Case Study (Asthma)
Diunggah oleh
AIMJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Case Study (Asthma)
Diunggah oleh
AIMHak Cipta:
Format Tersedia
CASE STUDY
(ASTHMA)
Submitted by:
Tyrone Marc B. Asuncion
John Clements D. Galiza
Jannica Rei T. Guillermo
Angelic I. Mateo
Mary Ellayne A. Oducayen
Group 2 BSN IV-A, Cluster 1
Submitted to:
Mr. Jayflor L. Ronquillo
Clinical Instructor
Rona Marie T. Bergonia
Student Head Nurse
March 29, 2019
CASE STUDY: ASTHMA
Patient Profile
E.S. is a 35 y/o mother of two school-age boys who arrives via ambulance in the
emergency department (ED) with severe wheezing, dyspnea, and anxiety. She was in
the ED 6 hours earlier with an asthma attack.
Subjective Data
Treated during previous ED visit with nebulized albuterol and responded quickly
Allergic to cigarette smoke
Began to experience increasing tightness in her chest and shortness of breath when
she returned home following her previous ED visit
Used the albuterol several times after she returned home with no relief
Diagnosed with asthma 2 years ago
Does not have a health care provider and is not on any medications
Objective Data
Physical Examination
Sitting upright and using accessory muscles to breathe
Talks in one-to-three-word sentences
RR: 34 and shallow
Audible wheezing
Auscultation of lung fields reveals no air movement in lower lobes
HR: 126 bpm
Noted to be extremely anxious and restless
Diagnostic Studies
ABGs: pH 7.46, PaCO2 36 mmHg, PaO2 76 mmHg, O2 saturation 88%
Chest x-ray: bilateral lung hyperinflation with lower lobe atelectasis
CBC with differential and electrolytes: within normal limits
An IV is started in her left forearm with normal saline infusing at 100 ml/hr
Questions and Answers:
1. What other assessment information should be obtained from E.S.?
The other information needed to be assessed and obtained are:
Diaphoresis, increased anteroposterior thoracic diameter,
hyperresonance, and visual disturbance.
2. Priority decision: What is the priority collaborative intervention for E.S.?
Pulmonary Function studies including response to bronchodilator therapy.
The priority intervention is administering O2 since the patient’s RR is 34.
Dyspnea and using accessory muscles with an oxygen saturation of 88%.
3. What data obtained from the brief history, physical examination, and diagnostic
studies indicate that E.S. is experiencing a severe or life-threatening asthma
attack?
“Talks in 1 to 3 word sentences”. According to Mohamedali (2018), having
the inability to speak is one of the life threatening features of asthma.
4. Identify two classifications of medications the nurse should expect to be
administered to this patient. What effect is expected with these medications?
a. Short-acting beta2 Adrenergic Drugs: For bronchodilation
Long-acting beta2 adrenergic Drugs: To manage symptoms day to day
and keep airways open.
b. Leukotriene Modulators: To reduce local inflammatory response in
lungs and to reduce exacerbation.
5. In addition to medication administration and close monitoring of the patient, what
other key role can the nurse take in helping the patient through this episode?
The other key role that a nurse can be in helping the patient is being a
Nurse educator. Since the patient was not on any medication and does not have
a health care provider, the nurse should educate the patient about the
importance of regular check-ups to avoid complications and to improve health
condition. In addition, the nurse must also:
a. Monitor respiration; patient’s respiratory status can continue to
deteriorate; look at respiratory rate, effort, use of accessory muscle,
skin color, breath sound.
b. Place the patient in high fowler’s position to ease respiration
c. Monitor v/s, look for changes in BP, if there is tachycardia or
tachypnea.
d. Give patient 3L of fluid per day to help liquify any secretions.
e. Administer supplemental oxygen to help meet body’s needs.
6. What value would peak expiratory flow rate (PEFR) measures have during the
care of E.S.?
Yellow zone: This means “Caution” (50-80%) since the patient manifests
mild symptoms such as feeling tired, shortness of breath and increased
tightness of the chest.
7. Priority Decision: Based on the assessment data presented, what are the
priority nursing diagnoses? What are the collaborative problems?
Explain the use of a peak flow meter
Encourage to do pursed-lip and diaphragmatic breathing.
Instructed to do coughing and deep breathing exercises
Instructed to drink water at least 3L/day
Instructed to avoid known allergies/dust
Encouraged adequate rest periods
Teach about the importance of using mask.
Instruct family to avoid burning waste.
Anda mungkin juga menyukai
- Management of Tuberculosis: A guide for clinicians (eBook edition)Dari EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Belum ada peringkat
- Case Analysis Bronchial AsthmaDokumen21 halamanCase Analysis Bronchial AsthmaKim LladaBelum ada peringkat
- Bronchial Asthma in AEDokumen14 halamanBronchial Asthma in AECharmie Lou Dadivas CelestialBelum ada peringkat
- Bronchial AsthmaDokumen3 halamanBronchial AsthmaSabrina Reyes0% (1)
- Dermatomyositis NCPDokumen3 halamanDermatomyositis NCPMakki MarcosBelum ada peringkat
- ER Treatment for Asthmatic PatientDokumen4 halamanER Treatment for Asthmatic PatientEver Green100% (2)
- Case Study On AsthmaDokumen8 halamanCase Study On AsthmaDoff Cruz100% (1)
- Bronchial Asthma: Islamic University Nursing CollegeDokumen27 halamanBronchial Asthma: Islamic University Nursing CollegeRenuka SivaramBelum ada peringkat
- Case Presentation 3 DR Oscar Laryngitis TBDokumen33 halamanCase Presentation 3 DR Oscar Laryngitis TBmarajuu50% (2)
- Case Study (Bronchial Asthma)Dokumen11 halamanCase Study (Bronchial Asthma)DhanNie Cenita50% (2)
- Case Presentation - Acute Otits MediaDokumen31 halamanCase Presentation - Acute Otits MediaJean nicole Garibay0% (1)
- Case Study On AsthmaDokumen21 halamanCase Study On AsthmaJerome Vergara75% (4)
- Case Study of Bronchial Asthma in Acute ExacerbationDokumen19 halamanCase Study of Bronchial Asthma in Acute ExacerbationEzra Dizon ManzanoBelum ada peringkat
- Asthma (Case Study 6)Dokumen14 halamanAsthma (Case Study 6)Mylz MendozaBelum ada peringkat
- Community Health Assessment Form 1Dokumen4 halamanCommunity Health Assessment Form 1Vrent Mica SilotBelum ada peringkat
- Pneumonia Case Presentation on Respiratory Alkalosis (39Dokumen20 halamanPneumonia Case Presentation on Respiratory Alkalosis (39Camille Honeyleith Lanuza Fernando80% (5)
- Case Summary of Patient With Chronic Obstructive PulmonaryDokumen27 halamanCase Summary of Patient With Chronic Obstructive PulmonaryUzair Muhd0% (1)
- Case Study TBDokumen9 halamanCase Study TBCheche_Guinto_8235100% (2)
- Understanding Bronchial AsthmaDokumen25 halamanUnderstanding Bronchial AsthmaRio Jane AsimanBelum ada peringkat
- I Can'T Breathe If Breathing Is Without: Bronchial AsthmaDokumen33 halamanI Can'T Breathe If Breathing Is Without: Bronchial AsthmaklamorenaBelum ada peringkat
- Iloilo Doctors' College Case Study on PneumoniaDokumen38 halamanIloilo Doctors' College Case Study on PneumoniaLuna JadeBelum ada peringkat
- Case Study 1 - PneumoniaDokumen14 halamanCase Study 1 - PneumoniaJilkiah Mae Alfoja CampomanesBelum ada peringkat
- Administration of OxygenDokumen52 halamanAdministration of OxygenSivabarathy50% (2)
- INTUSSUSCEPTIONDokumen43 halamanINTUSSUSCEPTIONValarmathi100% (3)
- Case Management of Ari at PHC LevelDokumen29 halamanCase Management of Ari at PHC Levelapi-3823785Belum ada peringkat
- Nursing Care Plans of Bronchial AsthmaDokumen8 halamanNursing Care Plans of Bronchial AsthmaKannanBelum ada peringkat
- Bronchial Asthma in Acute Exacerbation - FinalDokumen17 halamanBronchial Asthma in Acute Exacerbation - Finalmary_sulit_150% (2)
- ConjunctivitisDokumen16 halamanConjunctivitisClark LopezBelum ada peringkat
- COPD Case Presentation on Exacerbation ManagementDokumen16 halamanCOPD Case Presentation on Exacerbation ManagementSafoora RafeeqBelum ada peringkat
- Case Study On Pulmonary TuberculosisDokumen12 halamanCase Study On Pulmonary TuberculosisKirstie Claire100% (1)
- BRONCHIAL ASTHMA Case Presentation. EditedDokumen37 halamanBRONCHIAL ASTHMA Case Presentation. Edited92006770% (10)
- Case Study Sa Surgical WardDokumen8 halamanCase Study Sa Surgical WardAiza ToledanaBelum ada peringkat
- Case PresentationDokumen30 halamanCase PresentationMenard Tobias VelascoBelum ada peringkat
- Nursing Care for Acute Pancreatitis PatientDokumen54 halamanNursing Care for Acute Pancreatitis PatientMark Norriel Cajandab100% (1)
- Pneumonia Anatomy and PhysiologyDokumen2 halamanPneumonia Anatomy and PhysiologyIanaCarandang50% (4)
- Tuberculosis (The Disease)Dokumen24 halamanTuberculosis (The Disease)DiLahBelum ada peringkat
- Status Asthmaticus Case StudyDokumen18 halamanStatus Asthmaticus Case Studygeorgeloto12Belum ada peringkat
- Case Study PneumoniaDokumen12 halamanCase Study PneumoniaFretzie Mae RamasBelum ada peringkat
- A Case Study of Bronchial Asthma in Acute Exacerbation (Baiae)Dokumen13 halamanA Case Study of Bronchial Asthma in Acute Exacerbation (Baiae)Samantha BolanteBelum ada peringkat
- A Descriptive Study To Assess The Knowledge Regarding Substance Abuse and Ill Effects Among P.U. Students in The Selected P.U. College of BagalkotDokumen3 halamanA Descriptive Study To Assess The Knowledge Regarding Substance Abuse and Ill Effects Among P.U. Students in The Selected P.U. College of BagalkotInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- 02 Bronchial Asthma Circ 2018-2019Dokumen15 halaman02 Bronchial Asthma Circ 2018-2019Mooha Alanzy100% (1)
- Clinical Presentation on TonsillectomyDokumen46 halamanClinical Presentation on TonsillectomySREEDEVI T SURESH100% (1)
- Case Study PneumoniaDokumen8 halamanCase Study PneumoniaThesa FedericoBelum ada peringkat
- Ceftriaxone IM Drug StudyDokumen5 halamanCeftriaxone IM Drug StudyCastillo MikaellaBelum ada peringkat
- Caring for TB Patients Using Orem's TheoryDokumen13 halamanCaring for TB Patients Using Orem's TheoryRazel Kinette AzotesBelum ada peringkat
- Diabetes Case Presentation Liver AbscessDokumen26 halamanDiabetes Case Presentation Liver AbscessGarima Kamboj Mirok100% (1)
- Iloilo Doctors' College Nursing Care Plan for Anaphylactic ShockDokumen7 halamanIloilo Doctors' College Nursing Care Plan for Anaphylactic ShockAbie Jean BalbontinBelum ada peringkat
- Case Study of BronchoPneumoniaDokumen64 halamanCase Study of BronchoPneumoniaJomari Zapanta100% (2)
- MSN II 01.7.2020-OSCE in Instillation of Ear DropsDokumen3 halamanMSN II 01.7.2020-OSCE in Instillation of Ear DropsYAMINIPRIYANBelum ada peringkat
- Jaundice Case StudyDokumen5 halamanJaundice Case StudyUday KumarBelum ada peringkat
- Case Presentation About Hypertension Stage 2-BeluanDokumen36 halamanCase Presentation About Hypertension Stage 2-BeluanKeepItSecretBelum ada peringkat
- Theories and Models in Community Health NursingDokumen38 halamanTheories and Models in Community Health NursingSujatha J Jayabal80% (5)
- A Case Study On Bronchial Asthma in Acute ExacerbationDokumen71 halamanA Case Study On Bronchial Asthma in Acute ExacerbationATEHAN BORDSBelum ada peringkat
- Class 2 Lesson PlanDokumen16 halamanClass 2 Lesson PlanArjun Neupane100% (1)
- Care Plan On: Submitted To: Submitted byDokumen38 halamanCare Plan On: Submitted To: Submitted byMoonBelum ada peringkat
- Medical Diagnosis: Bronchial Asthma Impaired Gas ExchangeDokumen2 halamanMedical Diagnosis: Bronchial Asthma Impaired Gas ExchangeAndrea Chua BuadoBelum ada peringkat
- Tuberculosis Case StudyDokumen43 halamanTuberculosis Case StudyAJIgama100% (1)
- Case Study (Asthma)Dokumen3 halamanCase Study (Asthma)AIM100% (1)
- GRPB CaseStudyASthmaDokumen3 halamanGRPB CaseStudyASthmaCherry Ann BalagotBelum ada peringkat
- Session 5Dokumen3 halamanSession 5Sistine Rose Labajo100% (1)
- Case Study (Asthma)Dokumen3 halamanCase Study (Asthma)AIM100% (1)
- MCHDokumen13 halamanMCHEhmzy Olimar JacintoBelum ada peringkat
- 160 Nursing Bullets Med SurgDokumen7 halaman160 Nursing Bullets Med SurgHailMarieSBarcenasBelum ada peringkat
- 225 Nursing Bullets - Psychiatric NursingDokumen11 halaman225 Nursing Bullets - Psychiatric Nursingdecsag06Belum ada peringkat
- 220 Nursing BulletsDokumen14 halaman220 Nursing Bulletsggrrk7Belum ada peringkat
- I. Patterns of Functioning and Levels of Competencies: AnalysisDokumen5 halamanI. Patterns of Functioning and Levels of Competencies: AnalysisAIMBelum ada peringkat
- Changes in eating, drinking, bladder and bowel patternsDokumen62 halamanChanges in eating, drinking, bladder and bowel patternsAIMBelum ada peringkat
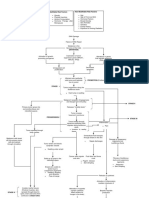
- Modifiable Risk Factors Non-Modifiable Risk Factors: Iv. Schematic DiagramDokumen3 halamanModifiable Risk Factors Non-Modifiable Risk Factors: Iv. Schematic DiagramAIMBelum ada peringkat
- Med MNGTDokumen7 halamanMed MNGTAIMBelum ada peringkat
- Cardiac MonitoringDokumen6 halamanCardiac MonitoringAIMBelum ada peringkat
- Case Diabetic KetoacidosisDokumen32 halamanCase Diabetic KetoacidosisAIMBelum ada peringkat
- Developmental and PatternsDokumen17 halamanDevelopmental and PatternsAIMBelum ada peringkat
- Brochure Breast Self ExamDokumen2 halamanBrochure Breast Self ExamAIMBelum ada peringkat
- Final ABCDokumen90 halamanFinal ABCAIMBelum ada peringkat
- MODIFIABLE RISK FACTORS OF CANCER More CompleteDokumen1 halamanMODIFIABLE RISK FACTORS OF CANCER More CompleteAIMBelum ada peringkat
- Everything You Need to Know About BPHDokumen3 halamanEverything You Need to Know About BPHAIMBelum ada peringkat
- Pulmonary Tuberculosis: Mycobacterium Tuberculosis Which Is A Gram-Positive, Acid-Fast Aerobic Bacillus and CanDokumen15 halamanPulmonary Tuberculosis: Mycobacterium Tuberculosis Which Is A Gram-Positive, Acid-Fast Aerobic Bacillus and CanAIMBelum ada peringkat
- Pulmonary Tuberculosis: Mycobacterium Tuberculosis Which Is A Gram-Positive, Acid-Fast Aerobic Bacillus and CanDokumen15 halamanPulmonary Tuberculosis: Mycobacterium Tuberculosis Which Is A Gram-Positive, Acid-Fast Aerobic Bacillus and CanAIMBelum ada peringkat
- PHE Complete Immunisation Schedule Jun2020 05Dokumen2 halamanPHE Complete Immunisation Schedule Jun2020 05GAnnBelum ada peringkat
- 1903 Pediatric Acute Icu: Anthony - Lee@Utsouthwestern - EduDokumen4 halaman1903 Pediatric Acute Icu: Anthony - Lee@Utsouthwestern - EdurupaliBelum ada peringkat
- Clinical Oncology PaperDokumen20 halamanClinical Oncology Paperapi-633111194Belum ada peringkat
- Telaah Kritis Artikel Terapi PZ 2020Dokumen7 halamanTelaah Kritis Artikel Terapi PZ 2020dewi arifahniBelum ada peringkat
- HSS International PDI Form - February 2023Dokumen2 halamanHSS International PDI Form - February 2023wyzxy2793Belum ada peringkat
- DSM-5 and Neurocognitive DisordersDokumen6 halamanDSM-5 and Neurocognitive DisordersluishelBelum ada peringkat
- SKIN, HAIR, and NAILSDokumen17 halamanSKIN, HAIR, and NAILSkhalidBelum ada peringkat
- DK Critical Appraisal EBM HarmDokumen17 halamanDK Critical Appraisal EBM HarmJoanita KurniadiBelum ada peringkat
- PART I: Vocabulary (20 Items - 4,0 Pts - 0,2 PTS/ Item) Questions 1-5Dokumen5 halamanPART I: Vocabulary (20 Items - 4,0 Pts - 0,2 PTS/ Item) Questions 1-5Nguyễn TavirelBelum ada peringkat
- Lesson 1 Height and WeightDokumen20 halamanLesson 1 Height and Weightglaidz100% (1)
- Prop Ae771263af039nwpDokumen4 halamanProp Ae771263af039nwpPenielle SaguindanBelum ada peringkat
- NCP BronchopneumoniaDokumen8 halamanNCP BronchopneumoniaCrisantaCasliBelum ada peringkat
- Triage and assessment of multiple trauma patientsDokumen5 halamanTriage and assessment of multiple trauma patientsChristabel EdithBelum ada peringkat
- Valadi - Guillain-Barré SyndromeDokumen5 halamanValadi - Guillain-Barré SyndromeMarcelo BedoyaBelum ada peringkat
- GOCABR ProtocolDokumen5 halamanGOCABR Protocolnunuk wijayantiBelum ada peringkat
- Nasal Obstruction: Nitha K 2nd Year MSC NursingDokumen65 halamanNasal Obstruction: Nitha K 2nd Year MSC NursingNITHA KBelum ada peringkat
- Laporan-Diagnosa DesemberDokumen421 halamanLaporan-Diagnosa DesemberPutri Annisa0% (1)
- Acute Isolated MyocarditisDokumen20 halamanAcute Isolated Myocarditismerin sunilBelum ada peringkat
- ROLE OF A MICROBIOLOGIST IN PREVENTION OF HEALTHCARE-ASSOCIATED INFECTIONS - v3Dokumen12 halamanROLE OF A MICROBIOLOGIST IN PREVENTION OF HEALTHCARE-ASSOCIATED INFECTIONS - v3vijayasree bavireddyBelum ada peringkat
- 18 Cellular AberrationsDokumen70 halaman18 Cellular AberrationsBea Bianca CruzBelum ada peringkat
- Salmonella in The CaribbeanDokumen3 halamanSalmonella in The CaribbeanAlvin KiruiBelum ada peringkat
- International Journal of Women's DermatologyDokumen5 halamanInternational Journal of Women's DermatologySbomBelum ada peringkat
- Covid-19 PCR Test ReportDokumen1 halamanCovid-19 PCR Test ReportPriyank MardaBelum ada peringkat
- M&M Hypovolemic ShockDokumen30 halamanM&M Hypovolemic ShockRyan FornollesBelum ada peringkat
- Gallstones: Causes, Complications and Treatment OptionsDokumen6 halamanGallstones: Causes, Complications and Treatment Optionsricky aditBelum ada peringkat
- Angliski SeminarskaDokumen13 halamanAngliski SeminarskaMarija AleksovaBelum ada peringkat
- Gulf Pain School Webinar Series II - Program - 0Dokumen5 halamanGulf Pain School Webinar Series II - Program - 0NIKOLAOS SYRMOSBelum ada peringkat
- COPD AE (Book) (20210118) (林冠霖)Dokumen15 halamanCOPD AE (Book) (20210118) (林冠霖)林冠霖Belum ada peringkat
- Microbial Food CantaminationDokumen39 halamanMicrobial Food CantaminationPrashant ItankarBelum ada peringkat
- Coronary Artery Disease-Cad OR Ischaemic Heart Disease - IhdDokumen99 halamanCoronary Artery Disease-Cad OR Ischaemic Heart Disease - IhdMwanja MosesBelum ada peringkat
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDari EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionPenilaian: 4 dari 5 bintang4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (13)
- The Comfort of Crows: A Backyard YearDari EverandThe Comfort of Crows: A Backyard YearPenilaian: 4.5 dari 5 bintang4.5/5 (23)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDari EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDari EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityPenilaian: 3.5 dari 5 bintang3.5/5 (2)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 5 dari 5 bintang5/5 (78)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBelum ada peringkat
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDari EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsPenilaian: 5 dari 5 bintang5/5 (1)
- Techniques Exercises And Tricks For Memory ImprovementDari EverandTechniques Exercises And Tricks For Memory ImprovementPenilaian: 4.5 dari 5 bintang4.5/5 (40)
- The Obesity Code: Unlocking the Secrets of Weight LossDari EverandThe Obesity Code: Unlocking the Secrets of Weight LossPenilaian: 5 dari 5 bintang5/5 (4)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDari EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisPenilaian: 4 dari 5 bintang4/5 (1)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDari EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisPenilaian: 5 dari 5 bintang5/5 (8)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDari EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsPenilaian: 4.5 dari 5 bintang4.5/5 (169)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDari EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingPenilaian: 3.5 dari 5 bintang3.5/5 (33)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDari EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsBelum ada peringkat
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingDari EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingPenilaian: 5 dari 5 bintang5/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Dari EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Penilaian: 4.5 dari 5 bintang4.5/5 (110)
- The Ultimate Guide To Memory Improvement TechniquesDari EverandThe Ultimate Guide To Memory Improvement TechniquesPenilaian: 5 dari 5 bintang5/5 (34)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDari EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDari EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifePenilaian: 4.5 dari 5 bintang4.5/5 (253)
- The Happiness Trap: How to Stop Struggling and Start LivingDari EverandThe Happiness Trap: How to Stop Struggling and Start LivingPenilaian: 4 dari 5 bintang4/5 (1)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsDari EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsBelum ada peringkat
- Recovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyDari EverandRecovering from Emotionally Immature Parents: Practical Tools to Establish Boundaries and Reclaim Your Emotional AutonomyPenilaian: 4.5 dari 5 bintang4.5/5 (201)
- The Tennis Partner: A Doctor's Story of Friendship and LossDari EverandThe Tennis Partner: A Doctor's Story of Friendship and LossPenilaian: 4.5 dari 5 bintang4.5/5 (4)