Etiology and Pathophysiology of Recurrent Aphthous Stomatitis: A Review
Diunggah oleh
Rebin AliDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Etiology and Pathophysiology of Recurrent Aphthous Stomatitis: A Review
Diunggah oleh
Rebin AliHak Cipta:
Format Tersedia
Arun Kumar M. et. al.
ETIOLOGY AND PATHOPHYSIOLOGY OF RECURRENT APHTHOUS STOMATITIS: A REVIEW
ETIOLOGY AND PATHOPHYSIOLOGY OF RECURRENT
APHTHOUS STOMATITIS: A REVIEW
IJCRR
Vol 06 issue 10 Arun Kumar M., Vasanthi Ananthakrishnan, Jaisri Goturu
Section: Healthcare
Category: Review Department of Physiology, M S Ramaiah Medical College and Teaching Hospitals,
Received on: 02/04/14
MSRIT post, MSR Nagar, Bangalore, KA, India
Revised on: 23/04/14
Accepted on: 12/05/14
E-mail of Corresponding Author: drarunkm@gmail.com
ABSTRACT
Recurrent aphthous stomatitis is the most common oral mucosal ulcer disease. It causes severe pain
and occurs repeatedly, causing discomfort in daily routine activities. The description of etiology is
varied and none of the explanations given so far are satisfactory. Clinically this condition presents itself
in three forms: major, minor and herpetiform ulcers. Causes for the ulcers could be related to host and /
or environment. Host factors include genetic, nutritional deficiency, immune dysregulation and stress
which can again be multifactorial. Environmental factors include trauma (both physical and chemical)
and infections. There are several clinical syndromes which are associated with RAS like Behcet’s
syndrome. There are several causes acting together in initiating formation of ulcer unlike a single
etiological factor as was thought previously. This means combination of host and environmental factors
are essential not only for triggering the ulcer but also for an increase in size. The severity of etiological
factors to which an individual is exposed would decide the type of ulcer. Identification of the trigger
for a particular individual seems to be important in management of the disease. Hence understanding
etiopathogenesis for recurrent aphthous stomatitis would be helpful in formulation of individualized
treatment modalities. This review is intended to understand the cause and pathogenesis of recurrent
aphthous stomatitis.
Keywords: Recurrent Aphthous Stomatitis, Oral Ulcers, RAS syndromes
INTRODUCTION in frequency and severity with age2. In about 80
Recurrent aphthous stomatitis (RAS) is a percent of patients with RAS, the condition
disease of the oral mucosa which appears typically develops before 30 years of age3.
as ulcers in the mouth and causes severe pain. Clinical Presentation
Repeated occurrence of ulcers is very debilitating. The ulcers are typically seen on the buccal
The prevalence, clinical presentation, etiology and mucosa, the labial mucosa, the floor of the mouth
pathogenesis of recurrent aphthous stomatitis will or the tongue. A prodrome of localized burning or
be discussed in this review. pain for 24 to 48 hours usually precedes the ulcers.
Prevalence of RAS (Recurrent aphthous The lesions are painful, with well defined margins
stomatitis) and shallow necrotic center. All ulcers have
RAS is a common oral mucosal condition and has yellow-grayish membrane at the base and are
been reported as affecting 20% of the general surrounded by raised margins and erythematous
population at any given time. It reaches a peak haloes. The pain is severe and gets aggravated on
of50% in selected populations such as university eating, swallowing and speaking. The pain usually
students1. RAS usually appears first during persists for three to four days3.
childhood, with a tendency for ulcers to diminish
Int J Cur Res Rev, May 2014/ Vol 06 (10)
Page 16
Arun Kumar M. et. al. ETIOLOGY AND PATHOPHYSIOLOGY OF RECURRENT APHTHOUS STOMATITIS: A REVIEW
Three clinical presentations of RAS are: Minor throughout the entire oral cavity, including the soft
aphthous stomatitis (Minor or Mikulicz’saphthea palate, tonsillar areas, and oropharynx. The longer
or mild aphthous ulcers), Major aphthous duration simulates the malignant ulcer.
stomatitis (MjRAS or periadenitis Herpetiformulcers: They typically occur as crops
mucosanecrotica recurrence or Sutton’s disease) of multiple ulcers measuring less than 5mm which
and Herpetiform ulcers. may coalesce to form larger confluent areas of
Minor RAS: This is the commonest type of RAS ulceration, usually with marked erythema. They
and 75-85% of RAS are of this type. They last for 10-14 days but severity of pain is more
typically measure 5-10 mm in size, last for 10-14 than other forms. 5-10% of RAS are of this type.
days and heal without scarring. Followingthe They resemble ulcers of primary Herpes simplex
healing of the ulcers, there is a variable ulcer free virus (HSV) infection. The recurrence period may
intervalof about 3–4 weeks. be variable1,2.
Major RAS: They typically measure more than 10 Etiology ofRecurrent aphthous stomatitis:
mm in size, last for more than two weeks to There are many hypotheses that are put forth for
months and generally heal by scarring. 10-15% of the etiology of RAS. There is no conclusive
RAS are of this type. MjRAS may produce lesions evidence regarding the etiopathogenesis of RAS.
Host Factors: Environmental factors:
Genetic factors Microtrauma.
Food allergy Local trauma
Vitamin deficiency Chemicalinjury or physical trauma.
Immune dysregulations Infections
Physical or emotional stress Smoking
1. Genetic Factors: Field and Allan in 2003 patients with RAS who previously were
described that there is a genetic predisposition diagnosed in patch tests as reactive to agents
for RAS and more than 40% of affected such as benzoic acid, 50% showed clinical
individuals have first degree relatives with improvement when certain foods were
RAS2. Scully et al 2004 found that the excluded from the diet8.
likelihood of RAS is 90% when both parents 3. Vitamin Deficiency: Hematinic (iron, folic
are affected, but only 20 % when neither parent acid, vitamins B-6 and B-12) deficiencies were
has RAS. A family history of recurrent twice as common in patients with RAS9. As
aphthous ulcers is evident in some patients. A many as 20% patients with RAS had a
familial connection includes a young age of hematinic deficiency. Lower dietary intake of
onset and symptoms of increased severity. folate and vitamin B-12 is more common
Recurrent aphthous ulcers are highly correlated among persons with aphthous ulcers and
in identical twins4. HLA subtypes like HLA treatment with 1000 mcg/d has shown benefit
B-515, HLA-B52, HLA-B446, HLA-DRW10 in individuals regardless of serum vitamin B-
and DQW17 antigens were found to be closely 12 levels10. A small group of adolescents were
associated with RAS. shown to have reduced incidence and pain
2. Nutrition: Foods such as chocolate, coffee, from RAS when given 2000 mg/d of ascorbic
peanuts, cereals, almonds, strawberries, cheese, acid11.
tomatoes (even the skin of the tomatoes) and 4. Immune Dysregulations: Immune
wheat flour (containing gluten) may be dysregulations may play a significant role but
implicated in some patients. In one study of no conclusive evidence has been noted.
Int J Cur Res Rev, May 2014/ Vol 06 (10)
Page 17
Arun Kumar M. et. al. ETIOLOGY AND PATHOPHYSIOLOGY OF RECURRENT APHTHOUS STOMATITIS: A REVIEW
Cytotoxic action of lymphocytes and initiated to determine whether standardized
monocytes on the oral epithelium seems to mechanical injury would lead to ulcers in
cause the ulceration, but the trigger remains patients prone to aphthous stomatitis when
unclear. Upon histologic analysis, RAS compared with normal controls. In this study
consists of mucosal ulcerations with mixed experimental biopsies failed to disclose any
inflammatory cell infiltrates. T-helper cells histological differences between mechanically
predominate in the pre-ulcerative and healing induced and spontaneous ulcers21.
phases, whereas T-suppressor cells 6. Physical or Psychological stress:
12
predominate in the ulcerative phase . Psychological stress may play a role in the
There is reduced response of patients' manifestation of recurrent aphthous stomatitis
lymphocytes to mitogens. There may be as a trigger or a modifying factor22. No studies
alterations in the activity of natural killer cells have conclusively proved stress as a causative
in various stages of disease13. Increased or precipitating factor for RAS.
adherence of neutrophils and reduced 7. Infections: The possible immunopathological
quantities and functionality of regulatory T destruction of oral mucosa by viridian
cells in tissue with lesions and release of tumor streptococci was under consideration until
necrosis factor-alpha (TNF-alpha) is seen14. 1986 but was disproved23.Streptococcus
There is significant involvement of mast cells sanguisor its L-form has been implicated, as
in the pathogenesis of RAS. Reduced cellular has autoimmunity to the oral mucosal
expression of heat shock protein 27 and homogenate. A common or cross-reactive
interleukin 10is seen15 in aphthous lesions16. antigen between streptococci and oral
There is an increase in the Toll-like receptor epithelium has been suggested and
activity in RAS17. Oxidative stress markers demonstrated between the streptococcal 60–65
(glutathione and malondialdehyde) show kD heat shock protein (HSP) and oral mucosal
altered levels and impaired balance18. Serum tissue. Significant increase in serum antibodies
IgE levels were found to be increased in RAS to HSP has been detected in patients with
patients by several investigators. Scully et al RAS24. Helicobacter pylori has been detected
reported that increased IgE concentrations in lesional tissue of oral ulcers, but the
might be related to cell-mediated phenomena frequency of serum immunoglobulin G
in the immunopathogenesis of RAS. antibodies to H pylori is not increased in
The expression of protein C, protein S and D- recurrent aphthous ulcers, and the organisms
dimer were increased, while t-PA (tissue have never proven causative25,26.
plasminogen activator) was reduced in patients 8. Tobacco smoking: Patients suffering from
with RAS and Behcet‘s disease. Remarkably, RAS usually are nonsmokers, and there is a
the expression of PAI-1(Platelet activator lower prevalence and severity of RAS among
inhibitor-1) was significantly elevated in both heavy smokers as opposed to moderate
Behcet’s Disease and RAS patients compared smokers. Some patients report an onset of RAS
with that in healthy controls19. The results after smoking cessation, while others report
suggest the abnormal fibrinolytic activity is control on re-initiation of smoking. The use of
due to increased inhibition of tissue smokeless tobacco is associated with a
plasminogen activator20. significantly lower prevalence of RAS.
5. Trauma: Local trauma may play a role in Nicotine-containing tablets also appear to
initiating the mucosal injury which leads to control the frequency of RAS27.
ulcers in patients with RAS. This study was
Int J Cur Res Rev, May 2014/ Vol 06 (10)
Page 18
Arun Kumar M. et. al. ETIOLOGY AND PATHOPHYSIOLOGY OF RECURRENT APHTHOUS STOMATITIS: A REVIEW
Recurrent aphthous stomatitis Associated by fever, neutrophil leukocytosis,
Syndromes erythematous skin plaques or nodules and,
i. Behcet’s disease (BD) is a multisystemic, often, classical RAS. It may occur in
chronic, relapsing vasculitis that affects nearly conjunction with malignant conditions, such as
all organs and systems. It is associated with leukemia2.
multiple oral, genital ulcers, arthritis, vi. Celiac disease (CD) is caused by gluten
hematemesis, melena, and epigastric pain as sensitivity of the small intestines. According to
predominant manifestations. Seung-Ho Rhee et study by SelimAydemir et al 2004 the CD
al 2005 in their study described that RAS and prevalence (40%) in patients with RAS is
BD had similar presenting symptoms like oral higher than in the normal population. It is also
lesions and abdominal pain. There was no described that RAS may be the presenting sign
clinical, endoscopical, histopathologicalor of the disease and may be used as a marker for
serological difference between patients with the CD31.
intestinal BD, RAS and healthy volunteers in vii. Crohn’s disease: The intraoral involvement
Anti-Neutrophil Cytoplasmic Antibodies in Crohn’s disease (CD) is observed in
28
(pANCA) . approximately 9% of cases and oral
ii. RAS is a part of PFAPA syndrome which inflammation precedes intestinal symptoms in
includes the Periodic Fever, Aphthous about 60% of these patients. Hence it is
stomatitis, Pharyngitis and cervical Adenitis. important to consider the differential diagnosis
PFAPA syndrome is regarded as a non- of Crohn’s disease in subjects with intestinal
hereditary disease of unknown etiology symptoms and RAS32.
although the clinical observation is that, in a
small proportion of cases, one of the parents or Pathophysiology of Recurrent aphthous
a more distant relative had similar symptoms stomatitis:
in childhood29. The complex interactions of various etiological
iii. MAGIC syndrome: Mouth And Genital factors together can trigger ulcer formation.
ulcers with Inflamed Cartilage syndrome (also Etiological factors can be classified into
known as "MAGIC syndrome") is a cutaneous predisposing factors and precipitating /
condition2. triggering factors. The factors like HLA
iv. Imerslund-Grasbeck syndrome (IGS) is associations, immune dysregulation, nutritional
characterized by Juvenile megaloblastic deficiency, personality type A are the
anemia due to vitamin B12 deficiency and predisposing factors. Microtrauma, infections,
proteinuria. All the three cases of Imerslund- stress could be the initiating or triggering
Grasbeck syndrome described in the study factor for ulcer formation.
ArnonBroides et al 2006 were associated with Those individuals who are susceptible when
RAS. Though it was described that defective exposed to the triggering factors for certain
neutrophil phagocytosis and neutropenia duration tend to develop ulcers. Based on the
caused by the Vitamin B12 deficiency may be intensity and duration of the triggering factors,
the possible mechanism for the causation of ulcer starts growing till the factors are
stomatitis, none of the patients had removed. Pain suffered by the patients is
neutropenia. The cause of RAS in IGS was directly proportional to the size of the ulcer
inconclusive30. and severity of the triggering factors. For
v. Sweet’s syndrome, also known as acute example the serum cortisol level: which is a
febrile neutrophilicdermatosis, is characterized biomarker of the stress was increased in the
Int J Cur Res Rev, May 2014/ Vol 06 (10)
Page 19
Arun Kumar M. et. al. ETIOLOGY AND PATHOPHYSIOLOGY OF RECURRENT APHTHOUS STOMATITIS: A REVIEW
subjects with RAS and the increase was stomatitis: A consensus approach. J Am
directly proportional to the ulcer size33. Dent Assoc 2004; 134: 200–207.
4. Miller MF, Garfunkel AA, Ram C, Ship II.
CONCLUSION Inheritance patterns in recurrent aphthous
Recurrent aphthous stomatitis or aphthous ulcers: twin and pedigree data. Oral Surg
ulcers are more common in younger adults. Med Oral Pathol. Jun 1977;43(6):886-91.
There are several causes that have been 5. Mustafa Özdemir1, HasanAcar et al. HLA-
explained for ulcer formation but no single B51 in Patients with Recurrent Aphthous
cause is definitive. The cause is still non- Stomatitis. ActaDermato-Venereologica.
specific. There are multiple factors which may 2008: 203-203.
be acting together in a complex manner in 6. LutfiJaber, Abraham Weinberger, Tirza
initiating the formation of ulcer unlike a single Klein, Isaac Yaniv, Mukamel. Close
etiological factor as was thought previously. Association of HLA-B52 and HLA-B44
This means a combination of host and Antigens in Israeli Arab Adolescents with
environmental factors are essential not only for Recurrent Aphthous Stomatitis. Arch
triggering the ulcer but also for an increase in Otolaryngol Head Neck Surg. 2001;
size. The severity of etiological factors to 127(2):184-187.
which an individual is exposed would decide 7. Wilhelmsen NS, Weber R, Monteiro F,
the type of ulcer. Underlying mechanisms Kalil J, Miziara ID. Correlation between
relating to pathogenesis need to be explored histocompatibility antigens and recurrent
inorder to establish the treatment protocol. aphthous stomatitis in the Brazilian
population. Braz J Otorhinolaryngol. May-
ACKNOWLEDGEMENT Jun 2009;75(3):426-31.
Authors acknowledge the immense help 8. Zuzanna Ślebioda1, Elżbieta Szponar1,
received from the scholars whose articles Anna Kowalska. Recurrent aphthous
are cited and included in references of this stomatitis: genetic aspects of etiology.
manuscript. The authors are also grateful to PostępyDermatologii i Alergologii XXX
authors / editors / publishers of all those 2013;2 :96-102
articles, journals and books from where the 9. Kozlak ST, Walsh SJ, Lalla RV. Reduced
literature for this article has been reviewed dietary intake of vitamin B12 and folate in
and discussed. patients with recurrent aphthous stomatitis.
J Oral Pathol Med. Feb 7 2010;
REFERENCES 10. Carrozzo M. Vitamin B12 for the treatment
1. Ship JA, Chavez EM, Doerr PA, Henson of recurrent aphthous stomatitis. Evid Based
BS, Sarmadi M. Recurrent aphthous Dent. 2009;10(4):114-115.
stomatitis. Quintessence Int. 2000; 11. Yasui K, Kurata T, Yashiro M, Tsuge M,
31(2):95-112. Ohtsuki S, Morishima T. The effect of
2. E. A. Field & R. B. Allan. Oral ulceration – ascorbate on minor recurrent aphthous
aetiopathogenesis, clinical diagnosis and stomatitis. ActaPaediatr. 2009; 99 (3): 442-
management in the gastrointestinal clinic. 445.
Aliment PharmacolTher 2003; 18: 949–962. 12. Rogers III RS. Recurrent aphthous
3. Scully C, Gorsky M, Lozada. The diagnosis stomatitis: Clinical characteristics and
and management of recurrent aphthous evidence for an immunopathogenesis. J
Invest Dermatol. 1977; 69: 499-509.
Int J Cur Res Rev, May 2014/ Vol 06 (10)
Page 20
Arun Kumar M. et. al. ETIOLOGY AND PATHOPHYSIOLOGY OF RECURRENT APHTHOUS STOMATITIS: A REVIEW
13. Sun A, Chu CT, Wu YC, Yuan JH. initiating recurrent aphthous stomatitis.
Mechanisms of depressed natural killer cell British Medical Journal 1981; 283: 1569-
activity in recurrent aphthous ulcers. 1570.
ClinImmunolImmunopathol. Jul 1991; 22. Camila de Barros Gallo, Maria Angela
60(1):83-92. Martins Mimura, Norberto Nobuo Sugaya.
14. Taylor LJ, Bagg J, Walker DM, Peters TJ. Psychological stress and recurrent aphthous
Increased production of tumour necrosis stomatitis. Clinics 2009; 64(6):645-648.
factor by peripheral blood leukocytes in 23. Hoover, J. A. Olson, J. S. Greenspan.
patients with recurrent oral aphthous Humoral Responses and Cross-reactivity to
ulceration. J Oral Pathol Med. Jan 1992; Viridans Streptococci in Recurrent
21(1):21-5. Aphthous Ulceration. J Dent Res 1986;
15. Hasan A, Childerstone A, Pervin K, et al. 65(8):1101-1104.
Recognition of a unique peptide epitope of 24. A Hasan, A Childerstone, K Pervin, et al.
the mycobacterial and human heat shock Recognition of a unique peptide epitope of
protein 65-60 antigen by T cells of patients the mycobacterial and human heat shock
with recurrent oral ulcers. protein 65-60 antigen by T cells of patients
ClinExpImmunol. Mar 1995;99(3):392-7. with recurrent oral ulcers.
16. Miyamoto NT Jr, Borra RC, Abreu M, ClinExpImmunol. 1995; 99(3): 392–397.
Weckx LL, Franco M. Immune-expression 25. Birek C, Grandhi R, McNeill K, Singe;r D,
of HSP27 and IL-10 in recurrent aphthous Ficarra G, Bowden G. Detection of
ulceration. J Oral Pathol Med. Sep Helicobacter pylori in oral aphthous ulcers.
2008;37(8):462-7. J Oral Pathol Med. May 1999;28(5):197-
17. Borra RC, de Mesquita Barros F, de 203.
Andrade Lotufo M, Villanova FE, Andrade 26. Elsheikh MN, Mahfouz ME. Prevalence of
PM. Toll-like receptor activity in recurrent Helicobacter pylori DNA in recurrent
aphthous ulceration. J Oral Pathol Med. aphthous ulcerations in mucosa-associated
Mar 2009;38(3):289-98. lymphoid tissues of the pharynx. Arch
18. Arikan S, Durusoy C, Akalin N, Haberal A, Otolaryngol Head Neck Surg 2005;131(9):
Seckin D. Oxidant/antioxidant status in 804-808.
recurrent aphthous stomatitis. Oral Dis. Oct 27. KamileMarakoğlu&RecepErolSezeret al.
2009; 15(7):512-5. Recurrentaphthous stomatitis frequency in
19. Seung-Ho Rhee, Young-Bae Kim, Eun-So the smoking cessation people: Clin Oral
Lee. Comparison of Behcet’s Disease and Invest 2007; 11:149–153.
Recurrent Aphthous Ulcer according to 28. Seung-Ho Rhee, Young-Bae Kim, Eun-So
Characteristics of Gastrointestinal Lee. Comparison of Behcet’s Disease and
Symptoms. J Korean Med Sci 2005; 20: Recurrent Aphthous Ulcer according to
971-6. Characteristics of Gastrointestinal
20. Hong Shang, Jingjing Ye, Min Ji. Symptoms. J Korean Med Sci 2005; 20:
Anticoagulant and Fibrinolytic Disorders in 971-6.
Patients with Behçet’s Disease and 29. Kelly L Brown1, Per Wekell et al., Profile
Recurrent Aphthous Ulcer. Chinese Journal of blood cells and inflammatory mediators
of Physiology 2011; 54:1-6. in periodic fever, aphthous stomatitis,
21. David Wray, Edward A Graykowski, Abner pharyngitis and adenitis (PFAPA)
Louis Notkins. Role of mucosal injury in syndrome: BMC Pediatrics 2010, 10:65.
Int J Cur Res Rev, May 2014/ Vol 06 (10)
Page 21
Arun Kumar M. et. al. ETIOLOGY AND PATHOPHYSIOLOGY OF RECURRENT APHTHOUS STOMATITIS: A REVIEW
30. ArnonBroides, Baruch Yerushalmi, Rachel 32. Roy S. Rogers III.Recurrent aphthous
Levy et al. Imerslund-Grasbeck Syndrome stomatitis: Clinical characteristics and
Associated With Recurrent Aphthous associated systemic disorders. Seminars in
Stomatitis and Defective Neutrophil Cutaneous Medicine and Surgery 1997; 16
Function. J PediatrHematolOncol 2006: (4): 278-283.
28(11); 715-720. 33. Arunkumar M, VasanthiAnanthakrishnan,
31. SelimAydemir, NilgünSolakTekin, JaisriGoturu. Role of Serum Cortisol in
ErolAktunç et al. Celiac disease in patients Recurrent Aphthous Stomatitis.
having recurrent aphthous Stomatitis. Turk Biomedicine 2012, 32(3), 331-336.
J Gastroenterol 2004; 15 (3): 192-195.
Int J Cur Res Rev, May 2014/ Vol 06 (10)
Page 22
Anda mungkin juga menyukai
- 11 Recurrent Aphthous Stomatitis Caused by Food AllergyDokumen6 halaman11 Recurrent Aphthous Stomatitis Caused by Food AllergyramaBelum ada peringkat
- Recurrent Aphthous Stomatitis e Etiology, Serum Autoantibodies, Anemia, Hematinic Deficiencies, and ManagementDokumen11 halamanRecurrent Aphthous Stomatitis e Etiology, Serum Autoantibodies, Anemia, Hematinic Deficiencies, and ManagementorizaBelum ada peringkat
- Koberova. 2020. RAS in ChildrenDokumen5 halamanKoberova. 2020. RAS in ChildrenRachel RoselanyBelum ada peringkat
- Essentials of Recurrent Aphthous Stomatitis (Review)Dokumen4 halamanEssentials of Recurrent Aphthous Stomatitis (Review)Akun TerorBelum ada peringkat
- Recurrent Aphthous Ulcerative Disease: Presentation and ManagementDokumen6 halamanRecurrent Aphthous Ulcerative Disease: Presentation and ManagementOfier SikiBelum ada peringkat
- T SridharDokumen7 halamanT SridharmutiaBelum ada peringkat
- Comparing The Effect of Injectable Vitamin B WithDokumen6 halamanComparing The Effect of Injectable Vitamin B WithRisa SasmitaBelum ada peringkat
- Recurrent Aphthous Stomatitis: Genetic Aspects of EtiologyDokumen7 halamanRecurrent Aphthous Stomatitis: Genetic Aspects of EtiologygeadisBelum ada peringkat
- Recurrent Aphthous Stomatitis Current Concepts inDokumen6 halamanRecurrent Aphthous Stomatitis Current Concepts indaniel_siitompulBelum ada peringkat
- Aphthous Ulceration PDFDokumen8 halamanAphthous Ulceration PDFpaolaBelum ada peringkat
- Recurrent Aphthous Stomatitis - A Review: S. Leena Sankari, K.M.K. Masthan, N.Aravindha Babu and C. PriyadharsiniDokumen7 halamanRecurrent Aphthous Stomatitis - A Review: S. Leena Sankari, K.M.K. Masthan, N.Aravindha Babu and C. PriyadharsiniFadli FadelBelum ada peringkat
- DE1 RA AbdulrehmanDokumen9 halamanDE1 RA Abdulrehmanzuhai martinusBelum ada peringkat
- Recurrent Aphthous Stomatitis: Sunday O. Akintoye, BDS, DDS, MS, Martin S. Greenberg, DDSDokumen17 halamanRecurrent Aphthous Stomatitis: Sunday O. Akintoye, BDS, DDS, MS, Martin S. Greenberg, DDSAngga NugrohoBelum ada peringkat
- DownloadDokumen6 halamanDownloadGeorgi GugicevBelum ada peringkat
- Intro About Aphthous UlcersDokumen11 halamanIntro About Aphthous UlcersSuraj AroteBelum ada peringkat
- A Comprehensive Review On Aphthous Stomatitis Its Types Management and Treatment AvailableDokumen8 halamanA Comprehensive Review On Aphthous Stomatitis Its Types Management and Treatment AvailabledelfBelum ada peringkat
- Sar DDDokumen5 halamanSar DD26 ThufailBelum ada peringkat
- Etiological Factors of Recurrent Aphthous Stomatitis: A Common PerplexityDokumen5 halamanEtiological Factors of Recurrent Aphthous Stomatitis: A Common PerplexityRebin AliBelum ada peringkat
- Akintoye2014 SariawanDokumen17 halamanAkintoye2014 SariawanHokeBelum ada peringkat
- Karan Synopsis CLG Apt - UlcDokumen23 halamanKaran Synopsis CLG Apt - UlcAnil Subhash RathodBelum ada peringkat
- Recurrent Aphthous Stomatitis: A ReviewDokumen7 halamanRecurrent Aphthous Stomatitis: A ReviewintanBelum ada peringkat
- Pharmacological Management of Common Soft Tissue Lesions of The Oral CavityDokumen16 halamanPharmacological Management of Common Soft Tissue Lesions of The Oral CavityAcisum2Belum ada peringkat
- Oral ManifestationDokumen18 halamanOral ManifestationDokterGigiBelum ada peringkat
- Clinical Practice Guidelines For Management of Recurrent Aphthous StomatitisDokumen9 halamanClinical Practice Guidelines For Management of Recurrent Aphthous Stomatitislauren pangestuBelum ada peringkat
- NIH Public Access: Recurrent Aphthous StomatitisDokumen22 halamanNIH Public Access: Recurrent Aphthous StomatitisRebin AliBelum ada peringkat
- PRD 12262Dokumen12 halamanPRD 12262Roxana OneaBelum ada peringkat
- Periodontology 2000 - 2019 - Bilodeau - Recurrent Oral Ulceration Etiology Classification Management and DiagnosticDokumen12 halamanPeriodontology 2000 - 2019 - Bilodeau - Recurrent Oral Ulceration Etiology Classification Management and DiagnosticCarlos Iván Cota ZavalaBelum ada peringkat
- Recurrent Aphthous Stomatitis: Preeti L, Magesh KT, Rajkumar K, Raghavendhar KarthikDokumen5 halamanRecurrent Aphthous Stomatitis: Preeti L, Magesh KT, Rajkumar K, Raghavendhar KarthikKen LewBelum ada peringkat
- Arduino 2017Dokumen8 halamanArduino 2017neetika guptaBelum ada peringkat
- Translate JR OMDokumen10 halamanTranslate JR OMMazaya Haekal IIBelum ada peringkat
- Sjögren's Syndrome: From Pathogenesis To Novel Therapeutic TargetsDokumen5 halamanSjögren's Syndrome: From Pathogenesis To Novel Therapeutic TargetsOcha24 TupamahuBelum ada peringkat
- Treatment of Zollinger Ellison SyndromeDokumen10 halamanTreatment of Zollinger Ellison SyndromeDwiek RuqoyahBelum ada peringkat
- Diagnosis and Management of Recurrent Herpetiform Stomatitis and Behçet Syndrome Like Recurrent Aphthous Stomatitis Herpetiform TypeDokumen8 halamanDiagnosis and Management of Recurrent Herpetiform Stomatitis and Behçet Syndrome Like Recurrent Aphthous Stomatitis Herpetiform TypeFahmil AgungBelum ada peringkat
- Fast Facts: Inflammatory Bowel Disease: Translating the science into compassionate IBD careDari EverandFast Facts: Inflammatory Bowel Disease: Translating the science into compassionate IBD careBelum ada peringkat
- A PH Thous UlcersDokumen23 halamanA PH Thous UlcersGindi Cinintia AsmarantakaBelum ada peringkat
- Recurrent Aphthous Stomatitis Genetic Aspects of EtiologyDokumen7 halamanRecurrent Aphthous Stomatitis Genetic Aspects of EtiologyHayu Qommaru ZalaBelum ada peringkat
- Effect of Stressful Life Events On The Onset and Duration of Recurrent Aphthous StomatitisDokumen5 halamanEffect of Stressful Life Events On The Onset and Duration of Recurrent Aphthous StomatitisFajar RamadhanBelum ada peringkat
- Case Report: Amoxycillin and Clavulanic Acid Induced Stevens-Johnson Syndrome: A Case ReportDokumen4 halamanCase Report: Amoxycillin and Clavulanic Acid Induced Stevens-Johnson Syndrome: A Case ReportEkaAriawanBelum ada peringkat
- Review Article: Oral Ulceration - Aetiopathogenesis, Clinical Diagnosis and Management in The Gastrointestinal ClinicDokumen14 halamanReview Article: Oral Ulceration - Aetiopathogenesis, Clinical Diagnosis and Management in The Gastrointestinal ClinicAmira KaddouBelum ada peringkat
- Aphthous Stomatitis - Background, Pathophysiology, EpidemiologyDokumen8 halamanAphthous Stomatitis - Background, Pathophysiology, EpidemiologyRizalRyamizardBelum ada peringkat
- Bacteriology, Histopathology, Sequelae and Pathogenesis of Oral Mucosal LesionsDokumen24 halamanBacteriology, Histopathology, Sequelae and Pathogenesis of Oral Mucosal LesionsVijetha RaiBelum ada peringkat
- Eficacy of Cryotherapy in The Prevention of Oral Mucosistis inDokumen15 halamanEficacy of Cryotherapy in The Prevention of Oral Mucosistis inPaola GilBelum ada peringkat
- Disentri AmubaDokumen8 halamanDisentri AmubaVivi DeviyanaBelum ada peringkat
- Lack of Association Between Celiac Disease and Dental Enamel HypoplasiaDokumen6 halamanLack of Association Between Celiac Disease and Dental Enamel HypoplasiaLjubomirErdoglijaBelum ada peringkat
- Occurrence of Recurrent Aphthous Stomatitis (RAS) As A Rare Oral Manifestation in A Patient With Gilbert's SyndromeDokumen5 halamanOccurrence of Recurrent Aphthous Stomatitis (RAS) As A Rare Oral Manifestation in A Patient With Gilbert's SyndromeDinesh RokayaBelum ada peringkat
- Impetigo and Scabies e Disease Burden and Modern Treatment StrategiesDokumen7 halamanImpetigo and Scabies e Disease Burden and Modern Treatment StrategiesHandy NugrahaBelum ada peringkat
- Diagnosis of Hirschsprung Disease: Lusine Ambartsumyan, Caitlin Smith, and Raj P KapurDokumen15 halamanDiagnosis of Hirschsprung Disease: Lusine Ambartsumyan, Caitlin Smith, and Raj P KapurGhina Mauizha WulandariBelum ada peringkat
- 3 Focal Infection of Periodontal Origin 2019Dokumen3 halaman3 Focal Infection of Periodontal Origin 2019fhiraBelum ada peringkat
- Gastroenterology For General SurgeonsDari EverandGastroenterology For General SurgeonsMatthias W. WichmannBelum ada peringkat
- Medical Hypotheses: M. P Arssinen, H. J Asberg, J.J.W. Mikkonen, A.M. KullaaDokumen4 halamanMedical Hypotheses: M. P Arssinen, H. J Asberg, J.J.W. Mikkonen, A.M. Kullaafkg unand 16Belum ada peringkat
- 46 Gruden PokupecDokumen3 halaman46 Gruden PokupecdrgozanBelum ada peringkat
- Hallopeau 10.1001@jamadermatol.2019.3515Dokumen1 halamanHallopeau 10.1001@jamadermatol.2019.3515Faten HayderBelum ada peringkat
- Muco-Cutaneous & Aphthous UlcerDokumen7 halamanMuco-Cutaneous & Aphthous Ulcerربيد احمد مثنى يحيى كلية طب الاسنان - جامعة عدنBelum ada peringkat
- Ep 3Dokumen10 halamanEp 3Mădălina ŞerbanBelum ada peringkat
- Efficacy of Steroidal Vs Non-Steroidal Agents in Oral Lichen Planus: A Randomised, Open-Label StudyDokumen9 halamanEfficacy of Steroidal Vs Non-Steroidal Agents in Oral Lichen Planus: A Randomised, Open-Label StudyRetno ManggalihBelum ada peringkat
- PemfigusDokumen5 halamanPemfigusSherlyBelum ada peringkat
- Diagnosis and Management of Autoimmune Hepatitis: A Clinical GuideDari EverandDiagnosis and Management of Autoimmune Hepatitis: A Clinical GuideMark W. RussoBelum ada peringkat
- Herbal Remedies For Mouth Ulcer: A Review: KeywordsDokumen7 halamanHerbal Remedies For Mouth Ulcer: A Review: KeywordsumapBelum ada peringkat
- Herbal Remedies For Mouth Ulcer: A Review: KeywordsDokumen7 halamanHerbal Remedies For Mouth Ulcer: A Review: KeywordsumapBelum ada peringkat
- Thickness and Marking Quality of Different Occlusal Contact Registration StripsDokumen6 halamanThickness and Marking Quality of Different Occlusal Contact Registration StripsRebin AliBelum ada peringkat
- Bite Force Measurement System Using Pressure-Sensitive Sheet and Silicone Impression MaterialDokumen7 halamanBite Force Measurement System Using Pressure-Sensitive Sheet and Silicone Impression MaterialRebin AliBelum ada peringkat
- Accurate Diagnosis of Occlusal Carious Lesions - A Stereo Microscope Evaluation of Clinical DiagnosisDokumen6 halamanAccurate Diagnosis of Occlusal Carious Lesions - A Stereo Microscope Evaluation of Clinical DiagnosisRebin AliBelum ada peringkat
- BD MarpeDokumen7 halamanBD MarpeRebin AliBelum ada peringkat
- In Vitro Study of White Spot Lesion: Maxilla and Mandibular TeethDokumen9 halamanIn Vitro Study of White Spot Lesion: Maxilla and Mandibular TeethRebin AliBelum ada peringkat
- Evaluation of Virtual Models (3shape Ortho System) in Assessing Accuracy and Duration of Model Analyses Based On The Severity of CrowdingDokumen8 halamanEvaluation of Virtual Models (3shape Ortho System) in Assessing Accuracy and Duration of Model Analyses Based On The Severity of CrowdingRebin AliBelum ada peringkat
- Export Price List: Straight MaterialDokumen4 halamanExport Price List: Straight MaterialRebin AliBelum ada peringkat
- Name Age Sex Occupation Systemic DiseaseDokumen10 halamanName Age Sex Occupation Systemic DiseaseRebin AliBelum ada peringkat
- Lichen Plan UsDokumen26 halamanLichen Plan UsRebin AliBelum ada peringkat
- Occupation Sex Crosstabulation SexDokumen10 halamanOccupation Sex Crosstabulation SexRebin AliBelum ada peringkat
- Ubc 2009 Spring Straga RobertDokumen8 halamanUbc 2009 Spring Straga RobertRebin AliBelum ada peringkat
- Table of ContentDokumen6 halamanTable of ContentRebin AliBelum ada peringkat
- RecommendationDokumen1 halamanRecommendationRebin AliBelum ada peringkat
- Etiological Factors of Recurrent Aphthous Stomatitis: A Common PerplexityDokumen5 halamanEtiological Factors of Recurrent Aphthous Stomatitis: A Common PerplexityRebin AliBelum ada peringkat
- NIH Public Access: Recurrent Aphthous StomatitisDokumen22 halamanNIH Public Access: Recurrent Aphthous StomatitisRebin AliBelum ada peringkat
- Appliance Design: Commonly Used Appliance DesignsDokumen7 halamanAppliance Design: Commonly Used Appliance DesignsRebin AliBelum ada peringkat
- Lec - 2 - Z, Double Z, T SpringDokumen4 halamanLec - 2 - Z, Double Z, T SpringRebin Ali100% (1)
- Appliance Design Lec. 1 2017Dokumen6 halamanAppliance Design Lec. 1 2017Rebin AliBelum ada peringkat
- Canine RetractorDokumen19 halamanCanine RetractorRebin AliBelum ada peringkat
- Book 1Dokumen1 halamanBook 1Rebin AliBelum ada peringkat
- Ubc 2009 Spring Straga RobertDokumen8 halamanUbc 2009 Spring Straga RobertRebin AliBelum ada peringkat
- 791651.annals of Anatomy 2016Dokumen5 halaman791651.annals of Anatomy 2016Rebin AliBelum ada peringkat
- Prof Chase B. Wrenn - The True and The Good - A Strong Virtue Theory of The Value of Truth-Oxford University Press (2024)Dokumen196 halamanProf Chase B. Wrenn - The True and The Good - A Strong Virtue Theory of The Value of Truth-Oxford University Press (2024)Mihaela DodiBelum ada peringkat
- Rights As Bribes ResaltadoDokumen89 halamanRights As Bribes ResaltadoAndresAmarillaBelum ada peringkat
- Emotional Intelligence - WikipediaDokumen10 halamanEmotional Intelligence - WikipediaJellie MendozaBelum ada peringkat
- LEC 2017 - Post-Test in Organized Crime InvesDokumen8 halamanLEC 2017 - Post-Test in Organized Crime InvesBokhary Dimasangkay Manok EliasBelum ada peringkat
- Precision Nutrition. Nutrient TimingDokumen21 halamanPrecision Nutrition. Nutrient TimingPaolo AltoéBelum ada peringkat
- Bago Project CharterDokumen6 halamanBago Project CharterLarize BautistaBelum ada peringkat
- Republic Act No. 1125Dokumen8 halamanRepublic Act No. 1125Jazlynn WongBelum ada peringkat
- Muzakarah Jawatankuasa Fatwa Majlis Kebangsaan Bagi Hal Ehwal Ugama Islam Malaysia Kali KeDokumen7 halamanMuzakarah Jawatankuasa Fatwa Majlis Kebangsaan Bagi Hal Ehwal Ugama Islam Malaysia Kali KeSiti Zubaidah ZulkhairieBelum ada peringkat
- DocumentDokumen4 halamanDocumentJuliana ZamorasBelum ada peringkat
- Physical Education: Learning Activity SheetDokumen13 halamanPhysical Education: Learning Activity SheetRhea Jane B. CatalanBelum ada peringkat
- 10 1108 - JKM 01 2020 0064Dokumen23 halaman10 1108 - JKM 01 2020 0064BBA THESISBelum ada peringkat
- 3rd Sunday After TrinityDokumen11 halaman3rd Sunday After TrinityHmkEnochBelum ada peringkat
- Revised Market Making Agreement 31.03Dokumen13 halamanRevised Market Making Agreement 31.03Bhavin SagarBelum ada peringkat
- The First Converts in Chin Hills - Ni Kong HongDokumen7 halamanThe First Converts in Chin Hills - Ni Kong HongLTTuangBelum ada peringkat
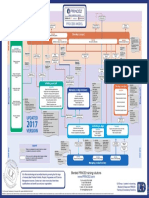
- p2 Process Model 2017Dokumen1 halamanp2 Process Model 2017Miguel Fernandes0% (1)
- Electrical Information: Service Training MechanikDokumen22 halamanElectrical Information: Service Training Mechanikfroilan ochoaBelum ada peringkat
- Figures of Speech StylisticsDokumen11 halamanFigures of Speech StylisticsCarmie Lactaotao DasallaBelum ada peringkat
- Xenophanes' ScepticismDokumen22 halamanXenophanes' Scepticismvince34Belum ada peringkat
- Curriculum Vitae: Lungnila Elizabeth School of Social Work, Senapati, Manipur August 2016-June 2018Dokumen4 halamanCurriculum Vitae: Lungnila Elizabeth School of Social Work, Senapati, Manipur August 2016-June 2018Deuel khualBelum ada peringkat
- Meralco v. CastilloDokumen2 halamanMeralco v. CastilloJoven CamusBelum ada peringkat
- Fanuc 10t Parameter Manual PDFDokumen1 halamanFanuc 10t Parameter Manual PDFadil soukri0% (2)
- Study On Perfromance Appraisal System in HPCLDokumen12 halamanStudy On Perfromance Appraisal System in HPCLomkinggBelum ada peringkat
- SSPC - Guia 12Dokumen6 halamanSSPC - Guia 12José Alvaro Herrera Ramos50% (2)
- Bottoms y Sparks - Legitimacy - and - Imprisonment - Revisited PDFDokumen29 halamanBottoms y Sparks - Legitimacy - and - Imprisonment - Revisited PDFrossana gaunaBelum ada peringkat
- Study On SantalsDokumen18 halamanStudy On SantalsJayita BitBelum ada peringkat
- Smith Vs CaDokumen11 halamanSmith Vs CaIrene QuimsonBelum ada peringkat
- Science Since BabylonDokumen224 halamanScience Since Babylonboris100% (1)
- Firewatch in The History of Walking SimsDokumen5 halamanFirewatch in The History of Walking SimsZarahbeth Claire G. ArcederaBelum ada peringkat
- Wulandari - Solihin (2016)Dokumen8 halamanWulandari - Solihin (2016)kelvinprd9Belum ada peringkat
- Calderon de La Barca - Life Is A DreamDokumen121 halamanCalderon de La Barca - Life Is A DreamAlexandra PopoviciBelum ada peringkat