Analgesic, Efficacy, Adverse Effects and Safety of Oxycodone Administered As Continous IV Infusion in Patient After Total Hip Arthroplasty
Diunggah oleh
gede ekaJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Analgesic, Efficacy, Adverse Effects and Safety of Oxycodone Administered As Continous IV Infusion in Patient After Total Hip Arthroplasty
Diunggah oleh
gede ekaHak Cipta:
Format Tersedia
Journal of Pain Research Dovepress
open access to scientific and medical research
Open Access Full Text Article ORIGINAL RESEARCH
Analgesic efficacy, adverse effects, and safety of
oxycodone administered as continuous intravenous
infusion in patients after total hip arthroplasty
Journal of Pain Research downloaded from https://www.dovepress.com/ by 181.215.39.115 on 30-Jul-2018
This article was published in the following Dove Press journal:
Journal of Pain Research
4 May 2017
Number of times this article has been viewed
Bogumił Olczak 1 Background: Total hip arthroplasty (THA) causes extensive tissue damage and severe pain.
Grzegorz Kowalski 1,2 This study aimed to assess the analgesic efficacy, adverse effects (AEs), and safety of continu-
Wojciech Leppert 2 ous intravenous (iv) oxycodone infusion with ketoprofen (injected into the iv line) in patients
Iwona after THA, and to assay serum oxycodone levels.
For personal use only.
Patients and methods: Fourteen patients, aged 59‒82 years with American Society of
Zaporowska-Stachowiak 3
Anesthesiologists (ASA) classification I or III, underwent THA with intrathecal analgesia and
Katarzyna
sedation induced by iv propofol. After the surgery, oxycodone (continuous iv infusion) at a
Wieczorowska-Tobis 2
dose of 1 mg/h (five patients) or 2 mg/h (nine patients) with 100 mg ketoprofen (injected into
1
Department of Anesthesiology, Józef the iv line) was administered to each patient every 12 h. Pain was assessed using a numerical
Struś Multiprofile Municipal Hospital,
2
Department of Palliative Medicine, rating scale (NRS: 0 – no pain, 10 – the most severe pain) at rest and during movement. AEs,
Poznan University of Medical Sciences, including hemodynamic unsteadiness, nausea, vomiting, pruritus, cognitive impairment, and
3
Department of Pharmacology, Poznan respiratory depression, were registered during the first 24 h after surgery.
University of Medical Sciences, Poland
Results: Oxycodone (continuous iv infusion) at a dose of 2 mg/h with ketoprofen (100 mg)
administered every 12 h provided satisfactory analgesia in all nine patients without the need
of rescue analgesics within the first 24 h after THA. In three out of five patients, oxycodone at
1 mg/h was effective. Oxycodone did not induce drowsiness, vomiting, pruritus, respiratory
depression, or changes in blood pressure. Bradycardia appeared in two patients, and nausea
was observed in one patient.
Conclusion: Oxycodone infusion with ketoprofen administered by iv is effective in patients
after THA. Intravenous infusion of oxycodone is a predictable, stable, and safe method of drug
administration.
Keywords: adverse effects, analgesia, opioid, oxycodone, pain.
Introduction
Approximately 47,000 total hip arthroplasty (THA) surgical procedures are done
annually in Poland.1 This is one of the most frequent and also one of the most burden-
some orthopedic procedures in terms of extent and number of complications. The
main indication for THA is advanced coxarthrosis, which affects both older men and
women with similar frequencies, occurs most frequently between ages 60 and 90 years,
and is a cause of severe chronic pain. Those patients often suffer from other advanced
comorbid diseases, the most frequent being hypertension, heart failure, diabetes, and
Correspondence: Wojciech Leppert
Department of Palliative Medicine, chronic obstructive pulmonary disease; therefore, the surgical procedure and period
Poznan University of Medical Sciences, of rehabilitation present significant burdens for patients. An effective perioperative
Osiedle Rusa 55, 61–245, Poland
Tel +48 61 738 000
analgesia prevents serious cardiovascular complications, decreases the number of
Email wojciechleppert@wp.pl infections, and shortens the hospitalization period. It is also a prerequisite for early
submit your manuscript | www.dovepress.com Journal of Pain Research 2017:10 1027–1032 1027
Dovepress © 2017 Olczak et al. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.
http://dx.doi.org/10.2147/JPR.S125449
php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the work
you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For
permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms (https://www.dovepress.com/terms.php).
Powered by TCPDF (www.tcpdf.org)
Olczak et al Dovepress
introduction of effective physiotherapy. In some THA studies, with oxycodone administered parenterally, although oxy-
the advantages of regional over general anesthesia have been morphone concentration is too low for significant clinical
demonstrated.2,3 However, a systematic review published in effects.15–18 Oxycodone’s plasma elimination half-life (T1/2)
2016 demonstrated a lack of sufficient evidence for regional is ~4 h, irrespective of the route of administration. Oxyco-
anesthesia advantages, although a shorter hospitalization done is excreted in the urine, mainly in the form of unbound
period was used.4 noroxycodone and oxymorphone conjugated with glucuronic
In the postoperative period, continuous epidural analgesia acid. Only about 10% of the administered oxycodone is
plays an important role. For patients with contraindications excreted unchanged in the urine.19–21
Journal of Pain Research downloaded from https://www.dovepress.com/ by 181.215.39.115 on 30-Jul-2018
or those who give no consent to this type of analgesia, an
intravenous (iv) route of analgesic administration is the main Aim of the study
method of pain treatment, especially during the first 24 h after The primary aim of the study was to assess the analgesic
the surgery. Extensive orthopedic surgery (such as knee or efficacy, AEs, and oxycodone safety administered as a con-
hip arthroplasty) involves extensive tissue damage, especially tinuous infusion with ketoprofen injected into the iv line to
of bone tissue, which in turn is associated with severe pain; patients after THA. A secondary aim was to assay serum
therefore, opioid administration is required in this patient oxycodone levels.
group. For many years, morphine has been the gold standard
of treatment for moderate-to-severe pain, although recently, Patients and methods
an interest in oxycodone for the treatment of postoperative The study protocol has been approved by the Bioethical
For personal use only.
pain has been observed. Oxycodone is used more frequently Committee of the Poznan University of Medical Sciences.
by physicians as it displays a beneficial pharmacological The study was conducted from March to November 2014 in
profile and lower percentage of adverse effects (AEs) in the Józef Struś Multiprofile Municipal Hospital in Poznan.
comparison to morphine. The studies published to date con- All patients provided written informed consent for this
firm oxycodone’s safety and high analgesic efficacy in pain study. A total of 14 patients who had undergone a total
treatment although most of the studies refer to the oral route non-cemented hip arthroplasty from a lateral access were
of administration.5–7 recruited for the study. The mean age of patients was 68±8
Oxycodone is a semisynthetic, thebaine opioid derivative, years. All patients had suffered from coxarthrosis. Several
which was synthesized for the first time in 1916 and used in tests were conducted before the surgery: 1) full blood count
1917.8 It has been widely used in the treatment of both acute and 2) determination of plasma concentrations of sodium,
and chronic pain for over 80 years. The mechanism of oxy- potassium, creatinine (for the calculation of the estimated
codone’s action is based on the activation of peripheral and glomerular filtration rate), urea, alanine aminotransferase,
central µ and κ opioid receptors. Compared with morphine, asparginate aminotransferase, total protein, and albumin. The
oxycodone displays a lower affinity to µ-opioid receptors, perioperative risk was American Society of Anesthesiologists
but it activates κ opioid receptors to a significantly larger (ASA) II in five patients and ASA III in nine patients. The
extent than morphine. In addition, its concentration in the mean height of patients was 170±6 cm, and the mean body
brain is approximately six times higher, owing to the active mass was 75±12 kg.
transport through the blood–brain barrier, which significantly Before surgery, all patients received oral midazolam
increases its analgesic efficacy.9–12 Moreover, in experimental (Dormicum tablets; Roche) at a dose of 7.5 mg. All patients
studies, a beneficial influence of oxycodone as a result of received analgesia consisting of 15 mg heavy bupivacaine
an increased expression of GABA-B receptors in sensory (Marcaine® Spinal 0.5% Heavy; AstraZeneca) via the sub-
neurons has been found. This increased expression induced arachnoid route at the L3/L4 level. In addition, sedation was
hyperalgesia inhibition in a neuropathic pain model induced induced during anesthesia by propofol injection (propofol 1%
by the cytostatic drug vincristine.13 MCT/LCT Fresenius) via the iv route at a dose of 1–3 mg/kg
Forty-five percent of oxycodone binds to serum proteins of body weight/h with oxygen therapy and maintenance of
(slightly more than morphine at 35%), and it is metabolized respiratory tract patency via the oropharyngeal airway or
through cytochrome P-450 liver enzymes to the first-order through a laryngeal mask airway, whenever necessary. After
metabolites, oxymorphone and noroxycodone.14 Only oxy- surgery, patients were transferred to a postoperative unit. If
morphone displays analgesic effects via agonist effects on no pain was present 3 h after spinal anesthesia, continuous
µ-opioid receptors, which are 14 times stronger compared infusion of oxycodone chloride (OxyNorm® ampoules;
1028 submit your manuscript | www.dovepress.com Journal of Pain Research 2017:10
Dovepress
Powered by TCPDF (www.tcpdf.org)
Dovepress Efficacy and safety of intravenous oxycodone
Mundipharma) via an iv route was started at a dose of 1 mg/h From the group of patients treated with oxycodone infu-
(n=5) or 2 mg/h (n=9). A dose of 1 mg/h was administered to sion at a dose of 1 mg/h, two patients required a single bolus
patients with a body mass <65 kg (n=5), and a dose of 2 mg/h of 2 mg oxycodone (NRS 5/6 at rest at the time of oxycodone
was given to patients whose body mass was >65 kg (n=9). All bolus administration), and the oxycodone dose in the infu-
patients in the postoperative unit received an iv ketoprofen sion was increased to 2 mg/h. Oxycodone concentration was
(100 mg) injection every 12 h. All patients were prescribed not assayed in these patients, and additional rescue doses of
a rescue dose (in the case of pain intensity over 4 according oxycodone were not required.
to a numerical rating scale [NRS]) of 2 mg of oxycodone In the rest of the analyzed group of patients, there was no
Journal of Pain Research downloaded from https://www.dovepress.com/ by 181.215.39.115 on 30-Jul-2018
administered via the iv route in the nurse-controlled analgesia need for rescue doses of oxycodone during the postoperative
system, which could be repeated every 10 min. period, both at rest and during movement. In the analyzed
Blood samples were taken for oxycodone concentration patients, oxycodone AEs such as vomiting, pruritus, cogni-
assays in blood serum (a free fraction and protein-bound) after tive impairment, respiratory depression, and blood pressure
30, 120, and 240 min after starting the drug infusion. At the changes were not observed. Bradycardia was observed in two
moment of blood sampling, patients were asked about pain patients, and one patient experienced nausea.
intensity according to NRS (0–10) at rest and during move- Mean total and protein-bound oxycodone serum concen-
ment. An NRS ≤3 at rest and an NRS ≤4 during movement (hip trations in three out of five patients receiving oxycodone at
flexion) were considered satisfactory. In the postoperative unit, a dose of 1 mg/h and mean pain intensity (NRS) at rest and
blood pressure, heart rate, blood oxygen saturation, and elec- during movement (n=3) are shown in Table 3. Mean total and
For personal use only.
trocardiogram were continuously monitored in all patients. protein-bound oxycodone concentrations in the blood serum
The number of oxycodone rescue doses was recorded, and in nine patients treated with oxycodone at a dose of 2 mg/h,
patients were also observed for the appearance of drug-related and mean pain intensity (NRS) at rest and during movement
AEs such as nausea, vomiting, pruritus, cognitive impairment are shown in Table 4.
(recognizing time, place, and appropriate responses to ques-
tions posed), and respiratory depression defined as <8 breaths/ Discussion
min with a decrease in oxygen blood saturation <90%. In this study, oxycodone, administered in a continuous infu-
sion for postoperative pain treatment in THA patients, was
Results coadministered with ketoprofen injected into the iv line every
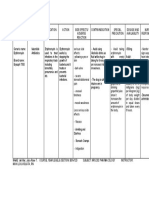
Patients’ basic demographic and clinical data are shown 12 h. Oxycodone was used at 1 and 2 mg/h depending on
in Table 1. Mean values of the laboratory parameters from patient’s body weight. In both patient groups, in consecutive
analyzed patients are demonstrated in Table 2. In all patients, observations, pain intensity was mild and did not exceed
laboratory parameters were within normal range. No factors
influencing metabolism and excretion of the selected drugs
were found (Table 2). The surgery time was 90±15 min, Table 3 Mean total and protein-bound serum oxycodone
concentrations (±SD) in patients who were treated with a dose
and the length of patients’ stay in the operation theater was
of 1 mg/h and mean pain intensity in NRS (±SD) at rest and during
150±15 min. movement (n=3)
Time (min) Total Bound NRS at NRS on
Table 1 Mean values and standard deviation of Patients’ basic of oxycodone oxycodone oxycodone rest movement
demographic and clinical data (n=14) infusion (ng/mL) (ng/mL)
Age Body weight Height ASA Surgery 30 0.49±0.20 0.18±0.06 0.3±0.6 1.7±0.6
(years) (kg) (cm) II/III duration (min) 120 6.04±2.64 5.73±0.39 2.3±0.6 3.7±0.6
68±8 75±12 170±6 5/9 90±15 240 24.37±2.86 17.32±1.14 2.3±0.6 3.3±0.6
Abbreviation: ASA, American Society of Anesthesiologists. Abbreviations: NRS, numerical rating scale; SD, standard deviation.
Table 2 Mean values and standard deviation of laboratory tests in the analyzed patients (n=14)
WBC Hb Hct (%) PLT Albumin Protein Na K (mmol/L) Creatinine Urea ALT AST
(103/µL) (mmol/L) (103/µL) (G/L) (G/L) (mmol/L) (µmol/L) (mmol/L) (U/L) (U/L)
7.06±2.13 7.55±0.93 35.8±4.6 211±83 25.1±2.7 47.5±6.1 138.7±4.2 4.28±0.47 70.9±26.4 6.81±2.87 11±7 15±11
Abbreviations: ALT, alanine transaminase; AST, aspartate transaminase; Hct, hematocryte; Hb, hemoglobin; PLT, platelets; WBC, white blood cells.
Journal of Pain Research 2017:10 submit your manuscript | www.dovepress.com
1029
Dovepress
Powered by TCPDF (www.tcpdf.org)
Olczak et al Dovepress
Table 4 Mean total and protein-bound serum oxycodone to achieve a serum drug steady state when administering
concentrations (±SD) in patients who were treated with a dose oxycodone as continuous iv infusion, another study with a
of 2 mg/h and mean pain intensity in NRS (±SD) at rest and during
longer assay period and more time points should be done.
movement (n=9)
Analgesia may be associated with serum opioid con-
Time (min) Total Bound NRS at NRS on
of oxycodone oxycodone oxycodone rest movement
centrations. In a study conducted by Kokki et al, patients
infusion ng/mL ng/mL undergoing laparoscopic cholecystectomy had oxycodone
30 0.85±0.30 0.60±0.14 0.6±0.7 1.0±1.0 concentrations equaling 20–50 ng/mL.22 In another study
120 22.68±5.90 10.00±5.69 1.1±0.9 2.7±1.0 performed among patients after cardiac surgery, oxycodone
Journal of Pain Research downloaded from https://www.dovepress.com/ by 181.215.39.115 on 30-Jul-2018
240 42.32±8.32 25.33±11.00 1.5±1.0 2.9±1.0 concentrations were in the range of 6–25 ng/mL.23 These
Abbreviations: NRS, numerical rating scale; SD, standard deviation.
observations demonstrate that oxycodone concentrations
may vary significantly depending on the doses used, time
3 (according to NRS) at rest and 4 during movement. In of blood sampling, and type of surgery. To the best of our
the group of patients treated with oxycodone at 1 mg/h, knowledge, no such data exist for orthopedic surgery. The
some patients did not require a dose increase to 2 mg/h. An data obtained in our study indicate that oxycodone con-
oxycodone dose of 2 mg/h provided all nine treated patients centrations in patients after THA may be in the range of
with satisfactory analgesic effects, which is substantiated by 24–42 ng/mL. However, a full pharmacokinetic/pharma-
the fact that no patient required administration of additional codynamic analysis of oxycodone administered after THA
doses of analgesics. The mean oxycodone concentration in surgery should be done.
For personal use only.
this patient group did not exceed 43 ng/mL of the total and The number of THA surgeries rises steadily. Patients
26 ng/mL of protein-bound oxycodone, whereas pain inten- undergoing this procedure are most frequently aged >60 years
sity did not exceed 3 (according to NRS). and apart from arthrosis, suffer from other advanced chronic
An oxycodone dose of 1 mg/h provided effective comorbidities, which require constant drug administration.
analgesia in three out of five treated patients with mean These comorbidities should thus be considered when choos-
oxycodone concentration in the three-patient group did not ing pre- and postsurgical analgesia methods, which would
exceed 25 ng/mL of the total and 18 ng/mL of protein-bound enable patients’ rapid return to normal functioning.
oxycodone. In three analyzed patients, pain intensity did not For many years, morphine has been the gold standard
exceed 4 (according to NRS). Two patients required admin- opioid for the treatment of moderate-to-severe pain. In 2009,
istration of rescue doses of 2 mg oxycodone (NRS 5/6 at the oxycodone was registered in Poland, and thus it was possible
moment of the drug administration) and a dose increase to to also start using oxycodone by the parenteral route, which
2 mg/h. Oxycodone concentrations in these patients were not had been widely used earlier in other countries mainly by the
measured. In the patient group with body weights <65 kg, oral route. Oxycodone is an opioid, which thanks to its unique
an oxycodone dose of 1 mg/h was effective only in some mode of action (affinity of µ and κ receptors, active transport
patients. A dose increase to 2 mg/h was used in cases of severe to central nervous system, and activation of the GABA sys-
pain intensity associated with extensive surgery and the fact tem) provides effective analgesia, also due to a short plasma
that bone pain usually displays severe intensity associated half-life, easy dose titration, and relatively mild AEs.
with mixed receptor and neuropathic components.12 Due to its agonist action on κ opioid receptors, oxycodone
Nausea, vomiting, bradycardia, and hypotension are is often successfully used in visceral pain treatment (such as
opioid-induced AEs. Oxycodone AEs such as vomiting, after extensive abdominal surgery), as these receptors have
pruritus, cognitive impairment, respiratory depression, and been shown to be present on nerve endings in the peritoneum
blood pressure changes were not observed. One patient expe- and dorsal horns of the spinal cord.24 The results of this study
rienced nausea, which disappeared after iv administration of demonstrated that oxycodone was also effective in postop-
ondansetron at a dose of 4 mg. Bradycardia was observed in erative pain treatment after an extensive orthopedic surgery
two patients (heart rate <45), and it also disappeared after iv during the first 24 h. The titration of an effective dose of
atropine administration at a dose of 0.5 mg. oxycodone administered by iv infusion allows a switch to
In both patient groups in the study period, serum oxyco- the oral route of or oxycodone administration that should be
done steady state was not achieved. Four hours after starting effective and safe for each patient.
oxycodone infusion, total and protein-bound drug concentra- Analgesia administered via the iv route in the early
tions were still increasing. To establish the time necessary postoperative period should provide fast pain relief, stable
1030 submit your manuscript | www.dovepress.com Journal of Pain Research 2017:10
Dovepress
Powered by TCPDF (www.tcpdf.org)
Dovepress Efficacy and safety of intravenous oxycodone
pharmacokinetics, and convenient dosing. THA is one of
most extensive orthopedic surgeries, and it is associated
References
1. Central Database of total hip arthroplasty of the National Health Fund in
with severe postoperative pain; therefore, apart from cen- Poland 2015. Available from: http://www.nfz.gov.pl/download/gfx/nfz/
pl/defaultstronaopisowa/349/30/1/cbe_za_2015.pdf. Polish. Accessed
tral and peripheral blockades, opioids from step 3 of the
October 15, 2016
World Health Organization analgesia classification are most 2. Basques BA, Toy JO, Bohl DD, Golinvaux NS, Grauer JN. General
commonly used. To limit oxycodone doses, a nonsteroidal compared with spinal anesthesia for total hip arthroplasty. J Bone Joint
Surg Am. 2015;97(6):455–461.
anti-inflammatory drug was added. In this case, ketoprofen 3. Helwani MA, Avidan MS, Ben Abdallah A, et al. Effects of regional
that possesses significant analgesic efficacy as far as bone versus general anesthesia on outcomes after total hip arthroplasty: a
Journal of Pain Research downloaded from https://www.dovepress.com/ by 181.215.39.115 on 30-Jul-2018
retrospective propensity-matched cohort study. J Bone Joint Surg Am.
pain is concerned was used. It should be noted that among
2015;97(3):186–193.
patients enrolled, no patient had been diagnosed with renal 4. Johnson RL, Kopp SL, Burkle CM, et al. Neuraxial vs general anaes-
and/or liver diseases or peptic ulcers, which would have been thesia for total hip and total knee arthroplasty: a systematic review
of comparative-effectiveness research. Br J Anaesth 2016;116(2):
contraindications to ketoprofen administration. Laboratory 163–176.
parameters were within normal range; thus, no factors that 5. Pergolizzi JV, Seow-Choen F, Wexner SD, Zampogna G, Raffa RB,
Taylor R. Perspectives on intravenous oxycodone for control of post-
would have influenced drug metabolism and excretion were
operative pain. Pain Pract. 2016;16(7):924–934.
found. In this study, opioid treatment had been started by the 6. Kokki H, Kokki M, Sjövall S. Oxycodone for the treatment of postop-
time central blockade analgesia subsided, and the patient had erative pain. Exp Opin Pharmacother 2012;13(7):1045–1058.
7. de Beer Jde V, Winemaker MJ, Donnelly GA, et al. Efficacy and safety
already recovered normal cognitive functions after propofol of controlled-release oxycodone and standard therapies for postoperative
sedation. pain after knee or hip replacement. Can J Surg. 2005;48(4):277–283.
For personal use only.
8. Falk E. Eukodal, ein neues Narkotikum. Munc Med Wochenschr.
Study limitations include lack of a control group, moder-
1917;20:381–384.
ate number of enrolled patients, short period of observation 9. Lugo RA, Kern SE. The pharmacokinetics of oxycodone. J Pain Palliat
(24 h), and limited number of serum oxycodone assays (done Care Pharmacother 2004;18(4):17–30.
10. Lalovic B, Kharasch E, Hoffer C, Risler L, Liu–Chen LY, Shen DD.
only at 4 h), which had not allowed drug steady state to be Pharmacokinetics and pharmacodynamics of oral oxycodone in healthy
reached. However, despite the aforementioned limitations, we human subjects: role of circulating active metabolites. Clin Pharmacol
Ther. 2006;79(5):461–479.
were able to demonstrate an effective analgesic effect, good
11. Boström E, Hammarlund-Udenaes M, Simonsson U. Blood–brain
profile of AEs, and safety of a combination of oxycodone barrier transport helps to explain discrepancies in vivo potency
infusion at a dose of 2 mg/h together with a bolus of 100 mg between oxycodone and morphine. Anesthesiology. 2008;108(3):
495–505.
ketoprofen administered every 12 h for severe pain intensity 12. Sacerdote P, Manfredi B, Mantegazza P, Panerai AE. Antinociceptive
treatment after THA surgery. and immunosuppressive effects of opiate drugs: a structure-related
activity study. Br J Pharmacol. 1997; 121(4): 834–838.
13. Thibault K, Calvino B, Rivals I, et al. Molecular mechanisms underly-
Conclusion ing the enhanced analgesic effect of oxycodone compared to morphine
Continuous oxycodone infusion at a dose of 2 mg/h in con- in chemotherapy-induced neuropathic pain. PLoS One. 2014;9(3):
e91297.
junction with ketoprofen (100 mg) every 12 h, both admin- 14. Leow KP, Wright AWE, Cramond T, Smith MT. Determination of the
istered via the iv route, can provide effective analgesia in serum protein binding of oxycodone and morphine using ultrafiltration.
Ther Drug Monit. 1993;15(5):440–447.
patients during the first 24 h after THA surgery. Oxycodone
15. Beaver WT, Wallenstein SL, Rogers A, Houde RW. Analgesic studies
at 1 mg/h administered as an iv infusion is effective in some of codeine and oxycodone in patients with cancer. II. Comparisons of
patients after THA. Oxycodone iv infusions at doses of 1 intramuscular oxycodone with intramuscular morphine and codeine.
J Pharmacol Exp Ther. 1978;207(1):101–108.
and 2 mg/h do not induce drowsiness, vomiting, pruritus, 16. Kaiko RF, Benziger DP, Fitzmartin RD, Burke BE, Reder RF, Gold-
respiratory depression, or blood pressure changes; however, enheim PD. Pharmacokinetic pharmacodynamic relationships of
controlled-release oxycodone. Clin Pharmacol Ther. 1996;59(1):
out of 14 treated patients, bradycardia was observed in two
52–61.
patients and nausea in one. Intravenous infusion of oxyco- 17. Pöyhiä R, Olkkola KT, Seppälä T, Kalso E. The pharmacokinetics of
done chloride in conjunction with iv ketoprofen provides oxycodone after intravenous injection in adults. Br J Clin Pharmacol.
1991;32(4):516–518.
analgesia that is effective and acceptable to patients dur- 18. Lalovic B, Phillips B, Risler LL, Howald W, Shen DD. Quantitative
ing the first 24 h after THA. Oxycodone administered as a contribution of CYP2D6 and CYP3A to oxycodone metabolism in
human liver and intestinal microsomes. Drug Metab Dispos. 2004;
continuous iv infusion is a safe pain management method in
32(4):447–454.
patients after THA. 19. Villesen HH, Banning AM, Petersen RH, et al. Pharmacokinetics of
morphine and oxycodone following intravenous administration in
elderly patients. Ther Clin Risk Manag. 2007;3(5):961–967.
Disclosure 20. Pöyhiä R, Seppälä T. Liposolubility and protein binding of oxycodone
The authors report no conflicts of interest in this work. in vitro. Pharmacol Toxicol. 1994;74(1):23–27.
Journal of Pain Research 2017:10 submit your manuscript | www.dovepress.com
1031
Dovepress
Powered by TCPDF (www.tcpdf.org)
Olczak et al Dovepress
21. Leow KP, Smith MT, Watt JA, Williams BE, Cramond T. Comparative 23. Pesonen A, Suojaranta-Ylinen R, Hammarén E, Tarkkila P, Seppälä T,
oxycodone pharmacokinetics in humans after intravenous, oral, and Rosenberg PH. Comparison of effects and plasma concentrations of
rectal administration. Ther Drug Monit. 1992;14(6):479–484. opioids between elderly and middle-aged patients after cardiac surgery.
22. Kokki M, Broms S, Eskelinen M, Rasanen I, Ojanperä I, Kokki H. Acta Anaesthesiol Scand. 2009;53(1):101–108.
Analgesic concentrations of oxycodone – a prospective clinical PK/ 24. Kalso E. Oxycodone. J Pain Symptom Manage 2005;29(5):S47–S56.
PD study in patients with laparoscopic cholecystectomy. Basic Clin
Pharmacol Toxicol. 2012;110:469–475.
Journal of Pain Research downloaded from https://www.dovepress.com/ by 181.215.39.115 on 30-Jul-2018
For personal use only.
Journal of Pain Research Dovepress
Publish your work in this journal
The Journal of Pain Research is an international, peer reviewed, open The manuscript management system is completely online and includes
access, online journal that welcomes laboratory and clinical findings a very quick and fair peer-review system, which is all easy to use. Visit
in the fields of pain research and the prevention and management http://www.dovepress.com/testimonials.php to read real quotes from
of pain. Original research, reviews, symposium reports, hypoth- published authors.
esis formation and commentaries are all considered for publication.
Submit your manuscript here: https://www.dovepress.com/journal-of-pain-research-journal
1032 submit your manuscript | www.dovepress.com Journal of Pain Research 2017:10
Dovepress
Powered by TCPDF (www.tcpdf.org)
Anda mungkin juga menyukai
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5795)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- Drug InteractionsDokumen21 halamanDrug InteractionsPawan Deshmukh100% (1)
- Drug Education Definition of Terms: Acute ToleranceDokumen6 halamanDrug Education Definition of Terms: Acute ToleranceAldrin CrutoBelum ada peringkat
- AHFS CategoriesDokumen12 halamanAHFS CategoriesEidetikosBelum ada peringkat
- Directorate General of Drug Administration: SL Name of The Pharmaceutical Address Location Licence No. Present StatusDokumen2 halamanDirectorate General of Drug Administration: SL Name of The Pharmaceutical Address Location Licence No. Present StatusAnamika SahaBelum ada peringkat
- Hospital Pharmacy Survey Tool PDFDokumen4 halamanHospital Pharmacy Survey Tool PDFEliana GerzonBelum ada peringkat
- Behavioral Psychosis in DementiaDokumen62 halamanBehavioral Psychosis in DementiaAlexander NavarraBelum ada peringkat
- Calculation of Doses - General ConsiderationsDokumen30 halamanCalculation of Doses - General Considerationsalibel caballeroBelum ada peringkat
- (INTERN 1) Internship ReflectionDokumen2 halaman(INTERN 1) Internship ReflectionSebastian MoronBelum ada peringkat
- Biliary Tract Cancers: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Dokumen96 halamanBiliary Tract Cancers: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Sabbir RaihanBelum ada peringkat
- A Comparison of Handwritten-1Dokumen3 halamanA Comparison of Handwritten-1Muzahidul IslamBelum ada peringkat
- Chapter Wise QuestionsDokumen6 halamanChapter Wise QuestionsDr. B. Sree Giri Prasad100% (2)
- UntitledDokumen5 halamanUntitledClinton MandelaBelum ada peringkat
- Cholesterol Drugs ComparedDokumen3 halamanCholesterol Drugs ComparedHeriberto MazaBelum ada peringkat
- CPR Guideline 2022Dokumen12 halamanCPR Guideline 2022Wyndham WooBelum ada peringkat
- Asas Pertolongan CemasDokumen25 halamanAsas Pertolongan CemasCarthy TangBelum ada peringkat
- Prefix, Suffix of DrugsDokumen6 halamanPrefix, Suffix of DrugsBriel Jake CabusasBelum ada peringkat
- SOLID ORAL MODIFIED RELEASE LectureDokumen13 halamanSOLID ORAL MODIFIED RELEASE LectureMa Rodelyn VivarBelum ada peringkat
- Case Scenario:: 6. Make A Pain and Comforting Cycle For Your Patient Using This Diagram: See The Diagram in Your ModuleDokumen1 halamanCase Scenario:: 6. Make A Pain and Comforting Cycle For Your Patient Using This Diagram: See The Diagram in Your ModulewokorowBelum ada peringkat
- Mechanisms of Drug Interactions: Pharmacodynamics and PharmacokineticsDokumen4 halamanMechanisms of Drug Interactions: Pharmacodynamics and Pharmacokineticsgowepa9266Belum ada peringkat
- Stok Opname Format Baru BPKDokumen6 halamanStok Opname Format Baru BPKLilly Hoo LeeBelum ada peringkat
- Kpi Aa Ip 2023Dokumen10 halamanKpi Aa Ip 2023Poppy FitraBelum ada peringkat
- Eye Drugs ComparisonDokumen444 halamanEye Drugs ComparisonEster GracesillyaBelum ada peringkat
- RKODokumen10 halamanRKOressamahendraBelum ada peringkat
- Drug Study AssignmentDokumen1 halamanDrug Study AssignmentDaniela Claire FranciscoBelum ada peringkat
- Swisderm DrugsDokumen4 halamanSwisderm DrugsJuliet EtingeBelum ada peringkat
- Mcqs 12Dokumen18 halamanMcqs 12Muhammad JavedBelum ada peringkat
- Alevo Alkem (Ulticare) (Levofloxacin) : Strength Presentation PriceDokumen21 halamanAlevo Alkem (Ulticare) (Levofloxacin) : Strength Presentation Pricepathan mohidBelum ada peringkat
- Reference Guide For Pharmacy Technician Exam: Manan ShroffDokumen50 halamanReference Guide For Pharmacy Technician Exam: Manan ShroffAira Gene Meneses100% (2)
- Emergency TreatmentDokumen5 halamanEmergency TreatmentAdina IqbalBelum ada peringkat
- Pharmacology - The Drug Development ProcessDokumen3 halamanPharmacology - The Drug Development ProcessCamilogsBelum ada peringkat