Pill in Pocket NEJM
Diunggah oleh
n2coolohHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Pill in Pocket NEJM
Diunggah oleh
n2coolohHak Cipta:
Format Tersedia
The new england journal of medicine
original article
Outpatient Treatment of Recent-Onset
Atrial Fibrillation with the “Pill-in-the-Pocket”
Approach
Paolo Alboni, M.D., Giovanni L. Botto, M.D., Nicola Baldi, M.D., Mario Luzi, M.D.,
Vitantonio Russo, M.D., Lorella Gianfranchi, M.D., Paola Marchi, M.D.,
Massimo Calzolari, M.D., Alberto Solano, M.D., Raffaele Baroffio, M.D.,
and Germano Gaggioli, M.D.*
abstract
background
From the Divisions of Cardiology, Ospe- In-hospital administration of flecainide and propafenone in a single oral loading dose
dale Civile, Cento (P.A., L.G.); Ospedale S. has been shown to be effective and superior to placebo in terminating atrial fibrillation.
Anna, Como (G.L.B., M.L.); Ospedale SS.
Annunziata, Taranto (N.B., V.R.); Ospe- We evaluated the feasibility and the safety of self-administered oral loading of flecainide
dale del Delta, Lagosanto (P.M.); Arcisped- and propafenone in terminating atrial fibrillation of recent onset outside the hospital.
ale Santa Maria Nuova, Reggio Emilia
(M.C.); Ospedali Riuniti, Lavagna (A.S.);
Ospedale Galmarini, Tradate (R.B.); and methods
Ospedale Civile, Sampierdarena (G.G.) — We administered either flecainide or propafenone orally to restore sinus rhythm in 268
all in Italy. Address reprint requests to Dr. patients with mild heart disease or none who came to the emergency room with atrial
Alboni at the Division of Cardiology, Os-
pedale Civile, I-44042 Cento, Italy, or at fibrillation of recent onset that was hemodynamically well tolerated. Of these patients,
p.alboni@ausl.fe.it. 58 (22 percent) were excluded from the study because of treatment failure or side effects.
Out-of-hospital self-administration of flecainide or propafenone — the “pill-in-the-
*Additional study investigators are listed
in the Appendix. pocket” approach — after the onset of heart palpitations was evaluated in the remaining
210 patients (mean age [±SD], 59±11 years).
N Engl J Med 2004;351:2384-91.
Copyright © 2004 Massachusetts Medical Society.
results
During a mean follow-up of 15±5 months, 165 patients (79 percent) had a total of 618
episodes of arrhythmia; of those episodes, 569 (92 percent) were treated 36±93 minutes
after the onset of symptoms. Treatment was successful in 534 episodes (94 percent);
the time to resolution of symptoms was 113±84 minutes. Among the 165 patients with
recurrences, the drug was effective during all the arrhythmic episodes in 139 patients
(84 percent). Adverse effects were reported during one or more arrhythmic episodes by
12 patients (7 percent), including atrial flutter at a rapid ventricular rate in 1 patient and
noncardiac side effects in 11 patients. The numbers of monthly visits to the emergency
room and hospitalizations were significantly lower during follow-up than during the
year before the target episode (P<0.001 for both comparisons).
conclusions
In a selected, risk-stratified population of patients with recurrent atrial fibrillation, pill-
in-the-pocket treatment is feasible and safe, with a high rate of compliance by patients,
a low rate of adverse events, and a marked reduction in emergency room visits and hos-
pital admissions.
2384 n engl j med 351;23 www.nejm.org december 2, 2004
The New England Journal of Medicine
Downloaded from nejm.org on April 18, 2018. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
pill-in-the-pocket treatment of atrial fibrillation
room visits and hospital admissions as compared
i n patients with recurrent atrial fi-
brillation, long-term oral prophylaxis with an-
tiarrhythmic drugs has long been used to pre-
vent recurrences. However, both the need for daily
administration of antiarrhythmic agents and the
with those in the year preceding enrollment in the
study.
methods
risk of adverse effects are recognized as disadvan-
tages of long-term prophylaxis.1-5 In addition, re- study population
lapses are frequent. During the past few years, ra- The inclusion criteria were an age of 18 to 75 years,
diofrequency catheter ablation of pulmonary veins emergency room intervention for an episode of elec-
has been introduced into clinical practice.6 Howev- trocardiographically documented atrial fibrillation
er, in all studies, the procedure has been used only of recent onset (<48 hours earlier), a mean heart rate
in patients who have frequent arrhythmic episodes of more than 70 beats per minute, and a systolic
despite long-term oral prophylaxis.7 Some patients pressure of 100 mm Hg or more. Additional criteria
with recurrent atrial fibrillation may present with for inclusion in the study were a history of palpita-
episodes that are not frequent and are well tolerated tions with an abrupt onset that were hemodynami-
but that are long enough in duration that they re- cally well tolerated (i.e., without symptoms such as
quire either emergency room intervention or hospi- dyspnea, presyncope, or syncope), at least 1 but few-
talization. er than 12 episodes of atrial fibrillation (excluding
Oral prophylaxis or catheter ablation may not be the target episode) in the previous year, and no car-
the most appropriate first-line treatment for such diac symptoms apart from the episodes of ar-
patients. An alternative treatment is the “pill-in-the- rhythmia.
pocket” approach, in which the patient takes a sin- Patients were excluded if they had one or more
gle oral dose of an antiarrhythmic drug at the time of the following findings: electrocardiographic
of the onset of palpitations. This type of treatment evidence of ventricular pre-excitation or bundle-
has already been investigated in studies carried out branch block (QRS interval, >120 msec), a previ-
in hospitalized patients with atrial fibrillation of re- ous episode of atrial fibrillation lasting seven days
cent onset. The oral drugs that have been used to or more, ischemic heart disease, dilated or hyper-
convert atrial fibrillation of recent onset to sinus trophic cardiomyopathy, a history of heart failure,
rhythm are class IA, class IC, and class III antiar- severe valvular heart disease, chronic cor pulmo-
rhythmic agents.8-22 The class IC agents flecai- nale, left ventricular dysfunction (ejection fraction,
nide and propafenone have the advantage of act- <50 percent), a long QT interval or the Brugada
ing rapidly, and their efficacy in converting atrial syndrome, the bradycardia–tachycardia syndrome
fibrillation of recent onset to sinus rhythm has (resting heart rate, ≤50 beats per minute, or re-
been documented in several placebo-controlled tri- petitive sinoatrial blocks during waking hours),
als.8,13,15,16,18,20,22,23 The two drugs had similar documentation of previous episodes of second-
efficacy in the studies, and the success rates ranged or third-degree atrioventricular block, previous
from 58 to 95 percent.8-13,15-20,23 In all controlled thromboembolic episodes, acute disease, very se-
studies, a low incidence of adverse effects has been vere chronic diseases (e.g., muscular dystrophies or
reported.8-13,15-20,22,23 The most serious side effect systemic collagen diseases), renal or hepatic insuf-
appears to be a transient atrial flutter with a rapid ficiency, previous hypokalemia (potassium level,
ventricular rate owing to an atrioventricular con- <3 mmol per liter), suspected or known pregnancy,
duction ratio of 1:1 (in about 1 percent of patients). a known intolerance of flecainide or current pro-
We conducted a study to assess the feasibility and pafenone, or current prophylactic antiarrhythmic
safety of treatment with either flecainide or pro- treatment.
pafenone administered as a single oral dose outside We obtained a medical history for all patients and
the hospital to terminate atrial fibrillation of recent performed a physical examination, electrocardiog-
onset in patients without severe heart disease who raphy, routine biochemical laboratory tests (includ-
have infrequent, well-tolerated arrhythmic episodes. ing an assay of thyroid hormones), and two-dimen-
The primary end points were the rate of success with sional echocardiography. Other investigations, such
this treatment and the rate of adverse events. The as exercise stress testing, were performed when
secondary end points were the rates of emergency clinically indicated. Patients were recruited from
n engl j med 351;23 www.nejm.org december 2, 2004 2385
The New England Journal of Medicine
Downloaded from nejm.org on April 18, 2018. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
September 1, 2001, to February 28, 2003; follow-up Before discharge, all patients who had been treat-
was terminated September 30, 2003. ed successfully in the hospital were instructed to
The study was approved by the local ethics com- take the drug five minutes after any subsequent on-
mittee, and written informed consent was obtained set of palpitations. After the ingestion of the drug,
from all participants. A committee monitored the a resting state (in a supine or sitting position) was
progress of the study. At two of the study sites recommended until the palpitations had stopped or
(Como and Taranto), all the patients requiring emer- at least four hours had passed. Patients were also
gency room intervention for atrial fibrillation of given a form and asked to record the number of ar-
recent onset were monitored in order to determine rhythmic episodes they had; the exact times of on-
the percentage of patients who were considered set of palpitations, drug ingestion, and termination
candidates for out-of-hospital treatment. of symptoms; and any adverse effects.
Patients were advised to contact the emergency
in-hospital antiarrhythmic treatment room if their palpitations had not ceased six to eight
The patients were treated either in the emergency hours after the ingestion of the drug, if they had
room or in the cardiology ward. Each hospital used symptoms that had not occurred during previous
its own criteria for admission, which were the same arrhythmic episodes (e.g., dyspnea, presyncope, or
during the study period as they were in the year pre- syncope), or if they felt a marked increase in heart
ceding enrollment. The researchers at each center rate after ingestion of the drug. Finally, patients were
used the drug (either flecainide or propafenone) advised not to take more than one oral dose during
with which they were more familiar. a 24-hour period. After discharge, patients were
For conversion of atrial fibrillation to sinus seen in the outpatient clinic every four months.
rhythm, oral flecainide or propafenone was admin-
istered in a single dose according to the weight of statistical analysis
the patient. The dose of flecainide was 300 mg if the All the investigators had full access to the data and
patient weighed 70 kg or more and was 200 mg oth- performed the data analysis. Data are expressed as
erwise; the dose of propafenone was 600 mg if the means ±SD. Continuous variables were compared
patient weighed 70 kg or more and was 450 mg by using Student’s t-test for independent samples.
otherwise. After administration of the drug, heart A two-tailed chi-square test was used to determine
rhythm was monitored for at least 8 hours, blood the statistical significance of associations in two-
pressure was measured every 30 minutes with the by-two tables. The efficacy of the oral drug was pro-
use of a cuff, and a 12-lead electrocardiogram was vided as a crude estimate. However, because calcu-
recorded every hour. The treatment was considered lation of drug efficacy may be biased if individual
successful if the interval between administration of patients have multiple treated episodes, an adjusted
the drug and conversion to sinus rhythm was six estimate of efficacy was obtained by using the gen-
hours or less and there were no observable side ef- eralized estimating equation with an exchangeable
fects, such as symptomatic hypotension (systolic correlation structure.24 This method controls for
blood pressure, ≤80 mm Hg), symptomatic brady- multiple responses from one patient by assuming a
cardia after restoration of sinus rhythm, dyspnea, common correlation between any two responses.
presyncope, syncope, conversion to atrial flutter or A P value of less than 0.05 by two-sided test was
atrial tachycardia, or episodes of sustained or un- considered to indicate statistical significance.
sustained ventricular tachycardia.
results
out-of-hospital episodic treatment
Patients were recruited for in-hospital treatment if in-hospital treatment
all the inclusion criteria were fulfilled and no exclu- A total of 268 consecutive patients with atrial fibril-
sion criteria were documented after the medical his- lation of recent onset received an in-hospital oral
tory had been obtained and physical examination dose of flecainide (mean dose, 263±54 mg) or pro-
and electrocardiographic studies performed. Pa- pafenone (mean dose, 555±81 mg). Of those pa-
tients were selected for out-of-hospital treatment tients, 138 were treated in the emergency room
from among those who were treated successfully in and 130 in the cardiology ward. Of the 268 patients
the hospital and were not excluded during subse- who were treated, 58 were not given out-of-hospi-
quent examination. tal treatment for the following reasons (Fig. 1): ex-
2386 n engl j med 351;23 www.nejm.org december 2 , 2004
The New England Journal of Medicine
Downloaded from nejm.org on April 18, 2018. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
pill-in-the-pocket treatment of atrial fibrillation
268 Patients treated in hospital
58 Patients excluded
3 Patients (1%) met echocardio-
graphic exclusion criteria
41 Patients (15%) had drug
inefficacy
14 Patients (5%) had adverse
effects
210 Patients enrolled for out-
of-hospital treatment
4 Patients (2%) lost to follow-up
41 Patients (20%) had no 165 Patients (79%) had
recurrences recurrences
618 Arrhythmic episodes
49 Untreated episodes (8%) 569 Treated episodes (92%)
5 Episodes (10%) involved 534 Episodes (94%) interrupted
ER contact ≤6 hr
16 Episodes (3%) interrupted
>6 hr; did not contact ER
26 Episodes (5%) involved
ER contact
Total of 31 episodes (5%) involved
ER contact
Figure 1. Enrollment and Treated and Untreated Episodes of Atrial Fibrillation.
Among the 569 treated episodes, 26 that required emergency room (ER) intervention included 7 in which the episode
was interrupted in less than six hours but the patient sought help for anxiety.
n engl j med 351;23 www.nejm.org december 2, 2004 2387
The New England Journal of Medicine
Downloaded from nejm.org on April 18, 2018. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
clusion criteria were identified during echocardio- the number of patients who were candidates for out-
graphic recording in 3 (1 percent), the drug was not of-hospital treatment was 65 (12 percent).
effective in restoring sinus rhythm within six hours
in 41 (15 percent), and the drug induced side effects clinical characteristics
in 14 (5 percent), including transient hypotension The clinical characteristics of the 210 patients
(4), transient atrial flutter (7), and slightly sympto- who were discharged and given flecainide or pro-
matic bradycardia (3). Of the seven patients who had pafenone are reported in Table 1. A total of 118 pa-
transient atrial flutter after drug administration, one tients had no signs of organic heart disease, and the
had an atrioventricular conduction ratio of 1:1 and remaining 92 (44 percent) had mild heart disease
six had an atrioventricular conduction ratio of 2:1 or (hypertension in 76, valvular heart disease without
more. The mean heart rate was more than 150 beats ventricular hypertrophy or dilatation in 12, and oth-
per minute in one patient (230 beats per minute); er conditions in 4).
none of the patients had syncope, presyncope, or
hypotension or needed electrical cardioversion. The out-of-hospital treatment
remaining 210 patients were discharged and given The mean follow-up period was 15±5 months
flecainide (74) or propafenone (136) for pill-in-the- (range, 7 to 19) (Fig. 1). Four patients (2 percent)
pocket treatment of recurrent atrial fibrillation. In were lost to follow-up. Of the remaining 206 pa-
these patients, the mean duration of atrial fibrilla- tients, 41 (20 percent) did not have any arrhythmic
tion before in-hospital treatment was 280±368 recurrences during the follow-up period, and 165
minutes (median, 120), and the mean time to con- reported a total of 618 episodes of palpitations with
version to sinus rhythm was 135±79 minutes (me- an abrupt onset, 569 (92 percent) of which were
dian, 120). treated with either flecainide (in 64 patients) or pro-
In Como and Taranto, where all patients with pafenone (in 101 patients). As compared with the
atrial fibrillation of recent onset who came to the patients who had recurrences, those without recur-
emergency room were monitored during the recruit- rences were younger (P=0.008) and had had fewer
ing period, the total number of patients was 541 and emergency room interventions (P<0.001) and hos-
pitalizations (P=0.01) during the previous year.
The mean time from the onset of symptoms to
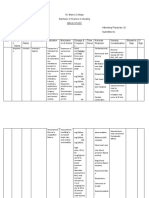
Table 1. Clinical Characteristics of 210 Patients Enrolled for Out-of-Hospital the ingestion of the drug was 36±93 minutes (me-
Treatment of Recurrent Atrial Fibrillation. dian, 10). The drug was effective (i.e., palpitations
were interrupted within six hours) in 534 of 569 ar-
Characteristic Value*
rhythmic episodes (94 percent; corrected efficacy,
Age — yr 59±11 93 percent; 95 percent confidence interval, 90 to
Male sex — no. (%) 122 (58) 95). The mean time to the resolution of symptoms
Mild heart disease — no. (%) 92 (44) after the ingestion of the drug was 113±84 minutes
History of atrial fibrillation — yr (median, 98). Flecainide was effective in 239 of 254
Mean 4±5 episodes (94 percent), and propafenone in 295 of
Median 3 315 (94 percent).
Symptomatic episodes of atrial fibrillation in previous year 3.3±2.6 Sixteen arrhythmic episodes (3 percent) were in-
— no./patient† terrupted after more than 6 hours (range, 390 to 890
Emergency room contacts in previous year — no./patient† 2.7±2.3 minutes) without the patients’ contacting the emer-
Hospitalizations in previous year — no./patient† 0.9±1.1 gency room. Twenty-six episodes (5 percent) re-
Duration of target episode before in-hospital treatment — min quired emergency room intervention, 10 of which
Mean 280±368 (2 percent) also required hospitalization. Of the to-
Median 120
tal of 618 episodes of palpitations, 49 were not treat-
ed, either because the patient felt that the arrhythmic
Previous prophylactic treatment — no. of patients (%) 72 (34)
attack was mild or because the drug was unavail-
Left ventricular ejection fraction — % 59±5
able, and 5 of these episodes (10 percent) required
Left atrial diameter — mm 39±5
emergency room intervention. Thus, during the fol-
low-up period, a total of 31 treated or untreated ar-
* Plus–minus values are means ±SD.
† Data do not include the target episode. rhythmic episodes (5 percent) resulted in emergen-
cy room visits, and 10 of these episodes required
2388 n engl j med 351;23 www.nejm.org december 2 , 2004
The New England Journal of Medicine
Downloaded from nejm.org on April 18, 2018. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
pill-in-the-pocket treatment of atrial fibrillation
hospitalization. Of the 31 emergency room visits, 2 (1 percent) because of adverse effects (atrial flut-
19 were due to episodes of atrial fibrillation that last- ter at a rapid ventricular rate in 1 and nausea in 1),
ed for more than six hours, 1 to acceleration of the and 5 (2 percent) because of psychological problems
heart rate after drug ingestion, and 11 to anxiety. or noncompliance.
(Among the calls that were attributed to anxiety, sev-
en involved a request for emergency room interven- discussion
tion even though the atrial fibrillation had lasted for
less than six hours and was well tolerated and four Several controlled studies carried out in hospital-
involved a request for an electrocardiogram al- ized patients have shown that oral flecainide and
though palpitations had ceased.) propafenone, in the first three to eight hours after
Among the 165 patients with recurrences, the administration, have a similar efficacy and are more
drug was effective during all the arrhythmic epi- effective than placebo and other oral antiarrhyth-
sodes in 139 (84 percent). Of the 27 patients who mic agents such as amiodarone and quinidine plus
had at least one episode that lasted for more than digoxin.8-13,15-20 Our study focused on out-of-hos-
six hours after the ingestion of the drug, 9 (5 per- pital treatment for atrial fibrillation of recent onset.
cent) did not request emergency room intervention, The main finding is that self-administration of a sin-
whereas 18 (11 percent) did. During the follow- gle oral loading dose of flecainide or propafenone is
up period, 31 patients took atrioventricular nodal feasible and safe and appears to be effective.
blockers for treatment of hypertension (beta-block- During the in-hospital phase, treatment with fle-
ers in 24 and verapamil in 7). cainide or propafenone was successful in about 80
percent of patients. We chose resolution of palpita-
comparison with the year tions within six hours after ingestion of the drug as
before enrollment the criterion of efficacy because after six hours, the
Among the 210 patients enrolled, the mean num- rate of success of oral class IC agents is similar to
ber of symptomatic episodes per month for the that of placebo; moreover, a period of six hours is
group was 59.8 in the year before enrollment (ex- reasonable from the clinical point of view. The dose
cluding the target episode) and 54.5 during the fol- we used had previously been demonstrated to be the
low-up period, not a significant difference. During most suitable for oral treatment.8,16,18,22,25
follow-up, the number of calls for emergency room After the exclusion of patients who had a conver-
intervention was 4.9 per month, which was signifi- sion to sinus rhythm after more than six hours or ad-
cantly lower than the number per month in the year verse effects during in-hospital treatment, we found
before the target episode (45.6, P<0.001). The num- that oral flecainide and propafenone interrupted 94
ber of hospitalizations per month during the follow- percent of the out-of-hospital arrhythmic episodes,
up period was also significantly lower (1.6 vs. 15.0, and in 84 percent of the patients, the treatment was
P<0.001). effective for all the arrhythmic episodes, with a
mean conversion time of about two hours. In the
adverse effects remaining patients, failure occurred during one or
Adverse effects during one or more arrhythmic ep- more episodes because the drug was ineffective or
isodes were reported in 12 of the 165 patients who unavailable. However, despite efficacy, about 5 per-
used the drug during follow-up (7 percent). One cent of the patients dropped out of the study be-
patient (0.6 percent) felt a marked acceleration of cause of multiple recurrences, side effects (especial-
heart rate after ingestion of the drug and contacted ly nausea), or anxiety.
the emergency room; the electrocardiogram showed During out-of-hospital treatment, the incidence
atrial flutter, with an atrioventricular conduction ra- of adverse effects was low. Only one patient (0.6 per-
tio of 1:1 and a ventricular rate of 210 beats per min- cent) felt a marked acceleration of the heart rate af-
ute. The remaining 11 patients reported noncardiac ter the ingestion of flecainide, and the electrocar-
side effects such as nausea, asthenia, and vertigo. diogram recorded in the emergency room showed
Twenty-seven of the 210 patients (13 percent) atrial flutter with a rapid ventricular rate. This find-
dropped out of the study after a mean of 7±3 ing indicates that successful in-hospital treatment
months: 13 (6 percent) because the drug was inef- does not rule out an atrial flutter at a high rate dur-
fective, 7 (3 percent) because of multiple episodes ing subsequent treatment out of the hospital.
requiring antiarrhythmic prophylactic treatment, The pill-in-the-pocket strategy markedly reduced
n engl j med 351;23 www.nejm.org december 2, 2004 2389
The New England Journal of Medicine
Downloaded from nejm.org on April 18, 2018. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
emergency room visits and hospital admissions. possibility that some episodes of palpitations were
The reduction in hospitalizations paralleled the re- the result of arrhythmias other than atrial fibrilla-
duction in emergency room visits. These data are of tion. The use of patient-activated transmission of
clinical significance because emergency room visits cardiac data by telephone in choosing the arrhyth-
and hospital admissions often represent the most mic episodes to be treated would have enabled us to
important concern for patients with recurrent atrial evaluate more precisely the efficacy of flecainide and
fibrillation. However, among the patients in our propafenone in terminating recurrent episodes of
study who contacted the emergency room during atrial fibrillation. However, this approach would not
the recruitment period, only a small group (12 per- have allowed us to investigate the safety of the pill-
cent) were candidates for out-of-hospital treat- in-the-pocket strategy in the real world.
ment. A not-unexpected finding was that the clin- The pill-in-the-pocket approach appears to be
ical course may deteriorate in some patients; this feasible and safe, in view of the high rate of patient
was the case in 7 of the 210 patients in the study compliance and the very low incidence of adverse
(3 percent), who were switched from pill-in-the- effects. Data from our study show that the pill-in-
pocket treatment to prophylactic antiarrhythmic the-pocket strategy with flecainide and propafenone
therapy owing to the occurrence of more frequent is effective for all the arrhythmic episodes in more
arrhythmic episodes. than 80 percent of patients with recurrent atrial fi-
In evaluating the out-of-hospital efficacy of class brillation, after selection of patients on the basis of
IC drugs in recurrent atrial fibrillation, we did not clinical features and the results of in-hospital treat-
perform a randomized comparison of these drugs ment. Out-of-hospital treatment minimizes the
with placebo because several in-hospital trials had need for subsequent emergency room visits and
already demonstrated the superiority of oral flecai- hospitalization, which should reduce the costs as-
nide and propafenone over placebo during obser- sociated with atrial fibrillation, albeit in a small
vation periods of four to eight hours. The purpose group of patients who have this tachyarrhythmia.
of our study was to investigate the feasibility and The safety of this approach without previous evalu-
safety of the pill-in-the-pocket approach. During ation of in-hospital treatment remains to be inves-
the follow-up period, arrhythmic episodes and con- tigated.
comitant drug treatment were assessed on the basis Supported by a grant from the Associazione Italiana di Aritmolo-
of the patients’ symptoms. We cannot exclude the gia e Cardiostimolazione.
ap p e n d i x
The members of the steering committee of the study (with their locations in Italy) were P. Alboni (Cento), N. Baldi (Taranto), G. Boriani (Bo-
logna), G.L. Botto (Como), M. Brignole (Lavagna), A. Capucci (Piacenza), A. Del Rosso (Fucecchio), A. De Simone (Maddaloni), G. Inama
(Crema), G. Marinoni (Pavia), C. Menozzi (Reggio Emilia), and A. Raviele (Mestre–Venezia). Participating centers and investigators includ-
ed Ospedale Civile, Cento, L. Gianfranchi; Ospedale S. Anna, Como, M. Luzi; Ospedale SS. Annunziata, Taranto, V. Russo; Ospedale del
Delta, Lagosanto, P. Marchi; Arcispedale Santa Maria Nuova, Reggio Emilia, M. Calzolari; Ospedali Riuniti, Lavagna, A. Solano; Ospedale
Galmarini, Tradate, R. Baroffio; Ospedale Civile, Sampierdarena, G. Gaggioli; Ospedale Renzetti, Lanciano, D. Tullio; Policlinico S. Orsola,
Bologna, G. Boriani; Ospedale Ceccarini, Riccione, N. Candiotti; Ospedale Ferrari, Casarano, A. Marzo; Ospedale S.C. di Gesù, Gallipoli, L.
Stella; Ospedale Civile, Sassuolo, F. Melandri.
refer enc es
1. Mannino MM, Metha D, Gomes JA. Cur- rhythm control in patients with recurrent frequency ablation for atrial fibrillation. Eur
rent treatment options for paroxysmal su- persistent atrial fibrillation. N Engl J Med Heart J 2003;5:Suppl:H34-H39.
praventricular tachycardia. Am Heart J 1994; 2002;347:1834-40. 8. Villani GQ, Rosi A, Piepoli M, et al. The
127:475-80. 5. Carlsson J, Miketic S, Windeler J, et al. efficacy of oral treatment with flecainide for
2. Hohnloser SH, Kuck KH, Lilienthal J. Randomized trial of rate-control versus paroxysmal atrial fibrillation: correlation
Rhythm or rate control in atrial fibrillation rhythm-control in persistent atrial fibrilla- with plasma concentration. G Ital Cardiol
— Pharmacological Intervention in Atrial tion: the Strategies of Treatment of Atrial Fi- 1990;20:564-8. (In Italian.)
Fibrillation (PIAF): a randomized trial. Lan- brillation (STAF) study. J Am Coll Cardiol 9. Capucci A, Lenzi T, Boriani G, et al. Ef-
cet 2000;356:1789-94. 2003;41:1690-6. fectiveness of loading oral flecainide for
3. Wyse DG, Waldo AL, DiMarco JP, et al. 6. Haissaguerre M, Jaïs P, Shah DC, et al. converting recent-onset atrial fibrillation to
A comparison of rate control and rhythm Spontaneous initiation of atrial fibrilla- sinus rhythm in patients without organic
control in patients with atrial fibrillation. tion by ectopic beats originating in the pul- heart disease or with only systemic hyper-
N Engl J Med 2002;347:1825-33. monary veins. N Engl J Med 1998;339:659- tension. Am J Cardiol 1992;70:69-72.
4. Van Gelder IC, Hagens VE, Bosker HA, 66. 10. Botto GL, Bonini W, Broffoni T, et al.
et al. A comparison of rate control and 7. Jaïs P, Shah DC, Hocini M, et al. Radio- Regular ventricular rhythms before conver-
2390 n engl j med 351;23 www.nejm.org december 2 , 2004
The New England Journal of Medicine
Downloaded from nejm.org on April 18, 2018. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
pill-in-the-pocket treatment of atrial fibrillation
sion of recent onset atrial fibrillation to sinus with single loading oral dose of propafenone: amiodarone for converting recent-onset atri-
rhythm. Pacing Clin Electrophysiol 1994;17: is in-hospital admission absolutely neces- al fibrillation. Am J Cardiol 1999;84:1029-32.
2114-7. sary? Pacing Clin Electrophysiol 1996;19: 21. Kishikawa T, Maruyoma T, Kaji Y, et al.
11. Capucci A, Boriani G, Botto GL, et al. 1939-43. Effects of oral repetitive loading of disopyra-
Conversion of recent-onset atrial fibrillation 16. Azpitarte J, Alvarez M, Baun O, et al. Val- mide on acute-onset atrial fibrillation with
by a single oral loading dose of propafenone ue of single oral loading dose of propafenone concurrent monitoring of serum drug con-
or flecainide. Am J Cardiol 1994;74:503-5. in converting recent-onset atrial fibrillation: centration. Int J Cardiol 1999;68:57-62.
12. Capucci A, Boriani G, Rubino I, Della results of a randomized, double-blind, con- 22. Khan IA. Single oral loading dose of
Casa S, Sanguinetti M, Magnani B. A con- trolled study. Eur Heart J 1997;18:1649-54. propafenone for pharmacological cardio-
trolled study on oral propafenone versus di- 17. Boriani G, Biffi M, Capucci A, et al. Oral version of recent-onset atrial fibrillation.
goxin plus quinidine in converting recent propafenone to convert recent-onset atrial fi- J Am Coll Cardiol 2001;37:542-7.
onset atrial fibrillation to sinus rhythm. Int J brillation in patients with and without under- 23. Capucci A, Villani GQ, Piepoli MF. Re-
Cardiol 1994;43:305-13. lying heart disease: a randomized, controlled producible efficacy of loading oral pro-
13. Boriani G, Capucci A, Lenzi T, San- trial. Ann Intern Med 1997;126:621-5. pafenone in restoring sinus rhythm in pa-
guinetti M, Magnani B. Propafenone for 18. Botto GL, Capucci A, Bonini W, et al. tients with paroxysmal atrial fibrillation.
conversion of recent-onset atrial fibrilla- Conversion of recent onset atrial fibrillation Am J Cardiol 2003;92:1345-7.
tion: a controlled comparison between oral to sinus rhythm using a single loading oral 24. Zeger SL, Liang KY, Albert PS. Models
loading dose and intravenous administra- dose of propafenone: comparison of two for longitudinal data: a generalized estimat-
tion. Chest 1995;108:355-8. regimens. Int J Cardiol 1997;58:55-61. ing equation approach. Biometrics 1988;
14. Halinen MO, Huttunen M, Paakkinen S, 19. Botto GL, Bonini W, Broffoni T, et al. 44:1049-60. [Erratum, Biometrics 1989;45:
Tarssanen L. Comparison of sotalol with di- Randomized, crossover, controlled compar- 347.]
goxin-quinidine for conversion of acute atri- ison of oral loading versus intravenous infu- 25. Capucci A, Boriani G, Marchesini B, et al.
al fibrillation to sinus rhythm (the Sotalol- sion of propafenone in recent-onset atrial fi- Minimal effective concentration values of
Digoxin-Quinidine Trial). Am J Cardiol 1995; brillation. Pacing Clin Electrophysiol 1998; propafenone and 5-hydroxy-propafenone in
76:495-8. 21:2480-4. acute and chronic therapy. Cardiovasc Drugs
15. Botto GL, Bonini W, Broffoni T, et al. 20. Blanc JJ, Voinov C. Maarek M. Compari- Ther 1990;4:281-7.
Conversion of recent onset atrial fibrillation son of oral loading dose of propafenone and Copyright © 2004 Massachusetts Medical Society.
journal editorial fellow
The Journal’s editorial office invites applications for a one-year
research fellowship beginning in July 2005 from individuals at any
stage of training. The editorial fellow will work on Journal projects
and will participate in the day-to-day editorial activities of the
Journal but is expected in addition to have his or her own inde-
pendent projects. Please send curriculum vitae and research in-
terests to the Editor-in-Chief, 10 Shattuck St., Boston, MA 02115
(fax, 617-739-9864), by January 15, 2005.
n engl j med 351;23 www.nejm.org december 2, 2004 2391
The New England Journal of Medicine
Downloaded from nejm.org on April 18, 2018. For personal use only. No other uses without permission.
Copyright © 2004 Massachusetts Medical Society. All rights reserved.
Anda mungkin juga menyukai
- Different in the therapy of pressure negtotheeva single-useDari EverandDifferent in the therapy of pressure negtotheeva single-useBelum ada peringkat
- Early Use of TIPS in Cirrhosis and Variceal BleedingDokumen10 halamanEarly Use of TIPS in Cirrhosis and Variceal Bleedingray liBelum ada peringkat
- Record 1 - THRDokumen11 halamanRecord 1 - THRNorhamdan Mohd YahayaBelum ada peringkat
- 12 - 2015 - LT Safety and Efficacy of Imatinib in PAH - IMPRES (10) 70Dokumen10 halaman12 - 2015 - LT Safety and Efficacy of Imatinib in PAH - IMPRES (10) 70edward the iiiBelum ada peringkat
- Thoracic Epidural For Modified Radical Mastectomy in A High-Risk PatientDokumen2 halamanThoracic Epidural For Modified Radical Mastectomy in A High-Risk PatientBianca CaterinalisendraBelum ada peringkat
- ClonidineDokumen4 halamanClonidineDR RAVI ANANDBelum ada peringkat
- GUSTO III ReteplaseDokumen6 halamanGUSTO III ReteplaseSalsabila RahmaBelum ada peringkat
- Jurding Paru 1Dokumen12 halamanJurding Paru 1Clinton SudjonoBelum ada peringkat
- JurnalDokumen32 halamanJurnalRiska Maulida ErizalBelum ada peringkat
- Original Research: Colchicine For Recurrent Pericarditis (CORP)Dokumen7 halamanOriginal Research: Colchicine For Recurrent Pericarditis (CORP)Ana HurtadoBelum ada peringkat
- Nej Mo A 1503184Dokumen12 halamanNej Mo A 1503184Amr MostafaBelum ada peringkat
- Syncope Update 2004Dokumen4 halamanSyncope Update 2004jkriengBelum ada peringkat
- Nej Mcl de 2311699Dokumen4 halamanNej Mcl de 2311699coniestivillBelum ada peringkat
- Ying Li 2016Dokumen8 halamanYing Li 2016Bogdan TrandafirBelum ada peringkat
- Journal ClubDokumen4 halamanJournal Clubbrittany postBelum ada peringkat
- Astronaut 2013Dokumen11 halamanAstronaut 2013Guilherme CarelliBelum ada peringkat
- On-Treatment Function Testing of Platelets and Long-Term Outcome of Patients With Peripheral Arterial Disease Undergoing Transluminal AngioplastyDokumen8 halamanOn-Treatment Function Testing of Platelets and Long-Term Outcome of Patients With Peripheral Arterial Disease Undergoing Transluminal AngioplastyGono GenieBelum ada peringkat
- High Prevalence of Proarrhythmic Events in PatientDokumen8 halamanHigh Prevalence of Proarrhythmic Events in PatientAlda AdeliaBelum ada peringkat
- NEJMclde2311699Dokumen4 halamanNEJMclde2311699felipetheBelum ada peringkat
- Cardaic ResynchronizationDokumen11 halamanCardaic ResynchronizationSamatha BiotechBelum ada peringkat
- Alteplase Data 4Dokumen9 halamanAlteplase Data 4Muhammad FirmansyahBelum ada peringkat
- Effect of IV Ondansetron on Maternal Hemodynamics During Spinal for C-SectionDokumen6 halamanEffect of IV Ondansetron on Maternal Hemodynamics During Spinal for C-Sectionputri maharani andesBelum ada peringkat
- DabigatranDokumen12 halamanDabigatranAdityaSaskaraBelum ada peringkat
- Closure of Patent Foramen Ovale Versus Medical Therapy After Cryptogenic StrokeDokumen9 halamanClosure of Patent Foramen Ovale Versus Medical Therapy After Cryptogenic StrokelaurasheerBelum ada peringkat
- Hyerion Trial en Arresto Cardiaco HipotermiaDokumen11 halamanHyerion Trial en Arresto Cardiaco HipotermiagomsuiBelum ada peringkat
- 9829 CE (Ra) F (SH) PF1 (SNAK) PFA (P)Dokumen4 halaman9829 CE (Ra) F (SH) PF1 (SNAK) PFA (P)razaqhussain00Belum ada peringkat
- 221 FullDokumen7 halaman221 FullFina NABelum ada peringkat
- Pronostico Fiebre Reumatica Con Penicilina Largo PlazoDokumen9 halamanPronostico Fiebre Reumatica Con Penicilina Largo PlazoEl TrémoloBelum ada peringkat
- Acute Necrotizing Pancreatitis: Treatment Strategy According To The Status of InfectionDokumen8 halamanAcute Necrotizing Pancreatitis: Treatment Strategy According To The Status of InfectionHandhika Dhio SumarsonoBelum ada peringkat
- The Effect of Early Canalith Repositioning On Benign Paroxysmal Positional Vertigo On RecurrenceDokumen5 halamanThe Effect of Early Canalith Repositioning On Benign Paroxysmal Positional Vertigo On RecurrencezanafiraBelum ada peringkat
- Op Time 2002Dokumen7 halamanOp Time 2002dalialamasbonita1093Belum ada peringkat
- Myocard InfarctionDokumen10 halamanMyocard InfarctionFelicia HoseaBelum ada peringkat
- 1576 Full PDFDokumen8 halaman1576 Full PDFRetno WidiastriBelum ada peringkat
- Early Postoperative ComplicationsDokumen6 halamanEarly Postoperative Complications49hr84j7spBelum ada peringkat
- Angioedema Induzido Por EscitalopramDokumen4 halamanAngioedema Induzido Por EscitalopramIratanFernandesBelum ada peringkat
- Late Results After Splenectomy in Adult Idiopathic Thrombocytopenic PurpuraDokumen7 halamanLate Results After Splenectomy in Adult Idiopathic Thrombocytopenic PurpuraBogdan TrandafirBelum ada peringkat
- Safety PPMDokumen11 halamanSafety PPMMonica TrifitrianaBelum ada peringkat
- CURE TrialDokumen9 halamanCURE TrialCristina PazmiñoBelum ada peringkat
- VTE Cases For StudentsDokumen46 halamanVTE Cases For StudentsHanifah Siti AisyahBelum ada peringkat
- Pneumonia in Acute Stroke Patients Fed by Nasogastric Tube: PaperDokumen5 halamanPneumonia in Acute Stroke Patients Fed by Nasogastric Tube: PaperLira PurnamawatiBelum ada peringkat
- Hemodynamic Response To Pharmacological Treatment of Portal Hypertension and Long-Term Prognosis of CirrhosisDokumen7 halamanHemodynamic Response To Pharmacological Treatment of Portal Hypertension and Long-Term Prognosis of CirrhosisBarbara Sakura RiawanBelum ada peringkat
- Genta Transtimpanica 3Dokumen9 halamanGenta Transtimpanica 3natalia.gallinoBelum ada peringkat
- Haematemesis and MalenaDokumen39 halamanHaematemesis and MalenaNikBelum ada peringkat
- Genta Transtimpanica 4Dokumen8 halamanGenta Transtimpanica 4natalia.gallinoBelum ada peringkat
- Management of Neoplastic Pericardial EffusionsDokumen4 halamanManagement of Neoplastic Pericardial EffusionsMamamia DonchanBelum ada peringkat
- 11 - 2015 - Efficacy and Safety of Long-Term Imatinib Therapy For PAH, Speich (10) 20Dokumen10 halaman11 - 2015 - Efficacy and Safety of Long-Term Imatinib Therapy For PAH, Speich (10) 20edward the iiiBelum ada peringkat
- Levo DobutaDokumen4 halamanLevo DobutaJorge Mario Largo GilBelum ada peringkat
- Jeyakumar 2006Dokumen5 halamanJeyakumar 2006johnweakBelum ada peringkat
- A Prospective, Randomized, Double-Blind, Multicenter Study Comparing Remifentanil With Fentanyl in Mechanically Ventilated PatientsDokumen8 halamanA Prospective, Randomized, Double-Blind, Multicenter Study Comparing Remifentanil With Fentanyl in Mechanically Ventilated PatientsJosé Carlos Sánchez-RamirezBelum ada peringkat
- A Prospective, Randomized, Double-Blind, Multicenter Study Comparing Remifentanil With Fentanyl in Mechanically Ventilated PatientsDokumen8 halamanA Prospective, Randomized, Double-Blind, Multicenter Study Comparing Remifentanil With Fentanyl in Mechanically Ventilated PatientsJosé Carlos Sánchez-RamirezBelum ada peringkat
- Topical Propranolol Improves Epistaxis Control in Hereditary Hemorrhagic Telangiectasia (HHT) : A Randomized Double-Blind Placebo-Controlled TrialDokumen12 halamanTopical Propranolol Improves Epistaxis Control in Hereditary Hemorrhagic Telangiectasia (HHT) : A Randomized Double-Blind Placebo-Controlled TrialAmaliah HakimBelum ada peringkat
- Nejmoa 010746Dokumen9 halamanNejmoa 010746Mmle BlaséBelum ada peringkat
- E423 FullDokumen11 halamanE423 FullCecepBelum ada peringkat
- Pharma Intervention StudyDokumen10 halamanPharma Intervention Studybryan chanBelum ada peringkat
- Kring JournalDokumen3 halamanKring JournalcbanguisBelum ada peringkat
- Efficacy and Safety of Thrombolytic Therapy in ProDokumen5 halamanEfficacy and Safety of Thrombolytic Therapy in ProgalalBelum ada peringkat
- Piracetam PDFDokumen5 halamanPiracetam PDFAriWahyuBelum ada peringkat
- Cardiac Arrest Upon Induction of General AnesthesiaDokumen7 halamanCardiac Arrest Upon Induction of General AnesthesiaIlona HiariejBelum ada peringkat
- Top Trials in Gastroenterology & HepatologyDari EverandTop Trials in Gastroenterology & HepatologyPenilaian: 4.5 dari 5 bintang4.5/5 (7)
- Management of TIC 2010 AANADokumen6 halamanManagement of TIC 2010 AANAn2coolohBelum ada peringkat
- Kidney Structure & HistologyDokumen8 halamanKidney Structure & Histologyn2coolohBelum ada peringkat
- Army Corps Evicting Everyone From Standing Rock On December 5Dokumen2 halamanArmy Corps Evicting Everyone From Standing Rock On December 5The Daily Haze50% (2)
- Final Review Fall 10Dokumen3 halamanFinal Review Fall 10n2coolohBelum ada peringkat
- Treatment of Tumor Lysis SyndromeDokumen13 halamanTreatment of Tumor Lysis Syndromen2coolohBelum ada peringkat
- Recognize and Manage Common Pediatric Cardiac EmergenciesDokumen73 halamanRecognize and Manage Common Pediatric Cardiac EmergenciesKristine CaringalBelum ada peringkat
- Syncope in Adults - Clinical Manifestations and Initial Diagnostic Evaluation - UpToDateDokumen21 halamanSyncope in Adults - Clinical Manifestations and Initial Diagnostic Evaluation - UpToDateBruno FernandesBelum ada peringkat
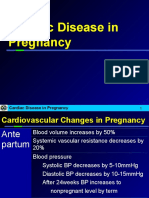
- Cardiac Disease in PregnancyDokumen21 halamanCardiac Disease in PregnancyRenata CilestrinaBelum ada peringkat
- St. Mary's College Nursing Drug StudyDokumen3 halamanSt. Mary's College Nursing Drug StudyKwin Saludares100% (1)
- Palpitations: DR Polamuri Tabitha PG First YrDokumen37 halamanPalpitations: DR Polamuri Tabitha PG First YrNinaBelum ada peringkat
- Cardio QuizDokumen100 halamanCardio QuizEvidence ChaibvaBelum ada peringkat
- Palpitation:evaluation, Ambulatory Monitoring, Mobile Telemetry Eg - MCOT@2012Dokumen19 halamanPalpitation:evaluation, Ambulatory Monitoring, Mobile Telemetry Eg - MCOT@2012Navojit ChowdhuryBelum ada peringkat
- DR Drug StudyDokumen6 halamanDR Drug Studyslashmortred100% (5)
- 4 Med LongDokumen135 halaman4 Med LongElla H. LeeBelum ada peringkat
- Nichols, Diane. the Demons Within, Confronting Performance Anxiety (Απόσπασμα, 1996)Dokumen2 halamanNichols, Diane. the Demons Within, Confronting Performance Anxiety (Απόσπασμα, 1996)lazer84100% (1)
- History Taking in Clinical Practice 2023Dokumen164 halamanHistory Taking in Clinical Practice 2023imran karimBelum ada peringkat
- Chronic Inappropriate Sinus Tachycardia (Lopera)Dokumen5 halamanChronic Inappropriate Sinus Tachycardia (Lopera)Raymond BernardusBelum ada peringkat
- Anti Arrhythmic Drugs - FINALDokumen25 halamanAnti Arrhythmic Drugs - FINALThanyun Yun100% (1)
- OET Stuff To MemorizeDokumen18 halamanOET Stuff To MemorizeAleksandr ShnyrovBelum ada peringkat
- Rubrics For Children in MurphyDokumen18 halamanRubrics For Children in MurphyVirag PatilBelum ada peringkat
- 1700 Mock 1 PDFDokumen68 halaman1700 Mock 1 PDFSiraj Ul IslamBelum ada peringkat
- Andrade, Ban, Salleva - Liver Cirrhosis - Objectives, Manifestations, Drug StudyDokumen9 halamanAndrade, Ban, Salleva - Liver Cirrhosis - Objectives, Manifestations, Drug StudyWindi Dawn SallevaBelum ada peringkat
- American Heart Association: Precourse Written Examination May 2001Dokumen10 halamanAmerican Heart Association: Precourse Written Examination May 2001Ericka SwordBelum ada peringkat
- 58 Cases History and Physical Exam BookDokumen102 halaman58 Cases History and Physical Exam BookeleazarmdBelum ada peringkat
- Heart Palpitations Top 6 Herbs According To A HerbalistDokumen31 halamanHeart Palpitations Top 6 Herbs According To A HerbalistCarl MacCordBelum ada peringkat
- 500 Single Best Answers in MedicineDokumen443 halaman500 Single Best Answers in MedicineOmar Ahmed100% (1)
- ACCSAP 10 Qs & As ReviewDokumen470 halamanACCSAP 10 Qs & As ReviewAdeel Lakhiar100% (9)
- PheochromocytomaDokumen6 halamanPheochromocytomaVenkatesh Tammineni100% (1)
- N220 W9 Nursing Care PlanDokumen3 halamanN220 W9 Nursing Care PlanVivian PhamBelum ada peringkat
- Cardiac Arrhythmias in ChildrenDokumen50 halamanCardiac Arrhythmias in ChildrenNorhafizah AhmadBelum ada peringkat
- Kiiko Matsumoto - TreatmentsDokumen25 halamanKiiko Matsumoto - TreatmentsHaryono zhu86% (7)
- Tests Module 2Dokumen59 halamanTests Module 2Haruna Bzaki100% (1)
- Emergency Nursing Assessment QuestionsDokumen10 halamanEmergency Nursing Assessment QuestionsTni JolieBelum ada peringkat
- Part IIDokumen64 halamanPart IIhussainBelum ada peringkat
- الباطنة كلها بالتفصيل في 160 صفحة فقط لازم تحمل المذكرة فوراDokumen163 halamanالباطنة كلها بالتفصيل في 160 صفحة فقط لازم تحمل المذكرة فورانادين مطر0% (1)