Subjective and Objective
Diunggah oleh
Raya Ibarra Lumogdang0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
10 tayangan2 halamanCool clinical pharmacy cases
Hak Cipta
© © All Rights Reserved
Format Tersedia
DOCX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniCool clinical pharmacy cases
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
10 tayangan2 halamanSubjective and Objective
Diunggah oleh
Raya Ibarra LumogdangCool clinical pharmacy cases
Hak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 2
SUBJECTIVE:
Patient’s complain of abdominal tenderness, nausea, and
vomiting. 2 days ago, patient experienced nausea, vomiting,
diarrhoea and chills.
OBJECTIVE:
Physical examinations: ill-appearing woman who is lethargic but
responsive
Temperature: 37˚C
Skin turgor: poor
Mucous membrane: dry
Eyeballs: shrunken and soft
Lungs: clear but respirations are deep and her breath has a fruity odor
Cardiac examination: within normal limits
Vital signs: Result Normal range Implication
Supine position:
Pulse rate 115 beats/min. 60-100 High
beats/min
Blood pressure 105/60 mmHg 120/80 mmHg Low
Upright position:
Pulse rate 140 beats/min 60-100 High
beats/min
Blood pressure 85/40 mmHg 120/80 mmHg Low
Electrolytes and Result Normal range Implication
Blood chemistry:
Blood glucose 750mg/dL 70-110mg/dL High
Sodium 148 mEq/L 135- 147 mEq/L High
Potassium 5.4 mEq/L 3.5-5.0 mEq/L High
Chlorine 106mEq/L 95-105 mEq/L High
Bicarbonate 6mEq/L 22-28 mEq/L Low
SrCr 2.0 mg/dL 0.6-1.2 mg/dL High
Complete blood Result Normal range Implication
count:
Hemoglobin 14.7g/dL 11.5-15.5g/Dl Normal
Hematocrit 49% 33%-43% High
WBC 15,000mm^3 3,200- High
9,800mm^3
Bands 3% 3-5% Normal
Polymorphonuclear 70% 54-62% High
neutrophils
Lymphocytes 27% 25-33% Normal
Serum ketones negative Normal
Urinalysis: Result Normal range Implication
Glucose 2% 0 High
pH 5.5 2.6-8 Normal
Specific gravity 1.029 1.020-1.025 High
Arterial blood gas: Result Normal range Implication
pH 7.05 7.36-7.44 Low
Pco2 20 mmHg 35-45 mmHg Low
Po2 120 mmHg 90-100 mmHg High
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
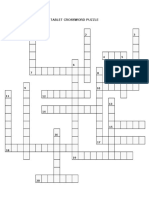
- PCOL2 CrosswordDokumen4 halamanPCOL2 CrosswordRaya Ibarra LumogdangBelum ada peringkat
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- CS2PDokumen3 halamanCS2PRaya Ibarra LumogdangBelum ada peringkat
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Pcol2 CrossDokumen1 halamanPcol2 CrossRaya Ibarra LumogdangBelum ada peringkat
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Hard Copy Sublingual FinalDokumen7 halamanHard Copy Sublingual FinalRaya Ibarra LumogdangBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Tablet PuzzleDokumen3 halamanTablet PuzzleRaya Ibarra LumogdangBelum ada peringkat
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- States of Matter NotesDokumen8 halamanStates of Matter NotesRaya Ibarra LumogdangBelum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Organizational Chart of Quality Control LaboratoryDokumen1 halamanOrganizational Chart of Quality Control LaboratoryRaya Ibarra Lumogdang100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- PCOGDokumen1 halamanPCOGRaya Ibarra LumogdangBelum ada peringkat
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- NailDokumen7 halamanNailRaya Ibarra LumogdangBelum ada peringkat
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- CholeraDokumen1 halamanCholeraRaya Ibarra LumogdangBelum ada peringkat
- Toxi Prelim To Finals 1Dokumen7 halamanToxi Prelim To Finals 1Raya Ibarra LumogdangBelum ada peringkat
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- ToxiiiiiiDokumen6 halamanToxiiiiiiRaya Ibarra LumogdangBelum ada peringkat
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A.M. P.M. Number Of: Name & Signature of Pharmacists-in-ChargeDokumen4 halamanA.M. P.M. Number Of: Name & Signature of Pharmacists-in-ChargeRaya Ibarra LumogdangBelum ada peringkat
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Carbon Disulfide: Sulfocyanate Test Lead Acetate TestDokumen1 halamanCarbon Disulfide: Sulfocyanate Test Lead Acetate TestRaya Ibarra LumogdangBelum ada peringkat
- Experiment 6 9 (Docu)Dokumen1 halamanExperiment 6 9 (Docu)Raya Ibarra LumogdangBelum ada peringkat
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Lab Report Act 6Dokumen6 halamanLab Report Act 6Raya Ibarra LumogdangBelum ada peringkat
- PLAN1Dokumen3 halamanPLAN1Raya Ibarra LumogdangBelum ada peringkat
- Pyra TBDokumen6 halamanPyra TBRaya Ibarra LumogdangBelum ada peringkat
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Urine PracticeDokumen11 halamanUrine PracticeJack Eito NeoBelum ada peringkat
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Lisgoold Cemetary RegisterDokumen15 halamanLisgoold Cemetary Registersmartin166100% (2)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Warli Art in Chennai: Young NightingaleDokumen8 halamanWarli Art in Chennai: Young NightingalerevatheeBelum ada peringkat
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Physiology of The Elite RowerDokumen8 halamanPhysiology of The Elite RowerLuky PratamaBelum ada peringkat
- Reversible Plate Compactor CatalougeDokumen4 halamanReversible Plate Compactor CatalougeDeep ZaveriBelum ada peringkat
- TvlistDokumen3 halamanTvlistSuryadi StanleyBelum ada peringkat
- Free Daily Planner MondayDokumen9 halamanFree Daily Planner MondayEdgarBelum ada peringkat
- Technical Service Information 12-07Dokumen4 halamanTechnical Service Information 12-07Planta Damiana2Belum ada peringkat
- Official F1 Esports Series: Online Rulebook V1.1Dokumen20 halamanOfficial F1 Esports Series: Online Rulebook V1.1Maury Vásquez JrBelum ada peringkat
- Código Descrição Preço Ash / LuporiniDokumen5 halamanCódigo Descrição Preço Ash / LuporiniHomero TeixeiraBelum ada peringkat
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Hyatt HotelsDokumen15 halamanHyatt Hotelshttp://www.infoseeds.co.inBelum ada peringkat
- Luciano PavarottiDokumen12 halamanLuciano PavarottiStefan AdrianBelum ada peringkat
- September 2015: Braham Moose Lodge #1544 Loyal Order of MooseDokumen2 halamanSeptember 2015: Braham Moose Lodge #1544 Loyal Order of MooseDoug GronertBelum ada peringkat
- Indices Laws RevisionDokumen5 halamanIndices Laws RevisionMarisa VetterBelum ada peringkat
- Overlord 2 - Official Game Guide - ExcerptDokumen11 halamanOverlord 2 - Official Game Guide - ExcerptPrima Games100% (1)
- PAS Semester Gasal-XIIDokumen5 halamanPAS Semester Gasal-XIIYuli PratiwiBelum ada peringkat
- BKC Poll KolaDokumen1 halamanBKC Poll KolaCourier JournalBelum ada peringkat
- WtA Ananasi SheetDokumen4 halamanWtA Ananasi SheetSetho shiniBelum ada peringkat
- Fiat Tractors 411r Service ManualDokumen9 halamanFiat Tractors 411r Service Manualteri100% (25)
- High-Torque, All-Hydraulic Auger DrillDokumen2 halamanHigh-Torque, All-Hydraulic Auger DrillAsif KhanzadaBelum ada peringkat
- Passive VoiceDokumen7 halamanPassive Voiceecha_16100% (2)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Chrysler Scan Tool Flash AvailabilityDokumen733 halamanChrysler Scan Tool Flash AvailabilityAlbert0% (1)
- Sato ManualDokumen1 halamanSato ManualJonBelum ada peringkat
- ObrasDokumen34 halamanObrasandy hernandez0% (1)
- Grand Theft Auto IV CheatsDokumen1 halamanGrand Theft Auto IV CheatssyonturiqeruBelum ada peringkat
- FT - Exámenes de Septiembre 2021 - Web 2Dokumen24 halamanFT - Exámenes de Septiembre 2021 - Web 2MATIAS QUINTANABelum ada peringkat
- IKC 4 Rule BookDokumen24 halamanIKC 4 Rule BookJee RyBelum ada peringkat
- MC500EDokumen23 halamanMC500EvicnitBelum ada peringkat
- Broken Sonnet by HaleDokumen2 halamanBroken Sonnet by Halewiggly18Belum ada peringkat
- Teaching English Through SongsDokumen5 halamanTeaching English Through SongsPatricia Pérez BerradeBelum ada peringkat
- BearingsDokumen20 halamanBearingsMuhammad AsadBelum ada peringkat