Paediatrics 29
Diunggah oleh
rendyjiwonoHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Paediatrics 29
Diunggah oleh
rendyjiwonoHak Cipta:
Format Tersedia
BAOJ Pediatrics
Michal Cahal, et al., BAOJ Pediat 2016, 2: 5
2: 029
Research
Associated Diagnoses, Treatment and Outcomes of Children with Hypokalemia
Michal Cahal1, Shirley Friedman2, Dennis Scolnik3, Ayelet Rimon1 and Miguel Glatstein1*
Division of Pediatric Emergency Medicine, Department of Pediatrics, Dana-Dwek Children Hospital, Sackler School of Medicine, Tel Aviv University,
1
Tel Aviv, Israel
Division of Pediatrics, Intensive Care Unit, Dana-Dwek Children Hospital, Sackler School of Medicine, Tel Aviv University, Tel Aviv, Israel
2
Divisions of Pediatric Emergency Medicine and Clinical Pharmacology and Toxicology, Department of Pediatrics, The Hospital for Sick Children,
3
University of Toronto, Toronto, Ontario, Canada
Abstract Hypokalemia is generally well tolerated in otherwise healthy
people, but it can be life threatening when severe. Hypokalemia
Objective
results from decreased oral intake, gastrointestinal losses caused
To determine the frequency of moderate and severe hypokalemia by repeated vomiting or diarrhea, urinary losses through increase
in emergency department. potassium secretion or decreased reabsorption, and processes that
Methods shift potassium into the intracellular compartment [5-7]. Severe
hypokalemia (<2.5 mEq/L) can cause rhabdomyolysis, and values
A 6 year retrospective study of children with moderate (2.5-2.9
less than 2.0 mEq/L can cause ascending paralysis with eventual
mEq/L) or severe (<2.5 mEq/L) hypokalemia between March 1st
respiratory arrest [8].
2008 - March 31st 2014 in the pediatric emergency department
(PED) or pediatric wards of a tertiary care pediatric hospital. All Hypokalemia in critically ill adults is well described, as is the
patients were admitted and initially assessed through the PED. management of potassium abnormalities in children, and although
hypokalemia is one of the most common electrolyte disturbances
Results
in sick children [9,10], the magnitude of the problem in current
24 patients with hypokalemia episodes, 14 (58%) were seen in the pediatric practice remains unknown. The present study compares
PED and 10 (42%) developed during hospitalization. Hypokalemia the frequency, interventions and outcomes of moderate (2.5-
was more severe in patients diagnosed during admission; these 2.9 mEq/L) and severe (<2.5 mEq/L) hypokalemia in children
patients also experienced longer hospital stays. In both groups presenting to the pediatric emergency department versus those
the majority of hypokalemic patients suffered from diarrhea and developing the condition subsequently during hospitalization in
dehydration (50%). Correction of severe hypokalemia was mostly the pediatric wards of a large tertiary care pediatric hospital.
accomplished by means of a combination of slow potassium
Methods
infusion and oral potassium. Two patients in each group required
rapid potassium infusions. This was a retrospective case series of children aged <16 years with
moderate (2.5-2.9 mEq/L) and severe (<2.5 mEq/L) hypokalemia
Conclusion: Moderate and Severe hypokalemia is not a common
in the six years between March 1st 2008 - March 31st 2014 in the
problem among pediatric patients in our institution; based on our
pediatric emergency department (PED) or pediatric wards of the
numbers of ED visits and admissions, in the PED, it was found
Dana-Dwek Children’s Hospital. We excluded cases diagnosed
in 0.007% of patients, and on the wards, it was 0.05%. Careful
primarily in the intensive care unit (that’s mean that they didn’t
monitoring after admission is necessary to minimize the impact of
the condition in patients during hospitalization. *Corresponding author: Miguel Glatstein, Division of Pediatric Emergen-
cy Medicine, Dana-Dwek Children Hospital, Sackler School of Medicine,
Keywords: Hypokalemia; Electrolytes; Pediatric Emergency Tel Aviv University, 6 Weizman Street, Tel- Aviv 64239, Israel, Fax: 972-3-
Department; Potassium 6961578; Tel: 972-527360724; E-mail: Nopasara73@hotmail.com
Background Rec Date: December 19, 2016, Acc Date: December 30, 2016, Pub Date:
December 30, 2016.
Abnormalities in serum potassium levels are common in critically
ill patients [1], and a low serum potassium concentration is one of Citation: Michal Cahal, Shirley Friedman, Dennis Scolnik, Ayelet Rimon,
the most common electrolyte abnormalities encountered in clinical and Miguel Glatstein (2016) Associated Diagnoses, Treatment and Out-
practice [2]. Defined as a serum level <3.6 mEq/L, hypokalemia comes of Children with Hypokalemia. BAOJ Pediat 2: 029.
is found in >20% of hospitalized patients [3,4]. Symptoms are Copyright: © 2016 Michal Cahal, et al. This is an open-access article dis-
typically not apparent until the serum level is <2.5 mEq/L, unless tributed under the terms of the Creative Commons Attribution License,
the serum potassium falls rapidly [5] or is associated with digitalis which permits unrestricted use, distribution, and reproduction in any
use [6]. medium, provided the original author and source are credited.
BAOJ Pediat, an open access journal Volume 2; Issue 5; 029
Citation: Michal Cahal, Shirley Friedman, Dennis Scolnik, Ayelet Rimon, and Miguel Glatstein (2016) Associated Diagnoses, Treatment Page 2 of 5
and Outcomes of Children with Hypokalemia. BAOJ Pediat 2: 029.
was seen at the PED). The hospital serves a catchment area of medications. In this setting, an infusion with a potassium
approximately 800 000 people and the PED seen approximately 35 concentration of no more than 40 mEq/L was given at a rate not
000 patients per year, of whom 10% are admitted. to exceed 0.5 to 1 mEq/kg of body weight per hour. The rapid
replacement was given in intravenous access or central vein and
All patients who are admitted to the hospital for several reasons
when the peripheral vein were given were well tolerable because
have blood work performed: Renal function and electrolyte levels
were given with normal saline.
at least in the PED.
These patients required continuous electrocardiographic (ECG)
All patients are admitted though the emergency department,
monitoring to detect changes due to hypokalemia, and also possibly
including those needing intensive care.
rebound hyperkalemia during replacement therapy.
Definitions
All the ECG was interpreted by the physician who treated.
1. Moderate hypokalemia: potassium concentration between 2.5-
Categorical and continuous variables were analyzed using Fisher’s
2.9 mEq/L [11].
exact and the Mann-Whitney U test respectively. A p value of
2. Severe hypokalemia: serum potassium concentration <2.5 <0.05 was considered statically significant. Statistical analysis was
mEq/L [11]. performed using SAS for Windows Version 9.4.
3. Pseudohypokalemia is a decrease in the amount of potassium The study was approved by the Institutional Ethics Committee.
that occurs due to excessive uptake of potassium by metaboli-
cally active cells in a blood sample after it has been drawn. It is
Results
a laboratory artifact that may occur when blood samples remain There were 24 episodes of hypokalemia during the study period;
in warm conditions for several hours before processing [12]. nine moderate and fifteen severe. Fourteen (58%) were diagnosed
in the PED and 10 (42%) developed later on the ward. There were
4. The following diseases were considered predisposing/risk factors
no significant differences in age or primary diagnosis between
to developing hypokalemia: drugs like beta adrenergic agonist
patients with hypokalemia on initial presentation in the PED
(albuterol, insulin), metabolic alkalosis, diabetic ketoacidosis,
versus those who developed the condition subsequently on the
Bartter/Gittelman, anorexia, renal disease, malnutrition, hepatic
ward (table I). Hypokalemia was more severe in the PED group
disease, steroid use, neurological disease, and chronic respira-
(p=0.05), but those developing hypokalemia only later, on the
tory disease.
ward, experienced longer admissions (62.5 days versus 5.5 days;
5. Intravenous replacement therapy was categorized as slow if the p<0.005). In both groups, most patients belonged to the diagnostic
patient received 4-6 mEq potassium per 100 ml of intravenous categories of diarrhea-induced dehydration (50%); other causes
fluids and rapid if the concentration was greater. included respiratory conditions, diabetic ketoacidosis, neurological
6. Maintenance potassium requirement: 3 mEq/100 mL causes (epilepsy disorder), primary hyperaldosteronism, sepsis and
intoxications (beta adrenergic agonist accidental ingestion).
water × 1,000 mL/day = 30 mEq/day 30 mEq/1, 800 mL ≈15–20
Eq/L. There were no significant differences in predisposing factors
to the development of hypokalemia; Eight patients (61%) with
7. Indication for rapid replacement: for severe hypokalemia, as
clinical dehydration during severe diarrhea condition was the
the potassium concentration falls to less than 2.5 mEq/L with
most important diagnostic in PED patients. Eight episodes of
clinical manifestation of weakness prominent, areflexic paralysis
hypokalemia were associated with ECG changes, consisting of flat
(respiratory failure may occur) or significant changes in the elec-
or absent T waves [6] and prominent U-waves [2].
trocardiogram.
Correction of severe and moderate hypokalemia was accomplished
Data on all patients who experienced hypokalemia on at least one
in a mean of 10.5 and 14.2 hours respectively. Two patients in
occasion during their PED or ward stay in our institution were
each group received rapid IV correction under continuous ECG
analyzed; the patients were identified from laboratory records.
monitoring for pre-infusion serum potassium levels ranging from
Details regarding age, sex, diagnoses, predisposing factors,
1.8-2.8 mEq/L (table II).
clinical course, outcomes including biochemical parameters such
as serum electrolyte levels, acid-base status and renal function, The one patient who died developed hypokalemia during hospital-
electrocardiograms and treatment were extracted from hospital ization in association with septicemia and disseminated intravas-
charts; (is the policy of our institution that every patient who gets cular coagulation.
admitted must get a basic electrolyte panel. Electrocardiographs Discussion
(ECG) were analyzed for changes characteristics of hypokalemia.
Moderate and Severe hypokalemia is not a common problem
For symptomatic patients we used in the intensive care setting the among pediatric patients in our institution. But sometime can have
rapid infusion: serious consequences and may require prompt intervention [11].
That required intravenously (IV) administration of potassium In our institution we found 24 patients cases over a six-year period,
chloride, particularly in those who are unable to take oral excluding cases diagnosed primarily in the intensive care unit.
BAOJ Pediat, an open access journal Volume 2; Issue 5; 029
Citation: Michal Cahal, Shirley Friedman, Dennis Scolnik, Ayelet Rimon, and Miguel Glatstein (2016) Associated Diagnoses, Treatment Page 3 of 5
and Outcomes of Children with Hypokalemia. BAOJ Pediat 2: 029.
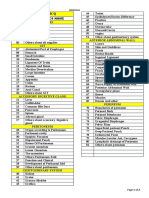
Patient Characteristic Hypokalemia in PED Hypokalemia During Hospitalization
Total P value
14 (58%) 10 (42%)
Age (mean in months) 49 months 54.7 months 0.04
<1 year [number (%)] 4 (30%) 1 (9%) 5 (20%) 0.36
1-6 years [number (%)] 7 (50%) 6 (60%) 13 (54%) 0.70
>6 years [number (%)] 3 (23%) 3 (27%) 6 (25%) 0.67
Hypokalemia
Moderate (>2.5<3 mEq/L) 7 (50%) 2(20%) 0.21
9 (37%)
Severe (<2.5 mEq/L) 7 (50%) 8 (80%) 0.21
15 (62%)
Mean [K] 2.53 4.01 0.05
Diagnosis [number (%)]
Predisposing factors* 5 (35%) 5 (50%) 10 (41%) 0.68
Diarrhea 8 (61%) 6 (60%) 14 (50%) 1.0
Respiratory conditions 2 (14 %) 2 (20%) 4 (8%) 1.0
Septicemia 0 1 (10%) 1 (4%) 0.42
Epilepsy disorder 1 (7%) 0 1 (4%) 1.0
Diabetic ketoacidosis 1 (7%) 0 1 (4%) 1.0
Isolated vomiting 0 1 (10%) 1 (4%) 0.42
Beta adrenergic agonist ingestion 1 (7%) 0 1 (4%) 1.0
1° hyperaldosteronism 1 (7%) 0 1 (4%) 1.0
Hospitalization
Length (days) 5.5 days 62.5 days 18.5 days 0.005
Intensive care admission 4 (28%) 3 (30%) 7 (29%) 1.0
Outcomes
ECG changes 6 (42%) 2 (20%) 8 (33%) 0.39
Mortality [number (%)] 0 1 (10%) 1 (4%) 0.42
Table 1: Hypokalemia in patients presenting to the PED compared to those developing the condition later on the ward.
*The following diseases were considered predisposing/risk factors to developing hypokalemia: drugs like beta adrenergic agonist (albuterol, insulin),
metabolic alkalosis, diabetic ketoacidosis, Bartter/Gittelman, anorexia, renal disease, malnutrition, hepatic disease, steroid use, neurological disease,
and chronic respiratory disease.
Duration of correc-
Potassium infusion rate – mEq/L Rapid IV correction Oral correction Mortality
Hypokalemia tion (hours)
10 20 40 60
Severe >2.5 mEq/L (N=15) 3 2 8 2 2 13 10.5 hours 0
Moderate 2.5-3 mEq/L (N=9) 1 2 5 1 2 5 14.2 hours 1
Table 2: Comparison of treatment and outcome in patients with moderate and severe hypokalemia
Although eight had ECG changes only four required rapid of infusions, Weiner et al concluded, that under intensive care
intravenous potassium replacement. Absence of ECG changes monitoring, IV administration of 20 mEq potassium/hour (central
should never be used to exclude significant hypokalemia [10]. or peripheral vein) were well tolerated [13]. There are studies that
Common ECG findings of hypokalemia include depression of the have documented the use of doses up to 100 mEq/hour in life
ST segment, decreased T-wave amplitude and increased U-wave threatening circumstances [17]. The goal of therapy is to correct
amplitude [13]. potassium deficit without provoking hyperkalemia. The choice
Fifty eight percent of patients presented with hypokalemia in the of oral or intravenous replacement depends on the severity of
PED and the remainder developed the electrolyte disturbance the disorder and the patient’s ability to tolerate enteral salts. Oral
on the ward, stressing the importance of monitoring for this replacement is preferred, except when there is no functioning
abnormality in admitted patients [14]. Four (16.6%) of our patients bowel or in the setting of ECG changes, neurological symptoms,
required rapid intravenous replacement under ECG monitoring. cardiac ischemia, or digitalis therapy. The main concern about
The maximum safe infusion rate for IV potassium is summarized the use of IV potassium supplementation is the inadvertent
elsewhere [15-16]. Based on experience with a large number administration of a large amount of potassium in a short period
BAOJ Pediat, an open access journal Volume 2; Issue 5; 029
Citation: Michal Cahal, Shirley Friedman, Dennis Scolnik, Ayelet Rimon, and Miguel Glatstein (2016) Associated Diagnoses, Treatment Page 4 of 5
and Outcomes of Children with Hypokalemia. BAOJ Pediat 2: 029.
of time, resulting in hyperkalemia. Safety measures to prevent this should start at 2-5 mEq/kg per day and be adjusted on the basis
complication include limiting the absolute amount of potassium of serial laboratory assessment. Oral supplements should be used
in any single container or bag of fluid, and using an infusion in patients predisposed to hypokalemia, such as those on diuretic
pump. IV potassium administration is also associated with pain therapy. If there is concurrent metabolic acidosis, potassium
and phlebitis when administered through a peripheral vein, which citrate or bicarbonate can be provided. If the child is unable to
can be minimized if the potassium content of the infusion is less take oral medications or is symptomatic, intravenous potassium
than 20 mEq/L. Central venous access is needed if the potassium should be provided as an intermittent infusion beginning with an
concentration exceeds 40 mEq/L. intravenous dose of 0.5-1 mEq/kg (typical maximum 30-40 mEq/
Most of our patients presenting in the PED suffered acute dose). If the child is not symptomatic, potassium can be added to
gastroenteritis. Diarrhea in children can cause electrolytes the maintenance fluids (20-40 mEq/L) via a peripheral vein. Some
abnormalities such as hyponatremia, hypokalemia and metabolic patients with severe hypokalemia do not manifest ECG changes,
acidosis with normal anion gap [18]. The concentration of and even in the absence of ECG abnormalities, rapid corrections
potassium in normal stool is 80-90 mMol/L, but because of the low have been shown to be safe and useful [19]. In order to avoid
volume of water in normal stool, only about 10 mMol of potassium insulin secretion, which promotes trans cellular shift of potassium
is normally lost each day [19]. In diarrheal states, although the into the intracellular space, potassium should be provided in a
potassium concentration in stool decreases, large quantities dextrose-free solution. Magnesium supplementation is indicated
of potassium can be lost as the volume of stool increases [20]. in hypokalemia associated with hypomagnesemia[13]. Potassium
Thus conditions, such as infectious diarrhea, that increase stool chloride or potassium phosphate may be used, although the use
volume can result in clinically significant potassium depletion and of phosphate salt is typically limited to the treatment of diabetic
hypokalemia. ketoacidosis or documented severe hypophosphatemia.
Children with mild hypokalemia are often asymptomatic. More Although our study covered a six year period in a busy tertiary care
significant potassium deficits (serum concentrations 2-3 mEq/L) pediatric hospital, the number of patients found to have moderate
cause generalized malaise and weakness. As the concentration to severe hypokalemia was relatively low, limiting the strength of
of potassium falls to <2 mEq/L, weakness becomes prominent, conclusions that can be drawn. Urine electrolytes were not assessed
and areflexic paralysis and respiratory failure may occur. in many of our patients, particularly those in the PED; knowledge
Rhabdomyolysis is also likely [21]. In all cases of significant of these measurements would have helped elucidate causes of
hypokalemia, monitoring for ECG changes and muscle strength is hypokalemia.
imperative, and if abnormalities are present immediate replacement Conclusion
is warranted.
Potassium deficiency alters the function of several organs, most
Potassium is a predominantly intracellular ion and an understand- prominently the cardiovascular and neurologic systems, muscles,
ing of the relationship between intra- and extra-cellular fluid mi- and kidneys. These effects ultimately determine the morbidity and
lieux and potassium handling by the kidneys, is important in the mortality related to this condition. Children and young adults
diagnosis and treatment of potassium disorders [3]. Metabolic tolerate greater degrees of hypokalemia with less risk than the
acidosis with a random urine potassium-creatinine ratio <1.5 sug- elderly. Although significant hypokalemia is relatively uncommon
gests excessive gastrointestinal losses due to diarrhea, or a shift of in pediatric emergency patients.
potassium into cells [21]. Measurement of blood pressure, blood
pH, renin and aldosterone levels, stool and urine volumes and the References
concentration of potassium in each patient would have helped clar- 1. Bilal A, Sadiq MA, Haider N (2016) Frequency of hyponatraemia
ify potassium homeostasis in our patients. and hypokalaemia in malnourished children with acute diarrhoea. J
Pak Med Assoc 66(9): 1077-1080.
For successful potassium replacement, the optimal potassium
preparation, route, and speed of administration, as well as severity, 2. Odey FA, Etuk IS, EtukudohMH, Meremikwu MM, et al. (2010)Hy-
pokalaemia in children hospitalised for diarrhoea and malnutrition in
acuity, associated clinical signs, comorbid conditions, and the
Calabar, Nigeria. Niger Postgrad Med J17(1):19-22.
expectation for ongoing loss should be considered [16]. In general,
potassium replacement is indicated when there has been potassium 3. Hoskote SS, Joshi SR, Ghosh AK (2008) Disorders of potassium ho-
loss. In clinical scenarios when potassium loss is accompanied by meostasis: pathophysiology and management. J Assoc Physicians In-
dia 56:685-93.
acid–base disturbance, a redistribution effect should be factored in
when losses are estimated. Supplementation during a redistributive 4. Schaefer TJ, Wolford RW (2005) Disorders of potassium. Emerg Med
process should proceed with close monitoring, given the risk of Clin North Am 23:723-747.
rebound hyperkalemia [22]. In cases when potassium has been 5. Gennari FJ (1998)Hypokalemia. N Engl J Med 339(7):451-8.
lost, there is no direct correlation between serum level and total 6. Gennari FJ (2002) Disorders of potassium homeostasis. Hypokalemia
body stores, and potassium deficit can only be approximated [9]. and hyperkalemia. Crit Care Clin 18(2):273-88.
If the child is clinically well, oral therapy is preferable and can be 7. Brown RS (1986)Extrarenal potassium homeostasis. Kidney Int
provided 2-4 times per day as potassium chloride [22]. Dosing 30(1):116-27.
BAOJ Pediat, an open access journal Volume 2; Issue 5; 029
Citation: Michal Cahal, Shirley Friedman, Dennis Scolnik, Ayelet Rimon, and Miguel Glatstein (2016) Associated Diagnoses, Treatment Page 5 of 5
and Outcomes of Children with Hypokalemia. BAOJ Pediat 2: 029.
8. Lenz T, Becker B, Bergner R (2004) Potassium in renal disease. Med 15. Kruse JA, Carlson RW (1990) Rapid correction of hypokalemia using
Klin (Munich) 99(7):355-61. concentrated intravenous potassium chloride infusions. Arch Intern
Med 150(3):613-7.
9. Glatstein M, ValaSnehal, Syed Amir A, Scolnik D (2012) Are Potassium
levels in Children with Hemolytic Uremic Syndrome Predictive Out- 16. Kim GH, Han JS (2002) Therapeutic approach to hypokalemia.
come?. Open Journal of Pediatrics (2)4: 264-267. Nephron 92 Suppl 1:28-32.
10. Singhi S, Gulati S, Prasad SV (1994) Frequency and significance of po- 17. Defronzo RA, Bia M (1981) Intravenous potassium chloride therapy.
tassium disturbances in sick children. Indian Pediatr 31(4):460-3. 245:2446.
11. Zieg J, Gonsorcikova L, Landau D (2016) Current views on the diag- 18. Shah GS, Das BK, Kumar S, Singh MK, Bhandari GP, et al. (2007) Acid
nosis and management of hypokalaemia in children. Acta Paediatr base and electrolyte disturbance in diarrhoea. Kathmandu Univ Med
105(7):762-72. J 5(1):60-2.
12. Sodi R, Davison AS, Holmes E, Hine TJ, Roberts NB, et al.(2009) “The 19. Gennari FJ (2002) Disorders of potassium homeostasis. Hypokalemia
phenomenon of seasonal pseudohypokalemia: effects of ambient and hyperkalemia. Crit Care Clin 18(2):273-88.
temperature, plasma glucose and role for sodium-potassium-ex- 20. Mandal AK (1997) Hypokalemia and hyperkalemia. Med Clin North
changing-ATPase. ClinBiochem 42 (9): 813-8. Am 81(3):611-39.
13. Weiner ID, Wingo CS (1997) Hypokalemia--consequences, causes, 21. Cummings BM, Macklin EA, Yager PH, Sharma A, Noviski N, et al.(2014)
and correction. J Am SocNephrol 8(7): 1179-88. Potassium abnormalities in a pediatric intensive care unit: frequency
14. Singhi S, Marudkar A (1996) Hypokalemia in a pediatric intensive care and severity. J Intensive Care Med 29(5):269-7.
unit. Indian Pediatr 33(1):9-14. 22. Asmar A, Mohandas R, Wingo CS (2012) A physiologic-based ap-
proach to the treatment of a patient with hypokalemia. Am J Kidney
Dis 60(3):492-7.
BAOJ Pediat, an open access journal Volume 2; Issue 5; 029
Anda mungkin juga menyukai
- Management of Immune Thrombocytopenic Purpura in Children: Paediatric Drugs August 2011Dokumen13 halamanManagement of Immune Thrombocytopenic Purpura in Children: Paediatric Drugs August 2011rendyjiwonoBelum ada peringkat
- 2017 Article 418 PDFDokumen6 halaman2017 Article 418 PDFrendyjiwonoBelum ada peringkat
- 2014 Neurogenic NeuroinflammationDokumen11 halaman2014 Neurogenic NeuroinflammationrendyjiwonoBelum ada peringkat
- The Prevalence of Blindness, Visual Impairment and Cataract Surgery in Tuoketuo and Shangdu Counties, Inner Mongolia, ChinaDokumen9 halamanThe Prevalence of Blindness, Visual Impairment and Cataract Surgery in Tuoketuo and Shangdu Counties, Inner Mongolia, ChinarendyjiwonoBelum ada peringkat
- OMDokumen9 halamanOMChristy AmandaBelum ada peringkat
- Serum Vitamin D Levels in Pulmonary Tuberculosis: SJIF Impact Factor 6.647Dokumen7 halamanSerum Vitamin D Levels in Pulmonary Tuberculosis: SJIF Impact Factor 6.647rendyjiwonoBelum ada peringkat
- JR Onko Breast PDFDokumen24 halamanJR Onko Breast PDFrendyjiwonoBelum ada peringkat
- Neonatal Resuscitation Using A Laryngeal Mask Airway: A Randomised Trial in UgandaDokumen6 halamanNeonatal Resuscitation Using A Laryngeal Mask Airway: A Randomised Trial in UgandarendyjiwonoBelum ada peringkat
- Pi Is 0012369208603700Dokumen10 halamanPi Is 0012369208603700Yan Sheng HoBelum ada peringkat
- SARCOPENIDokumen9 halamanSARCOPENIrendyjiwonoBelum ada peringkat
- Re Expansion Pulmonary EdemaDokumen4 halamanRe Expansion Pulmonary EdemarendyjiwonoBelum ada peringkat
- Biologic Drugs: A New Target Therapy in COPD?: COPD: Journal of Chronic Obstructive Pulmonary DiseaseDokumen10 halamanBiologic Drugs: A New Target Therapy in COPD?: COPD: Journal of Chronic Obstructive Pulmonary DiseaserendyjiwonoBelum ada peringkat
- 2011 ITP Pocket GuideDokumen28 halaman2011 ITP Pocket GuiderendyjiwonoBelum ada peringkat
- Ascitesupdate2013 PDFDokumen27 halamanAscitesupdate2013 PDFKun Anupong WansukhBelum ada peringkat
- Re Expansion Pulmonary EdemaDokumen4 halamanRe Expansion Pulmonary EdemarendyjiwonoBelum ada peringkat
- 329 FullDokumen7 halaman329 FullrendyjiwonoBelum ada peringkat
- Molecular Mechanisms of Appetite Regulation: ReviewDokumen8 halamanMolecular Mechanisms of Appetite Regulation: ReviewZackychunBelum ada peringkat
- NF-JB and Cancer: How Intimate Is This Relationship: Ó Springer Science+Business Media, LLC. 2009Dokumen13 halamanNF-JB and Cancer: How Intimate Is This Relationship: Ó Springer Science+Business Media, LLC. 2009rendyjiwonoBelum ada peringkat
- Urological Science: Haoping Tai, Jue-Hawn Yin, Zhon-Min Huang, Tang-Yi TsaoDokumen3 halamanUrological Science: Haoping Tai, Jue-Hawn Yin, Zhon-Min Huang, Tang-Yi TsaorendyjiwonoBelum ada peringkat
- 2011 ITP Pocket Guide PDFDokumen4 halaman2011 ITP Pocket Guide PDFWinda AlpiniawatiBelum ada peringkat
- Laboratory Diagnosis of CMV Infection: A ReviewDokumen6 halamanLaboratory Diagnosis of CMV Infection: A ReviewrendyjiwonoBelum ada peringkat
- The Prevalence of Blindness, Visual Impairment and Cataract Surgery in Tuoketuo and Shangdu Counties, Inner Mongolia, ChinaDokumen9 halamanThe Prevalence of Blindness, Visual Impairment and Cataract Surgery in Tuoketuo and Shangdu Counties, Inner Mongolia, ChinarendyjiwonoBelum ada peringkat
- 2011 ITP Pocket GuideDokumen28 halaman2011 ITP Pocket GuiderendyjiwonoBelum ada peringkat
- PXW 011Dokumen5 halamanPXW 011rendyjiwonoBelum ada peringkat
- 41 IngDokumen8 halaman41 IngrendyjiwonoBelum ada peringkat
- The Frequency, Cost, and Clinical Outcomes of Hypernatremia in Patients Hospitalized To A Comprehensive Cancer CenterDokumen8 halamanThe Frequency, Cost, and Clinical Outcomes of Hypernatremia in Patients Hospitalized To A Comprehensive Cancer CenterrendyjiwonoBelum ada peringkat
- 02-Susunan Acara RevisiDokumen5 halaman02-Susunan Acara RevisirendyjiwonoBelum ada peringkat
- The Frequency, Cost, and Clinical Outcomes of Hypernatremia in Patients Hospitalized To A Comprehensive Cancer CenterDokumen8 halamanThe Frequency, Cost, and Clinical Outcomes of Hypernatremia in Patients Hospitalized To A Comprehensive Cancer CenterrendyjiwonoBelum ada peringkat
- HighDokumen16 halamanHighrendyjiwonoBelum ada peringkat
- 3 Metabolisme IngDokumen4 halaman3 Metabolisme IngrendyjiwonoBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- G 62 - 14 PDFDokumen4 halamanG 62 - 14 PDFjose floresBelum ada peringkat
- Hazard & Turn Signal Lamp CircuitDokumen2 halamanHazard & Turn Signal Lamp CircuitTanya PiriyabunharnBelum ada peringkat
- Kingspan 30 GSNDokumen1 halamanKingspan 30 GSNNoella AguiarBelum ada peringkat
- Nasua NasuaDokumen9 halamanNasua NasuaJetsabellGutiérrezBelum ada peringkat
- Lenskart Solutions PVT LTD Company ProfileDokumen13 halamanLenskart Solutions PVT LTD Company ProfileAnujaBelum ada peringkat
- Easy Guide For Fujitsu T901 LaptopDokumen141 halamanEasy Guide For Fujitsu T901 LaptopElaineBelum ada peringkat
- CP Inf4Dokumen357 halamanCP Inf4Rugwed JadhavBelum ada peringkat
- Federal Bylaw 12 Air Pollution 2006 English Translation v2 OCRDokumen63 halamanFederal Bylaw 12 Air Pollution 2006 English Translation v2 OCRIsmail SultanBelum ada peringkat
- LEVEL 2-Anxiety-Adult (PROMIS Emotional Distress-Anxiety - Short Form)Dokumen1 halamanLEVEL 2-Anxiety-Adult (PROMIS Emotional Distress-Anxiety - Short Form)alemsaudementalBelum ada peringkat
- A Study On Risk Assessment in The Construction of High-Rise BuildingsDokumen5 halamanA Study On Risk Assessment in The Construction of High-Rise BuildingsMohamedSaidBelum ada peringkat
- Rig 166 Data SheetDokumen2 halamanRig 166 Data SheetEstuardo OlanBelum ada peringkat
- Sale of Property When - KP AstrologyDokumen2 halamanSale of Property When - KP Astrologyprajishvet100% (1)
- Interactions of Microplastic Debris Throughout The Marine Ecosystem Final Tracked-Galloway, TS Cole, M Lewis, CDokumen22 halamanInteractions of Microplastic Debris Throughout The Marine Ecosystem Final Tracked-Galloway, TS Cole, M Lewis, CTrydawBelum ada peringkat
- SuctioningDokumen58 halamanSuctioningAyusa PradhanBelum ada peringkat
- B11 - Overload Relays (Ref) ENDokumen20 halamanB11 - Overload Relays (Ref) ENAhmed AbazaBelum ada peringkat
- AngelDokumen21 halamanAngelNoj ZachBelum ada peringkat
- A MCQ: Si - No Sub Topics NameDokumen2 halamanA MCQ: Si - No Sub Topics NameInzamamul Haque ShihabBelum ada peringkat
- DinmjgDokumen10 halamanDinmjghaker linkisBelum ada peringkat
- Factory Program Library List v1.0Dokumen9 halamanFactory Program Library List v1.0Ronaldo DamattaBelum ada peringkat
- Mardi Gras Recipe Sampler by Mitchell Rosenthal, Author of Cooking My Way Back HomeDokumen13 halamanMardi Gras Recipe Sampler by Mitchell Rosenthal, Author of Cooking My Way Back HomeThe Recipe Club100% (1)
- Report On RoboticsDokumen40 halamanReport On Roboticsangelcrystl4774Belum ada peringkat
- BKC 80Dokumen2 halamanBKC 80jawaidchemicalsBelum ada peringkat
- RH Fs Risk FactorsDokumen2 halamanRH Fs Risk FactorsfentroispBelum ada peringkat
- Wire Rope Forensics Letter PDFDokumen50 halamanWire Rope Forensics Letter PDFAshley DeanBelum ada peringkat
- Nasa ThesisDokumen8 halamanNasa Thesisdnr3krf8100% (2)
- Winter Solstice, CGW 2011Dokumen38 halamanWinter Solstice, CGW 2011Lady HekateShadowMoonfire0% (1)
- Introduction To Food Analysis2020Dokumen2 halamanIntroduction To Food Analysis2020Ĝĭdęŷ KîřöşBelum ada peringkat
- Part PabrikDokumen2 halamanPart PabrikNaldy NaldyBelum ada peringkat
- Robotics Toolbox 9.6 TutorialDokumen149 halamanRobotics Toolbox 9.6 TutorialRogério Lopes100% (1)
- CatalogDokumen52 halamanCatalogtalabiraBelum ada peringkat