Burns Chapter
Diunggah oleh
galih widodoJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Burns Chapter
Diunggah oleh
galih widodoHak Cipta:
Format Tersedia
24 Plastic & Reconstructive Surgery
BURN SCAR CONTRACTURES & THEIR MANAGEMENT
K Walsh, D Nikkhah, B Dheansa
Burn scar contractures & their management
Plastic & Reconstructive Surgery
The LD50 (the lethal dose of burn in 50% of the population) in 1950 for a 21
year old was 40% total body surface area (TBSA), but now that figure is 90%.
This is due to improvements in the management of a burn injury (first aid,
fluid management, antibiotics, intensive care and surgery) (1). However, the
LD50 in the elderly population remains much lower at 40%. This is related to
other co-morbidities, longer hospital stay, poor wound healing, predisposition
to sustaining deeper burns as the skin is thinner and first aid may be limited
if they live alone.
Once a patient has been resuscitated, efforts are then made to improve
wound healing in order to prevent scarring and contractures. Contractures
Abstract lead to a loss of function, poor cosmetic outcome, reduced quality of life
In this article we discuss the different surgical approaches to burn scar (QOL), pain and psychological consequences (3,4). Function is determined
contractures. Burn scar contractures can lead to a poor functional and cosmetic by the range of movement (ROM) at a joint. Therefore the most important
outcome as well as possible psychological consequences. We describe the contracture sites are the joints of the upper limb, neck, mouth, trunk and
benefits and complications of the different modalities of treatment. By the knees. These contractures can impair the patient’s ability to move, to dress, to
end of this article the core trainee should be able to describe the different eat or drink and perform fine skills. Contractures of the neck, axilla and hand
types of management options for preventing and treating burn contractures. are shown in figures 1-4.
Keywords: burn, scar contracture.
Case Report
A 7 year old male presented to hospital with a 2% burn over his right
elbow due to a scald from boiling water. No first aid was applied when
the injury happened 2 hours previously. The burn was mixed in depth but
examination revealed the wound did not blanch, was not painful and was
pale in appearance indicating a dermal burn. In the following days a split
skin graft was performed along with the application of a splint. With active
physiotherapy over the course of 6 months, the range of movement was
normal with minimal scarring.
Introduction
Burns constitute the second highest incidence of trauma related deaths
globally, second to vehicular trauma (1). Within the U.K 250,000 burn injuries Figure 1: A thick linear contracture band
occur each year in which 1000 people are admitted to hospital and 300 of the neck and peri-orbital contractures.
patients die (2).
The most common mechanism of injuries are scald and flame burns,
accounting for 45% and 20% of burn injuries respectively. Flame burns
usually result in an increased depth of burn. Chemical and electrical burns are
less prevalent (<10%) (2).
FOR MORE INFORMATION, EMAIL INFO@123DOC.COM
Plastic & Reconstructive Surgery 25
BURN SCAR CONTRACTURES & THEIR MANAGEMENT
K Walsh, D Nikkhah, B Dheansa
Figure 2: Axillary contracture. Axillary contractures greatly reduce the Figure 4.
range of abduction, flexion and extension of the shoulder. Release of
axillary contractures greatly improves the quality of life for such patients. Pathophysiology of Scars and Contracture
Superficial partial thickness burns rarely lead to scarring. Conversely, deep
dermal or full thickness burns extend to the dermal reticulare, which destroys
the epidermal appendages and their extensions into the dermis. The wound
is less able to spontaneously epithelise and wound closure occurs from just
the wound edge rather from the central portion of the wound (1,5). This
leads to a delay in wound healing which increases the risk of scarring.
Deep dermal burns may lead to hypertrophic scarring. Peacock defines
hypertrophic scarring as: ‘a scar raised above the skin level that stays
within the confines of the original lesion’ (1,6). There is an over-proliferative
response of wound healing leading to excessive deposition of collagen and
ground substance. Collagen type III is the predominant connective tissue type
and is structurally disorganised and nodular (7).
Myofibroblasts proliferate at a wound site which causes the wound edges
to contract towards one another. Delayed healing and scar formation leads
Figure 3 and 4: Contractures of the Hand. Contractures of the palmar to an over-proliferation of myofibroblasts causing pathological contracture.
aspect of the hand form fixed flexion deformities. Figure 3 shows a Hypertrophic scars usually occur within the first three months of a burn
linear contracture band on the palmar aspect of the middle finger. injury. Dietch et al. concluded that one third of anatomical sites became
The little finger is unable to extend at the Proximal Interphalangeal hypertrophic if the healing time occurred between 14-21 days. After 21 days,
Joint and at the Distal Interphanageal Joint. Figure 4. Contracture 78% of scars became hypertrophic (8). Recognised factors which may delay
along the dorsal aspect of the thumb and the webspace between the wound healing include infection, smoking, supressed immune system, age,
dorsal aspect of the thumb and index finger limit the ability to form poor circulation and nutrition. Such factors may delay wound healing causing
a tight fist and grip. breakdown of the wound.
SUBSCRIBE TO AN ONLINE E-COURSE, VISIT WWW.123DOC.COM
26 Plastic & Reconstructive Surgery
BURN SCAR CONTRACTURES & THEIR MANAGEMENT
K Walsh, D Nikkhah, B Dheansa
Burn scar contractures & their management
Plastic & Reconstructive Surgery
Vancouver Scar Scale
Assessment of a contracture should begin with documenting the area and the
characteristics of the contracture. These include its laxity, whether it is linear
or a plaque and if the surrounding skin is burnt or scarred. Timing of surgery
The incidence of pain and pruritus are common during scar formation. is dictated by whether the surgery is an emergency. For example areas
These symptoms are both distressing for patients. Unfortunately, the exact which may limit the patient’s airway: the neck or tissues surrounding the
pathophysiological causes for these symptoms have not been elucidated. mouth. Contractures at the axilla require urgent release as they can quickly
It hypothesised to be due to histamine or kinin formation activating C-fibre lead to debilitating function of the shoulder, particular limiting the range of
nociceptors (5). abduction. Priority should also be given to proximal structures compared to
distal structures. There is no point releasing a web-space, if the patient is
Scar and Contracture Assessment unable to move their entire upper limb due to an axillary contracture (11).
The Vancouver Scar Scale (VSS) is one method to measure scars (as shown
in Table 1). The VSS attributes scar contractures with a score indicating a A history should be taken to determine problems involving self-care, social or
poor outcome of scar development (9). The VSS is widely used, although it work related problems. For example, a patient may be unable to bring their
is widely known to lack reliability and there are issues concerning observer hand towards their mouth in order to eat and subsequently would benefit
variability. VSS does not also rate itching or pain (10). A scar should be from surgery.
reviewed in clinics and the VSS score should be recorded to see whether
the scar deteriorates. Prevention of Burn Contractures
It is far better principle to prevent contractures rather than treat them. Major
burn cases have declined due to improvements in health and safety at work
and domestically (12). First aid is vital to prevent burn extending deep into
the dermis. First aid should include removal of clothes at the site of burn,
placing the injured site under a tepid tap of water for a minimum of 20
minutes and wrapping the site in cling film. Upon admission, burns should be
assessed to gauge the size, the depth of burn and the mechanism of injury.
This is a priority but unfortunately burns are not always assessed sufficiently.
One study showed 30% of patients performed appropriate first aid and
furthermore74% of burns upon admission were not assessed adequately (2).
Laser Doppler Imaging (LDI) is used to determine the blood flow at the burn
injury site. This provides an accurate description at the depth of the burn. It is
a useful aid to deciding when a burn will likely heal. LDI is used between 2-5
days following a burn injury.
Table 1.
FOR MORE INFORMATION, EMAIL INFO@123DOC.COM
Plastic & Reconstructive Surgery 27
BURN SCAR CONTRACTURES & THEIR MANAGEMENT
K Walsh, D Nikkhah, B Dheansa
A clinician should determine from their assessment if the burn is likely to
heal before or after 21 days. Cubison et al. concluded that there is a low risk
of hypertrophic scarring if the burn healed conservatively before 21 days.
Only intermediate burns that are expected to heal after 21 days were likely
to develop a hypertrophic scar should receive primary excision and skin graft.
Burns expected to heal before 21 days may be dressed with Biobrane, skin
allografts or with simple dressings. Biobrane is a biosynthetic silicon dressing
which contains an embedded sheet of nylon. This is left on the wound and
provides the wound with a 3D structure to heal to. The nylon sheet causes
blood and sera to clot forming a firm dressing (13). Cadaveric allografts
provide temporary closure of the wound. Such allografts behave like normal
skin but are rejected may require replacement. Application of such dressings Early Scar and Contracture Management
help to prevent early desiccation, prevent infection, reduce loss of water or
proteins and electrolytes. • Medical Options
There are lots of methods for early scar management. Splintage and
There is general agreement that major burns should be treated with physiotherapy, described previously, are incorporated into early contracture
aggressive excision and skin grafting. Split skin grafts (SSGs) should only management. Physiotherapy should be goal orientated and suit the individual
be reserved for burns likely to heal after 21 days (5). Large burns require needs e.g. going back to work or to be able to perform everyday tasks (17).
multiple operations and areas should be prioritised. Potentially, early excision Splintage and physiotherapy are used following surgery for contracture release.
and skin grafts will be delayed at certain sites, leading to prolonged healing
time and scarring. Also, the total amount of skin available for a graft should Moisturising and massaging the wound improves pliability of the scar,
be determined. A shortage of skin will require the use of a mesh graft as particularly if the scar is dry and uncomfortable. Corticosteroid injections are
opposed to a sheet split skin graft. A mesh graft however will contract greater also used to treat scars. 1mg of steroid is injected at sites 1 cm2 apart. Steroid
than a sheet SSG. injections take place every 6 weeks.
Schneider et al. concluded the importance of therapeutic positioning and Other forms of therapy include: application of silicone gel, wearing pressure
intensive therapy intervention. The study of 985 patients concluded that garments and the use of a laser to reduce scars. Such methods are
38.7% of patients developed a contracture at hospital discharge. The shoulder controversial as there is a plethora of literature which supports or refutes the
was the most common joint to undergo contracture (38%), followed by the effectiveness of each of these treatments.
elbow (34%) and the knee (22%) (14).
Surgical Options
Following a burn injury over the surface of a joint, splintage should be used to
place a joint in a position which will later allow a patient to maintain essential • Local Surgical Procedures
function e.g. eating, drinking, going to the toilet. There are a wide range of The Z-plasty is a commonly used local procedure for contracture release and
splints which stretch the skin and maintain positions of function (12, 15, 17). mainly used for bowstring contractures (11,12). The Z-plasty borrows skin
Burns to the flexor surface of the skin increase the risk of contracture as the from adjacent tissue sites to divide and lengthens the contracture band. As
flexor muscles are stronger than the extensors. Full co-operation is essential there is shortening within the transverse axis, there may be little room for
for reducing long term pain, providing a greater range of movement and further shortening with a z-plasty. A multiple z-plasty may be preferred as
reducing the requirement for further surgery. theoretically this reduces transverse shortening. The z-plasty should only
really be used when there is ample laxity of the surrounding tissue and not
Physiotherapy is important to prevent scar formation and limit contractures. in diffuse contractures.
Celis et al. showed that patients receiving additional, supportive physiotherapy
required less surgery for burn contractures than a group receiving basic The Y-V plasty (figure 5) is relatively simple to perform and is recommended
support (16). Adequate analgesia alongside patient education is a priority for linear bands. In comparison to the Z-plasty, the Y-V plasty does not require
as patients must move their affected joints despite perceived pain (14, 17). undermining, which reduces the risk of distal tip necrosis. Contractures can be
lengthened by 100%, whereas with a 60 degree Z-plasty, length is increased
by 75%. The Y-V plasty can also be repeated adjacently which is used when
there is a broad sheet of contracture. Patients are able to mobilise earlier
post-operatively than if the Z-plasty was chosen. Other techniques include,
the double reverse V-Y plasty and the W-plasty (11,12) (figure 6).
SUBSCRIBE TO AN ONLINE E-COURSE, VISIT WWW.123DOC.COM
28 Plastic & Reconstructive Surgery
BURN SCAR CONTRACTURES & THEIR MANAGEMENT
K Walsh, D Nikkhah, B Dheansa
Burn scar contractures & their management
Plastic & Reconstructive Surgery
• Flaps with and without tissue expanders
Free, local and fasciocutaneous flaps have been used to treat contractures
which limit the range of movement greater than 50%. Flaps are mainly
Figure 5. The V-Y plasty. used for broad sheet contractures. Within the upper limb, regional flaps
include; radial forearm fasciocutaneous flap, posterior interosseus artery flap,
latissimus dorsi flap or a propeller flap (12, 18, 19, 20). Often the scar tissue
can be used as part of the flap, however there is a potential risk of a poor
cosmetic outcome and diminished elasticity.
There are difficulties with the use of a free flap. A free flap is limited by the
amount of skin taken from a donor site. This donor site would require a SSG
which could potentiate contracture. Dissection of recipient vessels to connect to
the flap is difficult due to the distortion of tissue from the scar. Free flaps require
tissue to be imported which is of a different colour, bulk and texture (11). This
Figure 6. The W plasty. is can be overcome with the use of skin expanders however there are risks of
infection, skin ischaemia or leakage (11). In addition, the areas where tissue
expansion can be limited, particularly if the surrounding area is burnt.
FOR MORE INFORMATION, EMAIL INFO@123DOC.COM
Plastic & Reconstructive Surgery 29
BURN SCAR CONTRACTURES & THEIR MANAGEMENT
K Walsh, D Nikkhah, B Dheansa
• Skin Shortage
In comparison to full thickness skin grafts (FTSGs), split skin grafts (SSGs)
are easily harvested, can cover a larger area, release multiple joints and
broad sheet contractures. Unfortunately, SSGs are prone to form hypertrophic
scarring and further contracture of the wound site (1,5,11,12,14,17). If the
burn is large, a meshed split skin graft will lead to a greater degree of contract
than a sheet SSG. FTSGs have less contracture due to more dermis within the
graft. Conversely their take is dependent on a richer vascular bed (4,11). In
recent years SSGs have been incorporated with dermal templates.
Dermal templates consist of a bovine collagen matrix with an overlying
silicone sheet. Artificial skin substitutes lead to a reduced inflammatory
reaction and consequently reduced contracture. There are mixed reports of
their effectiveness at preventing contracture. Soejima et al. has reported
that in 75% of cases a good cosmetic outcome had been achieved with a
reduction in scar hypertrophy. However, Hunt et al. reported a high incidence
of re-contracture when dermal templates were used during neck contracture
release (11, 21, 22). Summary
• Surgical Planning After reading this article, the core trainee should be able to:
Large burns incorporate multifactorial obstacles such as a loss of function
to numerous joints and severe deformity. The surgeon should formulate 1) Understand the importance of adequate clerking of a burns patient
an organised plan for the entire rehabilitative process. The surgeon should 2) Be able to understand the pathophysiology of burns contracture
prioritise the order and time scale of surgical procedures so an earlier 3) Understand that the most important management
operation does not complicate future surgical procedures. Poor planning may of burns contracture is prevention
delay the rehabilitative process. This subsequently delays when a patient is 4) Assess a contracture
able to return to work or be able to support themselves. Also, one must think 5) Understand the principles of managing a burns contracture
of the cost effectiveness when planning the number of operations required.
Multiple operations may also need to be planned for the same time. The Q&A
surgeon should also be receptive to the patients’ needs. A scar contracture at
one joint may be more of a priority to a patient than the surgeon. This should 1) What is the most common mechanism of burn in the UK?
therefore be considered and the surgeon should be flexible in their plan for
the patients’ needs. A) Chemical
B) Electrical
Table for the Complications of Varying Treatments C) Scald
D) Flame
E) A cold burn
2) What period of healing time is associated with
the highest rate of hypertrophic scar formation?
A) 0 Day
B) 14 days
C) 21 days
D) 25 days
E) 30 days
SUBSCRIBE TO AN ONLINE E-COURSE, VISIT WWW.123DOC.COM
30 Plastic & Reconstructive Surgery
BURN SCAR CONTRACTURES & THEIR MANAGEMENT
K Walsh, D Nikkhah, B Dheansa
Burn scar contractures & their management
Plastic & Reconstructive Surgery
References:
1. Goel, A., Shrivastava, P. Post-burn scars and scar contractures. Indian
Jouornal of Plastic Surgery 2010; 43 63-71
2. Chipp, E., Walton, J., Gorman, D.F., Moiemen N.S. A 1 year study of burn
injuries in a British Emergency Department. Burns 2008: 34; 516-520
3. Egeland, B., More, S., Buchman, S.R., Cederna, P.S. Management of Difficult
Paediatric Facial Burns: Reconstruction of Burn-Related Lower Eyelid Ectropion
and Perioral Contractures. Journal of craniofacial surgery 2008: 19; 960-969
3) What is the main disadvantage of a Z-plasty
for the treatment of a contracture band? 4. Leblebici, B., Adam, M., Bagis, S., Tarim, A.M., Noyan, T., Akman, M.N.,
Haberal, M.A. Quality of life after burn injury: the impact of joint contracture.
A) A complication is ischaemia of the tip of the wound Journal of Burn Care Research 2006: 27; 864-868
B) Poor cosmesis
C) Recontracture 5. Cohen, I.K., Diegelmann, R.F., Lindblad, W..J. (1992) Wound Healing:
D) Requires flattening through physiotherapy Biochemical and clinical aspects. W.B Saunders Company, Philidelphia
E) Z-plasty does not dissect through the contracture
band as well as a Y-V band 6. Peacock ,Jr E.E., Madden, J.W., Trier, W.C. Biological basis for the treatment
of keloids and hypertrophic scars. Southern Medical Journal 1970: 63; 755-60
4) Which is not a principle of contracture removal?
7. Giele, H., Cassel, O. (2008). Oxford specialist handbooks in surgery: Plastic
A) A free flap is preferable to a skin graft and Reconstructive Surgery. 1st Edition. Oxford University Press, New York. PP
B) The distal joint should always be released before the proximal joint
C) Important underlying structures may need to be exposed 8. Dietch, E.A., Wheelahan, T.M., Rose, M.P., Clothier, J., Cotter, J. Hypertrophic
D) Each joint should be considered separately burn scars: analysis of variables. Journal of Trauma 1983: 77;744-751
E) Function should take priority over cosmesis
9. Cubison, T., Pape, S.A., Parkhouse, N. Evidence for the link between healing
Answers time and the development of hypertrophic scars (HTS) in paediatric burns due
to scald. Burns 2006: 32;992-999
1) C
2) E
3) A
4) B
Note: Written consent was obtained for figures 1-4.
Acknowledgements: Kate Murrell designed figures 5 and 6.
FOR MORE INFORMATION, EMAIL INFO@123DOC.COM
Plastic & Reconstructive Surgery 31
BURN SCAR CONTRACTURES & THEIR MANAGEMENT
K Walsh, D Nikkhah, B Dheansa
10. Idriss, N, Maibach, HI. Scar assessment scales: A dermatologic overview.
Skin Research and Technology 2009: 15(1); 1-5
11. Hudson, D.A., Renshaw, A. An algorithm for the release of burn
contractures of the extremities. Burns 2006: 32; 663-668
12. Schwarz., R.J.Management of postburn contractures of the upper
extremity. Journal of Burn Care research 2007: 28(2); 212-219
13. Book chapter: Boyd, JB. Burn Trauma. In Plastic and Reconstructive Surgery.
1st edition, Cleveland: Springer, 2006: 189-206.
14. Schneider, J.C., Holavanahalli, R., Helm, P., Goldstein, R., Kowalske, K.
Contractures in burn injury: defining the problem. Journal of burn care and
research 2006: 27(4); 508-514
15. Kwan, M.W., Ha, K.W. Splinting program for patients with burnt hand.
Hand Surgery 2002: 7; 231-241
16. Celis, M.M., Suman, O.E., Huang, T.T., Yen, P., Herndon, D.N. Effect of a
supervised exercise and phyisiotherapy program on surgical interventions in
children with thermal injury. Journal of burn care and rehabilitation 2003:
24(1); 57-61 Corresponding Author
17. Procter, F. Rehabilitation of the burn patient. Indian Journal of Plastic Karl Walsh
Surgery 2010: 43; 101-113 Queen Victoria Hospital,
Holtye Road,
18. Costa, H., Soutar, D.S. The distally based posterior interosseus fasciocutaneous East Grinstead RH19 3DZ
island flap. British Journal of Plastic Surgery 1988: 41; 221-226. Email: mosc7kw2@doctors.org.uk
19. Teo, T.C., Richard, B.M. The distally based posterior interosseous
fasciocutaneous island flap reconstruction flap in reconstruction of the hand
in leprosy. Indian Journal of Leprosy 1997: 69(1); 93-100
20. Aslan, G., Tuncali, D., Cigsar, B., Barutcu, A.Y., Terzioglu, A. The propeller
flap for burn postburn elbow contractures. Burns 2006: 32(1);112-115
21. Soejima, K., Nozaki, M., Sasaki, K., Takeuchi, M., Negishi, N. Reconstruction
of burn deformity using artifical dermis combined with thin split-grafting.
Burns 1997:23; 501-504
22. Hunt, J.A., Moisidis, E., Haertsch, P. Initial experience of Integra in the
treatment of post-burn anterior cervical neck contracture. British Journal of
Plastic Surgery 2000: 53(8); 652-658
SUBSCRIBE TO AN ONLINE E-COURSE, VISIT WWW.123DOC.COM
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- 2015 Article 12 PDFDokumen9 halaman2015 Article 12 PDFgalih widodoBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Bedah Anak: Peta Pasien Jum'At 30 Oktober 2015 Ayt/Dna/Pur/Imp/FerDokumen2 halamanBedah Anak: Peta Pasien Jum'At 30 Oktober 2015 Ayt/Dna/Pur/Imp/Fergalih widodoBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- Sabtuan Wonogiri 5 MowDokumen3 halamanSabtuan Wonogiri 5 Mowgalih widodoBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Case DR SADokumen16 halamanCase DR SAgalih widodoBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Bedah Anak: Peta Pasien Senin 2 November 2015 Galih/Ariya/Ond/Edr/Ayt/Map/Pur/Ben/Fer/VelDokumen2 halamanBedah Anak: Peta Pasien Senin 2 November 2015 Galih/Ariya/Ond/Edr/Ayt/Map/Pur/Ben/Fer/Velgalih widodoBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Clinical Case Advanced Breast CancerDokumen8 halamanClinical Case Advanced Breast Cancergalih widodoBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- LAPORAN EMERGENCY RSUD DR. SOEDIRAN MANGUN SOEMARSODokumen8 halamanLAPORAN EMERGENCY RSUD DR. SOEDIRAN MANGUN SOEMARSOgalih widodoBelum ada peringkat
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Liu Et Al-2016-Frontiers in Microbiology PDFDokumen9 halamanLiu Et Al-2016-Frontiers in Microbiology PDFgalih widodoBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
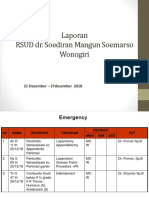
- Laporan RSUD Dr. Soediran Mangun Soemarso Wonogiri: 21 Desember - 27desember 2018Dokumen6 halamanLaporan RSUD Dr. Soediran Mangun Soemarso Wonogiri: 21 Desember - 27desember 2018galih widodoBelum ada peringkat
- Tibia Shaft Fracture TreatmentDokumen26 halamanTibia Shaft Fracture Treatmentgalih widodoBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- ONCOLOGY REPORTDokumen7 halamanONCOLOGY REPORTgalih widodoBelum ada peringkat
- Clinical Case Advanced Breast CancerDokumen8 halamanClinical Case Advanced Breast Cancergalih widodoBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Clinical Case Advanced Breast CancerDokumen10 halamanClinical Case Advanced Breast Cancergalih widodoBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- LAPORAN KEGIATAN IBS ORTHOPEDI RSUD MOEWARDDokumen7 halamanLAPORAN KEGIATAN IBS ORTHOPEDI RSUD MOEWARDgalih widodoBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- PETA PASIEN SABTU 31 OKTOBER 2015 BEDAH ANAKDokumen2 halamanPETA PASIEN SABTU 31 OKTOBER 2015 BEDAH ANAKgalih widodoBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Clinical Case Advanced Breast CancerDokumen8 halamanClinical Case Advanced Breast Cancergalih widodoBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- 5638451Dokumen6 halaman5638451galih widodoBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- 5638451Dokumen6 halaman5638451galih widodoBelum ada peringkat
- Overgranulation: A. Muhammad Reva A.MDokumen21 halamanOvergranulation: A. Muhammad Reva A.Mgalih widodoBelum ada peringkat
- 29 September 2017 Bedah OnkologiDokumen2 halaman29 September 2017 Bedah Onkologigalih widodoBelum ada peringkat
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- WHO-SEARO Snakebite Guidelines 2010Dokumen162 halamanWHO-SEARO Snakebite Guidelines 2010Galantry Ahmad AzhariBelum ada peringkat
- Maping Plastik 4 April 2017Dokumen2 halamanMaping Plastik 4 April 2017galih widodoBelum ada peringkat
- A New Surgical Treatment of Keloid Keloid Core ExcisionDokumen7 halamanA New Surgical Treatment of Keloid Keloid Core Excisiongalih widodoBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- A New Surgical Treatment of Keloid Keloid Core ExcisionDokumen7 halamanA New Surgical Treatment of Keloid Keloid Core Excisiongalih widodoBelum ada peringkat
- Mapping Onko 2 JuniDokumen2 halamanMapping Onko 2 Junigalih widodoBelum ada peringkat
- Accepted Manuscript: International Journal of Biological MacromoleculesDokumen66 halamanAccepted Manuscript: International Journal of Biological MacromoleculesMinuBelum ada peringkat
- Handwashing and Infection ControlDokumen23 halamanHandwashing and Infection ControlLiane BartolomeBelum ada peringkat
- Wipff Et Al. (2009) - Myofibroblasts Work Best Under StressDokumen7 halamanWipff Et Al. (2009) - Myofibroblasts Work Best Under StressTom StevensBelum ada peringkat
- TropocellsDokumen6 halamanTropocellsIsrael Exporter100% (1)
- Applications and Industrialisation of NanotechnologyDokumen310 halamanApplications and Industrialisation of NanotechnologyFátima VinhoteBelum ada peringkat
- Ways To Promote Wound HealingDokumen3 halamanWays To Promote Wound HealingEula Angelica OcoBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Platelet Rich PlasmaDokumen3 halamanPlatelet Rich PlasmaTaki bourezaneBelum ada peringkat
- FK Unpad - Draft Case 1.comulative ICDDokumen30 halamanFK Unpad - Draft Case 1.comulative ICDVirgi AhmadBelum ada peringkat
- Godbout, J. P., & Glaser, R. (2006) - Stress-Induced Immune Dysregulation. Implications For Wound Healing, Infectious Disease and CancerDokumen7 halamanGodbout, J. P., & Glaser, R. (2006) - Stress-Induced Immune Dysregulation. Implications For Wound Healing, Infectious Disease and CancerFranco Paolo Maray-GhigliottoBelum ada peringkat
- Biosensors and Bioelectronics: A 1 B 1 A BDokumen14 halamanBiosensors and Bioelectronics: A 1 B 1 A BHozefa DhilaBelum ada peringkat
- DR - VP Singh - Medrecon (FINAL)Dokumen45 halamanDR - VP Singh - Medrecon (FINAL)Virendar Pal SinghBelum ada peringkat
- Mushrooms-Rich Preparations On Wound Healing: From Nutritional To Medicinal AttributesDokumen9 halamanMushrooms-Rich Preparations On Wound Healing: From Nutritional To Medicinal AttributesFilipe GonçalvesBelum ada peringkat
- June 2009 Nursing Practice 1Dokumen9 halamanJune 2009 Nursing Practice 1Karl Gabriel BonifacioBelum ada peringkat
- Addressing Wound Chronicity FactorsDokumen5 halamanAddressing Wound Chronicity FactorsSaiyan DianBelum ada peringkat
- Bioregulatory Medicine - Chapter Two: The Future of Health and HealingDokumen13 halamanBioregulatory Medicine - Chapter Two: The Future of Health and HealingChelsea Green PublishingBelum ada peringkat
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Principios de La RehabilitacionDokumen17 halamanPrincipios de La RehabilitacionJessica PelazzoBelum ada peringkat
- Vetnizah Juniantito's CVDokumen3 halamanVetnizah Juniantito's CVjuniantitoBelum ada peringkat
- Wounds in GeneralDokumen19 halamanWounds in GeneralMuhammad ReyhanBelum ada peringkat
- USL Wound Management Guide ADokumen157 halamanUSL Wound Management Guide Aimec_coordinator7353100% (2)
- NCP - Risk For InfectionDokumen6 halamanNCP - Risk For Infectionlinnaroueyak100% (1)
- Wound ManagementDokumen3 halamanWound Managementade suhendriBelum ada peringkat
- Chapter 9 Medico Legal Aspects of Physical InjuriesDokumen13 halamanChapter 9 Medico Legal Aspects of Physical InjuriesMay Chan50% (2)
- Sutures and NeedlesDokumen11 halamanSutures and Needlesandreluizmendes100% (1)
- Fundamentals of NursingDokumen16 halamanFundamentals of Nursingsorilla_franceschelBelum ada peringkat
- Pharm 123L: Human Physiology and Pathophysiology: Activity No: 4 TitleDokumen7 halamanPharm 123L: Human Physiology and Pathophysiology: Activity No: 4 TitleEricka AbellaBelum ada peringkat
- Aloe Vera: Medicinal Uses, Benefits and PropertiesDokumen7 halamanAloe Vera: Medicinal Uses, Benefits and Properties80,795,086 likesBelum ada peringkat
- NCM 103 Chapter 36 Skin Integrity and Wound Care (Canvas)Dokumen121 halamanNCM 103 Chapter 36 Skin Integrity and Wound Care (Canvas)AinaB ManaloBelum ada peringkat
- The Integumentary SystemDokumen11 halamanThe Integumentary SystemHamdy Pagilit DimaporoBelum ada peringkat
- Cicatriz HipertroficaDokumen10 halamanCicatriz HipertroficaVictoria MaureiraBelum ada peringkat
- Wound Dressings Update: Carolina Weller, Geoff SussmanDokumen7 halamanWound Dressings Update: Carolina Weller, Geoff SussmanKevin AdrianBelum ada peringkat
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDari EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionPenilaian: 4 dari 5 bintang4/5 (402)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDari EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessPenilaian: 4.5 dari 5 bintang4.5/5 (327)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (13)
- The Ultimate Guide To Memory Improvement TechniquesDari EverandThe Ultimate Guide To Memory Improvement TechniquesPenilaian: 5 dari 5 bintang5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementDari EverandTechniques Exercises And Tricks For Memory ImprovementPenilaian: 4.5 dari 5 bintang4.5/5 (40)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDari EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsPenilaian: 3.5 dari 5 bintang3.5/5 (3)