Dying With Dignity in The Intensive Care Unit: Review Article
Diunggah oleh
RodrigoSachiFreitasJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Dying With Dignity in The Intensive Care Unit: Review Article
Diunggah oleh
RodrigoSachiFreitasHak Cipta:
Format Tersedia
The n e w e ng l a n d j o u r na l of m e dic i n e
review article
critical care medicine
Simon R. Finfer, M.D., and Jean-Louis Vincent, M.D., Ph.D., Editors
Dying with Dignity in the Intensive Care Unit
Deborah Cook, M.D., and Graeme Rocker, D.M.
T
From the Departments of Medicine, Clin- he traditional goals of intensive care are to reduce the
ical Epidemiology, and Biostatistics, Mc- morbidity and mortality associated with critical illness, maintain organ func-
Master University, Hamilton, ON (D.C.),
and the Department of Medicine, Dalhousie tion, and restore health. Despite technological advances, death in the intensive
University, Halifax, NS (G.R.) — both in care unit (ICU) remains commonplace. Death rates vary widely within and among
Canada. Address reprint requests to Dr. countries and are influenced by many factors.1 Comparative international data are lack-
Cook at the McMaster University Health
Sciences Center, Rm. 2C11, 1200 Main St. W, ing, but an estimated one in five deaths in the United States occurs in a critical care bed.2
Hamilton, ON, Canada, L8N 3Z5, or at In this review, we address the concept of dignity for patients dying in the ICU.
debcook@mcmaster.ca. When the organ dysfunction of critical illness defies treatment, when the goals of care
N Engl J Med 2014;370:2506-14. can no longer be met, or when life support is likely to result in outcomes that are
DOI: 10.1056/NEJMra1208795 incongruent with patients’ values, ICU clinicians must ensure that patients die with
Copyright © 2014 Massachusetts Medical Society.
dignity. The definition of “dying with dignity” recognizes the intrinsic, unconditional
quality of human worth but also external qualities of physical comfort, autonomy,
meaningfulness, preparedness, and interpersonal connection.3 Respect should be
fostered by being mindful of the “ABCDs” of dignity-conserving care (attitudes,
behaviors, compassion, and dialogue)4 (Table 1). Preserving the dignity of patients,
avoiding harm, and preventing or resolving conflict are conditions of the privilege
and responsibility of caring for patients at the end of life. In our discussion of prin-
ciples, evidence, and practices, we assume that there are no extant conflicts between
the ICU team and the patient’s family. Given the scope of this review, readers are
referred elsewhere for guidance on conflict prevention and resolution in the ICU.5,6
The concept of dying with dignity in the ICU implies that although clinicians
may forgo some treatments, care can be enhanced as death approaches. Funda-
mental to maintaining dignity is the need to understand a patient’s unique per-
spectives on what gives life meaning in a setting replete with depersonalizing
devices. The goal is caring for patients in a manner that is consistent with their
values at a time of incomparable vulnerability, when they rarely can speak for
themselves.7 For example, patients who value meaningful relationships may de-
cline life-prolonging measures when such relationships are no longer possible.
Conversely, patients for whom physical autonomy is not crucial may accept tech-
nological dependence if it confers a reasonable chance of an acceptable, albeit
impaired, outcome.8 At issue is what each patient would be willing to undergo for
a given probability of survival and anticipated quality of life.
On the Need for Pa l l i at i v e C a r e
The coexistence of palliative care and critical care may seem paradoxical in the
technological ICU. However, contemporary critical care should be as concerned
with palliation as with the prevention, diagnosis, monitoring, and treatment of life-
threatening conditions.
2506 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org by The NEJM iPad Edition on June 25, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
critical care medicine
The World Health Organization defines pal-
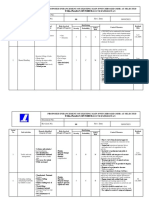
Table 1. Examples of the ABCDs of Dignity-Conserving Care.*
liative care as “an approach that improves the
quality of life of patients and their families Attitudes and assumptions can affect practice.
facing the problems associated with life-threat- Reflect on how your own life experiences affect the way in which you
ening illness, through the prevention and relief provide care.
of suffering by means of early identification Be aware that other clinicians’ attitudes and assumptions can affect their
and impeccable assessment and treatment of approach to patients.
pain and other problems, physical, psychosocial Teach learners to be mindful of how their perspectives and presumptions
can shape behaviors.
and spiritual.”9 Palliative care, which is essen-
tial regardless of whether a medical condition Behaviors should always enhance patient dignity.
is acute or chronic and whether it is in an early Demonstrate with nonverbal methods how patients and their families are
or a late stage, can also extend beyond the pa- important to you.
tient’s death to bereaved family members10 Do not rush; sit down and make eye contact when talking with patients
and their families.
(Fig. 1).
Turn off digital devices and avoid jargon when talking with patients and
their families.
El ici t ing the Va lue s of Pat ien t s
Compassion is sensitivity to the suffering of another and the desire to
relieve it.
Sometimes it is too late. A precipitating event
Elicit the personal stories that accompany your patient’s illness.
prompting an ICU admission that occurs within
a protracted downward trajectory of an illness Acknowledge the effect of sickness on your patient’s broader life
experience.
may be irreversible. When clinicians who are car-
Recognize and relieve suffering.
ing for a patient in such a scenario have not pre-
viously explored whether the patient would want Dialogue should acknowledge personhood beyond the illness.
to receive basic or advanced life support, the Explore the values that are most important to your patients.
wishes of the patient are unknown, and invalid Ask who else should be involved to help your patients through difficult
assumptions can be anticipated. Effective ad- times.
vance care planning, which is often lacking in Encourage patients and their families to reflect and reminisce.
such circumstances, elicits values directly from
* This approach is adapted from Chochinov.4
the patient, possibly preventing unnecessary suf-
fering associated with the use of unwelcome in-
terventions and thereby preserving the patient’s rative from patients (or more commonly, from
dignity at the end of life. family members) about relationships, activities,
Regardless of the rate and pattern of decline and experiences treasured by the patient. The
in health, by the time that patients are in the use of engaging, deferential questions, such as
ICU, most cannot hold a meaningful conversa- “Tell me about your . . .” or “Tell us what is im-
tion as a result of their critical condition or portant to . . . ,” is essential. Clinician guidance
sedating medications. In such cases, family for constructing an authentic picture of the in-
members or other surrogates typically speak capacitated patient’s values is offered in the Fa-
for them. In decisions regarding the withdraw- cilitated Values History,8 a framework that pro-
al of life support, the predominant determi- vides clinicians with strategies for expressing
nants are a very low probability of survival, a empathy, sensitively depicting common scenarios
very high probability of severely impaired cog- of death, clarifying the decision-making role of
nitive function, and recognition that patients surrogates, eliciting and summarizing values most
would not want to continue life support in such relevant to medical decision making, and link-
circumstances if they could speak for them- ing these values explicitly to care plans.
selves.11 Probabilistic information is thus often
more important than the patient’s age, coexist- C om munic at ion
ing medical conditions, or illness severity in
influencing decisions about life-support with- Before a critical illness develops, patients’ percep-
drawal. tions about what matters most for high-quality
Discussions can be initiated by eliciting a nar- end-of-life care vary, but human connections are
n engl j med 370;26 nejm.org june 26, 2014 2507
The New England Journal of Medicine
Downloaded from nejm.org by The NEJM iPad Edition on June 25, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
mation but assumes the primary responsibility
for decision making. At the other end of the con-
tinuum, the patient makes the decisions, and the
Intensity of Care
Curative care physician has an advisory role. In North America
and in some parts of Europe,17 the archetype is
Palliative care
the shared decision-making model, in which phy-
sicians and patients or their surrogates share in-
formation with one another and participate jointly
in decision making.18
Bereavement
Admission Time
Although preferences for decision-making roles
Death
to ICU vary among family members,19 physicians do not
always clarify family preferences.20 Family mem-
Figure 1. Curative and Palliative Approaches to Care throughout a Critical Illness.
bers may lack confidence about their surrogate
This diagram, which is adapted from a policy statement of the American
decision-maker role, regardless of the decision-
Thoracic Society,10 illustrates the relative intensity of curative and palliative
approaches to the care of patients at different stages of a critical illness. making model, if they have had no experience
In the palliative care model, the intensity of care increases at the end of life, as a surrogate or no prior dialogue with the
and support of the patient’s family continues beyond the patient’s death. patient about treatment preferences.21 Decision-
making burden is postulated as a salient source
of strain among family members of patients
key. Many seriously ill elderly patients cite effec- who are dying in the ICU; anxiety and depres-
tive communication, continuity of care, trust in sion are also prevalent.22,23
the treating physician, life completion, and avoid-
ance of unwanted life support.12 After critical ill- Prov iding Pro gnos t ic
ness develops, most patients or their surrogates Infor m at ion
find themselves communicating with unfamiliar
clinicians in a sterile environment at a time of Valid prognostic information is a fundamental
unparalleled distress. Challenges in communica- component of end-of-life discussions. Under-
tion are magnified when patients die at an early standing the predicted outcome of the critical
stage of critical illness, before rapport has been illness and recognizing the uncertainty of that
well established. prediction are helpful in making decisions that
Clear, candid communication is a determinant reflect the patient’s values. However, when it
of family satisfaction with end-of-life care.13 comes to prognosticating for seriously ill pa-
Notably, measures of family satisfaction with tients, families and physicians sometimes dis-
respect to communication are higher among agree.24 In one study, surrogate decision mak-
family members of patients who die in the ICU ers for 169 patients in the ICU were randomly
than among those of ICU patients who survive, assigned to view one of two videos of a simu-
perhaps reflecting the intensity of communica- lated family conference about a hypothetical
tion and the accompanying respect and compas- patient.25 The videos varied only according to
sion shown by clinicians for the families of dying whether the prognosis was conveyed in numeri-
patients.14 The power of effective communica- cal terms (“10% chance of survival”) or qualita-
tion also includes the power of silence.15 Family tive terms (“very unlikely to survive”). Numeri-
satisfaction with meetings about end-of-life care cal prognostic statements were no better than
in the ICU may be greater when physicians talk qualitative statements in conveying the progno-
less and listen more.16 sis. However, on average, surrogates estimated
twice as often as physicians that the patient
Decision M a k ing would survive.
In another study, when 80 surrogates of pa-
Decision-making models for the ICU vary inter- tients in the ICU interpreted 16 prognostic state-
nationally but should be individualized. At one ments, interviews suggested an “optimism bias,”
end of the continuum is a traditional parental in which the surrogates were likely to interpret
approach, in which the physician shares infor- the physicians’ grim prognostication as positive
2508 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org by The NEJM iPad Edition on June 25, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
critical care medicine
with respect to the patient’s condition.26 Clini- Prov iding Hol is t ic C a r e
cians should recognize that family members
who are acting as spokespersons for patients in Cultivating culturally and spiritually sensitive
the ICU are often “living with dying” as they care is central to the palliative approach. The pil-
face uncertainty while maintaining hope.27 Hope lars of both verbal and nonverbal communica-
should be respected during prognostic disclo- tion are crucial. Conscious nonverbal communi-
sure28 while a realistic view is maintained, an cation is rarely practiced yet can be as powerful
attitude that is aptly expressed by the simple but as verbal communication during end-of-life de
profound notion of “hoping for the best but pre- cision making. Physicians should be aware of
paring for the worst.”29 the cultural landscape reflecting an institution’s
catchment area, how cultural norms can influ-
M a k ing R ec om mendat ions ence admissible dialogue, and what is desirable
versus dishonoring in the dying process.33
Physicians in the ICU sometimes make recommen- The meaning assigned to critical illness, par-
dations to forgo the use of life-support technology. ticularly when death looms, is frequently inter-
In one study involving surrogates of 169 critically preted through a spiritual lens. For many people,
ill patients, 56% preferred to receive a physician’s critical illness triggers existential questions about
recommendation on the use of life support, 42% purpose (of life, death, and suffering), relation-
preferred not to receive such a recommendation, ships (past, present, and future), and destiny.
and 2% stated that either approach was accept- Clinicians should be able to pose questions about
able.30 A recent survey of ICU physicians showed spiritual beliefs that may bear on experiences
that although more than 90% were comfortable with respect to illness. Introductory queries can
making such recommendations and viewed them open doors, such as “Many people have beliefs
as appropriate, only 20% reported always providing that shape their lives and are important at times
recommendations to surrogates, and 10% reported like this. Is there anything that you would like
rarely or never doing so.31 In this study, delivering me to know?”34 A useful mnemonic for obtain-
such recommendations was associated with per- ing ancillary details is SPIRIT, which encom-
ceptions about the surrogate’s desire for, and agree- passes acknowledgment of a spiritual belief
ment with, the physician’s recommendations. system, the patient’s personal involvement with
Other potential influences are uncertainty, per- this system, integration with a spiritual commu-
sonal values, and litigation concerns. nity, ritualized practices and restrictions, impli-
Asking families about their desire for recom- cations for medical care, and terminal-events
mendations from physicians can be a starting planning 34 (Table 2).
point for shared deliberations about care plans.32 Although it is unrealistic to expect that clini-
Eliciting preferences for how patients or their cians will be familiar with the views of all the
families wish to receive information, particularly world religions regarding death, they should be
recommendations concerning life support, is not cognizant of how belief systems influence end-
an abnegation of responsibility but rather an ap- of-life care.35 Physicians may recommend differ-
proach that is likely to engender trust. Physi- ent approaches to similar situations, depending
cians should judiciously analyze each situation on their religious and cultural backgrounds, as
and align their language and approach with the has been self-reported36 and documented in ob-
preferred decision-making model, understand in- servational studies.37 Insensitivity to faith-based
terpersonal relationships, and avoid overempha- preferences for discussion and decision making
sizing a particular point of view. For example, in may amplify the pain and suffering of both pa-
the shared decision-making model of care for tients and their families. Clinicians should un-
dying patients, family discussions typically include derstand how spirituality can influence coping,
a review of the patient’s previous and present either positively or negatively.38 Chaplains are
status and prognosis, elicitation of the patient’s indispensable for addressing and processing
values, presentation of the physician’s recommen- existential distress, conducting life review, and
dations, deliberations, and joint decision making facilitating comforting prayers, rituals, or other
about ongoing levels of care. observances.
n engl j med 370;26 nejm.org june 26, 2014 2509
The New England Journal of Medicine
Downloaded from nejm.org by The NEJM iPad Edition on June 25, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
delay death so that the patient can accomplish
Table 2. Taking a Spiritual History.*
short-term life goals.41 Whatever approach is used,
S for spiritual belief system individualized pharmacologic therapy, which de-
P for personal spirituality pends on prevailing levels of analgesia and seda-
I for integration with a spiritual community tion at the time of decisions to forgo life sup-
R for ritualized practices and restrictions
port, should ensure preemptive, timely alleviation
of dyspnea, anxiety, pain, and other distressing
I for implications for medical care
symptoms.42 Clinicians can mitigate the stress of
T for terminal-events planning family members by discussing what is likely to
* This approach is adapted from Maugans.34 The mnemonic
happen during the dying process (e.g., unusual
SPIRIT can be used to elicit a spiritual history from a patient sounds, changes in skin color, and agonal breath-
as part of the goal of providing sensitive, compassionate ing). Physician attendance is paramount to re-
end-of-life care.
evaluate the patient’s comfort and talk with the
family as needed (Table 4).
The Fina l S teps
C onsequence s for Cl inici a ns
If a shift is made in the goals of care from cure
to comfort, it should be orchestrated with grace Dying patients and their families in the ICU are
and should be individualized to the needs of the not alone in their suffering. For some clinicians,
patient.39 Before proceeding with end-of-life views about the suitability of advanced life sup-
measures, it is necessary to prepare staff mem- port that diverge from those of the patient or
bers and the patient’s room, as well as the pa- family can be a source of moral distress. Clini-
tient (Table 3). The panoply of basic and ad- cians who detect physical or psychic pain and
vanced life-support equipment and the other negative symptoms may suffer indirectly,
mechanics of their deployment or discontinua- yet deeply. Vicarious traumatization results from
tion are chronicled in multiple studies, as well repeated empathic engagement with sadness and
as in discussion documents, consensus state- loss,43 particularly when predisposing character-
ments from professional organizations, and istics amplify clinicians’ response to this work-
task-force reports.10,17,32,40 Strategies should be place stress. Clinicians should be aware of how
openly discussed and informed by the same bal- their emotional withdrawal or lability and “com-
ance of benefits, burdens, and respect for the passion fatigue” can jeopardize the care of dying
preferences of patients and their surrogates that patients and their families.
apply to other aspects of end-of-life care.10 Informal debriefing or case-based rounds,44
There is no single, universally accepted tech- local meetings with other professionals, modi-
nical approach. Admissible strategies in most set- fied work assignments, and other strategies may
tings include variations and combinations of non- help clinicians to cope with the distress.45 Formal
escalation of current interventions, withholding of bereavement counseling that is designed espe-
future interventions, and withdrawal of some or cially for involved clinicians can enhance aware-
all interventions, except those needed for com- ness about vicarious traumatization and encour-
fort. When life-support measures are withdrawn, age adaptive personal and professional coping
the process of withdrawal — immediate or grad- strategies.
ual discontinuation — must be considered care-
fully. Mechanical ventilation is the most com-
End - of-L ife C a r e a s a
mon life-support measure that is withdrawn.11 Qua l i t y-Improv emen t Ta rge t
However, even in the case of mechanical ventila-
tion, legal or faith-based requirements, societal Palliative care is now a mainstream matter for
norms, and physician preferences influence de- quality-improvement agendas in many ICUs. A de-
cisions about withdrawal.32 The initiation of non cade ago, the Robert Wood Johnson Foundation
invasive ventilation with clear objectives for pa- Critical Care End-of-Life Peer Workgroup and
tients who are not already undergoing mechanical 15 associated nurse–physician teams in North
ventilation can sometimes reduce dyspnea and America conducted a review of reported practices
2510 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org by The NEJM iPad Edition on June 25, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
critical care medicine
Table 3. Practical Preparatory Procedures to Ensure Patient Dignity before Withdrawal of Life Support.
Prepare staff members
Review the planned procedures in detail with all relevant staff members.
Ensure that the referring physician is aware of the plans, if not already engaged.
Ensure that spiritual care services are offered, if not already engaged.
Remind staff members that all their actions should ensure the dignity of the patient.
Remind staff members that the patient and family are the unit of care.
Prepare a staffing schedule to maximize the continuity of care during the dying process, if possible.
Ensure that the bedside nurse has not been assigned to care for another acutely ill patient, if possible.
Ensure that the bedside nurse is experienced in palliative care; if not, change the assignment or arrange for
supervision to be provided by a nurse experienced in palliative care.
Ensure that physicians are readily available and do not abandon the patient or family.
Introduce the relevant housestaff members to the patient and family.
Introduce the respiratory therapist to the patient and family, when applicable.
Ensure that staff members minimize unnecessary noise immediately outside the room.
Prepare the patient’s room
Consider the comfort of the patient and family (e.g., lighting, temperature, personal items).
Liberalize visiting restrictions (e.g., timing, duration, number of visitors).
Remove unnecessary equipment.
Bring additional chairs into the room, if necessary.
Secure a quiet room for the family away from the bedside.
Prepare the patient
Position the patient as comfortably as possible.
Honor requests for cultural, spiritual, and religious rituals.
Dim the lighting on screens required for monitoring (e.g., electrocardiography).
Discontinue unnecessary monitoring (e.g., oximetry), unnecessary devices (e.g., feeding tubes), unnecessary tests
(e.g., blood work), and unnecessary treatments (e.g., enteral nutrition).
Discontinue medications that do not provide comfort and provide those that do.
Ensure that the patient is as calm and distress-free as possible before proceeding to withdraw life support.
for end-of-life care and named seven key domains conflicts, ethics consultations helped with con-
for quality improvement: patient- and family- flict resolution and reduced the duration of non-
centered decision making, communication, con- beneficial treatments that the patients received.48
tinuity of care, emotional and practical support, In a subsequent cluster-randomized trial involv-
symptom management, spiritual support, and ing 2318 patients in which investigators evaluat-
emotional and organizational support for ICU ed a five-component, clinician-focused end-of-life
clinicians.46 More than 100 potential interven- strategy,49 there were no significant differences
tions were identified as part of this project, di- between groups with respect to family satisfac-
rected at patients and their families, clinicians, tion with care, family or nurse ratings of the
ICUs, and health care systems. Candidate quality quality of dying, time to withdrawal of mechani-
indicators and “bundled indicators” can facili- cal ventilation, length of stay in the ICU, or other
tate measurement and performance feedback in palliative care indicators.
evaluating the quality of palliative care in ICU Favorable assessments of palliative care inter-
settings.47 ventions in the ICU are beginning to emerge. In
In a multicenter, randomized trial involving one study, family members of 126 dying patients
critically ill patients who were facing value-related in 22 ICUs were randomly assigned to participate
n engl j med 370;26 nejm.org june 26, 2014 2511
The New England Journal of Medicine
Downloaded from nejm.org by The NEJM iPad Edition on June 25, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 4. Considerations and Cautions in the Withdrawal of Life Support.*
Variable Considerations Cautions
Discontinuation of renal-replace- Confers a low risk of physical distress Death may take several days if this is
ment therapy the only advanced life support
withdrawn
Discontinuation of inotropes Confers no risk of physical distress Death may not occur quickly if the pa-
or vasopressors Death may occur quickly if the patient tient requires low doses, particular-
requires high doses, with or with- ly if mechanical ventilation is
out withdrawal of mechanical ven- ongoing
tilation
Weaning from inotropes Confers no risk of physical distress May prolong the dying process, partic-
or vasopressors ularly if the patient requires low
doses and this is the only life sup-
port withdrawn
Discontinuation of mechanical Confers risk of dyspnea Preemptive sedation is typically need-
ventilation Death may occur quickly if the patient ed to blunt air hunger due to rapid
requires high pressure settings or changes in mechanical ventilation
high oxygen levels Death may not occur quickly if the pa-
tient requires low pressure settings
or low oxygen levels
Weaning from mechanical Confers low risk of dyspnea May prolong the dying process, partic-
ventilation ularly if the patient requires low
pressure settings or low oxygen
levels and this is the only life sup-
port withdrawn
Extubation Confers risk of dyspnea Informing families about possible
Avoids discomfort and suctioning physical signs after extubation can
of endotracheal tube prepare and reassure them
Can facilitate oral communication Secretions may cause noisy breathing,
Allows for the most natural which may be reduced with the use
appearance of glycopyrrolate; the use of gluco-
corticoids may reduce stridor
Airway obstruction may occur; jaw
thrust or repositioning of the pa-
tient may help
Not advised if the patient has hemop-
tysis
* The choice regarding the type and dose of medications depends on prevailing levels of analgesia and sedation at the
time of the decision, the mode and sequence of the planned withholding or withdrawal of life support, and myriad other
factors.42 These factors preclude any specific dose recommendations. Physician availability for the family during the dy-
ing process is as important as individualized adjustment of medication.
in a standard end-of-life family conference or to were assigned to the standard-conference group,
participate in a proactive family conference and re with no significant between-group difference in
ceive a brochure on bereavement.50 The mnemonic the length of stay in the ICU or the hospital.
“VALUE” framed the five objectives of the pro Caregivers in the proactive-conference group, as
active family conference: value and appreciate compared with the standard-conference group,
what family members say, acknowledge the fam- were less negatively affected by the experience
ily members’ emotions, listen to their concerns, and were less likely to have anxiety, depression,
understand who the patient was in active life by and symptoms of post-traumatic stress 90 days
asking questions, and elicit questions from the after the patients’ deaths.
family members. Patients whose family mem-
bers were assigned to the proactive-conference C onclusions
group were treated with significantly fewer non-
beneficial interventions after the family confer- Palliative care in the ICU has come of age. Its
ence than were those whose family members guiding principles are more important than ever
2512 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org by The NEJM iPad Edition on June 25, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
critical care medicine
in increasingly pluralistic societies. Ensuring port the bereaved family members. Ensuring death
that patients are helped to die with dignity begs with dignity in the ICU epitomizes the art of med-
for reflection, time, and space to create connec- icine and reflects the heart of medicine. It de-
tions that are remembered by survivors long after mands the best of us.
a patient’s death. It calls for humanism from all No potential conflict of interest relevant to this article was
reported.
clinicians in the ICU to promote peace during the Disclosure forms provided by the authors are available with
final hours or days of a patient’s life and to sup- the full text of this article at NEJM.org.
References
1. Adhikari NK, Fowler RA, Bhagwanjee 14. Wall RJ, Curtis JR, Cooke CR, Engel- methods to disclose prognosis to surro-
S, Rubenfeld GD. Critical care and the berg RA. Family satisfaction in the ICU: gate decision makers in intensive care
global burden of critical illness in adults. differences between families of survivors units. Am J Respir Crit Care Med 2010;
Lancet 2010;376:1339-46. and nonsurvivors. Chest 2007;132:1425- 182:905-9.
2. Angus DC, Barnato AE, Linde-Zwirble 33. 26. Zier LS, Sottile PD, Hong SY, Weiss-
WT, et al. Use of intensive care at the end 15. Lilly CM, Daly BJ. The healing power field LA, White DB. Surrogate decision
of life in the United States: an epidemio- of listening in the ICU. N Engl J Med 2007; makers’ interpretation of prognostic in-
logic study. Crit Care Med 2004;32:638- 356:513-5. formation: a mixed-methods study. Ann
43. 16. McDonagh JR, Elliott TB, Engelberg Intern Med 2012;156:360-6.
3. Proulx K, Jacelon C. Dying with dignity: RA, et al. Family satisfaction with family 27. Sinuff T, Giacomini M, Shaw R, Swin-
the good patient versus the good death. Am conferences about end-of-life care in the ton M, Cook DJ. “Living with dying”: the
J Hosp Palliat Care 2004;21:116-20. intensive care unit: increased proportion evolution of family members’ experience
4. Chochinov HM. Dignity and the es- of family speech is associated with in- of mechanical ventilation. Crit Care Med
sence of medicine: the A, B, C, and D of creased satisfaction. Crit Care Med 2004; 2009;37:154-8.
dignity conserving care. BMJ 2007;335: 32:1484-8. 28. Simpson C. When hope makes us vul-
184-7. 17. Carlet J, Thijs LG, Antonelli M, et al. nerable: a discussion of patient-healthcare
5. Prendergast TJ. Conflicts, negotiations Challenges in end-of-life care in the ICU: provider interactions in the context of
and resolution: a primer. In: Rocker G, statement of the 5th International Con- hope. Bioethics 2004;18:428-47.
Puntillo K, Azoulay E, Nelson J, eds. End sensus Conference in Critical Care: Brus- 29. Back AL, Arnold RM, Quill TE. Hope
of life care in the ICU: from advanced dis- sels, Belgium, April 2003. Intensive Care for the best, and prepare for the worst.
ease to bereavement. Oxford, England: Med 2004;30:770-84. Ann Intern Med 2003;138:439-43.
Oxford University Press, 2010:202-8. 18. Charles C, Whelan T, Gafni A. What 30. White DB, Evans LR, Bautista CA,
6. Choong K, Cupido C, Nelson E, et al. do we mean by partnership in making de- Luce JM, Lo B. Are physicians’ recommen-
ACCADEMY: a framework for resolving cisions about treatment? BMJ 1999;319: dations to limit life support beneficial or
disagreement during end of life care in the 780-2. burdensome? Bringing empirical data to
critical care unit. Clin Invest Med 2010; 19. Heyland DK, Cook DJ, Rocker GM, et the debate. Am J Respir Crit Care Med
33:E240-E253. al. Decision-making in the ICU: perspec- 2009;180:320-5.
7. Drazen JM. Decisions at the end of tives of the substitute decision-maker. 31. Brush DR, Rasinski KA, Hall JB, Alex-
life. N Engl J Med 2003;349:1109-10. Intensive Care Med 2003;29:75-82. ander GC. Recommendations to limit life
8. Scheunemann LP, Arnold RM, White 20. White DB, Braddock CH III, Bereknyei support: a national survey of critical care
DB. The facilitated values history: helping S, Curtis JR. Toward shared decision physicians. Am J Respir Crit Care Med
surrogates make authentic decisions for making at the end of life in intensive care 2012;186:633-9.
incapacitated patients with advanced ill- units: opportunities for improvement. 32. Truog RD, Campbell ML, Curtis JR, et
ness. Am J Respir Crit Care Med 2012;186: Arch Intern Med 2007;167:461-7. al. Recommendations for end-of-life care in
480-6. 21. Majesko A, Hong SY, Weissfeld L, the intensive care unit: a consensus state-
9. World Health Organization. WHO defi- White DB. Identifying family members ment by the American College [corrected]
nition of palliative care (http://www.who.int/ who may struggle in the role of surrogate of Critical Care Medicine. Crit Care Med
cancer/palliative/definition/en/). decision maker. Crit Care Med 2012;40: 2008;36:953-63.
10. Lanken PN, Terry PB, Delisser HM, et 2281-6. 33. Bowman K. Cultural issues and palli-
al. An official American Thoracic Society 22. Azoulay E, Pochard F, Kentish-Barnes ative care in the ICU. In: Rocker G, Pun-
clinical policy statement: palliative care N, et al. Risk of post-traumatic stress tillo K, Azoulay E, Nelson J, eds. End of
for patients with respiratory diseases and symptoms in family members of intensive life care in the intensive care unit: from
critical illnesses. Am J Respir Crit Care care unit patients. Am J Respir Crit Care advanced disease to bereavement. Oxford,
Med 2008;177:912-27. Med 2005;171:987-94. England: Oxford University Press, 2010.
11. Cook D, Rocker G, Marshall J, et al. 23. Pochard F, Darmon MI, Fassier T, et 34. Maugans TA. The SPIRITual history.
Withdrawal of mechanical ventilation in al. Symptoms of anxiety and depression Arch Fam Med 1996;5:11-6.
anticipation of death in the intensive care in family members of intensive care unit 35. Bülow HH, Sprung CL, Reinhart K,
unit. N Engl J Med 2003;349:1123-32. patients before discharge or death: a pro- et al. The world’s major religions’ points
12. Heyland DK, Dodek P, Rocker G, et al. spective multicenter study. J Crit Care 2005; of view on end-of-life decisions in the in-
What matters most in end-of-life care: per- 20:90-6. tensive care unit. Intensive Care Med
ceptions of seriously ill patients and their 24. Cox CE, Martinu T, Sathy SJ, et al. Ex- 2008;34:423-30.
family members. CMAJ 2006;174:627-33. pectations and outcomes of prolonged 36. Vincent JL. Forgoing life support in
13. Heyland DK, Rocker GM, Dodek PM, mechanical ventilation. Crit Care Med western European intensive care units:
et al. Family satisfaction with care in the 2009;37:2888-94, quiz 2904. the results of an ethical questionnaire.
intensive care unit: results of a multiple 25. Lee Char SJ, Evans LR, Malvar GL, Crit Care Med 1999;27:1626-33.
center study. Crit Care Med 2002;30:1413-8. White DB. A randomized trial of two 37. Sprung CL, Cohen SL, Sjokvist P, et al.
n engl j med 370;26 nejm.org june 26, 2014 2513
The New England Journal of Medicine
Downloaded from nejm.org by The NEJM iPad Edition on June 25, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
critical care medicine
End-of-life practices in European inten- 42. Kompanje EJO, van der Hoven B, Pronovost PJ. Improving comfort and
sive care units: the Ethicus Study. JAMA akker J. Anticipation of distress after
B communication in the ICU: a practical
2003;290:790-7. discontinuation of mechanical ventilation new tool for palliative care performance
38. Sulmasy DP. Spirituality, religion, and in the ICU at the end of life. Intensive measurement and feedback. Qual Saf
clinical care. Chest 2009;135:1634-42. Care Med 2008;34:1593-9. Health Care 2006;15:264-71.
39. Cook DJ, Giacomini M, Johnson N, 43. Kuhl D. What dying people want: 48. Schneiderman LJ, Gilmer T, Teetzel HD,
Willms D. Life support in the intensive practical wisdom for the end of life. New et al. Effect of ethics consultations on non-
care unit: a qualitative investigation of York: PublicAffairs, 2002. beneficial life-sustaining treatments in the
technological purposes. CMAJ 1999;161: 44. Hough CL, Hudson LD, Salud A, Lahey intensive care setting: a randomized con-
1109-13. T, Curtis JR. Death rounds: end-of-life dis- trolled trial. JAMA 2003;290:1166-72.
40. Davidson JE, Powers K, Hedayat KM, cussions among medical residents in the 49. Curtis JR, Nielsen EL, Treece PD, et al.
et al. Clinical practice guidelines for sup- intensive care unit. J Crit Care 2005;20:20-5. Effect of a quality-improvement interven-
port of the family in the patient-centered 45. Nelson JE, Angus DC, Weissfeld LA, tion on end-of-life care in the intensive
intensive care unit: American College of et al. End-of-life care for the critically ill: care unit: a randomized trial. Am J Respir
Critical Care Medicine Task Force 2004- a national intensive care unit survey. Crit Crit Care Med 2011;183:348-55.
2005. Crit Care Med 2007;35:605-22. Care Med 2006;34:2547-53. 50. Lautrette A, Darmon M, Megarbane
41. Curtis JR, Cook DJ, Sinuff T, et al. 46. Clarke EB, Curtis JR, Luce JM, et al. B, et al. A communication strategy and
Noninvasive positive pressure ventilation Quality indicators for end-of-life care in brochure for relatives of patients dying in
in critical and palliative care settings: un- the intensive care unit. Crit Care Med the ICU. N Engl J Med 2007;356:469-78.
derstanding the goals of therapy. Crit 2003;31:2255-62. [Erratum, N Engl J Med 2007;357:203.]
Care Med 2007;35:932-9. 47. Nelson JE, Mulkerin CM, Adams LL, Copyright © 2014 Massachusetts Medical Society.
2514 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org by The NEJM iPad Edition on June 25, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Anda mungkin juga menyukai
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Worksheet Modul 6 - Food and Beverage DivisiondDokumen10 halamanWorksheet Modul 6 - Food and Beverage DivisiondIAN WIDJAYABelum ada peringkat
- Review of Related Literature of Jackfruit SeedDokumen4 halamanReview of Related Literature of Jackfruit SeedPrince Martin John Villamor80% (5)
- I Hi Psychology of Change Framework White PaperDokumen32 halamanI Hi Psychology of Change Framework White PaperMELISABelum ada peringkat
- TRALEG KYABGON - The-Influence-of-Yogacara-on-Mahamudra PDFDokumen145 halamanTRALEG KYABGON - The-Influence-of-Yogacara-on-Mahamudra PDFFilippo Lunardo100% (1)
- Surge Arrester Function and Working PrinciplesDokumen25 halamanSurge Arrester Function and Working PrinciplesMidhun Varghese100% (1)
- Instructional Design HypertensionDokumen8 halamanInstructional Design HypertensionGeoffrey OnyanchaBelum ada peringkat
- What Is Learning Anyway? A Topographical Perspective ConsideredDokumen18 halamanWhat Is Learning Anyway? A Topographical Perspective ConsideredCristian SalazarBelum ada peringkat
- Lake Lanao Policy StudyDokumen30 halamanLake Lanao Policy StudyGodfrey MordenoBelum ada peringkat
- Medical Marijuana Is The Cart Before The Horse?Dokumen2 halamanMedical Marijuana Is The Cart Before The Horse?RodrigoSachiFreitasBelum ada peringkat
- Potential Clinical Benefits of CBD-Rich Cannabis Extracts Over Purified CBD in Treatment-Resistant Epilepsy - Observational Data Meta-AnalysisDokumen9 halamanPotential Clinical Benefits of CBD-Rich Cannabis Extracts Over Purified CBD in Treatment-Resistant Epilepsy - Observational Data Meta-AnalysisRodrigoSachiFreitasBelum ada peringkat
- Trial of Invasive Versus Medical Therapy in Elderly Patients Wit 2001Dokumen7 halamanTrial of Invasive Versus Medical Therapy in Elderly Patients Wit 2001RodrigoSachiFreitasBelum ada peringkat
- Original Contributions: Ten Best Practices For Improving Emergency Medicine Provider-Nurse CommunicationDokumen13 halamanOriginal Contributions: Ten Best Practices For Improving Emergency Medicine Provider-Nurse CommunicationRodrigoSachiFreitasBelum ada peringkat
- Zi Elske 2014Dokumen9 halamanZi Elske 2014RodrigoSachiFreitasBelum ada peringkat
- Multidisciplinary Management of The Post-Cardiac Arrest Patient - Madder2018Dokumen17 halamanMultidisciplinary Management of The Post-Cardiac Arrest Patient - Madder2018RodrigoSachiFreitasBelum ada peringkat
- Coma Delirium Cognitive Dysfunction in Critical Illness Stevens 2007 (Apr-17-08)Dokumen18 halamanComa Delirium Cognitive Dysfunction in Critical Illness Stevens 2007 (Apr-17-08)RodrigoSachiFreitasBelum ada peringkat
- Effects of Early Exercise Rehabilitation On Functional Recovery in Patients With Severe SepsisDokumen9 halamanEffects of Early Exercise Rehabilitation On Functional Recovery in Patients With Severe SepsisRodrigoSachiFreitasBelum ada peringkat
- Significant Cognitive Dysfunction in Non-Delirious Patients Identified During and Persistent Following Critical Illness - Jones2006Dokumen4 halamanSignificant Cognitive Dysfunction in Non-Delirious Patients Identified During and Persistent Following Critical Illness - Jones2006RodrigoSachiFreitasBelum ada peringkat
- Pasternak 2018Dokumen8 halamanPasternak 2018RodrigoSachiFreitasBelum ada peringkat
- Prescott 2018Dokumen13 halamanPrescott 2018RodrigoSachiFreitasBelum ada peringkat
- Ni Hms 456737Dokumen18 halamanNi Hms 456737RodrigoSachiFreitasBelum ada peringkat
- Resilience in Survivors of Critical Illness in The Context of The Survivors' Experience and RecoveryDokumen10 halamanResilience in Survivors of Critical Illness in The Context of The Survivors' Experience and RecoveryRodrigoSachiFreitasBelum ada peringkat
- Lock Yer 2003Dokumen9 halamanLock Yer 2003RodrigoSachiFreitasBelum ada peringkat
- 1 Intensive-Care-Diaries PDFDokumen10 halaman1 Intensive-Care-Diaries PDFManish SharmaBelum ada peringkat
- Hypertensive Crisis JournalDokumen5 halamanHypertensive Crisis JournalRaena SepryanaBelum ada peringkat
- Nej MR A 1404489Dokumen11 halamanNej MR A 1404489Pablo IgnacioBelum ada peringkat
- Readmission Diagnoses after Severe SepsisDokumen5 halamanReadmission Diagnoses after Severe SepsisRodrigoSachiFreitasBelum ada peringkat
- Implementing Early Physical Rehabilitation and Mobilisation in The ICU Institutional, Clinician, and Patient Considerations - Parry2017Dokumen4 halamanImplementing Early Physical Rehabilitation and Mobilisation in The ICU Institutional, Clinician, and Patient Considerations - Parry2017RodrigoSachiFreitasBelum ada peringkat
- N Engl J Med p.429 PDFDokumen8 halamanN Engl J Med p.429 PDFRodrigoSachiFreitasBelum ada peringkat
- Inpatient Patient ExperienceDokumen12 halamanInpatient Patient ExperienceRodrigoSachiFreitasBelum ada peringkat
- Crise Hipertensiva 1Dokumen8 halamanCrise Hipertensiva 1RodrigoSachiFreitasBelum ada peringkat
- Monitoring Intensive Care Unit Performance-Impact of A Novel Individualised Performance Scorecard in Critical Care Medicine A Mixed-Methods Study ProtocolDokumen7 halamanMonitoring Intensive Care Unit Performance-Impact of A Novel Individualised Performance Scorecard in Critical Care Medicine A Mixed-Methods Study ProtocolRodrigoSachiFreitasBelum ada peringkat
- Optimising The Administration of Antibiotics in Critically Ill PatientsDokumen5 halamanOptimising The Administration of Antibiotics in Critically Ill PatientsRodrigoSachiFreitasBelum ada peringkat
- Nej MR A 1404489Dokumen11 halamanNej MR A 1404489Pablo IgnacioBelum ada peringkat
- Interpreting and Implementing The 2018 Pain, Agitation:Sedation, Delirium, Immobility, and Sleep Disruption Clinical Practice Guideline - Balas2018Dokumen7 halamanInterpreting and Implementing The 2018 Pain, Agitation:Sedation, Delirium, Immobility, and Sleep Disruption Clinical Practice Guideline - Balas2018RodrigoSachiFreitasBelum ada peringkat
- Crise Hipertensiva 2Dokumen10 halamanCrise Hipertensiva 2RodrigoSachiFreitasBelum ada peringkat
- A Clinic Model: Post-Intensive Care Syndrome and Post-Intensive Care Syndrome-FamilyDokumen8 halamanA Clinic Model: Post-Intensive Care Syndrome and Post-Intensive Care Syndrome-FamilyRodrigoSachiFreitasBelum ada peringkat
- Editorial Board 2015 Intensive and Critical Care NursingDokumen1 halamanEditorial Board 2015 Intensive and Critical Care NursingRodrigoSachiFreitasBelum ada peringkat
- Jss Academy Unit 1 BDokumen13 halamanJss Academy Unit 1 BbomtozorBelum ada peringkat
- D3.6.SmartAKIS - Recommendations Danemarca Cu SiteDokumen47 halamanD3.6.SmartAKIS - Recommendations Danemarca Cu SitebubuhomeBelum ada peringkat
- K.P.Mondal & Sons: Quality Assurance PlanDokumen1 halamanK.P.Mondal & Sons: Quality Assurance PlanTanmoy DuttaBelum ada peringkat
- Statepfofileofvidarbha PDFDokumen53 halamanStatepfofileofvidarbha PDFAditiBelum ada peringkat
- The Fundamental Building Block: The CellDokumen12 halamanThe Fundamental Building Block: The CellTanish JenaBelum ada peringkat
- Tata Group - Wikipedia, The Free EncyclopediaDokumen17 halamanTata Group - Wikipedia, The Free EncyclopediaSushil MundelBelum ada peringkat
- Ecotek DesignManual v2015 02Dokumen44 halamanEcotek DesignManual v2015 02benBelum ada peringkat
- Precious Metals AlfaDokumen83 halamanPrecious Metals AlfaPraveenBelum ada peringkat
- Anggraeni Kusuma Dewi Xii Iis Bahasa Inggris (UH 4/SOAL REPORT TEXT)Dokumen7 halamanAnggraeni Kusuma Dewi Xii Iis Bahasa Inggris (UH 4/SOAL REPORT TEXT)prabaswara xxBelum ada peringkat
- 63-2003 Local Water District Franchise and Income TaxDokumen2 halaman63-2003 Local Water District Franchise and Income Taxapi-247793055100% (1)
- ForumIAS CSAT Test 10Dokumen18 halamanForumIAS CSAT Test 10anilBelum ada peringkat
- Project Report On Employee Management SystemDokumen58 halamanProject Report On Employee Management Systemprivate69raghavBelum ada peringkat
- Ihp MicroDokumen13 halamanIhp MicroTejas HambirBelum ada peringkat
- JSA - MergeDokumen11 halamanJSA - MergeIzzuddin MustapaBelum ada peringkat
- Operation and Analysis of The Three Phase Fully Controlled Bridge ConverterDokumen24 halamanOperation and Analysis of The Three Phase Fully Controlled Bridge Convertermohammed aliBelum ada peringkat
- BC-5D Insert PDFDokumen1 halamanBC-5D Insert PDFGarcía XavierBelum ada peringkat
- 200 300 Series Installation Guide USDokumen48 halaman200 300 Series Installation Guide USLhexter Mhervin CoBelum ada peringkat
- Balzac GaitDokumen7 halamanBalzac Gaithieratic_headBelum ada peringkat
- SAP Sales Order Store Returns (Intercompany)Dokumen2 halamanSAP Sales Order Store Returns (Intercompany)Donny CorleonBelum ada peringkat
- 10TH Gseb PaperDokumen10 halaman10TH Gseb Paperkhushboo guptaBelum ada peringkat
- Ashrae Handbook 2000 CHDokumen32 halamanAshrae Handbook 2000 CHKazuto NakazatoBelum ada peringkat
- Grounding Systems and Safety Practices AnalysisDokumen29 halamanGrounding Systems and Safety Practices AnalysisFaiz MangalasseryBelum ada peringkat
- Mitsubishi: Technical Service BulletinDokumen11 halamanMitsubishi: Technical Service BulletinKonstantinBelum ada peringkat