W et al.
adults; cardiac dysrhythmias; and 12. Philip NS, Mello K, Carpenter LL et A double-blind, placebo-controlled study
al. Patterns of quetiapine use in psy- of quetiapine and paroxetine as mono-
metabolic dysfunctions (e.g., sig- chiatric inpatients: an examination of therapy in adults with bipolar depression
nificant weight gain, hyperglycemia, off-label use. Ann Clin Psychiatry. 2008; (EMBOLDEN II). J Clin Psychiatry. 2010;
hyperlipidemia), patients could pur- 20:15-20. 71:163-74.
13. Quetiapine. In: Drugdex System. Green- 28. Juri C, Chan P, Tapia J et al. Quetiapine
sue litigation against a prescribing wood Village, CO: Thomson Reuters for insomnia in Parkinson disease: results
physician, a dispensing pharmacy, (Healthcare). Updated periodically. from an open-label trial. Clin Neurophar-
or a drug manufacturer if harmed 14. Stahl SM. Selective histamine H1 antago- macol. 2005; 28:185-7.
nism: novel hypnotic and pharmacologic 29. Pasquini M, Speca A, Biondi M. Quetia-
by quetiapine used for an off-label actions challenge classical notions of anti- pine for tamoxifen-induced insomnia in
indication. histamines. CNS Spectr. 2008; 13:1027-38. women with breast cancer. Psychosomat-
15. Schutte-Rodin S, Broch L, Buysse D et ics. 2009; 50:159-61.
al. Clinical guideline for the evaluation 30. Tern A, Majadas S, Galan J. Quetiapine
Conclusion and management of chronic insomnia in in the treatment of sleep disturbances
Robust studies evaluating the adults. J Clin Sleep Med. 2008; 4:487-504. associated with addictive conditions: a
safety and efficacy of quetiapine for 16. Reeves R. Guideline, education, and peer retrospective study. Subst Use Misuse.
comparison to reduce prescriptions of 2008; 43:2169-71.
the treatment of insomnia are lack- benzodiazepines and low-dose quetia- 31. Yamashita H, Mori K, Nagao M et al.
ing. Given its limited efficacy data, pine in prison. J Correct Health Care. Influence of aging on the improvement
its adverse-effect profile, and the 2012; 18:45-52. of subjective sleep quality by atypical an-
17. Levin A. Concern raised over antipsy- tipsychotic drugs in patients with schizo-
availability of agents approved by chotics use for sleep problems. http:// phrenia: comparison of middle-aged and
FDA for the treatment of insomnia, psychnews.psychiatryonline.org/news older adults. Am J Geriatr Psychiatry.
quetiapines benefit in the treatment Article.aspx?articleid=116611 (accessed 2005; 13:377-84.
2013 Apr 4). 32. Todder D, Caliskan S, Baune BT. Night
of insomnia has not been proven 18. Kime P. DoD cracks down on off- locomotor activity and quality of sleep
to outweigh potential risks, even in label drug use. www.militarytimes.com/ in quetiapine-treated patients with de-
patients with a comorbid labeled in- news/2012/06/military-dod-cracks-down- pression. J Clin Psychopharmacol. 2006;
on-off-label-seroquel-use-061412w/ 26:638-42.
dication for quetiapine. (accessed 2013 Apr 4). 33. Baune BT, Caliskan S, Todder D. Effects
19. Walsh JK. Drugs used to treat insomnia of adjunctive antidepressant therapy with
References in 2002: regulatory-based rather than quetiapine on clinical outcome, quality
1. Roth T. Insomnia: definition, prevalence, evidence-based medicine. Sleep. 2004; of sleep and daytime motor activity in
etiology, and consequences. J Clin Sleep 27:1441-2. patients with treatment-resistant depres-
Med. 2007; 3(suppl):S7-10. 20. Thomson Reuters Micromedex Clinical sion. Hum Psychopharmacol Clin Exp.
2. Simon GE, VonKorff M. Prevalence, Evidence Solutions. http://thomsonreuters. 2007; 22:1-9.
burden, and treatment of insomnia in com/products_services/healthcare/ 34. Cates ME, Jackson CW, Feldman JM et
primary care. Am J Psychiatry. 1997; healthcare_products/clinical_deci_ al. Metabolic consequences of using low-
154:1417-23. support/micromedex_clinical_evidence_ dose quetiapine for insomnia in psychi-
3. Daley M, Morin CM, LeBlanc M et al. sols/med_safety_solutions/red_book atric patients. Community Ment Health J.
Insomnia and its relationship to health- (accessed 2013 Apr 4). 2009; 45:251-4.
care utilization, work absenteeism, pro- 21. Cohrs S, Rodenbeck A, Guan Z et al. 35. Gugger JJ, Cassagnol M. Low-dose que-
ductivity and accidents. Sleep Med. 2009; Sleep-promoting properties of quetia- tiapine is not a benign sedative-hypnotic
10:427-38. pine in healthy subjects. Psychopharma- agent. Am J Addict. 2008; 17:454-5.
4. Wade AG. The societal costs of insom- cology. 2004; 174:421-9. 36. Coe HV, Hong IS. Safety of low doses of
nia. Neuropsychiatr Dis Treat. 2011; 7:1- 22. Wiegand MH, Landry F, Brckner T et quetiapine when used for insomnia. Ann
18. al. Quetiapine in primary insomnia: a Pharmacother. 2012; 46:718-22.
Am J Health-Syst PharmVol 71 Mar 1, 2014 401
CLINICAL CONSULTATION Quetiapine
37. American Diabetes Association, Ameri-
can Psychiatric Association, American
Association of Clinical Endocrinologists,
North American Association for the
Study of Obesity. Consensus develop-
ment conference on antipsychotic drugs
and obesity and diabetes. Diabetes Care.
2004; 27:596-601.
38. IMS Institute for Healthcare Informatics.
The use of medicines in the United States:
review of 2011. www.imshealth.com/
ims/Global/Content/Insights/IMS%20
Institute%20for%20Healthcare%20
Informatics/IHII_Medicines_in_U.S_
Report_2011.pdf (accessed 2012 Jun 29).
39. Sansone RA, Sansone LA. Is Seroquel de-
veloping an illicit reputation for misuse/
abuse? Psychiatry. 2010; 7:13-6.
40. Waters BM, Joshi KG. Intravenous
quetiapine-cocaine use (Q-ball). Am J
Psychiatry. 2007; 164:173-4.
41. Pinta ER, Taylore RE. Quetiapine ad-
diction? Am J Psychiatry. 2007; 164:174.
Letter.
42. Kesselheim AS. Off-label drug use and
promotion: balancing public health goals
and commercial speech. Am J Law Med.
2011; 37:225-57.
402 Am J Health-Syst PharmVol 71 Mar 1, 2014
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Astellas Pharma: Launches Irribow OD Tablets in Japan For Diarrhea-Predominant Irritable Bowel SyndromeDokumen3 halamanAstellas Pharma: Launches Irribow OD Tablets in Japan For Diarrhea-Predominant Irritable Bowel SyndromeHerry HendrayadiBelum ada peringkat
- The Top 10 Generic Pharmaceutical CompaniesDokumen42 halamanThe Top 10 Generic Pharmaceutical CompaniesHerry HendrayadiBelum ada peringkat
- Kharkov National Medical University Department of Pharmacology Lecture on Anti-inflammatory DrugsDokumen82 halamanKharkov National Medical University Department of Pharmacology Lecture on Anti-inflammatory DrugsHerry HendrayadiBelum ada peringkat
- BCP 13010 PDFDokumen11 halamanBCP 13010 PDFHerry HendrayadiBelum ada peringkat
- Top 10 Generic Pharmaceutical CompaniesDokumen178 halamanTop 10 Generic Pharmaceutical CompaniesHerry HendrayadiBelum ada peringkat
- Lifecycle Management Strategies Maximizing ROI Through Indication Expansion Reformulation and Rx-To-OTC SwitchingDokumen176 halamanLifecycle Management Strategies Maximizing ROI Through Indication Expansion Reformulation and Rx-To-OTC SwitchingHerry Hendrayadi100% (1)
- 1 - Dr. KungDokumen18 halaman1 - Dr. KungWawan IndrawanBelum ada peringkat
- Practical Guide To Joint and Soft Tissue Injection TechniquesDokumen5 halamanPractical Guide To Joint and Soft Tissue Injection TechniquesHerry HendrayadiBelum ada peringkat
- Press Conference: Astellas' Growth StrategyDokumen31 halamanPress Conference: Astellas' Growth StrategyHerry HendrayadiBelum ada peringkat
- Growth Strategies in Generics Innovative and Aggressive Strategies and Their Impact On Branded PharmaceuticalsDokumen176 halamanGrowth Strategies in Generics Innovative and Aggressive Strategies and Their Impact On Branded PharmaceuticalsHerry HendrayadiBelum ada peringkat
- The Top 10 Generic Pharmaceutical CompaniesDokumen42 halamanThe Top 10 Generic Pharmaceutical CompaniesHerry HendrayadiBelum ada peringkat
- Pharmaceutical Growth Opportunities in Brazil, Russia, India and ChinaDokumen35 halamanPharmaceutical Growth Opportunities in Brazil, Russia, India and ChinaHerry HendrayadiBelum ada peringkat
- The Top 10 Generic Pharmaceutical CompaniesDokumen10 halamanThe Top 10 Generic Pharmaceutical CompaniesHerry HendrayadiBelum ada peringkat
- The Global AntiInfectives Market OutlookDokumen267 halamanThe Global AntiInfectives Market OutlookHerry HendrayadiBelum ada peringkat
- Standard Step-Wise Timelines in The Drug Discovery ProcessDokumen19 halamanStandard Step-Wise Timelines in The Drug Discovery ProcessHerry HendrayadiBelum ada peringkat
- Standard Step-Wise Timelines in The Drug Discovery ProcessDokumen19 halamanStandard Step-Wise Timelines in The Drug Discovery ProcessHerry HendrayadiBelum ada peringkat
- Achieving Market Dominance Through Reformulation.Dokumen12 halamanAchieving Market Dominance Through Reformulation.Herry HendrayadiBelum ada peringkat
- The Global AntiInfectives Market OutlookDokumen267 halamanThe Global AntiInfectives Market OutlookHerry HendrayadiBelum ada peringkat
- Growth Strategies in Generics Innovative and Aggressive Strategies and Their Impact On Branded PharmaceuticalsDokumen176 halamanGrowth Strategies in Generics Innovative and Aggressive Strategies and Their Impact On Branded PharmaceuticalsHerry HendrayadiBelum ada peringkat
- Achieving Market Dominance Through ReformulationDokumen223 halamanAchieving Market Dominance Through ReformulationHerry HendrayadiBelum ada peringkat
- Global Market AnalysisaAntibioticsDokumen23 halamanGlobal Market AnalysisaAntibioticsHerry HendrayadiBelum ada peringkat
- The Blockbuster Drugs Outlook PDFDokumen259 halamanThe Blockbuster Drugs Outlook PDFHerry HendrayadiBelum ada peringkat
- Indication Expansion Opportunities For Successful Lifecycle ManagementDokumen144 halamanIndication Expansion Opportunities For Successful Lifecycle ManagementHerry HendrayadiBelum ada peringkat
- Top 15 Therapeutic 2008 PDFDokumen95 halamanTop 15 Therapeutic 2008 PDFHerry HendrayadiBelum ada peringkat
- Pharma 2020 PWC ReportDokumen32 halamanPharma 2020 PWC ReportBrand SynapseBelum ada peringkat
- Management Pocketbooks - The Balance Sheet PocketbookDokumen309 halamanManagement Pocketbooks - The Balance Sheet PocketbookHerry Hendrayadi100% (1)
- Reader's Digest January 2013Dokumen148 halamanReader's Digest January 2013pereira_jus3430Belum ada peringkat
- Ijss Aug Oa12Dokumen5 halamanIjss Aug Oa12Herry HendrayadiBelum ada peringkat
- 2nd Announcement A5 Upload 1Dokumen18 halaman2nd Announcement A5 Upload 1Herry HendrayadiBelum ada peringkat
- Systemic Lupus Erythematosus and Neuropsychiatric DiseaseDokumen56 halamanSystemic Lupus Erythematosus and Neuropsychiatric DiseaseHerry HendrayadiBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Census August 8 - August 9, 2020Dokumen6 halamanCensus August 8 - August 9, 2020Patrick JohnBelum ada peringkat
- Far Eastern University: Module #3 - Oxygenation (Oxygen Therapy)Dokumen28 halamanFar Eastern University: Module #3 - Oxygenation (Oxygen Therapy)aaaaaBelum ada peringkat
- DLL - Fourth GradingDokumen5 halamanDLL - Fourth GradingMeek Adan RodriguezBelum ada peringkat
- Heart Disease Course PDALongDokumen84 halamanHeart Disease Course PDALongArpanpatelBelum ada peringkat
- Lecture 6 Cardiovascular: Vascular System - The HemodynamicsDokumen61 halamanLecture 6 Cardiovascular: Vascular System - The HemodynamicsAndreea ŞtefănescuBelum ada peringkat
- How To Measure Frailty in Your PatientsDokumen1 halamanHow To Measure Frailty in Your PatientsZahra'a Al-AhmedBelum ada peringkat
- Izatizon, As An Izatin-Thiosemicarbazone Derivative, Has Antiviral, Anti-Tumor Actions and No Side EffectsDokumen3 halamanIzatizon, As An Izatin-Thiosemicarbazone Derivative, Has Antiviral, Anti-Tumor Actions and No Side EffectsinventionjournalsBelum ada peringkat
- Test Bank For Introductory Maternity and Pediatric Nursing 2nd Edition by KlossnerDokumen9 halamanTest Bank For Introductory Maternity and Pediatric Nursing 2nd Edition by KlossnerJulieJacobsrkozw100% (84)
- Karthik Covid Report 1295Dokumen1 halamanKarthik Covid Report 1295Karthikeya PuttaguntaBelum ada peringkat
- 2006 Human and Developmental Toxicology - D. Bellinger (Informa, 2006) WW PDFDokumen555 halaman2006 Human and Developmental Toxicology - D. Bellinger (Informa, 2006) WW PDFGiovana BarbosaBelum ada peringkat
- Pathophysiology of Respiratory Diseases: Obstructed AlveoliDokumen3 halamanPathophysiology of Respiratory Diseases: Obstructed AlveoliApril Dianne ParungaoBelum ada peringkat
- 1.4.2 Making VaccinesDokumen21 halaman1.4.2 Making VaccinesVikas Viki0% (1)
- Material Safety Data Sheet: 1. Chemical Product and Company IdentificationDokumen7 halamanMaterial Safety Data Sheet: 1. Chemical Product and Company IdentificationKun Adi ReksatamaBelum ada peringkat
- Headache - 2001 - Jacome - Transitional Interpersonality Thunderclap HeadacheDokumen4 halamanHeadache - 2001 - Jacome - Transitional Interpersonality Thunderclap HeadacheactualashBelum ada peringkat
- Breast Cancer 1Dokumen14 halamanBreast Cancer 1Gînțăgan Denisa GabrielaBelum ada peringkat
- Modified Double Glove TechniqueDokumen1 halamanModified Double Glove TechniqueSohaib NawazBelum ada peringkat
- Ms. Michelle Lau Sook Yee (First Speaker)Dokumen5 halamanMs. Michelle Lau Sook Yee (First Speaker)Nurhidayah MuhamadBelum ada peringkat
- Managing Fatigue During PregnancyDokumen2 halamanManaging Fatigue During PregnancyBlanz Irybelle KindomBelum ada peringkat
- Lecture 12 Health Management Information SystemDokumen14 halamanLecture 12 Health Management Information SystemKamran SheikhBelum ada peringkat
- Secrets of Psychic HealingDokumen140 halamanSecrets of Psychic Healingkonoha G100% (39)
- What Is Water PollutionDokumen13 halamanWhat Is Water PollutiondumitrutudoranBelum ada peringkat
- Nami Understanding Psychosis BookletDokumen59 halamanNami Understanding Psychosis BookletSalma KarimahBelum ada peringkat
- Atopic Eczema in Adulthood and Risk of Depression and Anxiety: A Population-Based Cohort StudyDokumen26 halamanAtopic Eczema in Adulthood and Risk of Depression and Anxiety: A Population-Based Cohort Studyyenny handayani sihiteBelum ada peringkat
- Med Surg Nurse Brain SheetDokumen2 halamanMed Surg Nurse Brain SheetJan Marcus95% (20)
- Physiology of the Pleural Space: Visceral Pleura, Parietal Pleura, and Fluid FormationDokumen78 halamanPhysiology of the Pleural Space: Visceral Pleura, Parietal Pleura, and Fluid FormationAhmad RafiqiBelum ada peringkat
- PRAGYAN Vol 07 Issue 01Dokumen92 halamanPRAGYAN Vol 07 Issue 01PRAGYAN,Tinsukia CollegeBelum ada peringkat
- Book of Vile DarknessDokumen25 halamanBook of Vile Darknessv0idless100% (2)
- ICMIDokumen4 halamanICMIKim MingyuBelum ada peringkat
- Detailed Lesson Plan in Quarter 4 WK 1 Digestive ProcessDokumen10 halamanDetailed Lesson Plan in Quarter 4 WK 1 Digestive ProcessmalouBelum ada peringkat
- Thandi Facial Electrical Case StudyDokumen4 halamanThandi Facial Electrical Case StudyLionel YdeBelum ada peringkat