Cardiometabolic Health in Adults Born Premature With Extremely Low Birth Weight
Diunggah oleh
Shilvia Adita PutriJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Cardiometabolic Health in Adults Born Premature With Extremely Low Birth Weight
Diunggah oleh
Shilvia Adita PutriHak Cipta:
Format Tersedia
Cardiometabolic Health in
Adults Born Premature With
Extremely Low Birth Weight
Katherine M. Morrison, MD,a Laura Ramsingh, MSc,a Elizabeth Gunn, MSc,a David Streiner, PhD,b Ryan Van
Lieshout, MD, PhD,b Michael Boyle, PhD,b Hertzel Gerstein, MD,c Louis Schmidt, PhD,d Saroj Saigal, MDa
BACKGROUND: Young adults born with extreme prematurity have increased blood pressure and abstract
insulin resistance. This study documents their metabolic health as they enter their fourth
decade of life. The study objective was to compare body composition, glycemia, lipid levels,
and blood pressure in adults born with extremely low birth weight (ELBW) versus age- and
sex- matched normal birth weight (NBW) control subjects and to examine related previous
and current exposures.
METHODS: The study examines one of the oldest regionally representative cohorts of ELBW
subjects (birth weight <1 kg) and NBW individuals born between 1977 and 1982. The
primary outcome was dysglycemia (type 2 diabetes or prediabetes) based on results of a
75-g oral glucose tolerance test. Secondary outcomes include body composition, insulin
resistance, fasting lipid profile, and blood pressure. Potential predictive factors included
birth weight, maternal antenatal corticosteroid exposure, retinopathy of prematurity,
growth parameters, and smoking history.
RESULTS: Adults (mean age, 31.8 years) born ELBW (n = 100) had a higher percent body fat (P
= .004) and lower lean mass for height (P = .018) but similar waist circumference (P = .54)
and BMI (P = .61) compared with NBW control subjects. ELBW adults had a 4.0-fold (95%
confidence interval, 1.53–10.66) increased risk of developing dysglycemia. Adults born
ELBW also had higher systolic (P = .004) and diastolic (P = .02) blood pressures compared
with NBW control subjects, but there were no differences in lipid profile.
CONCLUSIONS: By their fourth decade, these adults born extremely premature had increased
body fat, lower lean mass, and a 4-fold increased risk of developing dysglycemia.
Departments of aPediatrics, bPsychiatry and Behavioural Neurosciences, cMedicine, and dPsychology,
WHAT’S KNOWN ON THIS SUBJECT: Survivors of
Neuroscience and Behaviour, McMaster University, Hamilton, Ontario, Canada extreme prematurity have increased blood pressure
and higher insulin resistance by the third decade of
Dr Morrison oversaw the study design, contributed to data acquisition and analysis, and wrote life.
and edited the manuscript; Ms Ramsingh contributed to study design and study conduct, wrote
the first draft of parts of the manuscript, and critically reviewed the manuscript; Ms Gunn WHAT THIS STUDY ADDS: In the fourth decade of
contributed to data acquisition and data analysis, wrote parts of the manuscript, and critically life, extremely low birth weight survivors were at
reviewed the manuscript; Dr Streiner contributed to study design and analysis and critically increased risk of developing dysglycemia and had
reviewed the manuscript; Dr Van Lieshout contributed to the conduct of the study and critically higher body fat and lower lean mass for height than
reviewed the manuscript; Dr Gerstein contributed to study design and critically reviewed the normal birth weight control subjects.
manuscript; Drs Schmidt and Boyle contributed to study design, conduct of the study, and critical
review of the manuscript; Dr Saigal initiated and oversaw the establishment and follow-up of
the cohort, contributed to study design and conduct of the study, and critically reviewed the
manuscript; and all authors approved the final version of the manuscript as submitted.
To cite: Morrison KM, Ramsingh L, Gunn E, et al.
DOI: 10.1542/peds.2016-0515 Cardiometabolic Health in Adults Born Premature With
Accepted for publication Jul 1, 2016 Extremely Low Birth Weight. Pediatrics. 2016;138(4):
e20160515
Downloaded from by guest on October 2, 2016
PEDIATRICS Volume 138, number 4, October 2016:e20160515 ARTICLE
Epidemiologic evidence linking NBW. The ELBW group comprised glucose level, I0 is the fasting plasma
low birth weight to subsequent individuals who weighed 501 to insulin value, and 22.5 is a constant.
cardiometabolic disorders has led 1000 g at birth and were recruited Participants were classified as
to the developmental origins of to a population-based study in normoglycemic or dysglycemic based
health and disease hypothesis.1 a geographically defined region on their fasting and 2-hour blood
This hypothesis suggests that of central-west Ontario, Canada, glucose levels and Canadian Diabetes
developmental stress experienced between 1977 and 1982. They have Association criteria.13 Dysglycemia
by an individual either prenatally or been followed up longitudinally included impaired fasting glucose
in early life encourages compensatory since birth, and health outcomes in (IFG), impaired glucose tolerance
mechanisms that aid survival in the survivors have been reported at 3, (IGT), IFG + IGT, or type 2 diabetes
short term but can have deleterious 5, and 8 years of age; at adolescence (T2DM) (IFG fasting glucose level,
impacts later in the life course. (12–16 years of age); and at young 6.1–6.9 mmol/L; IGT, 2-hour blood
Furthermore, low birth weight as a adulthood (22–26 years of age). glucose between 7.8 and11.0
result of preterm birth (<37 weeks’ The age-, sex-, and socioeconomic- mmol/L; T2DM, fasting glucose ≥7.0
gestation) is also associated with matched NBW group was identified mmol/L and/or 2-hour blood glucose
increased risk of cardiometabolic at 8 years of age. Similar to the ELBW ≥11.1 mmol/L). Those who self-
disturbances in childhood and in survivors, these children have been reported the diagnosis of preexisting
adulthood,2 including insulin resistance studied at 8 years, adolescence, and diabetes and were taking insulin
and increased blood pressure (BP). young adulthood. and/or oral hypoglycemic agents
In studies utilizing administrative did not complete an oral glucose
data, preterm birth is associated with Ethics tolerance test and were classified as
a 1.5- to 2-fold increased prevalence The study was approved by the joint having T2DM.
of diabetes by late middle age.3–5 The Research Ethics Board of McMaster
first generation of extremely low University and Hamilton Health Anthropometrics and Body Composition
birth weight (ELBW) infants who Sciences. Participants provided
Standing height was measured by
received neonatal intensive care is informed, signed consent.
using a Harpenden stadiometer
now entering their fourth decade of
Visits and Measurement (London, England). Weight was
life, and data on their long-term health
obtained by using an electronic
issues remain scarce. Higher BP and Data collection occurred at a single scale. Waist circumference (WC)
insulin resistance have been reported study visit scheduled in the morning was measured to the nearest 0.1 cm
in children,6 adolescents,7 and young after an 8- to 12-hour fast. by using a nonstretchable standard
adults8–10 born premature.11 Little is
Glucose Metabolism tape measure attached to a spring
known of later health outcomes.
balance exerting a force of 750 g.
The McMaster ELBW cohort is a Participants completed a 75-g oral
The measurement was taken over
population-representative cohort of glucose tolerance test with glucose
an unclothed abdomen at the
individuals born ELBW between1978 and insulin measured at baseline
smallest diameter between the costal
and 1982 and followed up since and after 120 minutes and analyzed
margin and the iliac crest. Three
birth and a matched, normal birth at Hamilton Health Sciences CORE
measurements of height, weight,
weight (NBW) control group. Laboratories (Hamilton, Ontario,
and WC were taken and averaged.
Periodic assessments of this cohort Canada). The insulin assay was the
BMI was calculated by using average
have contributed a great deal to our Abbott Diagnostics (Mississauga,
measurements of height and weight.
understanding of the implications Ontario, Canada) assay run on
of extreme preterm birth.12 The an i1000 analyzer (coefficient of Body composition was assessed
objectives of the present study were to variation, 1.9%–2.4%). Glucose by using dual-energy radiograph
evaluate cardiometabolic health in the metabolism was evaluated according absorptiometry on a GE Lunar
ELBW survivors compared with the to insulin resistance (homeostasis Prodigy Advance (Model #8743)
NBW group early in the fourth decade model assessment of insulin scanner (GE Healthcare, Mississauga,
of life and to identify related factors. resistance [HOMA-IR]) and glycemic Ontario, Canada). The dual-energy
status. HOMA-IR is widely used in radiograph absorptiometry method
clinical and epidemiologic studies is quick and of low health risk
METHODS to estimate insulin resistance. It is (radiation exposure <1 μSv or
calculated by using fasting glucose 1/100th of the radiation exposure
Participants and insulin levels with the following of a chest radiograph). It provides a
This longitudinal cohort included formula: HOMA-IR = G0 × I0/22.5, whole body scan and measurements
individuals born with ELBW and with where G0 is the fasting plasma of total body fat and fat free mass
Downloaded from by guest on October 2, 2016
2 MORRISON et al
(ie, lean mass). Total lean mass for SPSS Statistics, IBM Corporation, Imputation of Missing Data
each participant was adjusted for Armonk, NY). An α of P ≤.05 was
For individuals who did not attend
current adult height by calculating considered statistically significant.
this visit but were seen at the 24-year
the lean mass index (LMI = total lean To address our primary questions
visit, the data were also imputed
mass/height). We report body fat as related to differences in prevalence
by using the fully conditional
percent fat and as the fat mass index of dysglycemia and body composition
specification (Markov chain Monte
(FMI = total fat mass/height). between the ELBW and NBW groups,
Carlo) procedure in SPSS version
independent t tests for continuous
Current Health 22. Group membership, sex, height,
variables and χ2 tests for categorical
weight, self-reported diabetes,
After anthropometric measurements variables were used. To examine the
and estimated household income
were taken and before blood influence of being born appropriate
were used at the 24-year visit (all
sampling, BP was measured by using for gestational age compared with
data were available) to develop the
a BpTRU device (BpTRU Medical SGA, a 2-way analysis of variance
imputed data sets. The following
Devices, Coquitlam, BC, Canada) with was used.
variables were imputed: fasting
the participant seated and with an and 2-hour glucose level from the
appropriate-sized cuff. Categorization Univariate regression analysis was oral glucose tolerance test and
of prehypertension (systolic BP of used to analyze the contribution classification of prediabetes (IGT ±
120–139 mm Hg or diastolic BP of of predictors of insulin resistance IFG), T2DM and dysglycemia status,
80–89 mm Hg) and hypertension and fasting and 2-hour blood BP, and socioeconomic status at the
(systolic BP ≥140 mm Hg and/ glucose. Predictors included age, time of study visit. The minimum
or diastolic BP ≥90 mm Hg) was sex, socioeconomic status (at age and maximum constraints placed on
according to the Seventh Report of 8 years and in adulthood), BMI, WC, the imputed values of the following
the Joint National Committee on the total percent body fat, FMI, LMI, variables were as follows: systolic BP,
Prevention, Detection, Evaluation, and birth weight, birth weight group, minimum of 80 mm Hg; diastolic BP,
Treatment of High Blood Pressure.14 weight change from birth to 8 years minimum of 45 mm Hg and maximum
of age, BMI change from 8 years of 100 mm Hg; socioeconomic status
Participants completed
of age to current BMI, presence of (Hollingshead scale), minimum of 8
questionnaires related to lifestyle
retinopathy of prematurity, maternal and maximum of 66; and fasting and
behaviors (including alcohol intake
corticosteroid exposure, and smoking 2-hour glucose levels, minimum of
and cigarette smoking), demographic
history. Multivariate regression was 2.4 mmol/L. Five imputed data sets
characteristics (education, marital
used to determine the influence of were created, and we analyzed the
status, and income), and personal
variables significant in the univariate pooled estimates and compared these
and family health history, including
analysis on insulin resistance and versus the analysis of the original
medication use and family history
glycemia outcomes. Given the non- data set.
of diabetes and cardiovascular
normality in some variables, log
disease. The research staff member
transformations were performed
conducting the visit was not informed
to create normally distributed data
if the participant was ELBW or NBW. RESULTS
for BMI, LMI, HOMA-IR, 2-hour
Characteristics at Birth and in blood glucose, and BMI change
from 8 years of age to current
Study Participants
Childhood
findings. To eliminate problems of One hundred of the surviving 148
Birth weight was available for all multicollinearity in the multivariate (67.6%) ELBW subjects participated
participants, and additional clinical regression analyses, we chose 1 at this assessment (Table 1). Of the
characteristics were available for the measure of adiposity (WC) and used ELBW nonparticipants, we were
ELBW group. Small for gestational birth weight rather than birth weight unable to contact 38 subjects, 5
age (SGA) is defined as birth weight group. We compared models with declined the study, 1 was deceased,
<10th percentile based on Canadian each of 3 measures of adiposity (WC, and 5 were untestable. More than
standards.15 NBW subjects were percent body fat, and FMI), with one-quarter of the included ELBW
known to be born at term. At 8 years similar results. Logistic regression subjects had a birth weight <750 g,
of age, height, weight, BMI, and family analysis, controlling for age, sex, and and 25% were born before 26
socioeconomic status were available. percent body fat, was conducted to weeks’ gestation. Of the 133 NBW
determine the risk of prediabetes, participants recruited at age 8 years
Statistical Analysis
T2DM, and dysglycemia in the ELBW and seen at young adulthood, 89
Statistical analysis was conducted group compared with the NBW (66.9%) were seen at this visit.
by using SPSS version 22 (IBM control group. We were unable to contact 35
Downloaded from by guest on October 2, 2016
PEDIATRICS Volume 138, number 4, October 2016 3
TABLE 1 Characteristics and Cardiometabolic Health Indicators (at Current Visit) of ELBW and NBW Participants
Characteristic Valid n ELBW (n = 100) Valid n NBW (n = 89) P
Male 100 40 (40) 89 37 (42) .83
Age, y 100 31.63 ± 1.66 89 31.96 ± 1.42 .15
Married or common-law 96 43 (45) 87 51 (59) .06
Total household income, median, $ 100 40 000–49 999 89 60 000–69 999
Birth weight, g 100 829.00 ± 130.38 89 3391.30 ± 442.28 <.001*
Gestational age, wk 100 27.10 ± 2.45 — — —
Maternal smoking 100 18 (18) — — —
Maternal steroid exposure 93 45 (48) — — —
Retinopathy of prematurity 100 34 (34) — — —
Change in birth weight to 8 y, kg 94 21.37 ± 4.64 89 24.49 ± 5.24 <.001*
Medication
BP-lowering medication 100 4 (4) 89 4 (4) .87
Insulin or oral hypoglycemic agents 100 2 (2) 89 1 (1) .62
Never smoked 100 57 (57) 89 45 (51) .38
Family history of diabetes 100 54 (54) 89 40 (45) .27
Family history of early heart disease 100 39 (39) 89 24 (27) .21
Height, m 95 1.64 ± 0.10 88 1.71 ± 0.11 <.001*
Weight, kg 95 71.90 ± 16.54 88 77.50 ± 18.28 .03*
BMI 95 26.91 ± 6.41 88 26.49 ± 5.08 .63
Change in BMI from 8 y to current 91 11.97 ± 5.82 88 9.77 ± 4.68 .006*
WC, cm 95 85.69 ± 14.64 88 84.63 ± 13.55 .61
Total body fat, % 92 35.45 ± 10.81 80 30.75 ± 10.49 .004*
LMI, kg/m2 92 15.82 ± 2.40 80 16.71 ± 2.43 .02*
FMI, kg/m2 92 9.38 ± 4.80 80 7.73 ± 3.51 .012*
Systolic BP, mm Hg 94 113.77 ± 11.93 88 108.86 ± 10.59 .004*
Diastolic BP, mm Hg 94 73.74 ± 10.00 88 70.55 ± 8.27 .02*
Total cholesterol, mmol/L 89 4.77 ± 0.96 80 4.67 ± 0.87 .47
Triglycerides, mmol/L 89 1.38 ± 0.73 80 1.22 ± 1.01 .22
HDL cholesterol, mmol/L 89 1.50 ± 0.46 80 1.50 ± 0.40 .98
LDL cholesterol, mmol/L 89 2.69 ± 0.86 80 2.65 ± 0.76 .76
Total cholesterol/HDL cholesterol 89 3.47 ± 1.26 80 3.31 ± 1.07 .38
Fasting plasma glucose, mmol/L 81 5.17 ± 0.68 73 4.89 ± 0.59 .007*
2-h plasma glucose, mmol/L 78 6.49 ± 2.50 72 5.40 ± 1.77 .003*
Fasting insulin, pmol/L 75 94.79 ± 66.85 72 71.07 ± 64.36 .03*
HOMA-IR 75 1.76 ± 1.22 72 1.30 ± 1.14 .02*
Unless otherwise indicated, data are presented as n (%) or mean ± SD. HDL, high-density lipoprotein; LDL, low-density lipoprotein. —, no data for full term cohort.
* P < .05.
subjects, 8 declined the study, and previous visits. Although ELBW vs 8%; P = .003). The ELBW group
1 is deceased. Male sex predicted subjects had BMI and WC similar also had a higher prevalence of
nonparticipation in both the ELBW to the NBW subjects, their body prediabetes (14.6% vs 4%; P = .04).
and NBW participants and, among composition differed. ELBW subjects When we analyzed the data using the
the ELBW, SGA birth predicted had lower LMI (P = .018) and 5 imputed data sets, the prevalence
increased likelihood of participation. higher body fat (P = .004). ELBW of dysglycemia was higher in ELBW
There were no differences in age, sex, subjects also had higher systolic subjects (30.2% vs 15.6%; P = .004)
or ethnicity between the ELBW and and diastolic BP levels compared in the pooled estimates and in 4 of
NBW participants at this visit. The with the NBW control subjects the 5 imputed data sets.
current median household income (P = .004 and 0.02, respectively)
The ELBW adults had a 4.03-fold
was lower in those born ELBW. (Table 2). The prevalence of high BP
(95% confidence interval, 1.53–
Fifty-nine percent of NBW subjects (prehypertension or hypertension)
10.66) increased risk of having
were married or living common- was 35% in the ELBW group and
dysglycemia compared with the
law compared with 45% of ELBW 23% in the NBW group (P = .07).
NBW group (Table 3). Although
subjects (P = .06). ELBW and NBW groups had similar
adjusting for age, sex, and percent
fasting lipid profiles.
body fat reduced this differential risk
Clinical Outcomes in ELBW Subjects
Compared With NBW Subjects As shown in Fig 1, the prevalence of (odds ratio, 3.04 [95% confidence
dysglycemia (prediabetes and type interval, 1.01–9.21]) in ELBW adults
The ELBW survivors had lower 2 diabetes) was higher in the ELBW compared with NBW adults (P <
height (P < .001) as noted at group than in the NBW group (26% .049), it remained significant.
Downloaded from by guest on October 2, 2016
4 MORRISON et al
TABLE 2 Prevalence of Prediabetes, T2DM, and Dysglycemia in ELBW Subjects Compared With NBW Subjects by Using Pooled Estimates of 5 Imputed Data
Sets
Outcome ELBW (n = 147) NBW (n = 131) z P
Dysglycemia 30.2 (44.) 15.6 (20.4) 2.90 .004
Prediabetes (IGT ± IFG) 30.2 (44.4) 24.0 (31.4) 1.18 .238
T2DM 26.3 (38.6) 20.3 (26.6) 1.16 .246
Data are presented as % (n).
born SGA compared with those
born appropriate for gestational age
(Supplemental Table 6).
DISCUSSION
Now in their early thirties, the
ELBW survivors in this regionally
representative cohort are 4 times
more likely to develop dysglycemia
than matched, NBW control
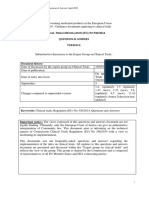
FIGURE 1 subjects. They also have higher
Prevalence of dysglycemia (prediabetes and T2DM) in the ELBW group compared with the NBW group. body fat and lower lean mass
*P < .05, **P < .01.
than the NBW control group but
similar BMI. The ELBW survivors
To understand the life course compared with the normoglycemic
with dysglycemia had higher BMI
and current correlates of glucose ELBW group. They also had higher
and WC in adulthood than the
metabolism, univariate and systolic BP levels (118 ± 11.9 mm Hg
normoglycemic ELBW subjects.
multivariate models of fasting vs 112 ± 10.5 mm Hg; P = .02) and
However, the ELBW subjects with
glucose, 2-hour glucose, and insulin higher fasting triglyceride levels
and without dysglycemia had similar
resistance are presented in Table 4. (1.8 ± 0.58 mmol/L vs 1.2 ± 0.74
gestational ages at birth, prevalence
Birth weight was inversely related mmol/L; P = .001) than the ELBW
of SGA, weight change from birth to 3
to insulin resistance, fasting blood subjects without dysglycemia. They
years and birth to 8 years, maternal
glucose levels, and 2-hour glucose did not, however, differ in sex,
glucocorticoid exposure, and
levels, and it continued to be gestational age at birth, birth weight,
maternal smoking history.
independently related to both insulin maternal corticosteroid exposure,
resistance and fasting blood glucose or maternal smoking history Hovi et al8 reported that individuals
levels in the multivariate models. during pregnancy (Supplemental in their mid-twenties who were
Current anthropometric measures Table 5). No differences in early born with very low birth weight
(WC, BMI, body fat, LMI, and FMI) growth trajectories were found. The had increased insulin resistance
were the strongest correlates of all dysglycemic group did, however, but no difference in prevalence of
glycemic measures in both univariate have a greater change in BMI from dysglycemia. Our cohort was ∼10
analyses and multivariate models. 8 years to adulthood than the years older than the Finnish cohort
Although the increase in weight normoglycemic group. and had more extreme prematurity
from 8 years of age to adulthood because the birth weight cutoff in
was related to all glucose variables In univariate analysis, the presence
our study was 1000 g compared with
in univariate analysis, it was not of retinopathy of prematurity was
1500 g. In population-based studies
significant in the fully corrected directly related to 2-hour glucose
level. In the fully adjusted model, that rely on administrative data
model. Growth from birth to 8 years
WC in adulthood was the strongest for diagnosis of diabetes, there is a
of age was unrelated to the glycemic
predictor (standardized β, 0.687; P = 1.5- to 2-fold increased prevalence
variables.
.02) but the presence of retinopathy of T2DM in adults born premature
Influence of Perinatal and Early of prematurity remained as an (<35 weeks’ gestation)4,5 by 40 to
Childhood Characteristics on Glycemic independent predictor (standardized 60 years of age. A population-based
Variables in Those Born ELBW β, 0.23; P = .05) (R2 = 0.27; P < .001). study in adults in a comparable age
The ELBW subjects with dysglycemia There were no differences in current range to the current study identified
had higher weight, BMI, and WC clinical health outcomes in the ELBW a slightly increased risk of diabetes
Downloaded from by guest on October 2, 2016
PEDIATRICS Volume 138, number 4, October 2016 5
TABLE 3 Risk of Prediabetes, T2DM, and Dysglycemia in ELBW Subjects Compared With NBW Subjects
Outcome Unadjusted Odds Ratio (95% CI) P Adjusted Odds Ratioa (95% CI) P
Dysglycemia 4.03 (1.53–10.66) .005 3.04 (1.01-9.21) .049
Prediabetes (IGT ± IFG) 3.77 (1.01–14.11) .049 2.17 (0.53-8.83) .281
T2DM 3.38 (0.89–12.81) .073 3.42 (0.676-17.33) .137
CI, confidence interval.
a Adjusted for age, sex, and percent body fat.
TABLE 4 Univariate and Multivariate Regression Analyses Examining Predictors of Insulin Resistance, Fasting Blood Glucose, and 2-Hour Blood Glucose
Predictor Univariate Analysis Multivariate Analysis
Standardized Parameter Estimate P Standardized Parameter P
Estimate
Insulin resistance
Sex 0.019 .82 0.028 .80
BMI 0.536 <.001* — —
WC 0.530 <.001* — —
Percent body fat 0.394 <.001* — —
FMI 0.491 <.001* 0.40 .01*
LMI 0.260 .002 0.235 .04*
Smoking history −0.053 .52 — —
Birth weight −0.268 .001* −0.224 .007*
Group 0.251 .002* — —
Change in BMI from 8 y to current 0.538 <.001* 0.028 .86
MODEL R2 adjusted, 0.315 <.001*
Fasting glucose
Sex 0.295 <.001* 0.449 <.001*
BMI 0.231 .004* — —
WC 0.342 <.001* — —
Percent body fat 0.063 .45 — —
FMI 0.163 .048* 0.463 .005*
LMI 0.275 .001* 0.091 .43
Smoking history −0.163 .04* −0.140 .06
Birth weight −0.206 .01* −0.170 .047*
Group 0.215 .007* — —
Change in BMI from 8 y to current 0.240 .003* −0.209 .21
Retinopathy of prematurity 0.167 .17 — —
MODEL R2 adjusted, 0.218 <.001*
2-h glucose
Sex −0.011 .90 0.133 .26
BMI 0.328 <.001* — —
WC 0.385 <.001* — —
Percent body fat 0.334 <.001* — —
FMI 0.396 <.001* 0.389 .021*
LMI 0.102 0 0.041 .74
Smoking history −0.180 .03* −0.146 .06
Birth weight −0.275 .001* −0.164 .07
Group 0.244 .003* — —
Change in BMI from 8 y to current 0.375 <.001* 0.028 .87
Retinopathy of prematurity 0.257 .037 — —
MODEL R2 adjusted, 0.210 <.001*
* P < .05.
(odds ratio, 1.2) in those born <37 diagnosis. Given the importance of The ELBW survivors had higher
weeks’ gestation but very few were prediabetes in increasing coronary body fat and lower lean mass for
born before 28 weeks’ gestation.16 artery disease risk17 and that height despite similar BMI. Previous
Population-based registry studies are prediabetes predicts progression to studies examining body composition
unable to identify prediabetes and T2DM,18 our study provides a more in those born prematurely have been
may underestimate the prevalence complete understanding of glycemic inconsistent in their conclusions.
of T2DM because they rely on status in adults born with extreme Total body fat in children born
medication prescription data for prematurity. prematurely has been similar to19
Downloaded from by guest on October 2, 2016
6 MORRISON et al
or lower than20 that in term-born weight. Perhaps the developing behaviors in the preterm population.
control subjects. Young adults born pancreatic β cell, which has low The age at which such intervention
at very low birth weight had reduced antioxidant defense mechanisms, should begin is uncertain, but strong
lean mass for height but body fat 28 is also sensitive to disturbances consideration should be given to the
similar to control subjects.21 In in oxygen exposure that occur in early origins literature that suggests
contrast, Breukhoven et al22 found perinatal life in association with beginning early in life may be most
increased body fat and similar lean extreme prematurity, leading to advantageous. Although retinopathy
mass in a large group of young abnormal vascularization as seen of prematurity may identify those
adults (mean age, 20.1 years) who in the retina.29 Although intriguing, at increased risk, these findings
were born preterm. Because we are this finding is preliminary, and should be confirmed in future studies
reporting on the oldest longitudinal further study is needed to evaluate with more direct measures of β-cell
cohort of ELBW survivors, it may cardiometabolic health in those with function.
be that body composition and retinopathy of prematurity in other
This study therefore contributes
metabolic disturbances are only cohorts.
to our understanding of the
revealed with advancing age. Our
implications of extreme perinatal
findings are consistent with studies Although our cohort is one of the
stress to health in adulthood. Given
in animal models in which prenatal largest and oldest prospective studies
changes in perinatal care since the
and perinatal stressors resulting of those born with ELBW, as with
adults studied in this cohort were
in reduced fetal growth enhanced other cohort studies, our results may
born, it is important that future
adipogenesis and fat accrual in have been influenced by differential
studies examine similar trajectories
the offspring.23 The critical period loss to follow-up. We did have similar
in metabolic health and body
for adipose tissue development findings when multiple imputations
composition in children born more
in humans is the third trimester. based on characteristics of the
recently. Consideration of mechanism
Because infants born extremely missing participants at their 24-year
and the development of interventions
premature are ex utero during visit were used. Perinatal care, and
to address these long-term concerns
this time, it is plausible that they parenteral and enteral nutrition
should be undertaken.
experience disturbances in early practices in particular, has changed
adipocyte development that may since these study participants were
influence adipose tissue function born. Increased focus on energy ACKNOWLEDGMENTS
throughout the life course. balance and on protein accretion
may influence body composition and The authors acknowledge the
Because the present study involved metabolic health over the life course. contributions of the research
a longitudinal, prospective cohort, it It is challenging to predict whether assistant, Vivian Vaughn-Williams.
can also contribute to understanding the differences we found in body Perhaps most importantly, the
the association between early life composition and metabolic health will authors thank the study participants
exposures and subsequent health be seen in more recent cohorts. Our who have contributed so generously
outcomes. Although previous studies findings underscore the importance of their time throughout their lives.
have suggested that maternal of evaluating these newer cohorts.
cigarette smoking24,25 and more rapid
“catch-up” growth in childhood26 ABBREVIATIONS
CONCLUSIONS
may heighten cardiometabolic risk
BP: blood pressure
in those with low birth weight, we Adults born with extreme
ELBW: extremely low birth
found no relationship between these prematurity have a 4-fold increased
weight
factors and glycemia. Although early risk of developing dysglycemia by
FMI: fat mass index
exposure to glucocorticoids has their fourth decade of life. They
HOMA-IR: homeostasis model
been postulated as a key mechanism also have increased adiposity and
assessment of insulin
underlying fetal programming,27 we reduced lean mass for height,
resistance
identified no relationship between differences that likely contribute
IFG: impaired fasting glucose
prenatal exposure to synthetic to their metabolic status. In those
IGT: impaired glucose tolerance
glucocorticoids and glycemia in our born ELBW, body fatness is the
LMI: lean mass index
study. Interestingly, we did identify strongest predictor of dysglycemia.
NBW: normal birth weight
a relationship between the presence Given the potentially modifiable
SGA: small for gestational age
of retinopathy of prematurity and the nature of body fatness, it will be
T2DM: type 2 diabetes
2-hour glucose level, independent of important to develop and evaluate
WC: waist circumference
anthropometric findings and birth interventions to influence lifestyle
Downloaded from by guest on October 2, 2016
PEDIATRICS Volume 138, number 4, October 2016 7
Address correspondence to Katherine M. Morrison, MD, HSC 3A59, 1280 Main St W, Hamilton ON L8N 3Z5. E-mail: kmorrison@mcmaster.ca
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright © 2016 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: All phases of this study were supported by grants from the Canadian Institutes of Health Research. Dr Morrison’s research program is also supported
by the Faculty of Health Sciences at McMaster and the McMaster Children’s Hospital Foundation through MAC Obesity.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
REFERENCES
1. Wadhwa PD, Buss C, Entringer S, insulin resistance: effects of birth 16. Crump C, Winkleby MA, Sundquist K,
Swanson JM. Developmental origins weight and postnatal growth in a Sundquist J. Risk of diabetes among
of health and disease: brief history of population based longitudinal study young adults born preterm in Sweden.
the approach and current focus on from birth into adult life. Diabetologia. Diabetes Care. 2011;34(5):1109–1113
epigenetic mechanisms. Semin Reprod 2006;49(3):478–485 17. Coutinho M, Gerstein HC, Wang Y,
Med. 2009;25(5):358–368 Yusuf S. The relationship between
10. Mathai S, Cutfield WS, Derraik JG,
2. Parkinson JR, Hyde MJ, Gale C, et al. Insulin sensitivity and β-cell glucose and incident cardiovascular
Santhakumaran S, Modi N. Preterm function in adults born preterm events. A metaregression analysis of
birth and the metabolic syndrome and their children. Diabetes. published data from 20 studies of 95,
in adult life: a systematic review and 2012;61(10):2479–2483 783 individuals followed for 12.4 years.
meta-analysis. Pediatrics. 2013;131(4). Diabetes Care. 1999;22(2):233–240
11. Tinnion R, Gillone J, Cheetham T,
Available at: www.pediatrics.org/cgi/ 18. Gerstein HC, Santaguida P, Raina P,
Embleton N. Preterm birth and
content/full/131/4/e1240 et al. Annual incidence and relative
subsequent insulin sensitivity: a
3. Lawlor DA, Davey Smith G, Clark H, Leon systematic review. Arch Dis Child. risk of diabetes in people with
DA. The associations of birthweight, 2014;99(4):362–368 various categories of dysglycemia: a
gestational age and childhood BMI systematic overview and meta-analysis
12. Saigal S, Stoskopf B, Streiner D, of prospective studies. Diabetes Res
with type 2 diabetes: findings from the Paneth N, Pinelli J, Boyle M. Growth
Aberdeen Children of the 1950s cohort. Clin Pract. 2007;78(3):305–312
trajectories of extremely low
Diabetologia. 2006;49(11):2614–2617 birth weight infants from birth to 19. Darendeliler F, Bas F, Bundak R,
young adulthood: a longitudinal, et al. Insulin resistance and body
4. Kajantie E, Osmond C, Barker DJ,
population-based study. Pediatr Res. composition in preterm born children
Eriksson JG. Preterm birth—a risk
2006;60(6):751–758 during prepubertal ages. Clin
factor for type 2 diabetes? The Helsinki
Endocrinol (Oxf). 2008;68(5):773–779
Birth Cohort Study. Diabetes Care. 13. Canadian Diabetes Association
2010;33(12):2623–2625 20. Fewtrell MS, Lucas A, Cole TJ, Wells
Clinical Practice Guideline. Definition,
JC. Prematurity and reduced body
5. Kaijser M, Bonamy AK, Akre O, et al. Classification and Diagnosis of
fatness at 8-12 y of age. Am J Clin Nutr.
Perinatal risk factors for diabetes in Diabetes, Prediabetes and Metabolic
2004;80(2):436–440
later life. Diabetes. 2009;58(3):523–526 Syndrome. Available at: http://
guidelines.diabetes.ca/browse/ 21. Hovi P, Andersson S, Järvenpää AL, et
6. Hofman PL, Regan F, Jackson WE, al. Decreased bone mineral density
Chapter3. Accessed August 4, 2016
et al. Premature birth and later in adults born with very low birth
insulin resistance. N Engl J Med. 14. Chobanian AV, Bakris GL, Black HR, weight: a cohort study. PLoS Med.
2004;351(21):2179–2186 et al; National High Blood Pressure 2009;6(8):e1000135
Education Program Coordinating
7. Singhal A, Fewtrell M, Cole TJ, Lucas Committee. The Seventh Report of 22. Breukhoven PE, Kerkhof GF, Willemsen
A. Low nutrient intake and early the Joint National Committee on RH, Hokken-Koelega AC. Fat mass
growth for later insulin resistance Prevention, Detection, Evaluation, and lipid profile in young adults born
in adolescents born preterm. Lancet. and Treatment of High Blood preterm. J Clin Endocrinol Metab.
2003;361(9363):1089–1097 Pressure: the JNC 7 report. JAMA. 2012;97(4):1294–1302
2003;289(19):2560–2572 23. Desai M, Beall M, Ross MG.
8. Hovi P, Andersson S, Eriksson JG, et al.
15. Kramer MS, Platt RW, Wen SW, et al. Developmental origins of obesity:
Glucose regulation in young adults
A new and improved population- programmed adipogenesis. Curr Diab
with very low birth weight. N Engl J
based Canadian reference for birth Rep. 2013;13(1):27–33
Med. 2007;356(20):2053–2063
weight for gestational age. Pediatrics. 24. Mamun AA, O’Callaghan MJ, Williams
9. Finken MJ, Keijzer-Veen MG, Dekker 2001;108(2): Available at: www. GM, Najman JM. Maternal smoking
FW, et al; Dutch POPS-19 Collaborative pediatrics.org/cgi/content/full/108/2/ during pregnancy predicts adult
Study Group. Preterm birth and later E35 offspring cardiovascular risk
Downloaded from by guest on October 2, 2016
8 MORRISON et al
factors - evidence from a community- 26. Ong KK, Ahmed ML, Emmett PM, Nat Rev Endocrinol. 2014;10(7):
based large birth cohort study. PLoS Preece MA, Dunger DB. Association 391–402
One. 2012;7(7):e41106 between postnatal catch-up 28. Lenzen S. Oxidative stress: the
growth and obesity in childhood: vulnerable beta-cell. Biochem Soc
25. Dior UP, Lawrence GM, Sitlani C, prospective cohort study. BMJ.
et al. Parental smoking during Trans. 2008;36(Pt 3):343–347
2000;320(7240):967–971
pregnancy and offspring cardio- 29. Hartnett ME, Penn JS. Mechanisms
metabolic risk factors at ages 27. Moisiadis VG, Matthews SG. and management of retinopathy
17 and 32. Atherosclerosis. Glucocorticoids and fetal of prematurity. N Engl J Med.
2014;235(2):430–437 programming part 1: Outcomes. 2012;367(26):2515–2526
Downloaded from by guest on October 2, 2016
PEDIATRICS Volume 138, number 4, October 2016 9
Cardiometabolic Health in Adults Born Premature With Extremely Low Birth
Weight
Katherine M. Morrison, Laura Ramsingh, Elizabeth Gunn, David Streiner, Ryan Van
Lieshout, Michael Boyle, Hertzel Gerstein, Louis Schmidt and Saroj Saigal
Pediatrics 2016;138;; originally published online September 2, 2016;
DOI: 10.1542/peds.2016-0515
Updated Information & including high resolution figures, can be found at:
Services /content/138/4/e20160515.full.html
Supplementary Material Supplementary material can be found at:
/content/suppl/2016/08/31/peds.2016-0515.DCSupplemental.
html
References This article cites 26 articles, 10 of which can be accessed free
at:
/content/138/4/e20160515.full.html#ref-list-1
Subspecialty Collections This article, along with others on similar topics, appears in
the following collection(s):
Endocrinology
/cgi/collection/endocrinology_sub
Metabolic Disorders
/cgi/collection/metabolic_disorders_sub
Fetus/Newborn Infant
/cgi/collection/fetus:newborn_infant_sub
Neonatology
/cgi/collection/neonatology_sub
Permissions & Licensing Information about reproducing this article in parts (figures,
tables) or in its entirety can be found online at:
/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
/site/misc/reprints.xhtml
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned, published,
and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk
Grove Village, Illinois, 60007. Copyright © 2016 by the American Academy of Pediatrics. All
rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from by guest on October 2, 2016
Cardiometabolic Health in Adults Born Premature With Extremely Low Birth
Weight
Katherine M. Morrison, Laura Ramsingh, Elizabeth Gunn, David Streiner, Ryan Van
Lieshout, Michael Boyle, Hertzel Gerstein, Louis Schmidt and Saroj Saigal
Pediatrics 2016;138;; originally published online September 2, 2016;
DOI: 10.1542/peds.2016-0515
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
/content/138/4/e20160515.full.html
PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
publication, it has been published continuously since 1948. PEDIATRICS is owned,
published, and trademarked by the American Academy of Pediatrics, 141 Northwest Point
Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2016 by the American Academy
of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.
Downloaded from by guest on October 2, 2016
Anda mungkin juga menyukai
- Insulin Resistance: Childhood Precursors of Adult DiseaseDari EverandInsulin Resistance: Childhood Precursors of Adult DiseasePhilip S. ZeitlerBelum ada peringkat
- 1346 FullDokumen6 halaman1346 FullYbc Berm CruzBelum ada peringkat
- Cardiometabolic Risks and Severity of Obesity in Children and Young AdultsDokumen11 halamanCardiometabolic Risks and Severity of Obesity in Children and Young AdultsYosie Yulanda PutraBelum ada peringkat
- 1993 - BARKER Et Al - Fetal Nutrition and Cardiovascular Disease in Adult LifeDokumen4 halaman1993 - BARKER Et Al - Fetal Nutrition and Cardiovascular Disease in Adult LifeSamanta MonteiroBelum ada peringkat
- Ejercicio Funcion Vascular DiabetesDokumen12 halamanEjercicio Funcion Vascular DiabetesMayra de CáceresBelum ada peringkat
- Hyperglycemia and Morbidity and Mortality in Extremely Low Birth Weight InfantsDokumen7 halamanHyperglycemia and Morbidity and Mortality in Extremely Low Birth Weight InfantsIvan VeriswanBelum ada peringkat
- DM & BBLRDokumen10 halamanDM & BBLRBunda BiyyuBelum ada peringkat
- Article - Ghrelin and Leptin in Insulin Resistance (CHECKED)Dokumen6 halamanArticle - Ghrelin and Leptin in Insulin Resistance (CHECKED)pixoguiasBelum ada peringkat
- ApproachpatientpwDokumen8 halamanApproachpatientpwPatricia Rearte CarvalhoBelum ada peringkat
- Ehrenkranz 1999Dokumen12 halamanEhrenkranz 1999amyBelum ada peringkat
- Overweight and The Metabolic Syndrome in Adult Offspring of Women With Diet-Treated Gestational Diabetes Mellitus or Type 1 DiabetesDokumen7 halamanOverweight and The Metabolic Syndrome in Adult Offspring of Women With Diet-Treated Gestational Diabetes Mellitus or Type 1 DiabetesMyoman FernandaBelum ada peringkat
- Physical Activity and Abnormal Blood Glucose Among Healthy Weight AdultsDokumen6 halamanPhysical Activity and Abnormal Blood Glucose Among Healthy Weight Adultssyafiqa abdullahBelum ada peringkat
- Jurnal Hiperemesis GravidarumDokumen6 halamanJurnal Hiperemesis GravidarumArief Tirtana PutraBelum ada peringkat
- Salt and Metabolic Syndrome 2007Dokumen6 halamanSalt and Metabolic Syndrome 2007irene hoffmannBelum ada peringkat
- Nutritional Rehabilitation For Children With Congenital Heart Disease With Left To Right ShuntDokumen10 halamanNutritional Rehabilitation For Children With Congenital Heart Disease With Left To Right ShuntJiradett Arm KerdsriBelum ada peringkat
- Differences in angiogenic factors and adipocytokines between early and late pre-eclampsiaDokumen7 halamanDifferences in angiogenic factors and adipocytokines between early and late pre-eclampsiaNi Wayan Ana PsBelum ada peringkat
- Metabolic Syndrome in Childhood: Association With Birth Weight, Maternal Obesity, and Gestational Diabetes MellitusDokumen9 halamanMetabolic Syndrome in Childhood: Association With Birth Weight, Maternal Obesity, and Gestational Diabetes MellitusAnnisa FujiantiBelum ada peringkat
- 2010 Article 69Dokumen6 halaman2010 Article 69gepang_metalBelum ada peringkat
- Obesity Metabolic Syndrome and Insulin Dynamics After CranipharyngiomaDokumen8 halamanObesity Metabolic Syndrome and Insulin Dynamics After CranipharyngiomaaandakuBelum ada peringkat
- Impact of lifestyle changes on obese childrenDokumen5 halamanImpact of lifestyle changes on obese childrensebastianBelum ada peringkat
- Jurnal AKIDokumen7 halamanJurnal AKIAnonymous Vz9teLBelum ada peringkat
- Maternal Pre-Gravid Health Predicts Infant BirthweightDokumen8 halamanMaternal Pre-Gravid Health Predicts Infant BirthweightMargrethe AndreassenBelum ada peringkat
- Growth Failure in Children With Sickle Cell AnaemiaDokumen7 halamanGrowth Failure in Children With Sickle Cell AnaemiaInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Fetal Origins of Adult DiseasesDokumen37 halamanFetal Origins of Adult DiseasesAbhinav AggarwalBelum ada peringkat
- Effect of BmiDokumen5 halamanEffect of BmiSyaiful Putra RanaBelum ada peringkat
- Weight Gain and Height Growth During Infancy, Childhood, and Adolescence As Predictors of Adult Cardiovascular RiskDokumen12 halamanWeight Gain and Height Growth During Infancy, Childhood, and Adolescence As Predictors of Adult Cardiovascular Risktom24Belum ada peringkat
- Comparative Studies of Diabetes in Adult Nigerians Lipid Profile and Antioxidants Vitamins A and CDokumen5 halamanComparative Studies of Diabetes in Adult Nigerians Lipid Profile and Antioxidants Vitamins A and CEditor IJTSRDBelum ada peringkat
- Hipo Glice MiaDokumen8 halamanHipo Glice MiaRosita Aguirre FloresBelum ada peringkat
- Kushchayeva 2019Dokumen13 halamanKushchayeva 2019pelinBelum ada peringkat
- Diabetes Gestacional 2022 NejmDokumen12 halamanDiabetes Gestacional 2022 NejmGabrielaBelum ada peringkat
- Metabolic Syndrome in Very Low Birth Weight Young Adults and Controls: The New Zealand 1986 VLBW StudyDokumen11 halamanMetabolic Syndrome in Very Low Birth Weight Young Adults and Controls: The New Zealand 1986 VLBW StudysatishBelum ada peringkat
- Lactancia MaternaDokumen6 halamanLactancia MaternaFernandaBelum ada peringkat
- The Relation of Overweight To Cardiovascular Risk Factors Among Children and Adolescents: The Bogalusa Heart StudyDokumen10 halamanThe Relation of Overweight To Cardiovascular Risk Factors Among Children and Adolescents: The Bogalusa Heart StudyaocuBelum ada peringkat
- Soal PG Endokrin MahasiswaDokumen5 halamanSoal PG Endokrin MahasiswaSandwingBelum ada peringkat
- Metabolic Evaluation of Young Women With Congenital Adrenal HyperplasiaDokumen7 halamanMetabolic Evaluation of Young Women With Congenital Adrenal HyperplasiaOnysapto PramanaBelum ada peringkat
- Maternal Diet, BreastfeedingDokumen6 halamanMaternal Diet, BreastfeedingRiska Diene PratiwiBelum ada peringkat
- What Is New in Diabetes in PregnancyDokumen2 halamanWhat Is New in Diabetes in PregnancyRyan SadonoBelum ada peringkat
- POSITION STATEMENTPreDMsop TRTRDokumen12 halamanPOSITION STATEMENTPreDMsop TRTRTony CoaBelum ada peringkat
- Blood Pressure, Serum Total Cholesterol and Contraceptive Pill Use in 17-Year-Old GirlsDokumen5 halamanBlood Pressure, Serum Total Cholesterol and Contraceptive Pill Use in 17-Year-Old GirlsLucerito MartinezBelum ada peringkat
- Maternal BMI's impact on pre-eclampsia phenotypeDokumen7 halamanMaternal BMI's impact on pre-eclampsia phenotypeAchmad Deza FaristaBelum ada peringkat
- HOMA Medicion EJIM2003Dokumen6 halamanHOMA Medicion EJIM2003Dr Dart05Belum ada peringkat
- Watne 2016Dokumen9 halamanWatne 2016Rizki Nandasari SulbahriBelum ada peringkat
- Dex 246Dokumen12 halamanDex 246Nur WahyuniBelum ada peringkat
- Maternal Insulin Treatment May Reduce Obesity Risk in OffspringDokumen4 halamanMaternal Insulin Treatment May Reduce Obesity Risk in OffspringSarly FebrianaBelum ada peringkat
- Metabolic Syndrome and Insulin Resistance in Obese AdolescentsDokumen8 halamanMetabolic Syndrome and Insulin Resistance in Obese AdolescentsHasriani rijalBelum ada peringkat
- Implications of Body Fat Distribution in An Older Twin PopulationDokumen5 halamanImplications of Body Fat Distribution in An Older Twin PopulationAle TabaskoBelum ada peringkat
- International Journal of Gerontology: Original ArticleDokumen5 halamanInternational Journal of Gerontology: Original ArticleIsra DeviyantiBelum ada peringkat
- Daniel Slip Id Screening 2008Dokumen13 halamanDaniel Slip Id Screening 2008Heart of the Valley, Pediatric CardiologyBelum ada peringkat
- 10.1515@jpem 2018 0516Dokumen8 halaman10.1515@jpem 2018 0516pelinBelum ada peringkat
- Origins of Adolescent Obesity and Hypertension: SciencedirectDokumen2 halamanOrigins of Adolescent Obesity and Hypertension: SciencedirectAurnha DewhiBelum ada peringkat
- tmp9C4E TMPDokumen3 halamantmp9C4E TMPFrontiersBelum ada peringkat
- Cardiometabolic Risks and Severity of Obesity in Children and Young AdultsDokumen1 halamanCardiometabolic Risks and Severity of Obesity in Children and Young AdultsPatrick StarkeyBelum ada peringkat
- Contribution of Lifestyle and Obesity To The Incidence of Pre-DiabetesDokumen7 halamanContribution of Lifestyle and Obesity To The Incidence of Pre-DiabetesRicky BooyBelum ada peringkat
- Jurnal PerinaDokumen7 halamanJurnal PerinaBhismo PasetyoBelum ada peringkat
- CONSENSUS STATEMENT: Childhood Obesity: Printed in U.S.ADokumen17 halamanCONSENSUS STATEMENT: Childhood Obesity: Printed in U.S.Aanang fajarBelum ada peringkat
- Characteristics of Children 2 To 5 Years of Age With Severe ObesityDokumen10 halamanCharacteristics of Children 2 To 5 Years of Age With Severe ObesityIvan BurgosBelum ada peringkat
- 2016 Risk of Hypertension in Overweight AdolescentsDokumen10 halaman2016 Risk of Hypertension in Overweight AdolescentsmaynaBelum ada peringkat
- Early Life Risk Factors For ObesityDokumen13 halamanEarly Life Risk Factors For Obesitybarragan-prosisaBelum ada peringkat
- Research Article: Predictors of Insulin Resistance in Children Versus Adolescents With ObesityDokumen8 halamanResearch Article: Predictors of Insulin Resistance in Children Versus Adolescents With ObesitySujanaBelum ada peringkat
- Prader-Willy Fda OzempicDokumen16 halamanPrader-Willy Fda OzempicJailza MartinsBelum ada peringkat
- Cryotherapy in Treatment of Keloids Evaluation ofDokumen5 halamanCryotherapy in Treatment of Keloids Evaluation ofShilvia Adita PutriBelum ada peringkat
- COPD 133148 Burden of Asthma Dyspnea and Chronic Cough in South Asia 040617Dokumen19 halamanCOPD 133148 Burden of Asthma Dyspnea and Chronic Cough in South Asia 040617Shilvia Adita PutriBelum ada peringkat
- Cryotherapy in Treatment of Keloids: Factors Affecting OutcomeDokumen18 halamanCryotherapy in Treatment of Keloids: Factors Affecting OutcomeShilvia Adita PutriBelum ada peringkat
- Ajr 12 9801Dokumen6 halamanAjr 12 9801Rahmatika IntianiBelum ada peringkat
- Association Between Menarche Age and Menstrual DisorderDokumen8 halamanAssociation Between Menarche Age and Menstrual DisorderShilvia Adita PutriBelum ada peringkat
- Massive Haemorrhage: P Donnelly B FergusonDokumen18 halamanMassive Haemorrhage: P Donnelly B FergusonRizqiBelum ada peringkat
- Group 9 - Dental FluorosisDokumen37 halamanGroup 9 - Dental Fluorosis2050586Belum ada peringkat
- Kepler and AlchemyDokumen13 halamanKepler and AlchemyMartha100% (1)
- CapstoneDokumen40 halamanCapstoneDevanshi GoswamiBelum ada peringkat
- Functional Abdominal Cramping Pain Expert Practical Guidance 2022Dokumen9 halamanFunctional Abdominal Cramping Pain Expert Practical Guidance 2022Mohamad MostafaBelum ada peringkat
- EMTALADokumen5 halamanEMTALAJimmy MillerBelum ada peringkat
- Measurements in Radiology Made Easy® PDFDokumen213 halamanMeasurements in Radiology Made Easy® PDFsalah subbah100% (2)
- Accomplishment ReportDokumen16 halamanAccomplishment ReportIsaias BigolBelum ada peringkat
- Clinical Study ReportDokumen5 halamanClinical Study ReportAlexandraCirlanBelum ada peringkat
- DR, OR, WardDokumen14 halamanDR, OR, WardjanBelum ada peringkat
- Audit Program Ppi (Mariani, SKM, Mha)Dokumen23 halamanAudit Program Ppi (Mariani, SKM, Mha)Dedy HartantyoBelum ada peringkat
- Mar ChecklistDokumen18 halamanMar ChecklistMin MawBelum ada peringkat
- Case Study - MyomaDokumen54 halamanCase Study - Myomauvinr100% (1)
- Dance BenefitsDokumen9 halamanDance Benefitsapi-253454922Belum ada peringkat
- Poster ROICAM 2018Dokumen1 halamanPoster ROICAM 2018ibrahimBelum ada peringkat
- DAFTAR PUSTAKA SarkomaDokumen2 halamanDAFTAR PUSTAKA SarkomaantaniaaaBelum ada peringkat
- Lecture 16-17 - Opioids AnalgesicsDokumen20 halamanLecture 16-17 - Opioids AnalgesicsJedoBelum ada peringkat
- Drug Study HydrocodoneDokumen1 halamanDrug Study HydrocodoneYlrenne DyBelum ada peringkat
- Pediatric PerfectionismDokumen20 halamanPediatric Perfectionismapi-438212931Belum ada peringkat
- Regulation5362014 Qa enDokumen143 halamanRegulation5362014 Qa enmeiBelum ada peringkat
- Broadline Epar Public Assessment Report enDokumen25 halamanBroadline Epar Public Assessment Report enPablo OrricoBelum ada peringkat
- Cghs Rates BangaloreDokumen26 halamanCghs Rates Bangaloregr_viswanathBelum ada peringkat
- Fundamentals of Tooth Preparation Periodontal AspectsDokumen74 halamanFundamentals of Tooth Preparation Periodontal AspectsVica Vitu100% (3)
- Joyetech Eroll Manual MultilanguageDokumen9 halamanJoyetech Eroll Manual MultilanguagevanlilithBelum ada peringkat
- Radial Club Hand TreatmentDokumen4 halamanRadial Club Hand TreatmentAshu AshBelum ada peringkat
- Pharmacovigilance Classification & CodingDokumen42 halamanPharmacovigilance Classification & Codingrakesh meher0% (1)
- Mal UnionDokumen10 halamanMal UnionYehuda Agus SantosoBelum ada peringkat
- 2014 Windsor University Commencement Ceremony PROOFDokumen28 halaman2014 Windsor University Commencement Ceremony PROOFKeidren LewiBelum ada peringkat
- Abdominal UltrasoundDokumen6 halamanAbdominal Ultrasounds0800841739100% (1)
- Gastric Dilatation Volvulus (GDV)Dokumen21 halamanGastric Dilatation Volvulus (GDV)ΦΩΦΩ ΣΠΕΝΤΖΙBelum ada peringkat