403 396 1 SM
Diunggah oleh
ichaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
403 396 1 SM
Diunggah oleh
ichaHak Cipta:
Format Tersedia
ORIGINAL ARTICLE
Age and Alarm Symptoms Predict
Upper Gastrointestinal Malignancy
among Patients with Dyspepsia
Hendra Koncoro*, I Ketut Mariadi**, Gde Somayana**,
IGA Suryadarma**, Nyoman Purwadi**, IDN Wibawa**
* Department of Internal Medicine, Faculty of Medicine
University of Udayana/Sanglah Hospital, Denpasar
** Division of Gastroenterology, Department of Internal Medicine
University of Udayana /Sanglah Hospital, Denpasar
ABSTRACT
Background: Upper gastrointestinal (UGI) malignancy is one of the major causes of cancer related death.
Endoscopy in dyspeptic patients above 45 years, or those with alarm symptoms may detect this condition. There
were only limited data in Indonesia about age and alarm symptoms to predict UGI malignancy. This study
was aimed to determine the prevalence of UGI malignancy among dyspepsia patients and to develop a simple
clinical prediction model.
Method: A cross-sectional study to 390 patients with dyspepsia underwent endoscopy in Endoscopy Unit
of Sanglah Hospital Denpasar between July 2012 and June 2013 was conducted. Demography and alarm
symptoms were documented. Chi-square and logistic regression test analysis were conducted to analyze variables
associated with UGI malignancy.
Results: Twenty (5.13%) of 390 patients with dyspepsia had UGI malignancy. Of the 20 patients, 65% were
gastric cancer and 30% were esophageal cancer. The mean age was 59 12 years. Variables associated with UGI
malignancy were weight loss (OR = 8.2), dysphagia (OR = 6.2), age > 45 years old (OR = 5.6), gastrointestinal
bleeding (OR = 5.5), persistent vomiting (OR = 5.4), and anemia (OR = 4.9). Using a simplified rule of age >
45 years and the presence of any alarm symptom, sensitivity was 85% and specificity was 67.57%.
Conclusions: UGI malignancy was found in 5.13% of patients with dyspepsia who underwent endoscopy.
Simple clinical prediction model states that age above 45 years and alarm symptoms may be used as a screening
tool to predict UGI malignancy.
Keywords: dyspepsia, alarm symptoms, upper GI malignancy, clinical prediction model
ABSTRAK
Latar belakang: Keganasan saluran cerna bagian atas merupakan salah satu penyebab terbanyak kematian
terkait kanker. Endoskopi pada pasien dispepsia di atas usia 45 tahun atau mereka dengan tanda bahaya dapat
mendeteksi kondisi ini. Saat ini hanya ada sedikit data di Indonesia mengenai usia dan gejala tanda bahaya
dalam memprediksi keganasan saluran cerna bagian atas. Penelitian ini bertujuan untuk menentukan prevalensi
keganasan saluran cerna pada pasien dispepsia dan untuk mengembangkan contoh prediksi klinis sederhana.
Metode: Suatu penelitian potong-lintang dilakukan terhadap 390 pasien dispepsia yang menjalani prosedur
pemeriksaan endoskopi di Unit Endoskopi Rumah Sakit Sanglah Denpasar antara bulan Juli 2012 sampai Juni
2013. Faktor demografi dan gejala tanda bahaya didokumentasikan. Analisis Chi-square dan tes regresi logistik
dilakukan untuk menganalisa variabel yang berhubungan dengan keganasan saluran cerna bagian atas.
Volume 14, Number 2, August 2013 73
Hendra Koncoro, I Ketut Mariadi, Gde Somayana, IGA Suryadarma, Nyoman Purwadi, IDN Wibawa
Hasil: Dua puluh (5.13%) dari 390 pasien dispepsia menderita keganasan saluran cerna bagian atas. Dari
20 pasien, 65% dengan kanker lambung, dan 30% dengan kanker esofagus. Rerata usia adalah 59 12 tahun.
Variabel yang berhubungan dengan keganasan saluran cerna bagian atas adalah penurunan berat badan (RO
= 8.2), disfagia (RO = 6.2), usia > 45 tahun (RO = 5.6), perdarahan saluran cerna (RO = 5.5), muntah yang
persisten (RO = 5.4), dan anemia (RO = 0.49). Dengan menggunakan aturan prediksi sederhana usia > 45
tahun dan adanya tanda bahaya, sensitivitas mencapai 85% dan spesifisitas mencapai 67.57%.
Simpulan: Keganasan saluran cerna bagian atas dijumpai pada 5.13% pasien dispepsia yang menjalani
prosedur pemeriksaan endoskopi. Contoh prediksi klinis sederhana menyatakan usia di atas 45 tahun dan adanya
tanda bahaya dapat digunakan sebagai alat penapis untuk memprediksi keganasan saluran cerna bagian atas.
Kata kunci: dispepsia, tanda bahaya, keganasan saluran cerna bagian atas, contoh prediksi klinis
INTRODUCTION not be applicable in Indonesia as the prevalence of
UGI diseases remarkably differs. There has been
Upper gastrointestinal (UGI) malignancy has been
no study of the effectiveness of age and alarm
estimated globally to happen in about 1.4 million
features for predicting UGI cancers among dyspeptic
new cases in 2008. 1 Gastric cancer itself is the
patients in Indonesia. The aim of this study was to
worlds second leading cause of cancer mortality.1,2
determine the prevalence of UGI malignancy among
GLOBOCAN estimates that 1.1 million cancer deaths
dyspepsia patients who underwent endoscopy and
occurred worldwide in 2008 is due to UGI malignancy.1
to develop a simple clinical prediction model for
Greater than 50% of the worlds new cases of gastric
UGI malignancy.
cancer, and greater than 70% of newly diagnosed
esophageal cancer worldwide occur in Asian countries.
METHOD
World Health Organization South-East Asia region
(WHO SEARO) recorded 67,000 new cases of gastric This study is a cross-sectional study from endoscopy
cancer in 2008 with 15,000 (22%) of them came from record of patient with dyspepsia. Three hundred ninety
Indonesia. Although the incidence of gastric cancer in patients with dyspepsia underwent UGI endoscopy in
Indonesia is very low, morbidity and mortality rates of Endoscopy Unit of Sanglah Hospital Denpasar between
gastric cancer in Asia remain the highest in the world. July 2012 and June 2013. The inclusion criteria were
Of 740,000 deaths worldwide which happened due to all patients with dyspepsia who had agreed to undergo
gastric cancer, 13,500 deaths occurred in Indonesia.3 UGI tract endoscopy examination. Exclusion criteria
UGI malignancy frequencies are varied.4-6 were patients with age under 17 years old and patients
Endoscopy is the standard examination to diagnose with documented chronic liver disease.
UGI malignancy.7 Nevertheless, a prompt endoscopy The data were documented from the medical
for every dyspeptic patient cannot be a practical records and questionnaire. Data acquired consisted of
approach because it is not cost-effective and increases demographic data, presenting symptoms, and alarm
the workload of healthcare workers. 8 Therefore, symptoms. Alarm symptoms included were weight
American Gastroenterology Association (AGA) loss, dysphagia, GI bleeding, anemia, and persistent
recommends dyspeptic patients over 55 years, or those vomiting. In addition, reports of available laboratory
with alarm features such as weight loss, dysphagia, and endoscopy investigations were also obtained.
gastrointestinal (GI) bleeding, anemia, or persistent Identified histological data on biopsies of the UGI
vomiting should undergo endoscopy.9 A study stated mucosa were also collected.
that alarm symptoms increased the risk of UGI Unintentional weight loss was defined as 10%
malignancy to 5-6-fold.10 Of these patients, more than loss of body weight in recent 6 months. Dysphagia
80% had alarm symptoms.11,12 was perception of an impediment to the normal
While there are clinical features that should alert passage of swallowed material. GI bleeding translated
clinicians to the possibility of UGI malignancy, the as any evidence of hematemesis and/ or melena.
effectiveness of these alarm features are unclear.13,14 Persistent vomiting included if there was at least 7
Moreover, the majority of study was conducted to 10 days of protracted vomiting, while anemia was
in Europe, North America, or East Asia.6,8,10,11,14 defined as hemoglobin values lower than 10 g/dL.
Conclusions from Western or East Asia studies may UGI malignancy was defined as any histologically
74 The Indonesian Journal of Gastroenterology, Hepatology and Digestive Endoscopy
Age and Alarm Symptoms Predict Upper Gastrointestinal Malignancy among Patients with Dyspepsia
confirmed esophageal, gastric or duodenal cancer RESULTS
detected during endoscopy.
Between July 2012 and June 2013, 390 patients
SPSS version 17 software was used in statistical
with dyspepsia underwent UGI endoscopy. Mean age
analysis of this study. Age was summarized as
of patients was 48.8 14.1 years, and 228 (58.5%)
mean and standard deviation (SD). Sex and each
patients were above the age of 45 years. The most
alarm symptoms were summarized as counts and
frequent age group was between 41-50 years (25.9%).
percentages. Test for differences in age between
There were 220 (56.4%) male and 170 (43.6%) female
patients with and without UGI malignancy were done
patient. Of these, 318 (81.5%) patients had at least one
using the independent samples T-test or the Mann-
alarm symptoms. GI bleeding (27.9%), weight loss
Whitney U-test as appropriate. Test for sex and each
(17.9%), and anemia (16.7%) were the commonest
alarm symptoms were performed using Chi-square or
alarm symptoms found in all patients (Figure 1; Table 1).
Fishers exact test as appropriate.
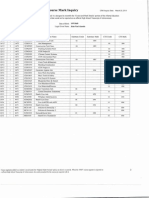
We estimated significant variables using bivariate Table 1. Demographic characteristics and distribution of alarm
symptoms in all dyspeptic patients
analysis. Backward stepwise selection in a multivariate
Dyspeptic patients
logistic regression was made for statistically significant
without upper with upper
factors. Subsequently, using an automated backward- Characteristics gastrointestinal gastrointestinal
stepwise multivariable method, we achieved the malignancy malignancy
n (%) n (%)
final model that only comprised the predictors with a
Mean age 48.8 14.1 59.0 12.0
multivariable p < 0.05. Once the variables included in
Age (years)
the model were defined, we examined the calibration > 45 210 (56.8%) 18 (90%)
of the model by performing Hosmer-Lemeshow 45 160 (43.2%) 2 (10%)
goodness-of-fit test. Based on regression model Sex
findings, we decided to report diagnostic accuracy Male 208 (56.2%) 12 (60%)
Female 162 (43.8%) 8 (40%)
measures using the area under the receiver operating
History of weight loss
characteristic (ROC) curve or AUC and its 95% Absent 313 (84.6%) 7 (35%)
confidence intervals (CI). Using histology as the Present 57 (15.4%) 13 (65%)
gold standard for diagnosis of UGI malignancies, we History of GI bleeding
Absent 274 (74.1%) 7 (35%)
calculated sensitivity, specificity, positive predictive
Present 96 (25.9%) 13 (65%)
value (PPV), and negative predictive value (NPV) History of persistent
of risk-prediction model based on selected age vomiting
classification model and alarm symptoms. We also Absent 330 (89.2%) 14 (70%)
Present 40 (10.8%) 6 (30%)
calculated diagnostic odds ratio (OR), and their related
History of dysphagia
95% confidence intervals for age, sex, and each of Absent 329 (88.9%) 11 (55%)
alarm symptoms using multivariable adjusted logistic Present 41 (11.1%) 9 (45%)
regression models. Anemia
Absent 315 (85.1%) 10 (50%)
Present 55 (14.9%) 10 (50%)
GI: gastrointestinal
All dyspeptic patients
Dyspepsia patients with upper
gastrointestinal malignancy
Figure 1. Proportion of all dyspeptic patient and patients with upper gastrointestinal malignancy in this study by age group
Volume 14, Number 2, August 2013 75
Hendra Koncoro, I Ketut Mariadi, Gde Somayana, IGA Suryadarma, Nyoman Purwadi, IDN Wibawa
A total of 20 UGI cancers were histologicaly Table 2. Endoscopic and histologic findings in study population
confirmed (5.13% prevalence) with 90% occurred in Criteria n (%)
subjects over 45 years of age. If the age of 55 had been Upper gastrointestinal endoscopy
No malignancy 370 (94.9%)
taken as the optimal age for screening, 60% cases would Esophageal malignancy 6 (1.5%)
have been missed. Patients with UGI malignancy were Gastric malignancy 13 (3.3%)
significantly older (mean age of 59.0 years) and more Duodenal malignancy 1 (0.3%)
likely to be male (60%) (Table 1). Patients reporting Cancer morphology
Esophageal SCC 3 (50%)
at least one of the alarm symptoms constituted 95% of
Adenocarcinoma 3 (50%)
patients with UGI malignancies compared to 53.3% in Gastric
patients without cancer (p < 0.001). Adenocarcinoma 8 (61.5%)
Table 2 shows the endoscopic and histological Signet ring cell carcinoma 3 (23.1%)
findings in the study participants. Of the 20 patients Others (GIST, MALT lymphoma) 2 (15.4%)
Duodenal
with cancer, 13 (65%) were diagnosed with gastric
Adenocarcinoma 1 (100%)
cancer, 6 (30%) with esophageal cancer, and 1 (5%) Cancer topography
with duodenal cancer. The majority of gastric cancers Esophageal middle-third 1 (16.7%)
was adenocarcinomas (61.5%) and was located in the Esophageal lower-third 5 (83.3%)
Gastric
antrum (38.4%). Esophageal cancers were consisted
Cardia 2 (15.4%)
of three adenocarcinomas and three squamous cell Corpus 3 (23.1%)
types and were located more in the distal-third of the Antrum 5 (38.4%)
esophagus (83.3%) (Table 2). Diffuse 3 (23.1%)
We used bivariate analysis to determine which Duodenal
D1 1 (100%)
variables were suitable for multivariate analysis. Male SCC: squamous cell carcinoma; GIST: gastrointestinal stromal tumor; MALT:
was not different to female of having UGI cancers (p mucosa-associated lymphoid tissue); D1: duodenum part 1
= 0.740). On the other hand, relations between age
and each alarm symptoms with UGI malignancy were Multivariate analysis found that age (> 45 years),
found. Each predictor variable (age > 45, weight loss, weight loss, dysphagia, bleeding, anemia, and
dysphagia, anemia, bleeding, and persistent vomiting) persistent vomiting were significant predictors of
was significant in the bivariate analysis (Table 3). having an upper GI malignancy (Table 4). The accuracy
Table 3. Bivariate analysis of variables predict UGI malignancy
Dyspeptic patients without Dyspeptic patients with
Characteristic UGI malignancy UGI malignancy p*
Frequency % Frequency %
Age ( SD) 48.8 14.1 59.0 12.0 0.002
Sex
Male 208 56.2 12 60 0.740
Female 162 43.8 8 40
History of weight loss
Absent 313 84.6 7 7 < 0.001
Present 57 15.4 13 65
History of gastrointestinal bleeding
Absent 274 74.1 7 35 < 0.001
Present 96 25.9 13 65
History of persistent vomiting
Absent 330 89.2 14 70 0.010
Present 40 10.8 6 30
History of dysphagia
Absent 329 88.9 11 55 < 0.001
Present 41 11.1 9 45
Anemia
Absent 315 85.1 10 50 < 0.001
Present 55 14.9 10 50
*p values are calculated using independent sample T-test for age and Chi-square tests for variables to compare the distribution of the variables between patient
with and without UGI malignancy; UGI: upper gastrointestinal
76 The Indonesian Journal of Gastroenterology, Hepatology and Digestive Endoscopy
Age and Alarm Symptoms Predict Upper Gastrointestinal Malignancy among Patients with Dyspepsia
of the multivariate model was shown in Figure 2. Due to low specificity of first model we tried to
The Hosmer-Lemeshow test showed p = 0.902 which specify new criteria combining age and any alarm
informed that this multivariate model had a good symptoms (weight loss, dysphagia, GI bleeding,
calibration. ROC analysis presented AUC 0.91 (95% anemia, and persistent vomiting). Instead of using
CI = 0.852-0.978) indicated that this model had good just one marker such as only age older than 45 years
statistic quality. or any components of alarm symptoms implied in
the classical criteria, we used new criteria that stated
Table 4. Multivariate analysis of variables predict upper age older than 45 years and any components of alarm
gastrointestinal malignancy
symptoms. Using this new model, 17 of 137 (12.41%)
Variables Coefficient p OR (95% CI)
History of weight loss 2.101 < 0.001 8.17 (2.63-25.44)
had an UGI malignancy (positive predictive value).
History of GI bleeding 1.712 0.006 5.54 (1.64-18.70) Negative predictive value of this model was 250 of
Persistent vomiting 1.696 0.019 5.45 (1.32-22.50) 253 (98.81%). The sensitivity of the new model was
History of dysphagia 1.830 0.004 6.23 (1.82-21.31) 85% and specificity was 67.57%. Applying these new
Anemia 1.585 0.011 4.88 (1.44-16.55)
criteria would have resulted in findings of 17 dyspeptic
Age > 45 years 1.726 0.037 5.62 (1.11-28.51)
Constant -7.141 < 0.001 0.001 patients with UGI malignancy.
GI: gastrointestinal; CI: confidence interval
DISCUSSION
UGI malignancy is still remaining as major health
problem. Existing data of every state is different. UGI
malignancies has different prevalence, ranging from
0.5 to 9.7% from several endoscopic studies.4,15 Study
in United Kingdom reported prevalence of 2.0 to
3.8%.16,17 Lower incidence reported from Hongkong
which is 0.90%.18 Records of more than 100,000
patients in China resulted prevalence of 4.2%.6
Another study in Cipto Mangunkusumo Hospital
Jakarta resulted 5.20% cases of UGI malignancy
among dyspeptic patients.12 In this study, the result is
5.13% UGI malignancy among 390 dyspeptic patient
underwent endoscopy. This result is greater than most
studies but seems to be in accordance with Cipto
Mangunkusumo Hospital study. This may be caused
by Sanglah Hospital which acts as regional referral
hospital from other hospitals, also from Nusa Tenggara.
Figure 2. ROC curve showing the relationship between
sensitivity and specificity of the prediction rule for major up- The distribution of UGI malignancy in this study is
per gastrointestinal pathology. The diagonal line represents a gastric cancer 3.33%, esophageal cancer 1.54% and
model which has zero predictive value. C statistic (area under
the ROC curve) = 0.91 duodenal cancer 0.26%. The result of this study is
higher compared to study conducted in Singapore and
Saudi Arabia where cases found were gastric cancer
We applied the simplified decision rule where
0.47% and 0.91%, esophageal cancer 0.06% and 1.49%
the presence of any significant predictor (age > 45
respectively. But it is still lower than center in Medan
years, weight loss, dysphagia, anemia, bleeding,
which showed incidence of 5.6%.19 This study shows
persistent vomiting) was considered as an indication
similarity with other studies conducted in Indonesia.
for endoscopy. Among patients aged more than 45 or
Study in Cikini Hospital Jakarta showed that incidence
those with significant predictors, 20 of 318 (6.29%)
of gastric cancer in 2005 was 3.9%.20
had an UGI malignancy (positive predictive value)
Most gastric cancer in our study was located at
(Table 4). Among younger patients with no significant
antrum (38.4%). This is in accordance with other
predictors, 72 of 72 (100%) had no UGI malignancy
studies in South-East Asia. 12,21 Gastric cancer is
(negative predictive value) (Table 4). The sensitivity of
still antral predominant cancer in Asian countries,
the simplified prediction rule was 100% and specificity
and though we did not study the association of
was 19.5%.
Helicobacter pylori (H. pylori) with the gastric
Volume 14, Number 2, August 2013 77
Hendra Koncoro, I Ketut Mariadi, Gde Somayana, IGA Suryadarma, Nyoman Purwadi, IDN Wibawa
cancer in our study, carcinogenesis-promoting effect Of these, weight loss and dysphagia were the most
of H. pylori seems to be responsible for this. In a important predictors. Male was not associated with
large prospective nested case-control study, H. pylori higher risk of UGI malignancy. Some previous studies
was strongly associated with distal gastric cancer.22 have also assessed the value of age and alarm symptoms
Adenocarcinoma constituted most of gastric cancer in in predicting risk of cancer in dyspeptic patients.6,16,30
our study. This finding was similar with other study Large samples study in China proposed criteria that
which stated that approximately 90% of gastric cancers stated age and some components of alarm symptoms
were adenocarcinomas.2,5,23,24 Findings of esophageal were valuable in diagnosing UGI malignancy.6A meta-
cancers location in our study were also similar with analysis by Fransen et al found limited diagnostic
other study conducted in Jakarta. Retrospective values including sensitivity, specificity and predictive
study in Jakarta found lower third part as the most values, for each individual alarm symptom.4 They
common site of esophageal cancer, as also proved by suggested using alarm symptoms in combination with
our study in Bali.25 This finding probably related to other factors such as age, sex, or smoking might
gastroesophageal reflux disease which may turn to be a better tool for selection of high-risk patients.
Barretts metaplasia and predispose to malignancy in Kapoor et al., built criteria that said dysphagia or
such location. weight loss may increase the opportunity of having
The mean age of UGI malignancy in this study was UGI malignancy.16 Khademi et al agreed criteria that
59.0 12.0 years, and 90% patients were above the age combine demographic factors and alarm symptoms as
of 45 years. Of 20 patients with UGI malignancy, 60% clues to do endoscopy.5
were male and 40% were female. Due to this condition In this study, six factors were found significant as
we used the age cut-off at 45 years at Sanglah hospital. predictors for UGI malignancy and then developed as
This is similar to the recommendation in several a risk-prediction model. Those factors were age more
studies.8,9,15,26 Hsu reaffirmed that the age threshold for than 45 years, weight loss, dysphagia, GI bleeding,
screening should be set at 40-50 years in Asia.8 Syam persistent vomiting, and anemia. Unfortunately
also agreed 45 years as the age cut-off to underwent male was not significant as predictive factor. Recent
endoscopy.26 Talley suggested an age cut-off of 55 study showed that men did not have significantly
years for Western countries and a lower threshold in higher chance of UGI cancers than women.5 The
some countries in the Asia-Pacific region.9 This higher discriminative values of alarm symptoms were further
incidence of UGI malignancy especially gastric cancer supported by their independent association with
observed among men is partially explained by higher malignancy. This was also proved by group in Taiwan
H. pylori infection rates in male as proved by a large, that found weight loss, GI bleeding and dysphagia as
population-based metaanalysis.27 predictive factors for UGI malignancy.8 Among all
Dyspepsia patients with alarm signs have been predictors in study conducted in Sanglah Hospital,
found in 19 (95%) patients, including decrease of weight loss was the strongest predictor of UGI cancers
bodyweight, melena, hematemesis, anemia and as implied in other study.5
dysphagia. Of all dyspeptic patients found, GI bleeding Risk-prediction model in our study consisted of
was the most common alarm sign presented (27.9%). age > 45 years and alarm symptoms. Using classical
This is similar with study conducted in Koja hospital prediction model that states recommendation of
which found GI bleeding as the most common alarm endoscopy in subjects older than 45 years or has any
symptoms found.28 Maconi et al reported that among components of alarm symptom, yield low specificity.
92 gastric cancer, 58.7% had uncomplicated dyspepsia Therefore, classic premise is not a proper tool as a
and 41.3% had alarm sign.29 screening test for UGI malignancy. By changing the
Alarm symptoms are accepted as an indication for premise into age older than 45 years and components of
direct endoscopy.4,9 However, the existing evidence alarm symptoms, the specificity increased. New criteria
does not consistently support the usefulness of alarm with better sensitivity and specificity proved to be a
symptoms for this matter.13 Another study found that good diagnostic tool in detection of UGI malignancy.
93% of patients had an alarm feature when diagnosis Hsu et al also demonstrated that age threshold of
of UGI malignancy was established.30 In this study, 45 years and alarm symptom would identify almost
age more than 45 years, weight loss, dysphagia, all dyspeptic patients with UGI malignancy.8 These
GI bleeding, persistent vomiting, and anemia were criteria that combine age cut-off and any components
all positively associated with risk of UGI cancers. of alarm symptoms may be used in the future among
78 The Indonesian Journal of Gastroenterology, Hepatology and Digestive Endoscopy
Age and Alarm Symptoms Predict Upper Gastrointestinal Malignancy among Patients with Dyspepsia
primary health care, to suspect patient who most likely database review of 102,665 patients from 1996 to 2006. Gut
2010;59:722-8.
need to be further investigated by endoscopy for any
7. Hirota WK, Zuckerman MJ, Adler DG, Davila RE, Egan J,
condition of UGI malignancy. This new criteria is cost- Leighton JA, et al. ASGE guideline: the role of endoscopy in
effective and may save burden of cost due to improper the surveillance of premalignant conditions of the upper GI
selection of candidate for endoscopy. tract. Gastrointest Endosc 2006;63:570-80.
The strengths of our study are relatively large 8. Hsu YC, Yang TH, Liou JM, Hsu WL, Lin HJ, Wu HT,
et al. Can clinical features stratify use of endoscopy for
sample size collected for one year, simple criteria dyspeptic patients with high background prevalence of upper
added in diagnosing UGI malignancy, and the first gastrointestinal cancer? Dig Liver Dis 2012;44:218-23.
study in Indonesia as far as we know that prove age 9. Talley NJ, Vakil N. Guidelines for the management of
and alarm symptoms as beneficial tool in detecting UGI dyspepsia. Am J Gastroenterol 2005;100:2324-37.
malignancy. Limitations of the study are unavailability 10. Salo M, Collin P, Kyronpalo S, Rasmussen M, Huhtala H,
Kaukinen K. Age, symptoms and upper gastrointestinal
of other demographic factors and clinical parameters malignancy in primary care endoscopy. Scand J Gastroenterol
such as H. pylori infection that may relate and add 2008;43:122-7.
accuracy in diagnosing UGI malignancy and no 11. Bowrey DJ, Griffin SM, Wayman J, Karat D, Hayes N, Raimes
external validation set. SA. Use of alarm symptoms to select dyspeptics for endoscopy
causes patients with curable esophagogastric cancer to be
overlooked. Surg Endosc 2006;20:1725-8.
CONCLUSION 12. Yusuf AI, Syam AF, Abdullah M, Makmun D, Simadibrata
M, Manan C, et al. Upper gastrointestinal malignancy among
Upper gastrointestinal malignancy was found in dyspepsia patients in Cipto Mangunkusumo Hospital Jakarta.
Indones J Gastroenterol Hepatol Dig Endosc 2009;10:92-5.
small portion of dyspeptic patients. The older the
13. Wallace B, Durkalski VL, Vaughan J, Palesch YY, Libby
age of patients and alarm symptoms are associated ED, Jowell PS, et al. Age and alarm symptoms do not predict
with the risk of upper gastrointestinal malignancy. endoscopic findings among patients with dyspepsia: a multicentre
Simple clinical prediction model states that older age database study. Gut 2001;49:29-34.
and any components of alarm symptoms may be used 14. Vakil N, Moayyedi P, Fennerty B, Talley NJ. Limited value
of alarm features in the diagnosis of upper gastrointestinal
as a screening tool for further endoscopy. Prediction malignancy: systematic review and meta-analysis.
strategies are cost-effective and may be useful among Gastroenterology 2006;131:390-401.
primary health care services as indications in predicting 15. Canga C, Vakil N. Upper gastrointestinal malignancy,
potential upper gastrointestinal malignancies which uncomplicated dyspepsia, and age threshold for early
endoscopy. Am J Gastroenterol 2002;97:600-3.
may warrant referral.
16. Kapoor N, Bassi A, Sturgess R, Bodger K. Predictive value of
alarm features in a rapid access upper gastrointestinal cancer
service. Gut 2005;54:40-45.
REFERENCES 17. Sundar N, Muraleedharan V, Pandit J, Green JT, Crimmins
1. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. R, Swift GL. Does endoscopy diagnose early gastrointestinal
GLOBOCAN 2008 v1.2. Cancer incidence and mortality cancer in patients with uncomplicated dyspepsia?. Postgrad
worldwide: IARC Cancer Base No. 10. Lyon, France: Med J 2006;82:52-4.
International Agency for Research on Cancer, 2010 [cited 18. Sung JJ, Lao WC, Lai MS, Li TH, Chan FK, Wu JC, et al.
2013 Jul 1]. Available from: http://globocan.iarc.fr. Incidence of gastro-esophageal malignancy in patients with
2. Kelley JR, Duggan JM. Gastric cancer epidemiology and risk dyspepsia in Hongkong: implication for screening strategies.
factors. J Clin Epidemiol 2003;56:1-9. Gastrointest Endosc 2001;54:454-8.
3. IARC. GLOBOCAN 2008. International agency for research 19. Soeripto, Indrawati, Indrayanti. Gastrointestinal cancer in
on cancer 2010 [cited 2013 Jul 1]. Available from: http:// Indonesia. Asian Pac J Cancer Prev 2003;4:289-96.
globocan.iarc.fr/factsheet.asp. 20. Saragih JB, Akbar N, Syam AF, Sirait S, Himawan S,
4. Fransen GAJ, Janssen MJR, Muris JWM, Laheij RJF, Jansen Soetjahyo E. Incidence of Helicobacter pylori infection and
JBMJ. Meta-analysis: the diagnostic value of alarm symptoms gastric cancer: an 8-year hospital based study. Acta Med
for upper gastrointestinal malignancy. Aliment Pharmacol Indones 2007;39:79-81.
Ther 2004;20:1045-52. 21. Kandasami P, Tan WJ, Norain K. Gastric cancer in Malaysia:
5. Khademi H, Radmard A-R, Malekzadeh F, Kamangar F, the need for early diagnosis. Med J Malaysia 2003;58:758-62.
Nasseri-Moghaddam S, et al. Diagnostic accuracy of age and 22. Kamangar F, Dawsey SM, Blaser MJ, Perez-Perez GI,
alarm symptoms for upper GI malignancy in patients with Pietinen P, Newschaffer CJ, et al. Opposing risks of gastric
dyspepsia in a gastrointestinal clinic: a 7-year cross-sectional cardia and noncardia gastric adenocarcinomas associated
study. PLoS ONE 2012;7:e39173. with Helicobacter pylori seropositivity. J Natl Cancer Inst
6. Bai Y, Li ZS, Zou DW, Wu RP, Yao YZ, Jin ZD, et al. 2006;98:1445-52.
Alarm features and age for predicting upper gastrointestinal 23. Crew KD, Neugut AI. Epidemiology of gastric cancer. World
malignancy in Chinese patients with dyspepsia with high J Gastroenterol 2006;12:354-62.
background prevalence of Helicobacter pylori infection
and upper gastrointestinal malignancy: an endoscopic
Volume 14, Number 2, August 2013 79
Hendra Koncoro, I Ketut Mariadi, Gde Somayana, IGA Suryadarma, Nyoman Purwadi, IDN Wibawa
24. Julius. Tumor Gaster. In: Sudoyo AW, Setyohadi B, Alwi I,
Simadibrata M, Setiati S, eds. Buku Ajar llmu Penyakit Dalam.
Jakarta: Interna Publ 2009.p.576-80.
25. Sutopo B, Makmun D, Simadibrata M. The profile of
hospitalized patients with esophageal cancer at Cipto
Mangunkusumo General National Hospital in 2002-2008.
Indones J Gastroenterol Hepatol Dig Endosc 2009;10:66-9.
26. Syam AF. Uninvestigated dyspepsia versus investigated
dyspepsia. Acta Med Indones 2005;37:113-5.
27. De Martel C, Parsonnet J. Helicobacter pylori infection
and gender: a meta-analysis of population-based prevalence
surveys. Dig Dis Sci 2006;51:2292-301.
28. Ndraha S, Simadibrata M. Upper gastrointestinal endoscopic
and histopathological findings in patients with dyspepsia.
Indones J Gastroenterol Hepatol Dig Endosc 2012;13:23-8.
29. Maconi O, Kurihara H, Panizzo P, Russo A, Cristaldi M,
Marrelli D, et al. Gastric cancer in young patients with no
alarm symptom: focus on delay in diagnosis, stage of neoplasm
and survival. Scand J Gastroenterol 2003;38:1249-55.
30. Berrill JW, Turner JK, Hurley JJ, Swift G, Dolwani S,
Green JT. Upper gastrointestinal cancer in its early stages
is predominantly asymptomatic. Frontline Gastroenterol
2012;3:47-51.
Correspondence:
IDN Wibawa
Division of Gastroentero-hepatology
Department of Internal Medicine
Sanglah General Hospital
Jl. Sanglah, Denpasar 80114 Indonesia
Phone/Facsimile: +62-361-244177
E-mail: dnwib@dps.centrin.net.id
80 The Indonesian Journal of Gastroenterology, Hepatology and Digestive Endoscopy
Anda mungkin juga menyukai
- Development of Type I Gastric Carcinoid in Patients With Chronic Atrophic GastritisDokumen9 halamanDevelopment of Type I Gastric Carcinoid in Patients With Chronic Atrophic GastritisAbristaSeptikasariBelum ada peringkat
- Admin,+58 Ism.v11i1.565Dokumen4 halamanAdmin,+58 Ism.v11i1.565hayyatBelum ada peringkat
- Clinical and Endoscopic Study of Dysphagia: A Prospective Crossectional Study at A Tertiary Care Centre at North - Eastern IndiaDokumen3 halamanClinical and Endoscopic Study of Dysphagia: A Prospective Crossectional Study at A Tertiary Care Centre at North - Eastern IndiaInternational Organization of Scientific Research (IOSR)Belum ada peringkat
- Dispepsia PDFDokumen8 halamanDispepsia PDFaldo holymanBelum ada peringkat
- Acalculous Cholecystitis Prevalence On Abdominal Ultrasonography Examination of HIV/HCV Co-Infection Patients in Cipto Mangunkusumo HospitalDokumen3 halamanAcalculous Cholecystitis Prevalence On Abdominal Ultrasonography Examination of HIV/HCV Co-Infection Patients in Cipto Mangunkusumo HospitalDiga AlbrianBelum ada peringkat
- Van Nella 2010Dokumen9 halamanVan Nella 2010Anonymous tSdibBveBelum ada peringkat
- Clinical Profile of Patients With Obstructive Jaundice: A Surgeon's PerspectivesDokumen5 halamanClinical Profile of Patients With Obstructive Jaundice: A Surgeon's Perspectivessitoxpadang ceriaBelum ada peringkat
- Research Article: Low Prevalence of Clinically Significant Endoscopic Findings in Outpatients With DyspepsiaDokumen7 halamanResearch Article: Low Prevalence of Clinically Significant Endoscopic Findings in Outpatients With DyspepsiaKurnia pralisaBelum ada peringkat
- Toddler's Diarrhea: Is It An Under-Recognized Entity in Developing Countries?Dokumen6 halamanToddler's Diarrhea: Is It An Under-Recognized Entity in Developing Countries?deonardBelum ada peringkat
- Clinico-Etiological Pattern of Upper Gastrointestinal Bleeding in ChildrenDokumen4 halamanClinico-Etiological Pattern of Upper Gastrointestinal Bleeding in ChildrenAsfiani PediatricianBelum ada peringkat
- Pathophysiology, Diagnosis, and Management of Chronic Intestinal Pseudo-ObstructionDokumen13 halamanPathophysiology, Diagnosis, and Management of Chronic Intestinal Pseudo-ObstructionJosealberto ArenasBelum ada peringkat
- Role of Symptoms in Diagnosis and Outcome of Gastric Cancer: EditorialDokumen7 halamanRole of Symptoms in Diagnosis and Outcome of Gastric Cancer: EditorialMarwin JouleBelum ada peringkat
- Validation of Instruments For The Assessment of Dysphagia Due To Malignancy of The EsophagusDokumen8 halamanValidation of Instruments For The Assessment of Dysphagia Due To Malignancy of The EsophagusLarissa MeloBelum ada peringkat
- Di Lillo 2019Dokumen7 halamanDi Lillo 2019putri permata SariBelum ada peringkat
- Barret 2015.Dokumen6 halamanBarret 2015.Elizabeth VegaBelum ada peringkat
- Laparotomy in Children in A Tertiary Hospital in A Developing CountryDokumen5 halamanLaparotomy in Children in A Tertiary Hospital in A Developing CountryWorld Journal of Clinical SurgeryBelum ada peringkat
- Upper and Lower Gastrointestinal Bleeding: A Retrospective Study On 10 Years Experiences in Southeastern IranDokumen6 halamanUpper and Lower Gastrointestinal Bleeding: A Retrospective Study On 10 Years Experiences in Southeastern IranAlne DanyBelum ada peringkat
- Prevalence of Gastroesophageal Reflux Disease (GERD) in Dyspepsia Patients in Primary Referral HospitalDokumen6 halamanPrevalence of Gastroesophageal Reflux Disease (GERD) in Dyspepsia Patients in Primary Referral HospitalAbrar TaraBelum ada peringkat
- Endoscopic Hemostasis in Intensive Care Unit Patients With Upper Digestive Tract BleedingDokumen7 halamanEndoscopic Hemostasis in Intensive Care Unit Patients With Upper Digestive Tract BleedingAgung KaryawinaraBelum ada peringkat
- Gastrointestinal Endoscopy Volume 71 Issue 7 2010 (Doi 10.1016/j.gie.2009.12.029) Lisette G. Capelle Annemarie C. de Vries Jelle Haringsma Fran - The Staging of Gastritis With The OLGA System by PDFDokumen9 halamanGastrointestinal Endoscopy Volume 71 Issue 7 2010 (Doi 10.1016/j.gie.2009.12.029) Lisette G. Capelle Annemarie C. de Vries Jelle Haringsma Fran - The Staging of Gastritis With The OLGA System by PDFAleida VivalloBelum ada peringkat
- Prevalence of Upper GI-Endoscopic Lesions in CKDDokumen7 halamanPrevalence of Upper GI-Endoscopic Lesions in CKDheba.barkasiehBelum ada peringkat
- Pattern of Persistent Liver Disorders in ChildrenDokumen7 halamanPattern of Persistent Liver Disorders in ChildrenInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Guideline: Pimentel-Nunes Pedro Et Al. MAPS II Endoscopy 2019 51: 365-388Dokumen24 halamanGuideline: Pimentel-Nunes Pedro Et Al. MAPS II Endoscopy 2019 51: 365-388Josseph EscobarBelum ada peringkat
- Ce 48 291Dokumen6 halamanCe 48 291Siska HarapanBelum ada peringkat
- Practices in Paediatric Gastrointestinal Endoscopy at Kenyatta National Hospital and Gertrudes Children's Hospital in Nairobi KenyaDokumen11 halamanPractices in Paediatric Gastrointestinal Endoscopy at Kenyatta National Hospital and Gertrudes Children's Hospital in Nairobi Kenyafrankline nyabutoBelum ada peringkat
- IBD-Rough Road - Case Study in IBD From Presentation To ManagementDokumen4 halamanIBD-Rough Road - Case Study in IBD From Presentation To ManagementBejan CorinaBelum ada peringkat
- Diagnostic Methods in Dyspepsia The Usefulness of Upper Abdominal Ultrasound and GastrosDokumen6 halamanDiagnostic Methods in Dyspepsia The Usefulness of Upper Abdominal Ultrasound and GastrosWingga Chrisna AjiBelum ada peringkat
- 2effectiveness of Systematic Alphanumeric Coded ESGE - Machacaquea2016Dokumen7 halaman2effectiveness of Systematic Alphanumeric Coded ESGE - Machacaquea2016Thạch tài liệu 1 BùiBelum ada peringkat
- Gastroparesis Updates On Pathogenesis and Management: ReviewDokumen11 halamanGastroparesis Updates On Pathogenesis and Management: Reviewputri permata SariBelum ada peringkat
- Gastritis and Gastropathy Perspectives From The EndoscopistDokumen4 halamanGastritis and Gastropathy Perspectives From The Endoscopisthenrique.uouBelum ada peringkat
- Endoscopic Management of Polyposis Syndromes: European Society of Gastrointestinal Endoscopy (ESGE) GuidelineDokumen19 halamanEndoscopic Management of Polyposis Syndromes: European Society of Gastrointestinal Endoscopy (ESGE) Guidelineseptian_tjayaBelum ada peringkat
- Scholl Hammer 2015Dokumen7 halamanScholl Hammer 2015jesslynBelum ada peringkat
- Eng 2014Dokumen6 halamanEng 2014Ahmad NurdiansyahBelum ada peringkat
- 2022 - Clinical Value of Abdominal USG in The Diagnosis of Acute Abdomen in ChildrenDokumen7 halaman2022 - Clinical Value of Abdominal USG in The Diagnosis of Acute Abdomen in ChildrenRevivo RindaBelum ada peringkat
- WJG 18 4335Dokumen7 halamanWJG 18 4335aalmadasalazarBelum ada peringkat
- Medical Science: Gjra - Global Journal For Research Analysis X 4Dokumen3 halamanMedical Science: Gjra - Global Journal For Research Analysis X 4ZulhamBelum ada peringkat
- Management of Ruptured Liver Abscess: A Study of 54 CasesDokumen4 halamanManagement of Ruptured Liver Abscess: A Study of 54 CasesIndah FebrianaBelum ada peringkat
- Masson Et Al-2007-Colorectal DiseaseDokumen4 halamanMasson Et Al-2007-Colorectal DiseaseCamy CarmenBelum ada peringkat
- Jejunojejunal Intussusception As Initial Presentation of Coeliac Disease: A Case Report and Review of LiteratureDokumen6 halamanJejunojejunal Intussusception As Initial Presentation of Coeliac Disease: A Case Report and Review of Literatureellya theresiaBelum ada peringkat
- Serologic and Urine Diagnostic Tests To Detect Helicobacter Pylori Infection in Functional Dyspepsia PatientsDokumen5 halamanSerologic and Urine Diagnostic Tests To Detect Helicobacter Pylori Infection in Functional Dyspepsia PatientsAnasthasia hutagalungBelum ada peringkat
- KJG074 01 04 PDFDokumen13 halamanKJG074 01 04 PDFNovita AfsariBelum ada peringkat
- Atlas of Inflammatory Bowel DiseasesDari EverandAtlas of Inflammatory Bowel DiseasesWon Ho KimBelum ada peringkat
- A Study of Preoperative Predictive Factors of Strangulation in Acute Small Intestinal ObstructionDokumen6 halamanA Study of Preoperative Predictive Factors of Strangulation in Acute Small Intestinal ObstructionSantosh BabuBelum ada peringkat
- Non Alcoholic Liver Disease PhilippinesDokumen5 halamanNon Alcoholic Liver Disease PhilippinesMara Benzon-BarrientosBelum ada peringkat
- Abstract: Gastritis Is An Inflammatory Process in The Mucosa and Sub Mucosa of The Stomach ThatDokumen8 halamanAbstract: Gastritis Is An Inflammatory Process in The Mucosa and Sub Mucosa of The Stomach ThatKatino RomerBelum ada peringkat
- William, Update On Approaches To Patients With Dyspepsia and Functional DyspepsiaDokumen6 halamanWilliam, Update On Approaches To Patients With Dyspepsia and Functional DyspepsiaRevalitha PutriBelum ada peringkat
- Accepted Manuscript: Clinical Gastroenterology and HepatologyDokumen20 halamanAccepted Manuscript: Clinical Gastroenterology and HepatologyСергей СадовниковBelum ada peringkat
- Adenoma y CA GastricoDokumen8 halamanAdenoma y CA GastricoJhon Jaime CarvajalBelum ada peringkat
- Jurnal DiagnosisDokumen9 halamanJurnal DiagnosisRenyBelum ada peringkat
- 375 PDFDokumen7 halaman375 PDFHasnan HabibBelum ada peringkat
- 9378 40654 1 PBDokumen8 halaman9378 40654 1 PBNabila ZainBelum ada peringkat
- 2017-05 Norfolk and Waveney CPDG Policy Briefing Paper - Capsule EndoscoDokumen4 halaman2017-05 Norfolk and Waveney CPDG Policy Briefing Paper - Capsule EndoscoAlessioNavarraBelum ada peringkat
- Clinical Guidelines Secondary Prevention of Gastric CancerDokumen1 halamanClinical Guidelines Secondary Prevention of Gastric Cancerhenrique.uouBelum ada peringkat
- En V27n4a02Dokumen6 halamanEn V27n4a02Humberto Liu BejaranoBelum ada peringkat
- B Celiaca Al Toma PDFDokumen31 halamanB Celiaca Al Toma PDFSimona JuncuBelum ada peringkat
- Candida EsofagitisDokumen5 halamanCandida EsofagitisVina IsmawatiBelum ada peringkat
- BMJ 2023 076017.fullDokumen7 halamanBMJ 2023 076017.fullStefanoBelum ada peringkat
- A Prospective Study On Acute Abdomen at Agogo Presbyterian Hospital (APH), Ghana: Identification of Common Causes and Pattern of PresentationDokumen7 halamanA Prospective Study On Acute Abdomen at Agogo Presbyterian Hospital (APH), Ghana: Identification of Common Causes and Pattern of PresentationInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Gastritis Atrofica ReviewDokumen33 halamanGastritis Atrofica ReviewFiorella Portella CordobaBelum ada peringkat
- JurnalDokumen5 halamanJurnalAlpi ApriansahBelum ada peringkat
- No No. Identitas Tanggal Reginik/No. Identitas Nama Terduga TB UmurDokumen21 halamanNo No. Identitas Tanggal Reginik/No. Identitas Nama Terduga TB UmurichaBelum ada peringkat
- 2021 Juni PendingDokumen36 halaman2021 Juni PendingichaBelum ada peringkat
- Perdir Prognas-8-9Dokumen2 halamanPerdir Prognas-8-9ichaBelum ada peringkat
- Medicinus JournalDokumen68 halamanMedicinus JournalDian Rosdiani FajrinBelum ada peringkat
- MR 4 Nov 2016Dokumen4 halamanMR 4 Nov 2016ichaBelum ada peringkat
- Jurnallll PDFDokumen6 halamanJurnallll PDFichaBelum ada peringkat
- Hypertension and Anaesthesia: Anaesthetics SupplementDokumen5 halamanHypertension and Anaesthesia: Anaesthetics SupplementichaBelum ada peringkat
- Improving Tsunami Warning Systems With Remote Sensing and Geographical Information System InputDokumen16 halamanImproving Tsunami Warning Systems With Remote Sensing and Geographical Information System InputichaBelum ada peringkat
- "Perioperativehypertension: Diagnosisandtreatment": ReviewDokumen6 halaman"Perioperativehypertension: Diagnosisandtreatment": ReviewichaBelum ada peringkat
- Kuliah Jamur FKMDokumen90 halamanKuliah Jamur FKMichaBelum ada peringkat
- Night Shifts, Sleep Deprivation, and Attention Performance in Medical StudentsDokumen7 halamanNight Shifts, Sleep Deprivation, and Attention Performance in Medical StudentsichaBelum ada peringkat
- Measuring Healthcare Preparedness: An All-Hazards Approach: Commentary Open AccessDokumen2 halamanMeasuring Healthcare Preparedness: An All-Hazards Approach: Commentary Open AccessichaBelum ada peringkat
- Towards Disaster Management in Indonesia Case Studies: Jakarta and Yogyakarta ProvincesDokumen12 halamanTowards Disaster Management in Indonesia Case Studies: Jakarta and Yogyakarta ProvincesichaBelum ada peringkat
- 1648-715x 2009 13 117-128 PDFDokumen13 halaman1648-715x 2009 13 117-128 PDFichaBelum ada peringkat
- Gambaran Lama Tidur Terhadap Prestasi Belajar SiswaDokumen7 halamanGambaran Lama Tidur Terhadap Prestasi Belajar SiswaichaBelum ada peringkat
- Pathogenic Escherichia Coli Associated With DiarrheaDokumen7 halamanPathogenic Escherichia Coli Associated With DiarrheaSiti Fatimah RadBelum ada peringkat
- Derivational and Inflectional Morpheme in English LanguageDokumen11 halamanDerivational and Inflectional Morpheme in English LanguageEdificator BroBelum ada peringkat
- Tese Beatbox - Florida PDFDokumen110 halamanTese Beatbox - Florida PDFSaraSilvaBelum ada peringkat
- Song Book Inner PagesDokumen140 halamanSong Book Inner PagesEliazer PetsonBelum ada peringkat
- Based On PSA 700 Revised - The Independent Auditor's Report On A Complete Set of General Purpose Financial StatementsDokumen12 halamanBased On PSA 700 Revised - The Independent Auditor's Report On A Complete Set of General Purpose Financial Statementsbobo kaBelum ada peringkat
- Chapter 5 Constructing An Agile Implementation PlanDokumen4 halamanChapter 5 Constructing An Agile Implementation PlanAHMADBelum ada peringkat
- 11.3.1 Some Special CasesDokumen10 halaman11.3.1 Some Special CasesSiddharth KishanBelum ada peringkat
- The New Order of BarbariansDokumen39 halamanThe New Order of Barbariansbadguy100% (1)
- Csir Life Sciences Fresh Instant NotesDokumen4 halamanCsir Life Sciences Fresh Instant NotesAlps Ana33% (3)
- CA21159 MG 8 Digital BookletDokumen5 halamanCA21159 MG 8 Digital BookletcantaloupemusicBelum ada peringkat
- Grammar and Vocabulary TestDokumen5 halamanGrammar and Vocabulary TestLeonora ConejosBelum ada peringkat
- Hockney-Falco Thesis: 1 Setup of The 2001 PublicationDokumen6 halamanHockney-Falco Thesis: 1 Setup of The 2001 PublicationKurayami ReijiBelum ada peringkat
- PM Jobs Comp Ir RandDokumen9 halamanPM Jobs Comp Ir Randandri putrantoBelum ada peringkat
- Reference Paper Literature ReviewDokumen5 halamanReference Paper Literature ReviewAani RashBelum ada peringkat
- Trina 440W Vertex-S+ DatasheetDokumen2 halamanTrina 440W Vertex-S+ DatasheetBrad MannBelum ada peringkat
- ABARI-Volunteer Guide BookDokumen10 halamanABARI-Volunteer Guide BookEla Mercado0% (1)
- Ch-10 Human Eye Notes FinalDokumen27 halamanCh-10 Human Eye Notes Finalkilemas494Belum ada peringkat
- Enlightened ExperimentationDokumen8 halamanEnlightened ExperimentationRaeed HassanBelum ada peringkat
- Chapter 10 Tute Solutions PDFDokumen7 halamanChapter 10 Tute Solutions PDFAi Tien TranBelum ada peringkat
- Highlights ASME Guides Preheat PWHT IDokumen4 halamanHighlights ASME Guides Preheat PWHT IArul Edwin Vijay VincentBelum ada peringkat
- GGG Sri MDokumen2 halamanGGG Sri MGiovanni LuigiBelum ada peringkat
- Caring For Women Experiencing Breast Engorgement A Case ReportDokumen6 halamanCaring For Women Experiencing Breast Engorgement A Case ReportHENIBelum ada peringkat
- D25KS Sanvick PDFDokumen4 halamanD25KS Sanvick PDFJiménez Manuel100% (1)
- Evidence Prove DiscriminationDokumen5 halamanEvidence Prove DiscriminationRenzo JimenezBelum ada peringkat
- Design of Reinforced Cement Concrete ElementsDokumen14 halamanDesign of Reinforced Cement Concrete ElementsSudeesh M SBelum ada peringkat
- Img 20150510 0001Dokumen2 halamanImg 20150510 0001api-284663984Belum ada peringkat
- AE Notification 2015 NPDCLDokumen24 halamanAE Notification 2015 NPDCLSuresh DoosaBelum ada peringkat
- PETAL Sentence StartersDokumen1 halamanPETAL Sentence StartersSnip x Hunt manBelum ada peringkat
- (20836104 - Artificial Satellites) Investigation of The Accuracy of Google Earth Elevation DataDokumen9 halaman(20836104 - Artificial Satellites) Investigation of The Accuracy of Google Earth Elevation DataSunidhi VermaBelum ada peringkat
- Coding Rubric Unifix XXXX 75Dokumen2 halamanCoding Rubric Unifix XXXX 75api-287660266Belum ada peringkat