Chronic Venous Insufficiency: (Rutherford's Vascular Surgery, 8th Edition, Chapter 12, Venous Patology, 170-173, 2014)
Diunggah oleh
Julita Yanti0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
56 tayangan8 halamanThis document summarizes the pathophysiology of chronic venous insufficiency (CVI). It describes the clinical manifestations of CVI from varicose veins to stasis dermatitis and ulceration. The pathophysiology involves venous reflux leading to venous hypertension, which causes vein wall damage and fibrosis over time. This impairs the veins' ability to contract and regulate hydrostatic pressure, worsening venous hypertension and progression of CVI. The document reviews historical theories on CVI and provides detailed descriptions of the pathology involved at each clinical stage of CVI.
Deskripsi Asli:
CVI
Judul Asli
Chronic Venous Insufficiency
Hak Cipta
© © All Rights Reserved
Format Tersedia
DOCX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniThis document summarizes the pathophysiology of chronic venous insufficiency (CVI). It describes the clinical manifestations of CVI from varicose veins to stasis dermatitis and ulceration. The pathophysiology involves venous reflux leading to venous hypertension, which causes vein wall damage and fibrosis over time. This impairs the veins' ability to contract and regulate hydrostatic pressure, worsening venous hypertension and progression of CVI. The document reviews historical theories on CVI and provides detailed descriptions of the pathology involved at each clinical stage of CVI.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
56 tayangan8 halamanChronic Venous Insufficiency: (Rutherford's Vascular Surgery, 8th Edition, Chapter 12, Venous Patology, 170-173, 2014)
Diunggah oleh
Julita YantiThis document summarizes the pathophysiology of chronic venous insufficiency (CVI). It describes the clinical manifestations of CVI from varicose veins to stasis dermatitis and ulceration. The pathophysiology involves venous reflux leading to venous hypertension, which causes vein wall damage and fibrosis over time. This impairs the veins' ability to contract and regulate hydrostatic pressure, worsening venous hypertension and progression of CVI. The document reviews historical theories on CVI and provides detailed descriptions of the pathology involved at each clinical stage of CVI.
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 8
CHRONIC VENOUS INSUFFICIENCY
(Rutherford`s Vascular Surgery, 8th edition, Chapter 12, Venous Patology, 170-173, 2014)
Limb manifestations of CVI are easy to recognize: variable swelling, varicosities,
hyperpigmentation, stasis dermatitis, ulceration, and pain (Figure 12-5). The symptoms are
widespread in the general population and are not always directly related to the magnitude of
venous insufficiency (e.g., degree of reflux). However, the most severe CVI symptoms are
related to venous reflux with an obstructed venous segment.
The best way to categorize CVI is with the CEAP (clinical, etiologic, anatomic,
pathologic) classification. This system is discussed in detail in Chapter 53; in brief, it is a
standardized system to grade CVI on the basis of symptoms, etiology, anatomy, and
pathophysiology. The higher the class, the more severe the symptoms and the patient’s disability.
For clarity of discussion, this section separately focuses on the pathology of class 2 to 3 and class
4 to 6 CVI, although there are many common factors and the pathology clearly represents a
spectrum.
Mechanisms of chronic vein injury with primary and secondary valve damage have been
reasonably well described (Table 12-3). The common mechanism is venous reflux between the
superficial and deep systems, either at the site of perforators or through other deep and
superficial system connections, which accounts for the increased venous hydrostatic pressure
transmitted to the superficial veins and tissues. An obstructed vein segment worsens this process.
Experimentally, venous hypertension activates leukocytes, although the activation is probably a
local phenomenon. The process of vein wall fibrosis plays a contributing role in valvular
damage, which then worsens the hydrostatic pressure regulation and consequently promotes
greater venous hypertension with the upright position. The molecular and cellular eventsseem to
point to adaptive responses to injury as well as abnormal healing.
Historical Perspective and General Background
Several important theories have been postulated regarding the etiology and
pathophysiology of CVI. In 1917, John Homans produced a clinical treatise on the diagnosis and
the management of patients with CVI and coined the term “post thrombotic syndrome.” Dr.
Alfred Blalock put forth the hypothesis that local hypoxia precipitated CVI. Local tissue hypoxia
and alterations in nutrient blood flow were proposed as an underlying etiology by Browse and
Burnand. Their important study directly demonstrated the effect of venous hypertension on the
venous microcirculation, and they observed histologically that in large capillaries, pericapillary
fibrin deposition, which they called the “fibrin cuff,” occurred (Fig. 12-6). Dr. P.D. Coleridge
Smith proposed that leukocyte trapping in slow-flow and distended venous segments may
underlie much of CVI development. Burnand et al also showed a positive correlation between
the inability of the calf pump to reduce foot vein pressure during exercise and the number of
capillaries in the skin.
Varicose Veins (CEAP Class 2 to 3 Disease)
Varicose veins (VVs) have been described since before the Common Era and are obvious
on the lower limbs of many people. The fact that varicose veins primarily affect the lower limb
directly implicates the upright nature of humans— specifically, the effect of hydrostatic pressure
on the pathophysiology of such veins. The relationship between body weight and extent of
varicose veins and symptoms is variable. Limb symptoms are generally local and consist of
pruritus and swelling. Occasionally, varicose veins can erode and bleed. Conversely, most such
veins do not thrombose, despite relatively slow blood flow through these torturous structures,
and this fact underlies the natural anticoagulant nature of venous endothelium, even in
structurally abnormal vessels.
The initial anatomic location of varicose veins is typically in the great and small
saphenous distributions and their tributaries in the superficial system. Related risk factors are
multiple, including primary etiologies associated with pregnancy, prolonged standing, female
gender, and, rarely, congenital absence of valves. In addition, varicosities may develop as a
result of prior DVT or trauma.
Studies support a genetic predisposition to varicose veins. In a prospective study of 402
subjects, the risk of development of varicose veins was 90% if both parents were affected, 25%
for males and 62% for females if one parent was affected, and 20% if neither parent was
affected. These data suggest an autosomal dominant with variable penetrance mode of genetic
transmission.
Studies are generally lacking in relation to early vein wall changes associated with
varicose veins, because most histologic studies are limited to end-stage surgical specimens. In
varicose veins, the orderly appearance of the medial layer is replaced by an intense and
disorganized deposition of collagen that separates the closely apposed muscle cells. Smooth
muscle cells appear elliptical and are likely a secretory phenotype, and both TGF-β and basic
fibroblast growth factor (bFGF) have been documented to be significantly increased in
hypertrophic segments of varicose veins. The underlying mechanism for these histologic changes
is unknown, but the inciting event of increased hydrostatic pressure or an intrinsic genetic defect
is probably primary.
Active vein wall remodeling is consistently observed in specimens of varicose veins with
abnormal matrix collagen metabolism. Quantitatively, higher collagen content and lower elastin
content in varicose veins have been measured in human samples, suggesting an imbalance in
connective tissue matrix regulation and turnover. Specific alteration in the type of collagen may
also contribute to vessel weakening, with an observed increase in tissue water and collagen type I
content in comparison with normal saphenous veins.
Conversely, collagen types III and V levels were lower than in normal veins, and less
type III collagen is associated with decreased elasticity. Similarly, in a separate study, varicose
veins had increased type I and decreased type III collagen gene expression. Comparison of
smooth muscle cells from varicose veins with controls has shown matrix dysregulation as well as
regional differentiation as measured by antigen markers in the cells from varicose veins.
Interestingly, a similar collagen dysregulation pattern has also been observed in patients with
varicose veins after dermal biopsies, suggesting an intrinsic genetic abnormal response to injury.
The observed pathology suggests a net effect of matrix deposition. One mechanism for
these changes may be local upregulation of MMPs and fibrinolytic activity within the
microenvironment. The upstream regulators of MMPs are in part, the plasmin system. Urinary
PA levels are three to five times higher than in controls, as assessed from media of specimen
organ culture from varicose veins. Interestingly, there is no difference in tPA activity or PAI-1
levels. Investigators have found that TIMP-1 and MMP-1 protein levels are higher at the
saphenofemoral junction in patients with varicose veins and that MMP-2 activity is lower in
normal controls. Similarly, high TIMP-1 activity and low MMP-2 activity have been observed in
varicose vein segments, with a threefold significant difference in comparison with normal
controls. Overall differences in MMP-9 protein have also been identified, and it is likely, with
the inflammatory influx, that MMP-9 is released primarily from PMNs but may be less important
than MMP-2.
This disordered vein structure also correlates with altered vasoreactivity. The contractual
response of varicose and normal great saphenous rings to various alpha-adrenergic and non–
alpha-adrenergic receptors has shown decreased contractility as compared with controls. This
lower contractility may be due to repeated overdistention or impaired contractility related to
persistent vein wall tension. However, it is a segmental response and likely adaptive. Receptor
downregulation may also play a role. For example, feedback inhibition of ETA receptor
secondary to increased endothelin-1 is also postulated to mediate the lower vasoreactivity
content in the walls of varicose veins. The ratio of prostacyclin to thromboxane A2 is also lower,
suggesting an increased basal contractile state. Finally, one investigation has suggested that
MMP-2 may act to dilate the vein by direct hyperpolarization effects, via a Ca+2 channel
mechanism.
Pathophysiology of Stasis Dermatitis and Dermal Fibrosis (CEAP Class 4 to 6 Disease)
Stasis venous dermatitis is a disease of chronic dermal inflammation due to persistent and
sustained cutaneous and dermal injury secondary to venous hypertension. The primary injury
may be extravasation of macromolecules and red blood cell products into the dermal interstitium,
which creates a secondary inflammatory response, and multiple pathophysiologic hypotheses
have been proposed. The clinical appearance is that of brawny induration, skin thickening,
swelling, and tissue breakdown with ulceration in the gaiter regions. Alteration in extracellular
matrix is clear on histologic assessment, with dermal space extracellular disorganized collagen
deposition and perivascular tissue cuffs.
The role of the common growth factor TGF-β1, which is secreted by activated endothelial
cells, fibroblasts, and platelets and stimulates matrix protein production, has been studied in
relation to venous ulcer development. TGF-β is an inducer of TIMP-1 and collagen production
and inhibits MMP activity and gene expression. The local upregulation of TGF-β1 thus favors
net collagen and matrix accumulation and is supported by histologic and clinical analysis,
although gene upregulation may occur at an earlier stage than protein production. Whether TGF-
β is acting directly or is associated with this process has not been substantiated in human studies
to date. Several other growth factors are elevated in the dermis of patients with CVI, including
platelet-derived growth factors α and β and VEGF. These various molecules are found within the
capillaries surrounding fibroblasts and inflammatory cells in patients with venous skin changes.
Further studies have suggested that endothelial activation results from venous
hypertension. A significant rise in plasma levels of endothelial leukocyte adhesion molecule-1
(ELAM-1), ICAM-1, and vascular cell adhesion molecule-1 were observed in patients with
venous hypertension, indirectly suggesting a role of these molecules in the pathogenesis.
Similarly, increased endothelial expression of ICAM-1, vascular cell adhesion molecule-1, and
leukocyte function-associated antigen-1 (LFA-1) has been documented in patients with dermal
disease.
Several studies suggest conflicting data with regard to whether MMP-2, MMP-9, and
TIMP-1 levels are higher or unaltered in patients with venous ulcers. This uncertainty may have
to do with the measurement of MMP gene, protein, or activity expression as well as with the
ulcer stage and patient characteristics that may not be controlled for. Another important
proteinase is elastase, primarily derived from PMNs. Higher levels of plasma elastase were
found in patients with venous ulceration than in those with uncomplicated varicose veins,
perhaps reflecting active degranulation in those with ulcers. However, this evidence is only
indirect, and whether proteinases are directly responsible for venous ulcer development is not
known.
Consistent with the tissue inflammation, leukocytes are markedly elevated in the gaiter
region in association with the venous ulcers. This finding correlates with preceding elevation of
IL-1α and ICAM-1 in the tissue of lipodermatosclerotic skin. The type and distribution of
leukocytes in patients with CEAP class 5/6 CVI have been studied histologically. Numbers of
mast cells and macrophages were two to four times greater around arterioles and postcapillary
venules in patients with CEAP class 4/5 CVI than in controls. Similarly, increased macrophages
are demonstrated around arterioles and postcapillary venules, although fibroblasts are the most
common cell observed in both gaiter and thigh biopsy specimens. It is likely that these
leukocytes regulate the tissue remodeling that results in dermal fibrosis.
Sluggish venous blood flow related to increased hydrostatic pressure leads to hypoxia and
PMN activation, with degranulation of mediators and proteinases that cause endothelial damage.
Skin hypoxia also occurs on the gaiter areas of limbs with severe venous disease and is
significantly different from controls, oxygen tension (tcPO2) differing by more than 20 mm.
Although leukocyte trapping within the capillaries is probably not the sole cause, it is likely that
leukocytes become activated, transmigrate into the vein walls, and mediate some of the observed
damage. Consistently, findings in punch biopsy specimens of ulcers suggest that leukocytes play
a role in the dermal manifestations of CVI. For example, leukocytes, macrophages, and mast
cells have all been observed in immunohistochemical and electron microscopic examinations of
affected tissue.
The dermal fibroblast may also be dysfunctional and allow perpetuation of the disease.
Decreased motility, in part mediated by the microenvironment, plays a role in the impaired
healing process of ulcer tissue. Comparison of venous ulcer fibroblasts with control fibroblasts
with stimulation with TGF-β suggested that there are differences in collagen production. With
stimulation, collagen production was increased 60% in controls, whereas the venous ulcer
fibroblasts were unresponsive. This finding may be related to an end-stage process,
overstimulation of the ulcer fibroblast, or an intrinsically dysfunctional fibroblast. Consistently,
the proliferative responses of fibroblasts from patients with CVI to TGF-1β correlated with
disease severity. Fibroblasts in patients with CEAP class 2 or 3 CVI retained agonist induce
proliferative capacity, whereas those from patients with class 4 or 5 CVI showed diminished
agonist-induced proliferation. Fibroblasts from patients with class 6 CVI and active ulcers did
not proliferate with TGF-1β, suggesting that these ulcer fibroblasts are refractory to stimulation
and may contribute to the inability to promote healing. Histologically, these fibroblasts appear
morphologically similar to fibroblasts undergoing cellular senescence, and therefore may be
proapoptotic from repeated injury. Another study showed similar impairment of dermal wound
fibroblast proliferation response to both basic fibroblast growth factor and EGF.
An interesting but unanswered question is which patients with similar degrees of reflux
and hydrostatic pressures from CVI are more predisposed to development of venous ulcers. Data
now suggest that iron metabolism and ulcer development are interrelated. Although commonly
thought of as a consequence of all the other mechanisms of CVI, the iron deposition itself may
cause tissue damage. More onvincingly, the risk of ulcer development among patients with class
4 to 6 CVI was sevenfold higher in those with the C282Y genotype, a mutation related to iron
processing.
Taken together, venous insufficiency and secondary cutaneous manifestations suggest
that active tissue remodeling occurs, likely via multiple mechanisms and in different stages.
Whether the growth factors, cytokines, and proteinases are directly responsible or secondary to
other factors of the disease has not been definitively answered. Regardless, the significant benefit
of compression in ulcer healing suggests these factors may play a secondary role. In one study
the benefit of compression therapy and how it may alter histologic and biochemical features was
shown after 4 weeks. Complete epithelialization was frequent, the hemosiderin and red blood
cell extravasation products had decreased, and fibrin cuffs were reversed. However, a single
“silver bullet” approach to therapy is unlikely to be successful. Rather, identifying patients at risk
for CVI with biomarkers (via genomics and proteomics) may be the best immediate translational
approach.
Anda mungkin juga menyukai
- 007: The Stealth Affair ManualDokumen11 halaman007: The Stealth Affair Manualcodigay769Belum ada peringkat
- The Secret of Forgiveness of Sin and Being Born Again by Pastor Ock Soo Park 8985422367Dokumen5 halamanThe Secret of Forgiveness of Sin and Being Born Again by Pastor Ock Soo Park 8985422367Justinn AbrahamBelum ada peringkat
- Oxford Math AA SL Exam Practise Additional ResourcesDokumen172 halamanOxford Math AA SL Exam Practise Additional ResourcesSıla DenizBelum ada peringkat
- Pediatric Coag Disorders PDFDokumen15 halamanPediatric Coag Disorders PDFFATIMA LAVADIABelum ada peringkat
- TA35 & TA40 Articulated Dumptruck Maintenance Manual: Click Here For Table ofDokumen488 halamanTA35 & TA40 Articulated Dumptruck Maintenance Manual: Click Here For Table ofKot878100% (2)
- Pipe Support Reference 8-29-14Dokumen108 halamanPipe Support Reference 8-29-14HITESHBelum ada peringkat
- Form ConstructionDokumen36 halamanForm ConstructionYhoga DheviantBelum ada peringkat
- AS Film Production Lesson.Dokumen13 halamanAS Film Production Lesson.MsCowanBelum ada peringkat
- Performance Management Systems and Strategies by Dipak Kumar BhattacharyyaDokumen385 halamanPerformance Management Systems and Strategies by Dipak Kumar Bhattacharyyasayal96amrit100% (3)
- Terraform AWSDokumen1.531 halamanTerraform AWSTilted Mowa100% (1)
- TODO Data Sheet PDFDokumen70 halamanTODO Data Sheet PDFJake ZyrusBelum ada peringkat
- Pathophysiology of Sepsis American Journal of PathologyDokumen10 halamanPathophysiology of Sepsis American Journal of PathologyStella Gracia OctaricaBelum ada peringkat
- Pathophysiology of Venous UlcerationDokumen10 halamanPathophysiology of Venous UlcerationcumbredinBelum ada peringkat
- Hemostatic Complications of Solid OrganDokumen18 halamanHemostatic Complications of Solid OrganWael AlkhiaryBelum ada peringkat
- Leg UlcersDokumen14 halamanLeg UlcersNovi Y'uZzmanBelum ada peringkat
- Lymphedema ReviewDokumen8 halamanLymphedema ReviewSAKAI69Belum ada peringkat
- Pathophysiology of Chronic Venous Disease and Venous UlcersDokumen11 halamanPathophysiology of Chronic Venous Disease and Venous UlcersBolivar IseaBelum ada peringkat
- BCP 14752Dokumen13 halamanBCP 14752Story WA DokterBelum ada peringkat
- Review: Peripheral Vascular Disease and Virchow's Triad For ThrombogenesisDokumen12 halamanReview: Peripheral Vascular Disease and Virchow's Triad For ThrombogenesisastriaciwidyaBelum ada peringkat
- Agnogenic Myeloid Metaplasia: Splenectomy: Charles MarksDokumen5 halamanAgnogenic Myeloid Metaplasia: Splenectomy: Charles MarksMuhammad RidwanBelum ada peringkat
- Liv VasDokumen24 halamanLiv Vasdrvishnu21Belum ada peringkat
- Jadaon - 2011 - Epidemiology of Activated Protein C Resistance and Factor V Leiden Mutation in The Mediterranean RegionDokumen11 halamanJadaon - 2011 - Epidemiology of Activated Protein C Resistance and Factor V Leiden Mutation in The Mediterranean RegionnadaBelum ada peringkat
- Blue Toe SyndromeDokumen20 halamanBlue Toe SyndromeDaeng MakelloBelum ada peringkat
- EsplenomegaliaDokumen24 halamanEsplenomegaliaJhonatan Efraín López CarbajalBelum ada peringkat
- Calciphylaxis Controversies in Pathogenesis, DiagDokumen11 halamanCalciphylaxis Controversies in Pathogenesis, DiagJosh Jimenez RochaBelum ada peringkat
- Superficial Thrombophlebitis Follow-Up Study: Legs: Randomized, ControlledDokumen7 halamanSuperficial Thrombophlebitis Follow-Up Study: Legs: Randomized, ControlledFlorin BzoviiBelum ada peringkat
- Pulmonary Hypertension: Advances in Pathogenesis and TreatmentDokumen12 halamanPulmonary Hypertension: Advances in Pathogenesis and Treatmentbdalcin5512Belum ada peringkat
- Angio Displa SiaDokumen4 halamanAngio Displa SiaBelaFawziaBelum ada peringkat
- Coagulation DisordersDokumen26 halamanCoagulation DisordersLia pramita0% (1)
- Diagnostic Approach To Inherited Bleeding Disorders: Clinical Chemistry and Laboratory Medicine February 2007Dokumen12 halamanDiagnostic Approach To Inherited Bleeding Disorders: Clinical Chemistry and Laboratory Medicine February 2007Mohamed MounirBelum ada peringkat
- Vasculitis-Immunology and Localization: A ReviewDokumen2 halamanVasculitis-Immunology and Localization: A ReviewThaddaeus PercivalBelum ada peringkat
- EsclerodermiaDokumen15 halamanEsclerodermiaIvette Andrea HQBelum ada peringkat
- The Pathophysiology of Edema Formation in The Nephrotic SyndromeDokumen9 halamanThe Pathophysiology of Edema Formation in The Nephrotic SyndromeViswas ChhapolaBelum ada peringkat
- Sickle Cell Disease: A Paradigm For Venous Thrombosis PathophysiologyDokumen20 halamanSickle Cell Disease: A Paradigm For Venous Thrombosis PathophysiologyMuhammad SaeedBelum ada peringkat
- Cerebral Venous Thrombosis: Review ArticleDokumen7 halamanCerebral Venous Thrombosis: Review Articlechuck55Belum ada peringkat
- Acquired Thrombophilic Syndromes: Daniela Matei, Benjamin Brenner, Victor J. MarderDokumen18 halamanAcquired Thrombophilic Syndromes: Daniela Matei, Benjamin Brenner, Victor J. MarderRahmat SuhitaBelum ada peringkat
- Recurrent Leg Ulcers in A Young Man With HyperhomoDokumen4 halamanRecurrent Leg Ulcers in A Young Man With HyperhomoalfonsoBelum ada peringkat
- Coagulation DisordersDokumen26 halamanCoagulation DisordersLia pramitaBelum ada peringkat
- Portal Vein Thrombosis: ReviewDokumen9 halamanPortal Vein Thrombosis: ReviewMahmoud AbouelsoudBelum ada peringkat
- Rheology For CliniciansDokumen8 halamanRheology For CliniciansRaluca LBelum ada peringkat
- Contemporary Management of Major Haemorrhage in Critical CareDokumen13 halamanContemporary Management of Major Haemorrhage in Critical CareYo MeBelum ada peringkat
- En V7n2a07Dokumen18 halamanEn V7n2a07Amalia PutriBelum ada peringkat
- M 105Dokumen8 halamanM 105midwfjessica4Belum ada peringkat
- Hematologic Changes in SepsisDokumen16 halamanHematologic Changes in SepsisnisaBelum ada peringkat
- Source: Price, Sylvia A & Wilson, Lorraine M. 2006. Patofisiologi E/6 Vol. 1. Jakarta: EGC (Hal: 292)Dokumen7 halamanSource: Price, Sylvia A & Wilson, Lorraine M. 2006. Patofisiologi E/6 Vol. 1. Jakarta: EGC (Hal: 292)ridwanBelum ada peringkat
- Patofisiologi Ulkus VarikosumDokumen5 halamanPatofisiologi Ulkus VarikosumLidya ChristyBelum ada peringkat
- 6Dokumen8 halaman6soledadDC329Belum ada peringkat
- Hemodynamics and Diagnosis Venous Disease-Jvs 1207Dokumen21 halamanHemodynamics and Diagnosis Venous Disease-Jvs 1207Fahrudin ŠabanovićBelum ada peringkat
- AtherosclerosisDokumen38 halamanAtherosclerosisaffansungkarBelum ada peringkat
- Aimee - Cutaneous and Systemic PlasmacytosisDokumen3 halamanAimee - Cutaneous and Systemic PlasmacytosisEva YustianaBelum ada peringkat
- Myeloproliferative Disordersandthe Hyperviscosity Sy NdromeDokumen18 halamanMyeloproliferative Disordersandthe Hyperviscosity Sy NdromeAhmad Harissul IbadBelum ada peringkat
- Spontaneous Bleeding in Thrombocytopenia - Is It Really Spontaneou 2018Dokumen7 halamanSpontaneous Bleeding in Thrombocytopenia - Is It Really Spontaneou 2018Janner S-RBelum ada peringkat
- Disseminated Intravascular Coagulopathy DICDokumen24 halamanDisseminated Intravascular Coagulopathy DICMassimiliano MalerbaBelum ada peringkat
- Ulceras Vasculares en MiDokumen11 halamanUlceras Vasculares en MiKarilBelum ada peringkat
- Sickle Cell AnemiaDokumen5 halamanSickle Cell Anemiaكل يوم فيديو ممتعBelum ada peringkat
- Platelet Factor 4 Is A Biomarker For Lymphatic-Promoted DisordersDokumen45 halamanPlatelet Factor 4 Is A Biomarker For Lymphatic-Promoted DisordersAlexandre Campos Moraes AmatoBelum ada peringkat
- Connective Tissue Diseases: Focus On Microcirculatory Bed: O.I. Zarudna, I.K. Venher, A.V. DovbushDokumen8 halamanConnective Tissue Diseases: Focus On Microcirculatory Bed: O.I. Zarudna, I.K. Venher, A.V. DovbushdjdBelum ada peringkat
- An Unusual Case of Polycythemia Vera With A Complication of Pancreatic PseudocystDokumen3 halamanAn Unusual Case of Polycythemia Vera With A Complication of Pancreatic PseudocystAgus PrimaBelum ada peringkat
- Case 1Dokumen7 halamanCase 1secretBelum ada peringkat
- Diagnostic Approach To Lower Limb EdemaDokumen6 halamanDiagnostic Approach To Lower Limb EdemarendhyBelum ada peringkat
- Deep Vein Thrombosis in Stroke Patients:: Eulogio R. SiosonDokumen6 halamanDeep Vein Thrombosis in Stroke Patients:: Eulogio R. SiosonDianti SuryonoBelum ada peringkat
- Defining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsDokumen7 halamanDefining The Thrombotic Risk in Patients With Myeloproliferative NeoplasmsZikry AuliaBelum ada peringkat
- Sferositosis HerediterDokumen18 halamanSferositosis HerediterMade Masagung KawiarthaBelum ada peringkat
- Plasmapheresis For AtherosclerosisDokumen10 halamanPlasmapheresis For AtherosclerosisEliDavidBelum ada peringkat
- Pediatric Coagulation DisordersDokumen15 halamanPediatric Coagulation DisorderslastrironauliBelum ada peringkat
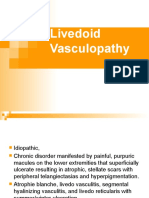
- Livedoid Vasculopathy A Review of Pathogenesis and Principles of ManagementDokumen11 halamanLivedoid Vasculopathy A Review of Pathogenesis and Principles of ManagementKata TölgyesiBelum ada peringkat
- Georgio Poul Ou 2010Dokumen17 halamanGeorgio Poul Ou 2010ireneaureliaBelum ada peringkat
- Anti-Neutrophil Cytoplasmic Antibody (ANCA) Associated VasculitisDari EverandAnti-Neutrophil Cytoplasmic Antibody (ANCA) Associated VasculitisRenato Alberto SinicoBelum ada peringkat
- Diseases of the Liver and Biliary TreeDari EverandDiseases of the Liver and Biliary TreeAnnarosa FloreaniBelum ada peringkat
- International Review of Experimental Pathology: Kidney DiseaseDari EverandInternational Review of Experimental Pathology: Kidney DiseaseG. W. RichterPenilaian: 5 dari 5 bintang5/5 (1)
- Growth Performance of Papaya Plants As Influenced by Organic MulchesDokumen9 halamanGrowth Performance of Papaya Plants As Influenced by Organic MulchesMa. Christine Lyn AustriaBelum ada peringkat
- Cultures of The West A History, Volume 1 To 1750 3rd PDFDokumen720 halamanCultures of The West A History, Volume 1 To 1750 3rd PDFtonnyBelum ada peringkat
- Unit-4.Vector CalculusDokumen32 halamanUnit-4.Vector Calculuskhatua.deb87Belum ada peringkat
- Assignment ProblemDokumen3 halamanAssignment ProblemPrakash KumarBelum ada peringkat
- ATMPP Diabetes Change and Review Proposal Npa 2012-18Dokumen8 halamanATMPP Diabetes Change and Review Proposal Npa 2012-18Juha TamminenBelum ada peringkat
- ToobaKhawar 6733 VPL Lab Sat 12 3 All TasksDokumen38 halamanToobaKhawar 6733 VPL Lab Sat 12 3 All TasksTooba KhawarBelum ada peringkat
- Present Perfect Mind MapDokumen2 halamanPresent Perfect Mind MappaulssBelum ada peringkat
- Tata Motors - Strategic ManagementDokumen16 halamanTata Motors - Strategic ManagementVaishakh MenonBelum ada peringkat
- Zielinski AnArcheology For AnArchivesDokumen10 halamanZielinski AnArcheology For AnArchivesPEDRO JOSEBelum ada peringkat
- R820T Datasheet-Non R-20111130 UnlockedDokumen26 halamanR820T Datasheet-Non R-20111130 UnlockedKonstantinos GoniadisBelum ada peringkat
- Amended August 8 2016Dokumen31 halamanAmended August 8 2016lux186Belum ada peringkat
- 5EMA BB Dem&Sup VW Bu&Se - 2.35&48&PDDokumen13 halaman5EMA BB Dem&Sup VW Bu&Se - 2.35&48&PDkashinath09Belum ada peringkat
- 4148-Article Text-14752-1-10-20211029Dokumen7 halaman4148-Article Text-14752-1-10-20211029Daffa AzkaBelum ada peringkat
- RCD - SEF (Liquidating)Dokumen40 halamanRCD - SEF (Liquidating)Chie NemzBelum ada peringkat
- Likert Scale Video Presentation RubricsDokumen1 halamanLikert Scale Video Presentation RubricsALDWIN B. BAYLONBelum ada peringkat
- Fulltext PDFDokumen454 halamanFulltext PDFVirmantas JuoceviciusBelum ada peringkat
- A. in What Way Is Khatri A Surplus Unit?Dokumen5 halamanA. in What Way Is Khatri A Surplus Unit?Aakriti SanjelBelum ada peringkat
- Logical Database Design ModelingDokumen2 halamanLogical Database Design ModelingGio Agudo100% (1)
- DrosteDokumen4 halamanDrosteapi-478100074Belum ada peringkat