CH Screening Cord Blood
Diunggah oleh
Kumar Gavali SuryanarayanaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
CH Screening Cord Blood
Diunggah oleh
Kumar Gavali SuryanarayanaHak Cipta:
Format Tersedia
RESEARCH LETTERS
Congenital Hypothyroidism rising trend in TSH. Out of these 41 cases, eight cases were
diagnosed to have hypothyroidism on follow-up; six on
Screening with Umbilical Cord day 5 and two on day 14. Cord blood TSH values and the
Blood: Retrospective Analysis number of hypothyroidism cases within each group are
provided in Table I. Congenital hypothyroidism was
diagnosed in 8 cases.
Incidence of congenital hypothyroidism varies across countries Cord blood TSH was >20 mU/L in all samples, except
and different geographic regions. A retrospective analysis of cord one where it was 18 mU/L. One baby showed a goiter in
blood thyroid stimulating hormone values, and their subsequent radionuclide scanning, whereas maternal hypothyroidism
follow-up, was done in a tertiary-care center in Kerala, India.
was present in two infants, and maternal hyperthyroidism
Congenital hypothyroidism was found at the rate of 1 in 244, which
is higher than reported incidence from other centers. in one child. No specific cause was found in the other five
babies.
Keywords: Congenital hypothyroidism, Incidence, Goiter.
A cord blood cut-off of 20 mU/L is considered
reasonable but it might be prudent to rescreen babies with
Congenital hypothyroidism has a worldwide incidence of a cord blood TSH above 10, as one of our patients had a
1 in 4000. A higher incidence has been reported from India cord blood TSH of 18 mU/L. Taking a cord blood TSH of
[1]. The objective of our study was to ascertain the 10 mU/L as cut off, our false positivity was 20%. Results
incidence of congenital hypothyroidism in South Malabar from this study population show a higher incidence of
area. congenital hypothyroidism than that has been reported
Our study was conducted in a tertiary care hospital in from other countries [3-5] or from other parts of India
Calicut, Kerala. We conducted a retrospective analysis of [1,6,7]. Increase in incidence within the same country over
umbilical cord thyroid stimulating hormone (TSH) values. subsequent years also has been reported [8]. The incidence
All inborn deliveries – from October 2012 to October of primary hypothyroidism vary depending on dietary
2013 – in a tertiary care hospital in Calicut, Kerala, were iodine sufficiency, laboratory methods of screening,
included. TSH, FT4 and FT3 were assayed by different test cut-off values, and demographic, geographic,
chemiluminiscent immunoassay method. A mixed cord racial and ethnic factors. Social customs like
blood sample obtained soon after birth was sent consanguinity also alter the incidence [9]. Transient
immediately for assay TSH. All cord blood TSH values of hypothyroidism also may contribute to varying prevalence
more than 10 mU/L were followed up at 72 hours of age [4]. Cord blood TSH provides a suitable first line
with a repeat TSH estimation. Those babies with a rising diagnosis congenital hypothyroidism, especially when a
trend in TSH were evaluated with TSH, FT4 and FT3 on 72-hour screen cannot be ensured. This study has
day 5 of life. Subsequent follow up was done at 2 weeks of limitations of being a hospital-based retrospective study.
age in individual cases. Congenital hypothyroidism was
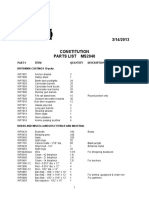
diagnosed if TSH on day 5 was >40 mU/L with a low FT4 TABLE I DISTRIBUTION OF HYPOTHYROIDISM CASES ACCORDING
or if at 2 weeks of age the TSH >10 mU/L with low FT4 TO CORD BLOOD TSH LEVELS
[2]. Radio nuclear scanning was not done in all cases prior
to treatment. Data retrieved from electronic medical Cord blood TSH (mU/L) No. Hypothyroidism cases
records were analyzed by SPSS version 16. >100 3 3
We excluded 120 cases from the analysis, which 90 -100 1 0
included perinatal deaths, those lacking adequate follow 60-70 1 1
ups, and those where a proper cord blood sample could not 50-60 4 0
be obtained. Total numbers of samples included in the 40-50 4 0
analysis were 1950 (1268 female) out of which 1551 were 30-40 13 1
term and 397, preterm. Median cord blood TSH value was
20-30 43 2
6.5 mU/L. Based on our policy of rescreening those with a
cord TSH of >10 mU/L, 403 babies needed rescreening at 10-20 334 1
72 hours. Upon rescreening at 72 hrs, 41 babies had a <10 1549 0
INDIAN PEDIATRICS 435 VOLUME 52__MAY 15, 2015
RESEARCH LETTERS
In view of higher incidence reported here, prospective hypothyroid screening using cord blood TSH. Singapore
studies on a larger population are needed to confirm the Med J. 1999;40:23-6.
findings and elucidate the reasons for the increased 4. Nascimento ML, Silva PC, Simoni G, Lobo GS, Souza CD.
incidence. Congenital hypothyroidism screening programme
preliminary results. J Pediatric (Rio J). 1997;73:176-9.
Contributors: AMR: conceived and designed the study, data 5. Ordookhani A, Mirmiran P, Najafi R, Hedayati M, Azizi F.
collection and analysis, and manuscript preparation. He will act Congenital hypothyroidism in Iran. Indian J Pediatr.
as the guarantor; PR and DN: data collection and preparation of 2003;70:625-8.
the manuscript. The final version was approved by all authors. 6. Kaur G, Srivastav J, Jain S, Chawla D, Chavan BS, Atwal
Funding: None; Competing interests: None stated. R, et al. Preliminary report on neonatal screening for
congenital hypothyroidism, congenital adrenal hyperplasia
*MR ANAND, PREETHA RAMESH AND DIVIA NATH and glucose-6-phosphate dehydrogenase deficiency: a
Department of Neonatology, Malabar Institute of Medical Chandigarh experience. Indian J Pediatr. 2010;77:969-73.
Sciences, Calicut, Kerala, India. *amr2003in@yahoo.co.in 7. Manglik AK, Chatterjee N, Ghosh G. Umbilical cord blood
REFERENCES TSH levels in term neonates: a screening tool for congenital
hypothyroidism. Indian Pediatr. 2005;42:1029-32.
1. Sanghvi U, Diwakar KK. Universal screening for 8. Dilli D, Çzbaº , Acican D, Yamak N, Ertek M, Dilmen U.
congenital hypothyroidism. Indian Pediatr. 2008;45:331-2. Establishment and development of a national newborn
2. Bhatia V. Congenital hypothyroidism is not always screening programme for congenital hypothyroidism in
permanent: caveats to newborn thyroid screen Turkey. J Clin Res Pediatr Endocrinol. 2013;5:73-9.
interpretation. Indian Pediatr. 2010;47:753-54. 9. Desai MP. Congenital hypothyroidism: screening
3. Wu LL, Sazali BS, Adeep N, Khalid BA. Congenital dilemma. Indian J Endocrinol Metab. 2012;16:153-5.
Iodine Status among School we enrolled 292 school children (108 from 2 schools and a
monastery of Shree Antu and 184 from 2 schools of
Children of remote Hilly regions of Ranke) aged 6-12 years by random number generation
Nepal using random number tables. We selected 6-12 years age
children because of greater impact of iodine-deficiency on
A cross-sectional study was conducted in remote hilly areas
them, and their easy availability through schools. Consent
(Shree Antu and Ranke) of eastern Nepal to assess iodine status was taken from guardian of children, and ethical clearance
.
among school children aged 6-12 years. Urinary iodine excretion from Institute Review Board of B P Koirala Institute of
was estimated in 292 urine samples. The median urinary iodine Health Sciences (BPKIHS) in 2012. About 10 mL of urine
excretion was 187.52 μg/L, and 33.6% children have insufficient
urinary iodine excretion.
samples were collected in clean plastic vials and
transported to biochemistry laboratory of BPKIHS
Keywords: Iodine deficiency, Nepal, Urinary iodine excretion. maintaining cold chain. UIE was estimated using
ammonium persulphate digestion method [3].
People living in mountainous and hilly regions of Nepal The median UIE in our study was 187.52 μg/L (227.53
have been found to be more iodine-deficient than those μg/L in Shree Antu and 175.45 μg/L in Ranke), which
living in the plain regions. A national survey in 2007 indicates adequate iodine nutrition among the children of
showed that 18.9% school children were iodine-deficient hilly regions [4]. Median UIE among boys and girls was
in the eastern hills [1]. Considering the reported low iodine 205.66 μg/L and 150.84 μg/L, respectively. Median UIE
in soil of this region [2], and the frequent non-availability was significantly different among genders (P=0.014) and
of iodized salts in remote hilly regions, we designed a among study areas (P=0.003). Iodine status on basis of
cross-sectional study for assessing iodine status in school UIE (WHO criteria) in the study areas and gender is shown
children of these regions. in Table I, which shows 33.6% children had UIE<100 μg/
L [4].
We selected Shree Antu (Ilam) and Ranke (Panchthar)
areas for sample collection after choosing Ilam and Nepal has been continuously improving in iodine
Panchthar as the representative hilly districts. Shree Antu nutrition [5]. The median UIE in our study was lower than
and Ranke areas are at high altitude of 3400 meters and in the study of Gelal, et al. [6], who has shown median UIE
2100 meters from sea level, respectively. Considering of 208.9 μg/L in hilly region. This suggests that
present iodine deficiency of 20% (approximate) in hills, improvement in median UIE is non-uniform within the
INDIAN PEDIATRICS 436 VOLUME 52__MAY 15, 2015
Anda mungkin juga menyukai
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Pathoftherosesyllabus2015 1 PDFDokumen12 halamanPathoftherosesyllabus2015 1 PDFsperm100% (7)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Gulika in Vedic AstrologyDokumen8 halamanGulika in Vedic AstrologyCatchdgreen100% (1)
- Emergency Department PolicyDokumen18 halamanEmergency Department PolicyKumar Gavali Suryanarayana100% (1)
- Spinal & Epidural AnaesthesiaDokumen31 halamanSpinal & Epidural AnaesthesiaKumar Gavali Suryanarayana0% (1)
- Kids and Their Favourite Food Key Reading Comprehension Exercises - 34436Dokumen2 halamanKids and Their Favourite Food Key Reading Comprehension Exercises - 34436MonicaMartirosyanBelum ada peringkat
- Weekly Calendar Landscape 5Dokumen1 halamanWeekly Calendar Landscape 5Duncan BusserBelum ada peringkat
- Neonatal Screening For Congenital Hypothyroidism Using Cord Blood Thyroid Stimulating HormoneDokumen3 halamanNeonatal Screening For Congenital Hypothyroidism Using Cord Blood Thyroid Stimulating HormoneKumar Gavali SuryanarayanaBelum ada peringkat
- Name: Project: Quarter: Q2, 2013 (April-June) : Activity April MAY June WK1 WK2 WK3 WK4 WK1 WK2 WK3 WK4 WK1 WK2 WK3Dokumen2 halamanName: Project: Quarter: Q2, 2013 (April-June) : Activity April MAY June WK1 WK2 WK3 WK4 WK1 WK2 WK3 WK4 WK1 WK2 WK3Kumar Gavali SuryanarayanaBelum ada peringkat
- Indian Railway Seat LayoutDokumen1 halamanIndian Railway Seat LayoutHarshmani Gupta100% (1)
- Quantitative Vs Qualitative Research MethodsDokumen9 halamanQuantitative Vs Qualitative Research MethodsKumar Gavali SuryanarayanaBelum ada peringkat
- Nephrotic Syndrome: Symposium On Pediatric NephrologyDokumen11 halamanNephrotic Syndrome: Symposium On Pediatric NephrologyKumar Gavali SuryanarayanaBelum ada peringkat
- Routine Exam NewbornDokumen18 halamanRoutine Exam NewbornKumar Gavali SuryanarayanaBelum ada peringkat
- Health Problems of Tribal Population Groups From The State of MaharashtraDokumen7 halamanHealth Problems of Tribal Population Groups From The State of MaharashtraKumar Gavali SuryanarayanaBelum ada peringkat
- CTRegistrationDokumen1 halamanCTRegistrationnami939Belum ada peringkat
- Fetal Valproate SyndromeDokumen8 halamanFetal Valproate SyndromeKumar Gavali SuryanarayanaBelum ada peringkat
- Interpretation of LR PDFDokumen6 halamanInterpretation of LR PDFKumar Gavali SuryanarayanaBelum ada peringkat
- MDR Tbguide 20mar2013Dokumen257 halamanMDR Tbguide 20mar2013Enrique SwayneBelum ada peringkat
- ARTI in Rural MysoreDokumen3 halamanARTI in Rural MysoreKumar Gavali SuryanarayanaBelum ada peringkat
- EfCats Talking TipsDokumen13 halamanEfCats Talking TipsKendall SmithBelum ada peringkat
- Brochure FellowshipDokumen2 halamanBrochure FellowshipKumar Gavali SuryanarayanaBelum ada peringkat
- Pyomyositis of MusclesDokumen4 halamanPyomyositis of MusclesKumar Gavali SuryanarayanaBelum ada peringkat
- Data Entry With ExcelDokumen36 halamanData Entry With ExcelKumar Gavali SuryanarayanaBelum ada peringkat
- Status of StatusDokumen2 halamanStatus of StatusKumar Gavali SuryanarayanaBelum ada peringkat
- Acute Adrenal Crisis in Criticall IllDokumen4 halamanAcute Adrenal Crisis in Criticall IllKumar Gavali SuryanarayanaBelum ada peringkat
- Ocular Manifestations of HIVDokumen4 halamanOcular Manifestations of HIVKumar Gavali SuryanarayanaBelum ada peringkat
- Taiwan API Manufacturer ListDokumen4 halamanTaiwan API Manufacturer Listkalyani dynamicsBelum ada peringkat
- MS2040 Constitution Parts ListDokumen6 halamanMS2040 Constitution Parts ListTemptationBelum ada peringkat
- LEVEL 2-Anxiety-Adult (PROMIS Emotional Distress-Anxiety - Short Form)Dokumen1 halamanLEVEL 2-Anxiety-Adult (PROMIS Emotional Distress-Anxiety - Short Form)alemsaudementalBelum ada peringkat
- Architect As An Environmental PlannerDokumen14 halamanArchitect As An Environmental PlannerJames Adrian MoralBelum ada peringkat
- Second Term English Exam: Level TCST June 2021Dokumen6 halamanSecond Term English Exam: Level TCST June 2021benfaresBelum ada peringkat
- J. Agric. Food Chem. 2005, 53, 9010-9016Dokumen8 halamanJ. Agric. Food Chem. 2005, 53, 9010-9016Jatyr OliveiraBelum ada peringkat
- Annals of The New York Academy of Sciences - 2023 - Hess - Accelerating Action To Reduce Anemia Review of Causes and RiskDokumen13 halamanAnnals of The New York Academy of Sciences - 2023 - Hess - Accelerating Action To Reduce Anemia Review of Causes and RiskIdmBelum ada peringkat
- Coulomb's Law and Electric Field Intensity: Engineering ElectromagneticsDokumen24 halamanCoulomb's Law and Electric Field Intensity: Engineering ElectromagneticsKenn SenadosBelum ada peringkat
- Catalogo Smartline Transmitter Family Ferrum Energy 变送器Dokumen12 halamanCatalogo Smartline Transmitter Family Ferrum Energy 变送器peng chaowenBelum ada peringkat
- ITAD BIR RULING NO. 026-18, March 5, 2018Dokumen10 halamanITAD BIR RULING NO. 026-18, March 5, 2018Kriszan ManiponBelum ada peringkat
- RB in Poultry Feed - 3Dokumen17 halamanRB in Poultry Feed - 3Vishwanath HebbiBelum ada peringkat
- CP Inf4Dokumen357 halamanCP Inf4Rugwed JadhavBelum ada peringkat
- AngelDokumen21 halamanAngelNoj ZachBelum ada peringkat
- PX 150 UsaDokumen138 halamanPX 150 UsaramiroBelum ada peringkat
- Vivo X5Pro Smartphone Specifications: Brand and ModelDokumen4 halamanVivo X5Pro Smartphone Specifications: Brand and ModelEric AndriantoBelum ada peringkat
- VisakhapatnamDokumen27 halamanVisakhapatnamCherukupalli Gopala KrishnaBelum ada peringkat
- Parker - Twin FilterDokumen6 halamanParker - Twin FilterNAHASALI11Belum ada peringkat
- CatalogDokumen52 halamanCatalogtalabiraBelum ada peringkat
- A Guide To Maintenance Metrics-ProgramDokumen5 halamanA Guide To Maintenance Metrics-ProgramLy QuanBelum ada peringkat
- SCSM 2022 Runners Information GuideDokumen36 halamanSCSM 2022 Runners Information GuideDollar SurvivorBelum ada peringkat
- Brunei 2Dokumen16 halamanBrunei 2Eva PurnamasariBelum ada peringkat
- Corrosion Resistant Steels: Stainless Steel AlloysDokumen11 halamanCorrosion Resistant Steels: Stainless Steel AlloysPraveen SamarthiBelum ada peringkat
- Gas Permeability, Diffusivity and Solubility of Nitrogen, Helium, Methane, CO2, CH2O in Dense Polymeric Membranes Using A New On-Line Permeation ApparatusDokumen12 halamanGas Permeability, Diffusivity and Solubility of Nitrogen, Helium, Methane, CO2, CH2O in Dense Polymeric Membranes Using A New On-Line Permeation ApparatusCinthiaCevallosBelum ada peringkat
- Pre Post Tests For HPPDokumen3 halamanPre Post Tests For HPPapi-434982019Belum ada peringkat
- Bearing Solutions and Service For Wind TurbinesDokumen16 halamanBearing Solutions and Service For Wind TurbinesDrZEIDIBelum ada peringkat
- StringTokenizer in JavaDokumen11 halamanStringTokenizer in JavaNeha saxena Neha saxenaBelum ada peringkat
- Calibrating Images TutorialDokumen14 halamanCalibrating Images TutorialtrujillomadrigalBelum ada peringkat