MENOpausia IMAGENES (2) y Prevalencia y Fisoología de La Misma Monteleone2018
Diunggah oleh
Felipe Torreblanca CoronaHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
MENOpausia IMAGENES (2) y Prevalencia y Fisoología de La Misma Monteleone2018
Diunggah oleh
Felipe Torreblanca CoronaHak Cipta:
Format Tersedia
REVIEWS
Symptoms of menopause —
global prevalence, physiology
and implications
Patrizia Monteleone, Giulia Mascagni, Andrea Giannini, Andrea R. Genazzani
and Tommaso Simoncini
Abstract | The symptoms of menopause can be distressing, particularly as they occur at a time
when women have important roles in society, within the family and at the workplace. Hormonal
changes that begin during the menopausal transition affect many biological systems.
Accordingly, the signs and symptoms of menopause include central nervous system-related
disorders; metabolic, weight, cardiovascular and musculoskeletal changes; urogenital and skin
atrophy; and sexual dysfunction. The physiological basis of these manifestations is emerging as
complex and related, but not limited to, oestrogen deprivation. Findings generated mainly
from longitudinal population studies have shown that ethnic, geographical and individual
factors affect symptom prevalence and severity. Moreover, and of great importance to clinical
practice, the latest research has highlighted how certain menopausal symptoms can be
associated with the onset of other disorders and might therefore serve as predictors of future
health risks in postmenopausal women. The goal of this Review is to describe in a timely
manner new research findings on the global prevalence and physiology of menopausal
symptoms and their impact on future health.
Hot flashes
In common belief, the symptoms of menopause arise neurochemical changes within the central nervous sys-
A sudden wave of body heat from the permanent cessation of menstrual periods, tem (CNS)2. In postmenopause, long-term manifesta-
accompanied by reddening of which defines this condition1. However, hot flashes and tions of definite oestrogen deprivation ensue, such as
the face and neck and profuse night sweats, insomnia and mood instability might urogenital atrophy and ageing of the skin, and osteopo-
sweating, sometimes
actually begin before the cessation of menses and are rosis might develop during this time. In addition, a shift
followed by a feeling of cold
and shivering.
the manifestation of incipient ovarian failure1. The tran- towards central body fat distribution and the consequent
sition from the reproductive period to the first year metabolic alterations might occur as a result of increases
Ovarian failure of postmenopause, termed perimenopause, occurs over in the androgen:oestrogen ratio3, which is also driven by
The definite loss of function of several years and is characterized by substantial bio- increased insulin resistance4.
the ovaries.
logical change. According to the widely accepted Stages The symptoms of menopause can be very distress-
of Reproductive Ageing Workshop (STRAW) staging ing and can considerably affect the personal, social
system, perimenopause encompasses three stages: early and work lives of women. Owing to the heterogeneous
menopausal transition (also known as early perimen- nature of menopausal symptoms, a firm understanding
opause), characterized by persistent irregularity of the of their physiological basis has been established only
Division of Obstetrics and menstrual cycle; late menopausal transition (also known following many years of investigation. The development
Gynecology, Department of as late perimenopause), characterized by an interval of of the STRAW staging system1 (TABLE 1), which is based
Clinical and Experimental amenorrhoea of ≥60 days in the prior 12 months; and on the menstrual patterns of women, has allowed inves-
Medicine, University of Pisa,
early postmenopause, which is the first year following tigators to generate more uniform scientific data regard-
Via Savi 10, Pisa 56126,
Italy. the final menstrual period (FMP)1. Perimenopause is ing events correlated with menopause and has prompted
Correspondence to A.R.G.
characterized by marked fluctuations in levels of sex research on the assessment of trajectories of hormonal
andrea.genazzani@med. hormones, which are greater than those that occur changes and their clinical correlates1. Moreover, over
unipi.it during the follicular and luteal phases of the menstrual the past decade, data from epidemiological studies
doi:10.1038/nrendo.2017.180 cycle during premenopause, and is associated with involving many women have been made available to
Published online 2 Feb 2018 the worst menopausal symptom burden, arising from investigators in the field of menopause. These large
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 1
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Key points Central nervous system-related symptoms
CNS-related symptoms are those arising as a conse-
• Menopausal symptoms have a substantial effect on the quality of life of women and quence of the neurobiochemical changes that occur after
on performance at the workplace; increased awareness of symptoms and acquisition ovarian failure, such as vasomotor symptoms, sleep dis-
of coping strategies might help turbances, anxiety and depression, migraine and changes
• Certain menopausal symptoms might serve as markers for future health; severe in cognitive performance.
vasomotor symptoms and sleep disorders might increase cardiovascular risk,
whereas severe vasomotor symptoms and depression might affect cognitive Vasomotor symptoms. Approximately 75% of women
function
experience vasomotor symptoms during menopause2.
• The nature of menopausal symptoms is common to all women; however, geographical Vasomotor symptoms are the hallmark of menopause
location and ethnicity influence the prevalence of certain symptoms
and are defined as hot flashes and sweating, sometimes
• Individual factors such as personal history, current health status (particularly followed by trembling and a feeling of coldness (FIG. 1).
obesity) and socioeconomic status considerably worsen a woman’s experience
These are typically the most frequent and bothersome
of menopause
symptoms associated with menopause due to their sud-
• Health-care providers should offer education to women on improving modifiable den and seemingly random onset during the day and
lifestyle factors to reduce the risk of future illness
even at night. Vasomotor symptoms can begin as early
• Menopause seems to accelerate the ageing process; therefore, the manifestation of as 2 years before the FMP, peak 1 year after the FMP and
menopausal symptoms might be in part due to ageing
continue for 4 years after the FMP in approximately half
of women6. Approximately 12% of women will continue
reporting symptoms as far as 11–12 years after the FMP6,7.
population studies have not only increased the robust- In fact, one study reported that approximately one-third
ness of research conclusions but have also incorporated of women aged 65–79 years still report vasomotor symp-
different ethnicities, allowing between-group obser- toms8. It seems that women who begin to experience
vations. Importantly, in contrast to the cross-sectional vasomotor symptoms earlier with respect to the FMP
studies that were performed in the past, new data have will experience these symptoms for longer periods in
been generated from longitudinal studies and therefore postmenopause, with a median time of 7.4 years9.
provide important insight into the temporal pattern Although vasomotor symptoms influence the quality
of the development of menopausal symptoms and the of life of women during daytime, they also greatly alter
associated hormonal changes. the quality of sleep. Indeed, women with nocturnal vaso-
The scope of this Review is to describe symptoms of motor symptoms have greater motor restlessness in bed,
menopause in light of new findings generated from the less efficient sleep and a reduced feeling of restedness in
study of ethnicity and geographical location, personal the morning compared to women without night-time
history and individual characteristics as factors influ- symptoms10. Nocturnal hot flashes are more common
encing a woman’s experience of menopause and the during the first 4 hours of sleep and are associated with
impact of these symptoms on her social and personal a greater number of episodes of waking after the onset
life. Up‑to‑date evidence on the complex physiology of sleep, whereas later rapid-eye-movement (REM)
of menopausal symptoms is provided. Moreover, as an sleep suppresses hot flashes, arousals and awakenings11.
important contribution to modern clinical practice, this Furthermore, following pharmacological induction of
Review offers insight into the associations between cer- temporary menopause using gonadotropin-releasing
tain menopausal symptoms and other disorders and the hormone (GnRH)-analogue administration in pre-
implications of these associations for future health in menopausal volunteers, vasomotor symptoms arise
postmenopausal women5. most commonly during the first stage of sleep and wake,
typically preceding or occurring simultaneously with
Menopause and its symptoms wake episodes12.
Menopause, with its signs and symptoms, occurs at a
time in a woman’s life when she is often actively engaged Sleep disruption. Sleep difficulties, particularly nocturnal
in family upbringing and/or handling a full-time job, awakenings, are major complaints and are reported by
Postmenopause during which time she might also have the responsibil- 40–60% of menopausal women13,14 (FIG. 1). The increased
The period of a woman’s life ity of caring for ageing parents. Women are often puz- occurrence of sleep disruptions has been clearly demon-
that follows the final menstrual
period.
zled by the remarkable changes in mood, sleep patterns, strated among perimenopausal and postmenopau-
memory and body shape that occur, as well as the onset sal women compared with premenopausal women in
Perimenopause of vasomotor and urogenital symptoms. As menopau- the multiethnic, community-based Study of Women’s
The period of a woman’s life sal symptoms can be very distressing and considerably Health Across the Nation (SWAN)15,16. Data from the
that encompasses the
affect a woman’s personal and social life, health-care Penn Ovarian Ageing Study collected over an 8‑year
menopausal transition and the
first year following the final providers caring for women at all levels of the health- period have suggested that the decline of sleep quality in
menstrual period. care system must be well prepared to guide patients menopausal women might be due to menopause-related
through this transition and provide advice to improve symptoms, namely, hot flashes and depressive symp-
Amenorrhoea quality of life. In this section, a detailed description of toms17. Moreover, a recent polysomnography study found
The absence of menstrual
periods for 3 or more
the wide range of symptoms experienced by women at that self-reported and physiological hot flashes are more
consecutive months in a menopause, in relation to the affected biological system, common in menopausal women with insomnia than in
woman of reproductive age. is provided (FIG. 1). women who do not develop clinical insomnia and that
2 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 1 | The Stages of Reproductive Ageing Workshop staging system
Stage Duration Terminology Menstrual cycle characteristics
Menarche
−5 Variable Reproductive: early Variable to regular
−4 Variable Reproductive: peak Regular
−3b Variable Reproductive: late Regular
−3a Variable Reproductive: late Subtle changes in flow length
−2 Variable Menopausal transition: early Variable length: persistent ≥7 day difference
in length of consecutive cycles
−1 1–3 years Menopausal transition: late Interval of amenorrhea of ≥60 days
Final menstrual period
+1a 2 years Postmenopause: early –
+1b 3–6 years Postmenopause: early –
+1c 3–6 years Postmenopause: early –
+2 Remaining Postmenopause: late –
lifespan
Adapted with permission from REF. 208, Elsevier.
the presence of objective hot flashes predicts the num- and twice that in men28. Women with a personal history
ber of awakenings, indicating a clear contribution for of major depression are at risk of relapse during peri-
hot flashes in sleep disturbance18. Sleep electroenceph- menopause23,25,29 and in the first 2 years of postmeno-
alography has demonstrated that the underlying cause pause but not beyond30. However, it is unclear whether
of impaired sleep quality in late perimenopausal and women who have never experienced major depression in
postmenopausal women might be related to a change in their premenopausal years are at increased risk during or
arousal levels during both REM and non-REM sleep19. after menopausal transition31,32. Regarding anxiety, data
Sleep disruption in menopause might be exacerbated from the SWAN cohort have indicated that women with
by disordered breathing due to obstructive sleep apnoea, high levels of anxiety premenopausally continue to expe-
independent of body weight and age 20. Moreover, rience such anxiety through the menopausal transition,
obstructive sleep apnoea affects more women in post- whereas women with low anxiety premenopausally are at
menopause than in premenopause20. Data have emerged increased risk of developing high levels of anxiety during
in the literature linking sleep disorders with an increased and after the menopausal transition32. Thus, the meno-
risk of cognitive decline in menopausal women, particu- pausal transition might be a critical time for women who
larly with respect to attention, episodic memory and are susceptible to anxiety disorders32.
executive function21. Furthermore, cognitive function
was found to be worse in early postmenopausal women Cognitive changes. Perimenopausal women often report
at high risk of obstructive sleep apnoea compared to a decline in memory and concentration (FIG. 1), which
those at low risk of sleep apnoea22. might be distressing and is clinically relevant 33. Data
from the SWAN cohort analysing cognitive function
Depression and anxiety. The menopausal transition is longitudinally over a 4‑year period have demonstrated
a vulnerable period for the onset of depressive symp- that there is a reduction in cognitive performance, spe-
toms (FIG. 1). Longitudinal studies and meta-analyses cifically a lack of learning, but that it is isolated to the
have shown that women in the menopausal transition perimenopausal stage of the transition34. More specif-
and early postmenopausal years are more likely to report ically, a lack of improvement in verbal memory was
a depressed mood than premenopausal women23–26. In reported in the early and late perimenopausal stages, and
the SWAN cohort, data collected from the Center for deficits in processing speed with repeated testing were
Epidemiological Studies Depression Scale (CES‑D) ques- seen in the late perimenopausal stage compared with
tionnaire — which evaluated sadness, loss of interest, the premenopausal and postmenopausal stages34. These
appetite, sleep, concentration, feelings of guilt, tiredness, data suggest that the detrimental effect of menopause
agitation and suicidal ideation24 — showed that across on cognitive performance is transient and limited to the
5 years, women were substantially more likely to report perimenopausal stage. In addition, other longitudinal
Obstructive sleep apnoea
A sleeping disorder caused by a high symptom score during early perimenopause, late studies examining women in the menopausal transi-
repetitive upper airway perimenopause and postmenopause compared with tion have indicated modest declines in processing speed
collapse during sleep, leading premenopause, and also during late perimenopause and verbal episodic memory (delayed recall)24,35,36. In a
to intermittent hypoxia and compared with early perimenopause25. Extended lon- study published in 2017, the estimated rates of cognitive
characterized by loud snoring,
apnoea during sleep, insomnia,
gitudinal data from this same cohort confirmed these decline over a 10 year period were reported as 4.9% of
excessive daytime sleepiness, observations27. With respect to major depression, the the mean baseline score for processing speed and 2%
morning headache and fatigue. lifetime prevalence of this disorder is >20% in women of the mean baseline score for delayed recall37.
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 3
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
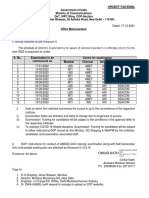
Central nervous system Skin, mucosal and hair changes Moreover, the presence of moderate to severe vasomotor
• Vasomotor symptoms • Reduced skin thickness symptoms has been associated with a greater number of
• Sleep disruption • Reduced elasticity complaints of poor memory function41. Finally, as sleep
• Depression and anxiety • Reduced hydration
• Cognitive changes • Increased wrinkling is important for learning and memory consolidation42,
• Migraine • Hair loss it is very plausible that disordered sleeping, particularly
sleep apnoea22, contributes substantially to the memory
lapses reported by many perimenopausal women.
Migraine. The prevalence of migraine during meno-
pause ranges from 10% to 29%43 (FIG. 1). It seems that
women who are susceptible, particularly those with
Weight and metabolic changes
premenstrual migraine during fertile years, have more
• Weight gain migraine headaches as they transition through meno-
• Increased visceral adiposity pause44. In community-based studies, the prevalence
• Increased waist circumference
Sexual function of migraine headache in women migraineurs has been
• Decreased sexual desire reported to increase in perimenopause and decrease in
• Dyspareunia
postmenopause44. Importantly, a study that enrolled a
large number of women reported that the risk of high fre-
quency headache was markedly increased in women dur-
Urogenital system ing perimenopause compared with premenopause34,45;
• Vaginal dryness high frequency headaches affected 8% of premenopau-
• Vulvar itching and burning
• Dysuria sal women, compared with 12.2% of perimenopausal
• Urinary frequency women and 12% of postmenopausal women.
• Urgency
• Recurrent lower urinary Musculoskeletal system
tract infections • Joint pain Weight and metabolic changes
• Sarcopenia
One of the main complaints from women at midlife
is increased weight 46 (FIG. 1). Indeed, the prevalence of
obesity is higher in postmenopausal women than in pre-
menopausal women46. Absolute weight gain in women
at midlife seems to be fundamentally related to age-
ing rather than to menopause itself 46. In women aged
40–55 years, the average weight gain was reported by
one study to be 2.1 kilograms over 3 years47. What seems
to be menopause-dependent is a redistribution of body
Nature Reviews | Endocrinology fat 47,48 characterized by accumulation of mostly visceral
Figure 1 | Overview of menopausal symptoms. Symptoms of menopause include
central nervous system (CNS)-related disorders, bodily alterations related to adiposity at the trunk, leading to an increase in waist cir-
cardio-metabolic changes, musculoskeletal alterations, urogenital and skin atrophy and cumference and an obvious change in body shape47. In
sexual dysfunction. Perimenopause is associated with the worst menopausal symptom addition, studies using techniques such as dual-energy
burden, arising from neurochemical changes within the CNS leading to severe X‑ray absorptiometry (DXA), CT and MRI have docu-
vasomotor symptoms, sleep disorders and depression, which might affect cognitive mented the increase in visceral abdominal fat deposi-
function. Long-term manifestations of definite oestrogen decline result in urogenital tion in postmenopause compared with premenopause48.
atrophy and ageing of the skin, whereas osteoporosis and sarcopenia might develop
Visceral adipose tissue poses a greater health risk than
during the postmenopausal period.
subcutaneous fat and, in general, is an independent
cause of cardiovascular disease (CVD), primarily due to
Surgical menopause has more severe consequences the increase in insulin resistance and the consequent risk
on cognitive functions than natural menopause and is of developing diabetes mellitus and the metabolic syn-
associated with an increased risk of cognitive impair- drome36. Furthermore, evidence that ovarian failure is
ment or dementia in later life38. One study reported that causative of visceral fat accumulation during menopause
surgical menopause after 45 years of age was associated has come from cross-sectional49,50 and longitudinal stud-
with lower performance in verbal learning and a decline ies51,52. In support of this hypothesis, surgically induced
in visual memory compared with natural menopause, menopause seems to accelerate weight gain in the years
whereas a decrease in semantic memory was observed in following surgery compared with ovarian-sparing
women who underwent oophorectomy before 45 years hysterectomy or natural menopause53.
of age39. Interestingly, oophorectomy after natural meno
Surgical menopause pause is not associated with alterations in cognitive Cardiovascular changes
Menopause induced by the performance39. Atherosclerosis and the risk of cardiovascular adverse
surgical removal of the ovaries. In the SWAN cohort, although the cognitive deficits events increase in women after menopause, which might
observed during perimenopause are independent of be due in part to the production of pro-inflammatory
Visceral adiposity
Accumulation of adipose tissue
mood symptoms, women with more depressive symp- cytokines and adipokines in visceral adipose tissue54,55.
in the abdomen and around toms displayed a worse processing speed, and those with Increased deposition of visceral fat in postmenopau-
internal organs. higher degrees of anxiety had a poorer verbal memory 40. sal women might be associated with fat accumulation
4 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
in other visceral tissues such as the heart 56. Indeed, it Urogenital symptoms
has been reported that late perimenopausal and post Although they are not frequently reported, urogenital
menopausal women have markedly greater volumes symptoms are often present after menopause63 (FIG. 1)
of heart fat than premenopausal women independ- and include vaginal dryness, dyspareunia, vulvar
ent of age, race, obesity or other covariates57. Notably, itching and burning, dysuria, urinary frequency and
blood lipid profiles tend to become atherogenic in urgency and recurrent lower urinary tract infections64.
women within the year following the FMP, with major The US Real Women’s Views of Treatment Options for
increases in total cholesterol, LDL cholesterol and apo- Menopausal Vaginal Changes (REVIVE) survey high-
lipoprotein B (APOB), independent of ethnicity, age or lighted a reluctance among postmenopausal women to
weight 58. Moreover, the anti-atherogenic effect of HDL address these symptoms with their health-care provid-
cholesterol seems to be abolished as women transition ers, causing a delay in their management 65. The inter-
through menopause; increases in HDL cholesterol levels national Vaginal Health: Insights, Views and Attitudes
are, at this stage, independently associated with greater (VIVA) study reported the prevalence of individual
progression of carotid intima–media thickness59. The urogenital symptoms in a large cohort of women with
markedly reduced exposure to oestrogen during meno vaginal discomfort as 83% for vaginal dryness, 42% for
pause might have a negative effect on endothelial cell pain during intercourse, 30% for involuntary urination,
growth and reduce the inhibitory effect of female sex 27% for soreness, 26% for itching, 14% for burning and
hormones on the growth and proliferation of vascular 11% for pain when touching the vagina66. In the same
smooth muscle cells60. Moreover, although blood pres- study, 62% of women with vaginal discomfort reported
sure levels seem to be lower on average in premeno- the severity of these symptoms as moderate or severe66.
pausal women than in their male counterparts, this The recent European REVIVE survey — which included
advantage is lost around the time of menopause, and the largest cohort of postmenopausal women studied
blood pressure levels start to rise in women, reaching to date — confirmed that vulvovaginal atrophy is still
levels similar to those of men of the same age group61. underdiagnosed and undertreated67. It is widely accepted
The prevalence of salt sensitivity also increases in post- that this group of symptoms — now termed genitouri-
menopausal women and doubles as early as 4 months nary syndrome68 (BOX 1) — typically manifests 4–5 years
after surgical menopause, therefore contributing to after menopause in the presence of stably low levels of
their increased risk of developing hypertension 61. oestrogen. Longitudinal studies have also reported an
Taken together, these negative changes in cardiovascu- increase in urinary incontinence symptoms with meno
lar features increase the risk of adverse cardiovascular pause69,70; however, it is unclear whether this change
events, a risk that is even greater in women younger is attributable to the menopausal transition itself or to
than 45 years who experience premature or early-onset the concomitant weight gain that typically occurs dur-
menopause62 (FIG. 1). ing this time69. Indeed, it has been demonstrated that
an increase in body weight of 1 kg is associated with a
higher incidence of urinary incontinence in women at
Box 1 | Origin and clinical characteristics of genitourinary syndrome
midlife70. Furthermore, cross-sectional studies have also
affirmed that menopausal status per se is not a determi-
Oestrogen receptors (ERα, ERβ) are present in the vagina, vestibule of the vulva, nant of urinary incontinence71; the risk of developing
urethra and trigone of the bladder; in different myofascial structures and ligaments stress incontinence increases with obesity and parity,
such as utero-sacral ligaments, levator ani muscles and pubo-cervical fascia; and also whereas the risk of urge urinary incontinence increases
on autonomic and sensory neurons in the vagina and vulva68,162. The highest
with age. Moreover, mixed incontinence is positively
concentration of ERs is in the vagina, with ERα being the only active form
after menopause.
correlated with higher BMI and hysterectomy 71.
Genitourinary syndrome symptoms are manifestations of the changes that occur at
menopause due to oestrogen withdrawal. Loss of lubrication, burning, dryness, Sexual dysfunction
itching and entry dyspareunia with fissuring are some of the vulvovaginal Longitudinal and cross-sectional studies have reported
symptoms64,68. Urinary symptoms include recurrent urinary tract infections, urgency that the menopausal transition is associated with a
and urge incontinence, stress incontinence, dysuria and voiding issues67,68. These decrease in sexual desire, independent of ageing 72 (FIG. 1).
might enhance loss of libido and sexual dysfunction in terms of arousal and orgasm. Specifically, the menopausal transition is characterized
Signs of genitourinary syndrome are numerous and heterogeneous and consist of by a change in hormone-driven sexual desire73. The
decreased elasticity and moisture, labia minora resorption, pallor, erythema, decline in sexual function in perimenopausal women is
loss of vaginal rugae, tissue fragility, loss of hymenal remnants, introital retraction,
greatest between 20 months before the FMP and 1 year
urethral eversion or prolapse, prominence of urethral meatus and recurrent urinary
tract infections64,68,160.
after the FMP74, and women seem to exhibit a decrease
The aim of management and treatment of genitourinary syndrome is to provide in sexual desire and an increase in painful intercourse
symptom relief. However, counselling for genitourinary syndrome symptoms is also beginning in late perimenopause72. Curiously, masturba-
an appropriate time to discuss lifestyle, diet and exercise, smoking cessation and tion — a behaviour that is not dependent on partner sta-
appropriate alcohol consumption. Treatment will depend on the signs and symptoms tus — increases temporarily in early perimenopause and
and degree of severity. Nonhormonal therapies include personal lubricants, vaginal declines thereafter in postmenopause72. Sexual activity
moisturizers and vaginal laser treatment (of which the long-term safety and continues to decrease, but at a slower rate, throughout
effectiveness have not been established). Hormonal therapies include vaginal oestriol the 5 years following the FMP, independently of vaginal
cream or pessaries, vaginal oestradiol tablets or systemic hormone therapy dryness, lubricant use or mood disorders74. Further on,
(menopause hormone therapy).
vulvovaginal symptoms can add to sexual dysfunction
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 5
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
and interfere with social, interpersonal and psycho there is a loss of collagen-producing dermal fibroblasts
logical well-being as the consequent dyspareunia can and reduced elastin proteoglycan content and water
lead to avoidance of sexual intimacy with a partner 73. retention87. Moreover, similar changes occur in the
Indeed, the European REVIVE study reported that pain mucosa of the orogastrointestinal and urinary tracts,
during intercourse has a substantially negative influence which also become more fragile. Moreover, menopause
on sexual satisfaction67. In addition, a decline in general seems to increase susceptibility to mucosal injury and
self-esteem and well-being after menopause might also delay mucosal healing owing to a less robust humoral
contribute to the loss in sexual intimacy with a partner 75. and cellular immune response and to increased per-
Nonetheless, being in a long-lasting relationship seems meability of the mucosa to pathogens in the presence
to preserve a satisfying sexual life, even in older late of oestrogen deficiency 88. Changes in hair distribution
menopausal women73. might also occur at menopause with the appearance of
facial terminal hairs and a decrease in body and scalp
Musculoskeletal symptoms hair 89 (FIG. 1). Hair loss in perimenopausal women usu-
A major concern in menopausal women is a decline in ally appears as a dispersed thinning of hair, primarily in
bone health. Postmenopausal osteoporosis is a degen- the central and forehead region, and can also occur
erative bone disorder characterized by reduced BMD in parietal and occipital regions89.
(FIG. 1) and altered bone structure, such as thinning and
increased porosity of the cortex and decreased connec- Personal and social impact
tivity of trabeculae76. Osteoporosis increases the risk Midlife is a time of profound personal and social change
of fractures76 — which occur most frequently in the for women. The perception and interpretation of meno-
spine, hip and wrist in postmenopausal women with pausal symptoms, and therefore their interference with
osteoporosis77 — and might lead to long-term disability. day‑to‑day life, are influenced by social and cultural
Although there are minimal changes in BMD during beliefs90. On an international level, ~20% of women
premenopause or early perimenopause, BMD sharply perceive menopause as a disease, even if they are not
declines during late perimenopause78. The annual rates necessarily fully aware of its symptoms and health
of bone loss after the FMP are estimated to be 1.8–2.3% implications90,91. Depending on personal and working
in the spine and 1.0–1.4% in the hip78. Epidemiological characteristics, even mild menopausal symptoms can be
studies have shown that the incidence of wrist and spine distressing for some women, and most women with per-
fractures in postmenopausal women rises before hip frac- vasive menopausal symptoms will experience profound
tures77; this observation seems to be related to the rapid trouble in coping with daily life.
bone loss that occurs in the first 3–5 years after meno The personal experience of menopausal symptoms,
pause, which primarily affects trabecular bone tissue, particularly bodily changes that occur related to ageing
whereas that which occurs in the following 10–20 years and the awareness of the loss of fertility, can alter self-
involves both trabecular and cortical bone76. image. Life events might produce a change of role and/or
Changes in body composition that occur in women identity around the time of the menopausal transition.
at midlife also affect lean muscle mass (FIG. 1), which, The empty nest syndrome, retirement from work, hav-
as opposed to fat mass, seems to decrease79. Although ing frail or ill parents and the loss of a parent or partner
sarcopenia cannot be currently attributed to meno- are all conditions that frequently occur at midlife. These
pause, this degenerative process is more evident in age- new conditions imply a depletion of personal and social
ing women than ageing men and seems to occur more networks, a repositioning towards a less prestigious sta-
rapidly after menopause80,81. Resistance exercise82 and tus, an increase in caregiving activities, with an overall
adequate dietary protein intake70 are important lifestyle decline in quality of life91. Thus, midlife and the meno-
factors that help to maintain lean muscle mass and pausal transition are often perceived as a time of crisis
consequently preserve mobility and postural stability, by women, and the presence of distressing menopausal
reducing the risk of falls and bone fractures. symptoms adds to the perception of deteriorating mental
In addition, the prevalence of osteoarthritis increases and physical well-being with indirect consequences on
greatly after the FMP83, and pain specifically affecting health92. Nonetheless, many women perceive menopause
the distal interphalangeal joints of the fingers and as a natural phase of life without negative implications93.
base of the thumb due to osteoarthritis of the hand is The reasons for this interpersonal variability in the per-
a commonly reported symptom in the perimenopau- ception of menopause might be attributable to the rela-
sal period73. Although osteoarthritis of the hand dur- tive intensity of symptoms but might also depend on how
ing perimenopause usually subsides within 2–3 years, women interpret and manage these symtoms94 according
it is predictive of successive joint disease in the knee to their social position and cultural inclination95,96.
and spine84. With respect to knee osteoarthritis, most Approximately 30–40% of women report that men-
affected women report the onset of symptoms during opausal symptoms reduce performance in the work-
perimenopause or within 5 years of the FMP85. place94, and the most disruptive symptoms are hot
flashes, insomnia, a feeling of tiredness and poor concen-
Skin, mucosal and hair changes tration96. Even in women who are not heavily burdened
Menopause reduces skin thickness, elasticity and by menopausal symptoms, the cost is often paid in terms
hydration and leads to an increase in wrinkling 86 (FIG. 1). of perception of worsened social desirability and feel-
Structural changes occur mainly in the dermis where ings of shame or embarrassment, which are sometimes
6 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
due to unwelcome comments from colleagues94,97–99. was associated with higher climate temperatures, and
Targeted strategies to make the menopausal transition these symptoms were more frequent and problematic
and its symptoms recognized socially and accepted for women living in higher temperature and lower alti-
in the workplace94,95,100 — such as promoting self-help tudes112. However, the frequency and severity of these
readings, specific training, flexible working hours or symptoms were not influenced by seasonal variation in
shift changes and reviews of workplace ventilation and temperature112, an observation that was confirmed
temperature — have proved valuable in helping women in studies involving women from other continents109,110.
to share their experiences with peers and together seek As previously stated, menopausal women have an
solutions and develop coping strategies. increased risk of cardiovascular events65,66; however, this
elevated risk seems to be higher in black postmenopau-
Incidence and prevalence of symptoms sal women with obesity than in white postmenopausal
International and interethnic epidemiological studies women with obesity, even in the absence of the metabolic
have shown that the incidence and prevalence of men- syndrome113.
opausal symptoms might vary according to the study Skin ageing at menopause also varies according to
population. Individual characteristics and comorbidi- skin colour. In a study that enrolled menopausal women
ties also have a role in the manifestation of menopausal within 36 months of the FMP, black women were shown
symptoms. to have lower skin wrinkling scores over a period of
4 years than white women, possibly due to the lower sus-
Ethnic differences ceptibility of black women to photoageing 114. Skin rigid-
Differences in the age of natural menopause have been ity, a measure of collagen and water content in skin that
reported on a global level. Indeed, a recent meta-analysis changes rapidly in response to oestrogen deprivation, was
of 36 international studies evaluating age at natural also positively correlated with the time since menopause,
menopause reported an overall mean of 48.78 years, with but only in the white subpopulation of the study 114.
a range of 46 to 52 years101. The age at menopause was Regarding sexual functioning, African-American
reported to be generally lower in women from African, women transitioning through menopause report a
Latin American, Asian and Middle Eastern countries higher frequency of sexual intercourse than other ethnic
and was the highest in Europe and Australia, followed groups83. Moreover, North American women of Chinese
by the USA101. and Japanese descent have been reported to be less sex-
Disparities in reported symptoms of menopause ually active and attribute less importance to this aspect
have been described among women of different eth- than Western women83. However, data from the pan-
nicities and/or geographical regions. Although the Asian REVIVE survey have revealed that genitourinary
nature of menopausal symptoms is common to women syndrome is underdiagnosed and undertreated in Asian
of all geographical regions and ethnicities, the preva- women and that, when present, vaginal dryness and
lence of certain symptoms varies considerably. Women irritation have the greatest negative influence on sexual
of European and Latin American ethnicity predom- enjoyment and intimacy in this demographic115.
inantly have CNS-related symptoms, including hot The prevalence of osteoporotic fracture in postmeno
flashes, sleeplessness, mood changes, irritability and pausal women, mostly involving the hip, varies consid-
reduced sex drive102–104. In North America, where the erably across the world, with the highest prevalence in
population is multiethnic and comprises women of Scandinavia and lowest prevalence in Africa116. Within
African-American, Asian and Hispanic descent as well the European continent, the highest rates of osteoporotic
as white women, the SWAN study reported that vaso- fracture are recorded in northern countries compared
motor symptoms were more prevalent among African- with the more southern Mediterranean countries,
American and Hispanic women and less prevalent presumably owing to differences in sun exposure and
among Japanese-American and Chinese-American therefore endogenous production of vitamin D, which
women than among white women105. However, emerg- is essential for calcium absorption and bone mineral-
ing analyses of studies performed in Thailand, China ization117. Interestingly, the rate of hip fractures has
and Singapore report that the prevalence of hot flashes increased threefold in China over the past 25 years,
and/or night sweats in Asian women is similar to those which might be attributable to westernization and a shift
of Western countries106,107. The prevalence of vasomotor towards a more sedentary lifestyle118.
symptoms was also reported to be lower in India and
in Middle Eastern countries, such as the United Arab Individual differences
Emirates and Saudi Arabia, with respect to Western A woman’s experience of menopause is extremely per-
countries108–110. African-American women tend to have sonal, and therefore the incidence and prevalence of
vasomotor symptoms that are particularly persistent symptoms, particularly CNS-related symptoms, are
compared with the average 7.4 years20, with a median influenced by personal characteristics, personal history
total duration of 10.1 years20; however, this might be and environmental factors.
due to the higher rate of obesity in African-American
women than in other ethnicities in North America111. Personal history. A strong predictive association has
In addition, a multicentre study involving Spain and been described between somatic anxiety and the risk
Spanish-speaking Latin American countries revealed of menopausal hot flashes119. Anxiety, perceived stress
that the prevalence of hot flashes and night sweats and depressive symptoms also seem to lead to persistent
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 7
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
vasomotor symptoms20. Interestingly, one study120 reported household incomes and social support, poor educa-
that women who have experienced one or more form of tion, fair or poor general health and a history of surgical
abuse over the previous year, mostly verbal and/or emo- menopause and stressful life events132.
tional abuse, have higher scores for menopausal symp-
toms such as sleep disturbances, decline in cognitive Physiology of menopausal symptoms
function, bowel and bladder dysfunction, lower sexual Menopausal symptoms arise from the failure of ovar-
activity and decline in general health but not for hot ian function owing to the depletion of ovarian folli-
flashes and night sweats. In addition, women who have cles5 (FIG. 2). This process involves a series of hormonal
experienced moderate to severe premenstrual syndrome alterations over a period of years, a period known as
have an increased risk of developing depression, poor menopausal transition, beginning with the decline in
quality of sleep, feeling less attractive and, in particu- levels of inhibin B, resulting in a decline in their nega-
lar, memory and concentration problems after meno- tive feedback action on the follicle-stimulating hormone
pause121. Conversely, a history of hypertensive diseases (FSH) release from the pituitary 1,5. Increases in FSH
during pregnancy seems to predispose women to more levels of follow, promoting erratic increases in oestra-
severe and persistent hot flashes and night sweats122. diol secretion. This has been demonstrated in a study
of women classified according to the STRAW staging
Obesity. Excess adiposity is a major factor that influ- system as mid-reproductive age, late-reproductive age,
ences a woman’s quality of life during the menopausal early menopausal transition and late menopausal tran-
transition. Obesity is associated with a longer meno- sition133; in 37% of the ovulatory cycles during men-
pausal transition duration49 and a higher prevalence of strual transition, a second rise and fall in oestradiol
vasomotor symptoms123. In fact, gains in body fat over levels was observed during the mid-luteal and late-
time are predictive of risk and frequency of vasomo- luteal phase, resembling that of the follicular phase but
tor symptoms124. Moreover, concurrent BMI and waist superimposed on the luteal phase, as well as decreases
circumference measurements are positively related to in progesterone secretion. This luteal out‑of‑phase
incident vasomotor symptoms in early menopause125; increase in oestradiol levels seemed to be triggered by a
on the basis of these data, the SWAN investigators have long-term elevation of FSH levels in the follicular phase
suggested that maintaining a healthy weight during early and lower inhibin B levels early in the cycles. Moreover,
menopause might help prevent vasomotor symptoms. the unopposed oestradiol production that is associated
A SWAN substudy found that a pro-inflammatory adi- with stimulation of follicular development is exacer-
pokine profile is associated with an increased incidence bated by increases in FSH and luteinizing hormone
of vasomotor symptoms, particularly at early stages (LH) levels in response to diminished negative feedback
in the menopausal transition, suggesting that a pro- on the FSH–LH release from the pituitary due to loss
inflammatory milieu produced by adipose tissue neg- of inhibin B and progesterone1,5. Eventually, the ovary
atively affects thermoregulatory activity in the CNS126. is less responsive to gonadotropin stimulation during
Overweight also seems to be linked with a twofold to perimenopause, leading to reduced oestradiol produc-
fourfold higher incidence of urogenital symptoms in tion1. In turn, LH stimulation is blunted and insufficient
women with normal weight, including vaginal dis- to elicit ovulation.
charge, itching and irritation127, and increases the risk Anovulation leads to the loss of progesterone produc-
of developing urinary incontinence128. Body weight and tion1,5. Conversely, the postmenopausal ovary continues
body composition are also relevant to the incidence of to contribute substantially to the circulating levels of tes-
osteoporotic fractures. Weight loss in older women is tosterone for years134. Moreover, serum concentrations of
associated with a general increased risk of fracture129, adrenal androgens in midlife women might variably and
whereas weight gain is associated with a reduced risk of transiently increase in the late menopausal transition135.
hip fractures but an increased risk of other peripheral In particular, a rise in mean serum concentrations of
fractures, such as wrist fractures130. dehydroepiandrosterone sulfate (DHEAS) occurs in
most women between the early menopausal transition
HIV infection. HIV infection in menopausal women is and early postmenopause stages135. This changing hor-
associated with more severe hot flashes compared with monal environment produces a cascade of CNS-related
women who are not infected with HIV, independent of and peripheral symptoms of variable severity for an
CD4+ T cell count or duration of HIV positivity, and unpredictable amount of time.
leads to interference with daily activities and a lower
quality of life131. More support should be provided for Vasomotor symptoms and sleep disruption
Premenstrual syndrome women who are HIV positive in coping with meno- Alterations in thermoregulation are the leading hypo
A heterogeneous group of
pausal symptoms, as a reduction in quality of life might thesized mechanisms underlying vasomotor symp-
emotional symptoms, such as
irritability and food cravings, reduce adherence to anti-retroviral therapy 131. toms136. Menopause is associated with a reduction in
and physical symptoms, such the thermoneutral zone of the body, meaning that
as bloating, breast tenderness Socioeconomic status. Approximately 5% of perimen- minor increases in core body temperature can trigger
and abdominal pain, that opausal women experience symptoms in clusters132. In an excessive thermoregulatory reaction and promote
precede the menstrual period.
particular, symptoms related to mood, sleep and sexual heat dissipation by peripheral vasodilation and sweat-
Anovulation activity arise simultaneously, and factors that favour the ing 137. The thermoregulatory circuit is composed of
The absence of ovulation. emergence of these clustered symptoms include low functional elements that are under catecholaminergic
8 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
and/or serotonergic control138, and the hypothalamus is role in stabilizing the thermoneutral zone. Indeed, vas-
ascribed a key role in the integration of thermal informa- omotor phenomena are more common in periods of
tion and in the control of thermoregulatory reactions138. amenorrhoea, which are characterized by fluctuations
During perimenopause, hormonal cycles desynchronize, in oestrogen levels139. The slow progression, reduction
leading to erratic levels of sex hormones, which often peak and final disappearance of vasomotor symptoms dur-
and plummet133. Thermoregulatory dysfunction might be ing menopausal transition suggest a readjustment of the
a result of a maladaptation of the brain to this acyclicity, brain to the different concentrations of hormones and
with alterations in the function of noradrenergic and sero- neurotransmitters, a process that might require a variable
toninergic pathways137 (FIG. 2) that normally have a decisive amount of time, depending on the individual.
b
a
Mood and cognitive functions:
Vasomotor symptoms neuroendocrine activity
and sleep disruption ↑ Noradrenaline ↓ GABA-ergic function
↑ Noradrenaline ↓ Dopamine ↓ β-endorphin
↓ Dopamine
↓ Serotonin
↓ Serotonin ↓ Allopregnanolone c
↓ Androstenedione ↓ DHEA Urogenital symptoms,
↑ Neurokinin B ↓ Testosterone ↓ DHEAS
↑ Kisspeptin libido and sexual arousal
↓ E2 ↑ Cortisol ↓ E1
↑ Dynorphin ↑ Amyloid-β ↑ Cortisol:DHEA ratio
↑ Cortisol ↓ E2
↓ Androstenedione
g ↓ Testosterone
↓ Inhibin B ↓ DHEA
Skin ageing ↓ DHEAS
and hair changes ↑ FSH
↓ Oestrogen:androgen ratio ↑ LH
↓ Testosterone ↓ E2
↓ Dihydrotestosterone ↓ Progesterone
d
f Metabolic and cardiovascular changes
Bone remodelling ↑ LDL cholesterol ↓ HDL cholesterol
↓ E2 ↑ IL-1 e ↑ FFA ↓ SHBG
↑ N-telopeptide ↑ IL-6 Muscle changes ↑ Triglycerides ↓ GH
of type 1 collagen ↑ TNFα ↓ GH ↑ Cortisol ↓ IGF1
↑ C-terminal telopeptide ↓ TGFβ ↓ IGF1 ↑ Testosterone ↓ GH:IGF1 ratio
of type 1 collagen ↑ T-cell activation ↓ IGFBP3 ↑ Leptin ↓ Adiponectin
↑ Pyridinoline crosslinks ↓ Testosterone ↑ Renin–angiotensin ↓ NO
system
Figure 2 | Endocrine implications of menopausal symptoms and changes. After menopause, NaturetheReviews | Endocrinology
ovaries are depleted of
follicles, oestradiol (E2) and inhibin B production falls and ovulation and menstruation no longer occur. The loss of ovarian
sensitivity to follicle-stimulating hormone (FSH) and luteinizing hormone (LH) and the loss of negative feedback of E2 and
inhibin B on the hypothalamic–pituitary unit result in increased production and release of gonadotropin release hormone
(GnRH), FSH and LH. Increased FSH levels are particularly specific to postmenopause. a | Modifications of gonadotropins, E2,
alterations in the function of noradrenergic and serotoninergic pathways, and opioid tone in the hypothalamus cause the
onset of vasomotor symptoms and consequent sleep disruption. Thermoregulatory dysfunction might be a result of a
maladaptation of the brain to kisspeptin, neurokinin B and dynorphin (KNDy) neuron hypertrophy, which project to the
preoptic thermoregulatory area. b | Mood, cognitive functions and neuroendocrine activity, which are closely related to
the impairment of GABAergic, opioid and neurosteroid neurotransmitter milieu in the central nervous system (CNS), occur
with ageing. Failure of the main target of neurosteroids, the GABA‑A receptor, to adapt to changes in levels of
allopregnanolone over the course of the menopausal transition might lead to depressive symptoms, mood and cognitive
dysfunctions. c | Peripheral levels of oestrogen (oestrone (E1), and E2) withdrawal affects all the tissue expressing oestrogen
receptors (ERs), such as the epithelial tissues of the bladder trigone, urethra, vaginal mucosa, pelvic muscles, and fascia and
gastrointestinal mucosa, leading to vulvovaginal atrophy and urogenital symptoms, the so-called genitourinary syndrome.
The menopausal condition induces reductions in oestrogens and ovarian and adrenal steroids (testosterone,
androstenedione, dehydroepiandrosterone (DHEA) and dehydroepiandrosterone sulfate (DHEAS)), which might contribute
to the onset of sexual dysfunction. d | Increased levels of LDL cholesterol, triglycerides, free fatty acids (FFA), cortisol and
testosterone, together with the decreased levels of HDL cholesterol, sex hormone-binding globulin (SHBG), growth
hormone (GH), insulin-like growth factor 1 (IGF1) and the GH:IGF1 ratio, facilitate the onset of menopausal metabolic
syndrome, which is characterized by an altered lipid profile, hyperinsulinaemia, increased gluconeogenesis, abdominal
obesity and overweight with a consequent rise in cardiovascular risk. e | Loss of oestrogen exposure leads to a progressive
decline in levels of GH and IGF1 and their binding protein insulin-like growth factor-binding protein 3 (IGFBP3), which
reduces muscle mass. The associated decline in androgen production is responsible for the onset of sarcopenia.
f | Circulating E2 levels decline after menopause, and bone resorption exceeds bone formation. Loss in bone mass is
demonstrated by the rise in circulating levels of bone resorption markers, such as N‑telopeptide of type 1 collagen,
C‑terminal telopeptide of type 1 collagen and pyridinoline crosslinks. In bone, oestrogen deficiency also leads to immune
cell activation, resulting in increased pro-inflammatory cytokine levels. g | Dihydrotestosterone, the peripherally active
form of testosterone, is responsible for the gradual involution of scalp hair follicles in androgenic alopecia and hair
changes. NO, nitric oxide; TGFβ, transforming growth factor-β; TNFα, tumour necrosis factor-α.
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 9
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Although initial studies reported that LH pulses occur neuropeptides (such as β‑endorphin and neurosteroids,
during hot flashes in postmenopausal women, a causative namely, allopregnanolone and dehydroepiandrosterone
link was never found139. The emerging hypothesis link- (DHEA)) (FIG. 2) and can also influence the electrical
ing these two events temporally involves the discovery excitability, function and morphological features of the
that kisspeptin, neurokinin B and dynorphin (KNDy) synapses148. Thus, unstable levels of oestrogen during
neurons, which project to the preoptic thermoregula- perimenopause might cause the transient cognitive defi-
tory area, also regulate the hypothalamic GnRH pulse cits that are observed clinically at this time148. However,
generator, most likely by mediating oestrogen-dependent the link between circulating levels of oestradiol and cog-
negative feedback of LH secretion140. At postmenopause, nitive impairment is not well established, and clinical
KNDy neurons undergo hypertrophy, and the expres- trials evaluating hormone therapy in women at midlife
sion of the genes encoding neurokinin B and kisspeptin have not shown improvements in cognition45. It has been
increases as a result of oestrogen withdrawal, leading to shown that the concomitant rise in LH levels that occur
increased signalling to heat dissipation effectors in the with ovarian failure might drive both cognitive dysfunc-
CNS and to GnRH neurons140 (FIG. 2). tion and loss of spine density in an independent man-
There is also evidence in the literature that severe ner 149. Indeed, animal studies have shown that lowering
vasomotor symptoms are associated with activation of the peripheral levels of LH using leuprolide acetate, a
the hypothalamus–pituitary–adrenal axis, as increased GnRH agonist, improved cognition and spatial memory
urinary cortisol secretion has been reported during the and increased spine density 149. Persistently high levels
late menopausal transition stage in women with severe of FSH and LH have been linked to Alzheimer disease in
vasomotor symptoms compared with women who have postmenopausal women, and it is hypothesized that these
mild complaints141, and higher salivary cortisol levels hormones might be responsible for increased production
have also been associated with more frequent, severe of amyloid‑β, a main constituent of senile plaques150.
and bothersome daily self-reported hot flashes142. Higher Indeed, pharmacological suppression of LH and FSH
circulating concentrations of cortisol and noradrenaline using leuprolide acetate reduced plaque formation in
were also reported in women at the menopausal tran- animal models of Alzheimer disease151.
sition or the early postmenopausal stages who experi- According to the oestradiol withdrawal hypothesis,
enced vasomotor symptoms143. Increased cortisol might migraine in women are triggered by the sudden decline
activate a stress response with a consequent increase in in oestrogen levels that occurs immediately before
catecholamines, adrenaline and noradrenaline, which, menses, during the menopausal transition or in the
in turn, induce vasodilation141. early postmenopausal period152. There is accumulat-
The biological mechanisms underlying the sleep dif- ing evidence that changes in oestradiol levels in the
ficulties that develop during menopausal transition are brain might precipitate a kind of neurogenic inflam-
still unclear. Lower levels of inhibin B, a marker of the mation that is characterized by vasodilation, release
early menopausal transition, have been found to strongly of pro-inflammatory mediators and plasma extra
predict poor sleep quality 39,144 in women at late meno- vasation153, leading to the typically reported throbbing
pausal transition and at postmenopause, whereas higher and pulsing pain.
mean urinary FSH levels, the hallmark of ovarian failure,
have been associated with poor sleep quality in premen- Mood changes
opausal and perimenopausal women50,145. In addition, a The most accredited likely biological hypothesis under-
faster rate of increase in FSH levels has been associated lying changes in mood is that fluctuations in levels of
with longer sleep duration, indicative of less restful sleep steroid hormones, more than their decline, might trigger
and more non-REM sleep24. Postmenopausal women also perimenopausal depression154. It seems that the longer
show an advanced onset of melatonin release compared the duration of the menopausal transition, and there-
with premenopausal women146; therefore, advanced cir- fore the longer the exposure to fluctuating hormones,
cadian phase might contribute to early morning awak- the greater the risk of perimenopausal depression155.
ening, a common complaint in menopausal women35. In the Penn Ovarian Ageing Study 156, it was found that
Furthermore, obstructive sleep apnoea might exacerbate a more rapid rise in FSH levels before the FMP was pre-
these sleep difficulties in menopausal women. Reduced dictive of a lower risk of depressive symptoms after the
levels of progesterone, a respiratory stimulant, in peri- FMP, suggesting that a shorter menopausal transition
menopausal woman might be the underlying cause of protects against perimenopausal depression. A subset
this nocturnal breathing disorder 147. of perimenopausal women might have an increased
sensitivity to changes in gonadal steroids, specifically
Cognitive changes and migraine oestrogens and progesterone, which in turn modulate
Oestradiol is believed to have a major role in cognitive neuroregulatory systems associated with mood and
performance as anatomical studies have demonstrated behaviour 154. In particular, fluctuating oestrogen levels
that the hippocampus and prefrontal cortex, which medi- might lead to dysregulation of serotonin and noradren-
ate episodic and working memory, express high levels of aline pathways in the CNS as oestrogen facilitates a
oestrogen receptors (ERs)148. In these areas of the CNS, number of actions of serotonin and noradrenaline, spe-
oestradiol-dependent activation of ERs can modulate the cifically by modulating receptor binding and the avail-
synthesis, release and metabolism of neurotransmitters ability of these neurohormones at the synaptic level154.
(such as serotonin, dopamine and acetylcholine) and In an interesting theoretical model157, fluctuations in
10 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
progesterone-derived neurosteroids, particularly allo- partner are negatively associated with FSH levels163, the
pregnanolone, caused by changes in oestradiol and pro- summiting of which marks ovarian failure. Moreover,
gesterone levels might underlie menopause-associated waning oestrogen levels in the late menopausal transi-
depressive symptoms. In particular, failure of the tion lead to decreased vascular congestion and lubrica-
GABA-A receptor — the main target of neurosteroids — tion of the vagina, resulting in unsatisfactory or painful
to adapt to changes in levels of allopregnanolone (FIG. 2) intercourse165.
over the course of the menopausal transition might lead
to depressive symptoms in vulnerable women, such as Metabolic and cardiovascular changes
those with a history of premenstrual dysphoric disorder From an endocrinological perspective, longitudinal
and/or postpartum depression157. The inability to main- studies have revealed that the menopausal transition is
tain GABAergic homeostatic control might exacerbate characterized by a shift from a predominately oestro-
the response of the hypothalamus–pituitary–adrenal genic hormonal state to an androgenic state owing to
axis to stress. Indeed, there is increasing evidence that an increase in bioavailable testosterone levels3,62,166. The
dysregulation of the hypothalamus–pituitary–adrenal menopausal ovary continues to produce high amounts
axis, which is correlated with oestradiol fluctuation, of androgen for years after menopause, and the increase
might be implicated in the pathophysiology of peri- in gonadotropin levels drives ovarian androgen secretion
menopausal depression158. Moreover, very stressful life despite the substantial decline in oestrogen levels123. Sex
events seem to contribute greatly to the onset of depres- hormone-binding globulin (SHBG) levels decrease with
sive symptoms during the menopausal transition in the decreasing oestrogen concentrations, thereby increas-
presence of oestradiol variability 159 (FIG. 2). ing the free androgen index and enhancing the imbal-
ance between oestrogens and androgens3 (FIG. 2). The
Urogenital symptoms and sexual function increase in bioavailable testosterone can stimulate fat
The lower genital and lower urinary tracts share a com- accumulation in preadipocytes of visceral fat 64. Visceral
mon embryonic origin in the female and express high fat adipocytes express high levels of androgen receptors
numbers of ERs during the reproductive years160; as a that are downregulated by oestrogens167; therefore, when
result, both of these tissues are affected by long-term oestrogen levels decline, visceral fat might become more
hypoestrogenism during menopause. From a histological sensitive to the negative effects of androgens. Indeed, it
point of view, after menopause, these tissues exhibit seems that the change in the bioavailability of androgens
reduced collagen content and hyalinization, decreased can predict accumulation of visceral fat over a period
elastin content, thinning of the epithelium, altered mor- of 5 years168. Moreover, menopausal women with more
phology and function of smooth muscle cells, increased rapidly increasing levels of bioavailable testosterone
density of connective tissue and fewer blood vessels160,161. undergo larger increases in adiposity than women with
Vaginal blood flow is reduced, as well as the lubrication more stable levels, whereas women with slowly increas-
and elasticity of the vagina, leading to shortening and ing levels of bioavailable testosterone experience smaller
narrowing of the vagina and, consequently, dyspareunia increases in adipose tissue168. Rising FSH levels might
and easy fissuring of the vaginal walls160. Approximately also contribute to this phenomenon, as the FSH receptor
20% of postmenopausal women develop urge inconti- (FSHR) is expressed in visceral fat adipocytes169, and ani-
nence, and ~50% develop stress incontinence75; however, mal studies have indicated that FSHR signalling might
only the incidence of urge incontinence is affected by increase adipocyte lipid synthesis and lead to elevated
long-term oestrogen depletion. It is hypothesized that levels of leptin and decreased levels of adiponectin in
the lack of oestrogenic activity in the trigone of the blad- serum, therefore promoting fat accumulation169.
der and the urethra might decrease the sensory thresh- In postmenopausal women, increasing levels of bio-
old and lower the urethral closure pressure and Valsalva available testosterone and decreasing SHBG levels are
leak-point pressure, therefore contributing to urinary exacerbated by insulin resistance, and low SHBG lev-
urgency 162 (BOX 1). els are predictive of incident type 2 diabetes mellitus in
Pinpointing a biological cause for sexual dysfunction postmenopausal women170. Insulin resistance and central
in menopausal women is extremely difficult due to the obesity, the hallmarks of the metabolic syndrome, occur
complexity of this domain; changes in sexual activity in many postmenopausal women171. Furthermore, the
depend on changes in sexual desire and partner satis- lack of oestrogens per se seems to favour accumulation
Urethral closure pressure
faction, dyspareunia due to vaginal dryness and general and a central distribution of adipose tissue172. Studies
The fluid pressure needed to health. Important associations between endogenous performed in human and animals have shown that
open a closed urethra. levels of reproductive hormones and sexual function oestrogens regulate food intake negatively and energy
in women going through the menopausal transition expenditure positively, promote free fatty acid (FFA)
Valsalva leak-point pressure
have been reported. Masturbation, desire and arousal uptake and triacylglyceride synthesis in gluteofemoral
The lowest abdominal pressure
required during a stress activity were positively associated with levels of testosterone adipose tissue (rather than in abdominal subcutaneous
that causes the urethra to open and DHEAS, supporting a role for androgens in female adipose tissue) and inhibit adipose tissue depot-specific
and leak. sexual function163,164 (FIG. 2). Indeed, with the exception pathophysiological processes that lead to morbidity 172.
of surgical menopause, after which testosterone lev- In addition, lower concentrations of oestradiol were
Free androgen index
An index that represents the
els tend to decrease abruptly, androgen levels do not found to be markedly associated with greater volumes
ratio of bioactive circulating decline immediately following natural menopause134. of paracardial adipose tissue in women at midlife, while
testosterone. Masturbation, arousal and the ability to climax with a the free androgen index was found to correlate positively
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 11
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
with fat around the aorta, and SHBG levels were found of bone resorption markers — such as N‑telopeptide of
to correlate negatively with fat in all evaluated cardio- type 1 collagen, C‑terminal telopeptide of type 1 col-
vascular depots70. Negative changes in endothelial cell lagen and pyridinoline crosslinks — increase by 90%
function might also influence the increased risk of CVD after menopause, whereas markers of bone formation
that is observed in postmenopausal women. Oestrogen increase by only 45%185 (FIG. 2). Oestrogens are known
deficiency leads to activation of the renin–angiotensin to stimulate osteoblast proliferation and differentiation,
system, as well as upregulation of endothelin, a potent therefore promoting deposition and mineralization of
vasoconstrictor 173. Conversely, oestrogen deficiency leads bone matrix, and can also induce apoptosis in osteo-
to impaired oestradiol-induced signalling, resulting in clasts. Their effect on osteoblasts, osteoclasts and oste-
the reduced release of cardioprotective nitric oxide174. ocytes occurs through activation of high affinity ERs,
Together, these changes accelerate atherogenesis in per- including the ERα and ERβ isoforms186. In bone, oestro-
imenopausal women, increasing their susceptibility to gen deficiency also leads to immune cell activation and
ischaemic heart disease and CVD. the resulting pro-inflammatory cytokine milieu further
enhances bone resorption186.
Muscle loss and bone remodelling The loss of ovarian function might also be associated
Studies indicating the presence of ERs on muscle tis- with an increase in joint abnormalities with an increase
sue, particularly on type II muscle fibres, have led to the in pain. Indeed, ERs are present in joint tissues, and
hypothesis that a loss of ovarian function might have a hypoestrogenism might affect cartilage, periarticular
direct negative effect on muscle tissue175. As oestradiol bone, synovial lining, ligaments and the joint capsule187.
signalling through ERα and ERβ favours the binding of It is established that females are predisposed towards
myosin to actin during muscle contraction, the loss of knee osteoarthritis, which might be in part attribut-
oestrogen exposure might reduce the intrinsic quality able to sex differences in cartilage health, even before
of skeletal muscle whereby muscle fibres have a reduced the onset of clinical knee disease188. Indeed, women at
capacity to generate force176. Maintenance of muscle midlife show a markedly greater annual loss of total
mass is known to depend on growth hormone (GH) tibial and patellar cartilage than men188. However, more
secretion, and GH production decreases gradually with research is necessary to address joint health, specifically
age in both males and females177. However, menopause in menopausal women.
leads to a marked decline in 24‑hour mean serum concen-
trations of GH, insulin-like growth factor 1 (IGF1) and Skin ageing and hair changes
its binding protein insulin-like growth factor-binding Total collagen content was shown to decline at an aver-
protein 3 (IGFBP3), which are also involved in mainte- age rate of 2.1% per year in postmenopausal women
nance of muscle178 (FIG. 2). Secretion of GH is influenced over a period of 15 years, with a loss of as much as 30%
considerably by oestrogen levels, which probably occurs within the first 5 years after the FMP86. Consequently,
through ERα stimulation in the CNS178. Thus, oestro- skin thickness decreases at a rate of 1.13% per year in
gen deficiency might contribute to the ageing-related postmenopausal women97, whereas skin elasticity seems
decline in GH concentrations. This decline in GH levels to decline at a rate of 1.5% per year in early postmeno-
leads to a 1–1.5% reduction in muscle mass in men and pausal women189. The levels of melanocytes in skin also
women from approximately age 40 years onwards179, decline at a rate of 10–20% per decade in postmenopausal
which is paralleled by an increase in visceral fat con- women, leading to focal depigmentation and uneven col-
tent180. Visceral adiposity and hyperinsulinaemia, in turn, our of the skin98. These skin changes are worsened by the
can further reduce GH secretion, leading to the devel- atrophy of the dermal vascular network that occurs after
opment of a vicious cycle of muscle loss180. Increasing menopause, resulting in reduced provision of circulating
body weight with age, along with the increased levels nutrients and hormones97. In addition, hair loss might
of pro-inflammatory cytokines and oxidative stress that be due to an altered oestrogen:androgen ratio favouring
occur at menopause, might also favour muscle catabo- increased androgen activity (FIG. 2), resulting in a decrease
lism181. Together, these changes determine a decrease in in the duration of the anagen phase of the hair follicle190.
muscle mass, strength and mobility in postmenopausal Dihydrotestosterone — the peripherally active form of
women181–183. Finally, sarcopenia in women might also be testosterone produced by metabolism of testosterone via
related to the ultimate decline in androgen production. 5 alpha-reductase — is responsible for the gradual invo-
Indeed, a longitudinal study in ageing Japanese women lution of scalp hair follicles in androgenic alopecia191. In
demonstrated that the decrease in free testosterone levels genetically susceptible women, dihydrotestosterone pro-
can predict the risk of loss of appendicular muscle184. duces a transformation from terminal to vellus hairs191.
Arguably the most important change in the musculo The anagen phase of hair growth is progressively short-
skeletal system during menopause is the loss in BMD. ened, whereas the telogen phase is lengthened, leading,
After attainment of peak bone mass in early adulthood, over successive cycles, to the involution of hair follicles191.
maintenance of normal bone structure is ensured by a A prevalence of androgenic activity has an opposite effect
fine equilibrium between osteoblastic bone formation on facial hair, as nearly 50% of women report excessive
and osteoclastic bone resorption5. When oestrogen levels facial hair growth after menopause192; in this case, andro-
decline after menopause, bone resorption exceeds bone gens are responsible for increasing hair follicle size, hair
formation during each bone remodelling cycle, resulting shaft diameter and increased duration of the anagen
in a net loss in bone mass185. Indeed, circulating levels phase of terminal hairs192.
12 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Predicting future health increases the risk of specific pelvic floor disorders, such
Data are emerging from the literature demonstrating as pelvic organ prolapse or faecal incontinence205. Bone
that the presence of some menopausal symptoms might tissue also seems to deteriorate more in menopausal
predict a clinically relevant higher risk of developing women with vasomotor symptoms who have low spine
other disorders. An increasing number of studies are and femoral neck BMD206. Furthermore, menopausal
reporting that severe vasomotor symptoms might be women with vasomotor symptoms have increased rates
associated with poor cardiovascular health. Indeed, of hip fractures compared with asymptomatic women, as
women who reported frequent hot flashes were found observed in a prospective study with a mean follow‑up
to have a higher carotid intima–media thickness than of 8.2 years206.
women who did not report hot flashes193. In addition, Age acceleration effects can be estimated by comparing
a higher incidence of arterial endothelial dysfunction, DNA methylation age — measured in various tissues such
indicated by impaired flow-mediated dilation of the as blood, saliva and buccal mucosa — with an individual’s
brachial artery, has been reported in women during chronological age. A study from 2016 has demonstrated
the menopausal transition who present with hot that menopause accelerates epigenetic ageing in women,
flashes than in women lacking these symptoms194. Data therefore showing that age at menopause is a determinant
also indicate that women at midlife have decreased of biological ageing 207. The finding is particularly relevant
cardiac vagal control (that is, reduced parasympathetic for women who undergo bilateral oophorectomy before
cardiac regulation) during vasomotor symptoms195. natural menopause because the premature removal of
Furthermore, it has been reported that vasomotor the ovaries will accelerate the ageing process; this might
symptoms are associated with an unfavourable haemo- explain the increasing evidence that surgical menopause
dynamic profile characterized by a lower overall cardiac raises the risk of premature death, CVD, dementia,
index and stroke volume index, a higher overall vascular osteoporosis and bone fractures207.
resistance index and greater levels of the pro-inflamma-
tory cytokine IL‑6 (REF. 195). Finally, late postmenopau- Conclusions
sal women with vasomotor symptoms have a higher Symptoms of menopause are distressing for most
prevalence of a previous diagnosis of hypertension than women. CNS-related symptoms such as hot flashes,
women without symptoms, indicating that the endothe- mood and sleep disorders, migraine, and memory and
lial dysfunction developed during early postmenopause learning difficulties seem to depend on acyclical fluc-
might predict the development of hypertension at late tuations in oestradiol levels, specifically, sudden oestra-
postmenopause196. Vasomotor symptoms are also associ- diol withdrawal, which causes secondary neurochemical
ated with a procoagulant haemostatic profile and might changes. Apart from developing vasomotor symptoms
increase the risk of arterial or venous thrombosis197. such as hot flashes and night sweats, women transi-
When clinical cardiovascular events are considered, it tioning through menopause might also be vulnerable
seems that women with current signs and symptoms to developing anxiety, depression, poor quality of sleep
of myocardial ischaemia who present with vasomotor and migraine. By contrast, physical symptoms such as
symptoms beginning early in midlife have a higher mor- urogenital atrophy, ageing of the skin and skeletal frac-
tality due to CVD and reduced endothelial function than tures due to postmenopausal osteoporosis are secondary
women who have later onset of vasomotor symptoms198. to the decline in oestradiol levels. The accumulation and
Sleep disturbances, such as shorter duration and lower central distribution of body fat, hair loss, the develop-
overall quality of sleep, might also be risk factors for ment of facial hair and sexual dysfunction are seemingly
cardiovascular health as they have been associated with due to transitional increases in androgen bioavailability.
a greater degree of aortic calcification199 and increased Data from longitudinal studies have demonstrated
carotid atherosclerosis among women at midlife 200. that many factors can contribute to worsening a wom-
Furthermore, vasomotor symptoms in addition to an’s experience of menopause. Ethnicity seems to largely
poor sleep quality seem to favour the onset of depres- affect how a woman will experience the menopau-
Cardiac vagal control sive symptoms during the menopausal transition201. In sal transition. Indeed, European and Latin American
An index of parasympathetic a study where the GnRH agonist leuprolide was used women have a higher prevalence of hot flashes, sleepless-
contribution to cardiac to induce oestradiol suppression in premenopausal ness, mood changes, irritability and reduced sex drive
regulation. women, it was shown that depressive symptoms are asso- than women of other ethnicities, and African-American
Cardiac index
ciated with objectively and subjectively measured sleep women experience particularly persistent vasomotor
The volume of blood pumped disturbance and the number of night-time, but not day- symptoms. Climatic factors such as higher temperatures
by the heart in a minute per time, hot flashes202. In the SWAN cohort, women with or lower altitudes are also associated with higher inci-
body surface. more mood-related symptoms and moderate to severe dence of hot flashes and night sweats. In addition, low
vasomotor symptoms displayed worse cognitive perfor- exposure to sunlight, an issue particularly in northern
Stroke volume index
The volume of blood pumped mance51,52. Awareness of depressive symptoms at midlife European countries, increases the risk of osteoporotic
by the heart with each beat per is also important as there is some indication that they bone fracture. Obesity is another major individual fac-
body surface. might be associated with the development of dementia tor that influences symptom prevalence and, contrary
in later life203. Urinary symptoms, such as nocturia and to past belief, does not protect against hot flashes but
Vascular resistance index
An index representing the
stress incontinence, are associated with body fat and vis- actually increases the risk of severe vasomotor symp-
degree to which blood vessels ceral fat accumulation and also with sleep disorders204. toms. Moreover, obesity is associated with a higher
impede the flow of blood. Moreover, the presence of vulvovaginal symptoms incidence of urogenital symptoms (including vaginal
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 13
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
discharge, itching and irritation) compared with women the ageing process, it is conceivable that, in addition to
with normal weight and increases the risk of urinary loss of ovarian function, the manifestation of menopausal
incontinence. Anxiety and chronic illness (such as HIV symptoms might be in part due to ageing.
positivity) also heighten the risk of vasomotor symp- The large number of studies performed over the past
toms. Mood, memory and sleep disorders arise more in decade in women transitioning through menopause
women who experienced past abuse or those with a his- underscore the need to closely monitor health param-
tory of premenstrual syndrome. Lower socioeconomic eters at this stage and to promote a healthy lifestyle.
and educational background, poor general health and These changes in health-care practice should start before
stressful life events also favour the onset of menopausal the menopausal transition to counteract the emergent
symptoms in clusters. cardiovascular risk factors and possibly reduce bother-
An emerging concept is that some menopausal symp- some symptomatology. It is also important for medical
toms might be predictive of future health complications. practitioners to consider a woman’s home and work
Indeed, severe vasomotor symptomatology and poor environment and also her ethnicity, as these factors will
quality of sleep are associated with an increased risk of also profoundly affect her experience through meno-
CVD and postmenopausal depression. Furthermore, pause. Although the management of symptoms through
depressive symptoms, vasomotor symptoms and sleep pharmacological or cognitive-behavioural therapy
disorders might increase the susceptibility to developing approaches might improve quality of life in the short
cognitive dysfunction. Severe hot flashes have also been term, future research will be necessary to develop strat-
associated with an increased risk of osteoporosis and egies to modify health risks, which are often intensified
bone fracture. Finally, as menopause seems to accelerate by the loss of ovarian function, in the long term.
1. Harlow, S. D. et al. Executive summary of the stages of 17. Pien, G. W., Sammel, M. D., Freeman, E. W., Lin, H. & 31. Freeman, E. W. Depression in the menopause
reproductive aging workshop +10: addressing the DeBlasis, T. L. Predictors of sleep quality in women in transition: risks in the changing hormone milieu as
unfinished agenda of staging reproductive aging. the menopausal transition. Sleep 31, 991–999 observed in the general population. Womens Midlife
Menopause 19, 387–395 (2012). (2008). Health 1, 1 (2015).
2. Woods, N. F. & Mitchell, E. S. Symptoms during the 18. Baker, F. C., Willoughby, A. R., Sassoon, S. A., 32. Bromberger, J. T. et al. Does risk for anxiety increase
perimenopause: prevalence, severity, trajectory, and Colrain, I. M. & de Zambotti, M. Insomnia in women during the menopausal transition? Study of women’s
significance in women’s lives. Am. J. Med. 118, 14–24 approaching menopause: beyond perception. health across the nation (SWAN). Menopause 20,
(2005). Psychoneuroendocrinology 60, 96–104 (2015). 488–495 (2013).
3. Sutton-Tyrrell, K. et al. Reproductive hormones and 19. Campbell, I. G. et al. Evaluation of the association 33. Weber, M. T., Mapstone, M., Staskiewicz, J. &
obesity: 9 years of observation from the study of of menopausal status with delta and beta EEG Maki, P. M. Reconciling subjective memory complaints
women’s health across the nation. Am. J. Epidemiol. activity during sleep. Sleep 34, 1561–1568 with objective memory performance in the
171, 1203–1213 (2010). (2011). menopausal transition. Menopause 19, 735–741
4. Barbieri, R. L., Smith, S. & Ryan, K. J. The role of 20. Jordan, A. S., McSharry, D. G. & Malhotra, A. Adult (2012).
hyperinsulinemia in the pathogenesis of ovarian obstructive sleep apnoea. Lancet 383, 736–747 34. Greendale, G. A. et al. Effects of the menopause
hyperandrogenism. Fertil. Steril. 50, 197–212 (2014). transition and hormone use on cognitive performance
(1988). 21. Kerner, N. A. & Roose, S. P. Obstructive sleep apnea is in midlife women. Neurology 72, 1850–1857
5. Davis, S. R. et al. Menopause. Nat. Rev. Dis. Primers. linked to depression and cognitive impairment: (2009).
1, 15004 (2015). evidence and potential mechanisms. Am. J. Geriatr. 35. Epperson, C. N., Sammel, M. D. & Freeman, E. W.
6. Politi, M. C., Schleinitz, M. D. & Col, N. F. Revisiting Psychiatry 24, 496–508 (2016). Menopause effects on verbal memory: findings from a
the duration of vasomotor symptoms of menopause: 22. Lal, C., DiBartolo, M. M., Kumbhare, S., Strange, C. & longitudinal community cohort. J. Clin. Endocrinol.
a meta-analysis. J. Gen. Intern. Med. 23, 1507–1513 Joseph, J. E. Impact of obstructive sleep apnea Metab. 98, 3829–3838 (2013).
(2008). syndrome on cognition in early postmenopausal 36. Fuh, J. L., Wang, S. J., Lee, S. J., Lu, S. R. &
7. Freeman, E. W., Sammel, M. D., Lin, H., Liu, Z. & women. Sleep Breath. 20, 621–626 (2016). Juang, K. D. A longitudinal study of cognition change
Gracia, C. R. Duration of menopausal hot flushes 23. Freeman, E. W. et al. Hormones and menopausal during early menopausal transition in a rural
and associated risk factors. Obstet. Gynecol. 117, status as predictors of depression in women in community. Maturitas 53, 447–453 (2006).
1095–1104 (2011). transition to menopause. Arch. Gen. Psychiatry 61, 37. Karlamangla, A. S., Lachman, M. E., Han, W.,
8. Zeleke, B. M., Bell, R. J., Billah, B. & Davis, S. R. 62–70 (2004). Huang, M. & Greendale, G. A. Evidence for cognitive
Vasomotor and sexual symptoms in older Australian 24. Bromberger, J. T. et al. Depressive symptoms during aging in midlife women: study of women’s health
women: a cross-sectional study. Fertil. Steril. 105, the menopausal transition: the study of women’s across the nation. PLoS One 12, e0169008 (2017).
149–155 (2016). health across the nation (SWAN). J. Affect. Disord. 38. Rocca, W. A. et al. Increased risk of cognitive
9. Avis, N. E. et al. Duration of menopausal vasomotor 103, 267–272 (2007). impairment or dementia in women who underwent
symptoms over the menopause transition. JAMA 25. Woods, N. F. et al. Depressed mood during the oophorectomy before menopause. Neurology 69,
Intern. Med. 175, 531–539 (2015). menopausal transition and early postmenopause: 1074–1083 (2007).
10. Kravitz, H. M. et al. An actigraphy study of sleep and observations from the Seattle midlife women’s health 39. Kurita, K. et al. Association of bilateral oophorectomy
pain in midlife women: the study of women’s health study. Menopause 15, 223–232 (2008). with cognitive function in healthy, postmenopausal
across the nation sleep study. Menopause 22, 26. Weber, M. T., Maki, P. M. & McDermott, M. P. women. Fertil. Steril. 106, 749–756 (2016).
710–718 (2015). Cognition & mood in perimenopause: a systematic 40. Greendale, G. A., Derby, C. A. & Maki, P. M.
11. Freedman, R. R. & Roehrs, T. A. Effects of REM review & meta-analysis. J. Steroid Biochem. Mol. Biol. Perimenopause and cognition. Obstet. Gynecol. Clin.
sleep and ambient temperature on hot flash- 142, 90–98 (2014). North Am. 38, 519–535 (2011).
induced sleep disturbance. Menopause 13, 27. Bromberger, J. T. et al. Longitudinal change in 41. Drogos, L. L. et al. Objective cognitive performance is
576–583 (2006). reproductive hormones and depressive symptoms related to subjective memory complaints in midlife
12. Bianchi, M. T., Kim, S., Galvan, T., White, D. P. & across the menopausal transition: results from the women with moderate to severe vasomotor symptoms.
Joffe, H. Nocturnal hot flashes: relationship to study of women’s health across the nation (SWAN). Menopause 20, 10 (2013).
objective awakenings and sleep stage transitions. Arch. Gen. Psychiatry 67, 598–607 (2010). 42. Medic, G., Wille, M. & Hemels, M. E. Short- and long-
J. Clin. Sleep Med. 12, 1003–1009 (2016). 28. Kessler, R. C. et al. The epidemiology of major term health consequences of sleep disruption.
13. Joffe, H., Massler, A. & Sharkey, K. M. Evaluation and depressive disorder: results from the national Nat. Sci. Sleep 9, 151–161 (2017).
management of sleep disturbance during the comorbidity survey replication (NCS‑R). JAMA. 289, 43. Ripa, P. et al. Migraine in menopausal women:
menopause transition. Semin. Reprod. Med. 28, 3095–3105 (2003). a systematic review. Int. J. Womens Health 7,
404–421 (2010). 29. Bromberger, J. T., Schott, L., Kravitz, H. M. & 773–782 (2015).
14. Polo-Kantola, P. Sleep problems in midlife and beyond. Joffe, H. Risk factors for major depression during 44. Freeman, E. W., Sammel, M. D., Lin, H., Gracia, C. R.
Maturitas 68, 224–232 (2011). midlife among a community sample of women with & Kapoor, S. Symptoms in the menopausal transition:
15. Kravitz, H. M. et al. Sleep difficulty in women and without prior major depression: are they the hormone and behavioral correlates. Obstet. Gynecol.
at midlife: a community survey of sleep and the same or different? Psychol Med. 45, 1653–1664 111, 127–136 (2008).
menopausal transition. Menopause 10, 19–28 (2014). 45. Martin, V. T. et al. Perimenopause and menopause
(2003). 30. Bromberger, J. T. et al. Major depression during and are associated with high frequency headache in
16. Kravitz, H. M. & Joffe, H. Sleep during the after the menopausal transition: study of women’s women with migraine: results of the American
perimenopause: a SWAN story. Obstet. Gynecol. Clin. health across the nation (SWAN). Psychol Med. 9, migraine prevalence and prevention study. Headache
North Am. 38, 567–586 (2011). 1–10 (2011). 56, 292–305 (2016).
14 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
46. Davis, S. R. et al. Understanding weight gain at 69. Waetjen, L. E. et al. Factors associated with worsening 95. Gartoulla, P., Bell, R. J., Worsley, R.& Davis, S. R.
menopause. Climacteric 15, 419–429 (2012). and improving urinary incontinence across the Moderate-severely bothersome vasomotor symptoms
47. Sternfeld, B. et al. Physical activity and changes in menopausal transition. Obstet. Gynecol. 111, 667–677 are associated with lowered psychological general
weight and waist circumference in midlife women: (2008). wellbeing in women at midlife. Maturitas 81,
findings from the study of women’s health across the 70. Legendre, G., Ringa, V., Panjo, H., Zins, M. & Fritel, X. 487–492 (2015).
nation. Am. J. Epidemiol. 160, 912–922 (2004). Incidence and remission of urinary incontinence at 96. Sarti, S.& Zella, S. Changes in the labour market and
48. Karvonen-Gutierrez, C. & Kim, C. Association of mid- midlife: a cohort study. BJOG. 122, 816–824 health inequalities during the years of the recent
life changes in body size, body composition and (2015). economic downturn in Italy. Soc. Sci. Res. 57,
obesity status with the menopausal transition. 71. Botlero, R., Davis, S. R., Urquhart, D. M., 116–132 (2016).
Healthcare 4, E42 (2016). Shortreed, S. & Bell, R. J. Age-specific prevalence of, 97. Jack, G. et al. Menopause in the workplace: what
49. Kanaley, J. A., Giannopoulou, I., Tillapaugh-Fay, G., and factors associated with, different types of urinary employers should be doing. Maturitas 85, 88–95
Nappi, J. S. & Ploutz-Snyder, L. L. Racial differences in incontinence in community-dwelling Australian women (2016).
subcutaneous and visceral fat distribution in assessed with a validated questionnaire. Maturitas 98. Gartoulla, P. et al. Menopausal vasomotor symptoms
postmenopausal black and white women. Metabolism 62, 134–139 (2009). are associated with poor self-assessed work ability.
52, 186–191 (2003). 72. Avis, N. E. et al. Longitudinal changes in sexual Maturitas 87, 33–39 (2016).
50. Tchernof, A. et al. Ovarian hormone status and functioning as women transition through menopause: 99. Pinkerton, J. A. Money talks: untreated hot flashes
abdominal visceral adipose tissue metabolism. J. Clin. results from the study of women’s health across the cost women, the workplace, and society. Menopause
Endocrinol. Metab. 89, 3425–3430 (2004). nation (SWAN). Menopause 16, 442–452 (2009). 22, 254–255 (2015).
51. Lovejoy, J. C., Champagne, C. M., de Jonge, L., Xie, H. 73. Nappi, P. R. et al. Female sexual dysfunction (FSD): 100. Payne, S. & Doyal, L. Older women, work and health.
& Smith, S. R. Increased visceral fat and decreased prevalence and impact on quality of life (QoL). Occup. Med. 60, 172–177 (2010).
energy expenditure during the menopausal transition. Maturitas 94, 87–91 (2016). 101. Schoenaker, D. A., Jackson, C. A., Rowlands, J. V. &
Int. J. Obes. 32, 949–958 (2008). 74. Avis, N. E. et al. Change in sexual functioning over the Mishra, G. D. Socioeconomic position, lifestyle
52. Janssen, I., Powell, L. H., Kazlauskaite, R. & menopausal transition: results from the study of factors and age at natural menopause: a systematic
Dugan, S. A. Testosterone and visceral fat in midlife women’s health across the nation. Menopause 24, review and meta-analyses of studies across six
women: the study of women’s health across the nation 379–390 (2017). continents. Int. J. Epidemiol. 43, 1542–1562
(SWAN) fat patterning study. Obesity (Silver Spring) 75. Dundon, C. M. & Rellini, A. H. More than sexual (2014).
18, 604–610 (2010). function: predictors of sexual satisfaction in a sample 102. Genazzani, A. R. et al. The European menopause
53. Gibson, C. J., Thurston, R. C., El Khoudary, S. R., of women age 40–70. J. Sex. Med. 7, 896–904 survey 2005: women’s perceptions on menopause
Sutton-Tyrrell, K. & Matthews, K. A. Body mass index (2010). and postmenopause hormone therapy. Gynecol.
following natural menopause and hysterectomy with 76. Manolagas, S. C., O’Brien, C. A. & Almeida, M. The Endocrinol. 22, 369–375 (2006).
and without bilateral oophorectomy. Int. J. Obes. 37, role of estrogen and androgen receptors in bone 103. Chedraui, P., Aguirre, W., Hidalgo, L. & Fayad, L.
809–813 (2013). health and disease. Nat. Rev. Endocrinol. 9, 699–712 Assessing menopausal symptoms among healthy
54. Pou, K. M. et al. Visceral and subcutaneous adipose (2013). middle-aged women with the menopause rating scale.
tissue volumes are cross-sectionally related to 77. van Staa, T. P., Dennison, E. M., Leufkens, H. G. & Maturitas 57, 271–278 (2007).
markers of inflammation and oxidative stress: Cooper, C. Epidemiology of fractures in England and 104. Chedraui, P., San Miguel, G. & Avila, C. Quality of life
the Framingham Heart Study. Circulation 116, Wales. Bone 29, 517–522 (2001). impairment during the female menopausal transition
1234–1241 (2007). 78. Finkelstein, J. S. et al. Bone mineral density changes is related to personal and partner factors. Gynecol.
55. Lee, C. G. et al. Adipokines, inflammation, and visceral during the menopause transition in a multiethnic Endocrinol. 25, 130–135 (2009).
adiposity across the menopausal transition: a cohort of women. J. Clin. Endocrinol. Metab. 93, 105. Green, R. & Santoro, N. Menopausal symptoms and
prospective study. J. Clin. Endocrinol. Metab. 94, 861–868 (2008). ethnicity: the study of women’s health across the
1104–1110 (2009). 79. Douchi, T. et al. Relative contribution of aging and nation. Womens Health (Lond.) 5, 127–133 (2009).
56. Ravussin, E. & Smith, S. R. Increased fat intake, menopause to changes in lean and fat mass in 106. Islam, R. M., Bell, R. J., Rizvi, F. & Davis, S. R.
impaired fat oxidation, and failure of fat cell segmental regions. Maturitas 42, 301–306 (2002). Vasomotor symptoms in women in Asia appear
proliferation result in ectopic fat storage, insulin 80. Maltais, M. L. Desroches, J. & Dionne, I. J. Changes in comparable with women in Western countries:
resistance, and type 2 diabetes mellitus. Ann. NY muscle mass and strength after menopause. a systematic review. Menopause 24, 1313–1322
Acad. Sci. 967, 363–378 (2002). J. Musculoskelet. Neuronal Interact. 9, 186–197 (2017).
57. El Khoudary, S. R. et al. Cardiovascular fat, (2009). 107. Sriprasert, I. et al. An International menopause
menopause, and sex hormones in women: the SWAN 81. Rolland, Y. M. et al. Loss of appendicular muscle society study of vasomotor symptoms in Bangkok and
cardiovascular fat ancillary study. J. Clin. Endocrinol. mass and loss of muscle strength in young Chiang Mai, Thailand. Climacteric 20, 171–177
Metab. 100, 3304–3312 (2015). postmenopausal women. J. Gerontol. A Biol. Sci. (2017).
58. Matthews, K. A. et al. Are changes in cardiovascular Med. Sci. 62, 330–335 (2007). 108. Al Dughaither, A., Al Mutairy, H. & Al Ateeq, M.
disease risk factors in midlife women due to 82. Asikainen, T. M., Kukkonen-Harjula, K. & Miilunpalo, S. Menopausal symptoms and quality of life among
chronological aging or to the menopausal transition? Exercise for health for early postmenopausal women: a Saudi women visiting primary care clinics in Riyadh,
J. Am. Coll. Cardiol. 54, 2366–2373 (2009). systematic review of randomised controlled trials. Saudi Arabia. Int. J. Womens Health. 29, 645–653
59. El Khoudary, S. R. et al. Increase HDL‑C level over Sports Med. 34, 753–778 (2004). (2015).
the menopausal transition is associated with greater 83. Srikanth, V. K. et al. A meta-analysis of sex differences 109. Stefanopoulou, E. et al. IMS study of climate, altitude,
atherosclerotic progression. J. Clin. Lipidol. 10, prevalence, incidence and severity of osteoarthritis. temperature and vasomotor symptoms in the United
962–969 (2016). Osteoarthritis Cartilage 13, 769–781 (2005). Arab Emirates. Climacteric 17, 425–432 (2014).
60. Mendelsohn, M. E. Mechanisms of estrogen action in 84. Felson, D. T. Developments in the clinical 110. Stefanopoulou, E. et al. An International menopause
the cardiovascular system. J. Steroid Biochem. Mol. understanding of osteoarthritis. Arthritis Res. Ther. society study of climate, altitude, temperature (IMS-
Biol. 74, 337–343 (2000). 11, 203 (2009). CAT) and vasomotor symptoms in urban Indian
61. Taddei, S. Blood pressure through aging and 85. Nadkar, M. Y., Samant, R. S., Vaidya, S. S. & regions. Climacteric 17, 417–424 (2014).
menopause. Climacteric 1, 36–40 (2009). Borges, N. E. Relationship between osteoarthritis of 111. Gold, E. B. et al. Longitudinal analysis of the
62. Muka, T. et al. Association of age at onset of knee and menopause. J. Assoc. Physicians India 47, association between vasomotor symptoms and race/
menopause and time since onset of menopause with 1161–1163 (1999). ethnicity across the menopausal transition: study of
cardiovascular outcomes, intermediate vascular traits, 86. Calleja-Agius, J. & Brincat, M. The effect of women’s health across the nation. Am. J. Public
and all-cause mortality. JAMA Cardiol. 1, 767–776 menopause on the skin and other connective tissues. Health 96, 1226–1235 (2006).
(2016). Gynecol. Endocrinol. 28, 273–277 (2012). 112. Hunter, M. S. et al. The International menopause
63. Parish, S. J. et al. Impact of vulvovaginal health on 87. Archer, D. F. Postmenopausal skin and estrogen. study of climate, altitude, temperature (IMS-CAT)
postmenopausal women: a review of surveys on Gynecol. Endocrinol. 28, 2–6 (2012). and vasomotor symptoms. Climacteric 16, 8–16
symptoms of vulvovaginal atrophy. Int. J. Womens 88. Grishina, I., Fenton, A. & Sankaran-Walters, S. Gender (2013).
Health 5, 437–447 (2013). differences, aging and hormonal status in mucosal 113. Schmiegelow, M. D. et al. Race and ethnicity, obesity,
64. Robinson, D. & Cardozo, L. D. The role of estrogens in injury and repair. Aging Dis. 5, 160–169 (2014). metabolic health, and risk of cardiovascular disease in
female lower urinary tract dysfunction. Urology 6, 89. Herskovitz, I. & Tosti, A. Female pattern hair loss. postmenopausal women. J. Am. Heart Assoc. 4,
45–51 (2003). Int. J. Endocrinol. Metab. 11, e986 (2013). e001695 (2015).
65. Freedman, M. A. Perceptions of dyspareunia in 90. MacPherson, K. Menopause as disease: the social 114. Wolff, E. et al. Skin wrinkles and rigidity in early
postmenopausal women with vulvar and vaginal construction of a metaphor. Adv. Nurs. Sci. 3, 95–114 postmenopausal women vary by race/ethnicity:
atrophy: findings from the REVIVE survey. Womens (1981). baseline characteristics of the skin ancillary study of
Health 10, 445–454 (2014). 91. Nusrat, N. et al. Knowledge, attitude and experience the KEEPS trial. Fertil. Steril. 95, 658–662 (2011).
66. Nappi, R. E. & Kokot-Kierepa, M. Vaginal health: of menopause. J. Ayub Med. Coll. Abbottabad 20, 115. Chua, Y. et al. Genitourinary syndrome of
insights, views and attitudes (VIVA) — results from an 56–59 (2008). menopause in five Asian countries: results from the
international survey. Climacteric 15, 36–44 (2012). 92. Opree, S. J. & Kalmijn, M. Exploring causal effects of Pan-Asian REVIVE survey. Climacteric 20, 367–373
67. Nappi, R. E., Palacios, S., Panay, N., Particco, M. & combining work and intergenerational support on (2017).
Krychman, M. L. Vulvar and vaginal atrophy in four depressive symptoms among middle-aged women. 116. Cauley, J. A., Chalhoub, D., Kassem, A. M. &
European countries: evidence from the European Ageing Soc. 32, 130–146 (2012). Fuleihan, G. E.‑H. Geographic and ethnic disparities in
REVIVE Survey. Climacteric 19, 188–197 (2016). 93. Lyons, A. C. & Griffin, C. Managing menopause: osteoporotic fractures. Nat. Rev. Endocrinol. 10,
68. Portman, D. J. & Gass, M. L. Genitourinary syndrome of a qualitative analysis of self-help literature for 338–351 (2014).
menopause: new terminology for vulvovaginal atrophy women at midlife. Soc. Sci. Med. 56, 1629–1642 117. Johnell, O., Gullberg, B., Allander, E. & Kanis, J. A.
from the International Society for the Study of Women’s (2003). The apparent incidence of hip fracture in Europe:
Sexual Health and the North American Menopause 94. Hall, L. et al. Meanings of menopause. J. Holist. Nurs. a study of national register sources. Osteoporos. Int.
Society. Menopause 21, 1063–1068 (2014). 25, 106–118 (2016). 2, 298–302 (1992).
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 15
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
118. Xia, W. B. et al. Rapidly increasing rates of hip fracture 140. Rance, N. E., Dacks, P. A., Mittelman-Smith, M. A., 162. Mannella, P., Palla, G., Bellini, M. & Simoncini, T.
in Beijing, China. J. Bone Miner. Res. 27, 125–129 Romanovsky. A. A. & Krajewski-Hall, S. J. Modulation The female pelvic floor through midlife and aging.
(2012). of body temperature and LH secretion by Maturitas 76, 230–234 (2013).
119. Freeman, E. W. & Sammel, M. D. Anxiety as a risk hypothalamic KNDy (kisspeptin, neurokinin B and 163. Randolph, J. F. Jr, Zheng, H., Avis, N. E.,
factor for menopausal hot flashes: evidence from the dynorphin) neurons: a novel hypothesis on the Greendale, G. A. & Harlow, S. D. Masturbation
penn ovarian aging cohort. Menopause 23, 942–949 mechanism of hot flushes. Front. Neuroendocrinol. frequency & sexual function domains are associated
(2016). 34, 211–227 (2013). with serum reproductive hormone levels across the
120. Vegunta, S. et al. The association between recent 141. Woods, N. F., Carr, M. C., Tao, E. Y., Taylor, H. J. & menopausal transition. J. Endocrinol. Metab 100,
abuse and menopausal symptom bother: results from Mitchell, E. S. Increased urinary cortisol levels during 258–266 (2015).
the data registry on experiences of aging, menopause, the menopausal transition. Menopause 13, 212–221 164. Woods, N. F., Mitchell, E. S. & Smith‑Di Julio, K.
and sexuality (DREAMS). Menopause 23, 494–498 (2006). Sexual desire during the menopausal transition &
(2016). 142. Gibson, C. J., Thurston, R. C. & Matthews, K. A. early postmenopause: observations from the Seattle
121. Hautamäki, H. et al. Premenstrual symptoms in fertile Cortisol dysregulation is associated with daily diary- midlife women’s health study. J. Womens Health
age are associated with impaired quality of life, but reported hot flashes among midlife women. Clin. (Larchmt) 19, 209–218 (2010).
not hot flashes, in recently postmenopausal women. Endocrinol. 85, 645–651 (2016). 165. Dennerstein, L., Lehert, P. & Burger, H. The relative
Menopause 21, 1287–1291 (2014). 143. Gordon, J. L. et al. Cardiovascular, hemodynamic, effects of hormones and relationship factors on
122. Drost, J. T., van der Schouw, Y. T., Herber-Gast, G. C. & neuroendocrine, and inflammatory markers in women sexual function of women through the natural
Maas, A. H. More vasomotor symptoms in menopause with and without vasomotor symptoms. Menopause menopausal transition. Fertil. Steril. 84, 174–180
among women with a history of hypertensive pregnancy 23, 1189–1198 (2016). (2005).
diseases compared with women with normotensive 144. Freeman, E. W. et al. Symptoms associated with 166. Janssen, I., Powell, L. H., Jasielec, M. S. &
pregnancies. Menopause 20, 1006–1011 (2013). menopausal transition and reproductive hormones in Kazlauskaite, R. Covariation of change in bioavailable
123. Thurston, R. C. et al. Adiposity and reporting of midlife women. Obstet. Gynecol. 110, 230–240 testosterone and adiposity in midlife women. Obesity
vasomotor symptoms among midlife women: the (2007). (Silver Spring) 23, 488–494 (2015).
study of women’s health across the nation. 145. Kravitz, H. M. et al. Relationship of day-today 167. Björntorp, P. Hormonal control of regional fat
Am. J. Epidemiol. 167, 78–85 (2008). reproductive hormone levels to sleep in midlife distribution. Hum. Reprod. 12, 21–25 (1997).
124. Thurston, R. C. et al. Gains in body fat and vasomotor women. Arch. Intern. Med. 165, 2370–2376 (2015). 168. Guthrie, J. R. et al. Central abdominal fat and
symptom reporting over the menopausal transition: 146. Pines, A. Circadian rhythm and menopause. endogenous hormones during the menopausal
the study of women’s health across the nation. Climacteric 19, 551–552 (2016). transition. Fertil. Steril. 79, 1335–1340 (2003).
Am. J. Epidemiol. 170, 766–774 (2009). 147. Andersen, M. L., Bittencourt, L. R., Antunes, I. B. & 169. Liu, X. M. et al. FSH regulates fat accumulation and
125. Gold, E. B. et al. Longitudinal analysis of changes in Tufik, S. Effects of progesterone on sleep: a possible redistribution in aging through the Gαi/Ca2+ pathway.
weight and waist circumference in relation to incident pharmacological treatment for sleep-breathing Aging Cell 14, 409–420 (2015).
vasomotor symptoms: the study of women’s health disorders? Curr. Med. Chem. 13, 3575–3582 170. Kalyani, R. R. et al. The association of endogenous
across the nation (SWAN). Menopause 24, 9–26 (2017). (2006). sex hormones, adiposity, and insulin resistance
126. Thurston, R. C., Chang, Y., Mancuso, P. & 148. Genazzani, A. R., Pluchino, N., Luisi, S. & Luisi, M. with incident diabetes in postmenopausal women.
Matthews, K. A. Adipokines, adiposity, and vasomotor Estrogen, cognition and female ageing. Hum. Reprod. J. Clin. Endocrinol. Metab. 94, 4127–4135
symptoms during the menopause transition: findings Update 13, 175–187 (2007). (2009).
from the study of women’s health across the nation. 149. Blair, J. A. et al. Luteinizing hormone downregulation 171. Gaspard, U. Hyperinsulinaemia, a key factor of the
Fertil. Steril. 100, 793–800 (2013). but not estrogen replacement improves ovariectomy- metabolic syndrome in postmenopausal women.
127. Pastore, L. M., Carter, R. A., Hulka, B. S. & Wells, E. associated cognition and spine density loss Maturitas 62, 362–365 (2009).
Self-reported urogenital symptoms in postmenopausal independently of treatment onset timing. Horm. 172. Leeners, B., Geary, N., Tobler, P. N. & Asarian, L.
women: women’s health initiative. Maturitas 49, Behav. 78, 60–66 (2016). Ovarian hormones and obesity. Hum. Reprod. Update.
292–303 (2004). 150. Short, R. A., Bowen, R. L., O’Brien, P. C. & 23, 300–321 (2017).
128. Waetjen, L. E. et al. Association between menopausal Graff-Radford, N. R. Elevated gonadotropin levels in 173. Maric-Bilkan, C. & Manigrasso, M. B. Sex differences
transition stages and developing urinary incontinence. patients with Alzheimer disease. Mayo Clin. Proc. 76, in hypertension: contribution of the renin-
Obstet. Gynecol. 114, 989–998 (2009). 906–909 (2001). angiotensin system. Gend. Med. 9, 287–291
129. Ensrud, K. E., Cauley, J., Lipschutz, R. & 151. Casadesus, G. et al. Evidence for the role of (2012).
Cummings, S. R. Weight change and fractures in older gonadotropin hormones in the development of 174. Simoncini, T. et al. Interaction of oestrogen receptor
women. Study of osteoporotic fractures research Alzheimer disease. Cell. Mol. Life Sci. 62, 293–298 with the regulatory subunit of
group. Arch. Intern. Med. 157, 857–863 (1997). (2005). phosphatidylinositol‑3‑OH kinase. Nature 407,
130. Crandall, C. J. et al. Postmenopausal weight change 152. Wöber, C. et al. Prospective analysis of factors related 538–541 (2000).
and incidence of fracture: post hoc findings from to migraine attacks: the PAMINA study. Cephalalgia 175. Wiik, A., Ekman, M., Johansson, O., Jansson, E. &
women’s health initiative observational study and 27, 304–314 (2007). Esbjornsson, M. Expression of both oestrogen
clinical trials. BMJ 350, h25 (2015). 153. Karkhaneh, A., Ansari, M., Emamgholipour, S. & receptor alpha and beta in human skeletal muscle
131. Looby, S. E. et al. Increased hot flash severity and Rafiee, M. H. The effect of 17β‑estradiol on gene tissue. Histochem. Cell Biol. 131, 181–189 (2009).
related interference in perimenopausal human expression of calcitonin gene-related peptide and 176. Lowe, D. A., Baltgalvis, K. A. & Greising, S. M.
immunodeficiency virus-infected women. Menopause some pro-inflammatory mediators in peripheral blood Mechanisms behind estrogen’s beneficial effect on
21, 403–409 (2014). mononuclear cells from patients with pure menstrual muscle strength in females. Exerc. Sport Sci. Rev. 38,
132. Prairie, B. A. et al. Symptoms of depressed mood, migraine. Iran. J. Basic Med. Sci. 18, 894–901 61–67 (2010).
disturbed sleep, and sexual problems in midlife (2015). 177. Fanciulli, G., Delitala, A. & Delitala, G. Growth
women: cross-sectional data from the study of 154. Schmidt, P. J. & Rubinow, D. R. Sex hormones and hormone, menopause and ageing: no definite evidence
women’s health across the nation. J. Womens Health mood in the perimenopause. Ann. NY Acad. Sci. for ‘rejuvenation’ with growth hormone. Hum. Reprod.
(Larchmt) 24, 119–126 (2015). 1179, 70–85 (2010). Update 15, 341–358 (2009).
133. Hale, G. E., Hughes, C. L., Burger, H. G., 155. Avis, N. E., Brambilla, D., McKinlay, S. M. & Vass, K. A 178. Cosma, M., Joy, B., Miles, J. M., Bowers, C. Y. &
Robertson, D. M. & Fraser, I. S. Atypical estradiol longitudinal analysis of the association between Veldhuis, J. D. Pituitary and/or peripheral estrogen-
secretion and ovulation patterns caused by luteal menopause and depression. Results from the receptor regulates follicle-stimulating hormone
out‑of‑phase (LOOP) events underlying irregular Massachusetts women’s health study. Ann. Epidemiol. secretion, whereas central estrogenic pathways direct
ovulatory menstrual cycles in the menopausal 4, 214–220 (1994). growth hormone and prolactin secretion in
transition. Menopause 16, 50–59 (2009). 156. Freeman, E. W., Sammel, M. D., Boorman, D. W. & postmenopausal women. J. Clin. Endocrinol. Metab.
134. Fogle, R. H. et al. Ovarian androgen production in Zhang, R. Longitudinal pattern of depressive 93, 951–958 (2008).
postmenopausal women. J. Clin. Endocrinol. Metab. symptoms around natural menopause. JAMA 179. Janssen, I., Heymsfield, S. B., Wang, Z. M. & Ross, R.
92, 3040–3043 (2007). Psychiatry. 71, 36–43 (2014). Skeletal muscle mass & distribution in 468 men &
135. McConnell, D. S., Stanczyk, F. Z., Sowers, M. R., 157. Gordon, J. L. et al. Ovarian hormone fluctuation, women aged 18–88 yr. J. Appl. Physiol. 89, 81–88
Randolph, J. F. & Lasley, B. L. Menopausal transition neurosteroids, and HPA axis dysregulation in (2000).
stage-specific changes in circulating adrenal perimenopausal depression: a novel heuristic model. 180. Clasey, J. L. et al. Abdominal visceral fat and fasting
androgens. Menopause 19, 658–663 (2012). Am. J. Psychiatry. 172, 227–236 (2015). insulin are important predictors of 24‑hour GH release
136. Freedman, R. R. Hot flashes: behavioral treatments, 158. Gordon, J. L., Eisenlohr-Moul, T. A., Rubinow, D. R., independent of age, gender, and other physiological
mechanisms, and relation to sleep. Am. J. Med. 118, Schrubbe, L. & Girdler, S. S. Naturally occurring factors. J. Clin. Endocrinol. Metab. 86, 3845–3852
124–130 (2005). changes in estradiol concentrations in the menopause (2001).
137. Rossmanith, W. G. & Ruebberdt, W. What causes hot transition predict morning cortisol and negative mood 181. Carville, S. F., Rutherford, O. M. & Newham, D. J.
flushes? The neuroendocrine origin of vasomotor in perimenopausal depression. Clin. Psychol. Sci. 4, Power output, isometric strength and steadiness in
symptoms in the menopause. Gynecol. Endocrinol. 919–935 (2016). the leg muscles of pre- and postmenopausal women;
25, 303–314 (2009). 159. Gordon, J. L., Rubinow, D. R., Eisenlohr-Moul, T. A., the effects of hormone replacement therapy.
138. Boulant, J. A. Role of the preoptic-anterior Leserman, J. & Girdler, S. S. Estradiol variability, Eur. J. Appl. Physiol. 96, 292–298 (2006).
hypothalamus in thermoregulation and fever. stressful life events, and the emergence of depressive 182. Cooper, R., Mishra, G., Clennell, S., Guralnik, J. &
Clin. Infect. Dis. 31, S157–S161 (2000). symptomatology during the menopausal transition. Kuh, D. Menopausal status and physical performance
139. Hale, G. E., Hitchcock, C. L., Williams, L. A., Menopause 23, 257–266 (2016). in midlife: findings from a British birth cohort study.
Vigna, Y. M. & Prior, J. C. Cyclicity of breast 160. Nappi, R. E. & Palacios, S. Impact of vulvovaginal Menopause 15, 1079–1085 (2008).
tenderness and night-time vasomotor symptoms in atrophy on sexual health and quality of life at 183. Kurina, L. M. et al. The effect of menopause on grip
mid-life women: information collected using the Daily postmenopause. Climacteric 17, 3–9 (2014). and pinch strength: results from the Chicago, Illinois,
Perimenopause Diary. Climacteric 6, 128–139 161. MacBride, M. B., Rhodes, D. J. & Shuster, L. T. Vulvo- site of the study of women’s health across the nation.
(2003). vaginal atrophy. Mayo Clin. Proc. 85, 87–94 (2010). Am. J. Epidemiol. 160, 484–491 (2004).
16 | ADVANCE ONLINE PUBLICATION www.nature.com/nrendo
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
184. Yuki, A., Ando, F., Otsuka, R. & Shimokata, H. 194. Thurston, R. C., Sutton-Tyrrell, K., Everson- 203. Ownby, R. L., Crocco, E., Acevedo, A., John, V. &
Low free testosterone is associated with loss of Rose, S. A., Hess, R. & Matthews, K. A. Hot flashes Loewenstein, D. Depression and risk for Alzheimer
appendicular muscle mass in Japanese community- and subclinical cardiovascular disease: findings from disease: systematic review, meta-analysis, and
dwelling women. Geriatr. Gerontol. Int. 15, 326–333 the study of women’s health across the nation metaregression analysis. Arch. Gen. Psychiatry 63,
(2015). heart study. Circulation 118, 1234–1240 530–538 (2006).
185. Garnero, P., Sornay‑Rendu, E., Chapuy, M. C. & (2008). 204. Terauchi, M. et al. Prevalence and predictors of
Delmas, P. D. Increased bone turnover in late 195. Thurston, R. C. et al. Changes in heart rate variability storage lower urinary tract symptoms in
postmenopausal women is a major determinant of during vasomotor symptoms among midlife women. perimenopausal and postmenopausal women
osteoporosis. J. Bone Miner. Res. 11, 337–349 Menopause 23, 499–505 (2016). attending a menopause clinic. Menopause 22,
(1996). 196. Silveira, J. S., Clapauch, R., Souza, M. D. & 1084–1090 (2015).
186. Eastell, R. et al. Postmenopausal osteoporosis. Bouskela, E. Hot flashes: emerging cardiovascular risk 205. Erekson, E. A., Li, F. Y., Martin, D. K. & Fried, T. R.
Nat. Rev. Dis. Primers. 29, 16069 (2016). factors in recent and late postmenopause and their Vulvovaginal symptoms prevalence in postmenopausal
187. Roman-Blas, J. A., Castaneda, S., Largo, R. & association with higher blood pressure. Menopause women and relationship to other menopausal
Herrero-Beaumont, G. Osteoarthritis associated with 23, 846–855 (2016). symptoms and pelvic floor disorders. Menopause 23,
estrogen deficiency. Arthritis Res. Ther. 11, 241 197. Thurston, R. C. et al. Are vasomotor symptoms 368–375 (2016).
(2009). associated with alterations in hemostatic and 206. Crandall, C. J. et al. Associations of menopausal
188. Hanna, F. S. et al. Women have increased rates of inflammatory markers? Findings from the study of vasomotor symptoms with fracture incidence. J. Clin.
cartilage loss and progression of cartilage defects at women’s health across the nation. Menopause 18, Endocrinol. Metab. 100, 524–534 (2015).
the knee than men: a gender study of adults without 1044–1051 (2011). 207. Levine, M. E. et al. Menopause accelerates biological
clinical knee osteoarthritis. Menopause 16, 666–670 198. Thurston, R. C. et al. Menopausal symptoms and aging. Proc. Natl Acad. Sci. USA 113, 9327–9332
(2009). cardiovascular disease mortality in the women’s (2016).
189. Henry, F., Piérard-Franchimont, C., Cauwenbergh, G. ischemia syndrome evaluation (WISE). Menopause 208. Harlow, S. D. et al. Executive summary of the stages of
& Piérard, G. E. Age-related changes in facial skin 24, 126–132 (2016). reproductive aging workshop +10: addressing the
contours and rheology. J. Am. Geriatr. Soc. 45, 199. Matthews, K. A. et al. Do reports of sleep unfinished agenda of staging reproductive aging.
220–222 (1997). disturbance relate to coronary and aortic calcification Fertil. Steril. 97, 843–851 (2012).
190. Piérard-Franchimont, C. & Piérard, G. E. Alterations in in healthy middle-aged women? Study of women’s
hair follicle dynamics in women. Biomed Res. health across the nation. Sleep Med. 14, 282–287 Author contributions
Int. 2013, 957432 (2013). (2013). P.M., G.M. and A.G. researched data for the article. All
191. Blume-Peytavi, U., Atkin, S., Gieler, U. & Grimalt, R. 200. Thurston, R. C. et al. Sleep characteristics and authors made a substantial contribution to discussion of con-
Skin academy: hair, skin, hormones and menopause carotid atherosclerosis among midlife women. Sleep tent, wrote the manuscript and reviewed and/or edited the
— current status/knowledge on the management of http://dx.doi.org/10.1093/sleep/zsw052 (2016). manuscript before submission.
hair disorders in menopausal women. Eur. 201. de Kruif, M., Spijker, A. T. & Molendijk, M. L.
J. Dermatol. 22, 310–318 (2012). Depression during the perimenopause: a meta- Competing interests statement
192. Price, V. Androgenic alopecia in women. J. Investig. analysis. J. Affect. Disord. 206, 174–180 (2016). The authors declare no competing interests.
Dermatol. Symp. Proc. 8, 24–27 (2003). 202. Joffe, H. et al. Independent contributions of nocturnal
193. Thurston, R. C. et al. Hot flashes and carotid intima hot flashes and sleep disturbance to depression in Publisher’s note
media thickness among midlife women. Menopause estrogen-deprived women. J. Clin. Endocrinol. Metab. Springer Nature remains neutral with regard to jurisdictional
18, 352–358 (2011). 101, 3847–3855 (2016). claims in published maps and institutional affiliations.
NATURE REVIEWS | ENDOCRINOLOGY ADVANCE ONLINE PUBLICATION | 17
©
2
0
1
8
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
Anda mungkin juga menyukai
- Medicamentos en La MENOPAUSIA (Síntomas de La Menopausia y Su Tratamiento) Santoro2015Dokumen19 halamanMedicamentos en La MENOPAUSIA (Síntomas de La Menopausia y Su Tratamiento) Santoro2015Felipe Torreblanca CoronaBelum ada peringkat
- Falla Hepatica Aguda Singanayagam2015Dokumen8 halamanFalla Hepatica Aguda Singanayagam2015Felipe Torreblanca CoronaBelum ada peringkat
- Dolor en DermatologíaDokumen21 halamanDolor en DermatologíaFelipe Torreblanca CoronaBelum ada peringkat
- Common Questions About Chronic ProstatitisDokumen7 halamanCommon Questions About Chronic ProstatitisFelipe Torreblanca CoronaBelum ada peringkat
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Parenting Assessment ToolDokumen17 halamanParenting Assessment Toolayzlim100% (2)
- Articles-Personality Process and Levels of DevelopmentDokumen16 halamanArticles-Personality Process and Levels of DevelopmentbenhazanBelum ada peringkat
- Nursing Care PlanDokumen4 halamanNursing Care PlanAlvin DagumbalBelum ada peringkat
- The Feasibility of Combined Aloe Vera Gela and Virgin Coconut Oil As Skin Revitalizer PDFDokumen62 halamanThe Feasibility of Combined Aloe Vera Gela and Virgin Coconut Oil As Skin Revitalizer PDFMiciano Renjan Browneyes75% (8)
- Advantages and Disadvantages of Local Autonomy 20160905Dokumen7 halamanAdvantages and Disadvantages of Local Autonomy 20160905grassBelum ada peringkat
- Ely Effervescent Powders PDFDokumen8 halamanEly Effervescent Powders PDFAjinBelum ada peringkat
- General Apperance: by Seid JemalDokumen44 halamanGeneral Apperance: by Seid JemalAndebet HabtamBelum ada peringkat
- Mckenzie Method: Sreeraj S RDokumen21 halamanMckenzie Method: Sreeraj S RR HariBelum ada peringkat
- UT Dallas Syllabus For nsc3361.001.08f Taught by Van Miller (vxm077000)Dokumen5 halamanUT Dallas Syllabus For nsc3361.001.08f Taught by Van Miller (vxm077000)UT Dallas Provost's Technology GroupBelum ada peringkat
- The Use of Smartphone Health Apps and Other Mobile Health (Mhealth) Technologies in Dietetic Practice - A Three Country StudyDokumen14 halamanThe Use of Smartphone Health Apps and Other Mobile Health (Mhealth) Technologies in Dietetic Practice - A Three Country StudyUmialqyBelum ada peringkat
- Eoc Risk Assessment Jci-1 PDFDokumen136 halamanEoc Risk Assessment Jci-1 PDFYulanda SeptaBelum ada peringkat
- Salvia For Dementia Therapy: Review of Pharmacological Activity and Pilot Tolerability Clinical TrialDokumen9 halamanSalvia For Dementia Therapy: Review of Pharmacological Activity and Pilot Tolerability Clinical TrialAleksa LukicBelum ada peringkat
- Eugenio (NCP and Patient Education)Dokumen6 halamanEugenio (NCP and Patient Education)Sam EugenioBelum ada peringkat
- Green Horn - Volume 31, Edition 4Dokumen24 halamanGreen Horn - Volume 31, Edition 4Springfield VT NewsBelum ada peringkat
- Mannitol Baxter Viaflo Sol F Inf ENGDokumen10 halamanMannitol Baxter Viaflo Sol F Inf ENGBojan BjelajacBelum ada peringkat
- Bayanihan To Recover As One (Bayanihan 2) BillDokumen54 halamanBayanihan To Recover As One (Bayanihan 2) BillRappler100% (6)
- Nurs 5024 - Soap - Well AdultDokumen6 halamanNurs 5024 - Soap - Well Adultapi-308904543100% (1)
- Basf Masterprotect P 659Dokumen2 halamanBasf Masterprotect P 659Hassan Ahmed SyedBelum ada peringkat
- S V Daniels 1983 3 SA 275 (A)Dokumen20 halamanS V Daniels 1983 3 SA 275 (A)Thabiso67% (3)
- NZ e 1641797811 Finish It Writing Activity Sheets - Ver - 1Dokumen4 halamanNZ e 1641797811 Finish It Writing Activity Sheets - Ver - 1Amirah AkhyarBelum ada peringkat
- Resolution 2017Dokumen2 halamanResolution 2017Thess Tecla Zerauc Azodnem90% (21)
- Benefits of Fitness Training 1. Improves Your Brain PowerDokumen39 halamanBenefits of Fitness Training 1. Improves Your Brain PowerDante Jr. BitoonBelum ada peringkat
- Research On Child Psychopathology - Research Designs, Ethical Issues - NOTESDokumen11 halamanResearch On Child Psychopathology - Research Designs, Ethical Issues - NOTESMAHIMA DASBelum ada peringkat
- Complete Guide To Endurance TrainingDokumen282 halamanComplete Guide To Endurance TrainingLynseyBelum ada peringkat
- Correcting Mold MisinformationDokumen8 halamanCorrecting Mold MisinformationhazmatlinkBelum ada peringkat
- Preview Dental AssistantDokumen62 halamanPreview Dental AssistantReihan Kaur100% (1)
- Magna Carta For Persons With DisabilityDokumen12 halamanMagna Carta For Persons With DisabilityJemarie AlamonBelum ada peringkat
- GMDSS Exam Schedule For Year 2022Dokumen7 halamanGMDSS Exam Schedule For Year 2022Mani ThapaBelum ada peringkat
- CD Rom 1 Optional Introduction SlidesDokumen3 halamanCD Rom 1 Optional Introduction SlidesTâm Nguyễn MinhBelum ada peringkat
- Environmental Determinants of Distribution of Freshwater Snails and Trematode Infection in The Omo Gibe River Basin, Southwest EthiopiaDokumen10 halamanEnvironmental Determinants of Distribution of Freshwater Snails and Trematode Infection in The Omo Gibe River Basin, Southwest Ethiopiahaymanotandualem2015Belum ada peringkat