Def Ronzo
Diunggah oleh
Lidyawati SabutHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Def Ronzo
Diunggah oleh
Lidyawati SabutHak Cipta:
Format Tersedia
Balas.
qxd 19/2/08 3:21 pm Page 45
DPP-4 Inhibition in Type 2 Diabetes Management
The Role of Dipeptidyl Peptidase-4 Inhibitors in the
Management of Type 2 Diabetes
a report by
B o g d a n B a l a s 1 and R a l p h A D e F r o n z o 2
1. Post-doctoral Fellow; 2. Professor of Medicine and Chief, Division of Diabetes, University of Texas Health Science Center, San Antonio
DOI:10.17925/EE.2007.00.02.45
Insulin resistance manifests itself early in life and involves multiple tissues, to respond to infused GIP. The progressive decline in GLP-1 secretion in IGT
including the liver, muscles and adipocytes. 1,2 However, as long as the and type 2 diabetes correlates closely with the impairment in insulin
β cell is able to augment its secretion to offset the defect in insulin action, secretion.26 The increase in plasma GIP levels and development of GIP
glucose tolerance remains normal. With time, however, as the β cell begins
3 resistance occurs in all forms of diabetes (type 2 diabetes, type 1 diabetes,
to fail, the β cell compensatory response becomes insufficient to offset the cystic fibrosis, chronic pancreatitis) and can be reversed by restoration of
insulin resistance, and impaired glucose tolerance (IGT)/impaired fasting normoglycaemia,27 indicating that it is a form of glucotoxicity. Because GIP
glycaemia (IFG) and, eventually, overt type 2 diabetes ensues.4,5 Type 2 levels are elevated and the β cells are resistant to GIP, this has not become
diabetes is a chronic metabolic disorder characterised by defects in insulin a target for diabetic therapy. However, if normoglycaemia can be restored
secretion and insulin resistance.6 Current therapeutic approaches focus by other means, this would lead to return of normal β-cell sensitivity27 to GIP;
on improving insulin sensitivity or preserving/augmenting β-cell function, this could become an exciting new tool to prevent β-cell failure and treat
or both, with the goal of re-establishing normal glucose homeostasis. type 2 diabetes.
Incretins and β-cell Failure GLP-1 is a potent insulin secretagogue28,29 and continuous intravenous/
Multiple factors contribute to progressive β-cell failure in type 2 diabetes subcutaneous GLP-1 infusion has provided proof of concept that this
(see Figure 1). Multiple studies have shown that genetic factors play an incretin hormone could be used effectively to improve β-cell function and
important role in the development of impaired insulin secretion.7 improve glycaemic control in type 2 diabetes patients.30,31 The discovery of
Acquired factors – including lipotoxicity,8,9 glucotoxicity10 and amylin exendin-4, a long-acting GLP-1 analogue, in the salivary gland of the Gila
accumulation within the β cell – have also been shown to contribute to
11 monster has led to the development of incretin replacement therapy as an
the impairment in insulin secretion. effective means to improve β-cell function and glycaemic control in type 2
diabetes patients.12 Alternatively, inhibition of DPP-4 – the enzyme that
Over the last decade, considerable attention has been focused on the role cleaves both GLP-1 and GIP32 – has proved to be an effective approach to
of incretin hormones in the pathogenesis of progressive β-cell failure in augmenting circulating incretin levels and improving glycaemic control in
type 2 diabetes.12 It has been known for over 50 years that the insulin- type 2 diabetes patients. Sitagliptin (Januvia®, Merck) is the first DPP-4
secretory response to an oral glucose load is three- to four-fold greater inhibitor approved in the US for the treatment of type 2 diabetes, and
following oral versus intravenous glucose administration13 (see Figure 2). vildagliptin is currently under regulatory review by the US Food and Drug
The search for the missing ‘incretin’ hormones that augment insulin Administration (FDA). A number of other DPP-4 inhibitors are currently in
secretion in response to the gastrointestinal route of glucose phase III clinical trials, and the results look quite promising.
administration has identified two peptides – glucagon-like peptide-1
(GLP-1) and gastric inhibitory polypeptide, also called glucose-dependent Mechanism of Action of Dipeptidyl Peptidase-4 Inhibitors
insulinotropic polypeptide (GIP) – that together account for more than The major mechanism by which DPP-4 inhibitors improve glycaemic
90% of the incretin response.14–17 GLP-1 and GIP are secreted by the control is by augmenting plasma GLP-1 levels.33,34 However, considerable
L cells and K cells in the intestinal tract in response to meal ingestion.
GLP-1 and GIP are secreted into the portal vein18,19 and act on the β cell
Bogdan Balas is a Post-doctoral Fellow in the Division of
to stimulate glucose-dependent insulin secretion.12,20,21 The secreted Diabetes at the University of Texas Health Science Center,
GLP-1 and GIP are rapidly degraded by the enzyme dipeptidyl peptidase-4 San Antonio. His research focuses on delineating the
pathogenesis of type 2 diabetes mellitus and the mechanism
(DPP-4), an enzyme that is ubiquitous in plasma and cell membranes. This
of action of drugs that improve insulin sensitivity and insulin
accounts for the short half-life (four to five minutes) of GLP-1 and GIP in secretion in humans and animals. Dr Balas obtained his
the circulatory system, and ensures that after the stomach is devoid of medical degree from the University of Bucharest in 2000.
food, insulin secretion will cease and hypoglycaemia will be avoided. E: bbalas74@yahoo.com
Since the secretion of both GLP-1 and GIP is glucose-dependent, once the
Ralph A DeFronzo is a Professor of Medicine and Chief of
blood sugar level has returned to normal, insulin release by the β cell the Division of Diabetes at the University of Texas Health
stops, providing another defence against hypoglycaemia.22,23 Science Center, San Antonio. He is a world-renowned
authority on the pathogenesis of type 2 diabetes, the insulin
resistance syndrome and the treatment of type 2 diabetes.
In individuals with impaired glucose tolerance and type 2 diabetes there is a
progressive decline in plasma levels of GLP-114 and a rise in the plasma GIP
concentration.24,25 This suggests that the β cells are resistant to GIP, and this
has been confirmed by the failure of the β cells in type 2 diabetes patients
© TOUCH BRIEFINGS 2007 45
Balas.qxd 19/2/08 3:22 pm Page 46
DPP-4 Inhibition in Type 2 Diabetes Management
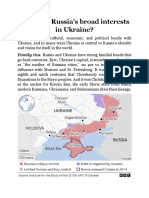
Figure 1: Pathogenetic Factors Implicated in the Progressive have shown that the insulin secretory rate is increased following a
Impairment in Insulin Secretion in Type 2 Diabetes Mellitus single-dose administration of vildagliptin.42 It is important to note,
however, that plasma glucose levels decline significantly following both
short-term and chronic administration of DPP-4 inhibitors. Both the
absolute and the incremental plasma glucose levels are important
e
tanc
determinants of the insulin secretory response, and they both decline
resis
Gene
after DPP-4 inhibition. A similar insulin response in the face of a reduced
lin
tics
Insu
plasma glucose stimulus indicates an important stimulatory effect of the
Glu
cos DPP-4 inhibitors on insulin secretion. Thus, the incremental insulin
e tox
icit e
y Ag response divided by the incremental glucose response has been shown to
increase following administration of both sitagliptin46 and vildagliptin.49,50
Homeostatic model assessment (HOMA) β cell,48,51,52 as well as insulin
secretion, measured with the minimal model,53 has been shown to
Beta-cell Amylin (IAPP)
Lipotoxicity ↑ FFA increase following DPP-4 inhibition.
Failure
Because the main mechanism of action of the DPP-4 inhibitors is
He
mediated by GLP-1, and because GLP-1 potentiates insulin release only
ffect xo
sam during conditions of hyperglycaemia, the glucose-lowering effect of
i ne ine
ret s
Inc the DPP-4 inhibitors is self-limiting. 12,22 In theory, therefore,
↓
hypoglycaemia should not be a problem with the DPP-4 inhibitors, and
α
Other
TNF
this has been proved in clinical studies.54,55 Moreover, when given in
association with insulin sensitisers such as metformin and the
thiazolidinediones, hypoglycaemia is also distinctly uncommon.49,56–58
DPP-4 inhibitors are not approved for use with insulin, and appear to
be less effective in reducing glycated haemoglobin (HbA1c) when
TNF-α = tumor necrosis factor-alpha.
Source: DeFronzo RA, Med Clin N Am, 2004;88:787–835. combined with this agent.59
evidence suggests that factors in addition to increased plasma GLP-1 Effect on Glucagon Secretion
levels contribute to the beneficial effects of DPP-4 inhibitors on glucose GLP-1 is a potent inhibitor of glucagon secretion by the pancreatic
homeostasis. Clinical studies have demonstrated that the rise in β cells,60 and this inhibitory effect is glucose-dependent.61,62 Not
endogenous GLP-1 concentration after DPP-4 inhibition is modest, and 35 surprisingly, a decline in plasma glucagon concentration has
these drugs have a delayed effect (weeks) on improving glucose consistently been observed in diabetic patients treated with DPP-4
homeostasis.36,37 When similar increases in GLP-1 are produced by inhibitors.47,50 The decrease in plasma glucagon concentration has
exogenous infusion, the effect on insulin secretion and glucose levels is been correlated with the suppression of basal and post-meal42 rate of
not nearly as robust.38 It is possible that the DPP-4 inhibitors work not hepatic glucose production in type 2 diabetes patients treated with
only by increasing GLP-1 levels, but also by augmenting the release of DPP-4 inhibitors. Although GIP levels increase during treatment
other deficient incretins, including GIP, pituitary adenylate cyclase- with DPP-4 inhibitors, GIP has no suppressive effect on glucagon
activating peptide (PACAP), gastrin-releasing peptide (GRP) and other as secretion, and some studies have shown an increase in circulating
yet unidentified hormones.39 DPP-4 inhibition may, in fact, have a glucagon levels in response to GIP.45
multitude of pleiotropic effects since this enzyme has been shown to
inhibit the degradation of over 20 peptides in the human body.40
Neuropeptides stored in islet nerve terminals are also affected by DPP-4 The main effect of dipeptidyl
inhibition, and this could regulate islet function.39–41 Lastly, we have
shown that the pattern – as well as the amplitude – of incretin release is
peptidase-4 inhibition in type 2
significantly altered following DPP-4 inhibition. Thus, plasma GLP-1 and diabetes is to augment glucagon-like
GIP concentrations do not immediately return to basal levels, but remain
peptide-1 and gastric inhibitory
elevated for up to 12 hours.42
polypeptide secretion, leading to
Effect on Insulin Secretion
increased secretion of insulin and
The main effect of DPP-4 inhibition in type 2 diabetes is to augment GLP-
1 and GIP secretion, leading to increased secretion of insulin and inhibition inhibition of glucagon secretion.
of glucagon secretion.43,44 Because the β cell in type 2 diabetes is resistant
to the stimulatory effect of GIP on insulin secretion, and because GIP does
not inhibit glucagon secretion,45 GLP-1 is the primary incretin hormone Effect on Insulin Sensitivity
that mediates the beneficial glycaemic effect of the DPP-4 inhibition. The effect of long-term DPP-4 inhibition on insulin sensitivity has been less
well studied in humans. There are no insulin clamp data, and most existing
Circulating plasma insulin levels are unchanged or increased after human studies rely on surrogate indices – the HOMA-Insulin Resistance
short-term treatment with sitagliptin46 and vildagliptin.47,48 However, we (HOMA-IR) index, Quantitative Insulin Sensitivity Check Index (Quicky) and
46 EUROPEAN ENDOCRINE DISEASE 2007
Balas.qxd 19/2/08 3:22 pm Page 47
The Role of Dipeptidyl Peptidase-4 Inhibitors in the Management of Type 2 Diabetes
Figure 2: Plasma Insulin Response to Oral Glucose (50g) and Isoglycaemic Intravenous Glucose in Controls
8
10
Oral
IV
Oral
8
IV 6
Plasma insulin (µU/ml)
Plasma glucose (mmol/l)
86
Glucose infusion (g/15min)
4
5
4
∗ ∗
∗
∗ ∗
∗ 2
∗
2
0
0 0
0 60 120 180 0 60 120 180
Time (min) Time (min)
Adapted from: Nauck, Creutzfeldt, et al., Diabetologia, 1986;29:46–52.
Oral Glucose Insulin Sensitivity (OGIS) index. Both sitagliptin and vildagliptin that persist long after initiation of therapy. Whether these beneficial
have been shown to improve insulin sensitivity after both short- and long- effects will continue to persist after three to five years remains to be
term administration.48,50 However, whether this is a direct effect of the drug determined. Moreover, in man it is not possible to discern whether the
or simply reflects amelioration of glucotoxicity remains to be established. In
one study in normal, glucose-tolerant subjects in whom plasma
glucose/insulin/glucagon levels during a typical mixed meal were reproduced Dipeptidyl peptidase-4 inhibition has
by intravenous glucose/hormone administration in the presence and
absence of GLP-1, no effect on insulin sensitivity was noted.63 Animal
been shown to reduce streptozotocin-
models of diabetes have more consistently demonstrated a beneficial effect induced β-cell injury. However, it
of DPP-4 inhibition on insulin sensitivity.64–66
remains to be determined whether
GLP-1 receptors are expressed in the liver and, when stimulated, could such potential to augment β-cell mass
improve hepatic insulin sensitivity, suppress hepatic glucose
exists in man.
production (HGP) and reduce fasting plasma glucose concentration.67
With regard to this, we have shown that a single dose of vildagliptin
given with the evening meal significantly suppresses post-meal HGP increase in insulin secretion is due to an enhanced β-cell function or
and post-prandial glycaemic excursion from 6pm until 8am the increased β-cell mass. It also remains to be determined whether
following morning (see Figure 3).42 The suppression of HGP correlated initiation of DPP-4 therapy at the initial onset of type 2 diabetes or at the
closely with the decline in plasma glucagon concentration (r=0.49; stage of IGT can prevent the progressive β-cell failure that characterises
p<0.05), but a direct effect of GLP-1 on the liver cannot be excluded. the natural history of type 2 diabetes.
Effect on β-cell Neogenesis Regulation of Appetite and Weight
In rodents, GLP-1 stimulates proliferation and inhibits apoptosis of Unlike the GLP-1 analogues, which have a potent effect on suppressing
β cells and promotes the differentiation of β cells from ductal cell- appetite and promoting weight loss,75,76 the DPP-4 inhibitors have no
derived precursor cells. 68–71 Because DPP-4 inhibitors increase GLP-1 effect on appetite regulation and are weight-neutral.58 This difference is
levels, the effect of these drugs on β-cell mass has been examined. In most likely explained by the fact that the DPP-4 inhibitors increase plasma
rats and mice, DPP-4 inhibition has been shown to stimulate β-cell GLP-1 level to or only modestly above normal,47 whereas GLP-1
replication and neogenesis and to inhibit apoptosis. 72 DPP-4 inhibition administration leads to a pharmacological elevation in the circulating
has been shown to reduce streptozotocin-induced β-cell injury.73 incretin concentration.77
However, it remains to be determined whether such potential to
augment β-cell mass exists in man.74 Clinical Trials
In a double-blind, placebo-controlled study in which vildagliptin was Dipeptidyl Peptidase-4 Inhibitors as Monotherapy
administered for 52 weeks to patients inadequately treated with Vildagliptin monotherapy has been evaluated in five trials ranging in
metformin, there was a sustained improvement in glycated duration from four to 52 weeks.47,52,56,78–80 The decrease in HbA1c
haemoglobin (HbA1c) in the vildagliptin-treated group. 58 This sustained ranged from -0.31% when administered as 50mg/day52 to -1.1%
effect indicates that DPP-4 inhibitors may have β-cell protective effects when given in a dose of 100mg/day.80 100mg/day of vildagliptin was
EUROPEAN ENDOCRINE DISEASE 2007 47
Balas.qxd 19/2/08 3:23 pm Page 48
DPP-4 Inhibition in Type 2 Diabetes Management
Figure 3: Plasma Glucose and Change from Baseline in the Rate of Endogenous Glucose Production
Meal
Meal
0
350
X -0.3
300 ** Placebo
* *
Delta EGP (mg•kg-1•min-1)
Plasma glucose (mg/dl)
* Vildagliptin
-0.6
250 * * * * * *
* * * *
*
200 -0.9
*
150 -1.2 Placebo
* * Vildagliptin
* *
* ** * *
100 -1.5 * ** * * *
*
5pm 8pm 11pm 2am 5am 8am 5pm 8pm 11pm 2am 5am 8am
Time Time
Left: during the meal tolerance test. Right: during the post-absorptive period after ingestion of vildagliptin and placebo. Taken from Balas et al., J Clin Endocrinol Metab, 2007;92:1249–55.
shown to be non-inferior to rosiglitazone 8mg/day, with no weight elevated, which would have minimised any differences between the two
gain in the vildagliptin group,56 but was inferior by 0.4% in HbA1c, groups. It is noteworthy that DPP-4 inhibitors, unlike the GLP-1 analogues
with 1% reduction versus 1.4% reduction over 52 weeks, to (exenatide), do not promote weight loss.58 No phase III data have been
metformin 2,000mg/day. However, vildagliptin showed a superior published with any other DPP-4 inhibitor.
gastrointestinal side effect profile.81
Who Should Receive Treatment with
Sitagliptin monotherapy has been shown to be similarly effective to Dipeptidyl Peptidase-4 Inhibitors?
vildagliptin.51,82–84 Across the dose range, the reduction in HbA1c ranged The primary mechanism of action of the DPP-4 inhibitors is to increase
from -0.4% (25mg/day) 82,83 to -0.94% (200mg/day). 84 There are no plasma incretin levels, leading to the stimulation of insulin secretion and
available non-inferiority data on sitagliptin monotherapy. inhibition of glucagon release. Because individuals with IGT/IFG have lost
80% of their β-cell function4,5 and have a 40–50% reduction in β-cell
Combination Therapy mass,89 it makes more sense that DPP-4 inhibitor therapy should be
DPP-4 inhibitors have been proved most successful in reducing HbA1c initiated early in the natural history of type 2 diabetes when significant
when used in combination with metformin. In two separate studies, β-cell function remains. One might predict that the DPP-4 inhibitors could
addition of vildagliptin to metformin reduced HbA1c by 1.1%.58,85 be least effective if started late in the natural history of type 2 diabetes
when little β-cell function remains. One would argue that individuals with
IGT/IFG who still possess significant β-cell function are most likely to
benefit from DPP-4 inhibitor therapy. The combination of a DPP-4
Dipeptidyl peptidase-4 inhibitors have inhibitor with metformin seems especially effective. This can be explained
emerged as promising new treatments by the fact that metformin monotherapy significantly increases the
circulating levels of GLP-190 and, when added to the increase in plasma
for patients with type 2 diabetes
GLP-1 concentration elicited by DPP-4 inhibitors, leads to a critical GLP-1
mellitus, and they can be used both level that synergistically augments insulin secretion, inhibits glucagon
secretion and acts as the missing ‘gut factor’91 to augment hepatic
as monotherapy and in combination
glucose uptake following ingestion of an oral glucose load. Lastly, the
with other oral agents. combination of a DPP-4 inhibitor with a thiazolidinedione may prove to
be very effective in enhancing/maintaining insulin secretion, since the
thiazolidinediones are well established to exert clinically relevant effects
In three studies, addition of sitagliptin 100mg/day to metformin reduced to preserve β-cell function.92–96
HbA1c by 0.67%.46,53,57 In initial combination, sitagliptin and metformin
showed HbA1c reductions of -2.07%.86 Dipeptidyl Peptidase-4 Inhibitors or Incretin Mimetics?
Incretin mimetics (exenatide) and DPP-4 inhibitors appear to have
Addition of vildagliptin 100mg/day to pioglitazone reduced HbA1c by 1%, comparable effectiveness in achieving glucose control, although no
an amount similar to that seen with metformin;49 addition of sitagliptin to direct head-to-head comparisons are available.97 This is most likely
pioglitazone reduced HbA1c by 0.7%. In initial combination, vildagliptin 87 explained by the fact that exenatide is given as a pharmacological
and pioglitazone showed HbA1c reductions of –1.9%.88 The combination injection and results in supraphysiological levels of the GLP-1
of sitagliptin plus metformin was similarly effective to glipizide plus analogue, which cause a greater increase in insulin secretion than
metformin,57 although the starting HbA1c (~7.6%) was only modestly those seen after DPP-4 inhibition.97 These supraphysiological levels of
48 EUROPEAN ENDOCRINE DISEASE 2007
Balas.qxd 19/2/08 3:23 pm Page 49
The Role of Dipeptidyl Peptidase-4 Inhibitors in the Management of Type 2 Diabetes
GLP-1 also produce sustained weight loss,76 which exerts its own of adverse events. However, this has not proved to be the case, and the
beneficial effect to improve glycaemic control. The DPP-4 inhibitors do safety profile of the DPP-4 inhibitors has been shown to be excellent.
not promote weight loss, most likely because they only normalise or
only modestly increase plasma GLP-1 levels. Moreover, if a beneficial Special attention has been paid to the immune system, since DPP-4
effect of incretin replacement therapy is to be observed on (CD 26) is present in abundant amounts on lymphocytes.99 However,
preservation of/increase in β-cell function/mass, it is more likely to be inhibition of DPP-4 activity on lymphocytes does not seem to have a
observed with the supraphysiological incretin levels reached with deleterious effect on the immune response.100
injection of exenatide. However, due to the possibility of the above-
mentioned ‘pleiotropic’ effects of DPP-4 inhibition, it is possible that A theoretical risk associated with DPP-4 inhibition is the prolongation
there will be additional benefits of the DPP-4 inhibitors that are of action of a multitude of small peptide hormones, neuropeptides,
currently not recognised. With regard to this, decreases in plasma growth factors, cytokines and chemokines that are normally cleaved
triglyceride46,56 and apolipoprotein B98 levels have been described with by this protease.40 Despite these theoretical concerns, clinical studies
DPP-4 inhibition. In patients treated with exenatide, significant have shown a particularly good safety profile,47,52,78,80,82,84 although
reductions in plasma triglyceride concentration and blood pressure long-term (three- to five-year) studies will be required to establish
and increases in plasma high-density lipoprotein (HDL) cholesterol definitively the safety of this new class of oral antidiabetic drugs.
have been observed. These beneficial effects are largely related to the
associated weight loss. Combination therapy with exenatide and a Conclusions
DPP-4 inhibitor has not yet been evaluated, but, because the DPP-4 inhibitors have emerged as promising new treatments for
pleiotropic effects of the DPP-4 inhibitors have yet to be elucidated, patients with type 2 diabetes, and they can be used both as
the possibility of using these two classes of drugs together remains to monotherapy and in combination with other oral agents. Although
be examined. they appear to be no more or slightly less potent than other oral
antidiabetic medications, they offer advantages in the form of simple
Safety administration (once-daily oral dose), lack of hypoglycaemia and
Since DPP-4 is ubiquitously present in the body, initially it was excellent safety profile. Whether the DPP-4 inhibitors can
postulated that DPP-4 inhibition might be associated with a multitude restore/preserve β-cell function remains to be determined. ■
1. DeFronzo RA, Pathogenesis of type 2 diabetes: Metabolic and 15. Drucker DJ, Minireview: The glucagon-like peptides, (GIP) receptor expression in beta cells, FASEB J, 2003;17:91–3.
molecular implications for identifying diabetes genes, Diabetes Endocrinology, 2001;142:521–7. 28. Schmidt WE, Siegel EG, Creutzfeldt W, Glucagon-like peptide-1
Rev, 1997;4:177–269. 16. Nauck MA, Bartels E, Orskov C, et al., Additive insulinotropic but not glucagon-like peptide-2 stimulates insulin release from
2. DeFronzo RA, Lilly lecture 1987, The triumvirate: Beta-cell, effects of exogenous synthetic human gastric inhibitory isolated rat pancreatic islets, Diabetologia, 1985;28:704–7.
muscle, liver. A collusion responsible for NIDDM, Diabetes, polypeptide and glucagon-like peptide-1-(7-36) amide infused 29. Ritzel R, Orskov C, Holst JJ, Nauck MA, Pharmacokinetic,
1988;37:667–87. at near-physiological insulinotropic hormone and glucose insulinotropic, and glucagonostatic properties of GLP-1 [7-36
3. Diamond MP, Thornton K, Connolly-Diamond M, et al., concentrations, J Clin Endocrinol Metab, 1993;76:912–17. amide] after subcutaneous injection in healthy volunteers.
Reciprocal variations in insulin-stimulated glucose uptake and 17. Ahren B, Larsson H, Holst JJ, Effects of glucagon-like peptide-1 Dose-response-relationships, Diabetologia, 1995;38:720–25.
pancreatic insulin secretion in women with normal glucose on islet function and insulin sensitivity in noninsulin-dependent 30. Rachman J, Barrow BA, Levy JC, Turner RC, Near-normalisation
tolerance, J Soc Gynecol Investig, 1995;2:708–15. diabetes mellitus, J Clin Endocrinol Metab, 1997;82:473–8. of diurnal glucose concentrations by continuous administration
4. Ferrannini E, Gastaldelli A, Miyazaki Y, et al., Beta-cell 18. Holst JJ, Gromada J, Role of incretin hormones in the of glucagon-like peptide-1 (GLP-1) in subjects with NIDDM,
function in subjects spanning the range from normal glucose regulation of insulin secretion in diabetic and nondiabetic Diabetologia, 1997;40:205–11.
tolerance to overt diabetes: A new analysis, J Clin Endocrinol humans, Am J Physiol Endocrinol Metab, 2004;287:E199–206. 31. Zander M, Madsbad S, Madsen JL, Holst JJ, Effect of 6-week
Metab, 2005;90:493–500. 19. Deacon CF, What do we know about the secretion and course of glucagon-like peptide 1 on glycaemic control, insulin
5. Gastaldelli A, Ferrannini E, Miyazaki Y, et al., San Antonio degradation of incretin hormones?, Regul Pept, 2005;128: sensitivity, and beta-cell function in type 2 diabetes: A parallel-
metabolism study. Beta-cell dysfunction and glucose 117–24. group study, Lancet, 2002;359:824–30.
intolerance: Results from the san antonio metabolism (SAM) 20. Drucker DJ, Glucagon-like peptides, Diabetes, 32. Ahren B, Gut peptides and type 2 diabetes mellitus treatment,
study, Diabetologia, 2004;47:31–9. 1998;47:159–69. Curr Diab Rep, 2003;3:365–72.
6. DeFronzo RA, Pathogenesis of type 2 diabetes mellitus, Med 21. Holst JJ, Therapy of type 2 diabetes mellitus based on the 33. Deacon CF, Hughes TE, Holst JJ, Dipeptidyl peptidase IV
Clin North Am, 2004;88:787–835, ix. actions of glucagon-like peptide-1, Diabetes Metab Res Rev, inhibition potentiates the insulinotropic effect of glucagon-like
7. Groop L, Bottazzo GF, Genetic susceptibility to non-insulin 2002;18:430–41. peptide 1 in the anesthetized pig, Diabetes, 1998;47:764–9.
dependent diabetes, BMJ, 1994;308:534. 22. Vilsboll T, Krarup T, Madsbad S, Holst JJ, No reactive 34. Ahren B, Simonsson E, Larsson H, et al., Inhibition of
8. McGarry JD, Banting lecture 2001: Dysregulation of fatty acid hypoglycaemia in type 2 diabetic patients after subcutaneous dipeptidyl peptidase IV improves metabolic control over a 4-
metabolism in the etiology of type 2 diabetes, Diabetes, administration of GLP-1 and intravenous glucose, Diabet Med, week study period in type 2 diabetes, Diabetes Care,
2002;51:7–18. 2001;18:144–9. 2002;25:869–75.
9. Kashyap S, Belfort R, Gastaldelli A, et al., A sustained increase 23. Knop FK, Vilsboll T, Larsen S, et al., No hypoglycemia after 35. Ahren B, What mediates the benefits associated with
in plasma free fatty acids impairs insulin secretion in subcutaneous administration of glucagon-like peptide-1 in lean dipeptidyl peptidase-IV inhibition?, Diabetologia,
nondiabetic subjects genetically predisposed to develop type 2 type 2 diabetic patients and in patients with diabetes 2005;48:605–7.
diabetes, Diabetes, 2003;52:2461–74. secondary to chronic pancreatitis, Diabetes Care, 36. Nauck MA, El-Ouaghlidi A, The therapeutic actions of DPP-IV
10. Rossetti L, Giaccari A, DeFronzo RA, Glucose toxicity, Diabetes 2003;26:2581–7. inhibition are not mediated by glucagon-like peptide-1,
Care, 1990;13:610–30. 24. Lardinois CK, Mazzaferri EL, Starich GH, et al., Increased Diabetologia, 2005;48:608–11.
11. Kahn SE, Andrikopoulos S, Verchere CB, Islet amyloid: A long- gastric inhibitory polypeptide is not reduced in patients with 37. Holst JJ, Deacon CF, Glucagon-like peptide-1 mediates the
recognized but underappreciated pathological feature of type 2 noninsulin-dependent diabetes mellitus treated with intense therapeutic actions of DPP-IV inhibitors, Diabetologia,
diabetes, Diabetes, 1999;48:241–53. insulin therapy, J Clin Endocrinol Metab, 1985;61:1089–92. 2005;48:612–15.
12. Deacon CF, Therapeutic strategies based on glucagon-like 25. Crockett SE, Mazzaferri EL, Cataland S, Gastric inhibitory 38. Nauck MA, Heimesaat MM, Orskov C, et al., Preserved incretin
peptide 1, Diabetes, 2004;53:2181–9. polypeptide (GIP) in maturity-onset diabetes mellitus, Diabetes, activity of glucagon-like peptide 1 [7-36 amide] but not of
13. Nauck M, Stockmann F, Ebert R, Creutzfeldt W, Reduced 1976;25:931–5. synthetic human gastric inhibitory polypeptide in patients with
incretin effect in type 2 (non-insulin-dependent) diabetes, 26. Orskov C, Wettergren A, Holst JJ, Secretion of the incretin type-2 diabetes mellitus, J Clin Invest, 1993;91:301–7.
Diabetologia, 1986;29:46–52. hormones glucagon-like peptide-1 and gastric inhibitory 39. Ahren B, Hughes TE, Inhibition of dipeptidyl peptidase-4
14. Vilsboll T, Krarup T, Deacon CF, et al., Reduced postprandial polypeptide correlates with insulin secretion in normal man augments insulin secretion in response to exogenously
concentrations of intact biologically active glucagon-like throughout the day, Scand J Gastroenterol, 1996;31:665–70. administered glucagon-like peptide-1, glucose-dependent
peptide 1 in type 2 diabetic patients, Diabetes, 27. Lynn FC, Thompson SA, Pospisilik JA, et al., A novel pathway insulinotropic polypeptide, pituitary adenylate cyclase-
2001;50:609–13. for regulation of glucose-dependent insulinotropic polypeptide activating polypeptide, and gastrin-releasing peptide in mice,
EUROPEAN ENDOCRINE DISEASE 2007 49
Balas.qxd 19/2/08 3:24 pm Page 50
DPP-4 Inhibition in Type 2 Diabetes Management
Endocrinology, 2005;146:2055–9. Care, 2004;27: 2874–80. randomized, placebo-controlled, multiple-dose study, Horm
40. Mentlein R, Dipeptidyl-peptidase IV (CD26)—role in the 59. Fonseca V, Schweizer A, Albrecht D, et al., Addition of Metab Res, 2007;39:218–23.
inactivation of regulatory peptides, Regul Pept, 1999;85:9–24. vildagliptin to insulin improves glycaemic control in type 2 81. Dejager S, Lebeaut A, Couturier A, Schweizer A, Sustained
41. Ahren B, Autonomic regulation of islet hormone secretion— diabetes, Diabetologia, 2007;50:1148–55. reduction in HbA1c during one-year treatment with vildagliptin
implications for health and disease, Diabetologia, 2000;43: 60. Hvidberg A, Nielsen MT, Hilsted J, et al., Effect of glucagon- in patients with type 2 diabetes (T2DM), Diabetes, 2006;55
393–410. like peptide-1 (proglucagon 78-107amide) on hepatic glucose (Suppl. 1):120–OR.
42. Balas B, Baig MR, Watson C, et al., The dipeptidyl peptidase production in healthy man, Metabolism, 1994;43:104–8. 82. Scott R, Wu M, Sanchez M, Stein P, Efficacy and tolerability of
IV inhibitor vildagliptin suppresses endogenous glucose 61. Degn KB, Juhl CB, Sturis J, et al., One week’s treatment with the dipeptidyl peptidase-4 inhibitor sitagliptin as monotherapy
production and enhances islet function after single-dose the long-acting glucagon-like peptide 1 derivative liraglutide over 12 weeks in patients with type 2 diabetes, Int J Clin
administration in type 2 diabetic patients, J Clin Endocrinol (NN2211) markedly improves 24-h glycemia and alpha- and Pract, 2007;61:171–80.
Metab, 2007;92:1249–55. beta-cell function and reduces endogenous glucose release in 83. Herman GA, Hanefeld M, Wu M, et al., Effect of MK-0431,
43. Balkan B, Kwasnik L, Miserendino R, et al., Inhibition of patients with type 2 diabetes, Diabetes, 2004;53:1187–94. dipeptidyl peptidase IV (DPP-IV) inhibitor, on glycemic control
dipeptidyl peptidase IV with NVP-DPP728 increases plasma 62. Nauck MA, Heimesaat MM, Behle K, et al., Effects of glucagon- after 12 weeks in patients with type 2 diabetes, Curr Med Res
GLP-1 (7-36 amide) concentrations and improves oral glucose like peptide 1 on counterregulatory hormone responses, Opin, 2005;54 (Suppl. 1):A134.
tolerance in obese zucker rats, Diabetologia, cognitive functions, and insulin secretion during 84. Aschner P, Kipnes MS, Lunceford JK, et al., Sitagliptin Study
1999;42:1324–31. hyperinsulinemic, stepped hypoglycemic clamp experiments in 021 Group. Effect of the dipeptidyl peptidase-4 inhibitor
44. Ahren B, Holst JJ, Martensson H, Balkan B, Improved glucose healthy volunteers, J Clin Endocrinol Metab, 2002;87:1239–46. sitagliptin as monotherapy on glycemic control in patients with
tolerance and insulin secretion by inhibition of dipeptidyl 63. Vella A, Shah P, Basu R, et al., Effect of glucagon-like peptide type 2 diabetes, Diabetes Care, 2006;29:2632–7.
peptidase IV in mice, Eur J Pharmacol, 2000;404:239–45. 1(7-36) amide on glucose effectiveness and insulin action in 85. Bosi E, Camisasca RP, Collober C, et al., Effects of vildagliptin
45. Ross SA, Brown JC, Dupre J, Hypersecretion of gastric people with type 2 diabetes, Diabetes, 2000;49:611–17. on glucose control over 24 weeks in patients with type 2
inhibitory polypeptide following oral glucose in diabetes 64. Pospisilik JA, Stafford SG, Demuth HU, et al., Long-term diabetes inadequately controlled with metformin, Diabetes
mellitus, Diabetes, 1977;26:525–9. treatment with the dipeptidyl peptidase IV inhibitor P32/98 Care, 2007;30:890–95.
46. Charbonnel B, Karasik A, Liu J, et al., Sitagliptin Study 020 causes sustained improvements in glucose tolerance, insulin 86. Goldstein BJ, Feinglos MN, Lunceford JK, et al., Effect of initial
Group. Efficacy and safety of the dipeptidyl peptidase-4 sensitivity, hyperinsulinemia, and beta-cell glucose combination therapy with sitagliptin, a dipeptidyl peptidase-4
inhibitor sitagliptin added to ongoing metformin therapy in responsiveness in VDF (fa/fa) zucker rats, Diabetes, inhibitor, and metformin on glycemic control in patients with
patients with type 2 diabetes inadequately controlled with 2002;51:943–50. type 2 diabetes, Diabetes Care, 2007.
metformin alone, Diabetes Care, 2006;29:2638–43. 65. Pospisilik JA, Stafford SG, Demuth HU, et al., Long-term 87. Rosenstock J, Brazg R, Andryuk PJ, et al., Sitagliptin Study 019
47. Ahren B, Landin-Olsson M, Jansson PA, et al., Inhibition of treatment with dipeptidyl peptidase IV inhibitor improves Group. Efficacy and safety of the dipeptidyl peptidase-4
dipeptidyl peptidase-4 reduces glycemia, sustains insulin levels, hepatic and peripheral insulin sensitivity in the VDF zucker rat: inhibitor sitagliptin added to ongoing pioglitazone therapy in
and reduces glucagon levels in type 2 diabetes, J Clin A euglycemic-hyperinsulinemic clamp study, Diabetes, patients with type 2 diabetes: A 24-week, multicenter,
Endocrinol Metab, 2004;89:2078–84. 2002;51: 2677–83. randomized, double-blind, placebo-controlled, parallel-group
48. Ahren B, Pacini G, Foley JE, Schweizer A, Improved meal- 66. Burkey BF, Li X, Bolognese L, et al., Acute and chronic effects study, Clin Ther, 2006;28:1556–68.
related beta-cell function and insulin sensitivity by the of the incretin enhancer vildagliptin in insulin-resistant rats, 88. Rosenstock J, Kim SW, Baron MA, et al., Efficacy and
dipeptidyl peptidase-IV inhibitor vildagliptin in metformin- J Pharmacol Exp Ther, 2005;315:688–95. tolerability of initial combination therapy with vildagliptin and
treated patients with type 2 diabetes over 1 year, Diabetes 67. Prigeon RL, Quddusi S, Paty B, D’Alessio DA, Suppression of pioglitazone compared with component monotherapy in
Care, 2005;28:1936–40. glucose production by GLP-1 independent of islet hormones: A patients with type 2 diabetes, Diabetes Obes Metab,
49. Garber AJ, Schweizer A, Baron MA, et al., Vildagliptin in novel extrapancreatic effect, Am J Physiol Endocrinol Metab, 2007;9(2):175–85.
combination with pioglitazone improves glycaemic control in 2003;285:E701–7. 89. Butler AE, Janson J, Bonner-Weir S, et al., Beta-cell deficit and
patients with type 2 diabetes failing thiazolidinedione 68. Egan JM, Bulotta A, Hui H, Perfetti R, GLP-1 receptor agonists increased beta-cell apoptosis in humans with type 2 diabetes,
monotherapy: A randomized, placebo-controlled study, are growth and differentiation factors for pancreatic islet beta Diabetes, 2003;52:102–10.
Diabetes Obes Metab, 2007;9:166–74. cells, Diabetes Metab Res Rev, 2003;19:115–23. 90. Mannucci E, Ognibene A, Cremasco F, et al., Effect of
50. Mari A, Sallas WM, He YL, et al., Vildagliptin, a dipeptidyl 69. Stoffers DA, Desai BM, DeLeon DD, Simmons RA, Neonatal metformin on glucagon-like peptide 1 (GLP-1) and leptin
peptidase-IV inhibitor, improves model-assessed beta-cell exendin-4 prevents the development of diabetes in the levels in obese nondiabetic subjects, Diabetes Care,
function in patients with type 2 diabetes, J Clin Endocrinol intrauterine growth retarded rat, Diabetes, 2003;52:734–40. 2001;24:489–94.
Metab, 2005;90:4888–94. 70. Zhou J, Wang X, Pineyro MA, Egan JM, Glucagon-like peptide 91. DeFronzo F, Ferrannini E, Wahren J, Felig P, Lack of a
51. Raz I, Hanefeld M, Xu L, et al., Sitagliptin Study 023 Group. 1 and exendin-4 convert pancreatic AR42J cells into glucagon- gastrointestinal mediator of insulin action in maturity-onset
Efficacy and safety of the dipeptidyl peptidase-4 inhibitor and insulin-producing cells, Diabetes, 1999;48:2358–66. diabetes, Lancet, 1978;2:1077–9.
sitagliptin as monotherapy in patients with type 2 diabetes 71. Farilla L, Bulotta A, Hirshberg B, et al., Glucagon-like peptide 92. DREAM (Diabetes REduction Assessment with ramipril and
mellitus, Diabetologia, 2006;49:2564–71. 1 inhibits cell apoptosis and improves glucose responsiveness rosiglitazone Medication) Trial Investigators, Gerstein HC,
52. Ristic S, Byiers S, Foley J, Holmes D, Improved glycaemic of freshly isolated human islets, Endocrinology, Yusuf S, Bosch J, et al., Effect of rosiglitazone on the frequency
control with dipeptidyl peptidase-4 inhibition in patients with 2003;144:5149–58. of diabetes in patients with impaired glucose tolerance or
type 2 diabetes: Vildagliptin (LAF237) dose response, Diabetes 72. Pospisilik JA, Martin J, Doty T, et al., Dipeptidyl peptidase IV impaired fasting glucose: A randomised controlled trial, Lancet,
Obes Metab, 2005;7:692–8. inhibitor treatment stimulates beta-cell survival and islet 2006;368:1096–1105.
53. Brazg R, Xu L, Dalla Man C, et al., Effect of adding sitagliptin, neogenesis in streptozotocin-induced diabetic rats, Diabetes, 93. Dormandy JA, Charbonnel B, Eckland DJ, et al., PROactive
a dipeptidyl peptidase-4 inhibitor, to metformin on 24-h 2003;52:741–50. investigators. Secondary prevention of macrovascular events in
glycaemic control and beta-cell function in patients with type 2 73. Duttaroy A, Voelker F, Merriam K, et al., The DPP-4 inhibitor patients with type 2 diabetes in the PROactive study
diabetes, Diabetes Obes Metab, 2007;9:186–93. vildagliptin increases pancreatic beta cell neogenesis and (PROspective pioglitAzone clinical trial in macroVascular events):
54. Bergman AJ, Stevens C, Zhou Y, et al., Pharmacokinetic and decreases apoptosis, 2005;54(Suppl. 1):A141. A randomised controlled trial, Lancet, 2005;366:1279–89.
pharmacodynamic properties of multiple oral doses of 74. Holst JJ, Glucagon-like peptide-1: From extract to agent. the 94. Azen SP, Peters RK, Berkowitz K, et al., TRIPOD (TRoglitazone
sitagliptin, a dipeptidyl peptidase-IV inhibitor: A double-blind, claude bernard lecture, 2005, Diabetologia, 2006;49:253–60. in the prevention of diabetes): A randomized, placebo-
randomized, placebo-controlled study in healthy male 75. Flint A, Raben A, Astrup A, Holst JJ, Glucagon-like peptide 1 controlled trial of troglitazone in women with prior gestational
volunteers, Clin Ther, 2006;28:55–72. promotes satiety and suppresses energy intake in humans, J diabetes mellitus, Control Clin Trials, 1998;19:217–31.
55. Herman GA, Stevens C, Van Dyck K, et al., Pharmacokinetics Clin Invest, 1998;101:515–20. 95. Kahn SE, Haffner SM, Heise MA, et al., ADOPT Study Group.
and pharmacodynamics of sitagliptin, an inhibitor of dipeptidyl 76. DeFronzo RA, Ratner RE, Han J, et al., Effects of exenatide Glycemic durability of rosiglitazone, metformin, or glyburide
peptidase IV, in healthy subjects: Results from two (exendin-4) on glycemic control and weight over 30 weeks in monotherapy, N Engl J Med, 2006;355:2427–43.
randomized, double-blind, placebo-controlled studies with metformin-treated patients with type 2 diabetes, Diabetes 96. Gastaldelli A, Ferrannini E, Miyazaki Y, et al.,
single oral doses, Clin Pharmacol Ther, 2005;78:675–88. Care, 2005;28:1092–1100. Thiazolidinediones improve beta-cell function in type 2 diabetic
56. Rosenstock J, Baron MA, Dejager S, et al., Comparison of 77. Fehse F, Trautmann M, Holst JJ, et al., Exenatide augments patients, Am J Physiol Endocrinol Metab, 2007;292:E871–83.
vildagliptin and rosiglitazone monotherapy in patients with first- and second-phase insulin secretion in response to 97. Drucker DJ, Nauck MA, The incretin system: Glucagon-like
type 2 diabetes: A 24-week, double-blind, randomized trial, intravenous glucose in subjects with type 2 diabetes, J Clin peptide-1 receptor agonists and dipeptidyl peptidase-4
Diabetes Care, 2007;30:217–23. Endocrinol Metab, 2005;90:5991–7. inhibitors in type 2 diabetes, Lancet, 2006;368:1696–705.
57. Nauck MA, Meininger G, Sheng D, et al., Sitagliptin Study 024 78. Pratley RE, Jauffret-Kamel S, Galbreath E, Holmes D, Twelve- 98. Matikainen N, Manttari S, Schweizer A, et al., Vildagliptin
Group. Efficacy and safety of the dipeptidyl peptidase-4 week monotherapy with the DPP-4 inhibitor vildagliptin therapy reduces postprandial intestinal triglyceride-rich
inhibitor, sitagliptin, compared with the sulfonylurea, glipizide, improves glycemic control in subjects with type 2 diabetes, lipoprotein particles in patients with type 2 diabetes,
in patients with type 2 diabetes inadequately controlled on Horm Metab Res, 2006;38:423–8. Diabetologia, 2006;49:2049–57.
metformin alone: A randomized, double-blind, non-inferiority 79. Pi-Sunyer FX, Schweizer A, Mills D, Dejager S, Efficacy and 99. Morimoto C, Schlossman SF, The structure and function of
trial, Diabetes Obes Metab, 2007;9:194–205. tolerability of vildagliptin monotherapy in drug-naive patients CD26 in the T-cell immune response, Immunol Rev,
58. Ahren B, Gomis R, Standl E, et al., Twelve- and 52-week with type 2 diabetes, Diabetes Res Clin Pract, 2007;76:132–8. 1998;161:55–70.
efficacy of the dipeptidyl peptidase IV inhibitor LAF237 in 80. Dejager S, Razac S, Foley JE, Schweizer A, Vildagliptin in drug- 100.Cordero OJ, Yang CP, Bell EB, On the role of CD26 in CD4
metformin-treated patients with type 2 diabetes, Diabetes naive patients with type 2 diabetes: A 24-week, double-blind, memory T cells, Immunobiology, 2007;212:85–94.
50 EUROPEAN ENDOCRINE DISEASE 2007
Anda mungkin juga menyukai
- ACT December 2018 Form B05 PDFDokumen54 halamanACT December 2018 Form B05 PDFPranav ChatiBelum ada peringkat
- Sample Internship PPTDokumen19 halamanSample Internship PPTSangeeta JamadarBelum ada peringkat
- The Integumentary System Development: Biene, Ellen Angelic Flores, Andrie BonDokumen29 halamanThe Integumentary System Development: Biene, Ellen Angelic Flores, Andrie BonMu Lok100% (3)
- Incretin PharmDokumen3 halamanIncretin PharmSlim SaaryBelum ada peringkat
- Dipeptidyl Peptidase (DPP) - IV InhibitorDokumen2 halamanDipeptidyl Peptidase (DPP) - IV InhibitorAndhi FahrurrojiBelum ada peringkat
- Saxagliptin and Metformin in Fixed Combination For The Treatment of Type 2 Diabetes in AdultsDokumen11 halamanSaxagliptin and Metformin in Fixed Combination For The Treatment of Type 2 Diabetes in AdultsLaura MelatiBelum ada peringkat
- Incretin Mimetics and EnhancersDokumen3 halamanIncretin Mimetics and EnhancersRoger CBelum ada peringkat
- DMSOTT 4790 Inhibition of Dipeptidyl Peptidase 4 The Mechanisms of Acti 061109Dokumen8 halamanDMSOTT 4790 Inhibition of Dipeptidyl Peptidase 4 The Mechanisms of Acti 061109Hania Asmarani RahmanitaBelum ada peringkat
- Improving Glucagon-Like Peptide-1 Dynamics in Patients With Type 2 Diabetes MellitusDokumen5 halamanImproving Glucagon-Like Peptide-1 Dynamics in Patients With Type 2 Diabetes MellitusscribdBelum ada peringkat
- GLP - 1 As Preferred Treatment For T2D Over GIPDokumen7 halamanGLP - 1 As Preferred Treatment For T2D Over GIPdhannyakBelum ada peringkat
- Review Inhibition of Dipeptidyl Peptidase-4 With Vildagliptin A Potential New Treatment For Type 2 DiabetesDokumen8 halamanReview Inhibition of Dipeptidyl Peptidase-4 With Vildagliptin A Potential New Treatment For Type 2 DiabetesAndhi FahrurrojiBelum ada peringkat
- DM WordDokumen14 halamanDM WordmasrorohBelum ada peringkat
- Incretin HealthyDokumen12 halamanIncretin HealthyRoger CBelum ada peringkat
- Role of Dipeptidyl Peptidase-Iv (Dpp-4) Inhibitor in The Management of Type 2 DiabetesDokumen16 halamanRole of Dipeptidyl Peptidase-Iv (Dpp-4) Inhibitor in The Management of Type 2 Diabeteshar1977Belum ada peringkat
- Improved β-cell Function and Prolonged Remission of Diabetes Type 1 by GLP-1 Agonist Treatment in Newly Diagnosed AdolescencesDokumen4 halamanImproved β-cell Function and Prolonged Remission of Diabetes Type 1 by GLP-1 Agonist Treatment in Newly Diagnosed Adolescencesscience world publishingBelum ada peringkat
- Glucagon-Like Peptide 1: New: TherapiesDokumen3 halamanGlucagon-Like Peptide 1: New: TherapiesRidha Surya NugrahaBelum ada peringkat
- A Comprehensive Review and Perspective On Natural Sources As Dipeptidyl Peptidase-4 Inhibitors For Management of DiabetesDokumen18 halamanA Comprehensive Review and Perspective On Natural Sources As Dipeptidyl Peptidase-4 Inhibitors For Management of DiabetesPuspaBelum ada peringkat
- Perspectives: G Protein-Coupled Receptors As Targets For Anti-Diabetic TherapeuticsDokumen13 halamanPerspectives: G Protein-Coupled Receptors As Targets For Anti-Diabetic TherapeuticsAlicia Cerpa LunaBelum ada peringkat
- British Journal of Diabetes & Vascular Disease-2006-Pratley-150-6Dokumen8 halamanBritish Journal of Diabetes & Vascular Disease-2006-Pratley-150-6Nurul FajrinaBelum ada peringkat
- Ajhp 140168Dokumen12 halamanAjhp 140168cherrygems99Belum ada peringkat
- F 2433 CMED Saxagliptin A Selective DPP 4 Inhibitor For The Treatment of Type 2 D.PDF 3311Dokumen12 halamanF 2433 CMED Saxagliptin A Selective DPP 4 Inhibitor For The Treatment of Type 2 D.PDF 3311Ridha Surya NugrahaBelum ada peringkat
- Coppari 2012. Bases Molecular de La Resistencia A La LeptinaDokumen17 halamanCoppari 2012. Bases Molecular de La Resistencia A La LeptinaClaudioValdiviaBelum ada peringkat
- Clinical Trial Results of Glp-1-Related Agents: The Early EvidenceDokumen5 halamanClinical Trial Results of Glp-1-Related Agents: The Early EvidenceRidha Surya NugrahaBelum ada peringkat
- Available Online Through: Glucagon Like Peptide - 1: A New Era in Treatment of Type-2 Diabetes MellitusDokumen8 halamanAvailable Online Through: Glucagon Like Peptide - 1: A New Era in Treatment of Type-2 Diabetes MellitusRidha Surya NugrahaBelum ada peringkat
- Recent Advances in Incretin-Based Pharmacotherapies For The Treatment of Obesity and DiabetesDokumen3 halamanRecent Advances in Incretin-Based Pharmacotherapies For The Treatment of Obesity and DiabetesAndrés ChávezBelum ada peringkat
- 02 - Update Article New Oral Antidiabetic AgentsDokumen7 halaman02 - Update Article New Oral Antidiabetic AgentsMuhammad Lutfi Al AyubiBelum ada peringkat
- Pharmacological Management of Type 2 Diabetes Mellitus: Rationale For Rational Use of InsulinDokumen9 halamanPharmacological Management of Type 2 Diabetes Mellitus: Rationale For Rational Use of InsulinAditya Rachman Van Der ArjunaqueeBelum ada peringkat
- Glycemic and IRDokumen10 halamanGlycemic and IRAyman AleemBelum ada peringkat
- Inzucchi 2008 New Drugs For The Treatment of DiabDokumen11 halamanInzucchi 2008 New Drugs For The Treatment of Diabiacob ancutaBelum ada peringkat
- Alogliptin - A Review of Its Use in Patients With Type 2 Diabetes MellitusDokumen20 halamanAlogliptin - A Review of Its Use in Patients With Type 2 Diabetes Mellitus13201940Belum ada peringkat
- PMC4020327-jdi 12214Dokumen11 halamanPMC4020327-jdi 12214anca irinaBelum ada peringkat
- Incretin Mimetics and Dipeptidyl Peptidase-4 Inhibitors: Innovative Treatment Therapies For Type 2 DiabetesDokumen11 halamanIncretin Mimetics and Dipeptidyl Peptidase-4 Inhibitors: Innovative Treatment Therapies For Type 2 DiabetesRidha Surya NugrahaBelum ada peringkat
- Comparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic PatientsDokumen5 halamanComparison of Efficacy and Safety Profile of Empagliflozin Versus Dapagliflozin As Add On Therapy in Type 2 Diabetic Patientsthomas albertBelum ada peringkat
- Practical Use of Glucagon-Like Peptide-1 Receptor Agonist Therapy in Primary CareDokumen10 halamanPractical Use of Glucagon-Like Peptide-1 Receptor Agonist Therapy in Primary CareRidha Surya NugrahaBelum ada peringkat
- Is GLP-1 A Hormone: Whether and When?: David D 'AlessioDokumen6 halamanIs GLP-1 A Hormone: Whether and When?: David D 'AlessioGaby NRmzBelum ada peringkat
- Dipeptidyl Peptidase-4 Inhibitors: Their Role in The Management of Type 2 DiabetesDokumen3 halamanDipeptidyl Peptidase-4 Inhibitors: Their Role in The Management of Type 2 DiabetesRidha Surya NugrahaBelum ada peringkat
- Chapter 60Dokumen7 halamanChapter 60Ridha Surya NugrahaBelum ada peringkat
- Linagliptin in Type 2 Diabetes Media Fact Sheet: June 2010Dokumen3 halamanLinagliptin in Type 2 Diabetes Media Fact Sheet: June 2010Mike StevensBelum ada peringkat
- Diabetes Mellitus: Nhamier M. Jikiri, RN, MD, FPCP Internal MedicineDokumen27 halamanDiabetes Mellitus: Nhamier M. Jikiri, RN, MD, FPCP Internal MedicineNursidar Pascual MukattilBelum ada peringkat
- Agonistas Del Receptor Péptido 1 Similar Al Glucagon Una Terapia para El Control de La DiabetesDokumen8 halamanAgonistas Del Receptor Péptido 1 Similar Al Glucagon Una Terapia para El Control de La DiabetesLuisa GonzálezBelum ada peringkat
- Incretin Hormon ReviewDokumen17 halamanIncretin Hormon ReviewIntan OktapiaBelum ada peringkat
- Kalra 2011Dokumen7 halamanKalra 2011jinsung parkBelum ada peringkat
- The Role of GLP-1 Receptor Agonists in Managing Type 2 DiabetesDokumen9 halamanThe Role of GLP-1 Receptor Agonists in Managing Type 2 Diabetes이호원Belum ada peringkat
- Postprandial Glucose in Diabetes Time For Action.6Dokumen2 halamanPostprandial Glucose in Diabetes Time For Action.6mannkindfanBelum ada peringkat
- The Role of Tirzepatide, Dual GIP and GLP-1 Receptor Agonist, in The Management of Type 2 Diabetes: The SURPASS Clinical TrialsDokumen15 halamanThe Role of Tirzepatide, Dual GIP and GLP-1 Receptor Agonist, in The Management of Type 2 Diabetes: The SURPASS Clinical TrialsLilian Aracely Gaspar caceresBelum ada peringkat
- International Journal of Pharmaceutical Science Invention (IJPSI)Dokumen10 halamanInternational Journal of Pharmaceutical Science Invention (IJPSI)inventionjournalsBelum ada peringkat
- Comparison of Vildagliptin-Metformin and Glimepiride-Metformin Treatments in Type 2 Diabetic PatientsDokumen7 halamanComparison of Vildagliptin-Metformin and Glimepiride-Metformin Treatments in Type 2 Diabetic PatientsGregory VeintimillaBelum ada peringkat
- GLP 1 R AgonistDokumen8 halamanGLP 1 R AgonistHninBelum ada peringkat
- Biology 09 00473 v3Dokumen20 halamanBiology 09 00473 v3Gaby CarellanoBelum ada peringkat
- Newer Drugs in The Management of Diabetes MellitusDokumen8 halamanNewer Drugs in The Management of Diabetes MellitusAstri Faluna SheylavontiaBelum ada peringkat
- Incretin-Based Therapies: Joshua J. NeumillerDokumen23 halamanIncretin-Based Therapies: Joshua J. NeumillerAbulHasan Idrus IstarBelum ada peringkat
- PharmacologyDokumen7 halamanPharmacologyEvans KorirBelum ada peringkat
- NauckDokumen8 halamanNauckIqaBelum ada peringkat
- Lead 4Dokumen7 halamanLead 4afamhbkBelum ada peringkat
- Journal of Translational MedicineDokumen13 halamanJournal of Translational MedicinetrirahmiBelum ada peringkat
- Mehanna 2013Dokumen20 halamanMehanna 2013iacob ancutaBelum ada peringkat
- Tirzepatide Versus Semaglutide Once Weekly in Patients With Type 2 DiabetesDokumen13 halamanTirzepatide Versus Semaglutide Once Weekly in Patients With Type 2 Diabetesmanish chaudharyBelum ada peringkat
- The Effects of Licogliflozin, A Dual SGLT12 Inhibitor, On BodyDokumen11 halamanThe Effects of Licogliflozin, A Dual SGLT12 Inhibitor, On BodyJose Mario HoyosBelum ada peringkat
- Kimed IrenDokumen10 halamanKimed Ireniren meylaniBelum ada peringkat
- 08 14 DeepikaDokumen10 halaman08 14 DeepikaRidha Surya NugrahaBelum ada peringkat
- New Combination Treatments in The Management of Diabetes: Focus On Sitagliptin - MetforminDokumen10 halamanNew Combination Treatments in The Management of Diabetes: Focus On Sitagliptin - MetforminGd PadmawijayaBelum ada peringkat
- International Textbook of Diabetes MellitusDari EverandInternational Textbook of Diabetes MellitusR. A. DeFronzoBelum ada peringkat
- Behaviour of Investors in Indian Equity Markets: Submitted byDokumen26 halamanBehaviour of Investors in Indian Equity Markets: Submitted byDibyanshu AmanBelum ada peringkat
- Sta. Lucia National High School: Republic of The Philippines Region III-Central LuzonDokumen7 halamanSta. Lucia National High School: Republic of The Philippines Region III-Central LuzonLee Charm SantosBelum ada peringkat
- Memory and History in The Folklores Reinvented Through BeowulfDokumen10 halamanMemory and History in The Folklores Reinvented Through BeowulfDebojyoti DanBelum ada peringkat
- Managing Ambiguity and ChangeDokumen7 halamanManaging Ambiguity and ChangeTracey FeboBelum ada peringkat
- COMM 103 Floyd Chapters Study GuideDokumen4 halamanCOMM 103 Floyd Chapters Study GuideMad BasblaBelum ada peringkat
- Soal Midtest + Kunci JawabanDokumen28 halamanSoal Midtest + Kunci JawabanYuyun RasulongBelum ada peringkat
- Roman Villas at Tor Marancia and CentocelleDokumen10 halamanRoman Villas at Tor Marancia and CentocelleIgor ĆirkovićBelum ada peringkat
- Polynomials Level 3Dokumen17 halamanPolynomials Level 3greycouncilBelum ada peringkat
- Marriage Practices Among The Gidda Oromo, Northern Wollega, EthiopiaDokumen2 halamanMarriage Practices Among The Gidda Oromo, Northern Wollega, Ethiopiajoseph mathewBelum ada peringkat
- Vrushalirhatwal (14 0)Dokumen5 halamanVrushalirhatwal (14 0)GuruRakshithBelum ada peringkat
- Rizal ExaminationDokumen3 halamanRizal ExaminationBea ChristineBelum ada peringkat
- What Are RussiaDokumen3 halamanWhat Are RussiaMuhammad SufyanBelum ada peringkat
- India Marine Insurance Act 1963Dokumen21 halamanIndia Marine Insurance Act 1963Aman GroverBelum ada peringkat
- Report On Soap StudyDokumen25 halamanReport On Soap StudyAbhishek JaiswalBelum ada peringkat
- Caltech RefDokumen308 halamanCaltech RefSukrit ChatterjeeBelum ada peringkat
- Oration For Jon Kyle ValdehuezaDokumen2 halamanOration For Jon Kyle ValdehuezaJakes ValBelum ada peringkat
- Biometric Security ConcernsDokumen27 halamanBiometric Security ConcernsprinceuchenduBelum ada peringkat
- Darkness Points Reminder 2Dokumen2 halamanDarkness Points Reminder 2Tata YoyoBelum ada peringkat
- Institute of Actuaries of India: Subject CT3-Probability and Mathematical Statistics May 2008 ExaminationDokumen10 halamanInstitute of Actuaries of India: Subject CT3-Probability and Mathematical Statistics May 2008 ExaminationeuticusBelum ada peringkat
- Clothing, Personality and Impressions PDFDokumen11 halamanClothing, Personality and Impressions PDFAhmad RaoBelum ada peringkat
- Ylarde vs. Aquino, GR 33722 (DIGEST)Dokumen1 halamanYlarde vs. Aquino, GR 33722 (DIGEST)Lourdes Loren Cruz67% (3)
- Measure For Measure AngeloDokumen1 halamanMeasure For Measure AngeloRoger Knight100% (1)
- Reaction PaperDokumen3 halamanReaction PaperCecille Robles San JoseBelum ada peringkat
- Olinger v. The Church of Jesus Christ of Latter Day Saints Et Al - Document No. 1Dokumen4 halamanOlinger v. The Church of Jesus Christ of Latter Day Saints Et Al - Document No. 1Justia.comBelum ada peringkat
- Defending A Dogma: Between Grice, Strawson and Quine: Elvis ImafidonDokumen10 halamanDefending A Dogma: Between Grice, Strawson and Quine: Elvis ImafidonYang Wen-LiBelum ada peringkat
- Rape and Challenging Contemporary ThinkingDokumen17 halamanRape and Challenging Contemporary ThinkingKirthna MadhavanBelum ada peringkat
- IB Math Studies - Triangle Trigonometry Practice Key: MarkschemeDokumen45 halamanIB Math Studies - Triangle Trigonometry Practice Key: MarkschemeRafael Tayo0% (1)