India Narayana Summary
Diunggah oleh
anuragHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
India Narayana Summary
Diunggah oleh
anuragHak Cipta:
Format Tersedia
Asia India
Healthcare for All: Narayana
Hrudayalaya, Bangalore
Prepared by Prabakar Kothandaraman & Sunita Mookerjee
(India)
Sector: Health
Enterprise Class: Local SME
Summary
In a nation of over one billion, healthcare is yet to be recognized as a fundamental right for
Indias citizens. Large sections of Indian society are unable to meet healthcare costs and are
denied even the most basic of healthcare. Health insurance, especially for the poor, is non-
existent and healthcare quality is sub-standard. Public health expenditures amount to only
0.9% of the GDP, while private healthcare expenditures add up to 4.2%. A doctor with a
mission who believed that a countrys poor needs to become healthy if the nation is to
become wealthy managed to light a fire in the minds of those that wanted to serve the market
for products and services for the lowest sections of the society. Dr. Devi Shetty, FRCS
(London)1 founded Narayana Hrudayalaya (NH), a cardiac hospital on the outskirts of the
southern Indian city of Bangalore in 2001 with a mission that focused fundamentally on
delivering state-of-the-art cardiac care to poor people. NH achieved its mission through a
series of innovations that involved technology, care-giving process, financial instruments and
human resource policies.
Challenges
The incidence of cardiac disease in India is very high. Indians have a particularly higher
genetic risk of heart disease than people of other ethnicities. The Indian sub-continent
accounts for nearly 45% of the worlds rate of coronary heart diseases.
Despite these indicators, only very few can afford the price of a heart operation that could
range from US$1,500 to $6,000 given that close to 34% of the population in India survive
on less than US$1 per day. Therefore, NH focused on solving the problem of making
cardiac care affordable for the poor.
Other challenges include the accessibility and quality of healthcare. In detecting heart
ailments, the first line of diagnosis involving primary healthcare givers is crucial.
However, several of the Indian primary care centers were short on either staff or
equipments or both. Access to diagnostics was extremely limited. Costs of pursuing
secondary diagnostics away from home villages were very expensive. This restricted
quality of healthcare available to the patient as proper operating room (OR) facilities and
qualified medical professionals necessary to deliver quality cardiac care were not
available for the poor. Finally, poor people could not afford to pay top dollar for cardiac
care.
Innovations
The chief innovation behind the NH solution to the poor was what Dr. Shetty termed the
wal-martization of healthcare.2 It was based on the simple premise that, just like retailing
products, retailing healthcare in India can use population as a strength to drive down costs
and establish unimaginable scale.
1
Fellow of the Royal College of Surgery (London)
2
Viswanathan, Vidya (2005), Heart Care for Everyone, Civil Society, Vol. 3, No.3, December.
Case Study Healthcare for All: Narayana Hrudayalaya, Bangalore 2
A combination of empowered satellite rural healthcare centers and state-of-the-art
communication and software technologies were used in multiple ways to improve access.
The remote healthcare centers did the initial screening and counseling, while satellite
communication technology provided access to consultants located several thousand miles
away.
NHs innovation in providing healthcare insurance at US$11 cents per month empowered
its poor patients and enhanced their ability to pay. NH also offered low-cost insurance
schemes, in partnership with government and foundations. Also, NH focused on upstream
innovation for producing technical staff to control its service quality.
Dr. Shetty managed to put together a team of highly motivated surgeons that focused only
on giving care and serving NHs mission. People want to be like Mother Teresa; they
just need to be channeled into the right environment, observed Dr. Shetty.
Positive Outcomes for the Poor
Between 2001 and May 2007, NH performed over 23,000 surgeries and 34,000
catheterization procedures. The hospital subsidized poor patients to the tune of US$2.5
million that benefited close to half of all the patients that came to NH for treatment
because they could not afford to pay their full cost.
The hospitals focus on children was highlighted by the fact that over 40% of its cases
were in the pediatric category and that enabled it to claim to be the largest cardiac care
facility for children in the world.
Challenges for the Future & Replication
Dr. Shetty was worried about the availability of qualified people to expand the facilities
beyond his current health city project that, when completed in 2008, would have 5,000 beds
serving specialties such as orthopedics, oncology, and eye care along with the core cardiac
care. The success of the health insurance scheme that NH developed for the poor had
prompted several other state governments that want to replicate it in their states. Some of
them also want NH to build cardiac hospitals in their states, as well. The telemedicine
coverage was expanding further, and more locations were likely to be added, which may put
more pressure on NHs resources.
Case Study Healthcare for All: Narayana Hrudayalaya, Bangalore 3
Anda mungkin juga menyukai
- 2013 He Zha LiDokumen10 halaman2013 He Zha LianuragBelum ada peringkat
- Audit Selection Strategy For Improving Tax Compliance - Application of Data Mining TechniquesDokumen10 halamanAudit Selection Strategy For Improving Tax Compliance - Application of Data Mining TechniquesanuragBelum ada peringkat
- Synergy Consulting Inc. Role Documentation - Master BookDokumen14 halamanSynergy Consulting Inc. Role Documentation - Master BookanuragBelum ada peringkat
- TM Dialling NoDokumen5 halamanTM Dialling NoKiran KumarBelum ada peringkat
- Synergy Consulting Inc. Role Documentation - Master BookDokumen14 halamanSynergy Consulting Inc. Role Documentation - Master BookanuragBelum ada peringkat
- Dissertation Project Work ListDokumen1 halamanDissertation Project Work ListanuragBelum ada peringkat
- Lagging Behind Zara and H&M in India, US Label Gap Finally Looks To Cut Prices by 10-15% - The Economic TimesDokumen2 halamanLagging Behind Zara and H&M in India, US Label Gap Finally Looks To Cut Prices by 10-15% - The Economic TimesanuragBelum ada peringkat
- Narayana HrudayalayaDokumen3 halamanNarayana Hrudayalayaanurag100% (1)
- Icici Bank Vodafone India Launch MpesaDokumen4 halamanIcici Bank Vodafone India Launch MpesaanuragBelum ada peringkat
- In TMT Future of e Commerce NoexpDokumen40 halamanIn TMT Future of e Commerce Noexpanurag100% (1)
- R&D Roadmap Blast FurnaceDokumen37 halamanR&D Roadmap Blast FurnaceVishal JainBelum ada peringkat
- Narayana HrudayalayaDokumen3 halamanNarayana Hrudayalayaanurag100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- NWH Hospitals Empanelled Under RBSK: Sl. No. Hospital Name Taluk DistrictDokumen3 halamanNWH Hospitals Empanelled Under RBSK: Sl. No. Hospital Name Taluk Districtraamki_99Belum ada peringkat
- NH Annual Report 2016 17 PDFDokumen260 halamanNH Annual Report 2016 17 PDFR.Rajalakshmi RajendranBelum ada peringkat
- Inventive IndianDokumen168 halamanInventive Indianvijay7775303Belum ada peringkat
- Narayana Hrudayalaya Hospitals Research PaperDokumen27 halamanNarayana Hrudayalaya Hospitals Research Paperapi-238825442Belum ada peringkat
- Narayana Hurdyalaya Business Model CanvasDokumen7 halamanNarayana Hurdyalaya Business Model CanvasShubham SinhaBelum ada peringkat
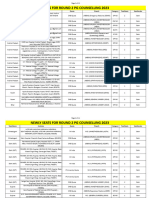
- Newly Seats For Round 2 PG Counselling 2023Dokumen11 halamanNewly Seats For Round 2 PG Counselling 2023Manoj KumarBelum ada peringkat
- 7p and 4i, NarayanaDokumen3 halaman7p and 4i, NarayanaVineet Pandey100% (1)
- Dr Devi Shetty on Affordable Healthcare SolutionsDokumen38 halamanDr Devi Shetty on Affordable Healthcare SolutionsVishwa SrivastavaBelum ada peringkat
- DETAILED PROJECT REPORT FOR OPERATION & MANAGEMENT SERVICES AT BHARUCH HOSPITALDokumen89 halamanDETAILED PROJECT REPORT FOR OPERATION & MANAGEMENT SERVICES AT BHARUCH HOSPITALzaheeruddin_mohdBelum ada peringkat
- NEET Super Speciality Counseling 2022 Round 1 Quota AbbreviationsDokumen208 halamanNEET Super Speciality Counseling 2022 Round 1 Quota AbbreviationsMinerva Medical Treatment Pvt LtdBelum ada peringkat
- Marketing AnalysisDokumen6 halamanMarketing AnalysisSwagato SarkarBelum ada peringkat
- Narayana Hrudalaya Heart HospitalDokumen17 halamanNarayana Hrudalaya Heart HospitalWaibhav Krishna100% (1)
- Narayana Hrudayalaya - 141215 PDFDokumen7 halamanNarayana Hrudayalaya - 141215 PDFrawatbs2020Belum ada peringkat
- Narayana HrudayalayaDokumen3 halamanNarayana Hrudayalayaanurag100% (1)
- Case 2 - Narayan HrudayalayaDokumen10 halamanCase 2 - Narayan Hrudayalayasujal vermaBelum ada peringkat
- DRAFT RED HERRING PROSPECTUS FOR NARAYANA HRUDAYALAYA IPODokumen548 halamanDRAFT RED HERRING PROSPECTUS FOR NARAYANA HRUDAYALAYA IPOShubham SinhaBelum ada peringkat
- Fixing - Nigeria (1) - 1 PDFDokumen40 halamanFixing - Nigeria (1) - 1 PDFFlying Doctors Nigeria100% (1)
- Devi ShettyDokumen38 halamanDevi ShettySujana RudrawaramBelum ada peringkat
- Narayana Hrudayalaya Corporate Overview and Vision to Become India's Largest Private Healthcare ProviderDokumen2 halamanNarayana Hrudayalaya Corporate Overview and Vision to Become India's Largest Private Healthcare ProviderChandra Sekhar100% (2)
- Axis Bank ListDokumen33 halamanAxis Bank ListNiketa OjhaBelum ada peringkat
- Post MBBS - Third Round Allotment DetailsDokumen89 halamanPost MBBS - Third Round Allotment DetailsAashish KapoorBelum ada peringkat
- Narayana HrudalayaDokumen20 halamanNarayana HrudalayaBikash Jaiswal100% (1)
- Narayan 2016Dokumen213 halamanNarayan 2016Jupe JonesBelum ada peringkat
- Company Profile Big BazaarDokumen17 halamanCompany Profile Big BazaarManikandan Mba0% (1)
- Peinv - Deals in PharmaDokumen9 halamanPeinv - Deals in PharmaSaurabh JainBelum ada peringkat
- On Narayana Hrudayalaya by Anup (Kumar OjhaDokumen10 halamanOn Narayana Hrudayalaya by Anup (Kumar Ojhaanupojha100% (2)
- Central Government Employees News - List of New Hospitals Empanelled Under CGHS, BengaluruDokumen7 halamanCentral Government Employees News - List of New Hospitals Empanelled Under CGHS, BengalururamanijiBelum ada peringkat
- Narayana Hrudayalaya - Section C - Group 5Dokumen22 halamanNarayana Hrudayalaya - Section C - Group 5raushanrahulBelum ada peringkat
- Narayana Hrudayalaya Cardiac Hospital Case Study LessonsDokumen11 halamanNarayana Hrudayalaya Cardiac Hospital Case Study LessonsSuhaib KhanBelum ada peringkat
- CGHS Empaneled HospitalsDokumen61 halamanCGHS Empaneled HospitalsAshutosh SaxenaBelum ada peringkat