Articles: Background
Diunggah oleh
Will PridmoreJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Articles: Background
Diunggah oleh
Will PridmoreHak Cipta:
Format Tersedia
Articles
Iron absorption from oral iron supplements given on
consecutive versus alternate days and as single morning
doses versus twice-daily split dosing in iron-depleted
women: two open-label, randomised controlled trials
Nicole U Stoffel, Colin I Cercamondi, Gary Brittenham, Christophe Zeder, Anneke J Geurts-Moespot, Dorine W Swinkels, Diego Moretti*,
Michael B Zimmermann*
Summary
Background Current guidelines to treat iron deficiency recommend daily provision of ferrous iron divided through Lancet Haematol 2017;
the day to increase absorption. However, daily dosing and split dosing might increase serum hepcidin and decrease 4: 524–33
iron absorption from subsequent doses. Our study aim was to compare iron absorption from oral iron supplements Published Online
October 9, 2017
given on consecutive versus alternate days and given as single morning doses versus twice-daily split dosing.
http://dx.doi.org/10.1016/
S2352-3026(17)30182-5
Methods We did two prospective, open-label, randomised controlled trials assessing iron absorption using See Comment page e500
(⁵⁴Fe)-labelled, (⁵⁷Fe)-labelled, or (⁵⁸Fe)-labelled ferrous sulfate in iron-depleted (serum ferritin ≤25 µg/L) women *Senior authors
aged 18–40 years recruited from ETH Zurich and the University of Zurich, Switzerland. In study 1, women were Department of Health Science
randomly assigned (1:1) to two groups. One group was given 60 mg iron at 0800 h (±1 h) on consecutive days for and Technology, ETH Zürich,
14 days, and the other group was given the same doses on alternate days for 28 days. In study 2, women were assigned Zürich, Switzerland
to two groups, stratified by serum ferritin so that two groups with similar iron statuses could be formed. One group (N U Stoffel MSc,
C I Cercamondi PhD,
was given 120 mg iron at 0800 h (±1 h) and the other was given the dose split into two divided doses of 60 mg at C Zeder MSc, D Moretti PhD,
0800 h (±1 h) and 1700 h (±1 h) for three consecutive days. 14 days after the final dose, the groups were each crossed Prof M B Zimmermann MD);
over to the other regimen. Within-individual comparisons were done. The co-primary outcomes in both studies were Department of Laboratory
iron bioavailability (total and fractional iron absorption), assessed by measuring the isotopic label abundance in Medicine, Radboud University
Medical Centre, Nijmegen,
erythrocytes 14 days after administration, and serum hepcidin. Group allocations in both studies were not masked Netherlands
and primary and safety analyses were done on an intention-to-treat basis. The studies were registered at ClinicalTrials. (A J Geurts-Moespot BSc,
gov, numbers NCT02175888 (study 1) and NCT02177851 (study 2) and are complete. Prof D W Swinkels PhD); and
Department of Pediatrics,
Columbia University, College of
Findings For study 1, 40 women were enrolled on Oct 15–29, 2015. 21 women were assigned to the consecutive-day Physicians and Surgeons,
group and 19 to the alternate-day group. At the end of treatment (14 days for the consecutive-day group and 28 days New York, NY, USA
for the alternate-day group), geometric mean (–SD, +SD) cumulative fractional iron absorptions were 16·3% (9·3, 28·8) (Prof G Brittenham MD)
in the consecutive-day group versus 21·8% (13·7, 34·6) in the alternate-day group (p=0·0013), and cumulative total Correspondence to:
iron absorption was 131·0 mg (71·4, 240·5) versus 175·3 mg (110·3, 278·5; p=0·0010). During the first 14 days of Prof Michael B Zimmermann,
Laboratory of Human Nutrition,
supplementation in both groups, serum hepcidin was higher in the consecutive-day group than the alternate-day Department of Health Science
group (p=0·0031). In study 2, 20 women were enrolled between Aug 13 and 18, 2015. Ten women were assigned to and Technology, ETH Zürich,
receive once-daily dosing and ten were assigned to receive twice-daily divided dosing. No significant differences were Zürich 8092, Switzerland
seen in fractional (day 1–3 geometric mean: 11·8% [7·1, 19·4] once daily vs 13·1% [8·2, 20·7] twice daily; p=0·33) or michael.zimmermann@hest.
ethz.ch
total iron absorption (day 1–3: 44·3 mg [29·4, 66·7] once daily vs 49·4 [35·2, 69·4] twice daily; p=0·33) between the
two dosing regimens. Twice-daily divided doses resulted in a higher serum hepcidin concentration than once-daily
dosing (p=0·013). No grade 3 or 4 adverse events were reported in either study.
Interpretation In iron-depleted women, providing iron supplements daily as divided doses increases serum hepcidin
and reduces iron absorption. Providing iron supplements on alternate days and in single doses optimises iron
absorption and might be a preferable dosing regimen. These findings should be confirmed in iron-deficient anaemic
patients.
Funding Swiss National Science Foundation, Bern, Switzerland.
Introduction To compensate for this low absorption, large iron doses
Oral iron supplementation with ferrous sulfate (FeSO4) is are often administered, but large amounts of unabsorbed
a recommended approach to treat iron deficiency iron might worsen gastrointestinal symptoms and reduce
anaemia.1 However, iron absorption from supplements in compliance.3 Hepcidin is the central regulatory molecule
iron-depleted patients is low: 2–13% when consumed in iron metabolism in mammals,4 and oral doses of
with food and 5–28% when consumed without food.2 supplemental iron acutely increase serum hepcidin.5–7
www.thelancet.com/haematology Vol 4 November 2017 e524
Articles
Research in context
Evidence before this study iron absorption with weekly versus daily iron supplementation
We initially searched PubMed using the search terms in human beings.
“iron supplementation” OR “iron supplements” OR “oral iron”,
Added value of this study
with no language or date restrictions. The date of our first
In this study, done in iron-depleted women using multiple iron
search was Jan 13, 2015, and our last search was on
stable isotope labels and serum hepcidin profiles, we
April 24, 2017. Many papers recommend oral iron
quantitatively assessed iron absorption from different dosing
supplementation to treat iron deficiency or iron deficiency
regimens by measuring cumulative isotopic label abundance in
anaemia, or both. Most guidelines and textbooks recommend
red blood cells 14 days after administration. We assessed iron
daily provision of ferrous iron divided throughout the day to
absorption, comparing consecutive-day versus alternate-day
increase absorption. Iron absorption from oral supplements
dosing over 28 days and single morning doses versus divided
measured using stable isotopes or radioisotopes of iron is
daily doses. We show that alternate-day oral supplementation
generally in the range of 5–30%. Several studies have reported
with 60 mg iron results in 34% higher iron absorption than
that acute oral doses of iron increase serum hepcidin.
with consecutive-day supplementation. We also show that
One short-term study using stable iron isotopes showed that
splitting a single oral dose of 120 mg iron into two daily doses
daily iron dosing and afternoon dosing might reduce iron
of 60 mg iron does not improve iron absorption.
absorption from subsequent doses. We could find no studies
that assessed whether these short-term effects on fractional Implications of all the available evidence
and total iron absorption persist during longer-term By contrast with most current recommendations on iron
supplementation, and no studies that directly compared iron supplementation, our findings suggest that providing oral iron
absorption using stable iron isotopes from single versus on alternate days in single morning doses increases iron
divided daily doses. Meta-analyses found daily iron absorption in young women and is an effective regimen to
supplementation to result in more side-effects than weekly optimise iron absorption. This regimen not only improves iron
or intermittent supplementation, but relative efficacy was absorption but also, because of its simplicity, might increase
uncertain. A previous study found no difference in fractional compliance.
We recently compared fractional absorption from a single administration.11 Large amounts of unabsorbed oral iron
oral dose of iron versus two consecutive day doses, and might cause gut inflammation, which might be due to
reported that fractional absorption from the second day’s irritation of the gut mucosa by high luminal
dose is decreased and associated with higher serum concentrations of free iron, adverse changes in the gut
hepcidin;5 both the decrease in fractional absorption and microbiota, or both.12 Faecal calprotectin is a non-specific
the increase in serum hepcidin were more pronounced at marker of gut inflammation that reflects neutrophil
higher doses. However, whether or not these short-term infiltration of the mucosa.13 Intestinal fatty acid binding
effects occur and persist during long-term supple- protein (I-FABP) is released into the bloodstream by
mentation is uncertain. A previous study found no damaged enterocytes14 and is a sensitive marker for
difference in fractional absorption between weekly and enterocyte injury.15 Therefore, we did two studies to assess
daily iron supplementation in women.2 the following hypotheses: (1) oral iron doses of 60 mg given
To treat iron deficiency, splitting an iron dose over the on alternate days for 28 days would result in higher
day, either into two or three divided doses, is commonly fractional and total absorption but lower faecal cal
recommended8 and thought to increase tolerability and protectin and I-FABP than when given every day for
bioavailability; however, little evidence supports this 14 days (equal total doses); (2) during 3 days of supple
practice. Because serum hepcidin follows a circadian mentation, splitting doses of 120 mg iron into two daily
rhythm and increases during the day,9 and the acute divided doses of 60 mg would not result in higher
hepcidin increase triggered by a morning dose augments fractional or total absorption than giving one 120-mg dose
this diurnal increase, afternoon doses might be particularly in the morning (equal total doses). In both studies, iron
poorly absorbed.5 We previously showed that administering bioavailability was assessed by measuring the isotopic
three oral iron doses of 60 mg in the morning, afternoon, label abundance in red blood cells 14 days after
and the following morning resulted in total iron absorption administration.
similar to two consecutive daily morning doses of 60 mg.5
However, whether iron absorption is higher from the same Methods
daily dose given entirely in the morning than that given in Study design and participants
two divided doses is uncertain. These open-label, randomised controlled trials were
Adverse gastrointestinal side-effects might be less done at the Human Nutrition Laboratory of the ETH
common with lower oral iron doses10 and intermittent Zurich in Zurich, Switzerland.
e525 www.thelancet.com/haematology Vol 4 November 2017
Articles
Healthy women were recruited by a study author (NUS) patient about adverse symptoms occurring since the
from the students and staff of ETH Zurich and the preceding iron dose. We measured I-FABP in serum and
University of Zurich, Switzerland, by email announcement. calprotectin in a fecal sample at baseline and after the
Inclusion criteria were as follows: age 18–45 years; depleted last supplement intake (at 14 days or 28 days).
iron stores, defined as serum ferritin 25 µg/L or less; In study 2, using a crossover design, patients received
haemoglobin more than 8 g/dL (to exclude individuals FeSO4 on three consecutive days, either as a single dose or
with moderate-to-severe anaemia); C-reactive protein split into a morning and an afternoon dose. Half of the
(CRP) less than 5 mg/L (to exclude individuals with participants started with the single dosing, the other half
inflammation); body-mass index 18·5–26·5 kg/m²; body started with the split dosing. Doses on the three different
weight less than 80 kg (to exclude overweight or obese supplementation days were labelled with ⁵⁴Fe, ⁵⁷Fe, and
patients because they often have subclinical inflammation); ⁵⁸Fe in both groups. Participants received a standardised
no chronic medication (except contraceptives); no major diet for the six study days. Patients were assigned to start
chronic disease; not pregnant or lactating; no blood with one of the two dosing regimens, and then crossed over
donation in the previous 4 months (because recent blood to the other regimen 14 days after finishing the first
donation might simulate erythropoiesis); non-smoking; regimen. For the single-dose regimen, 120 mg iron was
and no intake of mineral and vitamin supplements within administered at 0800 h (±1 h); for the split-dose regimen,
2 weeks of the study start (appendix). Exclusion criteria 60 mg was administered at 0800 h (±1 h) and again at See Online for appendix
were inability to follow study procedures or development 1700 h (± 1 h). As in study 1, participants were given the iron
of major illness. The studies were approved by the Zurich dose after an overnight fast and fasted for 3 h after the dose,
Cantonal Ethics Committee. All participants provided except a provided snack (yoghurt) at 1·5 h after the dose.
written informed consent. Participants receiving the twice-daily dosing had lunch
between 1100 h and 1300 h and dinner between 2000 h and
Randomisation and masking 2100 h so that they were fasting when receiving the
For study 1, participants were individually randomly afternoon iron dose. Before each iron dose, a venepuncture
assigned to the two study groups by a study author (NUS) blood sample (about 8 mL) was collected and the adverse
using a computer program; this author was involved in symptoms questionnaire was completed for each patient.
the rest of the trial. The number of participants per group Supplements consisted of 60 or 120 mg iron as
was defined, randomisation was done nine times, and of pharmaceutical grade (Ph.Eur.7·2) anhydrous FeSO4
the nine randomisations, we chose the schedule with the (Lohmann GmbH, Emmerthal, Germany) in gelatin
most similar means and SDs for haemoglobin and capsules administered with 200 mL of deionised
serum ferritin in both groups. high-purity water containing 0·5 mg (study 1) and 4 mg
For study 2, we assigned participants in a 1:1 ratio to (study 2) of labelled FeSO4 in the form of (⁵⁷Fe)-FeSO4,
two groups, stratified by serum ferritin, to have similar (⁵⁸Fe)-FeSO4, or (⁵⁴Fe)-FeSO4 (Chemgas, Boulogne-
iron statuses in both groups. For group assignment, Billancourt, France), prepared as previously described.16
NUS ordered the participants from the lowest to the Haemoglobin was measured with a Coulter counter.
highest baseline serum ferritin value and participants Blood was centrifuged at 3000 rpm for 10 min, and serum
were distributed equally to the two groups across the was stored at –20°C until the day of analysis. Serum was
range of serum ferritin values. Group assignment was analysed for serum ferritin, soluble transferrin receptor
not masked in either study. (sTfR), CRP, and alpha-1-acid glycoprotein (AGP) using a
multiplex ELISA.17 CRP and AGP are complementary
Procedures measures of systemic imflammation.17 Anaemia was
In study 1, we administered 60 mg iron as FeSO4 at defined as haemoglobin less than 12 g/dL; iron deficiency
0800 h (±1 h) either on 14 consecutive days or on alternate was defined as serum ferritin less than 15 µg/L or sTfR
days for 28 days. We labelled the first seven FeSO4 doses more than 8·3 mg/L, or a combination of these.18
with ⁵⁷Fe and the second seven doses with ⁵⁸Fe so that we Inflammation was defined as a CRP more than 5 mg/L or
could compare iron absorption from the first seven doses AGP more than 1 g/L. Serum iron and total iron binding
with that of the second seven doses. Participants were capacity (TIBC) were measured using colourimetry, and
given the iron dose after an overnight fast and fasted for transferrin saturation (%TS) was calculated using the
3 h after the dose, except for a provided snack (yoghurt) formula (serum iron/TIBC) × 100. Serum hepcidin was
at 1·5 h after the dose. The yoghurt was provided so the measured using c-ELISA.19 Serum samples were analysed
participants would not have to fast for the entire morning, for I-FABP using ELISA (Hycult Biotech, Uden,
and the small amount of calcium in the yoghurt was Netherlands); the manufacturer does not supply a refer
unlikely to affect iron absorption when consumed at ence range, but a study in 20 healthy European adults
1·5 h after the iron dose. A venepuncture blood sample reported a median value of 127 pg/mL (IQR 57–311).20
(about 8 mL) was collected just before administration of Stool samples were analysed for calprotectin using ELISA
each iron dose. Before administration of each iron dose, (Calprest, Eurospital, Trieste, Italy); the manufacturer’s
a structured questionnaire was completed for each reference range is less than 50 µg/g faeces.
www.thelancet.com/haematology Vol 4 November 2017 e526
Articles
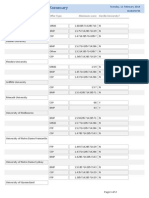
Consecutive-day Alternate-day p value
128 women assessed for eligibility
dosing for 14 days dosing for 28 days
Fractional iron absorption, %
88 excluded because they did not meet the Week 1, first 16·1 (8·9, 28·9) 21·3 (13·2, 34·3) 0·13
inclusion criteria seven doses
Week 2, second 16·6 (9·4, 29·6) 22·3 (13·9, 35·8) 0·11
seven doses
40 women randomly assigned
All 14 doses 16·3 (9·3, 28·8) 21·8 (13·7, 34·6) 0·0013
Total iron absorption, mg
Weeks 1 and 2, 66·9 (36·9, 121·1) 88·0 (54·8, 141·4) 0·13
21 allocated to consecutive-day supplementation 19 allocated to alternate-day supplementation first seven doses
Weeks 3 and 4, 69·3 (39·3, 122·2) 92·7 (58·8, 146·2) 0·11
second
3 discontinued intervention 2 discontinued intervention seven doses
2 refused supplements 1 refused supplements All 14 doses 131·0 (71·4, 240·5) 175·3 (110·3, 278·5) 0·0010
1 developed influenza 1 refused venepuncture
Data are geometric means (–SD, +SD). Analysed with mixed-effect models with
group as fixed factor and participant as random factor (fixed-effect estimation
18 completed allocated treatment 17 completed allocated treatment obtained with bootstrapping).
Table 2: Cumulative fractional and total iron absorption in study 1
21 included in analysis 19 included in analysis
Figure 1: Trial profile for study 1 in the blood, using the principles of isotopic dilution, and
assuming 80% incorporation of the absorbed iron into the
erythrocytes.22 The total absorbed iron was calculated by
Study 1 Study 2
multiplying the cumulative dose of iron administered
Consecutive-day Alternate-day dosing All women (n=20) over the study period by the fractional iron absorption.23
dosing (n=21) (n=19)
Haemoglobin, g/dL 12·8 (11·7, 14·0) 13·2 (12·5, 14·0) 13·1 (0·9) Outcomes
Serum ferritin, µg/L 13·8 (6·5, 29·3) 13·8 (8·1, 23·5) 20·0 (9·6) The coprimary outcomes in both studies were iron
Serum sTfR, mg/L 6·2 (3·6, 10·6) 5·6 (4·1, 7·5) 5·77 (3·82, 8·71) bioavailability (total and fractional iron absorption), assessed
Serum iron, µM 17·61 (6·72) 18·55 (6·13) 16·6 (6·6) by measuring the isotopic label abundance in erythrocytes
TIBC, µM 81·7 (75·3, 88·6) 83·4 (77·4, 89·9) 80·2 (9·3) 14 days after administration of final supplement, and
Transferrin saturation, % 21·5 (8·0) 22·1 (7·0) 21·1 (8·3) serum hepcidin concentration. The secondary outcomes in
Iron deficiency 10 (48%) 9 (47%) 6 (30%) study 1 were serum haemoglobin concentration, iron status
Serum hepcidin, nM 0·91 (0·49, 1·68) 0·63 (0·34, 1·14) 0·81 (0·38, 1·70) (defined by serum ferritin), and faecal calprotectin. Study 2
C-reactive protein, mg/L 0·80 (0·23, 2·72) 0·31 (0·08, 1·15) 0·18 (0·09–0·54) had no secondary outcomes. Safety was assessed using a
AGP, g/L 0·49 (0·25, 0·69) 0·44 (0·30, 0·65) 0·50 (0·13) forced-choice adverse symptoms questionnaire before each
I-FABP, pg/mL 364 (241, 550) 311 (196, 492) NA blood venepuncture, and adverse events were reported on a
Faecal calprotectin, µg/g faeces 3·65 (2·01, 6·61) 3·25 (1·59, 6·65) NA clinical report form.
Data are geometric mean (–SD, +SD), mean (SD), or n (%). sTFR=soluble transferrin receptor. TIBC=total iron binding
Statistical analysis
capacity. AGP=alpha-1-acid glycoprotein. I-FABP=intestinal fatty acid binding protein. NA=measurements not taken.
The sample size for study 2 was estimated to be
Table 1: Baseline characteristics of participants in studies 1 and 2 18 participants on the basis of data from previous iron
absorption studies providing FeSO4 supplements to
young women in our laboratory with an SD of 0·28 on
Iron absorption was assessed by measuring the log-transformed fractional iron absorption, a correlation
cumulative isotopic label abundance in red blood cells of absorption within participants of r=0·82, a type I error
14 days after the final iron dose. Blood samples were rate of 5%, and 80% power;5 this sample size would allow
analysed in duplicate for their iron isotopic composition us to detect a clinically relevant difference of 30% with
by multicollector inductively coupled plasma mass paired two-sided t tests. We estimated that 10% of parti
spectrometry (Neptune, Thermo-Finnigan, Bremen, cipants would drop out so aimed to recruit 20 people.
Germany) after microwave-assisted mineralisation with The previous SD of 0·28 on log-transformed fractional
nitric acid and separation of the iron from its sample iron absorption was derived from single labelled iron
matrix by anionic chromatography followed by a pre doses;5 we had no previous data from multiple admin
cipitation step with ammonium hydroxide.21 Fractional istrations on which to base our sample size calculation
absorption was calculated from isotopic ratios measured for study 1. We assumed that the cumulative measured
in blood samples and the concentration of iron circulating absorption from seven labelled doses per patient would
e527 www.thelancet.com/haematology Vol 4 November 2017
Articles
reduce the SD; this, combined with the use of two isotopes studies,5 fractional and total absorption were adjusted for
per patient (resulting in a doubling of observations), a serum ferritin level of 15 µg/L.24 In study 2, repeated-
would increase the power of the linear mixed-effects measures ANOVA was used to assess the effect of once-
model. We estimated that these effects would allow us to daily and twice-daily divided dosing. Fractional absorption,
distinguish a 30% difference in absorption between the serum hepcidin, serum ferritin, and TfR were the
consecutive-day and alternate-day regimens (two-sided, dependent variables for each separate model and the
between-patient comparisons) in study 1 with 18 patients dosing regimen and the day were added to the models as
per group. We estimated that 10% of participants would independent variables. For within-patient effects on
drop out so aimed to recruit 20 people per group. fractional absorption and serum hepcidin, dependent
Primary and safety analyses were done on an intention- sample t tests were used.Statistical analyses were done
to-treat basis. Normally distributed data were reported using SPSS (IBM SPSS statistics, version 22.0). The trials
as mean (SD), normally distributed data after log are registered at ClinicalTrials.gov, numbers NCT02175888
transformation were reported as geometric mean (study 1) and NCT02177851 (study 2).
(–SD, +SD), and non-normally distributed data after log
transformation were reported as median (IQR). In study 1, Role of the funding source
to assess the effects of consecutive and alternate dosing on The funder of the study had no role in study design, the
variables, we fitted linear mixed models. Since iron status collection, analysis, or interpretation of the data, or in the
and inflammatory markers are correlated, we did not writing of the report. NUS, DM, and MBZ had access to
correct p values for multiple comparisons. Dosing the raw data. MBZ had full access to all of the data and
regimen was defined as fixed effects, participants as the final responsibility to submit for publication.
random intercept effects using a variance component
structure matrix, and the corresponding baseline values Results
for each parameter as a covariate. To better estimate fixed- Between Oct 15 and Oct 29, 2015, 40 women were
effects estimates for fractional absorption, we did enrolled in study 1: 21 in the consecutive-day group and
bootstrapping (with resampling size of 1000). Log- 19 in the alternate-day group (figure 1). In the consecutive-
transformed data was used and estimates and CIs were day group, three women discontinued participation
obtained by back-transforming the obtained parameters. during the first week of supplementation (two refused to
To compare iron status and inflammation parameters take the supplements and one developed influenza) and
between the groups in study 1 at baseline, independent in the alternate-day group, two women discontinued
sample student t tests were used. When assessing the participation during the first 2 weeks of supplementation
effect of dosing regimen on serum hepcidin and iron (one refused to take the supplements and one refused
status parameters, baseline values of the corresponding venepuncture). The study was completed on Dec 14, 2015.
variable were included as covariates. Incidence of gastro Baseline characteristics of the women are shown in
intestinal side-effects was compared using the χ² test. To table 1. The median age of the women was 22 years
increase comparability of absorption data between the two (IQR 21–25) in the consecutive-day group and 22 years
study groups (study 1) and with previously published (21–24) in the alternate-day group. Four of the women
Consecutive-day dosing Alternate-day dosing for Group effect Time effect Time–group
for 14 days 28 days p value p value effect
pinteraction value
Haemoglobin, g/dL 13·2 (12·5, 14·0) 13·6 (12·9, 14·4) 0·16 0·90 0·70
Serum ferritin, µg/L 28·3 (15·7, 51·01) 23·6 (17·3, 32·1) 0·058 <0·0001 0·62
Serum sTfR, mg/L 6·3 (3·1, 12·6) 5·7 (4·1, 7·7) 0·99 0·0097 0·00028
Serum iron, µM 15·61 (5·40) 14·67 (6·22) 0·59 0·031 0·59
TIBC, µM 80·0 (74·6, 85·8) 83·4 (76·7, 90·6) 0·19 0·058 0·036
Transferrin saturation, % 18·4 (4·9) 18·5 (6·0) 0·40 0·081 0·43
Iron deficiency 3 (14%) 1 (5%) 0·56 <0·0001 0·59
Serum hepcidin, nM 1·09 (0·77, 1·54) 1·38 (0·78, 2·42) 0·23 0·024 <0·0001
C-reactive protein, mg/L 0·73 (0·26, 2·04) 0·65 (0·13, 3·19) 0·12 0·059 <0·0001
AGP (g/L) 0·39 (0·28, 0·56) 0·46 (0·31, 0·68) 0·086 0·80 0·0013
I-FABP, pg/mL 322 (119, 871) 251 (146, 433) 0·22 0·24 0·72
Faecal calprotectin, µg/g faeces 3·64 (2·14, 6·17) 3·97 (2·15, 7·34) 0·93 0·50 0·49
Data are geometric mean (–SD, +SD), mean (SD), or n (%). Group, time, and time by group effects are reported with no correction for multiple comparisons. sTFR=soluble
transferrin receptor. TIBC=total iron binding capacity. AGP=alpha-1-acid glycoprotein. I-FABP=intestinal fatty acid binding protein.
Table 3: Measurements after final supplement intake in study 1
www.thelancet.com/haematology Vol 4 November 2017 e528
Articles
were mildly anaemic (three in the consecutive-day and versus 175·3 mg (110·3, 278·5; p=0·0010; table 2).
one in the alternate-day group). No baseline differences During the intervention, we noted significant time–
were noted in any of the baseline variables. group interactions on sTfR, TIBC, CRP, and AGP
At the end of treatment (day 14 for the consecutive-day (table 3). An overall significant time–group interaction
group and day 28 for the alternate-day group), geometric on serum hepcidin was present for the entire duration of
mean (–SD, +SD) fractional iron absorptions were the study (p<0·0001 at 14 days in the consecutive-day
16·3% (9·3, 28·8) in the consecutive-day group versus group vs 28 days in the alternate-day group); serum
21·8% (13·7, 34·6) in the alternate-day group (p=0·0013), hepcidin was higher in the alternate-day group than the
and total iron absorption was 131·0 mg (71·4, 240·5) consecutive-day group at endpoint (table 3). By contrast,
during the first 14 days of supplementation in both
groups, we noted a significant time–group interaction
A
3·0 Consecutive
on serum hepcidin (p=0·0031), with higher serum
Alternate hepcidin in the consecutive-day group than the alternate-
2·5
day group (figure 2A, B). No significant time–group
interactions on faecal calprotectin or I-FABP were
p=0·0012 present (table 3). During the intervention, treatment
2·0
Serum hepcidin (nM)
group had a significant effect on cumulative fractional
and total iron absorption (table 2, figure 2C). Within
1·5
groups, no significant difference in fractional or total ab
sorption was noted when comparing the first seven
1·0
doses to the second seven doses (consecutive-day
dosing, p=0·73; alternate-day dosing, p=0·33; table 2 and
0·5
figure 2C).
All reported adverse events in study 1 were grade 1–2
0
First seven doses Second seven doses All doses (table 4). The total incidence of the two gastrointestinal
side-effects that were assessed (nausea and abdominal
B
pain) was 33% higher with consecutive-day dosing than
3·0 Consecutive with alternate-day dosing, although this difference was
Alternate not statistically significant (p=0·57).
2·5 Between Aug 13 and 18, 2015, 20 women were enrolled
in study 2: ten were assigned to the once-daily dosing
2·0 group, and ten were assigned to the twice-daily dosing
Serum hepcidin (nM)
group. Two women dropped out, one after completing the
1·5 once-daily dosing and one after completing the twice-daily
dosing, because they refused to take the supplements
1·0 (figure 3). The study was completed on Sept 25, 2015.
Baseline characteristics of the women (median age
0·5
27 years [IQR 24–30]) are shown in table 1. Two of the
women were mildly anaemic, and none had discernible
0
inflammation (defined by increased CRP or AGP). We did
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 not assess baseline differences between the two groups.
Day
Group allocation (one whole dose vs two divided doses)
C did not significantly affect either fractional or total
60 Consecutive iron absorption (p=0·33 for both) and no significant
Alternate
time–group interaction on fractional or total iron
50 absorption was seen (p=0·74 for both; table 5, figure 4A).
p=0·0013
Fractional iron absorption (%)
40
Figure 2: Serum hepcidin and fractional iron absorption in study 1
(A) Serum hepcidin concentrations in samples taken during the first seven iron
30 doses, the second seven doses, and during the entire supplementation phase,
by group. Circles show statistical outliers. (B) Serum hepcidin profile over the
study period presented as geometric means with shading indicating ±SD.
20
(C) Fractional absorption (%) during the first seven iron doses, the second
seven doses, and during the entire supplementation phase, by group. In (C)
10 and (A), the horizontal black lines show the median, the boxes show IQRs,
and whiskers show the range. A significant time–group interaction on serum
hepcidin over the duration of the study (p<0·0001) and a significant time effect
0
First seven doses Second seven doses All doses on serum hepcidin in both groups (p=0·024) was seen. Compared using paired
t test (A) and unpaired t test (C).
e529 www.thelancet.com/haematology Vol 4 November 2017
Articles
Study 1 Study 2
Consecutive-day dosing Alternate-day dosing Once-daily dosing Twice-daily dosing
Number of Number of Number of Number of Number of Number of Number of Number of
events people events people events people events people
(n=24) (n=21) (n=25) (n=19) (n=12) (n=10) (n=14) (n=10)
Nausea 11 (46%) 6 (29%) 6 (24%) 2 (11%) 1 (8%) 1 (10%) 2 (14%) 1 (10%)
Abdominal pain 5 (21%) 2 (10%) 3 (12%) 3 (16%) 2 (17%) 2 (26%) 2 (14%) 2 (20%)
Headache 4 (17%) 3 (14%) 11 (44%) 7 (37%) 9 (75%) 5 (50%) 10 (71%) 6 (60%)
Upper respiratory tract infection 4 (17%) 4 (19%) 5 (20%) 5 (26%) 0 0 0 0
Data are n (%). All events were grade 1–2; no grade 3–5 events were reported.
Table 4: Adverse events in studies 1 and 2
However, in both dosing regimens, a significant effect of
time on iron absorption (p<0·0001) was noted: absorption 74 women assessed for eligibility
on day 1 was significantly higher than on day 2 (p<0·0001)
or day 3 (p<0·0001), but did not differ significantly 54 excluded because they did not meet
between day 2 and day 3 (p=0·77). the inclusion criteria
Group allocation (p=0·013) and time (p<0·0001) had
significant effects on serum hepcidin, but no significant
20 women randomly assigned
time–group interaction was seen (p=0·40; table 5 and
figure 4B). During the 3 days, two daily divided doses
resulted in a significantly higher serum hepcidin than
once-daily dosing (p=0·013; table 5). In both dosing 10 allocated to daily supplementation followed 10 allocated to twice daily supplementation
by twice daily supplementation followed by daily supplementation
regimens, serum hepcidin was significantly higher on
day 2 (p<0·0001) and day 3 (p<0·0001) than on day 1, and
higher on day 2 versus day 3 (p=0·0066; table 5 and 1 discontinued intervention (refused 1 discontinued intervention (refused
figure 4B). During once-daily dosing, fractional supplement after completing daily supplement after completing twice-daily
supplementation phase) supplementation phase)
absorption and serum hepcidin were significantly
correlated on all three administration days: on day 1
(r=–0·485; p=0·035); day 2 (r=0·700; p=0·0012); day 3 9 completed allocated treatment 9 completed allocated treatment
(r=–0·535; p=0·018). By contrast, during divided dosing,
fractional absorption and serum hepcidin were signi
10 included in analysis 10 included in analysis
ficantly correlated on day 1 (r=–0·558; p=0·013), but not
on day 2 (r=–0·329; p=0·17) or day 3 (r=–0·239; p=0·33).
All reported adverse events in study 2 were grade 1–2 Figure 3: Trial profile for study 2
(table 4). The most common adverse event was headache
for both regimens, with nine in the once-daily dosing 2 weeks, during which consecutive-day dosing results in
group and ten in the twice-daily dosing group. significantly lower fractional and total absorption than
alternate-day dosing. The difference in total iron
Discussion absorption in study 1 between the two dosing regimens
The main findings of our studies are as follows: in iron- was approximately 44 mg. On the basis of these data,
depleted young women, alternate-day dosing of 60 mg alternate-day dosing, compared with consecutive-day
iron as FeSO4 significantly increases fractional and total dosing, would translate to an estimated difference in
iron absorption compared with dosing iron every day; and haemoglobin of approximately 7 g/L during a dosing
fractional and total absorption are not increased by regimen providing 1800 mg of iron (eg, 30 doses of
splitting a dose of 120 mg iron into two daily divided 60 mg).
doses. These data confirm and extend our previous short- We previously reported clear inverse associations
term studies.5 In those studies, also done in non-anaemic, between fractional absorption and serum hepcidin during
iron-depleted young women, we provided single morning two days of consecutive-day versus alternate-day iron
doses of isotopically labelled iron as FeSO4 (40–240 mg) supplementation.5 In our study, the simultaneous effects
given on one or two consecutive days. We showed that on serum hepcidin of repeated oral iron doses against a
24 h after doses of 60 mg or more, serum hepcidin was backdrop of improving iron status resulted in a more
significantly increased and fractional absorption was complex pattern. Although serum hepcidin gradually
decreased by 35–45%.5 Our findings in study 1 show that increased in both groups over time, consecutive-day dosing
this effect is maintained over a dosing schedule of resulted in higher serum hepcidin than alternate-day
www.thelancet.com/haematology Vol 4 November 2017 e530
Articles
Once-daily dosing Twice-daily dosing
Day 1 Day 2 Day 3 Day 1–3 Day 1 Day 2 Day 3 Day 1–3
Fractional iron 16·8 10·1 9·7 11·8 19·1 11·0 10·6 13·1
absorption, % (11·0, 25·7) (6·7, 15·1)* (6·0, 15·6)* (7·1, 19·4) (13·7, 26·7) (7·3, 16·4)* (7·1, 15·9)* (8·2, 20·7)
Total iron 17·5 10·8 10·4 44·3 19·8 11·7 11·4 49·4
absorption, mg (8·2, 37·3) (5·6, 20·7)* (5·2, 20·7)* (29·4, 66·7) (9·5, 41·3) (6·0, 22·7)* (5·9, 21·9)* (35·2, 69·4)
Serum hepcidin, 0·75 2·77 1·79 1·53 0·91 4·69 2·77 2·24
nM (0·40, 1·41) (0·88, 8·69)* (0·77, 4·18)*† (0·54, 4·32)‡ (0·40, 2·08) (2·01, 10·98)* (1·53, 5·02)*§ (0·80, 6·25)
Data are geometric means (–SD, +SD). Measurements were taken at 0800 h ±1 h each day before the iron dose. Fractional iron absorption and total iron absorption data are
adjusted for a serum ferritin concentration of 15 µg/L. Analysed by repeated-measures ANOVA with Bonferroni corrected multiple comparisons. A significant time effect on
fractional and total iron absorption was seen (p<0·0001 for both), but no group effect was seen. A significant time effect (p<0·0001) and group effect (p=0·013) was seen on
serum hepcidin. *p<0·0001 vs day 1; †p=0·024 vs day 2; ‡p=0·013 vs twice-daily dosing; §p=0·0051 vs day 2.
Table 5: Fractional and total iron absorption and serum hepcidin in study 2
group, possibly reflecting the longer supplementation
A period, but also improved iron status. Intracellular hepatic
50 Once daily
Twice daily
iron stores or hepatic endothelial cells might regulate
p<0·0001
p<0·0001 hepcidin translation independently from the known
p<0·0001
40 p<0·0001 signalling pathways, inducing hepcidin translation after an
Fractional iron absorption (%)
acute iron dose.25–27 An earlier study comparing weekly to
30
daily iron supplementation of 50 mg iron as radiolabelled
FeSO4 in 12 women found a non-significant 15% increase
with weekly supplementation (mean fractional absorption
20 was 9·8% for weekly vs 8·5% for daily supplementation);2
the difference to our findings might be because of the
10 smaller number of patients and lower dose in the previous
study.
Our findings in study 2 suggest that the common
0
practice of splitting an oral iron dose in two daily divided
B doses in an attempt to increase iron absorption is
25 unnecessary; divided dosing does not significantly affect
fractional or total absorption. This finding is consistent
p<0·0001
with our previous study5 in which we gave three 60-mg
20 p<0·0001
p=0·00015 iron doses (twice-daily dosing) within 24 h and reported
p<0·0001
that fractional and total absorption from three doses
Serum hepcidin (nM)
p=0·024
15 p=0·047 (two mornings and an afternoon) was not significantly
p=0·014
greater than that from two morning doses. Because of the
circadian regulation of iron metabolism, serum hepcidin
10
increases during the day and supplemental oral iron
p=0·039
enhances this effect.7,9 Our findings in study 2 might be
5 due to a combination of these effects: fractional absorption
from the 120 mg morning dose was decreased compared
0
with the 60 mg morning dose in the two daily divided
1 2 3 dosing, but this difference was largely offset by the
Days
decreased fractional absorption of the 60 mg afternoon
Figure 4: Fractional iron absorption and serum hepcidin in study 2 dose and the inhibiting effect of this afternoon dose on
Fractional iron absorption (A) and serum hepcidin (B). Horizontal black lines fractional absorption of the following 60 mg morning
show the median, boxes show IQRs, whiskers show ranges, and circles show
statistical outliers. A significant time effect on fractional and total iron absorption
dose. However, because we labelled the different days of
(both p<0·0001), but no group effect was seen. A significant time effect supplementation with different isotopes, rather than
(p<0·0001) and group effect (p<0·013) on serum hepcidin, but no significant labelling the morning and afternoon doses with different
time–group interaction was noted. Comparisons were done using paired t test. isotopes, we could not distinguish this effect.
In study 2, whether iron was given once daily or in
dosing during the initial 14-day phase of supplementation, two daily divided doses, serum hepcidin was lower on
possibly driven by the higher iron supplement frequency day 3 of supplementation than day 2, but without a
in the consecutive-day group. By contrast, serum hepcidin corresponding increase in iron absorption. These data
was higher in the second 14-day phase in the alternate-day are consistent with our previous data5 showing that
e531 www.thelancet.com/haematology Vol 4 November 2017
Articles
morning serum hepcidin on the day preceding oral iron In conclusion, our data show that providing 60–120 mg
administration is more predictive of iron absorption than iron on alternate days in single morning doses increases
is morning serum hepcidin on the day of administration. iron absorption in young women. This regimen not only
Additionally, although dosing regimen was a significant substantially improves iron absorption but also, because
predictor of serum hepcidin, with higher serum hepcidin of its simplicity, might increase compliance.
with two daily divided doses than with a single dose, iron Contributors
absorption did not differ significantly between two daily CIC, GB, DWS, DM, and MBZ conceived the studies and obtained
divided doses and once-daily dosing. funding. All authors contributed to the design of the trials. NUS, CIC,
DM, and MBZ conducted the studies. NUS and DM analysed the data
A meta-analysis comparing daily iron supplementation and wrote the first draft of the manuscript. All authors contributed to the
to intermittent supplementation found an overall decrease final version of the manuscript.
in reported side-effects for the intermittent dose.11 Our Declaration of interests
findings lend some support to this conclusion in that the DWS and AJG-M are employees of Hepcidinanalysis.com at
cumulative incidence of gastrointestinal side-effects was Radboud University and Medical Centre, a website that offers hepcidin
higher with consecutive-day dosing than with alternate- measurements for a fee. All other authors declare no competing interests.
day dosing, although this difference was not statistically Acknowledgments
significant. To assess adverse gastrointestinal effects from We would like to thank the participants, as well as the participating
nursing staff. This study was supported by the Swiss National Science
iron, we measured serum I-FABP and faecal calprotectin. Foundation (SNSF Grant: 320030_141044).
I-FABP is a cytosolic protein located mainly in mature
References
enterocytes of the small intestine, and is released into the 1 Cook JD. Diagnosis and management of iron-deficiency anaemia.
bloodstream after enterocyte damage.14 We are not aware Best Pract Res Clin Haematol 2005; 18: 319–32.
of any previous studies that have measured I-FABP in 2 Cook JD, Reddy MB. Efficacy of weekly compared with daily iron
supplementation. Am J Clin Nutr 1995; 62: 117–20.
response to oral iron supplementation. Faecal calprotectin 3 Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ.
is a biomarker for neutrophil infiltration of the gut wall, Ferrous sulfate supplementation causes significant gastrointestinal
and is increased in infectious and inflammatory con side-effects in adults: a systematic review and meta-analysis.
PLoS One 2015; 10: e0117383.
ditions.28 Previous controlled studies in African infants
4 Ganz T, Nemeth E. Hepcidin and iron homeostasis.
and children have shown that faecal calprotectin increases Biochim Biophys Acta 2012; 1823: 1434–43.
during iron treatment.12 In our study 1, we found no time 5 Moretti D, Goede JS, Zeder C, et al. Oral iron supplements
or treatment effects of dosing regimen on these bio increase hepcidin and decrease iron absorption from daily or
twice-daily doses in iron-depleted young women. Blood 2015;
markers, suggesting that oral iron supplementation 126: 1981–89.
in healthy young women does not cause significant 6 Lin L, Valore EV, Nemeth E, Goodnough JB, Gabayan V, Ganz T.
enterocyte damage or inflammation. Iron transferrin regulates hepcidin synthesis in primary hepatocyte
culture through hemojuvelin and BMP2/4. Blood 2007;
The strengths of this study are as follows: we studied 110: 2182–89.
iron-depleted young women (six of whom were mildly 7 Zimmermann MB, Troesch B, Biebinger R, Egli I, Zeder C,
anaemic), which is a target group for iron supple- Hurrell RF. Plasma hepcidin is a modest predictor of dietary iron
bioavailability in humans, whereas oral iron loading, measured by
mentation; in study 1, iron absorption and serum stable-isotope appearance curves, increases plasma hepcidin.
hepcidin profiles were accurately and repeatedly Am J Clin Nutr 2009; 90: 1280–87.
quantified by using stable iron isotope techniques and an 8 DeLoughery TG. Microcytic anemia. N Engl J Med 2014; 371: 2537.
immunoassay with high sensitivity over 14–28 days; 9 Schaap CC, Hendriks JC, Kortman GA, et al. Diurnal rhythm rather
than dietary iron mediates daily hepcidin variations. Clin Chem
tolerability and gastrointestinal effects were assessed 2013; 59: 527–35.
by interview (studies 1 and 2) and measurement of 10 Rimon E, Kagansky N, Kagansky M, et al. Are we giving too much
intestinal biomarkers (study 1); and in study 2, the iron? Low-dose iron therapy is effective in octogenarians.
Am J Med 2005; 118: 1142–47.
crossover design allowed within-patient comparisons of 11 Peña-Rosas JP, De-Regil LM, Dowswell T, Viteri FE.
iron absorption measurements and serum hepcidin. The Intermittent oral iron supplementation during pregnancy.
limitations of our study are as follows: we tested quite Cochrane Database Syst Rev 2012; 7: CD009997.
12 Zimmermann MB, Chassard C, Rohner F, et al. The effects of iron
small numbers of women because of the logistics and fortification on the gut microbiota in African children:
expense of using stable iron isotopes, which could have a randomized controlled trial in Cote d’Ivoire. Am J Clin Nutr 2010;
resulted in a β error in the comparisons of clinical 92: 1406–15.
13 Burri E, Beglinger C. The use of fecal calprotectin as a biomarker in
endpoints, such as side-effects; we did not study people gastrointestinal disease. Expert Rev Gastroent 2014; 8: 197–210.
with moderate-to-severe anaemia, who might respond 14 Pelsers MMAL, Namiot Z, Kisielewski W, et al. Intestinal-type
differently to those with no anaemia or mild anaemia; and liver-type fatty acid-binding protein in the intestine. Tissue
we assessed iron absorption using erythrocyte iron distribution and clinical utility. Clin Biochem 2003; 36: 529–35.
15 Schellekens DH, Grootjans J, Dello SA, et al. Plasma intestinal fatty
incorporation, which is a measure not only of intestinal acid-binding protein levels correlate with morphologic epithelial
iron absorption but also erythropoietic response and intestinal damage in a human translational ischemia-reperfusion
the utilisation of iron during the formation of new model. J Clin Gastroenterol 2014; 48: 253–60.
16 Moretti D, Zimmermann MB, Wegmuller R, Walczyk T, Zeder C,
erythrocytes; and subjective assessment of tolerability in Hurrell RF. Iron status and food matrix strongly affect the
study 1 might have been biased because the study was relative bioavailability of ferric pyrophosphate in humans.
not masked. Am J Clin Nutr 2006; 83: 632–38.
www.thelancet.com/haematology Vol 4 November 2017 e532
Articles
17 Erhardt JG, Estes JE, Pfeiffer CM, Biesalski HK, Craft NE. 23 Cercamondi CI, Egli IM, Mitchikpe E, et al. Total iron absorption
Combined measurement of ferritin, soluble transferrin receptor, by young women from iron-biofortified pearl millet composite
retinol binding protein, and C-reactive protein by an inexpensive, meals is double that from regular millet meals but less than that
sensitive, and simple sandwich enzyme-linked immunosorbent from post-harvest iron-fortified millet meals. J Nutr 2013;
assay technique. J Nutr 2004; 134: 3127–32. 143: 1376–82.
18 WHO. Iron deficiency anemia: assessment, prevention and control. 24 Cook JD, Dassenko SA, Lynch SR. Assessment of the role of
Geneva: World Health Organization, 2001. nonheme-iron availability in iron balance. Am J Clin Nutr 1991;
19 Kroot JJ, Laarakkers CM, Geurts-Moespot AJ, et al. 54: 717–22.
Immunochemical and mass-spectrometry-based serum hepcidin 25 Ramos E, Kautz L, Rodriguez R, et al. Evidence for distinct
assays for iron metabolism disorders. Clin Chem 2010; 56: 1570–79. pathways of hepcidin regulation by acute and chronic iron loading
20 Voth M, Duchene M, Auner B, Lustenberger T, Relja B, Marzi I. in mice. Hepatol 2011; 53: 1333–41.
I-FABP is a novel marker for the detection of intestinal injury in 26 Pantopoulos K. Iron regulation of hepcidin through Hfe and Hjv:
severely injured trauma patients. World J Surg 2017; common or distinct pathways? Hepatol 2015; 62: 1922–23.
doi:10·1007/s00268–017–4124–2. 27 Parrow NL, Fleming RE. Liver sinusoidal endothelial cells as iron
21 Hotz K, Krayenbuehl PA, Walczyk T. Mobilization of storage iron is sensors. Blood 2017; 129: 397–98.
reflected in the iron isotopic composition of blood in humans. 28 Konikoff MR, Denson LA. Role of fecal calprotectin as a biomarker
J Biol Inorg Chem 2012; 17: 301–09. of intestinal inflammation in inflammatory bowel disease.
22 Hosain F, Marsaglia G, Noyes W, Finch CA. The nature of internal Inflam Bowel Dis 2006; 12: 524–34.
iron exchange in man. Trans Assoc Am Physicians 1962; 75: 59–63.
e533 www.thelancet.com/haematology Vol 4 November 2017
Anda mungkin juga menyukai
- Frontiers in Clinical Drug Research - Hematology: Volume 3Dari EverandFrontiers in Clinical Drug Research - Hematology: Volume 3Belum ada peringkat
- Espresso Coffee PDFDokumen7 halamanEspresso Coffee PDFRoy ChaiBelum ada peringkat
- The Circulating PlateletDari EverandThe Circulating PlateletShirley A. JohnsonBelum ada peringkat
- Chapter 2Dokumen43 halamanChapter 2Puvaneswary SegharanBelum ada peringkat
- Carbapenem Resistant EnterobacteriaceaeDokumen15 halamanCarbapenem Resistant Enterobacteriaceaeja_sam_radivoje3093Belum ada peringkat
- Zidovudineinduced AnaemiaDokumen23 halamanZidovudineinduced AnaemiaSuresh ThanneruBelum ada peringkat
- Continuous Renal Replacement TherapyDokumen9 halamanContinuous Renal Replacement Therapydoc_next_doorBelum ada peringkat
- Introduction of CRRT 2006Dokumen25 halamanIntroduction of CRRT 2006yamtotlBelum ada peringkat
- Diagnosis and Management of Iron Deficiency Anaemia: A Clinical UpdateDokumen9 halamanDiagnosis and Management of Iron Deficiency Anaemia: A Clinical UpdateMARTHA ISABEL CHUNG REYES100% (1)
- DM Ppt. NewDokumen26 halamanDM Ppt. NewRio Ramon HilarioBelum ada peringkat
- Full Blood Count Apr04, DR Eva RaikDokumen7 halamanFull Blood Count Apr04, DR Eva RaikDanielcc LeeBelum ada peringkat
- Kidney Transplant Recipient BookDokumen24 halamanKidney Transplant Recipient BookIvo LeiteBelum ada peringkat
- Introduction To MRIDokumen49 halamanIntroduction To MRINahin AminBelum ada peringkat
- Alternate Day Versus Consecutive Day Oral Iron Supplementation - 2023 - EclinicDokumen11 halamanAlternate Day Versus Consecutive Day Oral Iron Supplementation - 2023 - Eclinicronaldquezada038Belum ada peringkat
- Bregman 2013-Hepcidin-THERAPHYDokumen5 halamanBregman 2013-Hepcidin-THERAPHYRINNY ARDINA S.ST., M.SiBelum ada peringkat
- RCT Irondose AdultsDokumen8 halamanRCT Irondose AdultsCristobal MendozaBelum ada peringkat
- SelviDokumen81 halamanSelvichaitanya suryawanshiBelum ada peringkat
- Therapeutic Effects of Oral Zinc Supplementation On Acute Watery Diarrhea With Moderate Dehydration: A Double-Blind Randomized Clinical TrialDokumen7 halamanTherapeutic Effects of Oral Zinc Supplementation On Acute Watery Diarrhea With Moderate Dehydration: A Double-Blind Randomized Clinical TrialRizqulloh Taufiqul Hakim BarsahBelum ada peringkat
- 271 592 1 SMDokumen7 halaman271 592 1 SMShandi Iriana SitorusBelum ada peringkat
- Ferrous Sulfate Supplementation CausesDokumen20 halamanFerrous Sulfate Supplementation CausesAF KoasBelum ada peringkat
- Development of Rat Model With Iron Deficiency AnemDokumen5 halamanDevelopment of Rat Model With Iron Deficiency AnemLimber Castro ChinoBelum ada peringkat
- Pediatric JournalDokumen5 halamanPediatric JournalSarah Martinauli HarahapBelum ada peringkat
- Iron Overload in Beta Thalassemia PDFDokumen5 halamanIron Overload in Beta Thalassemia PDFyesikaBelum ada peringkat
- Manoppo 2019Dokumen6 halamanManoppo 2019belveraqsunnyBelum ada peringkat
- Fullk 479Dokumen7 halamanFullk 479TanveerBelum ada peringkat
- 326 PDFDokumen13 halaman326 PDFAnugrah Adi Santoso100% (1)
- Effect of Iron Containing Supplements On Rats DenDokumen6 halamanEffect of Iron Containing Supplements On Rats Dendhea hutabaratBelum ada peringkat
- 13 PDFDokumen10 halaman13 PDFمحمدأميندماجBelum ada peringkat
- Rajkumari Linthoingambi - MeeDokumen6 halamanRajkumari Linthoingambi - Meechaitanya suryawanshiBelum ada peringkat
- Associations Between Dietary Intakes of Iron, Copper and Zinc With Risk of Type 2 Diabetes MellitusDokumen29 halamanAssociations Between Dietary Intakes of Iron, Copper and Zinc With Risk of Type 2 Diabetes MellitusNvo SpektarBelum ada peringkat
- Iron Deficiency in Young Children: A Risk Marker For Early Childhood CariesDokumen6 halamanIron Deficiency in Young Children: A Risk Marker For Early Childhood Carieswahyudi_donnyBelum ada peringkat
- Special Report Diagnosis and Management of Iron Deficiency in CKD: A Summary of The NICE Guideline Recommendations and Their RationaleDokumen11 halamanSpecial Report Diagnosis and Management of Iron Deficiency in CKD: A Summary of The NICE Guideline Recommendations and Their RationaledrnattoBelum ada peringkat
- Ijtk 11 (1) 78-80Dokumen3 halamanIjtk 11 (1) 78-80ZordaaaBelum ada peringkat
- PreethaDokumen91 halamanPreethaGunaBelum ada peringkat
- OralIronChelators PDFDokumen22 halamanOralIronChelators PDFMeydita MahardiBelum ada peringkat
- 03 - Can Diet-Induced Weight Loss Improve Iron Homoeostasis inDokumen16 halaman03 - Can Diet-Induced Weight Loss Improve Iron Homoeostasis inMatheus SouzaBelum ada peringkat
- A Study of Efficacy and Safety of Intravenous Iron Sucrose For The Treatment of Moderate Anaemia in Antenatal Women in South IndiaDokumen6 halamanA Study of Efficacy and Safety of Intravenous Iron Sucrose For The Treatment of Moderate Anaemia in Antenatal Women in South Indianazzz12Belum ada peringkat
- Comparison of Therapeutic Efficacy of Ferrous Ascorbate and Iron Polymaltose-EditedDokumen6 halamanComparison of Therapeutic Efficacy of Ferrous Ascorbate and Iron Polymaltose-EditedmariskaBelum ada peringkat
- Serum Magnesium Concentration in Children With Asthma: Original InvestigationDokumen4 halamanSerum Magnesium Concentration in Children With Asthma: Original InvestigationTanveerBelum ada peringkat
- Am J Clin Nutr 2008 Zimmermann 1026 31Dokumen6 halamanAm J Clin Nutr 2008 Zimmermann 1026 31Alanindra ALBelum ada peringkat
- MATERI 6 Mek. Toksisitas (Overdose)Dokumen7 halamanMATERI 6 Mek. Toksisitas (Overdose)PERMATASARI BKUBelum ada peringkat
- Tpmrss 6Dokumen12 halamanTpmrss 6Ale ZevallosBelum ada peringkat
- Comparative Study On Efficacy, Tolerability, and Cost of Different Iron Supplements Among Antenatal Women With Iron-Deficiency AnemiaDokumen8 halamanComparative Study On Efficacy, Tolerability, and Cost of Different Iron Supplements Among Antenatal Women With Iron-Deficiency AnemiaAjay DBelum ada peringkat
- Referensi Elabscience T2Dokumen12 halamanReferensi Elabscience T2Nandia SeptiyoriniBelum ada peringkat
- Ijmrhs Vol 2 Issue 4Dokumen321 halamanIjmrhs Vol 2 Issue 4editorijmrhsBelum ada peringkat
- European Journal of Biomedical AND Pharmaceutical SciencesDokumen3 halamanEuropean Journal of Biomedical AND Pharmaceutical SciencesMotasem Sirag Mohmmed othmanBelum ada peringkat
- Effect of Zinc Supplementation On Insulin Resistance and Metabolic Risk Factors in Obese Korean WomenDokumen5 halamanEffect of Zinc Supplementation On Insulin Resistance and Metabolic Risk Factors in Obese Korean WomenFahmy2015Belum ada peringkat
- Research Article: Prevalence, Predictive Factors, and Characteristics of Osteoporosis in Hyperthyroid PatientsDokumen7 halamanResearch Article: Prevalence, Predictive Factors, and Characteristics of Osteoporosis in Hyperthyroid Patientsdek fafaBelum ada peringkat
- Research Article: Prevalence, Predictive Factors, and Characteristics of Osteoporosis in Hyperthyroid PatientsDokumen8 halamanResearch Article: Prevalence, Predictive Factors, and Characteristics of Osteoporosis in Hyperthyroid PatientsMutiara DamayantiBelum ada peringkat
- Research Article: Prevalence, Predictive Factors, and Characteristics of Osteoporosis in Hyperthyroid PatientsDokumen8 halamanResearch Article: Prevalence, Predictive Factors, and Characteristics of Osteoporosis in Hyperthyroid PatientsMutiara DamayantiBelum ada peringkat
- The Efficacy of Divalent Iron Preparations With and Without Zinc in The Treatment of Iron Deficiency AnemiaDokumen5 halamanThe Efficacy of Divalent Iron Preparations With and Without Zinc in The Treatment of Iron Deficiency Anemiaerika phBelum ada peringkat
- 33 4 08-Dr Golmahammad LouDokumen4 halaman33 4 08-Dr Golmahammad LouCarloxs1Belum ada peringkat
- Polimorfismo AnemiaDokumen6 halamanPolimorfismo AnemiaAle ZevallosBelum ada peringkat
- Heme Vs Inorganic IronDokumen4 halamanHeme Vs Inorganic IronBlanca RuizBelum ada peringkat
- Pharmacokinetic Profile of Oral Magnesium HydroxideDokumen6 halamanPharmacokinetic Profile of Oral Magnesium HydroxideRegina Marsha XaveriaBelum ada peringkat
- A Prospective Randomized, Controlled Trial of Intravenous Versus Oral Iron For Moderate Iron Deficiency Anaemia of PregnancyDokumen11 halamanA Prospective Randomized, Controlled Trial of Intravenous Versus Oral Iron For Moderate Iron Deficiency Anaemia of Pregnancycharvindo vBelum ada peringkat
- Community and International NutritionDokumen6 halamanCommunity and International NutritionBarbara Bresani SalviBelum ada peringkat
- Journal Trace Elements in MedicineDokumen10 halamanJournal Trace Elements in MedicineOmar ReynosoBelum ada peringkat
- Copper MalnDokumen2 halamanCopper MalnTaufiq HidayatBelum ada peringkat
- 19355-Article Text-35885-1-10-20181211Dokumen14 halaman19355-Article Text-35885-1-10-20181211Vladimir LyubenovBelum ada peringkat
- IPTSDokumen2 halamanIPTSWill PridmoreBelum ada peringkat
- That Old Black Magic PDFDokumen2 halamanThat Old Black Magic PDFWill PridmoreBelum ada peringkat
- Shrek's Diverse Army of Fairytale Creatures Was Also Supported by Solid Costume Design and ADokumen2 halamanShrek's Diverse Army of Fairytale Creatures Was Also Supported by Solid Costume Design and AWill PridmoreBelum ada peringkat
- IJP Suicide Beliefs PDFDokumen2 halamanIJP Suicide Beliefs PDFWill PridmoreBelum ada peringkat
- Suicide EditorialDokumen4 halamanSuicide EditorialWill PridmoreBelum ada peringkat
- Is Suicide Prevention PossibleDokumen3 halamanIs Suicide Prevention PossibleWill PridmoreBelum ada peringkat
- Application FormDokumen1 halamanApplication FormWill PridmoreBelum ada peringkat
- Chemotherapy IntroductionDokumen12 halamanChemotherapy IntroductionWill PridmoreBelum ada peringkat
- 2014 Offers MedicineDokumen2 halaman2014 Offers MedicineWill PridmoreBelum ada peringkat
- Tefl GuideDokumen23 halamanTefl GuideWill PridmoreBelum ada peringkat
- Majesty - Prima Official EGuideDokumen287 halamanMajesty - Prima Official EGuideWill Pridmore100% (2)
- Work in Japanese Law FirmsDokumen8 halamanWork in Japanese Law FirmsWill PridmoreBelum ada peringkat
- Template For Public Transport FineDokumen2 halamanTemplate For Public Transport FineWill PridmoreBelum ada peringkat
- Wonderland Study GuideDokumen22 halamanWonderland Study GuideWill Pridmore67% (6)
- Basketball Referees PaperDokumen41 halamanBasketball Referees PaperWill PridmoreBelum ada peringkat
- Authorised Officers ActDokumen671 halamanAuthorised Officers ActWill PridmoreBelum ada peringkat
- Victorian Recreational Boating Safety HandbookDokumen156 halamanVictorian Recreational Boating Safety HandbookSofia PranaciptaBelum ada peringkat
- Letter of ComplianceDokumen1 halamanLetter of ComplianceWill PridmoreBelum ada peringkat
- Letter of ComplianceDokumen1 halamanLetter of ComplianceWill PridmoreBelum ada peringkat
- Change Your Insurance Form Public Sector DivisionDokumen8 halamanChange Your Insurance Form Public Sector DivisionWill PridmoreBelum ada peringkat
- Australia Counter Terrorism White Paper 2010Dokumen83 halamanAustralia Counter Terrorism White Paper 2010DaveBelum ada peringkat
- Working AbroadDokumen97 halamanWorking AbroadaequricoBelum ada peringkat
- Payback CallsDokumen14 halamanPayback CallsWill PridmoreBelum ada peringkat
- Code of Conduct For Public Transport Authorised OfficersDokumen9 halamanCode of Conduct For Public Transport Authorised OfficersWill PridmoreBelum ada peringkat
- Into The Woods - ScreenplayDokumen123 halamanInto The Woods - ScreenplayWill Pridmore100% (2)
- Medicine Admissions Guide 2015 2016 v1.1Dokumen80 halamanMedicine Admissions Guide 2015 2016 v1.1Will PridmoreBelum ada peringkat
- Ap, Lrrsisal of Roentgenograph, Ic: I SsayDokumen30 halamanAp, Lrrsisal of Roentgenograph, Ic: I SsayMindaugasStacevičiusBelum ada peringkat
- DP November 2017 Examination Schedule en PDFDokumen4 halamanDP November 2017 Examination Schedule en PDFSuperlucidoBelum ada peringkat
- Principles Involved in Baking 1Dokumen97 halamanPrinciples Involved in Baking 1Milky BoyBelum ada peringkat
- AppearancesDokumen4 halamanAppearancesReme TrujilloBelum ada peringkat
- Investigation of Skew Curved Bridges in Combination With Skewed Abutments Under Seismic ResponseDokumen5 halamanInvestigation of Skew Curved Bridges in Combination With Skewed Abutments Under Seismic ResponseEditor IJTSRDBelum ada peringkat
- Hashimoto's Thyroiditis: Veena RedkarDokumen10 halamanHashimoto's Thyroiditis: Veena RedkarSan RedkarBelum ada peringkat
- Javanese PeopleDokumen22 halamanJavanese PeopleDenisaBelum ada peringkat
- Beastlikebalsam - Muscle BuildingDokumen10 halamanBeastlikebalsam - Muscle BuildingBalsam LaaroussiBelum ada peringkat
- Cold Regions Science and TechnologyDokumen8 halamanCold Regions Science and TechnologyAbraham SilesBelum ada peringkat
- Eco JetDokumen15 halamanEco JetJustin CoyBelum ada peringkat
- Gondola CalculationDokumen6 halamanGondola CalculationBudi SusantoBelum ada peringkat
- The 10 Most Famousfilipino Artists and Their MasterworksDokumen3 halamanThe 10 Most Famousfilipino Artists and Their MasterworksGina MagtibayBelum ada peringkat
- Coding DecodingDokumen21 halamanCoding DecodingAditya VermaBelum ada peringkat
- G-3 L-17 Internal QuestionsDokumen4 halamanG-3 L-17 Internal QuestionsActivity MLZS BarhBelum ada peringkat
- 3 Curvilinear MotionDokumen50 halaman3 Curvilinear Motiongarhgelh100% (1)
- 08 - 2061 USTR 2222a (1) Supor EKVDokumen24 halaman08 - 2061 USTR 2222a (1) Supor EKVHassan Houdoud0% (1)
- Badminton ReviewerDokumen10 halamanBadminton ReviewerHailsey WinterBelum ada peringkat
- Science Magazine February 2020Dokumen133 halamanScience Magazine February 2020Elena González GonzálezBelum ada peringkat
- The Manufacture and Uses of Expanded Clay Aggregate: Thursday 15 November 2012 SCI HQ, LondonDokumen36 halamanThe Manufacture and Uses of Expanded Clay Aggregate: Thursday 15 November 2012 SCI HQ, LondonVibhuti JainBelum ada peringkat
- Wang Jinhui - Competitive Physics - Thermodynamics, Electromagnetism and Relativity (2019, World Scientific Publishing Co. Pte. LTD.)Dokumen961 halamanWang Jinhui - Competitive Physics - Thermodynamics, Electromagnetism and Relativity (2019, World Scientific Publishing Co. Pte. LTD.)Paritosh PandeyBelum ada peringkat
- Las Tech Drafting 3Q WKDokumen13 halamanLas Tech Drafting 3Q WKClemenda TuscanoBelum ada peringkat
- Isulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atDokumen1 halamanIsulat Lamang Ang Titik NG Tamang Sagot Sa Inyong Papel. (Ilagay Ang Pangalan, Section atMysterious StudentBelum ada peringkat
- Hypothesis Testing - IDokumen36 halamanHypothesis Testing - Isai revanthBelum ada peringkat
- Contoh CV / Daftar Riwayat HidupDokumen2 halamanContoh CV / Daftar Riwayat HiduprusmansyahBelum ada peringkat
- Pusheen With Donut: Light Grey, Dark Grey, Brown, RoséDokumen13 halamanPusheen With Donut: Light Grey, Dark Grey, Brown, RosémafaldasBelum ada peringkat
- Clocks (New) PDFDokumen5 halamanClocks (New) PDFAbhay DabhadeBelum ada peringkat
- 2017 Classification of Periodontal and Peri-Implant Diseases and Conditions. Decision Making Algorithms For Clinical PracticeDokumen40 halaman2017 Classification of Periodontal and Peri-Implant Diseases and Conditions. Decision Making Algorithms For Clinical PracticebbBelum ada peringkat
- Maintenance Páginas-509-580Dokumen72 halamanMaintenance Páginas-509-580Alexandra Gabriela Pacheco PrietoBelum ada peringkat
- Kami Export - Subject Complements-1 PDFDokumen3 halamanKami Export - Subject Complements-1 PDFkcv kfdsaBelum ada peringkat
- DJI F450 Construction Guide WebDokumen21 halamanDJI F450 Construction Guide WebPutu IndrayanaBelum ada peringkat
- Is That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeDari EverandIs That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifePenilaian: 5 dari 5 bintang5/5 (4)
- The Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsDari EverandThe Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsPenilaian: 4 dari 5 bintang4/5 (146)
- The Elements We Live By: How Iron Helps Us Breathe, Potassium Lets Us See, and Other Surprising Superpowers of the Periodic TableDari EverandThe Elements We Live By: How Iron Helps Us Breathe, Potassium Lets Us See, and Other Surprising Superpowers of the Periodic TablePenilaian: 3.5 dari 5 bintang3.5/5 (22)
- Monkeys, Myths, and Molecules: Separating Fact from Fiction, and the Science of Everyday LifeDari EverandMonkeys, Myths, and Molecules: Separating Fact from Fiction, and the Science of Everyday LifePenilaian: 4 dari 5 bintang4/5 (1)
- Chemistry for Breakfast: The Amazing Science of Everyday LifeDari EverandChemistry for Breakfast: The Amazing Science of Everyday LifePenilaian: 4.5 dari 5 bintang4.5/5 (90)
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincDari EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincPenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactDari EverandThe Nature of Drugs Vol. 1: History, Pharmacology, and Social ImpactPenilaian: 5 dari 5 bintang5/5 (5)
- Organic Chemistry for Schools: Advanced Level and Senior High SchoolDari EverandOrganic Chemistry for Schools: Advanced Level and Senior High SchoolBelum ada peringkat
- Handbook of Formulating Dermal Applications: A Definitive Practical GuideDari EverandHandbook of Formulating Dermal Applications: A Definitive Practical GuideBelum ada peringkat
- The Regenerative Grower's Guide to Garden Amendments: Using Locally Sourced Materials to Make Mineral and Biological Extracts and FermentsDari EverandThe Regenerative Grower's Guide to Garden Amendments: Using Locally Sourced Materials to Make Mineral and Biological Extracts and FermentsPenilaian: 5 dari 5 bintang5/5 (3)
- Water-Based Paint Formulations, Vol. 3Dari EverandWater-Based Paint Formulations, Vol. 3Penilaian: 4.5 dari 5 bintang4.5/5 (6)
- Transformer: The Deep Chemistry of Life and DeathDari EverandTransformer: The Deep Chemistry of Life and DeathPenilaian: 4.5 dari 5 bintang4.5/5 (13)
- Bioplastics: A Home Inventors HandbookDari EverandBioplastics: A Home Inventors HandbookPenilaian: 4 dari 5 bintang4/5 (2)
- Chemistry: a QuickStudy Laminated Reference GuideDari EverandChemistry: a QuickStudy Laminated Reference GuidePenilaian: 5 dari 5 bintang5/5 (1)
- Formulating, Packaging, and Marketing of Natural Cosmetic ProductsDari EverandFormulating, Packaging, and Marketing of Natural Cosmetic ProductsBelum ada peringkat
- A Perfect Red: Empire, Espionage, and the Quest for the Color of DesireDari EverandA Perfect Red: Empire, Espionage, and the Quest for the Color of DesirePenilaian: 4 dari 5 bintang4/5 (129)
- The Periodic Table of Elements - Alkali Metals, Alkaline Earth Metals and Transition Metals | Children's Chemistry BookDari EverandThe Periodic Table of Elements - Alkali Metals, Alkaline Earth Metals and Transition Metals | Children's Chemistry BookBelum ada peringkat
- Science Goes Viral: Captivating Accounts of Science in Everyday LifeDari EverandScience Goes Viral: Captivating Accounts of Science in Everyday LifePenilaian: 5 dari 5 bintang5/5 (1)
- Essential Oil Chemistry Formulating Essential Oil Blends that Heal - Aldehyde - Ketone - Lactone: Healing with Essential OilDari EverandEssential Oil Chemistry Formulating Essential Oil Blends that Heal - Aldehyde - Ketone - Lactone: Healing with Essential OilPenilaian: 5 dari 5 bintang5/5 (1)