NCP - Pulmonary Tuberculosis
Diunggah oleh
astriju0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
389 tayangan6 halamanJudul Asli
NCP- Pulmonary Tuberculosis.docx
Hak Cipta
© © All Rights Reserved
Format Tersedia
DOCX, PDF, TXT atau baca online dari Scribd
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
0 penilaian0% menganggap dokumen ini bermanfaat (0 suara)
389 tayangan6 halamanNCP - Pulmonary Tuberculosis
Diunggah oleh
astrijuHak Cipta:
© All Rights Reserved
Format Tersedia
Unduh sebagai DOCX, PDF, TXT atau baca online dari Scribd
Anda di halaman 1dari 6
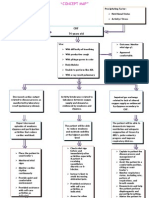
Nursing diagnosis: Ineffective airway clearance
NOC: Respiratory Status: Airway Patency
1. Maintain patent airway
2. Expectorate secretions without assistance.
3. Demonstrate behaviors to improve or maintain airway clearance.
4. Participate in treatment regimen, within the level of ability and situation.
5. Identify potential complications and initiate appropriate actions.
NIC: Airway Management
Independent:
1. Assess respiratory function, such as breath sounds, rate, rhythm, and depth, and use of
accessory muscles.
2. Note ability to expectorate mucus and cough effectively; document character and amount of
sputum and presence of hemoptysis.
3. Place client in semi- or high-Fowler’s position. Assist client with coughing and deep-breathing
exercises.
4. Clear secretions from mouth and trachea; suction as necessary.
5. Maintain fluid intake of at least 2500 mL/day unless contraindicated.
Collaborative
1. Humidify inspired oxygen.
2. administer medications, as indicated, for example: Mucolytic agents, such as acetylcysteine
(Mucomyst)
3. Bronchodilators, such as oxtriphylline (Choledyl) and theophylline (Theo-Dur)
4. Corticosteroids (prednisone)
5. Be prepared for and assist with emergency intubation.
Nursing diagnosis: Risk for impaired gas exchange
NOC: Respiratory status: Gas exchange
1. Report absence of or decreased dyspnea.
2. Demonstrate improved ventilation and adequate oxygenation of tissues by ABGs within
acceptable ranges.
3. Be free of symptoms of respiratory distress.
NIC: Respiratory Monitoring
Independent
1. Assess for dyspnea (using 0 to 10 [or similar] scale), tachypnea, abnormal breath sounds,
increased respiratory effort, limited chest wall expansion, and fatigue.
2. Evaluate change in level of mentation.
3. Note cyanosis or change in skin color, including mucous membranes and nailbeds.
4. Demonstrate and encourage pursed-lip breathing during exhalation, especially for clients with
fibrosis or parenchy- mal destruction.
5. Promote bedrest, or limit activity and assist with self-care activities as necessary.
Collaborative
1. Monitor serial ABGs and pulse oximetry.
2. Provide supplemental oxygen as appropriate.
Nursing diagnosis: Risk for Infection (spread/ reactivation)
NOC: Risk control: Infectious Process
1. Identify interventions to prevent or reduce risk of spread of infection.
2. Demonstrate techniques and initiate lifestyle changes to promote safe environment.
NIC: Infection Control
Independent
1. Review pathology of disease—active or inactive phases, dissemination of infection through
bronchi to adjacent tissues or via bloodstream and lymphatic system—and potential spread of
infection via airborne droplet during coughing, sneezing, spitting, talking, laughing, and
singing.
2. Identify others at risk, such as household members, close associates, and friends.
3. Instruct client to cough, sneeze, and expectorate into tissue and to refrain from spitting.
Review proper disposal of tissue and good hand-washing techniques. Request return
demonstration.
4. Review necessity of infection control measures, such as temporary respiratory isolation.
5. Monitor temperature, as indicated.
6. Identify individual risk factors for reactivation of tuberculosis, such as lowered resistance
associated with alcoholism, malnutrition, intestinal bypass surgery, use of immunosup-
pressant drugs, presence of diabetes mellitus or cancer, or postpartum.
7. Emphasize importance of uninterrupted drug therapy. Evaluate client’s potential for
cooperation.
8. Review importance of follow-up and periodic reculturing of sputum for the duration of
therapy.
9. Encourage selection and ingestion of well-balanced meals. Provide frequent small “snacks”
in place of large meals as appropriate.
Collaborative
1. Administer anti-infective agents, as indicated, for example:
2. Primary drugs: isoniazid (INH, Liniazid), rifampin (RIF, Rifadin, Rimactane), pyrazinamide
(PZA, Tebrazid), and ethambutol (Etbi, Myambutol) rufabutin (Mucobutin)
3. Investigational agents such as diarylquinoline (R207910)
4. Monitor laboratory studies, such as the following: Sputum smear results
5. Liver function studies, such as aspartate aminotransferase (AST), alinine aminotransferase
(ALT)
6. Notify local health department.
Nursing diagnosis: Imbalanced Nutrition: Less than body requirements
NOC: Nutritional status
Demonstrate progressive weight gain toward goal with normalization of laboratory values and
be free of signs of malnutrition. Initiate behaviors or lifestyle changes to regain and to maintain
appropriate weight.
NIC: Nutrition Management
Independent
1. Document client’s nutritional status on admission, noting skin turgor, current weight and
degree of weight loss, integrity of oral mucosa, ability to swallow, presence of bowel tones,
and history of nausea, vomiting, or diarrhea.
2. Ascertain client’s usual dietary pattern and likes and dislikes.
3. Monitor intake and output (I&O) and weight periodically.
4. Investigate anorexia, nausea, and vomiting. Note possible correlation to medications. Monitor
frequency, volume, and consistency of stools.
5. Encourage and provide for frequent rest periods. Provide oral care before and after respiratory
treatments.
6. Encourage small, frequent meals with foods high in protein and carbohydrates.
7. Encourage SO to bring foods from home and to share meals with client unless contraindicated.
Collaborative
1. Refer to dietitian/nutritionist for adjustments in dietary composition.
2. Consult with respiratory therapy to schedule treatments 1 to 2 hours before or after meals.
3. Monitor laboratory studies, such as blood urea nitrogen (BUN), serum protein, and prealbumin
and albumin.
4. Administer antipyretics, as appropriate.
Nursing diagnosis: Risk for ineffective Self-Health Management
NOC: Self Management: Chronic Disease
1. Verbalize understanding of disease process, prognosis, and prevention.
2. Initiate behaviors or lifestyle changes to improve general well-being and reduce risk of
reactivation of TB.
3. Identify symptoms requiring evaluation and intervention
4. Describe a plan for receiving adequate follow-up care.
5. Verbalize understanding of therapeutic regimen and rationale for actions.
NIC: Learning Facilitation
Independent
1. Assess client’s ability to learn, such as level of fear, concern, fatigue, participation level; best
environment in which client can learn; how much content the client can learn; best media and
language to teach the client; and determine who should be included.
2. Provide instruction and specific written information for client to refer to, such as schedule for
medications and follow-up sputum testing for documenting response to therapy.
3. Encourage client and SO to verbalize fears and concerns. Answer questions factually. Note
prolonged use of denial.
NIC: Teaching : Disesase Process
1. Identify symptoms that should be reported to healthcare provider, such as hemoptysis, chest
pain, fever, difficulty breathing, hearing loss, and vertigo.
2. Emphasize the importance of maintaining high-protein and carbohydrate diet and adequate
fluid intake. (Refer to ND: imbalanced Nutrition: less than body requirements.)
3. Explain medication dosage, frequency of administration, expected action, and the reason for
long treatment period. Review potential interactions with other drugs and substances.
Emphasize reportable side effects.
4. Review potential side effects of treatment, such as dry mouth, gastrointestinal (GI) upset,
constipation, visual disturbances, headache, and orthostatic hypertension, and problem-solve
solutions.
5. Emphasize need to abstain from alcohol while on INH.
6. Refer for eye examination after starting and then monthly during the course of ethambutol
(EMB).
7. Encourage abstaining from smoking.
8. Review that TB is transmitted primarily by inhalation of airborne organisms but may also
spread through stools or urine if infection is present in these organ systems; also review
hazards of reactivation.
9. Discuss and reinforce concerns, such as treatment failure, drug-resistant TB, and relapse.
10. Refer to public health agency as appropriate.
Referensi:
Doenges, Marilyn., Moorhouse, Mary F., & Murr, Alice C. 2014. Nursing Care Plan:
Guidelines for Individualizing Client Care Across the Life Span 9th Edition. USA: F.A. Davis
Company
Anda mungkin juga menyukai
- DP For Acute Respiratory FailureDokumen1 halamanDP For Acute Respiratory FailurePauline SalgadoBelum ada peringkat
- Case Scenarios 5Dokumen4 halamanCase Scenarios 5Bianca Mae0% (3)
- Word Ncp.......... TetanusDokumen6 halamanWord Ncp.......... TetanusaianrBelum ada peringkat
- Ineffective Airway ClearanceDokumen9 halamanIneffective Airway ClearanceFatiha Sri Utami TamadBelum ada peringkat
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDokumen3 halamanSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaBelum ada peringkat
- NCP BMDokumen1 halamanNCP BMSourabh MehraBelum ada peringkat
- NCPDokumen8 halamanNCPJoseph Anthony Benitez VerzosaBelum ada peringkat
- CP Intestinal Obstruction Nursing Care PlanDokumen7 halamanCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaBelum ada peringkat
- NURSING CARE PLAN For TB 2003Dokumen6 halamanNURSING CARE PLAN For TB 2003Princess Andrea Bulatao100% (1)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentDokumen4 halamanAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Short Term Goal: IndependentNinaBelum ada peringkat
- Nursing Care PlanDokumen20 halamanNursing Care PlanZamranosBelum ada peringkat
- NCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPDokumen2 halamanNCP Ineffective Airway Clearance Related To Presence of Secretion in Trachea-Bronchial Tree Secondary To History of CAPpa3kmedina100% (1)
- NCP 2 and Soapie 1Dokumen5 halamanNCP 2 and Soapie 1narsD100% (1)
- Nursing Care Plan: Pulmonary EbolismDokumen5 halamanNursing Care Plan: Pulmonary EbolismneuronurseBelum ada peringkat
- NCPDokumen2 halamanNCPShubhangi SarwanBelum ada peringkat
- NCP PTBDokumen6 halamanNCP PTBJay Dela VegaBelum ada peringkat
- ISBAR DocumentationDokumen1 halamanISBAR DocumentationFrancorussBelum ada peringkat
- NCP Copd4Dokumen15 halamanNCP Copd4Alessa Marie Crisostomo Salazar100% (1)
- 1 Ineffective Breathing PatternDokumen8 halaman1 Ineffective Breathing PatternNoel MontemayorBelum ada peringkat
- Angel Therisse B. Ramelb BSN Ii-C Nursing DiagnosisDokumen2 halamanAngel Therisse B. Ramelb BSN Ii-C Nursing DiagnosisSalvaje CaballeroBelum ada peringkat
- ANATOMY AND PHYSIOLOGY of RabiesDokumen5 halamanANATOMY AND PHYSIOLOGY of RabiesDavid CalaloBelum ada peringkat
- Pulmonary HypertensionDokumen10 halamanPulmonary HypertensionqingwenBelum ada peringkat
- Hyperthermia and Risk For AspirationDokumen3 halamanHyperthermia and Risk For AspirationAlmyr RimandoBelum ada peringkat
- Nursing Measures To Maintain Normal Respiratory Function and OxygenationDokumen2 halamanNursing Measures To Maintain Normal Respiratory Function and Oxygenationlodeth100% (2)
- NCPDokumen4 halamanNCPAndrea BroccoliBelum ada peringkat
- 6 Pleural Effusion Nursing Care PlansDokumen7 halaman6 Pleural Effusion Nursing Care PlansShaina Fe RabaneraBelum ada peringkat
- Nursing Care Plan For Inflammatory Bowel DiseaseDokumen17 halamanNursing Care Plan For Inflammatory Bowel DiseaseLyka Joy DavilaBelum ada peringkat
- 7 Hyperthyroidism Nursing Care Plan (NCP)Dokumen1 halaman7 Hyperthyroidism Nursing Care Plan (NCP)Apol PenBelum ada peringkat
- Nursing Care PlanDokumen14 halamanNursing Care PlanVin Landicho100% (1)
- Concept Map - Abby !Dokumen2 halamanConcept Map - Abby !Abegail Abaygar100% (3)
- ASTHMADokumen9 halamanASTHMAmildred alidonBelum ada peringkat
- Ncp-Impaired S.i.-NavidasDokumen4 halamanNcp-Impaired S.i.-NavidasFran LanBelum ada peringkat
- PoliomyelitisDokumen14 halamanPoliomyelitisEzekiel Reyes100% (1)
- Nursing Care Plan For Breast Cancer NCP PDFDokumen2 halamanNursing Care Plan For Breast Cancer NCP PDFMaina BarmanBelum ada peringkat
- CholecystitisDokumen1 halamanCholecystitisDianne ParungaoBelum ada peringkat
- Word Ncp.......... TetanusDokumen3 halamanWord Ncp.......... TetanusYvounne Ananias Bautista RNBelum ada peringkat
- Nursing Care PlanDokumen5 halamanNursing Care PlanPaola Marie VenusBelum ada peringkat
- PYOMYOSITISDokumen12 halamanPYOMYOSITISPaolo VillaBelum ada peringkat
- Impaired Verbal CommunicationDokumen6 halamanImpaired Verbal CommunicationLaura Sansonetti100% (1)
- Baiae NCPDokumen1 halamanBaiae NCPreignyfayeBelum ada peringkat
- Simple Schematic Diagram of PneumoniaDokumen1 halamanSimple Schematic Diagram of PneumoniaJason A. AdoyoganBelum ada peringkat
- NCA2 PosttestsDokumen20 halamanNCA2 PosttestsCzarena Ysabelle PayotBelum ada peringkat
- NCP AidsDokumen16 halamanNCP AidstferdianingsihBelum ada peringkat
- Cerebrovascular Accident (CVA) N C P BY BHERU LALDokumen1 halamanCerebrovascular Accident (CVA) N C P BY BHERU LALBheru LalBelum ada peringkat
- Nursing Management of AmoebiasisDokumen2 halamanNursing Management of Amoebiasisjiedysy100% (1)
- NCPDokumen4 halamanNCPyasayayasay yasayBelum ada peringkat
- NCP For SVTDokumen6 halamanNCP For SVTRen VillenaBelum ada peringkat
- Case PresentationDokumen5 halamanCase PresentationJARIETTA OCHOABelum ada peringkat
- Assessment Diagnosis Planning Intervention Rationale EvaluationDokumen1 halamanAssessment Diagnosis Planning Intervention Rationale EvaluationAira AlaroBelum ada peringkat
- Hypertension Nursing Care PlanDokumen3 halamanHypertension Nursing Care PlanAsylla PajijiBelum ada peringkat
- NCP For CTTDokumen1 halamanNCP For CTTJen Rhae LimBelum ada peringkat
- NCP For StokeDokumen5 halamanNCP For StokeMemedBelum ada peringkat
- Decreased Cardiac OutputDokumen3 halamanDecreased Cardiac OutputRizalyn QuindipanBelum ada peringkat
- NCP For Mi PainDokumen2 halamanNCP For Mi PainKahMallariBelum ada peringkat
- Nursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleDokumen8 halamanNursing Care Plan 1: Diagnosis Goal Nursing Interventions RationaleTrysna Ayu SukardiBelum ada peringkat
- Cardiovascular Drug ProjectDokumen3 halamanCardiovascular Drug ProjectHannaBelum ada peringkat
- Lung Cancer (Nursing Care)Dokumen5 halamanLung Cancer (Nursing Care)heiyuBelum ada peringkat
- Caring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyDokumen34 halamanCaring For Children Receiving Chemotherapy, Antimicrobial Therapy and Long-Term Insulin TherapyRubinaBelum ada peringkat
- Revised NCP (Baiae)Dokumen9 halamanRevised NCP (Baiae)Jennifer BactatBelum ada peringkat
- ReportDokumen4 halamanReportKyle DapulagBelum ada peringkat
- Fu Ling PresentationDokumen14 halamanFu Ling PresentationChristine BattenBelum ada peringkat
- DentalDokumen42 halamanDentalmahesardarBelum ada peringkat
- 2 Week Body Weight Boot CampDokumen28 halaman2 Week Body Weight Boot Camptano47Belum ada peringkat
- BMR Energy RequirementsDokumen9 halamanBMR Energy RequirementsRahul ThakranBelum ada peringkat
- BinGO HAWKS Score Card FillableDokumen1 halamanBinGO HAWKS Score Card FillableEmily AirhartBelum ada peringkat
- The Effect of A Nutrition Education ModuleDokumen58 halamanThe Effect of A Nutrition Education ModuleUli Kartika Sihaloho100% (1)
- Pe 111 Module PreliminaryDokumen90 halamanPe 111 Module PreliminaryEzra JungBelum ada peringkat
- Sports Nutrition Course Manual FinalDokumen98 halamanSports Nutrition Course Manual FinalZAX TIPSBelum ada peringkat
- NCP For Case StudyDokumen5 halamanNCP For Case StudySean Carl TubilBelum ada peringkat
- Buenger Resume 20201213Dokumen2 halamanBuenger Resume 20201213api-514993360Belum ada peringkat
- Vitamin A, EDokumen32 halamanVitamin A, EDakshitha DharmakeerthiBelum ada peringkat
- This Is An Edited Version of J&T2.0, If You Have Questions See The Write UpDokumen42 halamanThis Is An Edited Version of J&T2.0, If You Have Questions See The Write Upjuangar1992100% (1)
- Children 10 00695Dokumen16 halamanChildren 10 00695BBD BBDBelum ada peringkat
- Food Irradiation Q and ADokumen15 halamanFood Irradiation Q and AAshish SharmaBelum ada peringkat
- Step 3 Dieting - Exercises and QuizzesDokumen7 halamanStep 3 Dieting - Exercises and Quizzeshuynvnd711Belum ada peringkat
- LE8 How To Manage Blood PressureDokumen1 halamanLE8 How To Manage Blood PressureStephanie Mae RadamBelum ada peringkat
- Final Exams - NUTRI EXAM FINALSDokumen27 halamanFinal Exams - NUTRI EXAM FINALSJana Patricia JalovaBelum ada peringkat
- Polyethylene Glycols (Pegs) : Sheftel, Vo. Indirect Food Additives and PolymersDokumen6 halamanPolyethylene Glycols (Pegs) : Sheftel, Vo. Indirect Food Additives and PolymersJeff HeardBelum ada peringkat
- Midterm NDT Notes FinalDokumen28 halamanMidterm NDT Notes FinalSL GuillenaBelum ada peringkat
- Genocide? Abuse? Assaults? Live Journal From Vavuniya, Sri LankaDokumen4 halamanGenocide? Abuse? Assaults? Live Journal From Vavuniya, Sri LankaBailamanBelum ada peringkat
- CerealBoxProject 1Dokumen2 halamanCerealBoxProject 1Allison LawsonBelum ada peringkat
- Quantitative Analysis of 22 NMN Consumer Products Oct 2021Dokumen5 halamanQuantitative Analysis of 22 NMN Consumer Products Oct 2021Stanford LeeBelum ada peringkat
- Lesson 03 - Talking About Regrets: ObjetivosDokumen12 halamanLesson 03 - Talking About Regrets: Objetivosaleusp2009Belum ada peringkat
- Eating Non-Vegetarian Food RevisedDokumen3 halamanEating Non-Vegetarian Food RevisedKhaled Ahmed El SheriefBelum ada peringkat
- Different Way of Food PreservationDokumen22 halamanDifferent Way of Food PreservationMarynaire GallardoBelum ada peringkat
- The Premature BabyDokumen92 halamanThe Premature BabyTrishenth Fonseka100% (1)
- Holistic Health QuestionnaireDokumen28 halamanHolistic Health QuestionnaireMichael Grant WhiteBelum ada peringkat
- (International Studies Intensives) Kimberly A. Weir - From Jicama To Jackfruit - The Global Political Economy of Food (2014, Routledge)Dokumen223 halaman(International Studies Intensives) Kimberly A. Weir - From Jicama To Jackfruit - The Global Political Economy of Food (2014, Routledge)nipun namboodiriBelum ada peringkat
- Artificial Sweeteners: January 2019Dokumen10 halamanArtificial Sweeteners: January 2019siyengar1447Belum ada peringkat
- Digestive System TestDokumen7 halamanDigestive System Testapi-571616928Belum ada peringkat