Ikterus PDF
Diunggah oleh
Ribut NingsihJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Ikterus PDF
Diunggah oleh
Ribut NingsihHak Cipta:
Format Tersedia
CPG UpDATE
Management of neonatal jaundice in primary care
Wan ASL, Mat Daud S, Teh SH, Choo YM, Kutty FM on behalf of Development Group
Clinical Practice Guidelines Management of Neonatal Jaundice (Second Edition).
Wan ASL, Mat Daud S, Teh SH, et al. Management of neonatal jaundice in primary care. Malays Fam Physician. 2016;11(2 & 3);16–19.
Abstract
Keywords:
Neonatal jaundice, risk The Clinical Practice Guidelines on Management of Neonatal Jaundice 2003 was updated by a
factors, phototherapy, multidisciplinary development group and approved by the Ministry of Health Malaysia in 2014. A
primary care, prevention systematic review of 13 clinical questions was conducted using evidence retrieved mainly from Medline
and Cochrane databases. Critical appraisal was done using the Critical Appraisal Skills Programme
checklist. Recommendations were formulated based on the accepted 103 evidences and tailored to local
Authors: setting as stated below.
Angeline Wan Seng Lian Neonatal jaundice (NNJ) is a common condition seen in primary care. Multiple risk factors contribute
Consultant Neonatologist to severe NNJ, which if untreated can lead to adverse neurological outcomes. Visual assessment,
Hospital Pakar Sultanah Fatimah, transcutaneous bilirubinometer (TcB) and total serum bilirubin (TSB) are the methods used for the
Jalan Salleh Muar, 84000 Muar, detection of NNJ. Phototherapy remains the mainstay of the treatment. Babies with severe NNJ
Johor should be followed-up to detect and manage sequelae. Strategies to prevent severe NNJ include health
E-mail: angelinewsl@yahoo.com / education, identification of risk factors, proper assessment and early referral.
angelinewsl@gmail.com
Suzaini Mat Daud Introduction • rapid rise of total serum bilirubin (TSB)
Family Medicine Specialist • sepsis
Klinik Kesihatan Changloon Jaundice is one of the most common conditions, • lactation failure in exclusive breastfeeding
Jitra, Kubang Pasu, 06010 which needs medical attention in newborn babies. • high predischarge bilirubin level
Changloon, Kedah It is caused by high levels of bilirubin in the • cephalohaematoma or bruises
E-mail: drsuz67@yahoo.com.my blood. Globally, about 60% of the term babies • babies of diabetic mothers
and 80% of the preterm babies develop jaundice • family history of severe NNJ in siblings
Teh Siao Hean in the first week of life. In most of the babies,
Consultant Paediatrician early jaundice is physiological and harmless. Breastfeeding, because of its benefits, should be
Hospital Miri, Jalan Cahaya Miri, However, some babies may develop severe continued in babies with jaundice. Adequate
98000 Miri, Sarawak jaundice, which can be harmful if left untreated. lactation/breastfeeding support should be
E-mail: tehshean@gmail.com High levels of bilirubin can lead to brain damage, provided to all mothers, particularly those with
which may result in neurodevelopmental preterm babies. In jaundice-associated breastfed
Choo Yao Mun impairment such as cerebral palsy, and visual and babies with inadequate intake, excessive weight
Senior Lecturer & Consultant hearing loss. Hence early detection of neonatal loss (>10% of birth weight) or dehydration,
Neonatologist jaundice (NNJ) is very important, followed by supplementation with expressed breast milk or
Pusat Perubatan Universiti Malaya, timely referral and appropriate treatment. formula may be considered. Babies with weight
Lembah Pantai, 59100 Kuala Lumpur, loss >7% of birth weight should be evaluated and
Wilayah Persekutuan Kuala Lumpur An evidence-based Clinical Practice Guidelines closely monitored for jaundice.
E-mail: yaomun@um.edu.my on Management of Neonatal Jaundice (Second
Edition) was published in 2015, which addresses Methods of detection
Fazila Mohamed Kutty the management of NNJ in the term and
Consultant Neonatologist preterm babies excluding prolonged jaundice and All babies should be visually assessed for jaundice
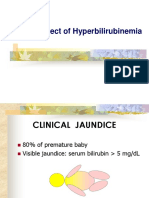
Hospital Serdang, Jalan Puchong conjugated hyperbilirubinaemia. at every opportunity. Kramer’s rule describes the
Kajang, 43000 Kajang, Selangor relationship between serum bilirubin levels and
E-mail: dfuzzy@gmail.com Risk factors the progression of skin discolouration (see Table
1 and Figure 1). Trained primary health workers
Risk factors of severe NNJ are as follows: may use this as a screening tool.
• prematurity
• low birth weight
• jaundice in the first 24 hours of life
• mother with blood group O or rhesus negative
• glucose-6-phosphate dehydrogenase (G6PD)
deficiency
16 Malaysian Family Physician 2016; Volume 11, Number 2 & 3
cpg update
Table 1. Visual assessment of NNJ (Kramer’s rule)
Range of serum bilirubin
Area of the body Level
µmol/L mg/dL
Head and neck 1 68–133 4–8
Upper trunk (above umbilicus) 2 85–204 5–12
Lower trunk and thighs (below umbilicus) 3 136–272 8–16
Arms and lower legs 4 187–306 11–18
Palms and soles 5 ≥306 ≥18
The transcutaneous bilirubinometer (TcB) is a
hand-held device that measures the amount of
bilirubin in the skin. If available, it may be used
in the assessment of NNJ. Mean differences
between TcB measurements and TSB levels
are large when the bilirubin levels exceed 205
μmol/L (12 mg/dL).
Visual assessment and TcB should not be used
to monitor bilirubin levels in the babies on
phototherapy.
TSB measurement is the gold standard for
detecting and determining the levels of
hyperbilirubinaemia. It is used to confirm
the levels of bilirubin detected from visual
assessment and TcB as well as to monitor the
babies on phototherapy.
Treatment
Phototherapy is the mainstay of treatment in
NNJ. Phototherapy should be commenced
when TSB reaches the phototherapy threshold
for NNJ (see Table 2). Phototherapy
Figure 1. Visual assessment of NNJ (Kramer’s thresholds are lower in the preterm and low
rule) birth weight babies.
Table 2. TSB levels for phototherapy and exchange transfusion (ET) in babies ≥35 weeks gestation
High risk
Medium risk
Low risk (35–37 weeks + 6 days with risk
Age (≥38 weeks with risk factors or
(≥38 weeks and well) factors)
35–37 weeks + 6 days and well)
TSB in mg/dL (µmol/L)
Hours
Conventional Conventional Conventional
of life ET ET ET
phototherapy phototherapy phototherapy
<24* - - - - - -
24 9 (154) 19 (325) 7 (120) 17 (291) 5 (86) 15 (257)
48 12 (205) 22 (376) 10 (171) 19 (325) 8 (137) 17 (291)
72 15 (257) 24 (410) 12 (205) 21 (359) 10 (171) 18.5 (316)
96 17 (291) 25 (428) 14 (239) 22.5 (385) 11 (188) 19 (325)
>96 18 (308) 25 (428) 15 (257) 22.5 (385) 12 (205) 19 (325)
a Start intensive phototherapy at TSB 3 mg/dL (51 µmol/L) above the level for conventional phototherapy or
when TSB increasing at >0.5 mg/dL (8.5 µmol/L) per hour.
b Risk factors are isoimmune haemolytic disease, G6PD deficiency, asphyxia and sepsis.
* Jaundice appearing within 24 hours of life is abnormal and needs further evaluation.
Malaysian Family Physician 2016; Volume 11, Number 2 & 3 17
cpg update
ET should be considered when TSB reaches the • Late preterm, G6PD deficiency and isoimmune
threshold levels in NNJ (see Table 2). haemolytic disease (ABO and rhesus
incompatibility) are the important risk factors
There is limited good evidence on the use for developing severe NNJ. Phototherapy
of pharmacotherapy (clofibrate, intravenous thresholds are lower for babies with these risk
immunoglobulin, human albumin and factors.
phenobarbitone) and complementary medicine in • All babies should be screened for G6PD
NNJ. deficiency at birth. If G6PD is deficient, babies
should be admitted and monitored for NNJ
Referral during the first 5 days of life. If they were
discharged earlier, they should be followed-up
Babies should be referred for phototherapy if closely.
their TSB reaches the phototherapy threshold • Breastfeeding should be encouraged and
(see Table 2). They should also be referred to the adequate lactation support should be provided
secondary/tertiary care when they are presented to all mothers.
with any of the following: • Predischarge screening in hospital using TcB
may be considered.
• onset of jaundice within 24 hours of life
• rapidly rising TSB of >6 mg/dL/day (103 Information for parents and carers
μmol/L/day)
• clinical jaundice below umbilicus, corresponding The following advices are helpful for parents/carers
to TSB of 12–15 mg/dL (205–257 μmol/L) on NNJ:
• clinical jaundice till the soles of the feet (urgent
referral for possibility of ET) 1. Look for jaundice daily during the first week of
• G6PD deficiency, if not previously hospitalised life.
• clinical symptoms/signs suggestive of sepsis 2. Check the naked baby for jaundice in bright
and preferably natural light, by blanching the
The overall summary on management is shown in skin with gentle finger pressure over the chest.
the Algorithm on Management of NNJ. 3. Presence of jaundice needs to be confirmed
by healthcare providers; blood tests may be
Long-term follow-up required.
4. Jaundice in the first 48 hours of life needs
Severe NNJ may cause acute bilirubin urgent review by healthcare providers.
encephalopathy (ABE). Babies with ABE 5. Continue breastfeeding even if the baby is
should have long-term follow-up to monitor the jaundiced. Contact the healthcare provider for
neurodevelopmental sequelae (athetoid cerebral assistance with breastfeeding if needed.
palsy, intellectual disability and high-frequency 6. Untreated jaundice may lead to deafness and
hearing loss). brain damage.
7. Phototherapy is a safe and effective form of
Babies with severe jaundice [TSB >20 mg/dL (342 treatment for NNJ.
μmol/L)] or those who require ETs should have 8. Traditional and alternative methods of
auditory brainstem response (ABR) testing done treating jaundice are unproven and likely to be
within the first 3 months of life. If the ABR is ineffective.
abnormal, neurodevelopmental follow-up should 9. Exposing the baby to sunlight as a form of
be continued. treatment may be harmful due to dehydration
and sunburn.
Healthy babies born at 35 weeks gestation and
above with non-haemolytic hyperbilirubinaemia Details of the evidence supporting the above
and TSB <25 mg/dL (428 μmol/L) may be statements can be found in Clinical Practice
followed-up at the primary care level. Guidelines on the Management of Neonatal
Jaundice (Second Edition) 2014, available
Strategies to prevent severe NNJ on the following website: Ministry of Health
Malaysia: http://www.moh.gov.my; and Academy
• Antenatal and postnatal strategies include: of Medicine: http://www.acadmed.org.my.
• health education on NNJ Corresponding organisation: CPG Secretariat,
• identification of risk factors Health Technology Assessment Section, Medical
• early detection of NNJ Development Division, Ministry of Health
• proper assessment of babies with NNJ Malaysia and contactable at htamalaysia@moh.
• early referral as indicated gov.my.
18 Malaysian Family Physician 2016; Volume 11, Number 2 & 3
cpg update
Algorithm on Management of Neonatal Jaundice
NNJ
G6PD deficiency
>24 Hours Life <24 Hours Life
Admit and observe
Assess risk Admit
factors Yes No
Jaundice
Yes
Need
Need treatment Phototherapy ± ET
admission
No
Jaundice resolved
Monitor as scheduled* Yes
No Rebound Monitor as scheduled
Jaundice Jaundice
resolved
No
Yes Discharge and
follow-up
* If jaundice persists beyond 14 days in the term babies and 21 days in the preterm babies, further evaluation for
prolonged jaundice is needed.
Malaysian Family Physician 2016; Volume 11, Number 2 & 3 19
Anda mungkin juga menyukai
- QR Management of Neonatal Jaundice (Second Edition) PDFDokumen8 halamanQR Management of Neonatal Jaundice (Second Edition) PDFOlayinka AwofoduBelum ada peringkat
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsDari EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsBelum ada peringkat
- Neonatal Jaundice Clinical Practice GuidelineDokumen35 halamanNeonatal Jaundice Clinical Practice GuidelineprinsepejesseBelum ada peringkat
- Pregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsDari EverandPregnancy Tests Explained (2Nd Edition): Current Trends of Antenatal TestsBelum ada peringkat
- Prevalence of Neonatal JaundiceDokumen4 halamanPrevalence of Neonatal JaundicekattysarkBelum ada peringkat
- QR Management of Neonatal Jaundice (Second Edition)Dokumen8 halamanQR Management of Neonatal Jaundice (Second Edition)نور حسليندا اسحاقBelum ada peringkat
- N NJ Grand RoundDokumen39 halamanN NJ Grand RoundIshfaq AhmadBelum ada peringkat
- The Prevalence of Neonatal Jaundice and Risk Factors in Healthy Term Neonates at National District Hospital in BloemfonteinDokumen6 halamanThe Prevalence of Neonatal Jaundice and Risk Factors in Healthy Term Neonates at National District Hospital in BloemfonteinniaBelum ada peringkat
- NNJDokumen20 halamanNNJLatifah AlsahaleyBelum ada peringkat
- JaundiceDokumen22 halamanJaundiceimanzurynn161Belum ada peringkat
- Inservices PhototherapyDokumen11 halamanInservices PhototherapySweta ManandharBelum ada peringkat
- 113 JMSCRDokumen12 halaman113 JMSCRRiki AntoBelum ada peringkat
- A91 The Accuracy of Transcutaneous BiliDokumen7 halamanA91 The Accuracy of Transcutaneous BiliFahri OvalıBelum ada peringkat
- Neonatal Jaundice - 2019Dokumen19 halamanNeonatal Jaundice - 2019floare de coltBelum ada peringkat
- Fetomaternal Outcome and Raised Bilirubin Level in PregnancyDokumen4 halamanFetomaternal Outcome and Raised Bilirubin Level in PregnancyPrima Hari PratamaBelum ada peringkat
- Jaundice in The Newborns: Division of Neonatology, Department of Pediatrics All India Institute of Medical SciencesDokumen23 halamanJaundice in The Newborns: Division of Neonatology, Department of Pediatrics All India Institute of Medical Sciencesbubble_inBelum ada peringkat
- JaundiceDokumen11 halamanJaundiceHusna Mat IsaBelum ada peringkat
- Neonatal Jaundice PDFDokumen10 halamanNeonatal Jaundice PDFibanggBelum ada peringkat
- Neonatal JaundiceDokumen65 halamanNeonatal JaundiceAditi BanerjeeBelum ada peringkat
- NNJ by DR MadhuDokumen59 halamanNNJ by DR MadhuNabrazz SthaBelum ada peringkat
- Maisel S 2012Dokumen5 halamanMaisel S 2012marsyaBelum ada peringkat
- Jemc V5i2 23384Dokumen6 halamanJemc V5i2 23384Students CBUBelum ada peringkat
- Phototherapy 2Dokumen8 halamanPhototherapy 2Dyah Putri PermatasariBelum ada peringkat
- 2489-Article Text-8656-3-10-20210204Dokumen4 halaman2489-Article Text-8656-3-10-20210204rexaBelum ada peringkat
- Final Case Study-Bili (ReVISED)Dokumen35 halamanFinal Case Study-Bili (ReVISED)malentot100% (1)
- Thesis On Neonatal HyperbilirubinemiaDokumen5 halamanThesis On Neonatal Hyperbilirubinemiajuliepottsdenton100% (4)
- PhototherapyDokumen8 halamanPhototherapyNylia AtibiBelum ada peringkat
- Neonatal JaundiceDokumen37 halamanNeonatal JaundiceAbraham ChiuBelum ada peringkat
- Annals of Pediatric Research: Open AccessDokumen6 halamanAnnals of Pediatric Research: Open AccessjanainaBelum ada peringkat
- HyperbilirubinemiaDokumen4 halamanHyperbilirubinemiaJuan Carlos Andrade SalumBelum ada peringkat
- Neonatal Jaundice Causes and ManagementDokumen5 halamanNeonatal Jaundice Causes and Managementrizkia pramadaniBelum ada peringkat
- Avaluació I TractamentDokumen10 halamanAvaluació I Tractamentanollaru38Belum ada peringkat
- International Journal of Pediatric Research Ijpr 7 073Dokumen9 halamanInternational Journal of Pediatric Research Ijpr 7 073Paul AsrBelum ada peringkat
- Risk Factors For Neonatal Hyperbilirubinemia: A Case Control StudyDokumen5 halamanRisk Factors For Neonatal Hyperbilirubinemia: A Case Control StudyRajba NazalahBelum ada peringkat
- Mahapedicon 2005Dokumen3 halamanMahapedicon 2005noelmendonsaBelum ada peringkat
- Neonatal Jaundice and Prolonged Jaundice in Newborn InfantsDokumen33 halamanNeonatal Jaundice and Prolonged Jaundice in Newborn InfantskeyRielleBelum ada peringkat
- Clinical Aspect of HyperbilirubinemiaDokumen39 halamanClinical Aspect of HyperbilirubinemiaAfdelina RizkyBelum ada peringkat
- Neonatal JaundiceDokumen16 halamanNeonatal JaundiceTatiana JalbaBelum ada peringkat
- HyperbilirubinemiaDokumen52 halamanHyperbilirubinemiaNheljane DelacruzBelum ada peringkat
- Original ResearchDokumen6 halamanOriginal ResearchShikhar PradhanBelum ada peringkat
- PhototherapyDokumen11 halamanPhototherapySweta ManandharBelum ada peringkat
- Phototherapy 2018 PDFDokumen22 halamanPhototherapy 2018 PDFDr-Dalya ShakirBelum ada peringkat
- Neonatal Jaundice Lecture,,By DR Kassahun GirmaDokumen25 halamanNeonatal Jaundice Lecture,,By DR Kassahun GirmaKassahun Girma GelawBelum ada peringkat
- Unconjugated Hyperbilirubinemia in Term and Late Preterm Infants - Management - UpToDateDokumen27 halamanUnconjugated Hyperbilirubinemia in Term and Late Preterm Infants - Management - UpToDateTran Trang AnhBelum ada peringkat
- Iap Guidelines For Epilepsy 2014Dokumen45 halamanIap Guidelines For Epilepsy 2014iannikkiBelum ada peringkat
- Iap Guidelines For Epilepsy 2014Dokumen45 halamanIap Guidelines For Epilepsy 2014Karpur ShirsatBelum ada peringkat
- Neonatal Jaundice JCG0013 v3.1Dokumen11 halamanNeonatal Jaundice JCG0013 v3.1Alejandro Motolinía100% (1)
- Ensemble1-2022-Analysis and Prediction of Gestational Diabetes MellitusDokumen20 halamanEnsemble1-2022-Analysis and Prediction of Gestational Diabetes MellitusMeriam Jemel HachichaBelum ada peringkat
- Comparing JM-105 and MBJ-20 Transcutaneous Bilirubinometers According To The Area Tested in Ethnically Diverse Late-Preterm and Term NeonatesDokumen8 halamanComparing JM-105 and MBJ-20 Transcutaneous Bilirubinometers According To The Area Tested in Ethnically Diverse Late-Preterm and Term NeonatesShikhar PradhanBelum ada peringkat
- Synopsis Phototherapy in JaunicDokumen5 halamanSynopsis Phototherapy in JaunicEngr Saeed Ur RehmanBelum ada peringkat
- Neonatal JaundiceDokumen3 halamanNeonatal JaundicevorezBelum ada peringkat
- Neonatal Jaundice (Wong)Dokumen54 halamanNeonatal Jaundice (Wong)Siti Hajar100% (1)
- 2 Jaundice in The NBDokumen33 halaman2 Jaundice in The NBCheru DugaseBelum ada peringkat
- Hyperbilirubinemia PaperDokumen7 halamanHyperbilirubinemia Paperapi-545292605Belum ada peringkat
- High-Intensity Phototherapy For The Treatment of Severe Nonhaemolytic Neonatal HyperbilirubinemiaDokumen4 halamanHigh-Intensity Phototherapy For The Treatment of Severe Nonhaemolytic Neonatal HyperbilirubinemiamoyretnowulanBelum ada peringkat
- Early VS Routine GDM Screening in Obese Pregnant WomenDokumen5 halamanEarly VS Routine GDM Screening in Obese Pregnant WomenIJAR JOURNALBelum ada peringkat
- Common Neonatal ProblemsDokumen32 halamanCommon Neonatal ProblemsbrhomzalatBelum ada peringkat
- Prenatal Screening SOGCDokumen13 halamanPrenatal Screening SOGCBrendaBelum ada peringkat
- Gestational Diabetes Screening in AustraliaDokumen9 halamanGestational Diabetes Screening in AustraliaRaniMSinghBelum ada peringkat
- Reflective Practice in Nursing - Saw. Final2Dokumen20 halamanReflective Practice in Nursing - Saw. Final2Anonymous HK3LyOqR2g100% (2)
- Breast Duct Excision ML38861Dokumen5 halamanBreast Duct Excision ML38861DrFeelgood WolfslandBelum ada peringkat
- 2023 Vertical Transmission Prevention Guideline 04092023 Signed WEB - 1Dokumen62 halaman2023 Vertical Transmission Prevention Guideline 04092023 Signed WEB - 1ipfiBelum ada peringkat
- The Damascus (Shami) Goat of CyprusDokumen10 halamanThe Damascus (Shami) Goat of CyprusblackvenumBelum ada peringkat
- Maternity Benefit Policy in BRACDokumen3 halamanMaternity Benefit Policy in BRACPayel BasakBelum ada peringkat
- IYCFDokumen179 halamanIYCFPiao Liang JingBelum ada peringkat
- Nutrition Guidance For The General Population V5 19th June 2020Dokumen32 halamanNutrition Guidance For The General Population V5 19th June 2020namakoolaBelum ada peringkat
- A Typology of Nursing Problems in Family Nursing ProblemDokumen5 halamanA Typology of Nursing Problems in Family Nursing ProblemRho Vince Caño MalagueñoBelum ada peringkat
- RA10028Dokumen9 halamanRA10028Unis BautistaBelum ada peringkat
- Edited SyllabusfcDokumen36 halamanEdited SyllabusfcRushikesh KarandeBelum ada peringkat
- Q2-Health-8 Egam M7Dokumen17 halamanQ2-Health-8 Egam M7GeceylBelum ada peringkat
- Nutrition and HIVDokumen28 halamanNutrition and HIVDrake Wa YesuBelum ada peringkat
- What Was Shakespeares England LikeDokumen6 halamanWhat Was Shakespeares England LikeWitnyBelum ada peringkat
- Community Health Nursing Exam 3Dokumen7 halamanCommunity Health Nursing Exam 3Hannah BuquironBelum ada peringkat
- Nutrients 13 01329Dokumen15 halamanNutrients 13 01329Ciara Maecy B. DomingoBelum ada peringkat
- Effectiveness of Different Massage Techniques For Breastfeeding Mothers To Increase Milk Production: A Systematic ReviewDokumen17 halamanEffectiveness of Different Massage Techniques For Breastfeeding Mothers To Increase Milk Production: A Systematic ReviewdriveamadeaBelum ada peringkat
- Module 4 Health, Water Sanitation, Hygiene Promotion...Dokumen14 halamanModule 4 Health, Water Sanitation, Hygiene Promotion...JM MagsayoBelum ada peringkat
- Antenatal ExaminationDokumen7 halamanAntenatal ExaminationTAMASHREE ROYBelum ada peringkat
- Nutrition During Infancy and Early Childhood PDFDokumen17 halamanNutrition During Infancy and Early Childhood PDFALNAKIBelum ada peringkat
- Pediatric History Taking & Pe Simulation: Student'S Task Done Not DoneDokumen8 halamanPediatric History Taking & Pe Simulation: Student'S Task Done Not DoneFrancis CervantesBelum ada peringkat
- Research ReferencesDokumen47 halamanResearch ReferencesVaishali SinghBelum ada peringkat
- Intrapartum HandoutDokumen29 halamanIntrapartum HandoutZahBelum ada peringkat
- Ecology of MalnutritionDokumen10 halamanEcology of MalnutritionnareshraopendyalaBelum ada peringkat
- NTG in NCM 120 Decent Work Topic 2 Laws Affecting Nursing Practice in The PHDokumen20 halamanNTG in NCM 120 Decent Work Topic 2 Laws Affecting Nursing Practice in The PHAntonette GrivialdeBelum ada peringkat
- Pediatrics Nutrition in PracticeDokumen349 halamanPediatrics Nutrition in Practicebalyaibnu_690869145100% (2)
- Nivolumab: Other Names: Opdivo®Dokumen6 halamanNivolumab: Other Names: Opdivo®Prabhjot SinghBelum ada peringkat
- Antihistamines (Hayfever) and BreastfeedingDokumen2 halamanAntihistamines (Hayfever) and BreastfeedingEzraGoenadiBelum ada peringkat
- Guideline HiperbilirubinemiaDokumen20 halamanGuideline HiperbilirubinemiaCaroline LimaBelum ada peringkat
- CEMONCDokumen10 halamanCEMONCApril GuiangBelum ada peringkat
- Prevention Early Identification and Intervention of DisabilitiesDokumen34 halamanPrevention Early Identification and Intervention of Disabilitiesapi-254947702100% (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 5 dari 5 bintang5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossDari EverandThe Obesity Code: Unlocking the Secrets of Weight LossPenilaian: 4 dari 5 bintang4/5 (6)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDari EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDPenilaian: 5 dari 5 bintang5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePenilaian: 2 dari 5 bintang2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (26)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDari EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionPenilaian: 4 dari 5 bintang4/5 (404)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDari EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisPenilaian: 4.5 dari 5 bintang4.5/5 (42)
- The Comfort of Crows: A Backyard YearDari EverandThe Comfort of Crows: A Backyard YearPenilaian: 4.5 dari 5 bintang4.5/5 (23)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDari EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsPenilaian: 5 dari 5 bintang5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDari EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDari EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisPenilaian: 4 dari 5 bintang4/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDari EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsBelum ada peringkat
- Why We Die: The New Science of Aging and the Quest for ImmortalityDari EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityPenilaian: 4 dari 5 bintang4/5 (3)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDari EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryPenilaian: 4 dari 5 bintang4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Dari EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Penilaian: 4.5 dari 5 bintang4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerDari EverandGut: the new and revised Sunday Times bestsellerPenilaian: 4 dari 5 bintang4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDari EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisPenilaian: 3.5 dari 5 bintang3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDari EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsPenilaian: 3.5 dari 5 bintang3.5/5 (3)
- The Marshmallow Test: Mastering Self-ControlDari EverandThe Marshmallow Test: Mastering Self-ControlPenilaian: 4.5 dari 5 bintang4.5/5 (58)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDari EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingPenilaian: 4 dari 5 bintang4/5 (1138)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDari EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningPenilaian: 4 dari 5 bintang4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDari EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsPenilaian: 4.5 dari 5 bintang4.5/5 (169)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDari EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessPenilaian: 4.5 dari 5 bintang4.5/5 (328)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsDari EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsPenilaian: 4.5 dari 5 bintang4.5/5 (6)