Microscopic (Non-Visible) Haematuria: Treat As Appropriate and Retest
Diunggah oleh
Anshar NurseDeskripsi Asli:
Judul Asli
Hak Cipta
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Microscopic (Non-Visible) Haematuria: Treat As Appropriate and Retest
Diunggah oleh
Anshar NurseHak Cipta:
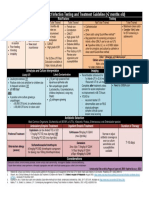
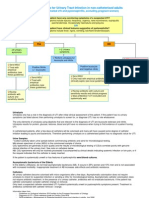
Microscopic (non-visible) haematuria
Treat as appropriate and retest
? Suspicion of UTI on dipsticks
NO UTI or clinically UTI
SEND MSU
NO ACTION REQUIRED
Significant IF high risk for urothelial cancer (SEE APPENDIX2)
(SEE APPENDIX1) Not Significant Consider: retesting urine
ultrasound (Kidney, ureters and bladder)
U&E, Creatinine, eGFR, glucose, BP
GREATER THAN LESS THAN Refer NEPHROLOGY
< 20 y.o.
50 years old 50 years old OR
YES via CHOOSE AND BOOK
• U&E, Creatinine, eGFR, glucose • U&E, Creatinine, eGFR, glucose < 30 y.o. with ≥2+ protein-
• FBC • FBC uria or abnormal renal
• PSA (male) • PSA (males) NO
function Refer UROLOGY
• Blood Pressure (SEE APPENDIX3)
via CHOOSE AND BOOK
• Blood Pressure
PLUS GP TO ARRANGE
USS (SEE APPENDIX4)
Refer via 2 WEEK WAIT
Microscopic Haematuria Clinic 20—30 years old
30—50 years old Urgent outpatient clinic
• Consultation IMAGING
Urgent haematuria appointment to discuss
• Urinalysis • > 50 yo CT Urogram +/- contrast
clinc need for further investi-
• Flexible cystoscopy • < 50 yo USS Plus IVU or CT Urogram gations
• Urine cytology (or equivalent) without contrast if micro haematuria (SEE APPENDIX6)
persistent greater than 3—6 months
Follow-up management
arranged by Urology.
All investigations normal Investigations abnormal or
further investigation required
Discharge via letter to patient and GP Follow-up advice for GP in letter
(SEE APPENDIX7)
Revision Sept 2008
APPENDIX 1
(Microscopic Haematuria)
RED BOXES Primary Care Action
GREEN BOXES Secondary Care Actions
1. Significant microscopic haematuria
Definition: The presence of non-visible haematuria on 2 out of 3 occasions in the absence of a urinary tract infection
2+ or 3+ on dipstick urinalysis has a good positive predictive value for haematuria and does not need confirming with microscopy
Trace or 1+ should be confirmed on microscopy and 10 RBC/ microlitre is regarded as significant
2. Risk Factors for Urothelial cancer
Smoking
Strong family history of bladder cancer (2 or more relatives)
Occupational exposure to carcinogens
Pelvic irradiation
Cyclophosphamide treatment
Previous schistosomiasis infection
Significant filling bladder symptoms in the absence of a urinary infection (urgency, frequency, dysuria)
3. PSA
PSA should be checked in male patients (after counselling)
i] above the age of 50 years old, with greater than 10 years life expectancy
ii] between 40—50 years old with a family history of prostate cancer or of African decent
iii] with an abnormal feeling prostate should be
4. Imaging
For patient greater than 50 years old this will be based on CT urography but may be changed to ultrasound plus IVU if CT scanning ‘slots’ are not available.
In patients < 50 years old USS will form the basis for initial investigation due to the risks associated with increased radiation exposure in a young age group.
This ultrasound should be arranged by primary care
5. Patients less than 30 years old
In patients less than 30 years old with significant microscopic haematuria the pick up rate of significant pathology is very low (< 2%). Investigation in addition
to the USS (arranged in primary care) may be required including cystoscopy. Flexible cystoscopy under local anaesthetic is poorly tolerated in this age group
and as such these patients will be seen in clinic to discuss the need for further investigations. A cystoscopy under general or local anaesthetic may be arranged
following this clinic visit.
6. Follow-up advice
If all investigations are normal the follow-up advice will be conveyed to the GP and patient via a letter. If the imaging modality was USS (i.e. in patients <50
year old) and there was no evidence of persistent microscopic haematuria for longer than 3—6 months then the GP may be asked to retest the urine at 3—6
months and if blood is still present then an IVU should be performed. If this is normal then no immediate further investigation is required.
Follow-up of patients with microscopic haematuria should include yearly urinalysis, U&E, Creatinine and eGFR and blood pressure for 3 years. Rereferral to
Urology should be made if new symptoms develop (e.g. Lower urinary tract symptoms or macroscopic haematuria) and to renal medicine if proteinuria, ab-
normal renal function or refractory hypertension develop.
Revision Sept 2008
Macroscopic (visible) haematuria
Treat as appropriate and retest
? Suspicion of UTI on dipsticks
NO UTI or clinically UTI
SEND MSU
GREATER THAN LESS THAN
30 years old 30 years old Refer via Cancer 2 WEEK 16—30 years old
• U&E, Creatinine, eGFR, glucose • U&E, Creatinine, eGFR, glucose WAIT Urgent outpatient
• FBC • FBC CANCER 2 WEEK
• PSA (male > 40 years old) • Blood Pressure WAIT slot
(SEE APPENDIX1) (SEE APPENDIX2)
• Blood Pressure
Download Fast Track Macroscopic
Haematuria Proforma from Intranet Urgent Clinic Appointment
• Consultation
• Urine cytology (or equivalent)
Refer via 2 WEEK WAIT Plan appointments for
• Imaging ?USS in first instance
• Cystoscopy (local or general anaesthetic)
Macroscopic Haematuria Clinic
• Consultation IMAGING
• Urinalysis • All patients will get urgent CT scan
• Flexible cystoscopy • (70% on the same day as the clinic ) Follow-up management
• Urine cytology (or equiva- (SEE APPENDIX3) arranged by Urology.
lent)
All investigations normal Investigations abnormal or
further investigation required
Discharge via letter to patient and GP Follow-up advice for GP in letter
(SEE APPENDIX4&5)
Revision Sept 2008
APPENDIX 2
(macroscopic ‘visible’ haematuria)
RED BOXES Primary Care Action
GREEN BOXES Secondary Care Actions
3. PSA
PSA should be checked in male patients (after counselling)
i] above the age of 50 years old, with greater than 10 years life expectancy
ii] between 40—50 years old with a family history of prostate cancer or of African decent
iii] with an abnormal feeling prostate should be
2. Patients less than 30 years old
In patients less than 30 years old with macroscopic haematuria the pick up rate of significant pathology is low (< 5%). Due to the increased radiation dose of
Ct scanning a ultrasound may be arranged as the first investigation. Furthermore as flexible cystoscopy under local anaesthetic is poorly tolerated in this age
group a discussion over the need for this investigation (advisable for most patients with painless macroscopic haematuria) will be had. A cystoscopy under
general or local anaesthetic may be arranged following this clinic visit.
3. The Fast Track Haematuria Clinic
Due to limited access to CT scanning session only 70% of patients will have their CT on the same day as their flexible cystoscopy. The remaining 30% will be
booked into an urgent CT slot within the following 2 weeks
4. Follow-up advice
If all investigations are normal (including CT scan) then the follow-up advice will be conveyed to the GP and patient via a letter. Follow-up of patients with
macroscopic haematuria should include yearly urinalysis, U&E, Creatinine and eGFR and blood pressure for 3 years. Rereferral to Urology should be made if
new symptoms develop (e.g. Lower urinary tract symptoms) or proteinuria or abnormal renal function develop.
If no cause is found in male patients over 40 years old the macroscopic haematuria may be ascribed to benign prostatic hyperplasia (a diagnosis of exclusion)
when medication (including 5 alpha reductase inhibitors) may be advised for recurrent bouts.
5. Persistent troublesome macroscopic haematuria
In some patients macroscopic haematuria persists despite negative initial investigations. In these patients further investigations may be required including renal
arteriography, retrograde ureterography, cystoscopy and biopsy and occasionally ureteroscopy. These will be arranged by secondary care
Revision Sept 2008
Anda mungkin juga menyukai
- Thyroid Encyclopedia: Encyclopedia of Thyroid Disease, Thyroid Conditions and Thyroid CancerDari EverandThyroid Encyclopedia: Encyclopedia of Thyroid Disease, Thyroid Conditions and Thyroid CancerBelum ada peringkat
- Hematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesDari EverandHematuria, (Blood in Urine) A Simple Guide to The Condition, Related Diseases And Use in Diagnosis of DiseasesPenilaian: 5 dari 5 bintang5/5 (2)
- Haematuria PathwaysDokumen4 halamanHaematuria PathwaysTressant DynarioBelum ada peringkat
- Uti Asbu Guidance FinalDokumen14 halamanUti Asbu Guidance FinalJohn Vincent Dy OcampoBelum ada peringkat
- Sirosis Hepatis Dan KomplikasiDokumen36 halamanSirosis Hepatis Dan KomplikasiMuhammad HafizdBelum ada peringkat
- Urology NotesDokumen33 halamanUrology NotesRight VentricleBelum ada peringkat
- DUB Feb24 - TaggedDokumen22 halamanDUB Feb24 - TaggedsarasamadieBelum ada peringkat
- Algorith UTI 20121218 PDFDokumen1 halamanAlgorith UTI 20121218 PDFIin fermitaBelum ada peringkat
- Abnormal Vaginal BleedingDokumen41 halamanAbnormal Vaginal BleedingAnnisa Westania DanialBelum ada peringkat
- Sirosis Hepatis Dan KomplikasiDokumen26 halamanSirosis Hepatis Dan KomplikasiTiyas UtamiBelum ada peringkat
- Sangrado Gastrointestinal OscuroDokumen20 halamanSangrado Gastrointestinal OscuroCristian Sandoval RojasBelum ada peringkat
- Hamed Alabad BPHDokumen47 halamanHamed Alabad BPHHamed AlabadBelum ada peringkat
- Prostate Cancer Clinical Pathway - July 2020Dokumen4 halamanProstate Cancer Clinical Pathway - July 2020VincentEguzoBelum ada peringkat
- Pingen, Kathleen Joy R. BSN 3ADokumen3 halamanPingen, Kathleen Joy R. BSN 3AKathleen Joy PingenBelum ada peringkat
- Dynamic Practice Guidelines For Emergency General SurgeryDokumen19 halamanDynamic Practice Guidelines For Emergency General SurgeryHarlyn MagsinoBelum ada peringkat
- Fibroids: Laparoscopy: DirectDokumen250 halamanFibroids: Laparoscopy: DirectIrish Eunice FelixBelum ada peringkat
- Abdominal Trauma Algorithm - FHADokumen53 halamanAbdominal Trauma Algorithm - FHAKevin AdrianBelum ada peringkat
- Abnormal Vaginal BleedingDokumen41 halamanAbnormal Vaginal BleedingmarkkerwinBelum ada peringkat
- Suggested Algorithm For Patients With Acute Upper .: BleedingDokumen4 halamanSuggested Algorithm For Patients With Acute Upper .: BleedingMimi Marjorie TecBelum ada peringkat
- Au Ca1-Clp - 01-Dexel Lorren R. Valdez Ob DownloadableDokumen2 halamanAu Ca1-Clp - 01-Dexel Lorren R. Valdez Ob DownloadableDexel Lorren ValdezBelum ada peringkat
- SL No Content NODokumen12 halamanSL No Content NOPdianghunBelum ada peringkat
- PrevacidDokumen1 halamanPrevacidAdrianne BazoBelum ada peringkat
- Margaret Xaira R. Mercado RNDokumen38 halamanMargaret Xaira R. Mercado RNxaira_rnBelum ada peringkat
- Peds UTIDokumen1 halamanPeds UTIMelesBelum ada peringkat
- Urinary Tract Infections in ChildrenDokumen6 halamanUrinary Tract Infections in ChildrenMarianBelum ada peringkat
- Endometrial Hyperplasia Debate 2020 FINAL PDFDokumen24 halamanEndometrial Hyperplasia Debate 2020 FINAL PDFPanitia Symposium UroginekologiBelum ada peringkat
- Benign Prostatic Hyperplasia-Gabrilia Geaby RoringDokumen19 halamanBenign Prostatic Hyperplasia-Gabrilia Geaby RoringDedylihawaBelum ada peringkat
- The Diagnosis of Prostatitis: Category I ABPDokumen4 halamanThe Diagnosis of Prostatitis: Category I ABPDaphne CelineBelum ada peringkat
- Cervical Ca CaseDokumen9 halamanCervical Ca CaseAbdullah FauziBelum ada peringkat
- Justification of Ultrasound Requests Hampshire Hospitals NHS Foundation Trust April 2022Dokumen11 halamanJustification of Ultrasound Requests Hampshire Hospitals NHS Foundation Trust April 2022eltel81Belum ada peringkat
- Guidelines of Investigations of Premenopausal Women With Abnormal Uterine Bleeding - 2020Dokumen6 halamanGuidelines of Investigations of Premenopausal Women With Abnormal Uterine Bleeding - 2020cara0319Belum ada peringkat
- Uterul Se Sectioneaza Cu Bisturiul ReceDokumen4 halamanUterul Se Sectioneaza Cu Bisturiul RecememecedarBelum ada peringkat
- Open Prostatectomy: Lab/SMF Bedah UrologiDokumen19 halamanOpen Prostatectomy: Lab/SMF Bedah Urologidevy pratiwiBelum ada peringkat
- Diagnostic Criteria For UTI in Confused PatientDokumen2 halamanDiagnostic Criteria For UTI in Confused PatientWallnut StreetBelum ada peringkat
- PDF TextDokumen2 halamanPDF TextJaiprakash GuptaBelum ada peringkat
- Guideline On Investigations of Premenopausal Women With Abnormal Uterine BleedingDokumen8 halamanGuideline On Investigations of Premenopausal Women With Abnormal Uterine Bleedingvera ditaBelum ada peringkat
- Colorectal Cancer Group 3Dokumen22 halamanColorectal Cancer Group 3JOHN DEXTER OLIVEROSBelum ada peringkat
- A2 (Comparison of Prostatic Artery Embolisation (PAE) Versus Transurethral Resection of The Prostate (TURP) For Benign Prostatic Hyperplasia Randomised, Open Label, Non-Inferiority Trial)Dokumen10 halamanA2 (Comparison of Prostatic Artery Embolisation (PAE) Versus Transurethral Resection of The Prostate (TURP) For Benign Prostatic Hyperplasia Randomised, Open Label, Non-Inferiority Trial)NadanNadhifahBelum ada peringkat
- Uti PDFDokumen1 halamanUti PDFKurouSakiBelum ada peringkat
- Pathogenesis and Management Sepsis - Aki: Fajar Yuwanto Rsud Abdul Moeloek Bandar LampungDokumen21 halamanPathogenesis and Management Sepsis - Aki: Fajar Yuwanto Rsud Abdul Moeloek Bandar LampungNodi Rahma DiniBelum ada peringkat
- Upper Gastrointestinal Bleeding: (UGIB)Dokumen39 halamanUpper Gastrointestinal Bleeding: (UGIB)api-19916399Belum ada peringkat
- AscitesDokumen4 halamanAscitesTheodoreBelum ada peringkat
- CPG Uti PDFDokumen7 halamanCPG Uti PDFhellokathyyyyyy100% (1)
- CPG Uti PDFDokumen7 halamanCPG Uti PDFhellokathyyyyyyBelum ada peringkat
- CPG Uti PDFDokumen7 halamanCPG Uti PDFhellokathyyyyyyBelum ada peringkat
- Coralie Therese D. Dimacali, MD, FPCP, FPSNDokumen48 halamanCoralie Therese D. Dimacali, MD, FPCP, FPSNJose Ph YuBelum ada peringkat
- Is Antibiotic Treatment Indicated in A Patient With A Positive Urine Culture But No SymptomsDokumen4 halamanIs Antibiotic Treatment Indicated in A Patient With A Positive Urine Culture But No Symptomstsiko111Belum ada peringkat
- Assessment Diagnosis Scientific Explanation Plan of Care Interventions Rationale EvaluationDokumen7 halamanAssessment Diagnosis Scientific Explanation Plan of Care Interventions Rationale Evaluationneil2206Belum ada peringkat
- Diagnostic Criteria For Urinary Tract InfectionDokumen2 halamanDiagnostic Criteria For Urinary Tract InfectioncandyslibioBelum ada peringkat
- Diagnostic Imaging Pathways Article PDFDokumen12 halamanDiagnostic Imaging Pathways Article PDFchald ald smithBelum ada peringkat
- ACG Clinical Guideline Upper Gastrointestinal And.14 PDFDokumen19 halamanACG Clinical Guideline Upper Gastrointestinal And.14 PDFIsrael GallardoBelum ada peringkat
- Penanganan Lesi Pra Kanker Serviks: I Nyoman Bayu MahendraDokumen76 halamanPenanganan Lesi Pra Kanker Serviks: I Nyoman Bayu MahendraHandy PutraBelum ada peringkat
- Menorraghia FINAL Bexley Pathway 3-14 v6 1Dokumen2 halamanMenorraghia FINAL Bexley Pathway 3-14 v6 1ika maulidaBelum ada peringkat
- Jaqt 06 I 1 P 30Dokumen7 halamanJaqt 06 I 1 P 30IndhumathiBelum ada peringkat
- 5-Upper Gastro-Intestinal BleedingDokumen33 halaman5-Upper Gastro-Intestinal BleedingAbdulrahman NanakaliBelum ada peringkat
- Sitologi PDFDokumen31 halamanSitologi PDFNadila Putri MaharaniBelum ada peringkat
- Philippine Clinical Practice Guidelines On The Diagnosis andDokumen83 halamanPhilippine Clinical Practice Guidelines On The Diagnosis andREnren ConsolBelum ada peringkat
- finalsURINARY ELIMINATION DIAGNOSTICSDokumen11 halamanfinalsURINARY ELIMINATION DIAGNOSTICSFrances LiqueBelum ada peringkat
- The Perfect Pancreatitis Diet Cookbook; The Complete Nutrition Guide To Managing And Healing Pancreatitis With Delectable And Nourishing Recipes;Dari EverandThe Perfect Pancreatitis Diet Cookbook; The Complete Nutrition Guide To Managing And Healing Pancreatitis With Delectable And Nourishing Recipes;Belum ada peringkat
- Top Trials in Gastroenterology & Hepatology, 2nd EditionDari EverandTop Trials in Gastroenterology & Hepatology, 2nd EditionBelum ada peringkat
- What Is A Bladder Diverticulum?Dokumen3 halamanWhat Is A Bladder Diverticulum?luckyariadneeBelum ada peringkat
- Urovaginal FistulaDokumen4 halamanUrovaginal FistulaUrology BandungBelum ada peringkat
- 011 Spesifikasi Video Camera System FHD (Set Endourology)Dokumen2 halaman011 Spesifikasi Video Camera System FHD (Set Endourology)Rizki Try AtmantiBelum ada peringkat
- Safety and Pain-Relief Efficacy of Urethral Catheter With Local-Anesthetic Injection PortDokumen5 halamanSafety and Pain-Relief Efficacy of Urethral Catheter With Local-Anesthetic Injection PortYudhi AuliaBelum ada peringkat
- Anaesthesia For UrologicDokumen62 halamanAnaesthesia For UrologicAfidah WinafBelum ada peringkat
- Urologi PDFDokumen237 halamanUrologi PDFAndi BintangBelum ada peringkat
- Practice CPC Exam - Coding Certification Tips (PDFDrive)Dokumen18 halamanPractice CPC Exam - Coding Certification Tips (PDFDrive)Sai SmaranBelum ada peringkat
- Journal 9Dokumen15 halamanJournal 9Muhammad FaisalBelum ada peringkat
- Papers 2022Dokumen6 halamanPapers 2022MDrakeBelum ada peringkat
- Surgical Strategies in Endourology For Stone DiseaseDokumen291 halamanSurgical Strategies in Endourology For Stone DiseaseHardiTariqHammaBelum ada peringkat
- Urinary RetentionDokumen11 halamanUrinary RetentionAngga PradianBelum ada peringkat
- NPT 3Dokumen8 halamanNPT 3chrizthineeBelum ada peringkat
- Vaginal FistulaDokumen14 halamanVaginal FistulaNainesh RavaliyaBelum ada peringkat
- EAU Pocket Guideline 2021Dokumen525 halamanEAU Pocket Guideline 2021Maria Angelica Rodriguez100% (1)
- Cystoscopy WordDokumen4 halamanCystoscopy WordMon ManguilinBelum ada peringkat
- Evaluation and Management of HematuriaDokumen12 halamanEvaluation and Management of HematuriaCarlos Daniel CruzBelum ada peringkat
- Bladder CancerDokumen1 halamanBladder CancerCarmina AguilarBelum ada peringkat
- Vesicovaginal FistulaDokumen6 halamanVesicovaginal FistulaMaiza TusiminBelum ada peringkat
- Genito-Urinary Fistulas: Yashar Najiaghdam M.DDokumen33 halamanGenito-Urinary Fistulas: Yashar Najiaghdam M.DyoghaBelum ada peringkat
- RZ Catalog Urology PDFDokumen75 halamanRZ Catalog Urology PDFrini setyawati50% (2)
- Prostatitis: Symptoms, Causes and TreatmentsDokumen16 halamanProstatitis: Symptoms, Causes and TreatmentsjoserodrrBelum ada peringkat
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 45Dokumen8 halamanMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 45sarasjunkBelum ada peringkat
- PDD Instrument Set Brochure 001 V1-En 20000101Dokumen16 halamanPDD Instrument Set Brochure 001 V1-En 20000101javixojdnBelum ada peringkat
- Hunner Lesion (Formerly Known As Hunner'S Ulcer)Dokumen4 halamanHunner Lesion (Formerly Known As Hunner'S Ulcer)Vasishta NadellaBelum ada peringkat
- Brad J Hornberger Cystoscopy Indications and Preparation. UAPA CME Conference 2012 (30 Min)Dokumen36 halamanBrad J Hornberger Cystoscopy Indications and Preparation. UAPA CME Conference 2012 (30 Min)Cristian OrozcoBelum ada peringkat
- Olympus Largest Business Domain: From Early Diagnosis To Minimally Invasive TherapyDokumen2 halamanOlympus Largest Business Domain: From Early Diagnosis To Minimally Invasive TherapyЭнхЗаяаBelum ada peringkat
- Pediatric TraumaDokumen5 halamanPediatric TraumaSyahdat NurkholiqBelum ada peringkat
- Feline Lower Urinary Tract Disease - 2018 Update: Zurich Open Repository and ArchiveDokumen4 halamanFeline Lower Urinary Tract Disease - 2018 Update: Zurich Open Repository and ArchiveFran RetruzBelum ada peringkat
- Assessment of Renal and Urinary Tract FunctionDokumen40 halamanAssessment of Renal and Urinary Tract FunctionBjorn Francisco100% (1)