Nutrition Care Plan - Dr. Dominguez
Diunggah oleh
Monique Angela Turingan Gangan0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
147 tayangan2 halamanA
Judul Asli
Nutrition Care Plan- Dr. Dominguez
Hak Cipta
© © All Rights Reserved
Format Tersedia
DOCX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniA
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
147 tayangan2 halamanNutrition Care Plan - Dr. Dominguez
Diunggah oleh
Monique Angela Turingan GanganA
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 2
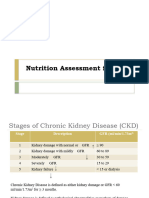
Nutrition Care Plan Dr.
Dominguez November 14, 2013
Condition Protein Requirement
Nutrition Care Plan Non- critically ill 0.8-2 gm/kg/day
How much and what type of nutrient to give (nutrient formulation) Critically ill, normal
Nutrient delivery process and monitoring determine the outcome or problem
success of the management process. Critically ill, with CKD
or dialysis
Components of Nutrition Care Plan Critically ill with CKD, 0.6-0.8 gm/kg/day
Nutritional assessment no dialysis
Nutritional requirements Burns 2.5 gm/kg/day
** Convert the TPR to kcal by multiplying TPR by 4 kcal/gm.
Nutritional Requirement **in the computation- use upper reference value (2, 0.8, 2.5)
Total Caloric Requirement
Total Protein Requirement Non- Protein Calories (NPC)
Non- Protein Calories NPC= TCR-TPR in calories
Electrolytes, vitamins, and trace elements
Condition CHO Fat
Total Caloric Requirement (TCR)
Usual 60-70% (70%) 30-40% (30%)
Condition Energy Factor
Critically ill (initial phase) 15-20 kcal/ kg/ day Critically ill 50% 50%
**in the computation- use 70% for CHO, and 30% for fat (usual condition), 50%
Critically ill (follow up phase) 20-25 kcal/ kg/ day CHO and 50% fat for critically ill
Non critically ill 25-30 kcal/ kg/ day
**in the computation- use upper reference value (20, 25, 30)
Body Composition Weight Reference to Use
Non- obese including ACTUAL/IDEAL/ESTIMATED
underweight body weight
Obese (BMI >/=30) IDEAL body weight
*IBW Formula
IBW for a woman may be estimated as 100 pounds for the first 5 feet plus
an additional 5 pounds for every inch over 5 feet. The IBW for a man is 106
pounds for the 5 feet plus an additional 6 pounds for every inch over 5
feet.
Total Protein Requirement (TPR)
Medical Nutrition Prelims Page 1
Nutrition Care Plan Dr. Dominguez November 14, 2013
1. CHO Formulation= NPCx % requirement divided by 4 kcal/ gm Nutrient Delivery
2. Fat Formulation= NPC x % requirement divided by 9 kcal/ gm Oral
Gastric feeding
Fluid Requirements: o Bolus (manual or gravity tube)
Usual complication: 30 ml/kg body wt o Intermittent or continuous using enteral pumps
Mostly dependent on fluid balance records Small intestine feeding
Critical care set up: include insensible water loss in the fluid balance o Intermittent or continuous using gravity drip
which is about 800- 1000ml/day o Enteral pumps
Access Monitoring Strategies
Oral Calorie count
Enteral Regular weight determinations (once a week)
o NGT Fluid balance
o PEG/ gastrostomy Complete blood count
o Jejunostomy Total lymphocyte count
Parenteral Nutrition Serum albumin
o Peripheral
o Central Case:
68- year old female
Nutrient Formulation Admission weight: 30kgs
Regular or special diet BMI: 12 kg/ m2
Oral supplements
Enteral Nutrition Dx: esophageal tumor
o Standard formulations: Pre- mixed solutions High risk/ severe malnutrition
o Modular formulations: Custom built- for the patients
o Special (elemental or semi- elemental) Nutrition Care Plan
Parenteral Nutrition
o Individual (amino acids, fat, dextrose) or 3 in 1 combinations TCR= 30 kgs x 20 kcal 600 kcal/ day
o Formulations for peripheral or central route
TPR= 30 kgs x 2 gm 60 gm/ day x 4 kcal/
g= 240 kcal/ day
NPC= 600 kcal- 240 kcal 360 kcal/ day
CHO= 360 kcal x 0.5/ 4 gm 45 gm/ day
Fat= 360 kcal x 0.5/ 9 gm 20 gm/ day
Fluid requirement= 30 ml x 30kg 900 ml/ day
Access
*PEG/ gastrostomy, jejunostomy, or Parenteral nutrition (Central)
Medical Nutrition Prelims Page 2
Anda mungkin juga menyukai
- AINAEDIToptimzing NutritionalDokumen69 halamanAINAEDIToptimzing Nutritionalgadis ainanurlailaBelum ada peringkat
- Nutritional Support in CHDDokumen31 halamanNutritional Support in CHDicuanak HarkitBelum ada peringkat
- Parenteral Nutrition Case StudyDokumen5 halamanParenteral Nutrition Case Studyapi-349873323100% (1)
- GNUR 297 (Nutrition) Exam 2 Study GuideDokumen17 halamanGNUR 297 (Nutrition) Exam 2 Study GuideMeghan Elizabeth100% (1)
- Optimizing Nutrition Therapy: Dr. Paul A Dwiyanu Pulmonologist, ConsultantDokumen69 halamanOptimizing Nutrition Therapy: Dr. Paul A Dwiyanu Pulmonologist, Consultantgadis ainanurlailaBelum ada peringkat
- NICU Resident Manual Chapter 3 Nutiriton 2013Dokumen17 halamanNICU Resident Manual Chapter 3 Nutiriton 2013kurniawatiBelum ada peringkat
- Total Parenteral NutritionDokumen12 halamanTotal Parenteral NutritionSheikhBelum ada peringkat
- Soap Note TPN MizeDokumen2 halamanSoap Note TPN Mizeapi-271354390Belum ada peringkat
- Nutrition in ICUDokumen18 halamanNutrition in ICUSi Thu Swe100% (2)
- Fluid and Nutrition in COVID (DR Prasenohadi)Dokumen23 halamanFluid and Nutrition in COVID (DR Prasenohadi)Ahmad ArbiBelum ada peringkat
- Total Parenteral NutritionDokumen32 halamanTotal Parenteral Nutritionlordoftheweb100% (13)
- ICU One Pager Enteral NutritionDokumen1 halamanICU One Pager Enteral NutritionjalilBelum ada peringkat
- Nutr 335 Adime NoteDokumen2 halamanNutr 335 Adime Noteapi-533845626Belum ada peringkat
- Triglyceride NCPDokumen2 halamanTriglyceride NCPapi-301024560Belum ada peringkat
- Nutr302l NCP NotesDokumen14 halamanNutr302l NCP Notesapi-271284613Belum ada peringkat
- Parenteral NutriDokumen11 halamanParenteral NutriMonica SurduBelum ada peringkat
- NutritionDokumen46 halamanNutritionKeren Karunya SingamBelum ada peringkat
- Oncology Case StudyDokumen3 halamanOncology Case Studyapi-622273373Belum ada peringkat
- Total Parenteral Nutrition: Presented byDokumen46 halamanTotal Parenteral Nutrition: Presented byMuhammad YamnainBelum ada peringkat
- Basic Nutrition PDFDokumen58 halamanBasic Nutrition PDFphinoetBelum ada peringkat
- Nutritional Support NotesDokumen14 halamanNutritional Support NotesAudrie Allyson GabalesBelum ada peringkat
- Nutrition PDFDokumen22 halamanNutrition PDFskBelum ada peringkat
- TPN ClassDokumen32 halamanTPN Classgamal attamBelum ada peringkat
- Parenteral Nutrition Recommendations For Pediatric PatientsDokumen14 halamanParenteral Nutrition Recommendations For Pediatric PatientsHenry M. BarberenaBelum ada peringkat
- 4 Assesmment + Case - FinalDokumen20 halaman4 Assesmment + Case - FinalSophie RoseBelum ada peringkat
- Pulm CDokumen10 halamanPulm CAqsa ShBelum ada peringkat
- Nutrition: - . - and The Surgical PatientDokumen39 halamanNutrition: - . - and The Surgical PatientJan Cyrill YuBelum ada peringkat
- Transdermal Drug Delivery SystemDokumen99 halamanTransdermal Drug Delivery SystemIshtiaq AhmedBelum ada peringkat
- NCM-105A-Exercise 15 AdultDokumen6 halamanNCM-105A-Exercise 15 AdultkathleyaBelum ada peringkat
- Glutaric Aciduria Type 1 (GA1) Dietetic Management PathwayDokumen7 halamanGlutaric Aciduria Type 1 (GA1) Dietetic Management PathwayMoroianu Irina-GabrielaBelum ada peringkat
- Pulm-C 3editedDokumen6 halamanPulm-C 3editedAqsa ShBelum ada peringkat
- Total Parenteral Nutrition:: By: Group 4Dokumen25 halamanTotal Parenteral Nutrition:: By: Group 4Mylz MendozaBelum ada peringkat
- Malnutrition AdimeDokumen2 halamanMalnutrition Adimeapi-508953960Belum ada peringkat
- Terapi Nutrisi: I Putu Pramana SuarjayaDokumen66 halamanTerapi Nutrisi: I Putu Pramana SuarjayaMouris DwiputraBelum ada peringkat
- 5 6 (TPN)Dokumen41 halaman5 6 (TPN)SAISH BBelum ada peringkat
- Oncology Nutrition FormularyDokumen2 halamanOncology Nutrition Formularyapi-530327871Belum ada peringkat
- Mini Case StudyDokumen3 halamanMini Case Studyapi-380538354Belum ada peringkat
- Reviewer For Nutrition and Diet TherapyDokumen4 halamanReviewer For Nutrition and Diet TherapyDa MiBelum ada peringkat
- GOLD 2020: Prepared and Presented byDokumen17 halamanGOLD 2020: Prepared and Presented byhamm hammmoudBelum ada peringkat
- NCP: Diabetes Mellitus Prepregnancy/GestationalDokumen11 halamanNCP: Diabetes Mellitus Prepregnancy/GestationalJavie85% (13)
- Referat NutrisiDokumen24 halamanReferat NutrisiYulisa Prahasti Dewa AyuBelum ada peringkat
- 2simpo Dialisis Terapi Nutrisi 2014Dokumen49 halaman2simpo Dialisis Terapi Nutrisi 2014tika.dyahmustikaBelum ada peringkat
- - - TPN presentation - نسخة-1 (3119)Dokumen24 halaman- - TPN presentation - نسخة-1 (3119)Dr mudasir nazirBelum ada peringkat
- 3 NUTRITION-FOR-HEALTH-AND-FITNESS-or-EATING-DISORDERS-or-BONE-AND-DENTAL-HEALTH-2Dokumen18 halaman3 NUTRITION-FOR-HEALTH-AND-FITNESS-or-EATING-DISORDERS-or-BONE-AND-DENTAL-HEALTH-2Trinidad SherwinBelum ada peringkat
- DM CaseDokumen14 halamanDM CaseNormana ZureikatBelum ada peringkat
- Penulisan Preskripsi Nutrisi Untuk Sp1 Dan Sp2Dokumen21 halamanPenulisan Preskripsi Nutrisi Untuk Sp1 Dan Sp2ndadilesBelum ada peringkat
- Metabolism in SurgeryDokumen5 halamanMetabolism in Surgeryjc_sibal13Belum ada peringkat
- Prof. Haerani - NutrisiDokumen29 halamanProf. Haerani - Nutrisirent3010Belum ada peringkat
- Syndrome Neurotic 2Dokumen5 halamanSyndrome Neurotic 2Msyr RaBelum ada peringkat
- Manajemen Nutrisi Pada Pasien PGK5 Dengan HDDokumen35 halamanManajemen Nutrisi Pada Pasien PGK5 Dengan HDASIS ADRIBelum ada peringkat
- Nutritional Support in ICU Patient TMKDokumen61 halamanNutritional Support in ICU Patient TMKhabtsh habshaBelum ada peringkat
- Neonatal Parenteral and Enteral Nutrition: A Resource Guide For The Student and Novice Neonatal Nurse PractitionerDokumen23 halamanNeonatal Parenteral and Enteral Nutrition: A Resource Guide For The Student and Novice Neonatal Nurse PractitionerMOHAMMED ALMAJEDBelum ada peringkat
- Malnutrition Case StudyDokumen3 halamanMalnutrition Case Studyapi-622273373Belum ada peringkat
- Eric Helms Nutrition CalculatorDokumen20 halamanEric Helms Nutrition CalculatorSmyle KatariaBelum ada peringkat
- MNT Renal Lab - Group 2 ChineseDokumen29 halamanMNT Renal Lab - Group 2 ChineseLEE JIE YEEBelum ada peringkat
- Apgh 4 18Dokumen2 halamanApgh 4 18Rashmi Ranjan BeheraBelum ada peringkat
- Neonatal Parenteral and Enteral NutritionDokumen23 halamanNeonatal Parenteral and Enteral NutritionPrimadiati Nickyta Sari100% (1)
- 2020 The Essential Diets - All Diets in One Book - Ketogenic, Mediterranean, Mayo, Zone Diet, High Protein, Vegetarian, Vegan, Detox, Paleo, Alkaline Diet and Much More: COOKBOOK, #2Dari Everand2020 The Essential Diets - All Diets in One Book - Ketogenic, Mediterranean, Mayo, Zone Diet, High Protein, Vegetarian, Vegan, Detox, Paleo, Alkaline Diet and Much More: COOKBOOK, #2Belum ada peringkat
- Ketogenic Weight Loss Diet for Beginners: Proven Secrets for Beginners Ketogenic Diet That Will Help You Burn Fat ForeverDari EverandKetogenic Weight Loss Diet for Beginners: Proven Secrets for Beginners Ketogenic Diet That Will Help You Burn Fat ForeverBelum ada peringkat
- Ketogenic Diet : No Sugar No Starch Diet To Turn Your Fat Into Energy In 7 Days (Bonus : 50 Easy Recipes To Jump Start Your Fat & Low Carb Weight Loss Today)Dari EverandKetogenic Diet : No Sugar No Starch Diet To Turn Your Fat Into Energy In 7 Days (Bonus : 50 Easy Recipes To Jump Start Your Fat & Low Carb Weight Loss Today)Penilaian: 3.5 dari 5 bintang3.5/5 (4)
- Testicular Ca NCCNDokumen90 halamanTesticular Ca NCCNMonique Angela Turingan GanganBelum ada peringkat
- Early Nutritional InterventionDokumen2 halamanEarly Nutritional InterventionMonique Angela Turingan GanganBelum ada peringkat
- Whats New in GINA 2021 FinalDokumen47 halamanWhats New in GINA 2021 FinalHeriestian eriesBelum ada peringkat
- Normal Urine Output: 30-60ml/min: Protein RequirementsDokumen6 halamanNormal Urine Output: 30-60ml/min: Protein RequirementsMonique Angela Turingan GanganBelum ada peringkat
- Nutrition Screening 2Dokumen2 halamanNutrition Screening 2Monique Angela Turingan GanganBelum ada peringkat
- Hyperlipidemias and Atherosclerosis Dr. ManaloDokumen3 halamanHyperlipidemias and Atherosclerosis Dr. ManaloMonique Angela Turingan GanganBelum ada peringkat
- Therapeutic Nutrition - Dr. ManaloDokumen2 halamanTherapeutic Nutrition - Dr. ManaloMonique Angela Turingan GanganBelum ada peringkat
- Diets in Fever and AnemiaDokumen6 halamanDiets in Fever and AnemiaMonique Angela Turingan GanganBelum ada peringkat
- 2019 Bar ExamDokumen7 halaman2019 Bar Examnathaniel50% (2)
- Diets in Fever and AnemiaDokumen6 halamanDiets in Fever and AnemiaMonique Angela Turingan GanganBelum ada peringkat
- Legal MedDokumen42 halamanLegal Medaisajane_rmt100% (6)
- Updated Covid GuidelinesDokumen42 halamanUpdated Covid GuidelinesMonique Angela Turingan GanganBelum ada peringkat
- Legal Medicine - ApmcDokumen10 halamanLegal Medicine - ApmcMonique Angela Turingan GanganBelum ada peringkat
- Legal Medicine ReviewerDokumen36 halamanLegal Medicine ReviewerMonique Angela Turingan Gangan100% (1)
- Recommended Allowance of Preference ProteinsDokumen2 halamanRecommended Allowance of Preference ProteinsMonique Angela Turingan GanganBelum ada peringkat
- UGIB Prob Sec To BPUD Vs Gastric Mass Alzheimer's DiseaseDokumen7 halamanUGIB Prob Sec To BPUD Vs Gastric Mass Alzheimer's DiseaseMonique Angela Turingan GanganBelum ada peringkat
- Guidelines On The Proper Recording of Physical Examination FindingsDokumen11 halamanGuidelines On The Proper Recording of Physical Examination Findingskitten garciaBelum ada peringkat
- Table of Lower Genital Tract Infections: Disease Etiology Pathogenesis SSX Diagnosis TreatmentDokumen3 halamanTable of Lower Genital Tract Infections: Disease Etiology Pathogenesis SSX Diagnosis TreatmentMonique Angela Turingan GanganBelum ada peringkat
- Respiratory DR - AntonioDokumen3 halamanRespiratory DR - AntonioMonique Angela Turingan GanganBelum ada peringkat
- Legal Medicine 1 Dr. RebosaDokumen1 halamanLegal Medicine 1 Dr. RebosaMonique Angela Turingan GanganBelum ada peringkat
- Nutrition in Git Diseases - DrramDokumen4 halamanNutrition in Git Diseases - DrramMonique Angela Turingan GanganBelum ada peringkat
- Inborn Errors of Metabolism - JjramDokumen4 halamanInborn Errors of Metabolism - Jjramjezreel terreBelum ada peringkat
- March 5, 2014 Lactose Intolerance in Infants and Children (Dr. Ramolete)Dokumen3 halamanMarch 5, 2014 Lactose Intolerance in Infants and Children (Dr. Ramolete)Monique Angela Turingan GanganBelum ada peringkat
- NUTRITION IN THE PRETERM AND SGA INFANTS/ Term Neonates/Children/Athletes-Dr. Ramolete Feb 5, 2014Dokumen6 halamanNUTRITION IN THE PRETERM AND SGA INFANTS/ Term Neonates/Children/Athletes-Dr. Ramolete Feb 5, 2014Monique Angela Turingan GanganBelum ada peringkat
- Diabetes Mellitus and Therapeutic Nutrition Dr. Manalo February 19, 2014Dokumen4 halamanDiabetes Mellitus and Therapeutic Nutrition Dr. Manalo February 19, 2014Monique Angela Turingan GanganBelum ada peringkat
- Inborn Errors of Metabolism - JjramDokumen2 halamanInborn Errors of Metabolism - JjramMonique Angela Turingan GanganBelum ada peringkat
- Inborn Errors of Metabolism - JjramDokumen4 halamanInborn Errors of Metabolism - Jjramjezreel terreBelum ada peringkat
- Inborn Errors of Metabolism - JjramDokumen2 halamanInborn Errors of Metabolism - JjramMonique Angela Turingan GanganBelum ada peringkat
- Surgical Nutrition-Dr. Cinio (Edited)Dokumen6 halamanSurgical Nutrition-Dr. Cinio (Edited)Monique Angela Turingan GanganBelum ada peringkat
- Diets in Fever and AnemiaDokumen4 halamanDiets in Fever and AnemiaMonique Angela Turingan GanganBelum ada peringkat
- Biblioshiny For BibliometrixDokumen6 halamanBiblioshiny For BibliometrixAngelaBelum ada peringkat
- Week 3 TLE 101 Implementing and Monitoring Infection Control Policies and ProceduresDokumen3 halamanWeek 3 TLE 101 Implementing and Monitoring Infection Control Policies and ProceduresJoel Mamocod100% (1)
- Health Information Calendar 2023Dokumen2 halamanHealth Information Calendar 2023HSE BGP HOBelum ada peringkat
- Unit 1: Introduction To Community Health Nursing Chapter 1: Fundamental Concepts of Community Health NursingDokumen140 halamanUnit 1: Introduction To Community Health Nursing Chapter 1: Fundamental Concepts of Community Health NursingChevelle Valenciano-GaanBelum ada peringkat
- Obesity in ChildrenDokumen15 halamanObesity in ChildrenJohn ConnorBelum ada peringkat
- Chapter 3-6 Biological Hazards PDFDokumen28 halamanChapter 3-6 Biological Hazards PDFAzib JuriBelum ada peringkat
- Assignment: Gollis UniversityDokumen11 halamanAssignment: Gollis UniversityAbdikaffi omarBelum ada peringkat
- Safe Motherhood Calcium Supplementation For Pregnant WomenDokumen14 halamanSafe Motherhood Calcium Supplementation For Pregnant WomenGa B B Orlongan0% (1)
- Hubungan Tingkat Pengetahuan, Sikap Terhadap Perilaku Cuci Tangan Pakai Sabun (CTPS) Pada SMPN 1 Surakarta Dan SMPN 6 SurakartaDokumen10 halamanHubungan Tingkat Pengetahuan, Sikap Terhadap Perilaku Cuci Tangan Pakai Sabun (CTPS) Pada SMPN 1 Surakarta Dan SMPN 6 SurakartaPlayer BucinBelum ada peringkat
- AKORIMO CHS DissertationDokumen101 halamanAKORIMO CHS Dissertationkamba bryanBelum ada peringkat
- Basic Concepts On Laboratory Biosafety-Converted - 1040766564Dokumen49 halamanBasic Concepts On Laboratory Biosafety-Converted - 1040766564johaylie porrasBelum ada peringkat
- Homework 3Dokumen10 halamanHomework 3sadiesadieBelum ada peringkat
- Azithromycin To Prevent Sepsis or Death in Women Planning A Vaginal BirthDokumen10 halamanAzithromycin To Prevent Sepsis or Death in Women Planning A Vaginal BirthLoisana Meztli Figueroa PreciadoBelum ada peringkat
- ECOLOGIC MODEL - CholedocholithiasisDokumen4 halamanECOLOGIC MODEL - CholedocholithiasisKristel PunoBelum ada peringkat
- Stage 1: Acute HIV Infection: Signs and SymptomsDokumen3 halamanStage 1: Acute HIV Infection: Signs and Symptomssalsa bilaBelum ada peringkat
- Medical Encounters in British IndiaDokumen82 halamanMedical Encounters in British Indiadarkknight2809100% (1)
- What Is Saturated FatDokumen12 halamanWhat Is Saturated FatAbhi kashyapBelum ada peringkat
- NCP Vaginal BleedingDokumen2 halamanNCP Vaginal Bleedingjayye.aronceBelum ada peringkat
- Water and Sanitation Thesis TopicsDokumen7 halamanWater and Sanitation Thesis Topicsshannongutierrezcorpuschristi100% (2)
- Cervical Incompetence Moh AbdallaDokumen46 halamanCervical Incompetence Moh AbdallaDr. mohammed50% (2)
- Vector Control Intro - Jan2019Dokumen18 halamanVector Control Intro - Jan2019rosana_527421859Belum ada peringkat
- WHO 2019 nCoV Advocacy - Brief Gender 2020.1 EngDokumen4 halamanWHO 2019 nCoV Advocacy - Brief Gender 2020.1 EnggrowlingtoyouBelum ada peringkat
- Jsa For PCCDokumen6 halamanJsa For PCCCICON EngineersBelum ada peringkat
- Kelompok 4 - UTS Kesling Pak RohimDokumen12 halamanKelompok 4 - UTS Kesling Pak RohimEni PurwaningsihBelum ada peringkat
- Pandemic Hotzone Na RulesDokumen8 halamanPandemic Hotzone Na RulesBelén Sánchez AlcaláBelum ada peringkat
- Mapeh Mps ElemDokumen3 halamanMapeh Mps ElemRodolfo Esmejarda Laycano Jr.Belum ada peringkat
- Study On The Incidence of Urinary Tract Infections, Organisms Causing It and Antibiotic Susceptibility in Patients With DIABETES MELLITUS IN AJIMS, MLORE" For The Registration of Dissertation To RajivDokumen26 halamanStudy On The Incidence of Urinary Tract Infections, Organisms Causing It and Antibiotic Susceptibility in Patients With DIABETES MELLITUS IN AJIMS, MLORE" For The Registration of Dissertation To RajivR Hari0% (1)
- 11.30.21 Large Event and Convention Masking Exception Guidance - FinalDokumen4 halaman11.30.21 Large Event and Convention Masking Exception Guidance - FinalFOX5 VegasBelum ada peringkat
- Nurse's NotesDokumen7 halamanNurse's NotesDelilah Murao MorlaBelum ada peringkat
- Buletin Farmasi 02/2013Dokumen19 halamanBuletin Farmasi 02/2013afiq83Belum ada peringkat