162
Diunggah oleh
Adriana VasilicaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
162
Diunggah oleh
Adriana VasilicaHak Cipta:
Format Tersedia
CASE REPORT
Persistent Atrial Standstill in Acute Myocarditis
*MUKUND A PRABHU, SRINIVAS PRASAD BV, ANEES THAJUDEEN AND NARAYANAN NAMBOODIRI
From Departments of Cardiology, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, and
*Sri Jayadeva Institute of Cardiovascular Sciences and Research, Bengaluru; India.
Correspondence to: Background: Atrial standstill manifests as absence of any atrial electrical activity in the
Dr Mukund A Prabhu, Electrophysiology surface ECG leads. Persistent atrial standstill secondary to acute myocarditis is
Unit, Department of Cardiology, extremely rare. Case report: 10-year-old girl had atrial standstill and heart failure due to
Sri Jayadeva Institute of Cardiovascular acute myocarditis. After recovery from myocarditis, heart failure resolved, but the atrial
Sciences and Research, 9th Block Jayanagar, standstill persisted. Outcome: Persistent atrial standstill was treated with permanent
Bannerghatta Road, Bengaluru 560 069, pacemaker and anticoagulation. Message: Acute myocarditis may rarely cause atrial
India. mukundaprabhu@gmail.com standstill that can last even after recovery from myocarditis.
Received: May 21, 2015;
Initial review: July 15, 2015; Keywords: Cardiac arrhythmias, Permanent pacemaker.
Accepted: December 07, 2015.
A
trial standstill or paralysis has been defined as suggestive of total atrial standstill (Fig. 2). An evaluation
the absence of any electrical or mechanical done for neuromuscular disease showed normal muscle
activity of atria [1-3]. In atrial standstill, strength and normal electromyography.
there is no evidence of atrial electrical
Electrophysiology study (EPS) showed no evidence
activity in the surface ECG leads or on
of atrial electrical activity. There was no atrial capture
electrophysiological evaluation. We report atrial
even at maximum pacing output (25mA), from multiple
standstill in acute myocarditis that persisted even after the
atrial sites (Web Fig. I), consistent with atrial standstill.
resolution of myocarditis.
She underwent a pacemaker implantation, and
CASE REPORT subsequently the right ventricular pacing parameters
were normal. Her ECG after 10 months showed no p
A 10-year-old girl presented with congestive heart failure
waves, and the fluoroscopy and echocardiography
(CHF) following an episode of low grade fever. She had
showed no suggestion of atrial contraction. Interrogation
no family history of cardiac illness, pacemaker
of the pacemaker confirmed that she was totally
implantation, embolic events or skeletal muscle disease.
pacemaker-dependent.
Investigations revealed a normal total leukocyte count
(7x 109/L) with 18% neutrophils. Serum electrolytes
were in the normal range. The ECG at the time of
presentation showed absent P waves and a wide QRS
regular escape rhythm at 40/min (Fig. 1). Cardiac
troponin T was raised (1793 ng/L). Echocardiogram
showed hypokinesia of the left ventricle and mild left
ventricular (LV) dysfunction. Her Anti-ds DNA and anti-
nuclear antibody titres were normal. She had received
intravenous immunoglobulins, ampicillin and ranitidine
before she was referred to our unit. We continued
conservative management with bed rest, diuretics, and
digoxin. Her CHF improved, and subsequently she was
discharged. At review visit 6 weeks later, she had no CHF
but had the same ventricular escape rhythm and
exertional fatigue. Echocardiogram showed improved LV
function (ejection fraction 51%). Mitral and tricuspid Fig. 1 The 12 Lead ECG showing idioventricular rhythm with
inflow Doppler study showed absence of a wave absence of P wave and wide QRS escape rhythm.
INDIAN PEDIATRICS 162 VOLUME 53__FEBRUARY 15, 2016
Copyright of Indian Pediatrics 2016
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
PRABHU, et al. PERSISTENT ATRIAL STANDSTILL
Persistent atrial standstill is a rare disorder [5], and
that occurring after myocarditis is even rarer. Straumanis,
et al. [6] have reported a 11-year-old child with biopsy-
proven necrotizing acute myocarditis causing atrial
standstill. However, this was transient and resolved after
3 days of treatment with methylprednisolone. Our patient
had persistence of atrial standstill, even after the
ventricular dysfunction recovered. Abdelwahab, et al. [7]
have reported a case of multiple atrial arrhythmias
(atrioventricular node re-entry and two different focal
atrial tachycardias) originating from the remaining atrial
myocardium after global scarring of both atria following
a remote viral myocarditis. Talwar, et al. [8] reported a
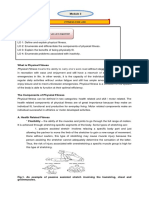
Fig. 2 Mitral inflow pulse wave Doppler showing absence of a case series in which two of the patients had lymphocytic
wave and paced rhythm at 60/minute. infiltrates on right ventricular endomyocardial biopsy. In
another case series of 11 patients with atrial standstill
reported by Nakazato, et al. [9], three had histological
DISCUSSION
evidence of chronic myocarditis. None of their patients
Atrial standstill has been reported to occur in inherited had a presentation suggestive of acute myocarditis.
myopathies, valvular cardiomyopathies, digitalis or
Pathological involvement of atria in atrial standstill
quinidine intoxication, hypoxia, hyperkalemia,
can be localised or diffuse. Our patient likely had a total
myocardial infarction, systemic lupus erythematous, and
atrial standstill as evidenced in mitral pulse wave Doppler
Chagas disease. Atrial standstill secondary to
showing absence of a wave. As atrial standstill is a well-
myocarditis, persisting long after the acute phase, is
known cause of cardiogenic embolism [9], anti-
extremely rare.
coagulation is mandatory; our patient was started on
Atrial standstill could be defined as partial or total Warfarin. The management of patients with atrial
[4]. In partial atrial standstill, conduction disturbance standstill include anticoagulation in all patients, and
within the right atrium alone is a more common finding. pacemaker implantation in patients who have
The absence of P waves in surface ECG occur in sinus symptomatic bradycardia due to insufficient rates of
node arrest with junctional escape rhythm which is thus a escape rhythm.
differential diagnosis of atrial standstill. However, in
We conclude that acute myocarditis can rarely cause
sinus arrest, the atria can be shown to be excitable by
extensive damage to the atria causing loss of electrical
pacing whereas in atrial standstill, atria are non-excitable
and mechanical function. This may herald atrial
and cannot be captured even with high pacing outputs.
standstill, which can persist even beyond the acute phase
This results in lack of mechanical functioning of atria,
when other changes have recovered.
and predispose to intra-atrial thrombus formation.
Contributors: MAP and SP: case management, drafting of
Our patient had a wide QRS escape rhythm with no P manuscript; AT and NN: case management critical revision of
waves. This indicates an escape rhythm from below the manuscript. All authors approved the final version.
level of His bundle (Infra-Hisian). The inability to Funding: None; Competing interests: None stated.
capture the atria even at high current output during the
EPS confirmed atrial standstill in our case. We used REFERENCES
digoxin for LV dysfunction in spite of patient having 1. Surawicz B. Electrolytes and the electrocardiogram. Am J
bradycardia because digoxin has minimal action on infra- Cardiol. 1963;12:656.
Hisian tissues, and is less likely to suppress the escape 2. James TN. Myocardial infarction and atrial arrhythmias.
rhythm. However, a stand by temporary pacemaker was Circulation. 1961; 24:761.
kept ready, and patient was closely monitored. 3. James TN, Rupe CE, Monte R. Pathology of the cardiac
conduction system in systemic lupus erythematosus. Ann
Isoprenaline, which can be used to increase the heart rate,
Intern Med. 1965;63:402.
can also worsen the conduction in infra-Hisian disease, 4. Lvy S, Pouget B, Bemurat M, Lacaze JC, Clementy J,
and hence was not used. She was closely monitored in the Bricaud H. Partial atrial electrical standstill: report of
acute phase, and as there was a possibility that her rhythm three cases and review of clinical and electrophysiological
may normalize once her myocarditis resolves, we waited features. Eur Heart J. 1980;1:107-16.
for six weeks before implanting a permanent pacemaker. 5. Allensworth DC, Rice CI, Lowe G. Persistent atrial
INDIAN PEDIATRICS 163 VOLUME 53__FEBRUARY 15, 2016
Copyright of Indian Pediatrics 2016
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
PRABHU, et al. PERSISTENT ATRIAL STANDSTILL
standstill in a family with myocardial disease. Med Am J. myocarditis. PACE. 2009;32:275-7.
1969;47:775-84. 8. Talwar KK, Dev V, Chopra P, Dave TH, Radhakrishnan
6. Straumanis, John PW, Henry BC, Christopher LR. S. Persistent atrial standstill clinical,
Resolution of atrial standstill in a child with myocarditis. electrophysiological and morphological study.
PACE. 1993;16:2196-202. PACE.1991;14:1274-81.
7. Amir A, John LS, Ratika P, Magdy B, Martin G. Mapping 9. Yuji N, Yasuro N, Teruhikoa H, Masataka S, Shunsuke O,
and ablation of multiple atrial arrhythmias in a patient Hiroshi Y. Clinical and electrophysiological characteristics
with persistent atrial standstill after remote viral of atrial standstill. PACE. 1995;18:1244-54.
INDIAN PEDIATRICS 164 VOLUME 53__FEBRUARY 15, 2016
Copyright of Indian Pediatrics 2016
For personal use only. Not for bulk copying or unauthorized posting to listserv/websites
Anda mungkin juga menyukai
- Nejmc2008597 PDFDokumen2 halamanNejmc2008597 PDFAdriana VasilicaBelum ada peringkat
- TEE in Congenital Heart DiseaseDokumen249 halamanTEE in Congenital Heart DiseaseAdriana VasilicaBelum ada peringkat
- Application of The 2019 ESC/EAS Dyslipidaemia Guidelines To Nationwide Data of Patients With A Recent Myocardial Infarction: A Simulation StudyDokumen10 halamanApplication of The 2019 ESC/EAS Dyslipidaemia Guidelines To Nationwide Data of Patients With A Recent Myocardial Infarction: A Simulation StudyAdriana VasilicaBelum ada peringkat
- Jez 041Dokumen15 halamanJez 041Adriana VasilicaBelum ada peringkat
- Nejmc2008597 PDFDokumen2 halamanNejmc2008597 PDFAdriana VasilicaBelum ada peringkat
- Clinical Review - FullDokumen5 halamanClinical Review - FullkunkkonkBelum ada peringkat
- Position Paper: European Heart Journal - Cardiovascular Imaging (2017) 18, 1073-1089 Doi:10.1093/ehjci/jex146Dokumen17 halamanPosition Paper: European Heart Journal - Cardiovascular Imaging (2017) 18, 1073-1089 Doi:10.1093/ehjci/jex146Adriana VasilicaBelum ada peringkat
- AHA Infective Endo PDFDokumen55 halamanAHA Infective Endo PDFRoselily AmitaBelum ada peringkat
- Clinical Practive Guidelines For The Management of Pain Agitation and Delirium in Adult PatientsDokumen44 halamanClinical Practive Guidelines For The Management of Pain Agitation and Delirium in Adult PatientsLuis GuerreroBelum ada peringkat
- Chapter 02 - How To Image - 0Dokumen8 halamanChapter 02 - How To Image - 0i.e.v.Belum ada peringkat
- Aortic Calcium Score and Vascular Atherosclerosis in Asymptomatic Individuals: Beyond The Coronary ArteriesDokumen4 halamanAortic Calcium Score and Vascular Atherosclerosis in Asymptomatic Individuals: Beyond The Coronary ArteriesAdriana VasilicaBelum ada peringkat
- Mar Fan and Sar TansDokumen3 halamanMar Fan and Sar TansAdriana VasilicaBelum ada peringkat
- Clinical Impact of Elevated Tricuspid Valve Inflow Gradients After TranscatheterDokumen13 halamanClinical Impact of Elevated Tricuspid Valve Inflow Gradients After TranscatheterAdriana VasilicaBelum ada peringkat
- ArvdDokumen17 halamanArvdAdriana VasilicaBelum ada peringkat
- Guideline Dapt PDFDokumen34 halamanGuideline Dapt PDFJicko Street HooligansBelum ada peringkat
- Atrial Infarction and Ischemic Mitral Regurgitation Contribute To Post-MI Remodeling of The Left AtriumDokumen12 halamanAtrial Infarction and Ischemic Mitral Regurgitation Contribute To Post-MI Remodeling of The Left AtriumAdriana VasilicaBelum ada peringkat
- Thyroid HormonesDokumen9 halamanThyroid HormonesAdriana VasilicaBelum ada peringkat
- 2013 ESC Guidelines On Cardiac Pacing and Cardiac Resynchronization TherapyDokumen49 halaman2013 ESC Guidelines On Cardiac Pacing and Cardiac Resynchronization TherapyAdriana VasilicaBelum ada peringkat
- Antithrombotic Therapy After Myocardial Infarction in Patients With Atrial Fibrillation Undergoing Percutaneous Coronary InterventionDokumen10 halamanAntithrombotic Therapy After Myocardial Infarction in Patients With Atrial Fibrillation Undergoing Percutaneous Coronary InterventionAdriana VasilicaBelum ada peringkat
- Acc Aha BradycardiaDokumen191 halamanAcc Aha BradycardiaPanneer SelvamBelum ada peringkat
- Ehra Consensus Document: Europace (2019) 0, 1-18 Doi:10.1093/europace/euz163Dokumen18 halamanEhra Consensus Document: Europace (2019) 0, 1-18 Doi:10.1093/europace/euz163Adriana VasilicaBelum ada peringkat
- Ileana Vulpescu - Carnetul Din Port-HartDokumen3 halamanIleana Vulpescu - Carnetul Din Port-HartAdriana VasilicaBelum ada peringkat
- LA Review JACC 2019Dokumen17 halamanLA Review JACC 2019Adriana VasilicaBelum ada peringkat
- Portopulmonary Hypertension and Hepatopulmonary Syndrome: A Clinician-Oriented OverviewDokumen11 halamanPortopulmonary Hypertension and Hepatopulmonary Syndrome: A Clinician-Oriented OverviewAdriana VasilicaBelum ada peringkat
- Guideline Dapt PDFDokumen34 halamanGuideline Dapt PDFJicko Street HooligansBelum ada peringkat
- Dasatinib Induced HTPDokumen5 halamanDasatinib Induced HTPAdriana VasilicaBelum ada peringkat
- Thyroid HormonesDokumen9 halamanThyroid HormonesAdriana VasilicaBelum ada peringkat
- MKMKM KDokumen38 halamanMKMKM KMark PradsBelum ada peringkat
- Circulationaha 113 002598 FullDokumen41 halamanCirculationaha 113 002598 FullAdriana VasilicaBelum ada peringkat
- Coronary Sinus Ostial Atresia With Unroofed.10Dokumen3 halamanCoronary Sinus Ostial Atresia With Unroofed.10Adriana VasilicaBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Esc 2023 Ic EngDokumen13 halamanEsc 2023 Ic EngAlba PalaciosBelum ada peringkat
- Mousab Kibreet Notes of Internal Medicine 2ed EditionDokumen253 halamanMousab Kibreet Notes of Internal Medicine 2ed EditionAbdulltif AliBelum ada peringkat
- Early Detection of Hepato-Biliary DisorderDokumen68 halamanEarly Detection of Hepato-Biliary DisorderIbsa GetachoBelum ada peringkat
- Magnetic Resonance ImagingDokumen5 halamanMagnetic Resonance ImagingIoan TimaruBelum ada peringkat
- HyperkalemiaDokumen9 halamanHyperkalemiaFabdul RaufBelum ada peringkat
- Profile: DashboardDokumen22 halamanProfile: DashboardGhenea Catalin-StefanBelum ada peringkat
- 2006 Lange OutlineDokumen570 halaman2006 Lange Outlinemequanint kefieBelum ada peringkat
- Topic 3-PEDokumen5 halamanTopic 3-PEgildo subillagaBelum ada peringkat
- Lateral Medullary SyndromeDokumen18 halamanLateral Medullary SyndromeGamer MadaBelum ada peringkat
- RosuvastatinDokumen3 halamanRosuvastatinHanniel MontecalboBelum ada peringkat
- Byzantine Surgery and Unnecessary Modern SurgeryDokumen14 halamanByzantine Surgery and Unnecessary Modern SurgerynicofreshwaterBelum ada peringkat
- Review Article: Biomedical Applications of Shape Memory AlloysDokumen16 halamanReview Article: Biomedical Applications of Shape Memory AlloysAntonela-Georgiana MateiBelum ada peringkat
- Hypertensive Emgerencies 2021Dokumen19 halamanHypertensive Emgerencies 2021Faranitach AiniBelum ada peringkat
- Peter Attia Measuring Cardiovascular Disease Risk and The Importance of ApoBDokumen14 halamanPeter Attia Measuring Cardiovascular Disease Risk and The Importance of ApoBabhimanyu50% (2)
- מערכת סטודנט MedExamsDokumen1 halamanמערכת סטודנט MedExamsReman HakroushBelum ada peringkat
- The Tamil Nadu Dr. M.G.R. Medical University - MSC Nursing Second YrDokumen10 halamanThe Tamil Nadu Dr. M.G.R. Medical University - MSC Nursing Second YrNoufal100% (1)
- Precautions With Diabetic Patients Undergoing SurgeryDokumen6 halamanPrecautions With Diabetic Patients Undergoing SurgeryErvin Kyle OsmeñaBelum ada peringkat
- Group 2 Case ScenarioDokumen6 halamanGroup 2 Case ScenarioNur SanaaniBelum ada peringkat
- Control and CoordinationDokumen43 halamanControl and CoordinationDukhi InsaanBelum ada peringkat
- Burat-Buret Echo Romi Revised PDFDokumen2 halamanBurat-Buret Echo Romi Revised PDFAsma.denmiBelum ada peringkat
- Pathognomonic SignsDokumen12 halamanPathognomonic Signsclarice_jimenezBelum ada peringkat
- Eyes and Stroke The Visual Aspects of Cerebrovascular DiseaseDokumen11 halamanEyes and Stroke The Visual Aspects of Cerebrovascular DiseaseAlessandro ZadraBelum ada peringkat
- Heart BlocksDokumen6 halamanHeart BlocksMark Hammerschmidt100% (1)
- Thrombolytic Therapy in Acute Myocardial InfarctionDokumen7 halamanThrombolytic Therapy in Acute Myocardial InfarctionRumela Ganguly ChakrabortyBelum ada peringkat
- Case 27 (LC Fix)Dokumen14 halamanCase 27 (LC Fix)galih suharno0% (1)
- Managing For Client With Diabetic MellitusDokumen23 halamanManaging For Client With Diabetic MellitusNur HikmaBelum ada peringkat
- QuizDokumen16 halamanQuizDawn MarcoBelum ada peringkat
- Respiratory System HandoutDokumen15 halamanRespiratory System HandoutJei SanBelum ada peringkat
- Hypertension Nursing Care Plan..nkDokumen16 halamanHypertension Nursing Care Plan..nkchishimba louisBelum ada peringkat
- الباطنة كلها بالتفصيل في 160 صفحة فقط لازم تحمل المذكرة فوراDokumen163 halamanالباطنة كلها بالتفصيل في 160 صفحة فقط لازم تحمل المذكرة فورانادين مطر0% (1)