Continuous Positive Airway Pressure Cpap in Neonatal Units
Diunggah oleh
nadhifa akHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Continuous Positive Airway Pressure Cpap in Neonatal Units
Diunggah oleh
nadhifa akHak Cipta:
Format Tersedia
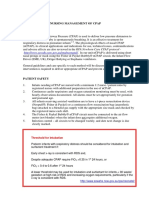
Continuous Positive Airway Pressure (CPAP) in Neonatal Units
CPAP was first used CPAP is mostly used for respiratory support in infants with COIN trial1 616
in 1971 Its use has respiratory distress syndrome/apnoea and after extubation in infants 25-28 wks
increased steadily infants with RDS gest randomised to
over the last 20 CPAP or intubation.
years. 58% CPAP infants
subsequently needed
It is now the Action: 1. Splints the upper airway & reduces intubation.
mainstay of obstructive apnoea 2. Prevents alveolar Pneumothorax rate
ventilatory support collapse 3. Reduces respiratory rate via 9% in CPAP & 3% in
for preterm infants. Herring Breuer deflation reflex intubated group. No
difference in death or
Consider extubation BPD.
of the ventilated
infant to CPAP if Administration: Infant Flow Driver (I.F.D.) SUPPORT trial2 1316
PCO2<8.6 kPa, infants 24-27 wks
pH>7.2, FiO2<50%, gest. randomised to
rate<20. CPAP or intubation.
Clinical Indications: For infants ≤ 26 wks gest. 34%CPAP infants
Infants on CPAP intubation & surfactant should be considered. subsequently needed
without Surfactant For infants 26-30 weeks gest. initial management ventilation.
administration are at should be CPAP unless intubation is needed for Pneumothorax rate
increased risk of resuscitation in which case give surfactant. 7% in both groups.
Pneumothorax 6-9%. Start Caffeine medication.
Be aware of this If infant >30 weeks gest. commence CPAP if there CPAP after
complication and are signs of RDS. Extubation- Cochrane
undertake trans- CPAP should be administered after extubation in review3 of 9 studies
illumination and who have had RDS. found that the use of
chest x-ray if the CPAP significantly
infant has any clinical reduced the need for
or blood gas reintubation (NNT 6).
deterioration. How to use CPAP: Apply nasal CPAP using
A nasal mask or short binasal prongs. Nasal mask is associated Trial of nasal prongs
Nasal prongs cause With a lower rate of subsequent intubation v nasal masks
nasal trauma in 7% Start PEEP 5 cms increasing to 8 cms if necessary showed5 masks had
of infants. Intubate if Apnoec, pH < 7.2, PCO2 >9 kPa, FiO2>40% a lower intubation
rate prongs
52%mask 28%5
NIPPV (Neonatal Nasal Intermittent Pos. Press. Ventilation)
Mostly in infants after extubation for RDS4. The optimal
settings are uncertain. Use PEEP 3-5 cms & PIP 8-15 cms,
rate 30/min
Paediatrics and Neonatology Clinical Programme Algorithms
References:
1. Morley CJ, Davis PG, Doyle LW. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med 2008;358:700-8
2. Finer N, Carlo W, Walsh M et al. Early CPAP versus surfactant in extremely preterm infants. SUPPORT study group. N Engl J Med
2010;362:1970-9
3. Davis PG, Henderson-Smart DJ. Nasal continuous positive airway pressure immediately after extubation for preventing morbidity in preterm
infants. Cochrane database of systematic reviews 2003, issue 2 Art No: CD 000143
4. Owen LS, Morley C, Davis PG. Neonatal nasal intermittent positive pressure ventilation: what do we know in 2007? Arch Dis Child
2007;92:F414-8
5. Kirplani H, Millar D, Lemyre B, Yoder BA , Twomey A et al. A trial comparing noninvasive ventilation strategies in preterm infants. N Engl J
Med 2013;369:611-20
6. Kieran EA, Twomey AR, Molloy EJ, MurphyJF, O’Donnell CP. Randomised trial of prongs or mask for CPAP in preterm infants. Pediatr
2012;130:1170-6
This care pathway has been produced by the National Paediatric and Neonatology Clinical Programme. It is aimed at medical, nursing and
allied health professionals working in Irish neonatal units.
Algorithm number: N7 Document drafted by: National Paediatric and Neonatology Clinical Programme
Revision number: 1.0 Document Status: Approved
Date of Last Update: 20/12/13 Document approved by: Paediatric and Neonatology Clinical Programme Working Group
Neonatal Clinical Advisory Group
Approval date: 13/01/14 Revision date: January 2016
Anda mungkin juga menyukai
- RPA Guidelines Continuous Positive Airway PressureDokumen10 halamanRPA Guidelines Continuous Positive Airway PressureHalima TahariBelum ada peringkat
- GIZZI 2012_Surfactant and non invasive ventilation for preterm infantsDokumen4 halamanGIZZI 2012_Surfactant and non invasive ventilation for preterm infantsRafael JustinoBelum ada peringkat
- POLIN 2009_Bubble CPAP- A Clash of Science Culture and ReligionDokumen2 halamanPOLIN 2009_Bubble CPAP- A Clash of Science Culture and ReligionRafael JustinoBelum ada peringkat
- Vladimiras Chijenas - NRS in Newborn InfantsDokumen31 halamanVladimiras Chijenas - NRS in Newborn InfantsFausiah Ulva MBelum ada peringkat
- Bubble CPAP Effectiveness Preterm Neonates RDSDokumen4 halamanBubble CPAP Effectiveness Preterm Neonates RDSJulyan ValenzaBelum ada peringkat
- Practical Application of CPAP: Dr. Srinivas MurkiDokumen8 halamanPractical Application of CPAP: Dr. Srinivas MurkiRaji MohanBelum ada peringkat
- Nasal IMV - Gatot PDFDokumen43 halamanNasal IMV - Gatot PDFtutiarlyBelum ada peringkat
- The Use of Bubble CPAP in Premature InfantsDokumen7 halamanThe Use of Bubble CPAP in Premature InfantsRyan Rahman OesmanBelum ada peringkat
- Cummings 2015Dokumen11 halamanCummings 2015MaluBelum ada peringkat
- 10 1016@j Jpeds 2020 10 045Dokumen24 halaman10 1016@j Jpeds 2020 10 045YasintaUnusBelum ada peringkat
- Non Invasive HFO Time For Consideration 2017Dokumen3 halamanNon Invasive HFO Time For Consideration 2017OsmanyBelum ada peringkat
- PICKERD 2014_idal Breathing in Preterm Infants Receiving and Weaning From Continuous Positive Airway PressureDokumen7 halamanPICKERD 2014_idal Breathing in Preterm Infants Receiving and Weaning From Continuous Positive Airway PressureRafael JustinoBelum ada peringkat
- Jurnal Pubme 1 RdsDokumen13 halamanJurnal Pubme 1 Rdsriri risna aBelum ada peringkat
- Nasalintermittentpositive Pressureventilationfor Neonatalrespiratorydistress SyndromeDokumen20 halamanNasalintermittentpositive Pressureventilationfor Neonatalrespiratorydistress SyndromeBella FebriantiBelum ada peringkat
- nCPAP ManagementDokumen11 halamannCPAP ManagementMon Russel FriasBelum ada peringkat
- Pediatr Pulmonol 2018 53 10 1422-1428Dokumen7 halamanPediatr Pulmonol 2018 53 10 1422-1428baltazarottonelloBelum ada peringkat
- 484400Dokumen7 halaman484400MaluBelum ada peringkat
- Journal ClubDokumen39 halamanJournal Clubgpediatrics myBelum ada peringkat
- Pedia ClerkshipDokumen4 halamanPedia Clerkshipmarjorie_eyesBelum ada peringkat
- Surfactant ReplacementDokumen40 halamanSurfactant ReplacementDr.Sushree Smita BehuraBelum ada peringkat
- The Effect of Extended Continuous Positive Airway Pressure on Lung VolumesDokumen15 halamanThe Effect of Extended Continuous Positive Airway Pressure on Lung Volumesblufire78Belum ada peringkat
- gupta2016 CPAP-physiology and comparioson of devicesDokumen8 halamangupta2016 CPAP-physiology and comparioson of devicesRafael JustinoBelum ada peringkat
- Cpap Science PhysiologyDokumen6 halamanCpap Science PhysiologyIuthisam HassanBelum ada peringkat
- Non-Invasive Respiratory Support in Preterm Infants 2022Dokumen7 halamanNon-Invasive Respiratory Support in Preterm Infants 2022DraalexBelum ada peringkat
- 25 - Glackin2016Dokumen4 halaman25 - Glackin2016Rosa PerezBelum ada peringkat
- CPAP ManualDokumen43 halamanCPAP ManualTachira Julher RiveraBelum ada peringkat
- DANI 2012_Surfactant replacement in preterm infants with RDSDokumen4 halamanDANI 2012_Surfactant replacement in preterm infants with RDSRafael JustinoBelum ada peringkat
- Kawaza: Low Cost Bubble CPAP For Managing Neonatal Respiratory Distress in MalawiDokumen31 halamanKawaza: Low Cost Bubble CPAP For Managing Neonatal Respiratory Distress in MalawiNewborn2013Belum ada peringkat
- CPAP Machines: DR - Ashok DeorariDokumen6 halamanCPAP Machines: DR - Ashok DeorariAC19UBM035 SOWMIYA.PBelum ada peringkat
- Fisiologia de Semin - Fetal - Neon - Med - 2016 - Jun - 21 (3) - 174Dokumen7 halamanFisiologia de Semin - Fetal - Neon - Med - 2016 - Jun - 21 (3) - 174MASIEL AMELIA BARRANTES ARCEBelum ada peringkat
- Journal Homepage: - : Manuscript HistoryDokumen5 halamanJournal Homepage: - : Manuscript HistoryIJAR JOURNALBelum ada peringkat
- Bubble nasal CPAP manual provides background and theoryDokumen43 halamanBubble nasal CPAP manual provides background and theorymecadineBelum ada peringkat
- Non Invasive Respiratory Support in Preterm I - 2022 - Paediatric Respiratory ReDokumen7 halamanNon Invasive Respiratory Support in Preterm I - 2022 - Paediatric Respiratory ReEduardo Rios DuboisBelum ada peringkat
- GUPTA 2009_A RCT of post extubation BCPAP versus infant flow driver CPAP in preterm infants with RDSDokumen8 halamanGUPTA 2009_A RCT of post extubation BCPAP versus infant flow driver CPAP in preterm infants with RDSRafael JustinoBelum ada peringkat
- 589-Article Text-1298-1-10-20220830 PDFDokumen12 halaman589-Article Text-1298-1-10-20220830 PDFBella FebriantiBelum ada peringkat
- Zhu 2023 Oi 230637 1687872003.91163Dokumen15 halamanZhu 2023 Oi 230637 1687872003.91163Lucia NiculaeBelum ada peringkat
- New Developments in Neonatal Respiratory MenagmentDokumen7 halamanNew Developments in Neonatal Respiratory MenagmentTin TomašićBelum ada peringkat
- CPAPDokumen53 halamanCPAPvibhurocksBelum ada peringkat
- Cpap 2011-13Dokumen5 halamanCpap 2011-13Rajender SinghBelum ada peringkat
- 8 - Shetty2016Dokumen5 halaman8 - Shetty2016Rosa PerezBelum ada peringkat
- Pediatric Pulmonology 2021, Dell'ortoDokumen8 halamanPediatric Pulmonology 2021, Dell'ortoRadu CiprianBelum ada peringkat
- Jnksreenan 2001Dokumen5 halamanJnksreenan 2001fitriBelum ada peringkat
- Bubble CPAPDokumen36 halamanBubble CPAPSamsul MujakarBelum ada peringkat
- Home-Made Continuous Positive Airways Pressure Device May Reduce Mortality in Neonates With Respiratory Distress in Low-Resource SettingDokumen5 halamanHome-Made Continuous Positive Airways Pressure Device May Reduce Mortality in Neonates With Respiratory Distress in Low-Resource SettingNovi AryandaBelum ada peringkat
- Non Invasive Ventilation Techniques for Respiratory DistressDokumen76 halamanNon Invasive Ventilation Techniques for Respiratory DistressTitik sukamtiBelum ada peringkat
- 146336-Article Text-386661-1-10-20161019Dokumen8 halaman146336-Article Text-386661-1-10-20161019Huri AbbasiBelum ada peringkat
- Guideline for Prevention and Management of Bronchopulmonary DysplasiaDokumen28 halamanGuideline for Prevention and Management of Bronchopulmonary Dysplasiajanfk2000Belum ada peringkat
- Premedication With Fentanyl For Less Invasive SurfDokumen19 halamanPremedication With Fentanyl For Less Invasive SurfRochnald PigaiBelum ada peringkat
- Guidelines For Surfactant Administration (Surfactant Replacement Therapy) University of Iowa Stead Family Children's Hospital 2Dokumen1 halamanGuidelines For Surfactant Administration (Surfactant Replacement Therapy) University of Iowa Stead Family Children's Hospital 2Anonymous 18GsyXbBelum ada peringkat
- KLJKLHJGHDokumen8 halamanKLJKLHJGHAnonymous qpHeArUBelum ada peringkat
- Bubble CPAP in Neonatal Unit of TUTHDokumen5 halamanBubble CPAP in Neonatal Unit of TUTHCALLA PARICAHUA MARINABelum ada peringkat
- Continuous Positive PDFDokumen13 halamanContinuous Positive PDFdwi wulanBelum ada peringkat
- Carmelli Mariae H. Calugay 8-23-13 BSN-2Dokumen1 halamanCarmelli Mariae H. Calugay 8-23-13 BSN-2Carmelli Mariae CalugayBelum ada peringkat
- DR Lily - Resp Distress in Newborn Infants PDFDokumen45 halamanDR Lily - Resp Distress in Newborn Infants PDFM Ilham MBelum ada peringkat
- Clinical Guidelines For CPAP TitrationDokumen15 halamanClinical Guidelines For CPAP Titrationsavvy_as_98Belum ada peringkat
- Bubble CPAPDokumen36 halamanBubble CPAPRima WulandariBelum ada peringkat
- 2010 Early CPAP Vs Surfactant in EPTI NEJMDokumen10 halaman2010 Early CPAP Vs Surfactant in EPTI NEJMFiorella VilcaBelum ada peringkat
- Guidelines For Use of Bubble-CPAP ConcentratorsDokumen10 halamanGuidelines For Use of Bubble-CPAP ConcentratorsevanBelum ada peringkat
- Termofisher Guide Stem CellDokumen60 halamanTermofisher Guide Stem Cellnadhifa akBelum ada peringkat
- Laporan Tumor UreterDokumen2 halamanLaporan Tumor Ureternadhifa akBelum ada peringkat
- Burn Patient Management Guidelines PDFDokumen41 halamanBurn Patient Management Guidelines PDFIndah Kurnia100% (3)
- Laporan Tumor UreterDokumen7 halamanLaporan Tumor Ureternadhifa akBelum ada peringkat
- Drugs Classification and Drugs Dosage FormsDokumen32 halamanDrugs Classification and Drugs Dosage Formsnadhifa akBelum ada peringkat
- Drug FormsDokumen23 halamanDrug Formsnadhifa akBelum ada peringkat
- Laporan Tumor UreterDokumen2 halamanLaporan Tumor Ureternadhifa akBelum ada peringkat
- Medical Surgical Nursing Review NotesDokumen209 halamanMedical Surgical Nursing Review Notesabusaifluay100% (1)
- Viasys Bird Avian VentilatorDokumen2 halamanViasys Bird Avian VentilatorEng-Akram AlwahibiBelum ada peringkat
- Week 9 GM and Internship SlidesDokumen75 halamanWeek 9 GM and Internship Slidesapi-235454491Belum ada peringkat
- Bronchiolitis in ChildrenDokumen16 halamanBronchiolitis in ChildrenNym Angga Santosa100% (1)
- NCP Ineffective Breathing PatternDokumen3 halamanNCP Ineffective Breathing PatternNecheal BaayBelum ada peringkat
- Awake Prone Positioning For Non-Intubated Oxygen Dependent COVID-19 Pneumonia PatientsDokumen4 halamanAwake Prone Positioning For Non-Intubated Oxygen Dependent COVID-19 Pneumonia PatientsMuri MurdianaBelum ada peringkat
- Chapter 15 BEDSIDE ASSESSMENT OF THE PATIENTDokumen16 halamanChapter 15 BEDSIDE ASSESSMENT OF THE PATIENTZahra Margrette SchuckBelum ada peringkat
- Special Articles: Awake Intubation Intubation After Induction of General AnesthesiaDokumen1 halamanSpecial Articles: Awake Intubation Intubation After Induction of General AnesthesiaOKE channelBelum ada peringkat
- Journal Club DR - MaleehaDokumen45 halamanJournal Club DR - MaleehaSYED MUHAMMAD SAMEEDBelum ada peringkat
- Bronchiolitis PDFDokumen5 halamanBronchiolitis PDFjuniorebindaBelum ada peringkat
- Cap No GraphyDokumen21 halamanCap No GraphyPrabhakar KumarBelum ada peringkat
- Nursing Care Plan for Bronchial Asthma PatientDokumen2 halamanNursing Care Plan for Bronchial Asthma Patient22 - Fernandez, Lyza Mae D.Belum ada peringkat
- ACUTE RESPIRATORY DISTRESSDokumen1 halamanACUTE RESPIRATORY DISTRESSchristine louise bernardo100% (1)
- Lab Report 1 Pulmonary Function-3Dokumen12 halamanLab Report 1 Pulmonary Function-3api-315973465Belum ada peringkat
- Guidelines Surfactant Therapy RDSDokumen4 halamanGuidelines Surfactant Therapy RDSDella Elvina RoeslandBelum ada peringkat
- AX400 - Specification V1.2 2020.2.1Dokumen6 halamanAX400 - Specification V1.2 2020.2.1AndresBelum ada peringkat
- Case Analysis PediatricsDokumen31 halamanCase Analysis PediatricsLYNDLY AGAGEOBelum ada peringkat
- Chest PT in Icu 1996@609.full PDFDokumen17 halamanChest PT in Icu 1996@609.full PDFDyah SafitriBelum ada peringkat
- Pathophysiology Planning InterventionDokumen1 halamanPathophysiology Planning InterventionBenz ParCoBelum ada peringkat
- Clinical Cheat Sheet: Radiographic AssessmentDokumen1 halamanClinical Cheat Sheet: Radiographic AssessmentTracy PopeBelum ada peringkat
- Tecme Neumovent Technical Manual 94Dokumen94 halamanTecme Neumovent Technical Manual 94Marina Garza GaliciaBelum ada peringkat
- ElVent G7 Technical Specifications, June 17 2021Dokumen10 halamanElVent G7 Technical Specifications, June 17 2021malik_saleem_akbarBelum ada peringkat
- VAP Prevention StrategiesDokumen6 halamanVAP Prevention StrategiesCGKN BanyuwangiBelum ada peringkat
- Bronchoscopy Case SeriesDokumen13 halamanBronchoscopy Case SeriesShivaranjani sakthivelBelum ada peringkat
- Respiratorymuscle Assessmentinclinical Practice: Michael I. PolkeyDokumen9 halamanRespiratorymuscle Assessmentinclinical Practice: Michael I. PolkeyanaBelum ada peringkat
- Bronchopulmonary DysplasiaDokumen17 halamanBronchopulmonary DysplasiaRuDy RaviBelum ada peringkat
- Childhood AsthmaDokumen40 halamanChildhood AsthmachinchuBelum ada peringkat
- First Announcement Pdpi Update 1Dokumen25 halamanFirst Announcement Pdpi Update 1sheeno2607Belum ada peringkat
- Endotracheal IntubationDokumen5 halamanEndotracheal IntubationDarell M. BookBelum ada peringkat
- Hypoxemic Respiratory FailureDokumen70 halamanHypoxemic Respiratory FailureMohamed Rikarz Ahamed RikarzBelum ada peringkat