Caro Dart Al 2013
Diunggah oleh
Wilson Fransiskus Chia GirsangHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Caro Dart Al 2013
Diunggah oleh
Wilson Fransiskus Chia GirsangHak Cipta:
Format Tersedia
Review
Neurological complications of dengue virus infection
Francisco Javier Carod-Artal, Ole Wichmann, Jeremy Farrar, Joaquim Gascn
Lancet Neurol 2013; 12: 90619 Dengue is the second most common mosquito-borne disease aecting human beings. In 2009, WHO endorsed new
Neurology Department, guidelines that, for the rst time, consider neurological manifestations in the clinical case classication for severe
Raigmore Hospital, Inverness, dengue. Dengue can manifest with a wide range of neurological features, which have been noteddepending on the
UK (F J Carod-Artal PhD);
clinical settingin 0521% of patients with dengue admitted to hospital. Furthermore, dengue was identied in
Medicine and Health Sciences
Faculty, Universitat 447% of admissions with encephalitis-like illness in endemic areas. Neurological complications can be categorised
Internacional de Catalunya into dengue encephalopathy (eg, caused by hepatic failure or metabolic disorders), encephalitis (caused by direct virus
(UIC), Barcelona, Spain invasion), neuromuscular complications (eg, Guillain-Barr syndrome or transient muscle dysfunctions), and neuro-
(F J Carod-Artal); Department
ophthalmic involvement. However, overlap of these categories is possible. In endemic countries and after travel to
for Infectious Disease
Epidemiology, Robert Koch these regions, dengue should be considered in patients presenting with fever and acute neurological manifestations.
Institute, Berlin, Germany
(O Wichmann MD); Oxford Introduction Four antigenically distinct serotypes (DENV 14) circulate
University Clinical Research
Dengue is a mosquito-borne viral disease caused by one simultaneously in endemic countries,11 and all can cause
Unit, Hospital for Tropical
Diseases, Centre for Tropical of four closely related dengue virus serotypes (DENV 14). severe disease. Transmission occurs via aedes mosquitoes
Medicine, Oxford University, It is the second most common mosquito-borne disease that feed during daytime, with Aedes aegypti and Aedes
Ho Chi Minh City, Vietnam aecting human beings after malaria.1 Around 4 billion albopictus being the two main vectors.1
(J Farrar FRCP); Department of
Medicine, National University
people are at risk of the disease, with about 100 million Dengue is endemic in almost all tropical and
of Singapore, Singapore cases of symptomatic dengue occurring annually.2 subtropical countries. The highest incidences are
(J Farrar); and Barcelona Center Reported case-fatality rates of severe dengue range from reported in Asia and in Central and South America,
for International Health less than 02% to 5%.1 Population growth, urbanisation, although reports are increasing from African countries.1
Research (CRESIB), Hospital
Clinic-Universitat de Barcelona,
deterioration of mosquito-control programmes, and an In prospective cohort studies from Thailand and
Barcelona, Spain (J Gascn PhD) increase in air travel and trade have contributed to the Cambodia, the incidence of symptomatic dengue virus
Correspondence to: emergence and geographical spread of the disease over infection was more than 20 cases per 1000 children a
Dr Francisco Javier Carod-Artal, past decades.1,3 year, leading to around 2646 admissions per
Neurology Department, In 2009, WHO released new dengue guidelines and a 1000 children.12 Among travellers, dengue is a common
Raigmore Hospital, Inverness
new case classication, which included CNS involvement disease. In a cohort of 1207 short-term travellers from the
IV2 3UJ, UK
javier.carodartal@nhs.net in the denition of severe disease.1 From the time dengue Netherlands in 200607, the incidence of symptomatic
was recognised as a clinical entity, neurological dengue virus infection was four cases per 1000 adults.13
manifestations of the disease have been described.4,5
Factors that might contribute to neurological mani- Clinical ndings
festations include prolonged shock, hyponatraemia, Most dengue virus infections are asymptomatic.14
hepatic failure, or intracranial bleeding.4,6 Therefore, the Symptomatic infections were classied traditionally into
noted abnormal neurological signs in patients with undierentiated fever, dengue fever, dengue haemor-
dengue could be due to encephalopathy and not rhagic fever, and dengue shock syndrome.15
encephalitis.4 Since the end of the 1990s, evidence of Fever, severe frontal and retro-ocular headache, muscle,
dengue virus neurotropism has increased and the bone and joint pain, abdominal pain, nausea, and
number of reports on dengue patients with virus isolation vomiting are common during dengue fever. A mild
from CSF or brain tissue has risen.79 transient skin rash can arise, and a maculopapular or
We did a literature review of evidence for dengue virus scarlatiniform rash can be seen after the third or fourth
neuroinvasion and the frequency either of neurological day in half of infected people (gure 1). Dengue
features in patients presenting with dengue or of dengue haemorrhagic fever is dened by the presence of four
diagnosis in patients presenting with encephalitis-like criteria: fever, haemorrhagic features (eg, ecchymosis,
illness, at hospitals in endemic areas. Here, we discuss petechial haemorrhage, epistaxis, gum bleeding, vaginal
the ndings of our literature search and describe the or gastrointestinal bleeding), thrombocytopenia
epidemiology of dengue, its diagnosis, clinical manifest- (<100 000 platelets per L blood), and evidence of plasma
ations, and treatment of the disease and its neurological leakage due to increased vascular permeability.15
features. However, augmented vascular permeability and plasma
leakage (rather than haemorrhagic manifestations) are
Epidemiology, virus, and vectors the key features that dierentiate dengue haemorrhagic
Dengue viruses consist of single-stranded RNA and are fever from dengue fever. Dengue shock syndrome has
members of the Flaviviridae family (genus Flavivirus). the same characteristics as dengue haemorrhagic fever
The RNA genome includes seven non-structural (NS) in addition to circulatory failure, hypotension, and shock.
protein genes and three structural protein genes that The traditional case classication for dengue fever and
encode the capsid, membrane, and envelope proteins.10 dengue haemorrhagic fever has been used for several
906 www.thelancet.com/neurology Vol 12 September 2013
Review
decades and has supported decision making for the terms have been used interchangeably. Furthermore,
management of dengue. However, this classication is results from CSF testing for dengue were reported
dicult to apply, and many cases of severe dengue have rarely, in only 13 of these 55 context studies. CSF testing
been missed in some studies.1618 The new dengue case was done in patients with neurological manifestations
classication, published by WHO in 2009, categorises to check for CSF abnormalities and dengue diagnosis
the disease into dengue without warning signs, dengue (eg, dengue virus RNA, NS1, or dengue virus-specic
with warning signs, and severe dengue (panel 1).1 antibodies in CSF). 12 studies are summarised in
By comparison with the traditional case classication, tables 1 and 2 and one study of fatal dengue cases is
the update had similar specicity (785% vs 755%) but presented in table 3 (additional study details are
better sensitivity (921% vs 390%) to capture severe presented in the appendix, pp 16).8,9,2233 See Online for appendix
dengue cases that needed treatment in an intensive-care Of all laboratory-conrmed cases of dengue presenting
unit in Nicaragua.17 By contrast with the traditional at hospital, the proportion with neurological mani-
system, the revised classication also includes severe festations ranged between 05% and 54% in four
organ manifestations such as liver failure, heart studies from southeast Asia and was 21% in a prospective
involvement, or CNS involvement. Nevertheless, neuro- study from Brazil (table 1).8,9,2225 Of those with
logical complications are not well described in the 2009 encephalitis-like illness or suspected CNS infection, the
guidelines, and little is known about the frequency of proportion of patients with dengue ranged between 46%
these manifestations. and 20% in ve studies from Asia and was 47% in a study
Why do most dengue virus infections lead to from Brazil and 26% in one from Puerto Rico (table 2).8,2632
asymptomatic or mild self-limiting disease, and why do CNS involvement has been described in all three
some infected people develop severe dengue? categories of the traditional case classication: dengue
Subsequent (secondary or tertiary) infection with a fever, dengue haemorrhagic fever, and dengue shock
heterologous dengue virus serotype has been postulated syndrome.
to be the main factor associated with severe disease, via 98 case reports and series were identied by the
antibody-dependent enhancement.19,20 According to this literature search on dengue-associated encephalitis and
hypothesis, non-neutralising antibodies from a encephalopathy, multiple neurological manifestations of
previous dengue virus infection facilitate cell invasion, dengue, and autopsy studies of patients with dengue who
enhance viraemia, and initiate a self-amplifying cascade had neurological manifestations (gure 2). Of these,
that can lead to release of cytokines and other pro- 67 were published between 2000 and 2013 and 31 were
inammatory mediators.21 However, severe dengue published between 1960 and 1999. 33 reports were of
cases have been described that are primary infections, patients with dengue encephalitis and 41 were of cases
and strains of dengue virus exist that cannot be with encephalopathy.
enhanced, suggesting that additional viral and host In total, eight autopsy studies were identied by our
factors have a role in the development of severe literature search that reported on fatal dengue virus
dengue.3 infection with neurological manifestations (table 3).4,3340 In
Neurological complications
Neurological complications of dengue virus infection can
be categorised into dengue encephalopathy, encephalitis,
immune-mediated syndromes, dengue muscle
dysfunction, and neuro-ophthalmic disorders. However,
in practice, classication can be dicult because these
categories overlap and clinical dataeg, for CSF
examinationsmight be missing.
In our literature search, we identied 247 publications
describing original studies or reports of dengue with
neurological, neuromuscular, or neuro-ophthalmic
complications (gure 2). In 55 of these, the number of
patients with neurological manifestations of dengue
was presented as a proportion either of total admissions
for dengue or of all individuals with encephalitis-like
illness (classied as context studies). Manifestations
compatible with encephalitis were mentioned in
24 context studies and complications according with
encephalopathy were noted in 20; in the remaining 11,
either both terms were used or multiple neurological
manifestations were described. However, these two Figure 1: Maculopapular rash in a 29-year-old man with dengue
www.thelancet.com/neurology Vol 12 September 2013 907
Review
In a retrospective assessment from Indonesia,
Panel 1: 2009 WHO clinical case classication for dengue1 152 (6%) patients with dengue encephalopathy were
Criteria for dengue and warning signs identied from 2441 people admitted to hospital for
Probable dengue dengue haemorrhagic fever.6 152 had normal CSF
Fever analyses, 146 had altered consciousness, and 123 had
and two of either seizures. Of 98 cases classied by the traditional case
Nausea or vomiting denition, most (78%) had pending or profound shock.
Rash The diagnosis of dengue haemorrhagic fever was based
Aches and pain (headache, myalgia, arthralgia) on clinical criteria only; no examinations were done to
Tourniquet test positive detect dengue virus or antibodies in CSF or serum.6 In
Leucopenia Thailand, neurological manifestations were recorded in
Any warning sign 80 (5%) of 1493 children with serologically conrmed
dengue, and half presented with encephalopathy
Warning signs
(table 1).23 Laboratory ndings included hyponatraemia,
Abdominal pain or tenderness
abnormal liver enzymes, and CSF pleocytosis. Dengue
Persistent vomiting
virus-specic IgM and dengue virus RNA in PCR were
Clinical uid accumulation
not recorded in 16 available CSF specimens; however, no
Mucosal bleeding
information was provided on the tests used and the day
Lethargy, restlessness
of illness. One of the 80 children had evidence of
Liver enlargement >2 cm
encephalitis based on histopathological ndings at
Increase in packed-cell volume concurrent with rapid fall
autopsy (four children died; results from autopsy were
in platelet count
provided for one).23 In a retrospective review from
Criteria for severe dengue Thailand of 18 people (including ten who died) with
Either dengue haemorrhagic fever and neurological features,
Severe plasma leakage leading to CSF was normal in all ve patients who were tested.4
Shock (dengue shock syndrome) Shock, jaundice, metabolic acidosis, and intracranial
Fluid accumulation with respiratory distress (subdural and pons) haemorrhage were noted. CSF or
Or brain tissue analyses for dengue virus RNA or antigen
Severe bleeding (assessed by clinician) were not done.4 In a retrospective review from Thailand
Or
of patients with dengue (199599), encephalopathy was
Severe organ involvement
most usually seen in obese children (13% vs 05% in
Liver enzyme concentrations, aspartate
children of normal weight) and in babies (41% vs 06%
aminotransferase or alanine aminotransferase
in children aged 1 year or older).42,43
1000 U/L
The outcome of individuals with dengue encephalo-
CNS involvement, impaired consciousness
pathy is variable and depends on causal factors. Without
Heart or other organ involvement
supportive treatment mortality can be high. In a case
series of 15 patients with dengue encephalopathy from
Sri Lanka (all dengue shock syndrome) seven cases were
these reports, dengue virus was identied by PCR or virus fatal.44 Factors that contributed to encephalopathy
isolation in CSF (two studies used this method) or in included acute liver failure (11 cases), electrolyte
brain tissue (four studies). Moreover, dengue virus antigen imbalances (12), and shock (six).
was identied by immunohistochemical methods in ve
studies. Autopsy ndings showed cerebral congestion or Encephalitis
oedema most typically, and histopathological evidence for In the past decade, an expanded clinical spectrum has
encephalitis was provided rarely (table 3). emerged of encephalitis due to CNS invasion and
neurotropic eects of dengue virus. Five studies were
Dengue encephalopathy identied by our literature search that provided results of
Acute encephalopathy is the most commonly reported CSF analysis of cell counts and detection of dengue virus
neurological disorder associated with dengue virus or dengue virus antigen among patients admitted with
infection. Dengue encephalopathy involves a diminished dengue (table 1).8,9,2224 In a prospective study from
level of consciousness that can be precipitated or caused Vietnam, 16 (1%) of 1691 patients admitted with suspected
by several factors, including prolonged shock, anoxia, dengue virus infection had neurological presentations,
cerebral oedema, metabolic disturbances (eg, hypo- and another ve dengue-positive patients had CNS
natraemia), systemic or cerebral haemorrhages, acute abnormalities.8 Of these 21 individuals, dengue virus was
liver failure, or renal failure.6,41 CSF analyses, including isolated or detected by PCR in CSF in ten. Nine of these
measurements of protein, glucose, and cell count, are patients were classied as having dengue with
usually normal. encephalitis. In a study from Brazil, 11 of 18 patients with
908 www.thelancet.com/neurology Vol 12 September 2013
Review
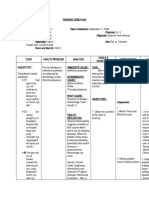
Search strategy (using PubMed and Scopus online databases): dengue AND (encephal*
OR neurolog* OR stroke OR myositis OR ophthalmic OR ocular OR unusual
manifestations) with publication dates from 1959 to June 4, 2013
1943 publications identified
24 found by hand-search
1696 excluded (not relevant to the topic)
247 publications
57 on dengue-associated neuromuscular 153 on dengue encephalitis, encephalopathy, 37 on dengue-associated neuro-ocular
or immune-mediated complications or stroke complications
55 context studies 98 case reports or case series
13 Guillain-Barr syndrome 35 admissions for dengue or dengue 33 encephalitis or meningitis 13 maculopathy
1 Miller-Fisher syndrome haemorrhagic fever 26 single case reports 9 case series, various ocular complications
7 ADEM 18 encephalitis or CNS infection 7 case series 5 retinal vasculitis, vein occlusion,
5 acute transverse myelitis 2 fatal dengue or fatal infectious 41 encephalopathy or oedema
9 neuropathy or plexopathy disease* 20 single case reports 3 optic neuritis or neuropathy
(eg, phrenic nerve or brachial) 8 case series 3 premacular or retinal haemorrhage
1 compressive myelopathy 13 haemorrhagic 1 corneal ulceration
1 parkinsonism 7 fatal and autopsy* 1 uveitis
4 hypokalaemic paresis 17 case series, various neurological 1 papilloedema
1 various neurological features complications 1 oculomotor paresis
12 myositis or myopathy 13 with CSF testing (cells, dengue
3 rhabdomyolysis virus PCR or isolation, IgM)
Figure 2: Search strategy showing identication and inclusion of relevant studies
Studies were classied into reports presenting cases with encephalitis or encephalopathy, according to the term used in the study. *For details see table 3. For details
see tables 1 and 2. ADEM=acute disseminated encephalomyelitis.
neurological features of dengue were classied as having whether these six patients represent true encephalitis (ie,
encephalitis (table 1).9 caused by direct virus invasion) or encephalopathy cases.
Table 2 presents the proportion of dengue among Some case reports and case series were identied by our
admitted patients with encephalitis-like illness (n=6) or literature search in which patients were described with
febrile encephalopathy (n=1).2632 In a hospital-based case probable dengue encephalitis (gure 2); however, in only a
series from Thailand, eight of 40 children admitted with few reports were data presented of CSF examinations for
encephalitis had dengue virus infection.26 In India, dengue virus or dengue virus antigen.7,4547 Other
dengue virus was the cause of acute febrile mechanisms apart from neuroinvasionsuch as blood
encephalopathy in 39 (15%) of 265 children.29 In 21 of brain barrier compromisemight lead to the presence of
29 CSF samples tested, the presence of dengue virus was virus in the intrathecal space. Pleocytosis and high viral
shown by PCR, and in 16 of 36 CSF samples, the white- load in CSF without blood contamination indicate the
blood-cell count was raised (44% polymorphs on neuroinvasive capacity of dengue virus. However, in most
average).29 In Brazil, ndings of a hospital-based studies that presented CSF results (tables 1 and 2), a
prospective case series showed that dengue not only was proportion of cases with dengue CNS involvement not
the leading cause of encephalitis (in eight of 17 cases) but only had no pleocytosis but also had no other underlying
also was detected in two of 20 patients with viral complications such as severe liver involvement, making
meningitis.31 Pleocytosis was present in two of two patients denite categorisation into either encephalitis or
clinically diagnosed with dengue meningitis and in encephalopathy dicult (panel 2).
two of eight patients with dengue encephalitis, and Nine publications presented data from autopsy studies
dengue virus was detected by PCR in CSF in both groups (table 3),4,3340 and additional fatal cases were reported
(table 2). However, because six of the eight patients with within some context studies (appendix pp 12).23,25 Evidence
encephalitis had normal CSF cellularity and none of of dengue virus neurotropism from these studies is
them had dengue virus-specic IgM, we are unsure convincing. Of three fatal cases from Thailand, dengue
www.thelancet.com/neurology Vol 12 September 2013 909
Review
Country Study design; population Proportion with neurological CSF diagnosis Clinical manifestations
features
Cam et al (2001)22 Vietnam Prospective case-control; 27 of 5400 (05%) 14 of 22 IgM-positive; Coma (26 of 27), seizures (21 of 27),
5400 children (age 015 years) one of 22 PCR-positive; hemiplegia (1 of 27);
admitted with dengue haemorrhagic 22 of 22 normal protein, glucose, cells 22% case fatality
fever
Domingues et al Brazil Prospective; 85 admissions (all ages) 18 of 85 (21%) Seven of 13 PCR-positive (copy number Encephalitis (11 of 18), encephalopathy
(2008)9 with laboratory-conrmed dengue 265417 per mL); (6 of 18), meningitis (1 of 18)
three of seven PCR-positive in CSF but
PCR-negative in serum;
four of six PCR-negative in CSF but
PCR-positive in serum
Pancharoen and Thailand Retrospective; 1493 children 80 of 1493 (54%) 0 of 16 IgM-positive; Encephalitis (42 of 80), seizures
Thisyakorn (2001)23 (age 015 years) admitted with 0 of 16 PCR-positive; (35 of 80), miscellaneous (3 of 80);
laboratory-conrmed dengue seven of 31 pleocytosis in CSF four (5%) of 80 died, one of 80 had
long-term neurological sequelae
Solomon et al (2000)8 Vietnam Prospective; 378 children and adults 16 of 1691 (1%) admissions Eight of 16 IgM-positive; Encephalitis (9 of 21), encephalopathy
with suspected CNS infection in for dengue; 16 of 378 (4%) four of 16 PCR-positive or (9 of 21), transverse myelitis (2 of 21),
intensive-care unit, and 1691 with suspected CNS infection; isolation-positive; three of four meningism (1 of 21)
admissions for dengue ve additional cases with CNS IgM-negative but PCR-positive or
abnormalities studied isolation-positive in CSF;
subsequently three of 21 with pleocytosis; seven of
21 with protein >45 g/L
Thisyakorn et al Thailand Prospective; 2975 children 30 of 2975 (1%) Two of 19 IgM-positive; Altered consciousness (23 of 30 with
(1999)25 (update (age 014 years) admitted with six of 28 pleocytosis CNS symptoms); seizures (19 of 30),
from 1994)24 serologically conrmed dengue pyramidal-tract signs (11 of 30),
meningeal signs (9 of 30)
Further study details are presented in the appendix (pp 12).
Table 1: Proportion of neurological features in patients admitted with dengue or dengue haemorrhagic fever
Country Study design; population Proportion with dengue CSF diagnosis Clinical manifestations
diagnosis
Chokephaibulkit et al Thailand Prospective; 40 children admitted Eight of 40 (20%) One of eight PCR-positive; All eight had signs of encephalitis, one of
(2001)26 with possible encephalitis or one of eight increased protein (69 g/L) eight had facial palsy (PCR-positive in CSF)
meningoencephalitis
Garca-Rivera et al Puerto Rico Prospective; 84 patients (all Nine of 34 (26%) with One IgM-positive; Encephalitis (9 of 11), motor disorder
(2009)27 ages) with suspected acute encephalitis-like illness; three of ve with mild pleocytosis; (2 of 11); two of 11 died
neurological infection (enhanced two of 11 (18%) with motor four of ve increased protein
hospital-based surveillance system), disorders
34 encephalitis-like illness, 25 aseptic
meningitis, 11 with motor disorder
Kankirawatana et al Thailand Prospective; 44 children Eight of 44 (18%) One PCR-positive (cranial nerve palsy); Altered consciousness (8 of 8), cranial
(2000)28 (age 712 years) with acute none of eight tested for pleocytosis; nerve palsy (1 of 8), meningism (2 of 8),
viral encephalitis one of eight mildly increased protein papilloedema (1 of 8)
Kumar et al (2008)29 India Prospective; 265 children 39 of 265 (15%) 21 of 29 PCR-positive (copy number Seizures (31 of 39), meningeal signs
(age 112 years) with acute 3568 718); 16 of 36 increased cell (7 of 39), hyperventilation (13 of 39),
febrile encephalopathy number cranial nerve palsies (4 of 39), neurological
decits (4 of 39); nine of 39 died
Le et al (2010)30 Vietnam Prospective; 194 children Nine of 194 (5%) Four of nine PCR-positive; six of nine Limb weakness (2 of 9), neck stiness
(age <16 years) admitted with acute virus isolation-positive; seven of nine (2 of 9), seizures (1 of 9); three of nine
encephalitis (presumed viral) IgM-positive; none of nine tested for with Glasgow coma score 9, one of nine
pleocytosis died
Soares et al (2011)31 Brazil Prospective; 37 adolescents and Eight of 17 (47%) with Of eight with encephalitis, one Seizures (7 of 8), mental confusion (4 of 8)
adults with viral meningitis (20) encephalitis; PCR-positive, one IgM-positive, and
or encephalitis (17) two of 20 (10%) with viral two with pleocytosis; of two with
meningitis meningitis, one PCR-positive, two with
pleocytosis
Srey et al (2002)32 Cambodia Prospective; 99 patients (47 adults, Four of 52 (8%) Three of four PCR-positive; one of four All four had encephalitis
52 children) admitted with clinical IgM-positive, but serum:CSF antibody
encephalitis titre ratio >40
Further study details are presented in the appendix (pp 34).
Table 2: Proportion of dengue diagnoses in patients admitted with encephalitis or encephalopathy
910 www.thelancet.com/neurology Vol 12 September 2013
Review
Country; study setting Description of fatal dengue CSF diagnosis Dengue testing of brain tissue Neuropathological autopsy
cases results
Arajo et al (2012)33 Brazil; retrospective 84 dengue cases among Seven of 41 PCR-positive; NA Histopathological evidence for
context study on fatal 150 deaths, including 41 with one of 41 isolation-positive; meningitis (9 of 75) and
cases (age 086 years) neurological features 22 of 41 NS1-antigen-positive; encephalitis (3 of 75); of 41 with
with suspected (45 dengue fever, 20 dengue 27 of 41 IgM-positive neurological features of dengue,
infectious disease haemorrhagic fever, 13 had cerebral congestion,
19 dengue not suspected) 23 oedema, one haemorrhage, two
brain necrosis, two cerebellum
oedema, two cerebellum congestion
(multiple ndings possible)
Bhoopat et al (1996)34 Thailand; Chiang Mai Three fatal cases NA Dengue virus antigen in NA
hospital (age 513 years) with parenchymal cells
neurological features (immunoperoxidase stain),
(all dengue haemorrhagic including cerebral cortex neurons,
fever) Purkinje cells in cerebellum,
microglia, and astrocytes
Chimelli et al (1990)35 Brazil; outbreak in Five fatal cases CSF not tested for dengue; Three of ve were positive for Brain oedema (3 of 5), focal
and Miagostovich et al Rio de Janeiro (age 1651 years) with one of two normal, one of two dengue virus antigen haemorrhages (5 of 5), perivascular
(1997, follow-up neurological features with 175 leucocytes per L (immunoperoxidase stain) in brain lymphocytes (5 of 5), perivenous
study)36 (all dengue fever) tissue demyelination (1 of 5)
Janssen et al (1998)40 Dutch traveller after One fatal case (age 25 years) NA PCR-positive (DENV 3); virus Brain diusely swollen, secondary
returning from Thailand with neurological features isolation-positive from brain tissue haemorrhage in the pons; no
(dengue fever) inltration of mononuclear cells;
no signs of meningoencephalitis
Nimmannitya et al Thailand; retrospective Ten fatal cases CSF not tested for dengue; NA Microscopic examination showed
(1987)4 review of autopsy (age 012 years) with unusual two of ve normal, three of no pathological evidence of
reports and microscopic neurological manifestations ve with red blood cells encephalitis; brain oedema
slides at Childrens (all dengue haemorrhagic (3 of 10), intracranial haemorrhage
Hospital, Bangkok fever) (6 of 10), unremarkable (1 of 10)
Nogueira et al (2002)37 Brazil; state of Rio One fatal case (age 67 years) NA Positive for dengue virus antigen Brain oedema; no inltration of
Grande do Norte with neurological features (immunoperoxidase stain) in mononuclear cells
(dengue fever) cerebral cortical grey matter;
DENV 2 isolation-positive and
PCR-positive
Nogueira et al (2005)38 Brazil; outbreak in 40 fatal cases (age 765 years); One of two PCR-positive; none Three of three PCR-positive; none Oedema and congestion of brain;
Rio de Janeiro proportion with neurological of two isolation-positive; of three isolation-positive; two of microhaemorrhagic foci; no
features unknown none of two IgM-positive seven positive striking inammatory reactions
immunohistochemistry noted; frequent meningeal
congestion
Ramos et al (1998)39 Mexico; outbreak in 1 fatal case (age 17 years) with NA PCR-positive in tissue from inferior Slight meningeal opacity; vein
Sinaloa neurological features (dengue olivary nucleus of medulla and congestion; generalised oedema
haemorrhagic fever) granular layer of cerebellum; with bilateral uncus herniation; no
positive immunohistochemistry distinctive histopathological
features of brain viral infection
NA=not available. Further study details are presented in the appendix (pp 56).
Table 3: Neurological manifestations of fatal dengue
virus antigen was detected in parenchymal cells of the seem more common in individuals with dengue
brain using immunoperoxidase stain.34 In a fatal case from encephalitis than in those with encephalopathy; in a
Brazil, analysis of cerebral cortical grey matter showed study of 16 patients with dengue encephalitis, generalised
dengue virus antigen and DENV 2 was detected by PCR in seizures were noted in roughly half of them.8 Epilepsia
ground brain.37 In a series of 40 laboratory-conrmed fatal partialis continua has been described as a manifestation
cases of dengue from Brazil,38 dengue virus was detected of dengue encephalitis in a case report.49
by PCR in three of three brain samples and dengue virus Because manifestations of dengue encephalitis and
antigen was recorded in two of seven samples. However, dengue encephalopathy are indistinguishable clinically,
despite the presence of dengue virus or dengue virus acute liver failure, hypovolaemic shock with metabolic
antigen in brain tissue, distinctive histopathological deteriorations, and intracranial haemorrhage need to be
features of viral brain infection were not noted (table 3). ruled out, and CSF examinations should be done if safe
Patients with dengue encephalitis can present with and feasible. The outcome of dengue encephalitis is
diminished consciousness, headache, dizziness, variable, with most patients recovering spontaneously in
disorientation, seizures, and behavioural symptoms.9,48 one case series whereas some deaths were noted in
Tetraparesis might be seen in severe cases.41 Seizures others.27,30,41
www.thelancet.com/neurology Vol 12 September 2013 911
Review
invasion can take place in the parainfectious stage
Panel 2: Proposed denitions for neurological features of dengue whereas immune-mediated factors are noted post-
Dengue diagnostic test highly suggestive of or conrming acute dengue virus infection, infection. Several cases of post-dengue acute transverse
as recommended by WHO*, AND one of the following clinical categories: myelitis have been reported.6166 Here, acute weakness
and numbness of the lower limbs and urinary retention
Dengue CNS involvement are seen. Post-infectious immune-mediated myelitis
At least one of the following: impaired consciousness (for children younger than 6 years, usually arises 12 weeks after the onset of initial
Blantyre coma score 4; for those older than 5 years, Glasgow coma score 14), neck symptoms,61 whereas parainfectious myelitis can take
stiness, focal neurological signs, or seizure place within the rst week of infection.63,64
Dengue encephalopathy Intrathecal synthesis of dengue virus-specic IgG
Dengue CNS involvement, AND antibodies has been detected in patients with dengue
Presence of one of the following dengue-associated complications: hepatic failure, myelitis.65 MRI of the spinal cord can either be normal or
metabolic acidosis, severe hyponatraemia, prolonged shock, disseminated show areas of high signal on T2-weighted sequences.61
intravascular coagulation, or brain haemorrhage, AND In some patients, T2-weighted MRI shows a high-
Normal CSF (in brain haemorrhage, blood in CSF is possible) intensity signal from the lower cervical to upper lumbar
Dengue encephalitis
regions in the spinal cord.64
Dengue CNS involvement, AND
Presence of dengue virus RNA, IgM, or NS1 antigen in CSF, AND
Acute disseminated encephalomyelitis and neuromyelitis optica
CSF pleocytosis without other neuroinvasive pathogens
Some cases of acute disseminated encephalomyelitis
have been reported in the convalescence stage of dengue
Immune-mediated dengue CNS involvement virus infection, in both classic dengue fever and dengue
Other or non-specied dengue CNS involvement haemorrhagic fever.50,65,6776 CSF analysis might show a
moderate rise in protein concentration and pleocytosis.69,72
Dengue-associated neuromuscular complications
Brain MRI can show areas of high signal on T2-weighted
Guillain-Barr syndrome
images and gadolinium enhancement on T1-weighted
Rhabdomyolysis
images (gure 3).69,72,77 In patients with neuromyelitis
Other or non-specied peripheral neuromuscular complications
optica, many high-intensity lesions can be seen on T2-
Dengue-associated neuro-ophthalmic complications weighted images in the spinal cord, whereas MRI images
One of the following clinical symptoms: blurred vision, eye ashes, oaters, sudden of the brain show no abnormalities.72
decrease in vision, visual eld defect, scotoma, eye redness, metamorphopsia, or
micropsia, AND Guillain-Barr syndrome
Eye examination with at least one of the following: optic neuropathy (optic disc Dengue virus infection preceding Guillain-Barr
swelling or hyperaemia), maculopathy (oedema or blot haemorrhages), retinal syndrome has been described in case reports and case
vasculitis, retinal haemorrhages, exudative retinal detachment, cotton wool spots, or series of patients presenting with various neurological
signs of foveolitis or anterior uveitis manifestations.27,59,60,65,70,7891 Acute onset of limb weakness
and areexia was noted a week after symptom
*Highly suggestive dengue is dened as: IgM-positive in one serum sample; or IgG-positive in one serum sample with
haemagglutination inhibition titre of 1280 or greater. Conrmed dengue is dened by one of the following: PCR-positive; virus
onset.59,70,7881,83 The acute pure axonal motor-sensory
culture-positive; IgM seroconversion in paired serum samples; IgM seroconversion in paired serum samples or four-times IgG variant of Guillain-Barr syndrome has also been
titre increase in paired serum samples.1 described after dengue virus infection.89 CSF analysis
might show increased protein concentrations without
Post-dengue immune-mediated syndromes pleocytosis (albumin-cytological dissociation). Guillain-
Post-dengue immune-mediated neurological syndromes Barr syndrome has also been described in patients with
include acute transverse myelitis, acute disseminated oligosymptomatic dengue virus infection.84
encephalomyelitis, and Guillain-Barr syndrome
(gure 2). Reports are rare of neuromyelitis optica,50 Cerebrovascular complications
Miller-Fisher syndrome,51 and mononeuropathies such Intracranial haemorrhages have been reported during the
as phrenic neuropathy,5254 long thoracic neuropathy,55 convalescence stage of dengue.75,92 The incidence of
isolated Bells palsy,56 abducens nerve palsy,57 and dengue-associated cerebrovascular complications is
oculomotor palsy.58 Usually, post-infectious disorders are unknown, although haemorrhagic stroke seems more
only linked temporally to dengue virus infection, with a common than ischaemic stroke. During an epidemic in
causal association merely inferred. Post-dengue India, 1148 laboratory-conrmed dengue patients were
syndromes generally resolve within weeks or a admitted to hospital and three had a stroke (026%).93
few months, as is typical with these disorders.54,57,59,60 During the 2003 epidemic in Brazil, only one patient with
brain haemorrhage was registered among 1585 conrmed
Acute transverse myelitis dengue cases.94 However, in dengue-endemic countries,
Spinal cord involvement can happen in patients with we assume that patients with haemorrhagic or ischaemic
dengue both during and after infection. Direct virus stroke are tested rarely for dengue.
912 www.thelancet.com/neurology Vol 12 September 2013
Review
Most patients have intracranial bleeding a week after
A B
fever onset.92 Acute intracranial bleeding can arise without
other (visible) haemorrhagic manifestations. Basal ganglia
haemorrhages and multiple haemorrhagic foci in brain
lobes are recorded.4 Less common presentations of
intracranial bleeding include bilateral cerebellar
haemorrhage with oedema, mass eect, and obstructive
hydrocephalus,93 pontine haemorrhage,94 acute subdural
haematoma,9597 multiple acute subdural haematomas,92
pituitary adenoma haemorrhage,98 subarachnoid
haemorrhage, and focal subarachnoid haemorrhage
4,75
associated with transient thrombocytopenia.99 In some
cases of fatal subarachnoid haemorrhage, post-mortem
examination did not show intracranial aneurysmeg, in
a traveller returning to Norway.100
Cases of dengue fever with thrombocytopenia and
ischaemic stroke are possible but infrequent.101 Brain CT
and MRI should be done to conrm a clinical suspicion
Figure 3: FLAIR and T2-weighted MRI of acute disseminated encephalomyelitis
of stroke. Several areas of watershed infarcts, small
(A) FLAIR MRI. (B) T2-weighted MRI. Images show involvement of bilateral lentiform nuclei in a 10-year-old girl
cortical infarctions, and dysarthria clumsy-hand with the rare post-dengue neurological manifestation acute disseminated encephalomyelitis. Reproduced from
syndrome due to corona radiata and putamen infarction Palma-da Cunha-Matta et al,70 with permission of Viguera Editores.
have been reported.93,102 Gradient-echo MRI can be useful
to detect small bleeds, and diusion-weighted images rhabdomyolysis.106,107,110 Motor weakness might range from
can show subacute infarctions. mild hypotonia and proximal muscle weakness in both
upper and lower limbs to asymmetrical weakness of lower
Dengue muscle dysfunction limbs and severe quadriparesis.108,110 Motor quadriplegia
Few epidemiological studies have been done to assess and neck, trunk, and respiratory muscle weakness that
the incidence of neuromuscular complications after could lead to death have been noted in severe cases.108,111
dengue virus infection. In a Saudi Arabian hospital- Amounts of creatine phosphokinase in serum can be
based study of 101 patients with dengue conrmed by raised during the rst week of illness; in one case series,
serological analysis (42% dengue haemorrhagic fever, values ranged from 500 IU/L to more than 100 000 IU/L,108
58% dengue fever), raised amounts of creatine with a median of 837 IU/L in another study.104 High
phosphokinase were recorded in 91%, myalgia in 63%, concentrations of creatine phosphokinase might be
and mild proximal muscle weakness in 3%.103 In India, of secondary to intense muscle inammation.108 Dengue
39 cases of dengue conrmed serologically, 16 had myositis and myocarditis, with augmentation of the
clinical and 15 had subclinical muscle involvement.104 creatine kinase muscle:brain ratio, can happen
Of these 31, eight people had severe weakness and ve simultaneously.104,112
had hyporeexia; severity correlated with creatine Dengue muscle dysfunction diers from typical
phosphokinase concentrations. In another study from inammatory myopathy because of a paucity of ndings
India, of 40 children with benign acute childhood on electromyography and an absence of spontaneous
myositis, 20 were positive for dengue virus-specic activity.104 An electromyogram can show early recruitment
antibodies, indicative of acute infection.105 of motor-unit action potentials with normal morphological
Clinical studies based on case reports (n=1) and small ndings and no spontaneous activity.108 Motor-unit action
case series (231 patients) describe pure motor weakness potentials might be of normal-to-short duration and
associated with dengue virus infection.104116 The clinical polyphasic with full recruitment, in accordance with mild
picture in these reports is highly variable. The weakness myopathic changes.104 Mild-to-moderate perivascular
was generally referred to as dengue myositis, but recently, mononuclear inltrates, interstitial haemorrhage with
the term dengue-associated transient muscle dysfunction occasional myonecrosis, and lipid accumulation have
has been proposed because of the benign and self- been noted in muscle biopsy specimens.110,113,117
limiting nature of the disorder.104 Dengue virus could be In general, dengue muscle dysfunction is judged a
one of the main causes of childhood benign acute viral benign presentation of dengue virus infection, and
myositisalso called myalgia cruris epidemicain spontaneous recovery happens in most patients within
tropical regions.105 12 weeks. Severe fulminant myositis and severe
Dengue virus infection can present with varying degrees persistent steroid-responsive myositis are reported
of transient myalgia, characterised by muscle tender- infrequently.108,111,114 Dierential diagnoses include
ness on stretching, motor weakness, raised amounts bacterial myositis and leptospirosis muscle involvement.
of muscle enzymes, andin very severe cases Normal ndings on nerve-conduction studies and an
www.thelancet.com/neurology Vol 12 September 2013 913
Review
absence of albumin-cytological dissociation are useful to brain tissue, and concomitant pleocytosis lends support
exclude Guillain-Barr syndrome. to the hypothesis of direct viral invasion of brain
parenchyma (tables 13). Furthermore, the simultaneous
Neuro-ophthalmic complications nding of viral RNA in CSF and negative RT-PCR in
Neuro-ophthalmic manifestations of dengue typically serum samples suggests that dengue virus might enter
entail the posterior segment. Anterior uveitis without the CNS actively and that the presence of virus in the
evidence of posterior segment involvement can happen CNS does not result from passive crossing of the blood
rarely and be associated with progressive loss of vision.118 brain barrier or vascular leakage.8,9
Ocular complications include dengue maculopathy, From a pathological point of view, encephalitis is a
retinal oedema, retinal haemorrhages, optic disc swelling, histopathological diagnosis based on inammation of
optic neuropathy, and vitritis. Incidence of these disorders brain parenchyma. Therefore, ndings of autopsy studies
is probably underestimated; neuro-ophthalmic com- provide substantive evidence for the neuroinvasive
plications usually develop during the convalescence stage capacity of dengue virus, by showing dengue virus or
of dengue virus infection and without systemic bleeding dengue virus antigen in brain tissue concomitant with
diathesis. Many patients with ocular complications have histopathological features of brain infection.23,25,33,36
classic dengue fever with normal platelet counts and However, in some autopsy studies, dengue virus or
without substantial haemodynamic derangement.119 In dengue virus antigen have been reported in brain tissue
Singapore, the estimated prevalence of dengue without histopathological brain changes (table 3); non-
maculopathy was 10% among 160 admissions for specic lesionsoedema, vascular congestion,
dengue.120 In India, ocular involvement was noted in 40% haemorrhagic foci, and perivascular lymphocytic
of 134 dengue admissions.121 inltrateswere predominant features in these patients.
Retinal vasculopathy might be the most common ocular Dengue virus replicates within the cells of the immune
manifestation of dengue virus infection.122 Another typical system, particularly macrophages and monocytes. Virus
feature is retinal haemorrhage attributable to increased entry via infected macrophages and histamine release
vascular permeability and breakdown of the inner blood have, therefore, been implicated as potential mech-
retinal barrier. Occlusion of precapillary arterioles can anisms.36,129,130 Dengue virus antigen has also been
provoke microinfarctions of the nerve bre layer, which detected in neurons of infected mice, and viral tropism
can be detected as cotton wool spots on ophthalmological for neurons of anterior horns, hippocampus, and
examination.123 In case series, the most common ocular cerebral cortex has been shown in vivo.131 Viral factors are
nding was dengue maculopathy presenting as macular important in neuropathogenesis, and changes in dengue
oedema, haemorrhage, or both, yellow spots in the virus replication and assembly might augment apoptosis.
macula, and focal chorioretinitis with or without retinal In a murine model of dengue encephalitis, mutations of
vasculitis.120,124 In a retrospective series of 41 patients with three aminoacids in DENV 1 produced a neurovirulent
impaired vision from dengue-related maculopathy, phenotype, resulting in extensive brain damage with
blurring vision (21 cases) and central scotoma (14 cases) encephalitis and leptomeningitis.132 Similar to other
were the most frequent visual complaints.124 Exudative aviviruses, the envelope protein might have an
maculopathy and small haemorrhages located in the optic important role in regulating CNS invasiveness and the
nerve bre layer can provoke reduced visual acuity. neurovirulence of dengue virus.133 However, since mice
Optic neuropathy has been described in a few cases.125,126 are not a perfect model for dengue virus, these ndings
Bilateral visual loss secondary to pituitary adenoma and cannot necessarily be extrapolated to account for the
bilateral vitreous haemorrhage associated with dengue pathogenesis in human beings.
fever have also been reported.98,127 Most patients recover
spontaneously to their best-corrected visual acuity Other dengue-associated neurological complications
without specic treatment between 1 week and 3 months Pathogenic mechanisms of dengue cerebrovascular
after onset.120 Nevertheless, some people might complain complications are not understood completely. Dengue
of persistent scotoma, and visual impairment could virus infection might result in the release of mediators
remain in cases of severe exudative maculopathy and (including cytokines, chemokines, and complement-
retinal haemorrhage.118,128 associated viral particles) with vasoactive or procoagulant
properties, capillary leakage, increased brinolysis, and
Pathogenesis of neurological features of dengue bleeding. Altered prothrombin time, severe thrombo-
Dengue virus encephalitis cytopenia, disseminated intravascular coagulation, and
The pathogenesis of dengue neurological involvement vasculitis can lead to haemorrhagic infarction and stroke.129
and underlying virushost interactions remain to be The precise pathogenesis of acute disseminated encephalo-
elucidated. For a long time, uncertainty surrounded myelitis remains unknown, but because virus has not
whether dengue virus crossed the bloodbrain barrier been isolated from the CSF of patients infected with
passively or whether active viral CNS invasion took place. dengue virus and with acute disseminated encephalo-
Detection of dengue virus RNA in CSF, viral antigen in myelitis, an immune-mediated cause is supported.41,69,75
914 www.thelancet.com/neurology Vol 12 September 2013
Review
Dengue virus could trigger a complex immune response, To dierentiate dengue encephalitis from encepha-
resulting in cytokine overproduction (interleukin 2, lopathy, detection of dengue virus, NS1 antigen, or
interferon , and tumour necrosis factor ) and inversion dengue virus-specic IgM antibodies in CSF is helpful.
of the CD4:CD8 ratio.134 Cytokines can provoke immune- Nevertheless, sensitivity of serological techniques can be
mediated dysfunction of endothelial cells.133 Furthermore, low. Dengue virus-specic IgM antibodies have been
increased vascular permeability with subsequent recorded in CSF of 2233% of patients diagnosed with
hypotension and prolonged shock, metabolic disturbances, dengue encephalitis (tables 1 and 2).90 Detection of
and hepatic dysfunction in patients with severe dengue dengue virus in CSF could be hampered by low sensitivity
might contribute to the pathogenesis and presentation of of RT-PCR in CSF, compared with ndings in serum,
other neurological complications, such as encephalopathy because of a lower viral load.137 Moreover, measurement
or even rhabdomyolysis.134 of IgM antibodies in CSF might not be a reliable
Pathogenic mechanisms of neuro-ophthalmic dengue diagnostic marker of dengue CNS involvement, owing to
are poorly understood, although an immune-mediated low titres in CSF.138 Abnormalities in CSFsuch as
process has been suggested.120 Immunological activation lymphocytic pleocytosissupport the diagnosis of
response with release of cytokines with vasoactive and dengue encephalitis, but they are not always present
procoagulant properties could account for the occurrence (tables 13). A mild increase in CSF protein has been
of retinal vascular occlusion. The usual 1-week delay in recorded.28 In a series of patients with neurological
appearance of neuro-ophthalmic symptoms after dengue complications of dengue, four of seven with encephalitis
disease onset favours the hypothesis of an immune- had no alterations in CSF.90 Therefore, normal CSF
mediated process. Findings of an autoimmune screen in cellularity should not exclude dengue encephalitis.
a patient with retinal vasculitis and macular detachment The case denitions in panel 2 are designed to be used
showed a low amount of C4 complement, suggesting epidemiologically and clinically and to guide diagnosis
that dengue virus infection could be the antigenic trigger and prognosis. Although we propose criteria for a
for immune complex deposition and vasculitis.135 classication scheme, a topic as challenging and as
controversial as dengue encephalitis needs to be addressed
Diagnosis in a standard way. Prospective studies are needed to assess
Clinical suspicion is essential for diagnosis of dengue the specicity and sensitivity of the proposed case
because many symptoms are non-specic. Various denitions and to generate supporting evidence. Cases
methods are available for laboratory conrmation. fullling neither the denition for encephalitis nor that
During the rst days of infection, dengue virus is present for encephalopathyeg, without CSF testing or when
in blood; thus, at that time, detection of NS1 antigen or categories are overlappingcan be categorised as other or
RNA by RT-PCR and viral culture are appropriate non-specied dengue CNS involvement.
diagnostic methods.1 Dengue virus-specic IgM Neuroimaging might provide additional clues in the
antibodies are present in serum samples 310 days after diagnosis of neurological complications of dengue. In
disease onset.1 IgM capture (MAC)-ELISA is the most dengue encephalitis, brain MRI can be normal or show
widely used serological test. Antibodies against other focal parenchymal abnormalities.22,41 Nevertheless, no
aviviruses (eg, Japanese encephalitis, West Nile virus, specic MRI ndings suggestive of dengue encephalitis
yellow fever) might cross-react with dengue virus, leading have been reported. Neuroimaging features of patients
to false-positive reactions.136 with dengue are diverse, with cerebral oedema the most
In endemic countries, or among travellers who recently commonly reported nding.77 Meningeal enhancement on
(<14 days) returned from such regions, dengue should be post-contrast MRI has been reported occasionally as well.77
ruled out in patients with fever and neurological features Finally, EEG abnormalities can be seen in dengue
(panel 2). If possible, lumbar puncture should be done and patients with neurological complications. In a study of
CSF analysed for abnormalities and for dengue virus- 23 patients with dengue virus infection and neurological
specic antibodies, NS1 antigen, or dengue virus RNA, symptoms, EEG abnormalities were recorded in
depending on available laboratory facilities. Dierential 12 people.139 Slowing on EEG can be seen, but this nding
diagnosis in patients with febrile encephalopathy includes is unspecic and could be attributable to seizures,
malaria, tuberculosis, leptospirosis, rickettsial infection, intracranial haemorrhage, and viral infection per se,
and other bacterial or viral diseases (caused by, for example, besides encephalopathy.77
Japanese encephalitis, West Nile virus, or herpes simplex
virus [HSV]), depending on the local epidemiology. In a Management
prospective hospital-based study in Vietnam, most children Currently, no eective antiviral agents are available to
with acute encephalitis of presumed viral origin were treat symptomatic dengue virus infection.140 Therefore,
infected with Japanese encephalitis (26%), followed by management remains supportive. In mild cases,
enteroviruses (9%) and dengue virus (5%).30 In adults and antipyretic drugs and oral uids could be useful.
adolescents in Brazil, dengue was the leading cause of viral Acetyl-salicylic derivatives and other non-steroidal
encephalitis (47%), followed by infections with HSV-1.31 anti-inammatory drugs should be avoided. Management
www.thelancet.com/neurology Vol 12 September 2013 915
Review
of haemorrhagic complications should be initially intravenous methylprednisolone for several days.50,69,72
conservative. Precise management of intravenous uids However, up to now, no randomised controlled trial has
is needed, and blood or platelet transfusion is only been undertaken to show the ecacy of this approach in
necessary when severe bleeding takes place.1 patients with dengue myelitis or acute dissemin-
In patients with severe dengue and signs of plasma ated encephalomyelitis. High doses of intravenous
leakage, prompt uid resuscitation is imperative, with immunoglobulin might be useful to treat post-dengue
close monitoring of packed-cell volume to avoid uid Guillain-Barr syndrome. Supportive treatment
overload. Isotonic crystalloid solutions should be used, including hydration and analgesic drugsis used for
with isotonic colloid solutions reserved for patients myalgia and transitory muscle dysfunction. The
presenting with profound shock or those who do not eectiveness of corticosteroids in dengue myositis
have a response to initial crystalloid treatment.140,141 In a remains to be proven.
randomised controlled trial from Vietnam,142 use of oral No treatment has been approved for neuro-ophthalmic
prednisolone during the early acute phase of dengue manifestations of dengue. Steroids have been admin-
infection was not associated with a reduction in the istered previously because of possible underlying
development of shock or other recognised complications immune mechanisms, although up to now no random-
of dengue virus infection. ised trials have been done. Topical steroids have been
For supportive management of patients with neuro- used to treat anterior uveitis, whereas pulsed intravenous
logical manifestations, possible underlying causes such as methylprednisolone or systemic oral steroids might be
intracranial bleeding, liver failure, hyponatraemia, indicated for extensive retinal vasculitis.120
hypokalaemia, or metabolic acidosis should be ruled out Currently, no vaccine is available for protection against
andif possiblecorrected. Management of dengue dengue. However, several vaccine candidates are in
encephalitis remains supportive and should include development.144,145
adequate hydration, nutrition, monitoring of con-
sciousness, and maintenance of airways.143 Symptomatic Conclusions and future research
seizures should be treated with non-hepatotoxic Dengue should be included in the dierential diagnosis
anticonvulsants. Decompressive craniotomy and cerebral of acute febrile disease with neurological manifestations
haematoma evacuation were done in two patients with in dengue-endemic countries and in patients with a
dengue after correction of prothrombin time and platelet recent travel history to an endemic region. Many
count.92 Nevertheless, prognosis is not good and, in one neurological manifestations of dengue have been
case series, two of ve patients died.92 At this moment, recorded, rangingwith substantial overlapfrom
haematoma surgery cannot be proposed as a routine encephalitis and encephalopathy to immune-mediated
treatment for dengue virus intracranial bleeding. syndromes and muscle involvement. Recent evidence
Some clinicians recommend treatment of immune- suggests that dengue virus has neuroinvasive capacity. In
mediated dengue CNS involvement with pulses of several studies in endemic areas, a large proportion of
viral encephalitis was caused by dengue virus.2632
However, even though CNS involvement is included now
Search strategy and selection criteria as a criterion for severe dengue in the 2009 WHO case
We searched Pubmed and Scopus for reports published between January, 1960, and June, classication,1 no standardised case denitions or
2013, with the terms (dengue) AND (neurolog* or encephal* or stroke or diagnostic criteria for dengue encephalitis or enceph-
myositis or ophthalmic complications or ocular or unusual manifestations). alopathy have been agreed, which leads to inconsistent
We did not include mental disorders after dengue virus infection in our search. We only use of these terms in published work.
considered original studies published in peer-reviewed journals in English, Spanish, An updated WHO dengue guideline should include a
Portuguese, German, or French. To verify our strategy, we hand-searched the reference case denition for dengue encephalitis and enceph-
lists of the 20 most cited primary articles on neurological manifestations in dengue alopathy, to guide clinicians and clinical epidemiological
patients and added relevant citations to our database. Next, we screened all titles and researchers into this topic. A case classicationsuch as
abstracts identied by the search and included those on dengue patients presenting with the one proposed in panel 2could serve as a starting
neuromuscular or immune-mediated complications; encephalitis, encephalopathy, or point, which could be reviewed by WHO, agreed by
stroke; or neuro-ophthalmic complications. We excluded irrelevant articles or reviews. consensus and best available current evidence, and rened
We then reviewed the full text of all included articles and abstracted relevant data. We as additional data become available from prospective
presented articles in summary tables if they fullled the following criteria: (1) contained studies. For this reason, assessment of CSF in patients
information on laboratory conrmation of dengue; (2) put dengue patients with with suspected neurological manifestations of dengue
neurological complications into context with either all dengue cases or all encephalitis should be standardised. Very few published reports
cases presenting in a clinic; and (3) presented results of CSF testing (cells, dengue-specic present ndings of CSF testing for dengue virus, dengue
antibodies, viral RNA) in a large proportion of dengue patients with suspected CNS virus-specic IgM antibodies, or NS1 antigen combined
involvement. Furthermore, articles presenting autopsy studies on fatal dengue cases with with CSF cellularity and conrmation of dengue in serum
neurological manifestations were abstracted and summarised in a table. samples in a consistent way. Further epidemiological and
neuropathological studies are needed to ascertain the true
916 www.thelancet.com/neurology Vol 12 September 2013
Review
incidence and burden of neurological complications of 20 Guzman MG, Kouri G, Valdes L, et al. Epidemiologic studies on
dengue, to elucidate the underlying pathophysiology, and Dengue in Santiago de Cuba, 1997. Am J Epidemiol 2000;
152: 79399.
to assess the sensitivity and specicity of diagnostic 21 Halstead SB. Pathogenesis of dengue: challenges to molecular
markers for dengue encephalitis. biology. Science 1988; 239: 47681.
Contributors 22 Cam BV, Fonsmark L, Hue NB, Phuong NT, Poulsen A,
Heegaard ED. Prospective case-control study of encephalopathy in
All authors contributed equally to writing of this Review, to preparation
children with dengue hemorrhagic fever. Am J Trop Med Hyg 2001;
of the tables and gures, and to the literature search. 65: 84851.
Conicts of interest 23 Pancharoen C, Thisyakorn U. Neurological manifestations in
We declare that we have no conicts of interest. dengue patients. Southeast Asian J Trop Med Public Health 2001;
32: 34145.
Acknowledgments 24 Thisyakorn U, Thisyakorn C. Dengue infection with unusual
JG receives research funds from the Agncia de Gesti dAjuts manifestations. J Med Assoc Thai 1994; 77: 41013.
Universitaris i de Recerca (AGAUR; grant 2009SGR385); JF receives 25 Thisyakorn U, Thisyakorn C, Limpitikul W, Nisalak A. Dengue
research funds from the Wellcome Trust UK, Li Ka Shing Foundation, infection with central nervous system manifestations.
Medical Research Council UK, Bill & Melinda Gates Foundation, and Southeast Asian J Trop Med Public Health 1999; 30: 50406.
Singapore Ministry of Health. No sponsorship was received to write this 26 Chokephaibulkit K, Kankirawatana P, Apintanapong S, et al. Viral
Review. etiologies of encephalitis in Thai children. Pediatr Infect Dis J 2001;
References 20: 21618.
1 WHO. Dengue guidelines for diagnosis, treatment, prevention and 27 Garca-Rivera EJ, Vorndam V, Rigau-Perez JG. Use of an enhanced
control. Geneva: World Health Organization, 2009. surveillance system for encephalitis and aseptic meningitis for the
2 Bhatt S, Gething PW, Brady OJ, et al. The global distribution and detection of neurologic manifestations of dengue in Puerto Rico,
burden of dengue. Nature 2013; 496: 50407. 2003. P R Health Sci J 2009; 28: 11420.
3 Guzmn MG, Kouri G. Dengue: an update. Lancet Infect Dis 2002; 28 Kankirawatana P, Chokephaibulkit K, Puthavathana P, Yoksan S,
2: 3342. Apintanapong S, Pongthapisit V. Dengue infection presenting with
central nervous system manifestation. J Child Neurol 2000;
4 Nimmannitya S, Thisyakorn U, Hemsrichart V. Dengue 15: 54447.
haemorrhagic fever with unusual manifestations.
Southeast Asian J Trop Med Public Health 1987; 18: 398406. 29 Kumar R, Tripathi S, Tambe JJ, Arora V, Srivastava A, Nag VL.
Dengue encephalopathy in children in Northern India: clinical
5 Kho LK, Sumarmo, Wulur H, Jahja EC, Gubler DJ. Dengue features and comparison with non dengue. J Neurol Sci 2008;
hemorrhagic fever accompanied by encephalopathy in Jakarta. 269: 4148.
Southeast Asian J Trop Med Public Health 1981; 12: 8386.
30 Le VT, Phan TQ, Do QH, et al. Viral etiology of encephalitis in
6 Hendarto SK, Hadinegoro SR. Dengue encephalopathy. children in southern Vietnam: results of a one-year prospective
Acta Paediatr Jpn 1992; 34: 35057. descriptive study. PLoS Negl Trop Dis 2010; 4: e854.
7 Lum LC, Lam SK, Choy YS, George R, Harun F. Dengue 31 Soares CN, Cabral-Castro MJ, Peralta JM, de Freitas MR, Zalis M,
encephalitis: a true entity? Am J Trop Med Hyg 1996; 54: 25659. Puccioni-Sohler M. Review of the etiologies of viral meningitis and
8 Solomon T, Dung NM, Vaughn DW, et al. Neurological encephalitis in a dengue endemic region. J Neurol Sci 2011;
manifestations of dengue infection. Lancet 2000; 355: 105359. 303: 7579.
9 Domingues RB, Kuster GW, Onuki-Castro FL, Souza VA, Levi JE, 32 Srey VH, Sadones H, Ong S, et al. Etiology of encephalitis
Pannuti CS. Involvement of the central nervous system in patients syndrome among hospitalized children and adults in Takeo,
with dengue virus infection. J Neurol Sci 2008; 267: 3640. Cambodia, 19992000. Am J Trop Med Hyg 2002; 66: 20007.
10 Rico-Hesse R. Dengue virus evolution and virulence models. 33 Arajo FM, Araujo MS, Nogueira RM, et al. Central nervous system
Clin Infect Dis 2007; 44: 146266. involvement in dengue: a study in fatal cases from a dengue
11 Wearing HJ, Rohani P. Ecological and immunological endemic area. Neurology 2012; 78: 73642.
determinants of dengue epidemics. Proc Natl Acad Sci USA 2006; 34 Bhoopat L, Bhamarapravati N, Attasiri C, et al.
103: 1180207. Immunohistochemical characterization of a new monoclonal
12 Wichmann O, Yoon IK, Vong S, et al. Dengue in Thailand and antibody reactive with dengue virus-infected cells in frozen tissue
Cambodia: an assessment of the degree of underrecognized disease using immunoperoxidase technique. Asian Pac J Allergy Immunol
burden based on reported cases. PLoS Negl Trop Dis 2011; 5: e996. 1996; 14: 10713.
13 Baaten GG, Sonder GJ, Zaaijer HL, van Gool T, Kint JA, 35 Chimelli L, Hahn MD, Netto MB, Ramos RG, Dias M, Gray F.
van den Hoek A. Travel-related dengue virus infection, the Dengue: neuropathological ndings in 5 fatal cases from Brazil.
Netherlands, 20062007. Emerg Infect Dis 2011; 17: 82128. Clin Neuropathol 1990; 9: 15762.
14 Endy TP, Chunsuttiwat S, Nisalak A, et al. Epidemiology of 36 Miagostovich MP, Ramos RG, Nicol AF, et al. Retrospective study
inapparent and symptomatic acute dengue virus infection: a on dengue fatal cases. Clin Neuropathol 1997; 16: 20408.
prospective study of primary school children in Kamphaeng Phet, 37 Nogueira RM, Filippis AM, Coelho JM, et al. Dengue virus infection
Thailand. Am J Epidemiol 2002; 156: 4051. of the central nervous system (CNS): a case report from Brazil.
15 WHO. Dengue haemorrhagic fever: diagnosis, treatment, Southeast Asian J Trop Med Public Health 2002; 33: 6871.
prevention, control, 2nd edn. Geneva: World Health Organization, 38 Nogueira RM, Schatzmayr HG, de Filippis AM, et al. Dengue virus
1997. type 3, Brazil, 2002. Emerg Infect Dis 2005; 11: 137681.
16 Balmaseda A, Hammond SN, Perez MA, et al. Short report: 39 Ramos C, Sanchez G, Pando RH, et al. Dengue virus in the brain of a
assessment of the World Health Organization scheme for fatal case of hemorrhagic dengue fever. J Neurovirol 1998; 4: 46568.
classication of dengue severity in Nicaragua. Am J Trop Med Hyg 40 Janssen HL, Bienfait HP, Jansen CL, et al. Fatal cerebral oedema
2005; 73: 105962. associated with primary dengue infection. J Infect 1998; 36: 34446.
17 Narvaez F, Gutierrez G, Perez MA, et al. Evaluation of the 41 Misra UK, Kalita J, Syam UK, Dhole TN. Neurological
traditional and revised WHO classications of dengue disease manifestations of dengue virus infection. J Neurol Sci 2006;
severity. PLoS Negl Trop Dis 2011; 5: e1397. 244: 11722.
18 Alexander N, Balmaseda A, Coelho IC, et al. Multicentre prospective 42 Kalayanarooj S, Nimmannitya S. Clinical presentations of dengue
study on dengue classication in four South-east Asian and three hemorrhagic fever in infants compared to children.
Latin American countries. Trop Med Int Health 2011; 16: 93648. J Med Assoc Thai 2003; 86 (suppl 3): S67380.
19 Sangkawibha N, Rojanasuphot S, Ahandrik S, et al. Risk factors in 43 Kalayanarooj S, Nimmannitya S. Is dengue severity related to
dengue shock syndrome: a prospective epidemiologic study in nutritional status? Southeast Asian J Trop Med Public Health 2005;
Rayong, ThailandI, the 1980 outbreak. Am J Epidemiol 1984; 36: 37884.
120: 65369.
www.thelancet.com/neurology Vol 12 September 2013 917
Review
44 Malavige GN, Ranatunga PK, Jayaratne SD, Wijesiriwardana B, 70 Palma-da Cunha-Matta A, Soares-Moreno SA,
Seneviratne SL, Karunatilaka DH. Dengue viral infections as a Cardoso-de Almeida A, Aquilera-de Freitas V, Carod-Artal FJ.
cause of encephalopathy. Indian J Med Microbiol 2007; 25: 14345. Neurological complications arising from dengue virus infection.
45 Hommel D, Talarmin A, Deubel V, et al. Dengue encephalitis in Rev Neurol 2004; 39: 23337 (in Spanish).
French Guiana. Res Virol 1998; 149: 23538. 71 Sundaram C, Uppin SG, Dakshinamurthy KV, Borgahain R. Acute
46 Hapuarachchi HC, Oh HML, Thein TL, et al. Clinico-genetic disseminated encephalomyelitis following dengue hemorrhagic
characterisation of an encephalitic dengue virus 4 associated with fever. Neurol India 2010; 58: 599601.
multi-organ involvement. J Clin Virol 2013; 57: 9194. 72 Gera C, George U. Acute disseminating encephalomyelitis with
47 Rao S, Kumar M, Ghosh S, Gadpayle AK. A rare case of dengue hemorrhage following dengue. Neurol India 2010; 58: 59596.
encephalitis. BMJ Case Rep 2013; published online Feb 13. 73 Gala HC, Avasthi BS, Lokeshwar MR. Dengue shock syndrome with
DOI:10.1136/bcr-2012-008229. two atypical complications. Indian J Pediatr 2012; 79: 38688.
48 Araujo F, Nogueira R, Araujo Mde S, et al. Dengue in patients with 74 Verma R, Sharma P, Garg RK, Atam V, Singh MK, Mehrotra HS.
central nervous system manifestations, Brazil. Emerg Infect Dis Neurological complications of dengue fever: experience from a tertiary
2012; 18: 67779. center of north India. Ann Indian Acad Neurol 2011; 14: 27278.
49 Verma R, Varatharaj A. Epilepsia partialis continua as a 75 Ferreira ML, Cavalcanti CG, Coelho CA, Mesquita SD. Neurological
manifestation of dengue encephalitis. Epilepsy Behav 2011; manifestations of dengue: study of 41 cases. Arq Neuropsiquiatr
20: 39597. 2005; 63: 48893 (in Portuguese).
50 Miranda de Sousa A, Puccioni-Sohler M, Dias Borges A, 76 Koshy JM, Joseph DM, John M, et al. Spectrum of neurological
Fernandes Adorno L, Papais Alvarenga M, Papais Alvarenga RM. manifestations in dengue virus infection in Northwest India.
Post-dengue neuromyelitis optica: case report of a Japanese- Trop Doct 2012, 42: 19194.
descendent Brazilian child. J Infect Chemother 2006; 12: 39698. 77 Wasay M, Channa R, Jumani M, Shabbir G, Azeemuddin M,
51 Gaultier C, Angibaud G, Laille M, Lacassin F. Probable Miller Zafar A. Encephalitis and myelitis associated with dengue viral
Fisher syndrome during dengue fever type 2. Rev Neurol (Paris) infection clinical and neuroimaging features. Clin Neurol Neurosurg
2000; 156: 16971 (in French). 2008; 110: 63540.
52 Chien J, Ong A, Low SY. An unusual complication of dengue 78 Oehler E, Le Hena O, Larre P, Ghawche F. Guillain-Barr
infection. Singapore Med J 2008; 49: e34042. syndrome following type 4 dengue in Polynesia. Med Trop (Mars)
53 Ansari MK, Jha S, Nath A. Unilateral diaphragmatic paralysis 2011; 71: 20304 (in French).
following dengue infection. Neurol India 2010; 58: 59698. 79 Goncalves E. Acute inammatory demyelinating
54 Ratnayake EC, Shivanthan C, Wijesiriwardena BC. Diaphragmatic polyradiculoneuropathy (Guillain-Barre syndrome) following
paralysis: a rare consequence of dengue fever. BMC Infect Dis 2012; dengue fever. Rev Inst Med Trop Sao Paulo 2011; 53: 22325.
12: 46. 80 Jackson ST, Mullings A, Bennett F, Khan C, Gordon-Strachan G,
55 Chappuis F, Justafre JC, Duchunstang L, Loutan L, Taylor WR. Rhoden T. Dengue infection in patients presenting with
Dengue fever and long thoracic nerve palsy in a traveler returning neurological manifestations in a dengue endemic population.
from Thailand. J Travel Med 2004; 11: 11214. West Indian Med J 2008; 57: 37376.
56 Peter S, Malhotra N, Peter P, Sood R. Isolated Bells palsy: 81 Chen TY, Lee CT. Guillain-Barre syndrome following dengue fever.
an unusual presentation of dengue infection. Asian Pac J Trop Med Ann Emerg Med 2007; 50: 9495.
2013; 6: 8284. 82 Santos NQ, Azoubel AC, Lopes AA, Costa G, Bacellar A.
57 Shivanthan MC, Ratnayake EC, Wijesiriwardena BC, Guillain-Barre syndrome in the course of dengue: case report.
Somaratna KC, Gamagedara LK. Paralytic squint due to abducens Arq Neuropsiquiatr 2004; 62: 14446.
nerve palsy: a rare consequence of dengue fever. BMC Infect Dis 83 Esack A, Teelucksingh S, Singh N. The Guillain-Barre syndrome
2012; 12: 156. following dengue fever. West Indian Med J 1999; 48: 3637.
58 Donnio A, Bral L, Olindo S, Cabie A, Merle H. Dengue, a new 84 Soares CN, Cabral-Castro M, Oliveira C, et al. Oligosymptomatic
etiology in oculomotor paralysis. Can J Ophthalmol 2010; 45: 18384 dengue infection: a potential cause of Guillain Barre syndrome.
(in French). Arq Neuropsiquiatr 2008; 66: 23437.
59 Kumar S, Prabhakar S. Guillain-Barre syndrome occurring in the 85 Chaudhary SC, Mohanty D, Sonkar SK, Gupta DK, Gupta A.
course of dengue fever. Neurol India 2005; 53: 25051. Unusual manifestation of dengue fever. BMJ Case Rep 2011;
60 Sulekha C, Kumar S, Philip J. Guillain-Barre syndrome following published online June 29. DOI:10.1136/bcr.02.2011.3839.
dengue fever. Indian Pediatr 2004; 41: 94850. 86 Hira HS, Kaur A, Shukla A. Acute neuromuscular weakness
61 Seet RC, Lim EC, Wilder-Smith EP. Acute transverse myelitis associated with dengue infection. J Neurosci Rural Pract 2012; 3: 3639.
following dengue virus infection. J Clin Virol 2006; 35: 31012. 87 Medina-Gonzlez R, Chvez-Garca R, Chiquete E,
62 Chanthamat N, Sathirapanya P. Acute transverse myelitis associated Paredes-Casillas P, Navarro-Bonnet J, Ruiz-Sandoval J. Sndrome
with dengue viral infection. J Spinal Cord Med 2010; 33: 42527. de Guillain-Barr asociado a dengue: reporte de caso.
63 Leao RN, Oikawa T, Rosa ES, et al. Isolation of dengue 2 virus from Rev Mex Neurocienc 2011; 12: 13440.
a patient with central nervous system involvement (transverse 88 Orsini M, De Freitas M, Nascimento O, et al. Sndrome de
myelitis). Rev Soc Bras Med Trop 2002; 35: 40104. Guillain-Barr ps-infeco por dengue: relato de caso.
64 Kunishige M, Mitsui T, Tan BH, et al. Preferential gray matter Rev Neurocienc 2010; 18: 2427.
involvement in dengue myelitis. Neurology 2004; 63: 198081. 89 Sharma CM, Kumawat BL, Ralot T, Tripathi G, Dixit S.
65 Puccioni-Sohler M, Soares CN, Papaiz-Alvarenga R, Castro MJ, Guillain-Barre syndrome occurring during dengue fever.
Faria LC, Peralta JM. Neurologic dengue manifestations associated J Indian Med Assoc 2011; 109: 675.
with intrathecal specic immune response. Neurology 2009; 90 Soares CN, Faria LC, Peralta JM, de Freitas MR, Puccioni-Sohler M.
73: 141317. Dengue infection: neurological manifestations and cerebrospinal
66 Larik A, Chiong Y, Lee LC, Ng YS. Longitudinally extensive uid (CSF) analysis. J Neurol Sci 2006; 249: 1924.
transverse myelitis associated with dengue fever. BMJ Case Rep 91 Qureshi NK, Begum A, Saha PR, Hossain MI. Guillain-Barre
2012; published online May 12. DOI:10.1136/bcr.12.2011.5378. syndrome following dengue fever in adult patient.
67 Brito CA, Sobreira S, Cordeiro MT, Lucena-Silva N. Acute J Med (Bangladesh) 2012, 13: 24649.
disseminated encephalomyelitis in classic dengue. 92 Kumar R, Prakash O, Sharma BS. Intracranial hemorrhage in
Rev Soc Bras Med Trop 2007; 40: 23638. dengue fever: management and outcomea series of 5 cases and
68 Chowdhury RN, Siddiqui M, Mahbub M, et al. Dengue fever as a review of literature. Surg Neurol 2009; 72: 42933.
cause of acute disseminated encephalomyelitis (ADEM). J Med 2011; 93 Mathew S, Pandian JD. Stroke in patients with dengue.
12: 18587. J Stroke Cerebrovasc Dis 2010; 19: 25356.
69 Yamamoto Y, Takasaki T, Yamada K, et al. Acute disseminated 94 de Souza LJ, Martins AL, Paravidini PC, et al. Hemorrhagic
encephalomyelitis following dengue fever. J Infect Chemother 2002; encephalopathy in dengue shock syndrome: a case report.
8: 17577. Braz J Infect Dis 2005; 9: 25761.
918 www.thelancet.com/neurology Vol 12 September 2013
Review
95 Kumar R, Prakash O, Sharma BS. Dengue hemorrhagic fever: a 121 Kapoor HK, Bhai S, John M, Xavier J. Ocular manifestations of
rare presentation as atypical acute subdural hematoma. dengue fever in an East Indian epidemic. Can J Ophthalmol 2006;
Pediatr Neurosurg 2008; 44: 49092. 41: 74146.
96 Dey AB, Chaudhury D, Mohapatra AK, Nagarkar KM, Malhotra OP. 122 Bacsal KE, Chee SP, Cheng CL, Flores JV. Dengue-associated
Fever, mucocutaneous haemorrhage, and severe headache during maculopathy. Arch Ophthalmol 2007; 125: 50110.
an epidemic of haemorrhagic fever. Postgrad Med J 1998; 74: 43335. 123 Haritoglou C, Dotse SD, Rudolph G, Stephan CM, Thurau SR,
97 Jain N, Gutch M, Kumar V, Naik AK. A fatal combo of dengue Klauss V. A tourist with dengue fever and visual loss. Lancet 2002;
shock syndrome with acute subdural hematoma. Neurol India 2012; 360: 1070.
60: 10506. 124 Teoh SC, Chee CK, Laude A, et al. Optical coherence tomography
98 Kumar V, Kataria R, Mehta VS. Dengue hemorrhagic fever: a rare patterns as predictors of visual outcome in dengue-related
cause of pituitary tumor hemorrhage and reversible vision loss. maculopathy. Retina 2010; 30: 39098.
Indian J Ophthalmol 2011; 59: 31112. 125 Sanjay S, Wagle AM, Au Eong KG. Optic neuropathy associated
99 Patey O, Ollivaud L, Breuil J, Lafaix C. Unusual neurologic with dengue fever. Eye 2008; 22: 72224.
manifestations occurring during dengue fever infection. 126 Arago RE, Barreira IM, Lima LN, Rabelo LP, Pereira FB. Bilateral
Am J Trop Med Hyg 1993; 48: 793802. optic neuritis after dengue viral infection: case report.
100 Jensenius M, Berild D, Ormaasen V, Maehlen J, Lindegren G, Arq Bras Oftalmol 2010; 73: 17578 (in Portuguese).
Falk KI. Fatal subarachnoidal haemorrhage in a Norwegian traveller 127 Sanjay S, Au Eong KG. Bilateral vitreous haemorrhage associated
with dengue virus infection. Scand J Infect Dis 2007; 39: 27274. with dengue fever. Eye 2007; 21: 14445.
101 Liou LM, Lan SH, Lai CL. Dengue fever with ischemic stroke: a case 128 Siqueira RC, Vitral NP, Campos WR, Orece F,
report. Neurologist 2008; 14: 4042. de Moraes Figueiredo LT. Ocular manifestations in dengue fever.
102 Seet RC, Lim EC. Dysarthria-clumsy hand syndrome associated Ocul Immunol Inamm 2004; 12: 32327.
with dengue type-2 infection. J Neurol 2007; 254: 112930. 129 Basu A, Chaturvedi UC. Vascular endothelium: the battleeld of
103 Said S, Elsaeed K, Alyan Z. Benign acute myositis in association dengue viruses. FEMS Immunol Med Microbiol 2008; 53: 28799.
with acute dengue viruses infections. 130 Salgado DM, Eltit JM, Manseld K, et al. Heart and skeletal muscle are
Egypt J Neurol Psychiatry Neurosurg 2008; 45: 193200. targets of dengue virus infection. Pediatr Infect Dis J 2010; 29: 23842.
104 Misra UK, Kalita J, Maurya PK, Kumar P, Shankar SK, 131 An J, Zhou DS, Kawasaki K, Yasui K. The pathogenesis of spinal
Mahadevan A. Dengue-associated transient muscle dysfunction: cord involvement in dengue virus infection. Virchows Arch 2003;
clinical, electromyography and histopathological changes. Infection 442: 47281.
2012; 40: 12530. 132 Bordignon J, Strottmann DM, Mosimann AL, et al. Dengue
105 Rajajee S, Ezhilarasi S, Rajarajan K. Benign acute childhood neurovirulence in mice: identication of molecular signatures in
myositis. Indian J Pediatr 2005; 72: 399400. the E and NS3 helicase domains. J Med Virol 2007; 79: 150617.
106 Lim M, Goh HK. Rhabdomyolysis following dengue virus infection. 133 Sips GJ, Wilschut J, Smit JM. Neuroinvasive avivirus infections.
Singapore Med J 2005; 46: 64546. Rev Med Virol 2012; 22: 6987.
107 Davis JS, Bourke P. Rhabdomyolysis associated with dengue virus 134 Oishi K, Saito M, Mapua CA, Natividad FF. Dengue illness: clinical
infection. Clin Infect Dis 2004; 38: e10911. features and pathogenesis. J Infect Chemother 2007; 13: 12533.
108 Paliwal VK, Garg RK, Juyal R, et al. Acute dengue virus myositis: 135 Chang PE, Cheng CL, Asok K, Fong KY, Chee SP, Tan CK. Visual
a report of seven patients of varying clinical severity including two disturbances in dengue fever: an answer at last? Singapore Med J
cases with severe fulminant myositis. J Neurol Sci 2011; 300: 1418. 2007; 48: e7173.
109 Ahmad R, Abdul Lati AK, Abdul Razak S. Myalgia cruris 136 Nunes MR, Nunes Neto JP, Casseb SM, et al. Evaluation of an
epidemica: an unusual presentation of dengue fever. immunoglobulin M-specic capture enzyme-linked
Southeast Asian J Trop Med Public Health 2007; 38: 108487. immunosorbent assay for rapid diagnosis of dengue infection.
110 Acharya S, Shukla S, Mahajan SN, Diwan SK. Acute dengue J Virol Methods 2011; 171: 1320.
myositis with rhabdomyolysis and acute renal failure. 137 Varatharaj A. Encephalitis in the clinical spectrum of dengue
Ann Indian Acad Neurol 2010; 13: 22122. infection. Neurol India 2010; 58: 58591.
111 Kalita J, Misra UK, Mahadevan A, Shankar SK. Acute pure motor 138 Kao CL, King CC, Chao DY, Wu HL, Chang GJ. Laboratory
quadriplegia: is it dengue myositis? Electromyogr Clin Neurophysiol diagnosis of dengue virus infection: current and future perspectives
2005; 45: 35761. in clinical diagnosis and public health. J Microbiol Immunol Infect
112 Sangle SA, Dasgupta A, Ratnalikar SD, Kulkarni RV. Dengue 2005; 38: 516.
myositis and myocarditis. Neurol India 2010; 58: 59899. 139 Kalita J, Misra UK. EEG in dengue virus infection with neurological
113 Malheiros SM, Oliveira AS, Schmidt B, Lima JG, Gabbai AA. manifestations: a clinical and CT/MRI correlation. Clin Neurophysiol
Dengue: muscle biopsy ndings in 15 patients. Arq Neuropsiquiatr 2006; 117: 225256.
1993; 51: 15964. 140 Simmons CP, Farrar JJ, van Vinh Chau N, Wills B. Dengue.
114 Finsterer J, Kongchan K. Severe, persisting, steroid-responsive N Engl J Med 2012; 366: 142332.
dengue myositis. J Clin Virol 2006; 35: 42628. 141 Wills BA, Nguyen MD, Ha TL, et al. Comparison of three uid
115 Beauvais P, Quinet B, Richardet JM. Dengue: apropos of 2 cases. solutions for resuscitation in dengue shock syndrome. N Engl J Med
Arch Fr Pediatr 1993; 50: 90507 (in French). 2005; 353: 87789.
116 Pimentel LH, de Oliveira GR, do Vale OC, Gondim Fde A. On the 142 Tam DT, Ngoc TV, Tien NT, et al. Eects of short-course oral
spectrum of acute dengue virus myositis. J Neurol Sci 2011; corticosteroid therapy in early dengue infection in Vietnamese
307: 17879. patients: a randomized, placebo-controlled trial. Clin Infect Dis 2012;
117 Kalita J, Misra UK, Maurya PK, Shankar SK, Mahadevan A. 55: 121624.
Quantitative electromyography in dengue-associated muscle 143 Ghosh M, Banerjee M, Das S, Chakraborty S. Dengue infection
dysfunction. J Clin Neurophysiol 2012; 29: 46871. with multi-organ involvement. Scand J Infect Dis 2011; 43: 31618.
118 Gupta A, Srinivasan R, Setia S, Soundravally R, Pandian DG. 144 Durbin AP, Whitehead SS. Next-generation dengue vaccines: novel
Uveitis following dengue fever. Eye 2009; 23: 87376. strategies currently under development. Viruses 2011; 3: 180014.
119 Lim WK, Mathur R, Koh A, Yeoh R, Chee SP. Ocular manifestations 145 Sabchareon A, Wallace D, Sirivichayakul C, et al. Protective ecacy
of dengue fever. Ophthalmology 2004; 111: 205764. of the recombinant, live-attenuated, CYD tetravalent dengue vaccine
120 Su DH, Bacsal K, Chee SP, et al. Prevalence of dengue maculopathy in Thai schoolchildren: a randomised, controlled phase 2b trial.
in patients hospitalized for dengue fever. Ophthalmology 2007; Lancet 2012; 380: 155967.
114: 174347.
www.thelancet.com/neurology Vol 12 September 2013 919
Anda mungkin juga menyukai
- Oral Biologic Defenses in Tooth Demineralization and RemineralizationDokumen14 halamanOral Biologic Defenses in Tooth Demineralization and RemineralizationWilson Fransiskus Chia GirsangBelum ada peringkat
- Life Cycle and Morphology of Steinina Ctenocephali (Ross 1909) Comb. Nov. (Eugregarinorida: Actinocephalidae), A Gregarine ofDokumen10 halamanLife Cycle and Morphology of Steinina Ctenocephali (Ross 1909) Comb. Nov. (Eugregarinorida: Actinocephalidae), A Gregarine ofWilson Fransiskus Chia GirsangBelum ada peringkat
- Central Nervous System Involvement in Dengue - AraujoDokumen9 halamanCentral Nervous System Involvement in Dengue - AraujoWilson Fransiskus Chia GirsangBelum ada peringkat
- Esti2014 P-0058Dokumen69 halamanEsti2014 P-0058sri mulianiBelum ada peringkat
- Immunological Study Antibodies, and With TyphoidDokumen7 halamanImmunological Study Antibodies, and With TyphoidWilson Fransiskus Chia GirsangBelum ada peringkat
- Dengue EnsefalitisDokumen19 halamanDengue EnsefalitisWilson Fransiskus Chia GirsangBelum ada peringkat
- 114 PDFDokumen7 halaman114 PDFWilson Fransiskus Chia GirsangBelum ada peringkat
- Recent Investigations On The Population Dynamics oDokumen6 halamanRecent Investigations On The Population Dynamics oWilson Fransiskus Chia GirsangBelum ada peringkat
- Diagnosis Kriteria Ensefalitis DengueDokumen1 halamanDiagnosis Kriteria Ensefalitis DengueWilson Fransiskus Chia GirsangBelum ada peringkat
- 209 FullDokumen15 halaman209 FullWilson Fransiskus Chia GirsangBelum ada peringkat
- 762320Dokumen17 halaman762320Wilson Fransiskus Chia GirsangBelum ada peringkat
- Supi NationDokumen3 halamanSupi NationWilson Fransiskus Chia GirsangBelum ada peringkat
- Jurnal Radiologi Xray UsgDokumen5 halamanJurnal Radiologi Xray UsgWilson Fransiskus Chia GirsangBelum ada peringkat
- Dengue EnsefalDokumen3 halamanDengue EnsefalWilson Fransiskus Chia GirsangBelum ada peringkat
- Dengue EnsefalitisDokumen19 halamanDengue EnsefalitisWilson Fransiskus Chia GirsangBelum ada peringkat
- 24 CR Dengue EncephalitisDokumen2 halaman24 CR Dengue EncephalitisWilson Fransiskus Chia GirsangBelum ada peringkat
- Jurnal Radiologi Xray UsgDokumen5 halamanJurnal Radiologi Xray UsgWilson Fransiskus Chia GirsangBelum ada peringkat
- Dengue Virus Infection J Neurol Sci. 2006Dokumen6 halamanDengue Virus Infection J Neurol Sci. 2006Wilson Fransiskus Chia GirsangBelum ada peringkat
- Supi NationDokumen3 halamanSupi NationWilson Fransiskus Chia GirsangBelum ada peringkat
- Jurnal Usg EfusiDokumen5 halamanJurnal Usg EfusiWilson Fransiskus Chia GirsangBelum ada peringkat
- Mechanism and EvaluationDokumen8 halamanMechanism and EvaluationWilson Fransiskus Chia GirsangBelum ada peringkat
- Efusi PleuraDokumen6 halamanEfusi PleuraWilson Fransiskus Chia GirsangBelum ada peringkat
- The Complete UrinalysisDokumen34 halamanThe Complete UrinalysisWilson Fransiskus Chia GirsangBelum ada peringkat
- Gambaran Glukosa Urin Pada Pasien Tuberkulosis Paru Dewasa Di Rsup Prof. Dr. R. D. Kandou ManadoDokumen6 halamanGambaran Glukosa Urin Pada Pasien Tuberkulosis Paru Dewasa Di Rsup Prof. Dr. R. D. Kandou ManadoWilson Chia GirsangBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- NEWSLETTERDokumen16 halamanNEWSLETTERMitzi Rica PalimaBelum ada peringkat
- Dengue Case PresentationDokumen26 halamanDengue Case PresentationLyssa Q.Belum ada peringkat
- The Pentagon Bio-Weapons - Dilyana - BGDokumen34 halamanThe Pentagon Bio-Weapons - Dilyana - BGOn The PathBelum ada peringkat
- Pandan Mosquito Coil: A Natural AlternativeDokumen19 halamanPandan Mosquito Coil: A Natural AlternativeJOHN CARLO LORBISBelum ada peringkat
- Seminar: Annelies Wilder-Smith, Eng-Eong Ooi, Olaf Horstick, Bridget WillsDokumen14 halamanSeminar: Annelies Wilder-Smith, Eng-Eong Ooi, Olaf Horstick, Bridget WillsAlexander ArguelloBelum ada peringkat
- DR. NOEL CASUMPANG vs. CORTEJODokumen15 halamanDR. NOEL CASUMPANG vs. CORTEJOAngelica de LeonBelum ada peringkat
- IMCI Guide for Assessing and Classifying Child with FeverDokumen4 halamanIMCI Guide for Assessing and Classifying Child with FeverMariah Jane TaladuaBelum ada peringkat
- Bin TaroDokumen87 halamanBin TaromanfishjackBelum ada peringkat
- Para Jumbles Test-1Dokumen4 halamanPara Jumbles Test-1vennelaBelum ada peringkat
- Priyadarshini, 2010Dokumen9 halamanPriyadarshini, 2010AmandaBelum ada peringkat
- Chikungunya Fever - WHO FactSheetDokumen2 halamanChikungunya Fever - WHO FactSheetDr.SagindarBelum ada peringkat
- DengueDokumen44 halamanDengueAl JihadBelum ada peringkat
- Knowledge, Attitude and Practices For Dengue ControlDokumen26 halamanKnowledge, Attitude and Practices For Dengue ControlCASY31Belum ada peringkat
- DIMENSION OF SYMPTOMS AND PRESENT PERFECT PROGRESSIVE TENSEDokumen13 halamanDIMENSION OF SYMPTOMS AND PRESENT PERFECT PROGRESSIVE TENSERida Dwika IrianiBelum ada peringkat
- Ebph 1Dokumen10 halamanEbph 1eko susiloBelum ada peringkat
- M.O.R.E 1119: Module For Remedial English SPM 1119Dokumen192 halamanM.O.R.E 1119: Module For Remedial English SPM 1119smile2jingBelum ada peringkat
- Pediatrics - Question Bank - RGUHSDokumen51 halamanPediatrics - Question Bank - RGUHSArun Kumar86% (7)
- Tawa-Tawa Contains Active Ingredients That May Help Dengue Hemorrhagic Fever (DHF) Patients - StudyDokumen2 halamanTawa-Tawa Contains Active Ingredients That May Help Dengue Hemorrhagic Fever (DHF) Patients - StudyLouiseBelum ada peringkat
- Science - July 8, 2022 USADokumen144 halamanScience - July 8, 2022 USASimej100% (1)
- Gayuma GroupDokumen43 halamanGayuma GroupLeonil Ian GayumaBelum ada peringkat
- National Center For Disease Prevention and Control De-Partment of HealthDokumen8 halamanNational Center For Disease Prevention and Control De-Partment of HealthMichael Cabrera RabinoBelum ada peringkat
- Cot-Problem and SolutionDokumen47 halamanCot-Problem and SolutionYnan Esteron HernandezBelum ada peringkat
- Patient's Name: Date of Admission: Age: Physician: Religion: Diagnosis: Nationality: Diet: Room and Bed No.Dokumen4 halamanPatient's Name: Date of Admission: Age: Physician: Religion: Diagnosis: Nationality: Diet: Room and Bed No.rammyestellaBelum ada peringkat
- Eng7 Q4 Mod3Dokumen29 halamanEng7 Q4 Mod3bevlesoyBelum ada peringkat
- E.O Anti Dengue CommitteeDokumen3 halamanE.O Anti Dengue CommitteePao Lonzaga100% (1)
- Electromedicine DefinedDokumen70 halamanElectromedicine DefinedMatthias WeisserBelum ada peringkat
- Infectious Diseases (Past Year)Dokumen2 halamanInfectious Diseases (Past Year)Esther HongBelum ada peringkat
- Dengue 2019Dokumen79 halamanDengue 2019Nou ChannarithBelum ada peringkat
- Arthropod Borne Infections - MHA (12 Files Merged)Dokumen377 halamanArthropod Borne Infections - MHA (12 Files Merged)MariaBelum ada peringkat
- Development of Economical Mosquito Repellent Using Marigold PlantDokumen9 halamanDevelopment of Economical Mosquito Repellent Using Marigold PlantSamuel LendioBelum ada peringkat