Lap PPP Pssss
Diunggah oleh
rezadeptiaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Lap PPP Pssss
Diunggah oleh
rezadeptiaHak Cipta:
Format Tersedia
Trauma remains the leading cause of death worldwide and the leading cause of death in
those less than 44 years old in the United States. Admission to a verified trauma center has been
shown to decrease mortality following a major injury. This decrease in mortality has been a direct
result of improvements in the initial evaluation and resuscitation from injury as well as continued
advances in critical care. As such, it is vital that intensive care practitioners be familiar with various
types of injuries and their associated treatment strategies as well as their potential complications in
order to minimize the morbidity and mortality frequently seen in this patient population. Keywords
trauma, injury, critical care Introduction Trauma-associated death is the leading cause of death
worldwide and the leading cause of death in those younger than 44 years old in the United States.1
Because of this, death following injury is responsible for the greatest number of potential lives lost
from any single cause. Over the last 20 years, trauma systems have evolved and have been shown to
significantly lessen mortality following injury.2-4 This has been due to improvements in
transportation time from the point of injury to verified trauma centers, methodologies in the initial
approach to evaluation and resuscitation from injury, and ongoing critical care techniques that allow
time for the patient to recover. As such, it is vital that intensive care practitioners be familiar with
the approach to various types of severe injuries as well as their potential complications and
expected hospital course. Although an exhaustive review of these topics is beyond the scope of this
article, we seek to provide an overview of these topics with an emphasis on potential complications
that are especially germane to the critical care practitioner. Due to space restrictions, this article
concentrates on the medical management of injuries and does not address the role of surgery per
se. Herein, we present a case scenario and discuss treatment strategies with the supporting
evidence that are relevant to the intensivist. Case Scenario A 25-year-old female is admitted to the
intensive care unit (ICU) after falling 20 ft off of a bridge. On initial presentation, she was found to
have a Glasgow Coma Score (GCS) of 9 and was intubated and sedated. Her injuries include skull
fracture with a subdural and subarachnoid hemorrhage, large left pneumothorax with multiple
broken ribs and a flail chest, grade III splenic laceration without contrast extravasation or
hemoperitoneum on computed tomography (CT) scan, and an open right femur fracture. Trauma
surgery, neurological surgery, orthopedic surgery, and possibly interventional radiology, in addition
to the intensivist, are involved in this patient’s care, and coordination of the care plan is pivotal to
the patient’s survival. Airway Intubation and Ventilation Initial evaluation and resuscitation of the
patient with trauma in the emergency department traditionally follows the ‘‘ABCD’’ approach—
assessment of the airway, breathing, circulation, and gross neu
Anda mungkin juga menyukai
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- PediatricsDokumen312 halamanPediatricsمحمد ابو مناضل الافينش100% (1)
- MacroalbuminemiaDokumen4 halamanMacroalbuminemiailma_ilemBelum ada peringkat
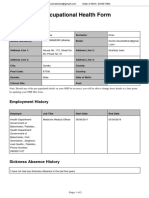
- Occupational Health Form: General DetailsDokumen2 halamanOccupational Health Form: General DetailsKhushal khanBelum ada peringkat
- WES Ablasi SVT AVRT - Travilla Bastian A. PangestutiDokumen1 halamanWES Ablasi SVT AVRT - Travilla Bastian A. PangestutiHervin RamadhaniBelum ada peringkat
- HNPDokumen47 halamanHNPSyifa RabiahBelum ada peringkat
- Major Depressive Disorder Symptoms and Prevalence For IB Abnormal PsychologyDokumen13 halamanMajor Depressive Disorder Symptoms and Prevalence For IB Abnormal PsychologychrissybissyBelum ada peringkat
- Nursing Care of A Hospitalized ChildDokumen17 halamanNursing Care of A Hospitalized ChildtinaBelum ada peringkat
- 2020 Anaphylaxis JACI 2020Dokumen42 halaman2020 Anaphylaxis JACI 2020Peter Albeiro Falla CortesBelum ada peringkat
- Diabetic Nephropathy BaruDokumen24 halamanDiabetic Nephropathy BaruRobiyanti Nur Chalifah HattaBelum ada peringkat
- EMR Documentation TemplatesDokumen25 halamanEMR Documentation TemplatesFlint Ray100% (1)
- WEVM Chapter 1Dokumen22 halamanWEVM Chapter 1Manoj KarkiBelum ada peringkat
- CortisolDokumen27 halamanCortisolCao YunBelum ada peringkat
- Talk by DR - Judy JeyakumarDokumen5 halamanTalk by DR - Judy JeyakumarKalmunai Mental Health AssociationBelum ada peringkat
- AttachmentDokumen39 halamanAttachmentshmlniz100% (1)
- Incision SitesDokumen4 halamanIncision SitesmidskiescreamzBelum ada peringkat
- Evidence-Based Guideline Summary: Evaluation, Diagnosis, and Management of Facioscapulohumeral Muscular DystrophyDokumen10 halamanEvidence-Based Guideline Summary: Evaluation, Diagnosis, and Management of Facioscapulohumeral Muscular DystrophyFitria ChandraBelum ada peringkat
- BIO 211 Chapter 18 AssignmentDokumen20 halamanBIO 211 Chapter 18 Assignmentf1l2o3r4e5n6Belum ada peringkat
- Tolak Angin TranslatedDokumen3 halamanTolak Angin TranslatedWadz MuharBelum ada peringkat
- Feeling GreatDokumen243 halamanFeeling GreatSunny LamBelum ada peringkat
- Eye Lids and Lacrimal System: Dr. Binto Akturusiano, SPMDokumen59 halamanEye Lids and Lacrimal System: Dr. Binto Akturusiano, SPMranz ibonkBelum ada peringkat
- Exercise #1 10Dokumen10 halamanExercise #1 10John Paul FloresBelum ada peringkat
- Lesson Plan On Post Natal ExercisesDokumen11 halamanLesson Plan On Post Natal Exercisesvarshasharma0593% (15)
- Acid Fast StainDokumen3 halamanAcid Fast StainMartina MicicBelum ada peringkat
- Medicina Chinesa JeremyDokumen2 halamanMedicina Chinesa JeremyJuan Gabriel CunhaBelum ada peringkat
- Elevated Levels of Bcl-3 Inhibits Treg Development and Function Resulting in Spontaneous ColitisDokumen14 halamanElevated Levels of Bcl-3 Inhibits Treg Development and Function Resulting in Spontaneous ColitisPaviliuc RalucaBelum ada peringkat
- SCE Practicaldiabetes - ElzohryDokumen107 halamanSCE Practicaldiabetes - ElzohryAE67% (3)
- EASL-GL Benign Tumor LiverDokumen13 halamanEASL-GL Benign Tumor LiveroliviaBelum ada peringkat
- Celiac DiseaseDokumen35 halamanCeliac DiseaseRye HanaBelum ada peringkat
- ApendikDokumen4 halamanApendikSepti AyaBelum ada peringkat
- 1.0 Thrombocytes SCDokumen10 halaman1.0 Thrombocytes SC西矢椛Belum ada peringkat