History Taking - Chief Complaint, HPI, PMH, FH, SH
Diunggah oleh
Gurpreet CharaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
History Taking - Chief Complaint, HPI, PMH, FH, SH
Diunggah oleh
Gurpreet CharaHak Cipta:
Format Tersedia
History taking – Medicine
1- Introduction:
2- Chief complaint
3- History of present illness
4- Past medical history
5- Family history
6- Social history
Introduction
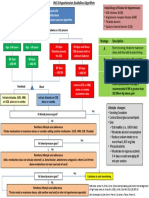
Known Chief complaint NOT known
Clear Unclear
Clarify CC
TIME: Os Cf D
CC Character: PQRST
↑ ↓
Causes and
Systems DD
HPI consequences
1. same system
2. near-by systems
AS
3. constitutional
4. risk factors
5. causes / consequences
6. review of systems
Allergy
Medications
PMH Diseases (DM, HTN, heart attack, stroke, cancer)
Hospitalization / surgery
LMP
Any long term disease
FH
Any specific disease
How do you support yourself financially?
SH With whom do you live?
SAD
2011-09- Medical History.doc Page 1 of 52
1- Introduction:
- Knock the door
- Go to the examiner ! give stickers ! use alcohol rub (disinfective)
- Stand at the edge of the chair
- Good evening Mr …, I am Dr …, I am the physician in charge today,
o < 18 years: use first name
o > 18 years: use Mr / Mrs / Ms
- I understand that you are here because of …,
Examples:
- History Taking: Good evening Mr …, I am Dr …, I am the physician on duty now,
and I understand that you are here today because of …. In the next few minutes I will
ask you some questions about your cc, to figure out a working plan that can help you.
If you have any concerns or questions, please fell free to stop me and let me know.
- Physical examination: Good evening Mr …, I am Dr …; I am the physician in charge
now. I understand that you are here today because of …. In the next few minutes I
will do a physical exam on your (e.g. shoulder), during which I will ask you to do
some movements that may cause some discomfort and may be some pain, if you feel
either, please do not hesitate to stop me. And if you have any concerns, please let me
know. And I will be telling the findings to the examiner while we proceed.
2- Chief complaint
[A] If the CC not known
- How can I help you today?
1. Start to ask based on the age:
MALE FEMALE
> 65 yrs " Do you take meds on regular basis? Do you have a list of it? Or the
bottles? Do you take sleeping pills?
" Do you have difficulties with sleeping?
" Do you have difficulties with your balance1, any falls?
" Do you have difficulties with urination (incontinence / retention)?
" Do you have changes in your vision / hearing?
" Do you have changes in your mood / memory?
50s " Do you have problem drinking ! use CAGE
" Depression2 ! identify through social history
" ED / Impotence
30s " Psychiatric problems
" SAD ! social history
Teen / 20s " Premature ejaculation " Abortion
" STDs " STDs
" Eating disorders
1
Normal pressure hydrocephalus: ataxia / incontinence / dementia
2
Common triad association: alcohol / depression / suicide
2011-09- Medical History.doc Page 2 of 52
2. Special conditions:
" Fatigue Domestic abuse
" Insomnia
" Headache
" Abdominal pain
" Vaginal bleeding
" Chest pain Panic attack
" SOB
" Heart racing
" Dizziness
" Numbness
[B] If the CC is known
CLEAR NOT clear
" Any pain: headache, chest pain " Vague symptoms: dizziness, tired
" Cough " When the patient uses medical terms:
" Fever abortion, jaundice, palpitation
" When the patient uses the words:
change / difficulty
Clarify: Clarify:
1. Start first open-ended questions: - Use closed ended questions
- What do you mean?
- Can you tell me more about this
2. Active listening:
- Do not interrupt
- Do not duplicate
3. Body language: nod your head
2011-09- Medical History.doc Page 3 of 52
3- History of present illness
[A] TIME (Os Cf D):
- Onset:
o How did it start (sudden / gradual)?
o Setting: what were you doing?
- Course:
o From that time till now, is your cc all the time or is it on and off (continuous
vs. intermittent)?
" Continuous:
• From the beginning
• Does it ↑ or ↓ or the same?
• Frequency: is it your first time?
" Intermittent:
• Frequency: how often did you have it in the last (…)?
• Are these attacks similar or different?
o ↑ in duration (longer) or ↑ in severity (more severe) or
↑ in frequency (more often)?
• What brings it? On doing certain thing, occurring at rest,
awakening you from sleep?
- Duration:
o Usually given in the question
o If > 24 hours ! empathy: were you able to sleep
[B] Character:
+ PAIN: PQRST always ask “from the beginning?”
- Position: where did it start? Can you point with one finger on it?
- Quality: how does it feel like? Squeezing, tightness, sharp, stabbing, burning?
- Radiation: does it shoot anywhere?
- Severity: on a scale of 10, 1 being the mildest pain you have ever had and 10 is the
most severe, how much do you rate this one?
o If bad pain ! empathy: this must be difficult
- Timing:
o Does it change with time; is it more in morning or towards the end of the day?
o Any variation?
- Triggers:
o What brings your headache?
o Is it related to: stress / lack of sleep / over sleep / flashing lights / smells?
o If female: is it related to your periods? Are you taking any meds or OCPs?
o Any diet triggers?
+ Fluids (e.g. bleeding, diarrhea, vomitus):
- COCA±B/D: colour, odour, contents/consistency, amount ± blood/discharge
2011-09- Medical History.doc Page 4 of 52
[C] What ↑ or ↓:
- What increases or decreases your cc?
- Examples: noise / quiet places / movements / resting / coughing / leaning forward /
lying down /
[D] ASSOCIATED SYMPTOMS:
- In addition to your cc, did you notice any other symptoms?
- Now, I am going to ask you more questions to see if you have any other symptoms
beside your cc.
+ By systems:
e.g. chest pain
1- Same system
2- Near-by systems
3- Constitutional symptoms [RED FLAGS]
4- Risk factors
Now, I am going to ask you more questions to see if you have any medical
conditions that may explain / cause / predispose your cc.
5- Causes and consequences
6- Review of systems:
+ By differential diagnosis:
e.g. headache
+ By causes and consequences:
e.g. Macrocytic anemia – Vit B12 deficiency
2011-09- Medical History.doc Page 5 of 52
4- Past medical history
Because it is the first time I see you, I need to ask you some questions about your past
medical history.
1- Allergy / medications:
a. Allergy
b. Medications (OTC, Rx meds, supplements, herbs)
2- Any history of diseases for which you see doctor on regular basis (DM, high
blood pressure, heart attack, stroke, cancer)?
3- Any history of hospitalization / procedures?
4- LMP for females
5- Family history
Because it is the first time I see you, I need to ask you some questions about your family
medical history, and by this I mean your parents and siblings.
1- Any long term disease in the family? DM, HTN, heart attack, stroke?
2- Any specific disease in the family?
6- Social history
1- How do you support yourself financially?
2- With whom do you live?
a. Alone ! are you in any relationship? Are you sexually active?
b. With a family ! how is the relation with …? Is she/he supportive?
3- SAD:
a. Do you smoke?
b. Do you drink alcohol?
i. How much?
ii. For how long?
c. Have you ever tried the recreational drugs?
2011-09- Medical History.doc Page 6 of 52
Notes
EMPATHY:
If during history taking you noticed the patient is in pain ! empathy: I can see you are
in pain, please bear with me for few minutes and I will give you a pain
medication as soon as I can
- In the short cases (5 minutes) ! use at least 1-2 empathy statement
- In the long cases (10 minutes) ! use at least 3 empathy statements
- Patient says “I’m not ok / I’m not so good” ! I am sorry to hear that
- Patient says “I fell down” ! Oh, did you hurt yourself / “No” – I am glad to hear that
- After suicide ! It looks like you have gone through difficult times, can you tell me
more about these difficulties you are facing
- Patient is regaining consciousness in the ER ! Mr … you have had … and you are in
the hospital now, you are ok now, I am Dr … and we are here to make sure you’re ok
I have a concern!
Whenever the patient says: “I have a concern”:
- Stop the interview!
- Can you tell me your concerns!
- Why are you concerned?
Worried / occupied patient!
Whenever the patient shows non-verbal clues of being worried / occupied:
- I can see that you are worried / occupied! Would you like to tell me more worries or
concerns?
Question types:
- Types of questions you can use: open-ended, closed-ended, choices
- Types of questions you can NOT use: leading questions, stacking questions
Time usage technique: 1 / 2 / 3
If you are stuck during the history taking; and could not find questions to ask;
- First time: Summarize
- Second time: Ask about constitutional symptoms / Review of systems
- Third time: PMH / FH / SH
Medications:
When you ask about the medications and even if the patient says NO, in certain diseases,
you need to confirm special medications, by saying, what about …
- Diarrhea ! what about antibiotics
- Asthma ! aspirin / β–blockers (HTN, heart failure, ↑ thyroid, social phobias)
- Migraine ! what about OCPs? (any birth control pills)
- Bleeding ! what about aspirin / blood thinners
- Torticollis ! do you take anti-psychotics? Do you see psychiatrist/
2011-09- Medical History.doc Page 7 of 52
For breaking bad news [SPIKES] approach:
o Setting
o Perception of the patient: what do you know about …
o Invitation: how much details you would like to know about …
o Knowledge: give knowledge in understandable pieces, and make sure the
patient understands this info.
o Empathy /+/ Expectations: what are your expectations from today’s visit
" You will have tremendous support, you are not working alone
" We will try to make you as comfortable as possible
" Oncology group AND palliative group: Referral: do you have any
doctor you are comfortable with?
o Summarize /+/ Strategy
MSD (mood / suicide / drinking): whenever you find one, screen for the others
When the patient comes with a chronic long duration complaint, ask him: and what
happened recently that made you decide to seek medical advice now?
Counselling:
1. Inform the patient
a. The medical condition is called “…”
b. Explain the pathophysiology
c. Consequences / complications of the condition! May happen again, may
affect ability to do certain things, …
d. Investigations that might be needed to conclude the condition OR to look
for complications
2. Preventive measures: e.g. modify the poly-pharmacy …
3. Treatment: life style / medications (side effects / alternatives / consequences)
4. Offer more info: brochures / web sites
5. Break every 30-60 seconds and ask the patient: does that make sense? Is this
acceptable? Reasonable? Is it clear?
Whenever you hear “car accident”:
- I am sorry to hear that!
- Was anyone hurt? I am sorry for that
- Were you driving or a passenger?
Whenever the patient has something affecting his life / social issue:
! Refer to social worker / services
2011-09- Medical History.doc Page 8 of 52
CHEST PAIN
Introduction: Good evening Mr …, I am Dr …, I am the physician on duty now, and I
understand that you are here because you have chest pain for the last … minutes. In the
next few minutes I will ask you some questions about your chest pain, to figure out a
working plan that can help you. If you have any concerns or questions, please fell free to
stop me and let me know
HPI:
A. OsCfD
o Onset / setting: what were you doing?
B. PQRST
o Position: where did it start? Can you point with one finger on it?
o Quality: how does it feel like? Squeezing, tightness
o Radiation: does it shoot anywhere?
" To my jaw ! what about your shoulders, your back, your hands?
o Severity
o Timing
o Triggers
C. What ↑ or ↓:
o How did you come to the clinic today?
" Ambulance ! did they give you aspirin / nitrates? Did it help you?
D. Associated symptoms:
" In addition to your pain, did you notice any other symptoms?
" By SYSTEMS:
1- Same system:
- Nausea / vomiting
- Sweating / feeling tired
- SOB ! if yes, analyze (OsCfD)
- Do you feel your heart racing?
- Did you feel dizzy / light headedness / LOC? Are you tired?
- Did you notice swelling in your ankles?
2- Near-by systems:
- CHEST:
• Any cough or phlegm?
• Chest tightness?
• Wheezes?
• Recent fever / flu like symptoms? Muscles/ joint ache?
- GIT:
• Difficulty swallowing (esophageal spasm)
• Heart burn / acidic taste in your mouth?
• Any hx of PUD?
- Chest wall: any trauma, any blisters / skin rash on your skin
- DVT: any pain / swelling / redness in your legs / calves? Any
recent long travel?
2011-09- Medical History.doc Page 9 of 52
3- Constitutional symptoms [RED FLAGS]:
- Fever / night sweats / chills
- How about your appetite? Any weight changes?
- Any lumps or bumps in your body?
4- Risk factors
Major Minor
- High blood pressure - Look for obesity:
- High blood sugar + Do you exercise
- High cholesterol: have you + How about your diet, do
got your cholesterol you eat fast food?
measured? - Are you under stress?
- Family hx of heart attack at
age < 50 yrs
- SAD:
+ Smoking
+ Cocaine: do not give beta
blockers ! unopposed alpha
! ↑ blood pressure
5- Causes and consequences
- Atherosclerosis:
• Hx of stroke? Weakness / numbness / change in vision /
difficulty finding words?
• Any sexual dysfunction?
• Do you feel abdominal pain after eating?
• Do you feel cold extremities
• Do you feel cold feet? Pain after walking?
Questions:
- Investigations:
o ECG
o Cardiac enzymes
- Treatment:
o A Aspirin
o B Beta blockers
o N Nitrates
2011-09- Medical History.doc Page 10 of 52
CHEST PAIN – SUMMARY
Introduction:
HPI:
E. OsCfD
F. PQRST
G. What ↑ or ↓:
o How did you come to the clinic today?
" Ambulance ! did they give you aspirin / nitrates? Did it help you?
H. Associated symptoms:
" In addition to your pain, did you notice any other symptoms?
" By SYSTEMS:
1- Same system (CVS)
2- Near-by systems:
- CHEST:
- GIT:
- Chest wall: any trauma, any blisters / skin rash on your skin
- DVT: any pain / swelling / redness in your legs / calves? Any
recent long travel?
3- Constitutional symptoms [RED FLAGS]:
4- Risk factors
Major Minor
- High blood pressure - Look for obesity:
- High blood sugar + Do you exercise
- High cholesterol: have you + How about your diet, do
got your cholesterol you eat fast food?
measured? - Are you under stress?
- Family hx of heart attack at
age < 50 yrs
- Smoking
5- Causes and consequences
- Atherosclerosis
PMH
FH
SH
2011-09- Medical History.doc Page 11 of 52
HEADACHE
Causes of headache
Primary headache Secondary headache
Intermittent, episodic 1- Infection
- Tension headache 2- Tumour: + benign ! mass effect
- Cluster headache + Malignant
- Migraine: 3- CVA
+ Classical (with aura) 4- Subdural hematoma
+ Non-classical (no aura) 5- Subarachnoid hge
6- Temporal arthritis
7- HTN
8- Extra-cranial: + Eye (glaucoma, errors of ref)
+ Ears (inflammation, discharge)
+ Sinusitis
+ Teeth problems
9- Medications: + Nitrates
+ Rebound headache
+ Withdrawal headache
10- Depression (in elderly)
11- CO poisoning
12- Abuse (domestic / elderly)
Introduction:
HPI:
A. OsCfD: gradual onset / all the time / increasing / for few days
B. PQRST: temporal area / vague deep pain / severe
o Severe: ! empathy: this must be difficult, were you able to sleep
o Triggers:
" What brings your headache?
" Is it related to: stress / lack of sleep / flashing lights / smells?
" If female: is it related to your periods? Are you taking any OCPs?
" Diet triggers of headache: (C3W) chocolate / coffee / cheese /// wine.
C. What ↑ or ↓
D. Associated symptoms:
" In addition to your headache, did you notice any other symptoms?
" By Differential Diagnosis:
1- Infection:
- Fever / night sweats / chills
- Neck pain / stiffness
- Recent flu like symptoms
- Bothered by light
- Nausea / vomiting
2- Neurological screening:
If while you are doing the neurological screening, you suspect particular cause, e.g.
temporal arteritis ! go to TA block then return to complete the neurological screening.
- Cranial nerves:
• Any change in smelling perception?
• Any difficulty in vision / vision loss?
• Any difficulty in hearing / buzzing sounds?
2011-09- Medical History.doc Page 12 of 52
• Difficulty finding words?
• Difficulty swallowing?
- UL/LL:
• Any weakness / numbness / tingling in your arms / legs
• Any difficulty in your balance / any falls?
- Spine:
• Any difficulty with urination / need to strain to pass urine?
• Any change in bowel movements?
- Brain:
• Any dizziness / light headedness / LOC?
• Any tremors / jerky movements / hx of seizures?
- Personality and cognition:
• Any memory / mood / concentration problems?
• Did anybody tell you that you there is a change in your
personality recently?
3- Subdural hematoma:
- Trauma
- SAD (Smoking, Alcohol, Drugs)
4- Subarachnoid hemorrhage:
- Very acute
- Very severe headache
- Pupil changes
- Bradycardia
5- Temporal arteritis:
- Age > 55 years
- When you touch this part of your head, is it painful?
- Do you feel cord-like structure?
- When you are chewing, is it painful, cramps in your jaws?
- Any weakness / numbness in your shoulders / hips?
- Is there any cough? Mild fever?
6- HTN:
- Do you know your bl pressure? Have you had it checked before?
- Were you diagnosed before with high blood pressure?
- Any history of repeated headaches?
7- Extra-cranial causes of headache:
- Eyes: any hx of glaucoma, red eye, pain in your eyes? Do you
usually wear eyeglasses? Do you see well? Any vision problems?
When was the last time you saw your optometrist?
- E – do you have any pain / discharge in your ears?
- N – nasal discharge / sinusitis / hx of facial pain?
- T – any teeth pain / difficulty swallowing?
8- Medications:
- Do you take any nitrates?
- Do use too much of advil (or other NSAIDs)? For how long?
- Were you used to take large amounts of coffee and then you
stopped abruptly?
2011-09- Medical History.doc Page 13 of 52
HEADACHE – SUMMARY
Introduction:
HPI:
A. OsCfD: gradual onset / all the time / increasing / for few days
B. PQRST: temporal area / vague deep pain / severe
o Severe: ! empathy: this must be difficult, were you able to sleep
o Triggers:
" What brings your headache?
" Is it related to: stress / lack of sleep / flashing lights / smells?
" If female: is it related to your periods? Are you taking any OCPs?
" Diet triggers of headache: (C3W) chocolate / coffee / cheese /// wine.
C. What ↑ or ↓
D. Associated symptoms:
" In addition to your headache, did you notice any other symptoms?
" By Differential Diagnosis:
1- Infection:
2- Neurological screening:
If while you are doing the neurological screening, you suspect particular cause, e.g.
temporal arteritis ! go to TA block then return to complete the neurological screening.
- Cranial nerves:
- UL/LL:
- Spine:
- Brain:
- Personality and cognition:
3- Subdural hematoma:
4- Subarachnoid hemorrhage:
5- Temporal arteritis:
6- HTN:
7- Extra-cranial causes of headache:
- Eyes
- Ears
- Nose
- Throat
8- Medications:
PMH
FH
SH
2011-09- Medical History.doc Page 14 of 52
BLOOD RESULTS – Macrocytic Anemia – B12 Deficiency
Good morning Mr …, I am Dr …, I understand that you are here today (OR we called you to
come) to get the results of your blood tests (OR x-ray) that you have done few days ago, I have it
and I am going to discuss it with you. However, because it is the first time that I see you, I need
first to ask you some questions to help me get better understanding and interpretation of these
results. Is it OK with you?
1- First let me ask you few questions about the lab test itself (this applies to any blood
work, x-ray, HIV testing, biopsy, jaundice, anemia):
- Why have you done this test?
- Is it the first time to have it?
- Who ordered this test for you? Why?
- When did you have it?
2- Give the information:
- If it is bad news ! SPIKES
- If abnormal blood results or x-ray: explain the results to patient, to decrease the
patient anxiety. The blood tests you had show that you have special kind of anemia that
we call “Macrocytic anemia” in which the size of the red blood cells (which are a
component of your blood) is larger than usual, there is different causes for this.
o If the patient panicked? Is it serious doctor?
" Do you have any concerns? OR
" There are different causes that may lead to this result, some of
them are serious, could be, we need to do more investigations.
3- I would like to ask you some questions to see how did this (anemia) affect you:
CONSEQUENCES of anemia:
- Anemia symptoms:
o Did you notice any ↓ in your activity level?
o SOB / chest pain with exercise?
o Any dizziness / light headedness / fainting?
- Neuro symptoms:
o Any tingling / numbness / in your feet?
o Difficulty in your balance / any falls?
o Any difficulty concentrating / memory problems?
4- I would like to ask you more questions to find what might be the cause:
CAUSES of Vit B12 deficiency:
- Diet intake: Are you vegetarian? For how long? Do you take supplements?
- Gastric causes:
o Did you have any surgeries in your stomach? When?
o Any heaviness / fullness after meals / indigestion?
o History of long standing PUD?
2011-09- Medical History.doc Page 15 of 52
o Were you ever yourself or any member of your family diagnosed with
what is called “autoimmune disease” by this I mean a condition called
“pernicious anemia”?
o Any thyroid problem? Change in bowel habits? Dry or moist skin?
o Any hx of DM? Do you drink a lot? Do you go to the washroom more
than usual? Weight changes?
- Terminal ileum:
o Did you have any bowel surgery before?
o Were you diagnosed with “Crohn’s disease” before?
o Any repeated attacks of diarrhea? Any foul smelling bulky stools?
- Pancreatic and liver failure:
o Any hx of liver / pancreatic disease?
o Yellowish discoloration / itching / dark urine / pale stools?
- Alcohol:
o Do you drink alcohol? How much? For how long?
- Meds:
o Do you take medications on regular basis? What kind?
o Have you ever been diagnosed with epilepsy? Do you take anti-epileptics?
o Do you see a psychiatrist? Do you take a mood stabilizer?
o Any hx of chemotherapy?
o Have you ever taken a drug called “methotrexate”?
- Hematological causes:
o Anyone told you that you are pale?
o Any recent bleeding (nose / gum / coughing / vomiting blood)? Any
bruises / dark urine / very dark stools?
o Any fever / night sweats / chills? Change in appetite / weight loss? Lumps
and bumps in your body (for LNs)? Bony pains? Any repeated infections?
- Parasites:
o Have you ever consumed raw fish (chronic intestinal infestation by the
fish tapeworm: Diphyllobothrium)?
2011-09- Medical History.doc Page 16 of 52
BLOOD RESULTS – Macrocytic Anemia – B12 Deficiency - SUMMARY
Good morning Mr …, I am Dr …, I understand that you are here today (OR we called
you to come) to get the results of your blood tests (OR x-ray) that you have done few
days ago, I have it and I am going to discuss it with you. However, because it is the first
time that I see you, I need first to ask you some questions to help me get better
understanding and interpretation of these results. Is it OK with you?
5- First let me ask you few questions about the lab test itself (this applies to any blood
work, x-ray, HIV testing, biopsy, jaundice, anemia):
- Why have you done this test?
- Is it the first time to have it?
- Who ordered this test for you? Why?
- When did you have it?
6- Give the information:
- If it is bad news ! SPIKES
- If abnormal blood results or x-ray: explain the results to patient, to decrease the
patient anxiety.
7- I would like to ask you some questions to see how did this (anemia) affect you:
CONSEQUENCES of anemia:
- Anemia symptoms:
- Neuro symptoms:
8- I would like to ask you more questions to find what might be the cause:
CAUSES of Vit B12 deficiency:
- Diet intake: Are you vegetarian? For how long? Do you take supplements?
- Gastric causes:
- Terminal ileum:
- Pancreatic and liver failure:
- Alcohol:
- Meds:
- Hematological causes:
- Parasites:
2011-09- Medical History.doc Page 17 of 52
ACUTE ABDOMINAL PAIN
GIT symptoms:
- Nausea / Vomiting - Heart burn / acidic taste in mouth
- Abdominal pain - Distension / bloating / gas
- Change in bowel movements: constipation / diarrhea
- Blood in stools / vomiting blood
- LIVER: yellowish discoloration / itching / dark urine / pale stools
OsCfD /+/ PQRST ! will give you an idea
You suspect obstruction ! nausea/ vomiting (COCA+B / coffee ground material) AND
bowel movements ! if vomiting ! screen for dehydration
! If you dx obstruction ! check risk factors of obst ! then rest of GI symptoms
! If not obst ! scan GIT ! near-by systems ! PMH for systemic disease
If you suspect kidney stones ! screen with renal symptoms
! If you dx renal stone ! check risk factors ! then rest of urinary symptoms
Intestinal obstruction:
HPI:
A. OsCfD: gradual, started colicky, and now continuous dull pain
B. PQRST
C. What ↑ or ↓
D. Associated symptoms:
" Screen for obstruction:
o Nausea/ vomiting
" Relation to pain, which started first, does it relief pain
" COCA + Blood
" Screen for dehydration (dizziness / light headedness / thirsty)
o Bowel movements
" How about any blood? Any time?
" Still passing gas?
" Risk factors for intestinal obstruction:
o Previous surgery? What? When?
o Fever/ night sweats/ chills / appetite / loss of weight / lumps & bumps
o PMH or FH of cancer or benign tumour
o Hx of Crohn’s disease (hx of abd pain/ bloody diarrhea) / family hx
o Hx of hernia / groin mass
o Gall bladder stones / right upper quadrant pain
" Differential diagnosis:
o Gastroenteritis:
" What did you eat yesterday? Place that you are not used to?
" Diarrhea / blood in stools?
" Anybody else ate with you and suffered from the same problem
o Renal: flank pain / burning sensation / going more to the washroom
o Liver: yellowish discoloration / itching / dark urine/ pale stools
o Hx of HTN / SOB / cough / phlegm
2011-09- Medical History.doc Page 18 of 52
DIFFICULTY SWALLOWING
What do you mean by difficulty swallowing?
- Do you feel difficulty initiating the swallowing?
- Do you feel pain when you swallow?
- Do you feel food is stuck? Can you point where it is usually stuck?
Dysphagia
Progressive Intermittent
All the time and ↑ On and Off
Solids then fluids Fluids first Fluids and solids Solids only
Then solids (Large bolus)
Mechanical Achalasia Esophageal spasm Esophageal webs
Cancer OR stricture Scleroderma and rings
Mechanical Dysphagia:
HPI:
A. OsCfD: gradual, ↑ progressively, to solids then fluids
B. PQRST
C. What ↑ or ↓
D. Associated symptoms:
1- The same system:
i. Nausea / vomiting / undigested food
2- Near-by systems:
i. Any chest pain / tightness
ii. Any cough / change in your voice
iii. Change in bowel movements
iv. Change in the size of the abdomen / abd pain / blood in stools
v. Liver: yellowish discoloration / itching / dark urine/ pale stools
3- Constitutional symptoms: fever/ night sweats/ chills / change in appetite /
loss of weight / lumps & bumps
4- Risk factors:
i. GERD / PUD:
1. Hx of heart burn
2. Were you ever diagnosed with a condition called GERD / PUD
3. Have you ever checked with a camera or a light (endoscope) inserted
into your stomach
ii. Smoking / Alcohol
iii. Family history: esophageal cancer
iv. Radiation to chest
v. Have you ever swallowed any chemical?
2011-09- Medical History.doc Page 19 of 52
ELEVATED LIVER ENZYMES
Introduction
HPI:
1- First let me ask you few questions about the lab test itself (this applies to any blood
work, x-ray, HIV testing, biopsy, jaundice, anemia):
- Why have you done this test?
- Is it the first time to have it?
- Who ordered this test for you? Why?
- When did you have it?
2- Give the information:
- Liver enzymes: AST / ALT ≥ 2
- Explanation: there is increase in one of the markers used to assess / check the
liver functions, it may indicate that there is an injury to your liver, I am happy you
came here today to discuss it so that we can figure this out.
3- I would like to ask you some questions to see how did this affect you:
CONSEQUENCES of liver injury:
- Acute phase:
o Recently, have you noticed any fever / flu-like symptoms / muscle/joint aches
o Constitutional symptoms: sweats / chills / appetite / weight / lumps
o Any yellowish discoloration / itching / dark urine/ pale stools
o Did you recently hate the taste of cigarettes?
- Chronic manifestations:
o Did you notice any increase in the size of your abdomen?
o Puffiness in your face? Swelling in your legs/ ankles?
o Bruises in your body?
o Vomited blood? Blood in stools?
o WITH ALCOHOL: did you notice changes in memory and concentration?
Any weakness / numbness? Balance and falls?
4- I would like to ask you more questions to find what might be the cause:
CAUSES of liver injury:
Now, I would like to ask you some questions to see if you were exposed to liver
disease without being aware of that, some of these questions may be personal, but it is
important to ask (start from least offensive to most offensive)
Including the alcohol, during which ! Drinking assessment
5- PMH:
- Were you ever diagnosed with liver disease before
- Were you ever checked for liver disease before
- Were you ever vaccinated for liver disease before
6- FH: suicide / depression / drinking / liver cancer
2011-09- Medical History.doc Page 20 of 52
Now, I would like to ask you some questions to see if you were exposed to liver disease
without being aware of that, some of these questions may be personal, but it is important
to ask (start from least offensive to most offensive)
Oral
- Any recent travel outside Canada?
- Did you eat any raw shell fish? Did you eat in new place that you are not used to?
Surgical
- Any history of surgeries / hospitalization?
- Any history of blood transfusion?
- Any history of blood donation?
Social
- How do you support yourself financially? If hazardous occupation?
- Did you get exposed to blood products / body fluids?
Risky behaviour
- Any tattooing or piercing?
- SAD?
o Do you smoke?
o Drink alcohol? How about the past? ! Drinking assessment
o Have you ever tried recreational drugs? Any injected drug use? When was
the last time?
- With whom do you live? For how long have you been together?
- Before being with your current partner, did you have other partners?
- When did you start to be sexually active? How many sexual partners did you have
from that time till now?
- What is your preference, men, women or both?
- What type of sexual activity do you practice? Did you practice safe sex all the
time? And by that I mean using condoms!
- Any history of sexually transmitted infections? And screening for STIs?
- Have you ever had sex with sex worker?
- Within the last 12 months, have you had any other sexual partners?
N.B. when do you need to take extensive sexual history? Risky behaviour!
- Liver enzymes
- Jaundice
- Fever
- LNs
- Discharge
- HIV test results
2011-09- Medical History.doc Page 21 of 52
DRINKING
Drinking assessment
Use / abuse MOAPS Impact
Medical Social Legal
Drinking hx Mood Liver Home
How much? Organic Memory / conc. Work
CAGE Anxiety B12
Psychosis Heart
Self-care /
suicide
Drinking history:
- Do you drink alcohol? How about the past?
- What do you drink?
o For how long?
o How often?
- How much?
o 2 bottles of wine a day? 12 beers a day? Have you drunk more than 6
drinks in one setting?
o Do you drink alone or with other people?
o Did you ever drink to the extent of black out?
o What do you feel if you did not drink? Any shaking / heart racing /
sweating? Have you ever had seizures before? Were you hospitalized? Did
you have delirium tremens?
o Do you avoid going to places where you do not have access to alcohol?
- CAGE:
o Did you ever think that you need to cut down on your drinks?
o Do you get annoyed by other people criticizing your drinking?
o Do you feel guilty for your drinking habits?
o Early morning drink?
Problem drinking: 2 of CAGE list for males OR 1 for females
MOAPS:
- Mood:
o How is your mood? Interest? If ok ! do not proceed
o MI PASS ECG
- Anxiety:
o Are you the person who worries too much?
o Do you have excessive fears or worries?
- Psychosis:
o Do you hear voices or see things that others do not?
o Do you think that someone else would like to hurt you?
- Self care / suicide
2011-09- Medical History.doc Page 22 of 52
Impact:
I am going to ask some questions to check what effects does alcohol have on your life?
- The medical is already done in the consequences of liver injury
- Social:
o With whom do you live? How is the relation? Is there any problems? Is it
related to your drinking habits?
o How do you support yourself financially? Where do you work?
" How is the relation with your coworkers / manager?
" Do you miss working days because of drinking?
" Do you need to drink at work?
- Legal:
o Did you have any legal issues related to your drinking?
o Fights? Arguments? Were you arrested before because of drinking?
o Were you charged before for DUI (driving under influence)?
Alcoholic beverages:
" Beer:
o Alcohol percent around 5%
o Pitcher (60 oz) = 3 pints (pint = 20 ounces)
o Ounce (oz) = around 28-30 ml
" Wine / Champaign:
o Alcohol percent around 12%
o Bottle: 750 ml
o Glass: 150 ml
" Hard liquor (whisky / gen):
o Alcohol percent around 40%
o 1 glass (shot) = 1 ½ oz (50 ml)
2011-09- Medical History.doc Page 23 of 52
FEVER – TIRED
Introduction
CC " Fever
" Do you have other concerns?
HPI Analysis OsCfD
" Did you measure it? How often? How? What is highest?
" And medications? Did it help?
" Any flu / illness / sickness
" Any diurnal variation? Any special pattern?
AS Constitutional symptoms
Extensive review " CNS: headache / neck pain / stiffness / nausea / vomiting /
of systems vision changes / bother by light / weakness / numbness
" ENT:
- Ears: pain / discharge
- Nose: runny nose / sinusitis (facial pain)
- Throat: sore throat / teeth pain / difficulty swallowing
" Cardiac: chest pain / heart racing
" Lung (pneumonia, PE (DVT), TB, cancer): cough / blood /
phlegm / wheezes / chest tightness / contact with TB pt
" GIT (except the liver3): abd pain / distension / change in
bowel movements / blood in stools
" Urinary: burning / frequency / flank pain / blood in urine
" MSK: joint pain / swelling / ulcers in your body / mouth /
skin rash / red eye
" Autoimmune: fm hx / dx before with autoimmune dis
" The LIVER:
- Local: yellow / itching / dark urine / pale stools
- Dx before with liver dis? Screened? Vaccinated?
- Transition to risky behaviour
" Do you have any discharge? Ulcers? Blisters? Warts?
PMH Cancer / Autoimmune disease
FH Cancer / Autoimmune disease
SH Does your partner have any fever? Discharge? Skin rash?
3
The liver will be put at the end as a transition to ask about risky behaviour (see liver enzymes case)
2011-09- Medical History.doc Page 24 of 52
CHRONIC DIARRHEA
Introduction
CC
HPI Analysis od CC OsCfD " What bout during night?
COCA - Yes ! organic
± B/Mucous - No ! irritable bowel syndrome (IBS)
↑↓ - How does if affect your sleep?
" Did you notice blood?
- Before you have your bowel move?
- Mixed (higher source of bleeding)?
- On the surface?
" Consistency: watery / loose / formed /
bulky. Any floating fat droplets / difficult
to flush / undigested food
" Impact:
- Acute! dehydration: feel thirsty / dizziness / light
headedness / LOC
- Chronic ! weight loss
AS " Pain ! OCD / PQRST
- If pain improves after bowel movement: IBS
" Vomiting
" Alteration with constipation
Red flags
" Constitutional symptoms – for infection / cancer
" For cancer: Fm Hx of Ca colon / change in the calibre of
stools / what kind of diet
Extra-intestinal " Rheumatic disease: red eyes / mouth ulcers / skin changes/
causes rash / nail changes / hx of psoriasis / joint pain / swelling /
back pain / stiffness (especially in morning) / discharge
" Hyperthyroidisms: heat intolerance
" Diet: Celiac disease / A lot of dairy products / lactose
intolerance / lots of juice / sugars
" Infectious: travel / camping / with whom do you live? Any
other person at home with diarrhea?
- HIV – if risk factors
" Medications: antibiotics / stool softeners
" Stress: How about your mood? MI PASS ECG
PMH
FH
SH What are you doing for life? Any stress?
2011-09- Medical History.doc Page 25 of 52
Counselling:
- Explanation:
o From what you have told me, the most likely explanation for your diarrhea
is the medical condition known as “Irritable Bowel Syndrome”.
o What do you know about IBS?
o It is a common condition, and a lot of people have it, this is a long term
disease, but it is treatable.
o What I need to do is to do physical exam, and do some blood works and
stool analysis to rule out other causes, how do you think about that?
- Management:
o The best way to treat this condition is by prevention:
" Stress management and life style modification
" Diet modification: to change the fibres content of diet
o Medications: Imodium
o If mood is low ! depression counselling, it might be a mood problem
o If drinks too much alcohol ! advise to decrease alcohol
- Offer more information:
o I will give you some brochures and web sites in case you want to read
more about that
2011-09- Medical History.doc Page 26 of 52
ACUTE DIARRHEA
Introduction
CC
HPI Analysis od CC OsCfD " Did you notice blood? When did it start?
COCA - Before you have your bowel move?
± B/Mucous - Mixed (higher source of bleeding)?
↑↓ - On the surface?
" Impact:
- Acute! dehydration: feel thirsty / dizziness / light
headedness / LOC
AS " Pain ! OCD / PQRST
" Vomiting
" Alteration with constipation
Red flags
" Constitutional symptoms – for infection / cancer
" Flu like symptoms
" Any body around you have the same diarrhea?
Extra-intestinal " Rheumatic disease: red eyes / mouth ulcers / skin changes/
causes rash / nail changes / hx of psoriasis / joint pain / swelling /
back pain / stiffness (especially in morning) / discharge
" Hyperthyroidisms: heat intolerance
" Diet: Celiac disease / A lot of dairy products / lactose
intolerance / lots of juice / sugars
" Infectious: travel / camping / with whom do you live? Any
other person at home with diarrhea?
- HIV – if risk factors
" Medications: antibiotics / stool softeners
PMH
FH
SH
Investigations for clostridium difficile:
- CBC / lytes and chemistry
- Stool assay for toxin
Treatment for clostridium difficile:
- Stop the antibiotic
- Metronidazole, if not effective ! vancomycin
2011-09- Medical History.doc Page 27 of 52
ASTHMA
Mr … comes to your office as post-ER visit follow-up, he had asthmatic attack three days ago.
He went to ER; he was treated and discharged with advice to see his family physician.
Introduction
How do you feel now?
Analyze the attack he had? " The setting
Os Cf D " Which medication was used?
" How many times he needed to puff?
Symptoms of asthma? " SOB / Tightness / Wheezes
" Sweating / heart racing / LOC
" Did you turn blue? Were you able to talk?
" Who called 911?
" Were you admitted to hospital? ER? Did they need to
put a tube? What were the discharge meds?
Asthma history " When were you diagnosed? How? Which type?
" Were you controlled? How many times do u puff?
" Recently, did you notice a need to ↑ the doses?
" Any attacks during the night?
" How many times did you have to go to ER?
Did he use peak flow meter?
Triggers Infection " Recent chest inf? Flu-like symptoms? Fever? Chills?
Medications " How do u use puffers? Stored properly? Not expired?
" Did you start new medication? β-blockers? Aspirin?
Outdoor Exercise Cold air
Dust Pollens (seasonal?)
Indoor " Do you smoke? Anybody around you?
" Do you have pets? People around you?
" Fabrics related: carpets floor? Any change in linen?
Pillows? Blankets? Mattress?
" Relation to any type of food?
" Do you live in a house (basement ! mold)?
" Any construction renovation? Exposure to chemicals?
Stress Any new stressful situations?
+ Question: Identify the trigger
+ Treatment: eliminate the triggers
2011-09- Medical History.doc Page 28 of 52
CARDIAC CASE:
Acute Chronic
Minutes – hours Hours – days Intermittent Continuous
Cardiac: Cardiac: Cardiac:
- CAD - Pericarditis - Unstable angina
- Aortic dissection - Unstable angina
Non-cardiac: Non-cardiac - Cancer
- Tension - Pneumonia - Herpes zoster
pneumothorax - Pleurisy - Trauma
Panic attack Pulmonary Panic attack
GIT: embolism GIT:
- GERD - GERD
- PUD - PUD
- Esophageal - Esophageal
spasm spasm
Risk factors for PERICARDITIS:
- Recent flu like symptoms
- Medications
- History of surgery
- History of heart attack
- History of kidney disease / puffy face
- History of TB
- History of autoimmune disease
Risk factors for PULMONARY EMBOLISM:
- Recent long flight
- History of malignancy
- Female:
o Pregnancy
o OCPs
o HRT
- Family history of blood clots
2011-09- Medical History.doc Page 29 of 52
UNSTABLE ANGINA:
Chest pain for 6 weeks
Introduction … But first I would like to ask you, at the moment, how do
you feel?
HPI: analysis of CC - OsCfD
- PQRST
- What ↑ or ↓
- Is it related to activity? How many blocks were you able
to walk? And now?
- How about night? And rest?
- When was the last attack
HPI: TRIGGERS - Exertion
- Stress
- Cold air
- Heavy meals
- Sexual activity
Risk factors Risk factors for ischemic heart diseases – IHD
Impact Manifestations of CHF:
- SOB
- Limitation of activity
- Swelling in your legs
- How many pillows do you use?
2011-09- Medical History.doc Page 30 of 52
GERD – GIT CAUSES OF CHEST PAIN:
Introduction … But first I would like to ask you, at the moment, how do
you feel?
HPI: analysis of CC - OsCfD
- PQRST
- What ↑ or ↓
- Is it related to activity? How many blocks were you able
to walk? And now?
- How about night? And rest?
- When was the last attack
HPI: TRIGGERS Angina triggers: GERD triggers:
- Exertion - Smoking / Alcohol
- Stress - Heavy / late meals
- Cold air - Coffee / mint
- Heavy meals - Pregnancy (progestin)
- Sexual activity - Playing golf (leaning
forward)
HPI: associated Cardiac symptoms GIT symptoms
symptoms
Risk factors Risk factors for ischemic
heart diseases – IHD
Impact Manifestations of CHF: Complications:
- SOB - Cough
- Limitation of activity - Change in the voice
- Swelling in your legs - Long term: cancer or
- How many pillows do stricture
you use?
+ The patient has a concern: is this IHD? Is his heart endangered?
1. This is quite a reasonable concern? What made you think about that?
2. Especially you have many risk factors that may predispose to heart attack. Right
now the physical exam is ok, but we still need to check your heart more, we will
do some lab works and an electrical tracing for your heart (ECG), then if we need
we still may need to stress ECG, in which test, we trace your heart while you are
exercising. Then we know for sure the condition of your heart.
3. However, we would like to take measures to try to decrease your risk of
developing heart attack, e.g. exercise / diet / smoking
4. On the other hand, the most likely diagnosis of what you have is a medical
condition called “GERD”, …see the details below …
2011-09- Medical History.doc Page 31 of 52
ANKLE SWELLING – BILATERAL
Introduction Differential diagnosis of BILATERAL
CC ankle swelling:
HPI: - Failure Heart
- Analyze the swelling (OCD – ↑↓) - Failure Liver
- Failure Kidney
Associated symptoms: - Hypoalbuminemia
- Local symptoms - Thyroid diseases
Lower extremities
Other swellings
- Systems review / Thyroid (DD)
- Specific cause within this system
PMH
FH
HPI:
Analyze the swelling:
- What ↑? Walking / standing what ↓? Raising legs
- How high does it go?
- How does this affect your life?
Local symptoms:
- In the lower extremities:
o Pain / fullness / heaviness / tightness
o Skin changes (redness / swelling / do you feel your feet warm?)
o Nail changes
- Any other swellings in your body?
o How about swelling in your face? Eye puffiness? Do you find it difficult
to open your eyes in the morning?
o How about your belly? Did you need to ↑ the size of your belt?
o Hands, did you feel it is tight to wear your ring?
Systems review / thyroid:
- Heart / Liver / Kidney / Thyroid
- Constitutional symptoms
Specific cause within this system (which kidney disease caused this)
- Hx of kidney disease (changes in urine / bruising / frequency / burning)
- Hx or Dx of DM
- Any medications (penicellamine, gold, NSAIDs, …)
- Recent sore throat
- Any skin infection / rash
- Hx of autoimmune disease
- How about diet? Is it balanced? Any diarrhea?
2011-09- Medical History.doc Page 32 of 52
ANKLE SWELLING – UNILATERAL
Introduction Differential diagnosis of UNILATERAL
CC ankle swelling:
HPI: - Gout
- Analyze the swelling (OCD – ↑↓) - DVT
- If pain ! PQRST - Arthritis,
- Gonorrhea septic arthritis
Associated symptoms: - Trauma and ankle twist
- Local symptoms - Infection, sepsis, cellulitis
Other ankle
Other joints
- Systems review (DD)
- Specific cause within this system
FH
HPI:
Analyze the swelling:
- How does this affect your life?
Local symptoms:
- Other ankle
- Other joints; toes?
o How about swelling in your face? Eye puffiness? Do you find it difficult
to open your eyes in the morning?
o How about your belly? Did you need to ↑ the size of your belt?
o Hands, did you feel it is tight to wear your ring?
Systems review (DD):
- Any trauma, any twist in your ankle?
- Constitutional symptoms
- Sexual history, penile discharge?
- Screen kidney ! for kidney stones
Specific cause within this system (which factor led to this gouty attack)
- Tell me more about your diet? Too much protein?
- How about alcohol?
- Medications?
- Hx of cancer / chemotherapy / radiation
- Family hx of gout / kidney stones
2011-09- Medical History.doc Page 33 of 52
CONGESTIVE HEART FAILURE:
68 years old man comes to ER with 4 weeks of SOB
Introduction
CC clarification 1- When do you say SOB; what do you mean?
1- Cardiac or chest - Is it difficult to breathe in and out? ! cardiac / anemia
2- Newly dx or acute - Is it difficult to breathe out? ! COPD / asthma
on top of CHF - Do you have any hx of asthma? Lung disease? Any
wheezes? Chest tightness / cough? Any racing heart?
Dizziness? LOC? Any hx of HTN?
2- Do you have any hx of heart disease?
- No ! newly dx
- Yes ! acute on top of CHF
HPI: analysis of CC - OsCfD
- PQRST
- What ↑ or ↓
" Is it first time? Or you had it before? When and how
were you diagnosed? How about treatment?
" Is it related to activity? How many blocks were you
able to walk? And now?
" How about night? And rest?
HPI: associated - Left ventricle:
symptoms " How many pillows do you use?
" Do you wake up at night gasping for air?
- Right ventricle:
" Any swelling in your LL? How high does it go?
Related to position / standing? Weight gain?
" Eye puffiness? Swollen face? Pain on the liver?
- Other cardiac symptoms:
" Chest pain? Nausea/vomiting? Sweating?
" Heart racing / dizziness / LOC? Do you feel tired?
Risk factors Risk factors for ischemic heart diseases – IHD
Impact - Heart failure
Are you receiving treatment? Are you under regular
F/U? How often? When was the last time?
Causes (that precipitated - Compliance:
acute on top of CHF) " Which medications do you take? How much? For
how long?
" Do you take it on regular basis? Any chance that you
may skip one or more doses?
" Do you take it by yourself or do you need help?
" Did you get your Digoxin level measured recently/
" Did you start new medication? Rx or (OTC) over the
counter? e.g. indomethacin
2011-09- Medical History.doc Page 34 of 52
- Diet:
" Do you have special diet? Salt-free diet? Do you
monitor that?
" Any new changes in diet?
" Any chance of salty food, e.g. pickles, canned food,
dried meet and fish
- New pathology:
" Any hx of long term disease (HTN / DM / Kidney /
Liver / Lung) disease
" Any hx of thyroid dx, any sweating / diarrhea?
" Any bleeding?
" Any change in your bowel movement
" Constitutional symptoms
" SAD
Notes:
Causes (to precipitate acute on top of CHF):
- F Forget to take medication
- A Anemia / Arrhythmia
- I Ischemia / Infarction / Infection
- L Life style (salty food)
- U Upper regulation: pregnancy / hyperthyroidism
- R Renal failure
- E Embolism
2011-09- Medical History.doc Page 35 of 52
FALL:
Orthostatic hypotension
76 years old male patient came to clinic because he fell few days ago. He was getting out
of bed, when he fell to the ground
Introduction … Did you hurt yourself? How do you feel?
HPI: analysis of CC - OsCfD Differential Diagnosis
(syncope):
- Was it related to: - Arrhythmia
" Emotions? - Ischemia
" Coughing? - CVA
" Urination? - Seizure
- Hypoglycemia
HPI: any During - Did you lose conscious?
Fall, LOC or - Were you alone or with someone? Did … describe it to
seizure you? Is … with you? If it is ok with you, after we finish, I
would like to ask … some questions!
- Were you shaking? Certain part of your body or whole?
- Were you breathing? Did you turn blue?
Before - Were you able to take few steps or did you fall
immediately (orthostatic hypotension)?
- Before you lose consciousness, did you feel:
" Dizzy, lightheaded, nausea, vomiting,
" Things are spinning around you
" Any chest pain, heart racing (cardiac)
" Weakness, numbness (stroke)
" Any flashing light, strange smells (epilepsy)
" Sweaty, shaky, hungry (hypoglycemia)
After - How long did it last?
- How did you regain consciousness? By yourself or did
you need intervention?
- After you regain consciousness; were you able to
recognize the surroundings? Able to talk? Able to move?
- Did you feel any weakness, numbness?
HPI: associated Any geriatric patient; ASK about:
symptoms - Balance
- Vision
- Hearing
- Urination
Risk factors - Is your room well lit? Any chance you tripped?
- Do you take any medications? Do you have a list?
" Go through it one by one
" Which one was added / changed recently?
" Each medication: ask about the disease, when started?
" Any OTC? Aspirin? Who prescribed it to you?
- Are you getting enough fluids
2011-09- Medical History.doc Page 36 of 52
Counsel - Inform the patient
" The condition is “orthostatic hypotension”
" Explain the pathophysiology
" Consequences: this might happen again
" Investigations
- Preventive measure:
" Contact the psychiatrist to check the poly-pharmacy
" While you are changing positions, do this slowly
- Offer more information
2011-09- Medical History.doc Page 37 of 52
HEART RACING:
For few weeks
Causes for AF: Causes for TACHYCARDIA
1- IHD 1- Exercise
2- Hypertension / CHF 2- Pregnancy
3- Valvular heart diseases 3- Caffeine / stimulants
4- Congenital heart diseases 4- Anemia
5- Hyper-thyroidism 5- Hypovolemia
6- Medications (e.g. digoxin, some anti- 6- Fever
arrhythmic meds – class I) 7- Stress
7- Electrolytes imbalance 8- Smoking
8- Loan AF 9- Hyper-thyroidism
9- Myocarditis 10- Pheochromocytoma
10- COPD / pneumonia
11- Cardiac surgery
12- Too much alcohol (holiday heart)
13- Cocaine
14- Any condition that lead to tachycardia in a
susceptible person
Introduction … But first I would like to ask you, at the moment, how do
you feel?
CC clarification When do you say your heart is racing; what do you mean?
- Do you feel your heart is going fast
- Or is skipping beats
- Can you tap it for me please? …
- It sounds irregular for me!
HPI: analysis of CC - OsCfD
- PQRST
- What ↑ or ↓
- Is it related to activity? How many blocks were you able
to walk? And now?
- How about night? And rest?
- When was the last attack? And what is the duration of the
longest attack?
HPI: TRIGGERS - Is it related to caffeine, chocolate, coke, any type of food?
- SAD (cocaine or any other stimulant)
HPI: associated Cardiac symptoms (chest pain / tightness / dizziness / light
symptoms headedness / LOC / pass out / did you feel your heart bouncing)
Causes - Any hx of heart disease / heart attack / any congenital or
valvular disease / rheumatoid fever / repeated sore throat?
- Chest diseases
- Thyroid
- Any anemia / bleeding
- Do you take medications on regular basis?
2011-09- Medical History.doc Page 38 of 52
Impact - CVA (any weakness / numbness / difficulty finding
words / visual problems)
- Heart failure (SOB / limitation of activity / swelling in
your legs / how many pillows do you use??
FH - Family history of sudden death at a young age?
(cardiomyopathy)
Physical examination - Vitals
- Cardiac exam (looking for mid-diastolic, mitral
stenosis, rumbling character)
- Thyroid exam
- Neurological exam: gross motor and reflexes
+ The patient daughter has a concern: my mother was diagnosed with AF, should I
worry about this?
1. This is a reasonable concern?
" AF may lead to embolic event (CVA)
" AF may lead to heart failure
" AF may lead to V. Fib
2. However, this is not uncommon condition, and it is treatable with medications
2011-09- Medical History.doc Page 39 of 52
PERIPHERAL VASCULAR DISEASE:
Calf pain / swelling
Introduction
HPI: analysis of CC - OsCfD
- PQRST
" R: what about other joints, knees? Thighs? Feet?
Peripheral Arterial - What ↑ or ↓: did you notice that your pain ↑ while
Disease versus Spinal walking up or down hill?
Canal Stenosis " ↑ while walking uphill: peripheral arterial disease
" ↑ while walking downhill: spinal stenosis
- Is it related to activity? How many blocks were you able to walk?
And now?
- How about night? And rest?
- When was the last attack? And what is the duration of the longest
attack?
HPI: associated Cardiac symptoms Neuro symptoms
symptoms - Cold feet / ulcers - Weakness / numbness /
Cardiac vs. neuro - Swelling / redness tingling
- Delayed wound healing - Back trauma / back pain
- Nail changes / hair loss - Sexual dysfunction
Constitutional symptoms
Risk factors - Smoking? How much and for how long?
- High blood pressure? For how long? Controlled or not?
- Diabetes mellitus
- Cholesterol measured? When? What was it?
PMH - Past history of heart disease / stroke
FH - Family history of heart disease
N.B. the 6 Ps of ischemia:
Pallor / Pain / Parathesia / Paralysis / Pulseless / Polar (cold)
2011-09- Medical History.doc Page 40 of 52
ANURIA:
Urinary symptoms:
- Obstructive (anuria in ♂ and incontinence in ♀):
" Difficulty to initiate urine? Do you need to strain?
" Any changes in the stream?
" Any dripping?
" After you pass urine, do you feel that you emptied your bladder completely or do
you need to go again?
- Irritative (frequency):
" How many times do you go to the washroom?
" How about before? Any change?
" How about during night time? How does this affect your sleep? How
about your concentration and mood?
" Do you need to rush to washroom? Are you able to make it all the time?
" Have you ever lost control or wet yourself?
" Any burning sensation? Any flank pain?
" Fever / night sweats / other constitutional symptoms
- Urine analysis (changes):
" COCA + B (content: frothy / cloudy / not clear)
Introduction Empathy – how do you feel right now?
HPI: analysis of CC - OsCfD
- PQRST
- What ↑ or ↓
Obstructive symptoms
Irritative symptoms
Urine analysis (changes)
Local symptoms - Any problems with passing stools? What? When?
- Any masses in the groin / pelvic mass / pain?
Constitutional symptoms
Complications Metastasis - Back: pain / weakness / numbness
- Liver: yellow / itchy / urine / stools
- Lungs: cough / phlegm / hemoptysis
- Brain: headache / nausea / vomiting
Renal failure Swelling / face puffiness / itching
Sexual Sexual dysfunction
Risk factors - Have you ever diagnosed with prostate disease? Screened
for prostate diseases? (DRE or PSA)
- Smoking? Alcohol?
- Family history of prostate disease / cancer bladder?
Differential diagnosis - Stones
- Back problem (trauma – cauda equine – metastasis)
- Stroke (diagnosed / weakness / numbness / difficulty)
- Medications: glaucoma / anti-psychotic medications
- Cancer bladder (radiation / dye / chemicals)
2011-09- Medical History.doc Page 41 of 52
INCONTINENCE:
Obstructive / 62 years old female, with hx of 3 years of urinary incontinence
Introduction Empathy – how do you feel right now?
HPI: analysis of CC - OsCfD
- PQRST
- What ↑ or ↓
Obstructive symptoms If at any time there is a frequency or some new symptom !
Irritative symptoms analyze it first then resume!
Urine analysis (changes)
Local symptoms - Any problems with passing stools? What? When?
- Any masses in the groin / pelvic mass / pain?
- Any perineal skin lesions?
Constitutional symptoms
Risk factors - Obstetric history
- Gynaecological history
- LMP
- Menopausal symptoms, and HRT
- Previous surgery
2011-09- Medical History.doc Page 42 of 52
LUMP – THYROID
Introduction
HPI: analysis of CC The lump
Constitutional symptoms + bone pains
Local symptoms Rule out infection: Any recent flu-like symptoms? Do you
feel tired/ fatigue? History of sinusitis/ Pain in your face?
Runny nose? Pain/discharge in ears? Any sore throat/ oral
ulcers/ tooth pain? Neck stiffness/pain? Headache? Vomiting?
HEAD SSS ! risky - A: includes recent travel
behaviour - Did you notice any vaginal discharge/ bleeding? Any
pain/ blisters/ warts? Discoloration/ itchiness?
PMH
FH
Physical exam - Vital signs
- LNs / Lymphatic system / LNs in groin / vaginal exam
- Liver / Spleen
LUMP:
- Can you point to it?
- OsCfD
- Can you estimate its size for me? Is it like a lent, olive, lemon, or larger? Did it
change in size? How fast was the change in size?
- Did you try to feel it? Does it feel soft / rubbery / hard?
- Is it painful? PQRST
- Do you feel it is fixed or moving?
- Any skin changes? Redness? Ulcers?
- Is it the only one? Did you notice other lumps in your body? How about your
neck? Arm pits? Groins?
Notes:
- Whenever there is IV drugs ! screen for liver symptoms / HIV
- Whenever there is risk for STIs ! screen for liver symptoms and PID
2011-09- Medical History.doc Page 43 of 52
LUMP – BREAST
Introduction
HPI: analysis of CC The lump
Constitutional symptoms + bone pains
Local symptoms Rule out infection: Any recent flu-like symptoms? Do you
feel tired/ fatigue? History of sinusitis/ Pain in your face?
Runny nose? Pain/discharge in ears? Any sore throat/ oral
ulcers/ tooth pain? Neck stiffness/pain? Headache? Vomiting?
Consequences of cancer - Headache/ vomiting?
metastasis - Back pain/ weakness/ numbness/ tingling in arms or legs?
- Chest pain/ cough/ phlegm/ wheezes/ heart racing?
- Liver: yellow discoloration/ itching/ urine/ stools?
Risk factors - Menstrual history: first period / last period / regular?
- History of pregnancies? Number of pregnancies? First
pregnancy at what age?
- Breast feeding? OCPs?
- Diet rich in fat
- PMH or FH of cancer breast / ovarian carcinoma
PMH Of cancer
FH Of cancer
LUMP:
- Can you point to it?
DO NOT POINT WITH YOUR HANDS OR FINGERS!
- OsCfD
- Is it one breast or both? Where did you notice it? You can ask verbally, is it
Lt / Rt? Upper / Lower? Outer / Inner?
- Can you estimate its size for me? Is it like a lent, olive, lemon, or larger? Did it
change in size? How fast was the change in size?
- Is it related to your period? Does it change with the period?
- Did you try to feel it? Does it feel soft / rubbery / hard?
- Is it painful? PQRST
- Do you feel it is fixed or sliding (moving)?
- Any skin changes? Redness? Ulcers?
- Any nipple changes? Discharge? Bleeding? Itching?
- Is it the only one? Did you notice other lumps in your body? How about your
neck? Arm pits? Groins?
Differential diagnosis:
- Benign disease
- Trauma ! fat necrosis
2011-09- Medical History.doc Page 44 of 52
INR – COUNSELLING
Introduction
Give the information
Consequences Bleeding / DVT relapse
Causes
DVT Complications
Warfarin / Blood thinners
IF FEMALE OCP / pregnancy / LMP / vaginal bleeding
Decision
Conclusion Offer brochures, support. If you have time: SAD / PMH
Introduction:
- Why are you doing this INR?
- When were you diagnosed? How?
- Were you admitted through the ER or outpatient?
- Was there any involvement of your lungs?
- Which medications were you taking?
- Do you measure your INR regularly? When was the last time? What was the
result? What is your target?
Give the information:
- Your measurement today shows INR of 1, any idea why?
o Compliance / forget / other medications / diet
- Are you still taking your warfarin? On regular basis?
- Do you take your medications on your own, or does someone else help you?
- Any chance that you missed a dose?
- Did you start a new medication? What? Why? When?
- Do you eat a lot of spinach? Or dark green vegetables? (rich in vit K)
- Did you stop your medication? Why?
Consequences:
Now, I would like to ask you some questions to check if you have bleeding or relapse of
your DVT or not, then we will go from there
Bleeding:
- Did you notice any bleeding?
- Did you notice bleeding from your gums / nose / coughing or vomiting blood /
bruises in your body / dark urine / urine in stools?
- Any weakness / numbness / difficulty finding words / vision difficulty?
- Did any one tell you that you look pale? Do you feel fatigued?
DVT relapse:
Because you stopped your medication, I would like to make sure that there is no
relapse
- Have you had any pain / swelling / redness in your calf muscles?
- Have you had any SOB, chest pain, heart racing?
2011-09- Medical History.doc Page 45 of 52
Based on what you have told me, there are no obvious serious consequences, if it is ok
with you, we can discuss your situation now!
What is your understanding about DVT?
Causes:
- It might happen after prolonged sitting without movements (like very long flights)
- Or due to certain medical condition,
- The blood tends to form clots in the deep veins of the lower extremities
Complication:
- Relapse 8%: without treatment, and that is concerning!
o Whenever we treat the patient, our target is to decrease the relapse rate to
0.8% which is 1/10 of the risk without treatment
- These clots are not fixed, and sometimes they get dislodged from your leg and
travel along your blood vessels, all the way to the lungs (chances are 3%):
o If large enough ! might cause sudden death
o If showers of small clots ! you may not feel anything right now, but it
later will cause pulmonary HTN, which is a debilitating disease, with
serious consequences and we do not have treatment for it till now
- Always in medicine, we try to balance the benefits and the side effects, and in this
condition, the benefits largely outweigh the risks.
Now, what do you about blood thinners?
- It is a medication used to make our blood thin, preventing our body from forming
clots by competing with vitamin K, which is needed for the formation of the
elements of blood clots.
- We take warfarin seriously, and that is why we monitor it closely and regularly,
by assessing the INR which is an indicator of the effect of warfarin. Therefore, as
long as your INR is within your target, the risk of bleeding is less than 1%, and
almost near 0% to have intra-cranial (brain) hemorrhage without having external
bleeding first. That is why you need to keep monitoring yourself, and seek
medical attention if you notice any signs of bleeding.
For FEMALES:
- Are you taking any OCPs? OCPs might increase the risk of developing DVT.
- Are you pregnant? Warfarin is not to be used during pregnancy; we will use
heparin instead of it.
- Have you had any vaginal bleeding?
Decision:
If the patient decides that he will restart the treatment:
- We will do it the same way as we did the first time:
o We will start heparin and warfarin together then stop heparin after 3 days
- We will need to measure the INR daily (till we reach our target) then twice a
week, then weekly, then every 2-4 weeks
2011-09- Medical History.doc Page 46 of 52
NOTES:
- Numbers to remember:
o Relapse (recurrence) of the DVT: 8% without treatment and 0.8% with
treatment.
o Possibility of DVT ! clots and PE: 3%
o Chances of having bleeding with warfarin: 1%, and almost near 0%
chance of having intra-cranial bleeding without having an extra-cranial
bleeding.
- The initial DVT counselling should have been done in the first time, when the
patient was diagnosed; which includes:
o General knowledge about DVT
o Causes and risk factors
o INR follow up
- My best friend was taking warfarin, and he had brain hemorrhage!
o I am sorry to hear that, this must be stressing / worrying, especially that
you are taking the same medication and he is a close friend to you.
o We prescribe warfarin for many reasons, the issue here is that your friend
was not my patient, and I do not know about his condition, so I am not in a
position to comment on this situation.
o I am glad you came here today, so that we can discuss this together.
- If you do not know the answer to a question:
o This is a good question / point, I will check it for you and we will discuss
it next visit.
o It is better to refer you to the specialist; there are too many points
regarding this issue that it will be better to discuss it with the specialist.
- A good statement to use in different counselling situations: always in medicine,
we balance the benefits and the side effects.
- Do NOT criticize other doctors or the patient
2011-09- Medical History.doc Page 47 of 52
PATIENT IS RECEIVING BLOOD – COUNSEL FOR ADVERSE REACTIONS
You were called to assess a patient who is receiving blood, and the nurse has concerns.
Adverse effects of blood transfusion:
" Febrile reaction: most common / not serious
" Anaphylactic reaction: not common / serious
" Haemolytic reaction: not common / serious
Introduction to nurse / what is your concerns / ethical challenge
Introduction to patient / ethical challenge
ABCD
History
Brief physical exam
Adverse reactions of blood transfusion
Plan
Introduction to nurse / what is your concerns / ethical challenge
- Good afternoon, I am Dr … May I get your name please?
- How can I help you? OR What are your concerns?
o There is a mistake!
- What do you mean by mistake? How is the patient doing?
o This was wrong blood!
- Did you stop the transfusion?
o Yes
- That is great, this is the first step in the right direction
- Now, what do you mean by “wrong blood”? Is it the same bld group or no? Cross
matched or not? Do we have the patient name on the units?
o It is the same group but with other patient name
o Doctor, please do not tell the patient!
- Why? Do you have any concerns?
o I might be fired!
- I see you have concerns here, but we need to stabilize the patient first. Then we
will speak about that. However, we need to investigate before making decisions.
- Can you tell me when did this happen? How much did he receive?
Introduction to patient / ethical challenge
- Good afternoon Mr …, I am Dr … The nurse was updating me about your
condition. It looks like there was an unintentional medical error took place, and I
need to make sure you are ok.
o Is it serious doctor?
- Could be! There are different possibilities; I need first to check you.
o Whose mistake is this? Is it the nurse mistake?
- Usually in the blood transfusion process, there are many steps; any one of those
might go wrong. It is early now to judge. I need first to make sure you are ok and
stable, and then I will file an incidence report. Investigations will be done, and
you will be informed with the results.
2011-09- Medical History.doc Page 48 of 52
ABCD
Let us make sure you are safe and stable first.
AB:
- Can you please open your mouth? Mouth is clear with no swelling. Do you have
any itchiness or swelling in your mouth?
- Trachea is central, no engorged jugular veins. Can I listen to your heart please!
Normal heart sounds.
C:
- Can I know the vitals please? Normal / stable.
- Can you remove the blood unit please, and send it to the blood bank. We need to
re-cross this patient blood with this unit.
- Can you put another IV line please! We need to take samples for: CBC /
differential / lytes / blood grouping and re-crossing / haptoglobin / bilirubin level
D:
- I am going to shine light in your eyes!
- Can you hold my fingers please? Do not let go.
- Do you feel me touching you?
- Patient is grossly neurologically free.
- If fever: give 2 tablets Tylenol 325 mg
- Can you please prepare:
o Epinephrine / steroids / Benadryl / for anaphylactic reaction
o Diuretics and fluids for haemolytic reaction
History
Now, I would like to ask you some questions:
- Why are you taking blood?
o They have found that I have anemia
- Did you take blood before? Or is this the first time?
- Do you feel warm? Shivering? Chills?
- Do you feel any itching or swelling in your lips / mouth?
- Any heart racing? SOB? Wheezes? Dizziness?
- Any flank pain? Back pain? Weakness?
Brief physical exam
- No IV line oozing
- No hives on skin
- No mouth swelling
- Listen to heart / lungs ! clear
- Press on flanks / spine ! no tenderness
Adverse reactions of blood transfusion
- Blood transfusion is a commonly used procedure, and it is life saving. A lot of
precautions are taken to make sure it is completed safely. However, like any other
medical intervention, it has some side effects.
2011-09- Medical History.doc Page 49 of 52
- The most common reaction that might happen is called “febrile reaction”. This is
not serious reaction and it is self limited. It might happen again, so if it happens,
next time we give you Tylenol before the transfusion.
- Another adverse effect, which is less common but more serious, it is called
“anaphylactic reaction”. This is a form of severe and serious sensitivity reaction,
in which the blood pressure drops suddenly, and there is a swelling of the tongue,
lips, and mouth, with difficult breathing. We do not have a method to predict it.
However, based on your symptoms, your physical exam and vital signs it is less
likely you have that.
- The third adverse effect is called “hemolytic reaction”, and it happens if the
patient receives blood that belongs to another blood group. It causes damage to
blood cells which leads to back pain and flank pain, and could have serious
consequences.
However, your symptoms, physical exam and vital signs, do not cope with this
reaction too.
And the fact that you received blood from the same blood group makes it less
likely you will have hemolytic reaction.
- We prepared medications to deal with any reaction and we will keep you for a
while to monitor you, to make sure that will not happen.
Plan
- Call the blood bank to withhold the other units (previously cross-matched)
- File an incident report
2011-09- Medical History.doc Page 50 of 52
Counselling – Ventilator
Mr Johnson is 75 years old gentleman, his life-long wife for 50 years has a terminal
COPD, with severe pneumonia, and she is on ventilator for the last 3 weeks, and it is not
possible to wean her from ventilator, you called him to inform him about the condition.
1- What do you know about your wife’s condition?
- Listen carefully
- Show understanding and empathy
2- Give information about her condition,
- Give clear simple information
- Stress on the progressive, irreversible nature of the disease
3- As regarding her condition now, have you ever discussed this with her? Has she ever
expressed her wishes about what would she like to be done to her if she needs to be
resuscitated or put on ventilator? Does she have any advance directives or living will?
4- Give alternatives:
- Remain on ventilator, with no evidence that she will be able to breath by own, and
with the possibilities of fatal complications like infections, bed sores, … Some
people does not like to have this quality of life
- Stop the ventilator and she will pass away in peace
5- What do you think about this now?
6- Offer time if he needs to discuss it with other close family members, or if he needs to
arrange any thing (e.g. I am just giving you information, and we can arrange a
meeting with the family within 2 days so that I can explain to them).
+ What if she does not want to be on ventilator but he would like to leave her on the
ventilator?
Mr Johnson, I am sorry to tell you that, actually it is not our decision or your
decision, it is her choice. And she expressed her wishes before; she decided that
she does not want to have this poor quality of life. We have to respect her wishes.
2011-09- Medical History.doc Page 51 of 52
ETHICAL QUESTIONS
" Patient has the right to access his/her medical file, we can not withhold it
" Patient wants to leave you as family physician ! it is his right, and he/she has the
right to take all his/her medical data and file
" If you want to terminate a patient from not seeing you as family physician:
o Give proper notice period
o See him/her for emergency
" Confidentiality; when to break confidentiality? To report for the ministry of
transportation for example:
o Dementia / delirium
o Vision problems
o Seizure disorders
o Schizophrenia (case-based)
o Heart attack ! 1 month not allowed to drive
o Alcoholic with liver failure (based on criteria: albumin / INR / bilirubin)
" Report for child safety ! CAS (Children Aid Society)
o Even if POTENTIAL or SUSPECTED
o Child neglect / abuse
" Patient wants to leave hospital against medical advice; e.g. patient has just had a heart
attack, and still insists to leave the hospital!
o I would like to make sure he is competent, not under influence of alcohol
or any substance, and to rule out suicidal ideation
o I would explain to the patient: diagnosis / treatment / side effects of
treatment / complications of not receiving treatment / alternatives
o I will document this, and I will ask the patient to sign a LAMA (leaving
against medical advice), and I will let him go
" Biological parent wants to know the medical details of his/her son, who is adopted by
another family!
o In order to determine whether I should release any information or no, I
would like first to know who has the legal custody (guardian) of this child.
It might be the adopting father, a social worker (case manager) …
" Any unconscious patient ! ask for DNR or advanced directives
" MMS exam score < 24 ! patient is incompetent;
o You have a case of patient, who had surgery, is taking medications, but he
developed delirium post-operative and now he wants to discontinue his
medications ! NO; he is delirious, incompetent to change decisions, he
already consented to take the medications before he entered this delirium.
o What if this patient broke his leg; do you want to operate him without
consent? This is a new condition; we do not know what would be his
competent wishes ! look for SDM (substitute decision maker).
2011-09- Medical History.doc Page 52 of 52
Anda mungkin juga menyukai
- Hypertension Protocol PDFDokumen2 halamanHypertension Protocol PDFHitesh PednekarBelum ada peringkat
- Template Soap NeuroDokumen2 halamanTemplate Soap NeuroJohan SitepuanBelum ada peringkat
- Krisis HipertensiDokumen12 halamanKrisis HipertensiDani NurseBelum ada peringkat
- CDR Ankle Card PDFDokumen2 halamanCDR Ankle Card PDFSalsa_Picante_BabyBelum ada peringkat
- Aquifer InternalMedicine09 - 55Dokumen7 halamanAquifer InternalMedicine09 - 55JulieBelum ada peringkat
- Patient Case Presentation StructureDokumen30 halamanPatient Case Presentation StructureAmira HelayelBelum ada peringkat
- OSCE Gynae HXDokumen3 halamanOSCE Gynae HXmpage3100% (1)
- CardiologyDokumen6 halamanCardiologyFrancis FransBelum ada peringkat
- Aquifer InternalMedicine11 - 45Dokumen8 halamanAquifer InternalMedicine11 - 45JulieBelum ada peringkat
- Case Summary Pediatrics03 3-Year-ODokumen10 halamanCase Summary Pediatrics03 3-Year-OJeffBelum ada peringkat
- Hypertensive CrisisDokumen1 halamanHypertensive Crisisapi-495201002Belum ada peringkat
- OBGYN HistoryDokumen1 halamanOBGYN Historysgod34Belum ada peringkat
- Dermatologic Exam GuideDokumen3 halamanDermatologic Exam GuideJessica Febrina WuisanBelum ada peringkat
- Common Signs and SymptomsDokumen36 halamanCommon Signs and SymptomsJamil AimanBelum ada peringkat
- History and Physical Exam TemplateDokumen3 halamanHistory and Physical Exam TemplatederekcftamBelum ada peringkat
- HistoryandPhysicalExamDokumen105 halamanHistoryandPhysicalExamsilentscream0618Belum ada peringkat
- Blood Pressure Screening Form 0907Dokumen2 halamanBlood Pressure Screening Form 0907Meganne Walsh100% (2)
- Md2017 Carms Mock Interview GuideDokumen6 halamanMd2017 Carms Mock Interview GuideLizamna ReynosoBelum ada peringkat
- Diabetes and Complications: When Documenting Diabetes, It's Important To Note The FollowingDokumen2 halamanDiabetes and Complications: When Documenting Diabetes, It's Important To Note The Followingmeikaizen100% (1)
- Mo Intern Handbook - FinalDokumen37 halamanMo Intern Handbook - FinalGideon K. MutaiBelum ada peringkat
- History Taking and Physical ExaminationDokumen53 halamanHistory Taking and Physical ExaminationBoruuf If GammachuuBelum ada peringkat
- Fetal assessment overview under 40 charsDokumen3 halamanFetal assessment overview under 40 charsAde Yonata100% (1)
- ECG Interpretation DR - Rawan AlshreemDokumen25 halamanECG Interpretation DR - Rawan AlshreemMarymii Al-sahlawiiBelum ada peringkat
- History and physical assessment guideDokumen31 halamanHistory and physical assessment guideShalini RavBelum ada peringkat
- Hypertensive Emergencies in The Emergency DepartmentDokumen13 halamanHypertensive Emergencies in The Emergency DepartmentLuis Lopez RevelesBelum ada peringkat
- Newborn AssessmentDokumen9 halamanNewborn AssessmentSusmita HalderBelum ada peringkat
- Acquifer Case 2Dokumen9 halamanAcquifer Case 2Emily SymesBelum ada peringkat
- AACE ACE 2016 Postmenopausal Osteoporosis Treatment Algorithm PDFDokumen1 halamanAACE ACE 2016 Postmenopausal Osteoporosis Treatment Algorithm PDFTabs NuñezBelum ada peringkat
- 5-1 HX & Exam Handbook Final PDFDokumen23 halaman5-1 HX & Exam Handbook Final PDFPépé TechopathamBelum ada peringkat
- Acute abdomen and bone fracture conditionsDokumen50 halamanAcute abdomen and bone fracture conditionsSharaz AhmedBelum ada peringkat
- Paediatric History TakingDokumen11 halamanPaediatric History TakingIlyas SaleemBelum ada peringkat
- Components of The Comprehensive History and Pe Write UpDokumen2 halamanComponents of The Comprehensive History and Pe Write Upnewbie2kBelum ada peringkat
- GI Signs and SymptomsDokumen40 halamanGI Signs and SymptomsJohnny BeeBelum ada peringkat
- A Seminar About History TakingDokumen13 halamanA Seminar About History Takingdr_jamal1983Belum ada peringkat
- Psychiatry Chapter 3Dokumen54 halamanPsychiatry Chapter 3Online Money In EthiopiaBelum ada peringkat
- Vital Signs Reference Chart - 1Dokumen1 halamanVital Signs Reference Chart - 1l10n_assBelum ada peringkat
- General Population (No Diabetes or CKD) Diabetes or CKD PresentDokumen1 halamanGeneral Population (No Diabetes or CKD) Diabetes or CKD PresentMuthia ArsilBelum ada peringkat
- Abdominal Examination: Male - Palpate Prostate Gland Female - Feel For CervixDokumen5 halamanAbdominal Examination: Male - Palpate Prostate Gland Female - Feel For CervixRemelou Garchitorena AlfelorBelum ada peringkat
- CONNECTIVE TISSUE AND BONE SYMPOSIUM: APPROACH TO JOINT PAINDokumen7 halamanCONNECTIVE TISSUE AND BONE SYMPOSIUM: APPROACH TO JOINT PAINJeffrey FBelum ada peringkat
- Antenatal Care: Physiological Changes in PregnancyDokumen2 halamanAntenatal Care: Physiological Changes in PregnancyAlexander Ennes100% (1)
- Gynecology and ObstetricsvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvDokumen133 halamanGynecology and ObstetricsvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvȚurcan IurieBelum ada peringkat
- History Taking: DR - Ahmed Gaber Ass. Prof of Neurology Ain Shams UniversityDokumen81 halamanHistory Taking: DR - Ahmed Gaber Ass. Prof of Neurology Ain Shams UniversityKhaled OssamaBelum ada peringkat
- Obstetrics History Taking in and Examination PowerpointDokumen15 halamanObstetrics History Taking in and Examination Powerpointياسر كوثر هانيBelum ada peringkat
- Pediatrics 04: 8-Year-Old Male Well-Child Check: Learning ObjectivesDokumen8 halamanPediatrics 04: 8-Year-Old Male Well-Child Check: Learning ObjectivesJeffBelum ada peringkat
- The 12-Lead EKG: A Step-by-Step GuideDokumen31 halamanThe 12-Lead EKG: A Step-by-Step GuideJay JiangBelum ada peringkat
- Skill Labs, Clinical History Taking, and ExaminationDokumen84 halamanSkill Labs, Clinical History Taking, and ExaminationJoo Se HyukBelum ada peringkat
- Respirology: Dr. C. Chan and Dr. J. Granton Sonya Cook and Jolene Brady, Chapter Editors Leora Horn, Associate EditorDokumen40 halamanRespirology: Dr. C. Chan and Dr. J. Granton Sonya Cook and Jolene Brady, Chapter Editors Leora Horn, Associate EditorfeedodeedoBelum ada peringkat
- H&P OutlineDokumen5 halamanH&P Outlineginadaislu100% (1)
- Disasters and Mass Casualty Incidents: The Nuts and Bolts of Preparedness and Response to Protracted and Sudden Onset EmergenciesDari EverandDisasters and Mass Casualty Incidents: The Nuts and Bolts of Preparedness and Response to Protracted and Sudden Onset EmergenciesMauricio LynnBelum ada peringkat
- Problem-based Approach to Gastroenterology and HepatologyDari EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisBelum ada peringkat
- The Nurse Practitioner in UrologyDari EverandThe Nurse Practitioner in UrologyMichelle LajinessBelum ada peringkat
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsDari EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsBelum ada peringkat
- Osce Basil.Dokumen304 halamanOsce Basil.AsuganyadeviBala94% (18)
- Ob-Gyn Clinical Cases (From Apgo Site)Dokumen221 halamanOb-Gyn Clinical Cases (From Apgo Site)jamieBelum ada peringkat
- Physician License USA PDFDokumen27 halamanPhysician License USA PDFGurpreet CharaBelum ada peringkat
- 2011 09 PsychiatryDokumen40 halaman2011 09 PsychiatryGurpreet Chara100% (1)
- 27th Annual Resident Research Day Memo - Updated - April 3, 2017 PDFDokumen5 halaman27th Annual Resident Research Day Memo - Updated - April 3, 2017 PDFGurpreet CharaBelum ada peringkat
- AffiliationsDokumen9 halamanAffiliationsGurpreet CharaBelum ada peringkat
- Smoking SogcDokumen18 halamanSmoking SogcGurpreet CharaBelum ada peringkat
- AHTDP RTMS Resistant Depression UofCDokumen162 halamanAHTDP RTMS Resistant Depression UofCGurpreet CharaBelum ada peringkat
- Space Infection: Dr. Amit T. Suryawanshi Oral and Maxillofacial Surgeon Pune, India Contact Details: Email IDDokumen121 halamanSpace Infection: Dr. Amit T. Suryawanshi Oral and Maxillofacial Surgeon Pune, India Contact Details: Email IDBinek NeupaneBelum ada peringkat
- Leptospirosis: A Bacterial Infection Spread Through Contact With Infected AnimalsDokumen14 halamanLeptospirosis: A Bacterial Infection Spread Through Contact With Infected AnimalsNica Paredes MiravallesBelum ada peringkat
- NDA - BIO - CH 6 - DiseasesDokumen4 halamanNDA - BIO - CH 6 - Diseaseshemanth varsanBelum ada peringkat
- Over View of IAP ALSDokumen12 halamanOver View of IAP ALSMohamed RasoolBelum ada peringkat
- Viii. Pathophysiology A. Overview of The Disease HypokalemiaDokumen4 halamanViii. Pathophysiology A. Overview of The Disease HypokalemiaCleo Joyce C. CristalBelum ada peringkat
- Approach To Dementia Author Schulich School of Medicine and Dentistry Western UniversityDokumen18 halamanApproach To Dementia Author Schulich School of Medicine and Dentistry Western UniversitySHERIF ZAHERBelum ada peringkat
- Male Genital Organ DiseasesDokumen8 halamanMale Genital Organ DiseasesjokoBelum ada peringkat
- Deterior Cognitivo LeveDokumen8 halamanDeterior Cognitivo LeveIrene VegaBelum ada peringkat
- Drug Induced ThrombocytopeniaDokumen8 halamanDrug Induced ThrombocytopeniapebbyfebrianBelum ada peringkat
- Childhood StrabismusDokumen25 halamanChildhood StrabismusRYrstmBelum ada peringkat
- Combined Pulmonary Fibrosis and Emphysema - Case Report and Literature ReviewDokumen6 halamanCombined Pulmonary Fibrosis and Emphysema - Case Report and Literature ReviewAMALIAHAKIMBelum ada peringkat
- Neonatal Sespsis - Drug StudyDokumen6 halamanNeonatal Sespsis - Drug StudyAlvincent D. BinwagBelum ada peringkat
- Burgers DiseaseDokumen21 halamanBurgers DiseaseshaitabliganBelum ada peringkat
- Cefoxitin, Metronidazole, RanitidineDokumen2 halamanCefoxitin, Metronidazole, RanitidineDaryl PaglinawanBelum ada peringkat
- Iron MetabolismDokumen43 halamanIron Metabolismrabiatahir421Belum ada peringkat
- Clozapine For Treatment-Resistant Bipolar Disorder: A Systematic ReviewDokumen13 halamanClozapine For Treatment-Resistant Bipolar Disorder: A Systematic ReviewAsepDarussalamBelum ada peringkat
- Galzote, R. - Ob Paper Case 1Dokumen4 halamanGalzote, R. - Ob Paper Case 1Rock GalzoteBelum ada peringkat
- Bacterial Skin InfectionsDokumen73 halamanBacterial Skin InfectionsAnthony Bravo CortezBelum ada peringkat
- Day 2 Unicorn 1Dokumen279 halamanDay 2 Unicorn 1Gustavo A OrtegonBelum ada peringkat
- RheumatologygjjkjgvDokumen4 halamanRheumatologygjjkjgvShrayan DuttaBelum ada peringkat
- Acute Kidney Injury and Chronic Kidney DiseaseDokumen59 halamanAcute Kidney Injury and Chronic Kidney Diseasesho bartBelum ada peringkat
- How cementum forms and supports teethDokumen123 halamanHow cementum forms and supports teethanshum guptaBelum ada peringkat
- Endocrine Review, Kuliah Mei 2008Dokumen47 halamanEndocrine Review, Kuliah Mei 2008nurliah armandBelum ada peringkat
- Non-Healing Ulcer Caused by ToxoplasmosisDokumen6 halamanNon-Healing Ulcer Caused by ToxoplasmosisSophia RubiaBelum ada peringkat
- 1,000 Questions To Help You Pass The Emergency Medicine BoardsDokumen338 halaman1,000 Questions To Help You Pass The Emergency Medicine Boardsduvayozare100% (1)
- MCQs LADokumen29 halamanMCQs LAPadmavathi C100% (1)
- Status and indication of drugsDokumen4 halamanStatus and indication of drugsWarapong LerdliangchaiBelum ada peringkat
- Tips by Masters of HomeopathyDokumen99 halamanTips by Masters of HomeopathyGeorge Montoya100% (3)
- CME Cyanotic Heart DiseaseDokumen38 halamanCME Cyanotic Heart DiseaseTan Zhi HongBelum ada peringkat
- ATAXIAS PTDokumen13 halamanATAXIAS PTKarunya VkBelum ada peringkat