Epithelial To Mesenchymal Transition
Diunggah oleh
Aryaman Shodhan0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
64 tayangan3 halamanThis is a literature review on the "Epithelial to Mesenchymal Transition" of cancer cells before metastasis. It has insights from a course on Coursera online - "Understanding Cancer Metastasis" - by Johns Hopkins University
Judul Asli
Epithelial to Mesenchymal Transition
Hak Cipta
© © All Rights Reserved
Format Tersedia
PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniThis is a literature review on the "Epithelial to Mesenchymal Transition" of cancer cells before metastasis. It has insights from a course on Coursera online - "Understanding Cancer Metastasis" - by Johns Hopkins University
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
64 tayangan3 halamanEpithelial To Mesenchymal Transition
Diunggah oleh
Aryaman ShodhanThis is a literature review on the "Epithelial to Mesenchymal Transition" of cancer cells before metastasis. It has insights from a course on Coursera online - "Understanding Cancer Metastasis" - by Johns Hopkins University
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 3
Epithelial
to Mesenchymal Transition (EMT)
In order for cancer to metastasize, the cells at the primary tumour site must
be able to overcome the linkages holding the cells together and gain
migratory characteristics. This is possible due to a process called Epithelial to
mesenchymal transition (EMT) that enables a polarized, adherent epithelial
cell to undergo multiple biochemical changes and mutations in its DNA that
enables the cell to develop a mesenchymal cell phenotype. This allows the cell
to migrate away from its initial growth site and spread to distant regions of
the body via the blood.
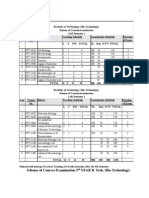
Epithelial cells vs. Mesenchymal cells
Epithelial Cell Mesenchymal Cell
Differentiated cells which may have Spindle shaped cells
specific shapes and structures
depending on their funcstions
Derived from the ectoderm of a Derived from the mesoderm of a
trilaminar embryo trilaminar embryo
Cells are tightly connected to each Cells are highly mobile and are linked
other at junctions to each other at focal points
Normal cells line organs and vessels, Normal cells can differentiate into
providing protection connective tissue and provide support
Cells show apico-basal polarity No evidence of polarity seen in cells
Cancerous cells cannot secrete Cancerous cells can secrete
extracellular matrix components extracellular matrix components to
support proliferation
The Go vs Grow Hypothesis
A cancer cell may either proliferate (grow) or move (go). Proliferation is a
characteristic central to primary tumour cells whereas movement is central to
metastasizing cells. Within a single cell, this going and growing is separated in
space as well as in time. Cancer cells may switch between these 2 processes
but a more proliferative cell is less mobile; the converse holds true. However,
some cancer cells may also show a mixture of these 2 phenotypes.
Types of EMT
Based on the various functional consequences of EMTs, there are 3 broad
categories for the same:
Type 1 EMT: This type of EMT mostly aids the developmental process of a
fetus by giving rise to the endoderm and mesoderm of the trilaminar embryo.
Type 1 primary epithelial cells, called epiblasts, may undergo an EMT to form
mesenchymal cells that may differentiate into secondary epithelial cells by the
reverse process- a mesenchymal to epithelial transition (MET).
Type 2 EMT: This type of EMT is responsible for the triggering of inflammation
and fibrosis or healing of organs. Type 2 EMT is expressed over extended time
periods and may destroy an affected organ if the cause of inflammation is not
terminated.
Type 3 EMT: Differentiated secondary epithelial cells may form cancer cells
which undergo Type 3 EMT to enable the invasive and metastatic
characteristics of the cells.
The process of EMT in cancer cells
While EMT is a vital process for wound healing, embryonic development, and
organ fibrosis, it is also the initiative process for cancer metastasis. Pressures
in the tumour microenvironment, including hypoxemia or low oxygen levels
for the tumour cells, low concentrations of cytokines, chemokines as well as
other signaling molecules may cause the tumour cells to express a different
set of genes in their DNA which result in several characteristics conferred by
these cells:
• The cells become spindle shaped
• The cells lose their polarization and their junction points break down so
that they detach and break through the extracellular matrix with the aid of
ECM-degrading enzymes like Matrix metalloproteinase-2
• Downregulation of tumour suppressor proteins like E-Cadherin and
upregulation of metastatic proteins like N-Cadherin with the aid of
transcription factors belonging to the SNAIL, ZEB and TWIST families.
• Progressive loss of epithelial markers and gain of mesenchymal markers
• Cells can secrete extracellular matrix components
• Reorganization of cytoskeletal proteins like ZO proteins and claudins
As a result of some of these biochemical changes, the motility of the cancer
cells increases and they invade the local region containing normal body cells
before intravasating into the blood vessels.
Signaling pathways involved in EMT
1) The TGF-beta signaling pathway: TGF-beta is a signaling molecule which
plays a dual role- inducing programmed cell death in the early stages of
tumour growth and EMT, migration and invasion in the later stages. The
TFG-beta molecule binds to a receptor protein in the cell surface
membrane of the cancer cell that has a complementary shape to the
signaling molecule. This triggers a G-protein to activate a regulatory
protein called SMAD. This protein travels to the nucleus of the cancer cell,
where it aids the transcription of EMT-inducing target genes which results
in EMT.
2) The Wnt signaling pathway: The Wnt pathway operates in a similar way to
the TGF-beta pathway. Wnt, a signaling molecule, binds to a specific cell
surface receptor protein called FRIZZLED. This inactivates an enzyme called
Glycogen synthase kinase 3-beta (GSK3-beta) that is responsible for the
prevention of the stabilization of beta-catenin molecules. In the absence of
the GSK3-beta molecule, stable beta-catenin molecules travel to the
nucleus of the cancer cell, where they aid the transcription of EMT-
inducing target genes.
Although diligent research has been going on to find a successful remedy for
cancer metastasis, little is known about the mechanism of EMT in cancer cells.
Further research concerning how to break the signaling pathways involved in
EMT may spur the development of chemotherapeutic drugs that target the
cancer cells undergoing EMT. In the future, this may reduce the incidence of
cancer metastasis and allude to a solution to one of the most puzzling aspects
of cancer cell histology.
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Nutrition: Bussines Case StudyDokumen4 halamanNutrition: Bussines Case StudyAntonia Michaela IonBelum ada peringkat
- Daftar Pustaka PDFDokumen10 halamanDaftar Pustaka PDFgunawanmulyana12Belum ada peringkat
- Fatty LiverDokumen2 halamanFatty LiverKarla Edith Rodriguez Nava100% (2)
- Skip To Main Content Accessibility Feedback: Turn Off Continuous Scrollingaccessibility HelpDokumen11 halamanSkip To Main Content Accessibility Feedback: Turn Off Continuous Scrollingaccessibility HelpbabaBelum ada peringkat
- Algal Growth in Photosynthetic Algal Microbial Fuel Cell and Its Subsequent Use For BiofuelsDokumen13 halamanAlgal Growth in Photosynthetic Algal Microbial Fuel Cell and Its Subsequent Use For BiofuelsKristopher Ray Simbulan PamintuanBelum ada peringkat
- Answers To Chapter 5: (In-Text & Asterisked Problems)Dokumen10 halamanAnswers To Chapter 5: (In-Text & Asterisked Problems)平野健太朗Belum ada peringkat
- A-Level Biology PDFDokumen44 halamanA-Level Biology PDFAshleigh NcubeBelum ada peringkat
- Catalog Life SciencesDokumen15 halamanCatalog Life SciencesSasmita NayakBelum ada peringkat
- Cactus (Opuntia Ficus-Indica) : A Review On Its Antioxidants Properties and Potential Pharmacological Use in Chronic DiseasesDokumen9 halamanCactus (Opuntia Ficus-Indica) : A Review On Its Antioxidants Properties and Potential Pharmacological Use in Chronic DiseasesAidBelum ada peringkat
- SD BIOLINE HIV 12 3.0 BrochureDokumen2 halamanSD BIOLINE HIV 12 3.0 BrochureDina Friance ManihurukBelum ada peringkat
- Glukoneogenesis: Prof - Dr. Suhartati, DR., MSDokumen25 halamanGlukoneogenesis: Prof - Dr. Suhartati, DR., MSDinda DhitaBelum ada peringkat
- 17-Chapter Manuscript-477-1-10-20200501Dokumen14 halaman17-Chapter Manuscript-477-1-10-20200501nikhilkapoor1999Belum ada peringkat
- 408 Pooja Shinde PROJECTDokumen35 halaman408 Pooja Shinde PROJECTPooja ShindeBelum ada peringkat
- Rashi - Effusion CytDokumen56 halamanRashi - Effusion CytShruthi N.RBelum ada peringkat
- Growth Kinetics of Oleaginous Yeast, Rhodosporidium Toruloides, in High Salinity ConditionDokumen79 halamanGrowth Kinetics of Oleaginous Yeast, Rhodosporidium Toruloides, in High Salinity ConditionShimme7Belum ada peringkat
- List of Video Lectures Available in Our Video BankDokumen25 halamanList of Video Lectures Available in Our Video Bankzeeshannajeeb80% (10)
- Mark Scheme (Results) October 2020: Pearson Edexcel International Advanced Subsidiary Level in Biology (WBI12) Paper 01Dokumen27 halamanMark Scheme (Results) October 2020: Pearson Edexcel International Advanced Subsidiary Level in Biology (WBI12) Paper 01Ahmad Luqman100% (2)
- Fine Test ELISA KitsDokumen376 halamanFine Test ELISA KitsDavid1002Belum ada peringkat
- Bio Set 1 (Answer Key)Dokumen5 halamanBio Set 1 (Answer Key)sajan161106Belum ada peringkat
- AdrwaDokumen19 halamanAdrwasnoopyboyBelum ada peringkat
- HKCEE - Biology - 1996 - Paper IDokumen9 halamanHKCEE - Biology - 1996 - Paper ICharlie Ng1216Belum ada peringkat
- Cutaneous Lymphomas PDFDokumen584 halamanCutaneous Lymphomas PDFPaulo Victor Amorim MarquesBelum ada peringkat
- B. Tech. Biotech Syllabus MDUDokumen51 halamanB. Tech. Biotech Syllabus MDUVineet50% (4)
- Midterms Reviewer Gee11Dokumen2 halamanMidterms Reviewer Gee11HarimasuBelum ada peringkat
- The Journey of Man A Genetic OdysseyDokumen7 halamanThe Journey of Man A Genetic OdysseylpinargotiBelum ada peringkat
- TTPB7THESTORYOFAUXIN ShortDokumen65 halamanTTPB7THESTORYOFAUXIN ShortDiksha GahlotBelum ada peringkat
- The Powers of The MindDokumen1 halamanThe Powers of The MindKen Walker100% (1)
- Phylogenetic TreesDokumen11 halamanPhylogenetic TreesManisha BishtBelum ada peringkat
- Kingdom ProtistsDokumen24 halamanKingdom ProtistsShankey Faith BediaBelum ada peringkat
- Christle Mangulabnan WebquestDokumen5 halamanChristle Mangulabnan WebquestChel MangulabnanBelum ada peringkat