Control of The Splanchnic Circulation in Man
Diunggah oleh
Muhammad ReyhanJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Control of The Splanchnic Circulation in Man
Diunggah oleh
Muhammad ReyhanHak Cipta:
Format Tersedia
Control of the Splanchnic Circulation in Man
ROLE OF BETA-ADRENERGIC RECEPTORS
By Henry L. Price, M.D., Lee H. Cooperman, M.D., and John C. Warden, M.B.
ABSTRACT
Some effects of the /3-adrenergic receptor blocker, propranolol, were studied
in 20 normal, fasting, conscious men. The measurements made included
cardiac output, splanchnic blood flow and oxygen consumption, arterial and
hepatic venous blood pressure, and heart rate. The intravenous administra-
tion of propranolol (0.13 mg/kg) was followed by significant reductions in
splanchnic blood flow and oxygen consumption, in cardiac output and in heart
rate. Splanchnic perfusion pressure was unchanged; the splanchnic vascular
resistance was significantly elevated. Previous treatment with glucose did not
alter these findings. Phenoxybenzamine prerreatment lessened the increase
in splanchnic vascular resistance which propranolol ordinarily caused. Ganglion-
ic blockade with hexamethonium prevented all of the changes which pro-
pranolol produced in untreated individuals. These results may best be ex-
plained by assuming that the splanchnic circulation in man is influenced both
by a receptors, which cause vasoconstriction when activated, and by /9 recep-
tors, which when activated cause vasodilatation and increase oxygen con-
sumption.
ADDITIONAL KEY WORDS propranolol hexamethonium
alpha-adrenergic receptor blockade splanchnic oxygen consumption
splanchnic vascular resistance phenoxybenzamine
beta-adrenergic receptor blockade
• One of us has reported (1) that the ad- these fibers caused vasodilation and stimu-
ministration of propranolol (a /3-adrenergic lation of metabolism. If this were true, the
receptor blocking drug of high specificity) increase in vascular resistance attending the
to human subjects anesthetized with cyclo- administration of propranolol could be ex-
propane caused a marked reduction in plained as the result of reducing or abolish-
splanchnic blood flow. This reduction resulted ing tonic /3-receptor stimulant activity which
from increased vascular resistance and was has, to date, remained undiscovered. In the
usually accompanied by a diminution in local experiments to be described, this possibility
oxygen consumption. Since cyclopropane is was examined and found to be likely.
believed to increase the impulse frequency
in sympathetic nerves supplying the abdom- Methods
inal viscera (2), these observations raised The subjects studied were 20 healthy, adult,
the question whether some of the activity of male volunteers. At preliminary meetings an in-
formed consent was obtained, a medical history
taken, and a physical examination, electrocardio-
From The Department of Anesthesia, University gram, urinalysis and blood count were performed.
of Pennsylvania, School of Medicine, Philadelphia, On the day of study, each subject reported to the
Pennsylvania 19104. laboratory in the early morning, having fasted
This work was supported in part by Public Health since the previous evening.
Service Grants GM-09070-05 and 5-T1-GM-215-O9 Under local anesthesia, a 100-cm no. 7 Lehman
from the National Institute of General Medical Sci- catheter was inserted into an antecubital vein and
ences and by a grant-in-aid from Ayerst Laboratories, advanced as far as possible into a right hepatic
Inc., New York. Dr. Cooperman is a Special Fellow
of the National Institutes of Health (1F3-GM-33-126-
vein and then withdrawn sufficiently (1-2 cm) to
01). Dr. Warden is the recipient of a travel grant from permit free aspiration of blood. In the opposite
the Postgraduate Medical Foundation, University of arm a 60-cm radiopaque no. 15 catheter, to be
Sydney, Sydney, Australia. used for dye injection, was inserted percutaneous-
Accepted for publication July 24, 1967. ly into a vein and positioned within the thorax.
Reiisrcb, Vol. XXI, Slplfrnilr 1967 333
Downloaded from http://circres.ahajournals.org/ by guest on March 8, 2015
334 PRICE, COOPERMAN, WARDEN
TABLE 1
General Hemodynamic Changes Following Treatment
Treatment Heart rate (beat'mimin)
Group Subject Ei Ei c Ei E-
I Propranolol
(0.13 mgAg)
3 57 53
4 61 57
5 52 48
6 64 56
32 73 65
Mean 61 56
Significance P < 0.01
II Glucose Propranolol
(20 to 30 g) (0.13 mgAg)
9 68 70 64
10 70 70 66
12 68 67 61
16 79 83 71
19 67 65 62
Mean 70 71 65
Significance P < 0.05
III Phenoxybenzamine Propranolol
(0.75 mgAg) (0.13 mgAg)
27 62 66 61
28 65 72 57
29 71 77 75
30 57 80 63
31 87 102 83
Mean 68 79 68
Significance P<0.05 P<0.05
IV Hexamethonium Propranolol
(0.85 mgAg) (0.13 mgAg)
11 69 84 83
17 63 102 87
18 69 93 87
20 64 95 83
22 86 105 98
Mean 70 96 88
Significance P < 0.01 P < 0.05
Abbreviations: TPR = . peripheral resistance; E2 and E2 = first and second experimental periods; C = control.
Significance: referred to column at left.
Placement of the two catheters was verified by Cardiac output was measured in duplicate by
image-intensification fluoroscopy. A Coumand the indicator-dilution technique using a Waters
needle was placed in the right femoral artery and densitometer and 5 or 10 mg of indocyanine
cup electrodes were fastened to the skin to permit green dye. Splanchnic blood flow was estimated
recording of the electrocardiogram. Arterial and by infusion of indocyanine green dye as described
hepatic venous pressures were transduced by by Caesar et al. (3) with corrections introduced
Statham strain gauges and recorded, with the by Nielsen (4). No subject extracted less than
electrocardiogram, on a Grass polygraph. Mean 5035 of arterial indocyanine gTeen dye in a single
pressures were obtained by electrical damping. hepatic passage. Splanchnic oxygen consumption
The reference level for pressure was 5 cm dorsal was estimated by multiplying blood flow and the
to the angle of Louis. arteriovenous oxygen content difference as meas-
CirfMon Riurcb, Vol. XXI, Stpumbtr 1967
Downloaded from http://circres.ahajournals.org/ by guest on March 8, 2015
CONTROL OF THE SPLANCHNIC CIRCULATION 335
Arterial pressure (nun HHf) Cardiac output (Uter/min) TPR (mm Hg/liter per rain)
c Ki Ei C Ei Ei C Ei Ei
87 94 6.25 4.78 13.3 20.5
80 77 5.19 5.10 15.9 15.7
70 75 6.01 5.30 12.0 14.1
91 95 5.07 4.45 18.8 21.3
75 76 4.63 5.87 15.1 13.6
80.6 83.9 5.43 5.10 15.0 17.1
85 87 87 5.68 4.93 15.0 17.3
90 95 90 6.98 5.68 13.6 15.9
87 89 92 8.04 6.25 11.8 14.5
80 83 83 7.73 5.37 10.3 15.5
75 75 75 7.08 4.88 10.6 15.7
83.4 85.8 85.9 7.10 5.42 12.3 15.8
P < 0.01 P < 0.01
76 74 72 6.74 5.60 11.1 13.4
80 68 76 7.56 9.18 6.58 10.3 7.1 6.5
75 75 68 6.30 8.97 6.60 11.9 8.4 10.3
82 74 70 4.66 7.51 4.88 16.1 7.3 13.3
87 75 74 7.05 7.23 7.06 12.8 10.4 10.4
80.0 73.2 72.0 6.39 7.93 6.14 12.8 8.9 10.8
F < 0.05 P < 0.05
85 83 82 5.34 5.62 15.9 15.1
86 77 75 7.52 7.00 11.0 10.3
73 58 71 7.19 9.40 10.4 7.8
85 69 65 7.11 5.84 12.7 11.1
74 67 69 6.75 7.50 10.4 9.7
80.6 70.6 72.4 6.78 7.07 12.1 10.8
P<0.05 P < 0.05
ured by the method of Van Slyke and Neill ( 5 ) . the pH of arterial and venous blood were meas-
Similar calculations were used for carbon dioxide ured using an Instrumentation Laboratories elec-
production. Splanchnic vascular resistance was cal- trode assembly model 113-S1. Blood glucose was
culated as perfusion pressure (mean arterial minus determined by an enzymatic method (6).
mean hepatic venous) divided by the mean rate During the 30-min study period, three deter-
of blood flow. Heart rate was counted from the minations of splanchnic blood flow and single
electrocardiogram. The hematocrit of arterial determinations of arterial and hepatic venous
blood was determined in capped Wintrobe Pco2, Po2) pH, O2 content and CO2 content were
tubes spun for 30 min at 2300 X g (at the tip). made. Glucose concentration was estimated in 15
Before analysis all blood samples were stored at individuals. Concentrations of epinephrine and
4°C. norepinephrine in arterial plasma were determined
The tensions of oxygen and carbon dioxide and in 11 cases by the method of Price and Price (7).
Restarcb, Vol. XXI, Stptmbtr 1967
Downloaded from http://circres.ahajournals.org/ by guest on March 8, 2015
336 PRICE, COOPERMAN, WARDEN
TABLE 2
Local Hemodynamics and Metabolic Changes Following Treatment
Perfuflion preuure (mm Hg) SBF (llter/min) SVR (mm He/liter per min)
Group Subject C Ei Ej c Ei Ei C Ei
i
3 86 91 1.55 .99 57 92
4 78 75 1.50 1.18 52 63
5 69 74 2.66 1.86 26 40
6 87 95 1.60 1.07 55 89
32 74 76 .92 .73 81 104
Mean 78.8 82.2 1.65 1.17 54.3 77.6
Significance P<0.05 P < 0.01
II
9 84 84 84 2.32 2.45 2.36 37 35
10 87 91 87 1.55 1.46 1.31 56 63
12 86 88 91 2.45 2.53 1.94 35 35
16 80 83 82 2.11 2.22 1.61 38 38
19 75 75 75 1.37 1.36 1.12 55 55
Mean 82.4 84.2 83.8 1.96 2.00 1.67 44.1 45.1
Significance P < 0.05
m 53
27 73 73 70 1.68 1.40 1.24 43
28 77 65 75 2.32 1.80 1.27 34 38
29 72 74 66 1.23 1.36 1.07 59 55
30 79 74 70 1.07 1.18 1.04 74 62
31 84 74 74 1.90 1.82 1.42 44 41
Mean 77.0 72.0 71.0 1.64 1.51 1.21 50.0 49.8
Significance P<0.05
IV
11 84 82 82 2.90 2.86 2.73 29 29
17 84 77 75 2.42 1.90 1.46 35 40
18 72 58 71 2.13 1.83 2.27 34 31
20 85 69 65 1.74 1.46 1.27 49 47
22 74 67 69 3.58 2.43 2.64 22 27
Mean 79.8 70.6 72.4 2.56 2.10 2.07 33.7 35.0
Significance P<0.05 P < 0.05
Perfusion pressure — mean arterial minus mean hepatic venous pressure; SBF = splanchnic blood flow; SVR =
splanchnic vascular resistance (perfusion pressure/splanchnic blood flow); Qo2 = splanchnic oxygen consumption, ?yo2 =
hepatic venous oxygen tension; RQ = respiratory quotient; and others as in Table 1.
The indocyanine green dye clearance technique received 300 ml of 10* glucose solution (one half
estimates hepatic blood flow directly since the as a rapid intravenous infusion and the remainder
liver is the only organ capable of removing the slowly during the remainder of the study). Five
dye from the circulation. The metabolic measure- subjects received hexamethonium (0.5 mg/kg in
ments, however, apply to the entire splanchnic divided doses). A final 5 subjects were given phen-
area, i.e. those viscera (liver, stomach, pancreas, oxybenzamine (0.7 mg/kg) by an infusion dur-
gallbladder, small intestine, large intestine above ing a 20-min period followed by a 40-min wait
the sigmoid colon and spleen) from which venous (to permit maximal action of the drug to occur).
drainage eventually enters the hepatic vein. In addition, all subjects received approximately
Following the control period, the first 5 subjects 200 ml of 0.9* NaCl solution to replace blood
were given propranolol1 (0.13 mg/kg iv) over a taken in sampling. The dose of propranolol se-
10-min period after which the measurements de- lected is the same as that used in our previous
tailed above were repeated. Five other individuals study (1); that of phenoxybenzamine was the
largest amount which could be tolerated consis-
tently without the occurrence of fainting. The last
iKindly supplied by Dr. Sahagian-Edwards of 15 individuals were subjected to three study
Ayerst Laboratories. periods, namely, (1) control, (2) following treat-
CtrcvUtion Rtsurcb, Vol. XXI, September 1967
Downloaded from http://circres.ahajournals.org/ by guest on March 8, 2015
CONTROL OF THE SPLANCHNIC CIRCULATION 337
Qo, (mj/min) P TOJ (mm Hg) RQ
EJ c Ei Ei c Ei Ei C Ei Ei
75 62 34 33 0.00 0.10
65 64 42 45 0.59 0.17
84 70 41 43 0.42 0.55
84 63 43 43 -0.75 0.23
46 41 39 34 0.50 0.74
70.6 60.0 39.8 39.6 -0.09 0.36
P < 0.05 P < 0.05
36 44 45 37 45 44 49 -0.16 0.00 0.00
67 72 71 59 37 34 43 0.48 0.75 0.68
47 122 76 66 49 42 43 0.61 0.65 0.51
51 53 63 41 44 48 48 0.40 0.65 0.41
67 48 48 44 41 42 42 0.12 0.42 0.19
53.6 67.8 60.4 49.3 41.5 41.9 44.9 0.29 0.49 0.36
P < 0.05 P < 0.05 P<0.05 P<0.05
57 72 71 60 41 40 37 0.46 0.58 0.51
59 62 77 55 46 37 40 0.37 0.20 0.83
62 42 50 40 45 46 45 0.13 0.13 0.62
68 61 53 56 37 39 38 0.40 0.49 0.69
52 49 69 50 49 45 46 0.11 0.86 0.58
59.4 57.1 63.9 52.2 43.6 41.3 41.1 0.29 0.45 0.65
P < 0.05 P < 0.05
30 68 64 61 52 56 56 -0.51 -2.01 -1.14
52 81 46 45 44 44 41 -0.14 -0.17 -0.01
32 72 48 70 41 43 38 0.50 -0.08 0.30
51 68 88 69 40 36 36 0.04 0.36 0.68
26 74 82 55 49 42 46 0.46 0.84 0.26
38.1 72.5 65.5 60.0 45.5 44.0 43.3 0.07 -0.21 0.02
ment with glucose, hexamethonium or phenoxy- ing subjects (group I) was followed by a
benzamine and (3) after administration of reduction in splanchnic blood flow, oxygen
propranolol. This sequence was followed to deter-
mine both the effects of glucose, hexamethonium consumption, and indocyanine green dye
or phenoxybenzamine and any modification of the clearance. Heart rate also was reduced. Cal-
response to propranolol which the previous treat- culated splanchnic vascular resistance in-
ment might effect. creased, as did the splanchnic respiratory
The data were analyzed for statistical signifi- quotient, but perfusion pressure (mean ar-
cance using paired f-tests where applicable (Ta-
bles 1 and 2); for unpaired data a nonpaired
terial minus mean venous) was unaltered.
f-test was used (Table 3). Cardiac output was reduced in 4 of 5 sub-
jects.
Results An infusion of glucose (group II) had no
The principal results are shown in Tables apparent effect, except to increase respira-
1 and 2. In Table 2 each value for flow, re- tory quotient, and the subsequent administra-
sistance, and perfusion pressure is an average tion of propranolol caused the same direc-
of three individual determinations. In brief, tional changes as in the absence of previous
the administration of propranolol to the fast- treatment with glucose, except that respira-
CircuUtion Resttrch, Vol. XXI, Stfumbtr 1967
Downloaded from http://circres.ahajournals.org/ by guest on March 8, 2015
338 PRICE, COOPERMAN, WARDEN
TABLE 3
Effect of Previous Treatment on Changes following Propranold Administration
SBF (liter/into) SVR (mm Hg'Hterper per min) PTOI t(mm Hg)
None Cyclo PBZ None Cyclo PBZ None Cyclo PBZ
Previous treatment
Initial value 1.65 1.29 1.51 54 80 50 40 44 41
After propranolol 1.17 0.61 1.21 77 133 60 40 28 41
Change 0.48 0.68 0.30 23 53 10 0 16 0
SE 0.11 0.13 0.07 5 14 3 1.2 3.2 1.3
Significance P<0.05 P<0.05 p <0.01 P < 0.01 P < 0.001
Abbreviations: Cyclo = subjects anesthetized with cycloproprane; PBZ = subjects who had previous treatment
with phenoxybenzamine; others as in Table 2.
Significance: referred to control.
tory quotient did not increase further in re- mine, or propranolol. During glucose admin-
sponse to the blocking agent. Comparison of istration the concentration in arterial blood
the magnitude of the various responses to averaged 147 mg per 100 ml of blood. The
propranolol showed no other significant dif- hepatic extraction of indocyanine green dye
ference depending upon previous treatment was unaltered by any of the drugs which were
except that the increase in splanchnic vascu- administered or by glucose.
lar resistance was less (P<0.01).
Phenoxybenzamine (group III) had no Discussion
apparent initial effect except to increase heart These results suggest that the splanchnic
rate. It apparently altered the response to vasculature in man is influenced by sympa-
propranolol as follows: (1) the respiratory thetic nerves which contain vasodilator as
quotient was still increased, but no longer well as vasoconstrictor fibers, or by identical
consistently so, (2) the increase in splanch- fibers which have both effects, depending
nic vascular resistance was smaller (P < upon whether a- or /J-receptors are activated.
0.001), and (3) the reduction in blood flow Our evidence for this is as follows:
was less (P<0.05). First, propranolol is an exceptionally spe-
In contrast, hexamethonium pretreatment cific /3-receptor blocker and is apparently de-
(group IV) apparently prevented all of the void of direct sympathomimetic or vascular
actions of propranolol that were observed in actions (8, 9). Among its effects in this study
the untreated subjects and in those who re- were an increase in splanchnic vascular re-
ceived either the glucose or the phenoxy- sistance and a reduction in blood flow and
benzamine pretreatment. The direct actions oxygen consumption. The present results
of hexamethonium were to reduce splanchnic (group IV) support the conclusion that these
indocyanine green dye clearance, perfusion actions depend upon the presence of tonic
pressure, and blood flow. sympathetic nervous activity, (i.e. are not
In no subject was an elevated concentra- caused by nonspecific drug actions). A pos-
tion of a catecholamine detected in arterial sible exception to this statement would occur
plasma; the levels in the fasting subjects if propranolol, like certain a-receptor block-
ranged from zero to 0.12 fig/liter epinephrine ing agents, interfered with the uptake and
and from zero to 0.48 /Ag/liter norepineph- restorage of the norepinephrine liberated up-
rine. Pao2 ranged from 73 to 107 mm Hg and on the arrival of nervous impulses at sym-
Paco2 from 34 to 45 mm Hg. Arterial glucose pathetic nerve terminals. This possibility has
concentrations ranged from 76 to 110 mg per not yet been examined, but it is believed to
100 ml of blood before treatment and were be unlikely.
unaffected by hexamethonium, phenoxybenza- Second, propranolol can exert its effect in
CiraiUtio* Rtstarcb, Vol. XXI, Sfpttmttr 1967
Downloaded from http://circres.ahajournals.org/ by guest on March 8, 2015
CONTROL OF THE SPLANCHNIC CIRCULATION 339
the presence of a-receptor blockade. Al- These differences are reflected in quantitative-
though we have no proof that a-receptor ly similar reductions in splanchnic blood flow.
blockade was total and complete this finding It is of interest that the hepatic venous oxy-
apparently rules out the possibilities that pro- gen tension, while insignificantly affected by
pranolol acts only directly (via a-receptor propranolol in fasting, conscious subjects, was
stimulation) or that it acts only reflexly (via conspicuously diminished in those receiving
increased a-adrenergic nervous activity). cyclopropane to a mean level approximat-
Third, there was no detectable level of ing 30 mm Hg. From the standpoint of
epinephrine in the plasma of our subjects. The splanchnic oxygen availability, it may be un-
method used can detect a concentration of wise to administer a y8-receptor blocking
0.1 /ig/liter in plasma which corresponds to agent when sympathetic nervous outflow is
a secretion rate of about 0.1 /tg/min, an augmented.
amount believed to be physiologically insig- The existence of both a- and /3-recep-
nificant (10). The rate at which norepineph- tors in the splanchnic viscera could also
rine is secreted from the adrenal medulla in explain the curious result (12) that hemor-
resting man is also believed to be physiologi- rhage, although undoubtedly increasing sym-
cally insignificant (10) and, moreover, the ef- pathetic nervous activity, may not increase
fect of infusing norepinephrine intravenously splanchnic vascular resistance. Although it is
is to cause splanchnic vasoconstriction, not stated that sympathetic vasodilator fibers do
dilatation (11). The effect of giving propran- not supply the splanchnic viscera (13, 14)
olol consequently could not have depend- the evidence for this statement is not con-
ed upon blocking an action mediated via cir- vincing.
culating catecholamines. Since the vasodilator effects of y3-receptor
Although a-receptor blockade did not sup- activation are accompanied by metabolic al-
press the response of the splanchnic vascula- terations, we were not surprised to find that
ture to propranolol, it did reduce it, and this the increase in splanchnic vascular resistance
would favor either the existence of a tonical- caused by propranolol was accompanied by
ly active sympathetic vasoconstrictor pathway metabolic changes. In particular, ^-receptor
in our subjects at rest or the reflex activation blockade resulted in a reduced splanchnic
of a-receptors by propranolol. It is interesting oxygen consumption and an increased re-
that in the previous study (1) performed in spiratory quotient. Splanchnic oxygen ex-
5 anesthetized subjects, who had an abnor- traction and the Po^ of hepatic venous blood
mally elevated level of sympathetic tone, the in our normal, unanesthetized subjects were
administration of propranolol caused a unaltered by propranolol, suggesting that the
significantly greater increase in splanchnic reduction in splanchnic blood flow resulted
vascular resistance than it did in the present from a quantitatively similar diminution in
investigation. Table 3 compares the effects oxygen demand.
of propranolol on splanchnic vascular re- It has been estimated that roughly 80* of
sistance, splanchnic blood flow and venous the oxygen consumed by the liver is used to
oxygen tension in three groups of individuals oxidize free fatty acids (15). Since the rate
studied by us who (presumably) had differ- at which free fatty acids are oxidized depends
ent initial levels of sympathetic tone. The directly upon their concentration in plasma
data recorded during administration of cyclo- (16), it is not unreasonable to expect that an
propane were obtained in an earlier study agent, such as propranolol, which blocks the
(1), but have not previously been fully re- mobilization of free fatty acids (17, 18) will
ported. The increase in resistance on giving reduce hepatic oxygen consumption. In addi-
propranolol is significantly augmented by cy- tion, the presence of circulating free fatty
cloproprane administration and reduced by acids causes inhibition of pyruvate kinase,
previous treatment with phenoxybenzamine. thus leading to gluconeogenesis (19). For this
CircuUtio* Rtis+rcb, Vol. XXI, Sepltmbtr 1967
Downloaded from http://circres.ahajournals.org/ by guest on March 8, 2015
340 PRICE, COOPERMAN, WARDEN
reason the hepatic respiratory quotient should man and canine plasma. II. A critique of the
be reduced by the presence of free fatty acids trihydroxyindole method. J. Lab. Clin. Med.
50: 769, 1957.
and increased by any inhibition of free fatty
8. SHANKS, R. G.: Pharmacology of beta sympa-
acid mobilization. Thus, not only the circula- thetic blockade. Am. J. Cardiol. 18: 308, 1966.
tory, but also the metabolic, effects of propran- 9. BRICK, I., GLOVER, W. E., HUTCHISON, K. J.,
olol may best be explained as consequences of AND RODDA, I. C : Effects of propranolol on
the interruption of a tonic /} activity. peripheral vessels in man. Am. J. Cardiol. 18:
With respect to the low splanchnic re- 329, 1966.
spiratory quotient values that we observed, our 10. PRICE, H. L.: Circulating adrenaline and nor-
results resemble those of Rowell and co-work- adrenaline during diethyl ether anaesthesia in
man. Clin. Sci. 16: 377, 1957.
ers (20). It is possible that ketosis accounts
11. BEARN, A. C , BUXTNG, B., AND SHERLOCK, S.:
in part for this finding, since the formation Effect of adrenaline and noradrenaline on
of ketones from free fatty acids requires oxy- hepatic blood flow and splanchnic carbohy-
gen but does not produce carbon dioxide. The drate metabolism in man. J. Physiol. (London)
effects of glucose and propranolol on this 115: 430, 1951.
ratio were those to be expected. We cannot 12. PRICE, H. L., DEUTSCH, S., MARSHALL, B. E.,
STEPHEN, G. W., BEHAR, M. G., AND NEU-
explain the occasional apparent uptake of
FELD, G. R.: Hemodynamic and metabolic
carbon dioxide by the splanchnic viscera, a effects of hemorrhage in man, with particular
phenomenon also noted by Rowell et al. reference to the splanchnic circulation. Circu-
lation Res. 18: 469, 1966.
References 13. UVNAS, B.: Central cardiovascular control. In
Handbook of Physiology, sec. I, vol. 2. Wash-
1. PRICE, H. L., DEUTSCH, S., DAVIDSON, I. A., ington, D. C , American Physiological Society,
CLEMENT, A. J., BEHAR, M. C , AND EPSTEIN, 1960, p. 1136.
R. M.: Can general anesthetics produce splanch- 14. GHAYSON, J., AND MENDEL, D.: Physiology of the
nic visceral hypoxia by reducing regional blood Splanchnic Circulation. Baltimore, Williams and
flow? Anesthesiology 27: 24, 1966. Wilkins, 1965, p. 91.
2. PRICE, H. L., DEUTSCH, S., COOPERMAN, L. H., 15. LUNDQUIST, F.: Metabolism of carbohydrates in
CLEMENT, A. J., AND EPSTEIN, R. M.: Splanch- the normal liver and under the influence of
nic circulation during cyclopropane anesthesia ethanol and hormones. Scand. J. Lab. Clin.
in normal man. Anesthesiology 26: 312, 1965. Invest. 18 (suppl. 92): 47, 1966.
3. CAESAR, J., SHALDON, S., CHIANDUSSI, L., GUE- 16. STEINBERG, D.: Catecholamine stimulation of fat
VARA, L., AND SHERLOCK, S.: Use of indocya- mobilization and its metabolic consequences.
nine green in the measurement of hepatic blood Pharmacol. Rev. 18: Parti, 217, 1966.
flow and as a test of hepatic function. Clin. 17. NAKANO, J., KUSAKARI, T., AND BERRY, J. L.:
Sci. 21: 43, 1981. Effects of propranolol on the circulatory
4. NIELSEN, N. C : Spectrophotometric determina- changes and mobilization of free fatty acids
tion of indocyanine green in plasma especially by isoproterenol. Arch. Intern. Pharmacodyn.
with a view to an improved correction for 164: 120, 1966.
blank density. Scand. J. Clin. Lab. Invest. 15: 18. Mum, G. G., CHAMBERLAIN, D. A., AND PEDOE,
613, 1963. D. T.: Effects of /9-sympathetic blockade on
non-esterified-fatty-acid and carbohydrate me-
5. VAN SLYKE, S. D., AND NETLL, J. A.: Determina-
tabolism at rest and during exercise. Lancet
tion of gases in blood and other solutions by 1: 930, 1964.
vacuum extraction and manometric measure-
19. WEBER, G., CONVERY, H. J. H., LEA, M. A.,
ments. J. Biol. Chem. 61: 523, 1924.
AND STAURM, N. B.: Feedback inhibition of
6. BERCMEYER, H., AND BERNT, E.: D-glucose. De- key glycolytic enzymes in liver: action of free
termination with glucose oxidase and peroxi- fatty acids. Science 154: 1357, 1966.
dase. In Methods of Enzymatic Analysis, edited
20. ROWELL, L. B., KRANING, K. K., EVANS, T. O.,
by H. Bergmeyer. New York, Academic Press, KENNEDY, J. W., BLACKMAN, J. R., AND KU-
1963. SUMI, F.: Splanchnic removal of lactate and
7. PRICE, H. L., AND PRICE, M. L.: Chemical estima- pyruvate during prolonged exercise in man.
tion of epinephrine and norepinephrine in hu- J. Appl. Physiol. 21: 1773, 1966.
OrcuUtion Rtiarcb, Vol. XXI, Stpttmbtr 1967
Downloaded from http://circres.ahajournals.org/ by guest on March 8, 2015
Control of the Splanchnic Circulation in Man: ROLE OF BETA-ADRENERGIC
RECEPTORS
HENRY L. PRICE, LEE H. COOPERMAN and JOHN C. WARDEN
Circ Res. 1967;21:333-340
doi: 10.1161/01.RES.21.3.333
Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1967 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7330. Online ISSN: 1524-4571
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circres.ahajournals.org/content/21/3/333
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further information
about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation Research is online at:
http://circres.ahajournals.org//subscriptions/
Downloaded from http://circres.ahajournals.org/ by guest on March 8, 2015
Anda mungkin juga menyukai
- SOCIETY For ENDOCRINOLOGY ENDOCRINE EMERGENCY GUIDANCE - Emergency Management of Acute Adrenal Insufficiency (Adrenal Crisis) in Adult PatientsDokumen3 halamanSOCIETY For ENDOCRINOLOGY ENDOCRINE EMERGENCY GUIDANCE - Emergency Management of Acute Adrenal Insufficiency (Adrenal Crisis) in Adult PatientsMuhammad ReyhanBelum ada peringkat
- Wounds in GeneralDokumen19 halamanWounds in GeneralMuhammad ReyhanBelum ada peringkat
- Radiological Signs of Lobar Collapse. Chest Radiographic Findings and CT ImagesDokumen38 halamanRadiological Signs of Lobar Collapse. Chest Radiographic Findings and CT ImagesMuhammad ReyhanBelum ada peringkat
- Exercise and Older Patients - Prescribing Guidelines PDFDokumen8 halamanExercise and Older Patients - Prescribing Guidelines PDFMuhammad ReyhanBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1091)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Tablas de Presión ArterialDokumen2 halamanTablas de Presión Arterialwasserpura100% (1)
- Dicionario NihonDokumen10 halamanDicionario NihonMario GuedesBelum ada peringkat
- Home Blood Pressure DiaryDokumen2 halamanHome Blood Pressure DiaryCherieBelum ada peringkat
- 2015 Book HandbookOfCardiacAnatomyPhysio PDFDokumen806 halaman2015 Book HandbookOfCardiacAnatomyPhysio PDFChema Sánchez100% (2)
- Project #7 - HypertensionDokumen2 halamanProject #7 - HypertensionKPBelum ada peringkat
- Ezpap - Effects of EzPAP Post Operatively in Coronary Artery Bypass Graft PatientsDokumen1 halamanEzpap - Effects of EzPAP Post Operatively in Coronary Artery Bypass Graft Patientsjesushenandez_ftrBelum ada peringkat
- STENTSDokumen260 halamanSTENTSRoberto J. Santos RibeiroBelum ada peringkat
- Rules For EKG StripsDokumen5 halamanRules For EKG StripsjessiBelum ada peringkat
- 30 Dec JoBs BY KHALIQ HASSAN - Watermarked PDFDokumen4 halaman30 Dec JoBs BY KHALIQ HASSAN - Watermarked PDFKamran Talpur100% (1)
- Department of Internal Medicine: Manila Doctors HospitalDokumen5 halamanDepartment of Internal Medicine: Manila Doctors HospitalFayeListanco100% (1)
- 2015 American Heart Association Guidelines Update For CPR and ECCDokumen32 halaman2015 American Heart Association Guidelines Update For CPR and ECCVauFauziah100% (2)
- Tetralogy of FallotDokumen18 halamanTetralogy of FallotAaronMaroonFive100% (1)
- Mitral Valve Disease Information Sheet-1Dokumen6 halamanMitral Valve Disease Information Sheet-1Ionela OprescuBelum ada peringkat
- Blood Pressure ChartDokumen5 halamanBlood Pressure ChartAnonymous LiddTaTaZTBelum ada peringkat
- Echocardiographic Features of Total Anomalous Pulmonary: VenousDokumen8 halamanEchocardiographic Features of Total Anomalous Pulmonary: VenousTanuj VermaBelum ada peringkat
- Diabetes and HypertensionDokumen196 halamanDiabetes and HypertensionMed Aj100% (1)
- Drugs Affecting BPDokumen36 halamanDrugs Affecting BPm1k0eBelum ada peringkat
- Allen: Transportation in Plants and AnimalsDokumen12 halamanAllen: Transportation in Plants and AnimalsAnant DwivediBelum ada peringkat
- MRCP Passmedicine Part II 2017Dokumen8.783 halamanMRCP Passmedicine Part II 2017Prakash MahatoBelum ada peringkat
- Case Presentation 2Dokumen27 halamanCase Presentation 2Sathish SPBelum ada peringkat
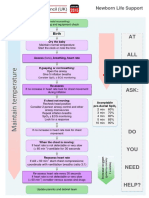
- Neonatal Life Support UK Ressusstation Council G2015 - NLSDokumen1 halamanNeonatal Life Support UK Ressusstation Council G2015 - NLSBharat Kumar SharmaBelum ada peringkat
- Lec Activity11 and 13 Blood Blood VesselDokumen2 halamanLec Activity11 and 13 Blood Blood Vesselapple BananaBelum ada peringkat
- Catheter Ablation For Atrial Fibrillation: Original ArticleDokumen7 halamanCatheter Ablation For Atrial Fibrillation: Original ArticleGavin WinkelBelum ada peringkat
- Vena Contracta Width Is A Semi-Quantitative Parameter To Assess The Severity of Mitral RegurgitationDokumen20 halamanVena Contracta Width Is A Semi-Quantitative Parameter To Assess The Severity of Mitral Regurgitationalex leeBelum ada peringkat
- HypoxemiaDokumen3 halamanHypoxemiaMark Angelo ChanBelum ada peringkat
- Normal ECGDokumen2 halamanNormal ECGGeneon100% (1)
- How To Do Internal Jugular Vein Cannulation - Critical Care Medicine - MSD Manual Professional EditionDokumen9 halamanHow To Do Internal Jugular Vein Cannulation - Critical Care Medicine - MSD Manual Professional EditionnaveenBelum ada peringkat
- Essentials of Cardiopulmonary Physical Therapy 4th Edition Hillegass Test BankDokumen10 halamanEssentials of Cardiopulmonary Physical Therapy 4th Edition Hillegass Test Banknancycarrollaocprizwen100% (9)
- Dental Management Medically Compromised Patient 9th Little Test BankDokumen5 halamanDental Management Medically Compromised Patient 9th Little Test BankSaifoqq100% (1)
- Post-Test - Google FormsDokumen18 halamanPost-Test - Google FormsTrixia AlmendralBelum ada peringkat