31041313
Diunggah oleh
carolinapolotorresHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
31041313
Diunggah oleh
carolinapolotorresHak Cipta:
Format Tersedia
REVIEW
published: 16 April 2019
doi: 10.3389/fmed.2019.00074
Treatment of Infections Due to MDR
Gram-Negative Bacteria
Matteo Bassetti 1*, Maddalena Peghin 1 , Antonio Vena 1 and Daniele Roberto Giacobbe 2
1
Clinica Malattie Infettive, Azienda Sanitaria Universitaria Integrata di Udine, Presidio Ospedaliero Universitario Santa Maria
della Misericordia, Udine, Italy, 2 Department of Health Sciences, University of Genoa, Genoa, Italy
The treatment of multidrug-resistant Gram-negative bacteria (MDR-GNB) infections in
critically ill patients presents many challenges. Since an effective treatment should be
administered as soon as possible, resistance to many antimicrobial classes almost
invariably reduces the probability of adequate empirical coverage, with possible
unfavorable consequences. In this light, readily available patient’s medical history
and updated information about the local microbiological epidemiology remain critical
Edited by: for defining the baseline risk of MDR-GNB infections and firmly guiding empirical
George Dimopoulos, treatment choices, with the aim of avoiding both undertreatment and overtreatment.
University General Hospital Attikon,
Greece Rapid diagnostics and efficient laboratory workflows are also of paramount
Reviewed by: importance both for anticipating diagnosis and for rapidly narrowing the antimicrobial
Despoina Koulenti, spectrum, with de-escalation purposes and in line with antimicrobial stewardship
University General Hospital Attikon,
principles. Carbapenem-resistant Enterobacteriaceae, Pseudomonas aeruginosa, and
Greece
Valter Viana Andrade-Neto, Acinetobacter baumannii are being reported with increasing frequencies worldwide,
Fundação Oswaldo Cruz (Fiocruz), although with important variability across regions, hospitals and even single wards.
Brazil
In the past few years, new treatment options, such as ceftazidime/avibactam,
*Correspondence:
Matteo Bassetti meropenem/vaborbactam, ceftolozane/tazobactam, plazomicin, and eravacycline have
matteo.bassetti@asuiud.sanita.fvg.it become available, and others will become soon, which have provided some much-
awaited resources for effectively counteracting severe infections due to these organisms.
Specialty section:
This article was submitted to
However, their optimal use should be guaranteed in the long term, for delaying as much
Infectious Diseases - Surveillance, as possible the emergence and diffusion of resistance to novel agents. Despite important
Prevention and Treatment,
progresses, pharmacokinetic/pharmacodynamic optimization of dosages and treatment
a section of the journal
Frontiers in Medicine duration in critically ill patients has still some areas of uncertainty requiring further study,
Received: 04 February 2019 that should take into account also resistance selection as a major endpoint. Treatment of
Accepted: 27 March 2019 severe MDR-GNB infections in critically ill patients in the near future will require an expert
Published: 16 April 2019
and complex clinical reasoning, of course taking into account the peculiar characteristics
Citation:
Bassetti M, Peghin M, Vena A and
of the target population, but also the need for adequate empirical coverage and the more
Giacobbe DR (2019) Treatment of and more specific enzyme-level activity of novel antimicrobials with respect to the different
Infections Due to MDR Gram-Negative
resistance mechanisms of MDR-GNB.
Bacteria. Front. Med. 6:74.
doi: 10.3389/fmed.2019.00074 Keywords: gram-negative, ICU, MDR, antimicrobial resistance, Pseudomonas, Acinetobacter, Klebsiella
Frontiers in Medicine | www.frontiersin.org 1 April 2019 | Volume 6 | Article 74
Bassetti et al. Gram-Negative Bacteria Infection Treatment
INTRODUCTION in the near future), that inevitably raise the question as to
whether the type of suspected resistance determinant (e.g., the
In the last 15 years, intensivists, and infectious diseases type of carbapenemase) should not only guide the choice of the
consultants have started to face novel peculiar challenges in the better agent/s to be administered, but also the decisions about
treatment of severe infections in critically ill patients in intensive escalation and de-escalation, in order to follow antimicrobial
care units (ICU), due to the selection and diffusion of multidrug- stewardship purposes also at the enzyme-level.
resistant Gram-negative bacteria (MDR-GNB) (1, 2). In this review, we discuss both current and future therapeutic
Indeed, although the development of resistance has approaches to severe MDR-GNB infections in critically-ill
accompanied antimicrobial therapy since its dawn, only in patients in ICU.
recent years GNB have started, in non-negligible numbers, to
manifest concomitant resistance to all commonly used classes of
antimicrobials. This has forced clinicians to consider treatment METHODS
approaches based on combinations of drugs with impaired
As the basis for the present narrative review, a literature
activity, and/or to rediscover old drugs with suboptimal
search was performed in the PubMed/MEDLINE database using
pharmacokinetics and toxicity issues, all in the absence of
various combinations of pertinent keywords (e.g., “ICU,” “Gram-
high-level evidence to firmly guide bedside decisions (3, 4).
negative,” “therapy,” “management,” “novel antibiotics,” “novel
Fortunately, this situation has started to change very recently,
drugs,” “Pseudomonas,” “Acinetobacter,” “Klebsiella,” “MDR”).
owing to the introduction into the market of novel drugs with
Subsequently, retrieved papers were discussed and further
potent activity against some MDR-GNB such as carbapenem-
iterative searches were conducted. Ultimately, two main narrative
resistant Enterobacterales (CRE) and carbapenem-resistant
chapters were organized as follows: (i) current treatment options
Pseudomonas aeruginosa (CRPA) (5, 6).
for MDR-GNB in critically-ill patients; (ii) future treatment
Nonetheless, the availability of novel agents does not
options for MDR-GNB in critically-ill patients.
automatically imply an easy and always successful treatment,
for several reasons: (i) most of available novel agents have still
suboptimal activity against carbapenem-resistant Acinetobacter CURRENT TREATMENT OPTIONS FOR
baumannii (CRAB); (ii) activity against CRE of novel β- MDR-GNB IN CRITICALLY-ILL PATIENTS
lactam/β-lactamase inhibitors (BL-BLI) is dependent of the
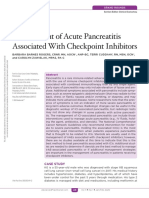
type of carbapenemase conferring resistance to carbapenems; The main characteristics of the currently available agents for the
(iii) resistance to novel antibacterials has already started to treatment of severe MDR-GNB infections in critically-ill patients
emerge, and widespread use of novel antibacterials should thus are briefly introduced in the following paragraphs, while an
be avoided, in order to relieve selective pressure for further example of possible clinical reasoning for guiding the treatment
development of resistance; (iv) on the other hand, adequate of MDR-GNB infections in critically-ill patients with currently
coverage for MDR should be empirically guaranteed in critically- available options is shown in Figure 1.
ill patients with severe infections and risk factors for MDR, in
order not to delay active treatment (7–9). With so many factors at Polymyxins
stake, treatment of MDR-GNB infections in critically-ill patients Polymyxins acts as detergents of the outer membrane of GNB,
are becoming a very complex task, which requires dedicated exerting bactericidal activity. Among those available for use
expertise, as well as an always updated knowledge of the patients’ in humans are colistin (polymyxin E) and polymyxin B. They
medical history and the local microbiology epidemiology, in were frequently used for the treatment of MDR-GNB infections
order to promptly recognize the risk of MDR-GNB and also the in the past few years, when they often remained among the
most likely resistance mechanisms involved. few (sometimes the only one) dependable options for CRE,
This latter factor is particularly important in light of CRPA, and CRAB (5, 10, 11). Nowadays, they are still among
the renewed possibility of treating severe MDR-GNB the first-line treatment options for CRAB infections (pending
infections with beta-lactams (some already available such approval of more effective agents), whereas for CRE and CRPA
as ceftazidime/avibactam, ceftolozane/tazobactam, and already available novel agents should be preferred whenever
meropenem/vaborbactam, and others that will be available possible, owing to the potential polymyxin-associated risks either
of nephrotoxicity or of suboptimal concentrations (especially
Abbreviations: ICU, intensive care units; MDR, multidrug-resistant; GNB, in the lung) (12). Furthermore, worrisome trends of increasing
Gram-negative bacteria; CRE, carbapenem-resistant Enterobacterales, CRPA, resistance have been reported in some countries (e.g., Italy and
carbapenem-resistant Pseudomonas aeruginosa; CRAB, carbapenem-resistant
Acinetobacter baumannii; β-lactam/β-lactamase inhibitors (BL-BLI); FDA, Food
Greece) (13, 14). Consequently, the use of polymyxins should
and Drug Administration; cUTI, complicated urinary tract infections; BSI, be optimized as much as possible in terms of dosages and
bloodstream infections; EMA, European Medicines Agency; RCT, randomized indications, in order both to maximize effectiveness and to curb
controlled trial; VAP, ventilator-associated pneumonia; cIAI, complicated the emergence of further polymyxin resistance. For this reason,
intraabdominal infections; HAP, hospital-acquired pneumonia; ESBL, extended- an international consensus document has been developed very
spectrum β-lactamases; HCAP, healthcare-associated pneumonia; metallo-β-
lactamases (MBL); mMITT, microbiological intent-to-treat; OMPTA, outer
recently, for guiding the proper use of polymyxins on all those
membrane protein targeting antibiotics; LptD, lipopolysaccharide transport occasions (e.g., CRAB infections, CRE and CRPA resistant to
protein D; NP, nosocomial pneumonia. novel BL-BLI) when they still remain essential (12).
Frontiers in Medicine | www.frontiersin.org 2 April 2019 | Volume 6 | Article 74
Bassetti et al. Gram-Negative Bacteria Infection Treatment
FIGURE 1 | Current clinical reasoning for the treatment of serious MDR-GNB infections in critically-ill patients. MDR-GNB, Multi-drug resistant Gram-negative
bacteria; CRE, carbapenem-resistant Enterobacterales; CRPA, carbapenem-resistant Pseudomonas aeruginosa; CRAB, carbapenem-resistant Acinetobacter
baumannii; BL-BLI, β-lactam/β-lactamase inhibitors; VAP, ventilator-associated pneumonia.
Aminoglycosides Tigecycline
Aminoglycosides are concentration-dependent, bactericidal Tigecycline, a glycylcycline antibiotic which binds to the bacterial
agents which inhibit the bacterial S30 ribosomal subunit. They 30S ribosomal subunit, usually display activity against CRE
have been frequently used in recent years for the treatment and CRAB, but not CRPA, since P. aeruginosa is inherently
of various carbapenem-resistant GNB, frequently in case resistant (23). Tigecycline has been used in combination with
of polymyxin resistance (15, 16). However, very similar to other agents for the treatment of severe CRE and CRAB
polymyxins, two factors hamper the effective use of classical infections, based mainly on favorable in vitro studies and
aminoglycosides (i.e., gentamicin, amikacin, tobramycin) for the observational experiences (24, 25). Of note, caution is needed
treatment of MDR-GNB infections: (i) potential nephrotoxicity in using tigecycline for ventilator-associated pneumonia (VAP),
and reduced lung concentrations (17); (ii) increasing rates of in line with an FDA warning based on pooled data from
resistance (18). With regard to this latter point, low rates of randomized clinical trials, reporting possible increased mortality
resistance have conversely been reported in vitro for plazomicin, in comparison with other regimens (26). When alternatives are
a novel aminoglycoside derivative of sisomicin, which retains not available and tigecycline is used for pneumonia, higher
stability against several aminoglycoside-modifying enzymes (19). dosages should be employed for achieving sufficient PK/PD
Its activity in vitro seems higher against CRE than against CRPA targets (27).
and CRAB, although possible resistance has been described
in some NDM-1-producing CRE, conferred by co-expression Carbapenems
of plazomicin-inactivating methyltransferases in these strains Although apparently paradoxical, the use of carbapenems in
(5, 20). Plazomicin is currently approved by the Food and Drug combinations with other agents for the treatment of carbapenem-
Administration (FDA) for the treatment of complicated urinary resistant MDR-GNB was frequent in the past (before the
tract infection (cUTI), based on the results of the phase 3 EPIC availability of novel BL-BLI). This approach was based on the
trial, in which superiority of plazomicin vs. meropenem was possibility of achieving sufficient carbapenem concentrations
shown (21). In a smaller randomized study, lower mortality against some resistant organisms with only slightly increased
was observed in patients with severe CRE infections receiving carbapenem MICs, and also because of possible synergistic
plazomicin than in those receiving colistin plus tigecycline effects (28–31). According to the results of large observational
or meropenem, although the evidence was not considered studies, this approach seemed ultimately favorable for severe CRE
substantial to achieve FDA approval for bloodstream infections infections caused by KPC-producing strains, whereas a recent
(BSI) (22). An application has been recently submitted to randomized, controlled trial (RCT) did not find differences in
European Medicines Agency (EMA) for approval of plazomicin survival between meropenem plus colistin vs. colistin alone
for cUTI and other severe infections. for the treatment of severe CRAB infections (10, 11, 32). In
Frontiers in Medicine | www.frontiersin.org 3 April 2019 | Volume 6 | Article 74
Bassetti et al. Gram-Negative Bacteria Infection Treatment
this regard, the high mortality reported in the trial in our patients with limited treatment options. In the double-blind,
opinion further stress the need for novel effective agents against double-dummy TANGO-I trial, meropenem/vaborbactam
CRAB (5). There are very few small observational studies on demonstrated superiority vs. piperacillin/tazobactam for the
carbapenem-including combinations for CRPA, and no firm treatment of cUTI, including acute pyelonephritis (41). The
conclusions can be drawn. open-label TANGO-II trial, in which meropenem/vaborbactam
was compared with best therapy available for CRE infections,
Fosfomycin was terminated early because of demonstrated superiority of
Fosfomycin is an analog of phosphoenolpyruvate which meropenem/vaborbactam. Patients had mostly bacteremia,
interferes with the formation of UDP N-acetylmuramic acid, a and rates of clinical cure were 65.6% in patients treated
peptidoglycan precursor. Its intravenous formulation has been with meropenem/vaborbactam (21/32) and 33.3% in those
used for the treatment of MDR-GNB, often in combinations receiving the comparators (5/15) (42). Against this backdrop,
with other agents, when few or none active alternatives were meropenem/vaborbactam is another novel and very effective
available (16, 33). In a small RCT including 94 patients with option for KPC-producing CRE. Nonetheless, similarly to
CRAB infections treated with colistin plus fosfomycin vs. colistin ceftazidime/avibactam, it should be used wisely, since resistance
alone, higher rates of microbiological response were observed might develop (although possibly less frequently) (6, 9). In this
in the combination arm, but no appreciable differences were light, we think future therapeutic algorithms for CRE infections
observed in survival time (34). In a small series of 48 critically-ill should carefully take into account the peculiar characteristics
patients with MDR-GNB infections who received fosfomycin and spectrum of activity of each of these two novel compounds,
(mostly in combination with tigecycline or colistin) at the dosage in order to maximize the effectiveness of anti-CRE therapies in
of 8 g every 8 h for 14 days, all-cause 28-day mortality was 37.5% each selected situation, as well as to preserve the activity of both
(35). In our opinion, because of the absence of larger studies and drugs in the long-term.
the reported risk of rapid selection of resistance, it might still be
prudent to reserve the use of fosfomycin for selected cases (16). Ceftolozane/Tazobactam
Ceftolozane/tazobactam is probably the novel, available BL-BLI
Ceftazidime/Avibactam with the most potent in vitro activity against CRPA (although
Ceftazidime/avibactam is a recently marketed BL-BLI not against carbapenemase-producing strains), whereas it is not
combination which is active against class A (e.g., KPC) active against CRE (43). Ceftolozane/tazobactam is approved
and class D (e.g., OXA) carbapenemase-producing CRE, by FDA and EMA for the treatment of cIAI and cUTI on the
and demonstrated activity against some CRPA isolates basis of the ASPECT-cIAI and ASPECT-cUTI trials (44, 45).
(36). Ceftazidime/avibactam is approved by FDA and EMA However, the most attractive use of ceftolozane/tazobactam at the
for cUTI, complicated intra-abdominal infections (cIAI), present time is perhaps the treatment of CRPA infections, also
hospital-acquired pneumonia (HAP), and VAP. Furthermore, for off-label indications. Indeed, this is confirmed by the growing
ceftazidime/avibactam received approval by EMA for infections amount of observational post-marketing data regarding the use
due to GNB in adults with limited treatment options. Although of ceftolozane/tazobactam for CRPA infections, in turn reflecting
efficacy of ceftazidime-avibactam in randomized clinical trials the frequent lack of more active in-label alternatives (46, 47).
was demonstrated against ceftazidime-resistant isolates, whereas In the future, ceftolozane/tazobactam could receive approval
CRE were not included, its activity against the latter is supported also for HAP and VAP, since achievement of non-inferiority
by the favorable results of observational studies (37–39). For vs. meropenem in the ASPECT-NP trial (NCT02070757) has
example, a lower 30-day mortality was observed among 104 been recently announced (48). Finally, the possibility of using
patients with BSI due to KPC-producing K. pneumoniae BSI ceftolozane/tazobactam as a carbapenem-sparing option for
treated with ceftazidime-avibactam (within the compassionate infections due to extended-spectrum β-lactamases (ESBL)-
use program) than among a matched cohort of 104 patients producing Enterobacterales has also been proposed, that might
receiving other agents (36.5 vs. 55.7%, respectively, p 0.005) be useful in selected scenarios pending confirmatory clinical and
(39). Consequently, ceftazidime/avibactam is an important, economic data (43).
effective, and already available option for the treatment of CRE,
the use of which should be necessarily optimized according Eravacycline
to antimicrobial stewardship principles. Indeed, some cases Eravacycline (TP-434) is a novel synthetic fluorocycline,
of resistance to ceftazidime/avibactam, conferred by blaKPC structurally similar to tigecycline, that has been recently FDA
mutations, have already been reported (8, 40). and EMA approved for the treatment of cIAIs. Eravacycline
has been synthetized to evade many resistance mechanisms
Meropenem/Vaborbactam observed for tetracycline. It has shown to be active against most
Meropenem/vaborbactam is another novel BL-BLI, exerting bacteria expressing the tetracycline targeting efflux channels or
potent and specific activity against class A (e.g., KPC) containing ribosomal protection mechanisms and β-lactamases
carbapenemase-producing CRE. After having received (49). As such, eravacycline has been shown to be broadly active
approval by FDA for cUTI, meropenem/vaborbactam was against Gram-positive, Gram-negative, and anaerobic bacteria
recently approved by EMA for cUTI, cIAI, HAP, VAP, and with the exception of P. aeruginosa and Burkholderia cenopacia
infections due to aerobic Gram-negative organisms in adult (50). Importantly, it has been found to be particularly successful
Frontiers in Medicine | www.frontiersin.org 4 April 2019 | Volume 6 | Article 74
Bassetti et al. Gram-Negative Bacteria Infection Treatment
against CRAB, and in one in vitro study it was the more potent iron and provides to the new drug a unique mechanism
than any drug tested (51). Eravacycline is highly bioavailable of action (58). The catechol side chain binds to ferric iron
after oral administration (more than 90%), has a high metabolic and is actively transported across the outer membrane via
stability and low potential drug-drug interactions. It can also be the bacterial iron transporters, which are up-regulated during
administered intravenously (51). host immune response to acute infection (58). In addition,
Clinically, eravacycline has been studies in four phase 3 cefiderocol is highly active against all classes of carbapenemase
clinical trials in the setting of cIAI and cUTI with conflicting (59). This combination of efficient cell entry and stability to
results: good performance in cIAI and suboptimal in cUTI. In carbapenemases allows cefiderocol to be highly active against a
the IGNITE 1 study, a randomized, double blind, non-inferiority variety of multidrug or extremely drug resistant gram-negative
trial, intravenous eravacycline at a dose of 1.0 mg/kg every 12 h bacteria, including KPC and VIM producing Enterobacteriaceae,
was compared with ertapenem 1 gr every 24 h. Among patients P. aeruginosa producing MBL, Stenotrophomonas maltophilia,
in the intent-to-treat populations, clinical cures were 86.8% for and A. baumannii producing OXA-type β-lactamase (59).
eravacycline and 87.6% for ertapenem, showing non-inferiority In a multicenter, double-blind phase 2 trial concerning
of eravacycline (52). In the IGNITE 2 (NCT019783938) (53) treatment of cUTI, cefiderocol (2 g every 24 h) was compared
and IGNITE 3 (NCT03032510) (54) eravacycline was compared with imipenem/cilastatin (1 g every 8 h) (60). Overall, 183/252
with levofloxacin and ertapenem, respectively, for the treatment (73%) patients treated with cefiderocol and 65/119 (55%) of
of cUTI. In both studies eravacycline did not reach non- those treated with imipenem-cilastatin met the primary efficacy
inferiority, and issues regarding the possible poor urinary tract endpoint of clinical cure and microbiologic eradication at
penetration have been raised. Another randomized, phase 3 trial test of cure (weighted difference 18.6%, 95% CI 8.2–28.9).
(IGNITE 4) of eravacycline in comparison to meropenem for Moreover, cefiderocol was safe and well tolerated. Only five
the treatment of cIAI demonstrated a favorable microbiological patients (<2%) discontinued cefiderocol because of either C.
response of 88.9 and 100% for eravacycline against infections due difficile, hypersensitivity, increased liver enzyme or diarrhea
to Enterobacteriaceae and A. baumannii, respectively (55). (60). Other two phase 3 clinical trials assessing the efficacy of
In our opinion, eravacycline may offer an important option cefiderocol for nosocomial pneumonia and serious infections
for patients with cIAI caused by MDR-GNB bacteria, including caused by carbapenem- resistant gram negative pathogens are
CRAB. In addition, its high oral bioavailability (>90%) allows for ongoing. The APEKS-NP (NCT03032380) is a randomized,
the switch from an intravenous to an oral formulation. double blind trial comparing all-cause mortality in adult patients
with HAP/VAP due to gram-negative pathogens receiving either
Other Treatment Options cefiderocol or meropenem (both in association with linezolid).
Variable in vitro synergy has been reported for rifampin in The estimated date for completion of the study is June 2019.
combination with other agents for the treatment of MDR-GNB Another randomized, open label phase 3 trial (CREDIBLE-
infections. Possible improvements in microbiological response CR, NCT02714595) has been initiated in 2017 in order to
by adding rifampin were observed in an RCT trial in which provide the evidence of efficacy of cefiderocol in patients with
210 patients with A. baumannii infections were randomized to serious infections (healthcare-associated pneumonia [HCAP],
receive either colistin or colistin plus rifampin (56). However, HAP, VAP, cUTI, and BSI) caused by carbapenem-resistant
similar mortality was observed in the two arms (56). GNB. In this trial, cefiderocol is compared with best available
Omadacycline is an aminomethylcycline recently approved therapy including up to 3 antibacterial agents for carbapenem-
by the FDA for the treatment of community-acquired bacterial resistant GNB with either a polymyxin-based or non-polymyxin-
pneumonia and acute skin and skin structure infections. In based regimen.
vitro activity against some MDR-GNB has been reported (57), Although definitive results from phase 3 trials are still not
although clinical post-marketing experience is needed to clarify available, we believe that cefiderocol represents one of the most
as to whether this drug will have a role in future treatment promising future therapeutic option for infections caused by
algorithms for MDR-GNB. serious carbapenem-resistant MDR-GNB, including CRE, CRPA,
and CRAB.
FUTURE TREATMENT OPTIONS FOR
MDR-GNB IN CRITICALLY-ILL PATIENTS Imipenem/Relebactam
Imipenem/relebactam is a combination of an existing
In this section we will discuss newly antibiotics against MDR carbapenem (imipenem-cilastatin) with a new potent non
Gram-negative pathogens in late stage of development. An β-lactam, bicyclic diazabicyclooctan, β-lactamase inhibitor
example of possible future clinical reasoning for guiding the (relebactam). Structurally related to avibactam, relebactam
choice of antimicrobials to treat MDR-GNB infections in inhibits the activity of class A, and C beta-lactamase, but does
critically-ill patients, also including agents currently in phase 3, not have activity against metallo-β-lactamases (MBL) and class
is shown in Figure 2. D carbapenemases (61). With this profile, relebactam primarily
restores the clinical activity of imipenem against imipenem-
Cefiderocol resistant isolates such as KPC- producing Enterobacteriaceae or
Cefiderocol is a novel siderophore antibiotic with a catechol against P. aeruginosa isolates showing carbapenem resistance
moiety on the third position side chain which chelates free due to porin loss in combination with AmpC expression
Frontiers in Medicine | www.frontiersin.org 5 April 2019 | Volume 6 | Article 74
Bassetti et al. Gram-Negative Bacteria Infection Treatment
FIGURE 2 | Possible future clinical reasoning for the treatment of serious MDR-GNB infections in critically-ill patients. MDR-GNB, Multi-drug resistant Gram-negative
bacteria; CRE, carbapenem-resistant Enterobacterales; CRPA, carbapenem-resistant Pseudomonas aeruginosa; CRAB, carbapenem-resistant Acinetobacter
baumannii; VAP, ventilator-associated pneumonia.
(62, 63). However, imipenem/relebactam is not active against who received imipenem/relebactam had a drug-related adverse
imipenem-resistant Enterobacteriaceae producing VIM, IMP, or event (16.1 vs. 31.3%, p = 0.001), including treatment-
NDM type of MBL as well as against A. baumannii, or IMP- or emergent nephrotoxicity (10 vs. 56%, p = 0.001). A second
VIM-producing P. aeruginosa (62). pivotal phase 3 trial (RESTORE-IMI2) comparing the efficacy
Relebactam’ s safety, tolerability, and efficacy have been of imipenem/relebactam with piperacillin/tazobactam for the
originally studied in two phase 2 clinical trials including patients treatment of HAP and VAP is currently ongoing (NCT02493764).
with cIAI or with cUTI. In those studies, the combination
of imipenem (500 mg every 6 h) with relebactam at different Murepavadin
dosage (125 mg every 6 h and 250 mg every 6 h) was non-inferior Murepavadin (POL7080) is a protein epitope mimetic that
to imipenem alone. Indeed, imipenem/relebactam showed high belongs to a new class of antibiotics called outer membrane
clinical response (>96%) in both infections and for both protein targeting antibiotics (OMPTA). It possesses a novel, non-
dosages (61, 64). In addition, the two doses (125 mg every 6 h lytic mechanism of action that targets the lipopolysaccharide
and 250 mg every 6 h) of relebactam were well tolerated and transport protein D (LptD), involved in lipopolysaccharide
imipenem/relebactam had the same safety profile compared with biogenesis of the outer membrane of P. aeruginosa (66).
imipenem-cilastatin alone. Therefore, murepavadin is highly active against P. aeruginosa
The RESTORE-IMI1 study was a multicenter, randomized, (66) with an expected limited impact on normal gastrointestinal
double-blind trial designed to assess the safety and efficacy of flora or resistance selection in other bacterial pathogens. In
imipenem/relebactam compared with colistin plus imipenem for vitro, it has demonstrated potent antimicrobial activity against
treating patients with HAP/VAP, cIAI or cUTI due to imipenem- P. aeruginosa, including carbapenemase-producing, colistin-
non-susceptible bacteria (but colistin and imipenem/relebactam- resistant, extremely drug-resistant and pan drug-resistant
susceptible). A favorable overall response for each different isolates (67, 68) and other tested Pseudomonas species, but
infection type in microbiological intent-to-treat (mMITT) is not active against other non-fermenting Gram-negative
population was evaluated as a primary endpoint. Preliminary pathogens or Enterobacteriaceae (69). The drug has a high
results from the RESTORE-IMI1 trial have been recently volume of tissue distribution with linear and dose-proportional
presented (65). In the mMITT population, the favorable pharmacokinetics, and a half-life of 2–5 h (69).
overall response was similar in the imipenem/relebactam arm Clinically, murepavadin has been studied in patients with
(n = 15; 71.4%) and the colistin plus imipenem arm (n VAP due to suspected or documented P. aeruginosa. In
= 7; 70%). At day 28, imipenem/relebactam was associated an open-label phase 2 study, murepavadin plus standard
with higher favorable clinical response (71.4 vs. 40%) and of care was administered in 25 patients with suspected of
lower all-cause mortality (9.5 vs. 30%) compared with colistin confirmed P. aeruginosa VAP (NCT02096328). Among 12
plus imipenem. Moreover, in a safety analysis, fewer patients patients with confirmed P. aeruginosa VAP (nine of which
Frontiers in Medicine | www.frontiersin.org 6 April 2019 | Volume 6 | Article 74
Bassetti et al. Gram-Negative Bacteria Infection Treatment
the infection was caused by a MDR or extremely drug- could represent another precious addition to the clinicians’
resistant isolate), clinical cure was achieved in 91% of the armamentarium in the future. For example, cefepime/zidebactam
patients at test of cure and 28-day all-cause mortality was of has shown promising activity against CRE, CRPA, and CRAB,
8%, far below the 20–40% expected mortality rate (70). No and both cefepime/zidebactam and meropenem/nacubactam
development of treatment-emergent resistance to murepavadin have demonstrated in vitro activity against MBL-producing
was observed during the study. The PRISM-UDR trial assessing CRE (5, 72–76). Ceftaroline/avibactam, cefepime/AAI101, TP-
the efficacy of murepavadin with ertapenem in the treatment 6076, VNXR-5133, WCK-5153, MEDI3902, COT-143, and RX-
of nosocomial pneumonia (NCT03582007) and the PRIMS- P2382 are other promising agents to be further evaluated for
MDR trial comparing murepavadin plus one anti-pseudomonas their activity against MDR-GNB during clinical development
antibiotic with two anti-pseudomonas antibiotics for VAP are (5, 77, 78).
ongoing (NCT03409679).
In conclusion, if the promising results observed in phase CONCLUSIONS
2 trials will be confirmed in phase 3 studies, murepavadin
could represent an important option in combination with other The treatment of MDR-GNB infections in critically ill patients
antibiotics for empirical treatment in patients with strong risk presents many challenges: (i) an effective treatment should
factors for P. aeruginosa infections, as well as for targeted be administered as soon as possible, but resistance to many
treatment. Efficacy data for other type of infection, including antimicrobial classes invariably reduces the probability of
bloodstream infections, cUTI or cIAI, are clearly needed. adequate empirical coverage, with possible unfavorable
consequences; (ii) there is an increasing need for rapid
Aztreonam/Avibactam diagnostics and efficient laboratory workflows to anticipating
Aztreonam is the only available monobactam antibiotic that has diagnosis rapidly narrowing the antimicrobial spectrum, in line
been approved for treatment of gram infection since 1986. It is with antimicrobial stewardship principles; (ii) infection-control
active against MBL-producing bacteria, but it is hydrolyzed by initiatives are also of paramount important, since CRE, CRPA,
Ambler class A beta-lactamases (e.g., ESBL and KPCs) and class and CRAB are being reported with increasing frequencies
C (e.g., AmpC) beta-lactamases. Therefore, the combination of worldwide, although with important variability across regions
aztreonam with avibactam is able to inhibit cell wall synthesis in and even hospitals.
MBL-producing strains despite the presence of other co-carried Novel treatment options have become available in recent
beta-lactamases or carbapenemases (59). Aztreonam/avibactam years, providing some much-awaited resources for effectively
showed a potent in-vitro activity against ESBL, class C b- counteracting some severe MDR-GNB infections. However, their
lactamase, MBL, and KPC-producing strains with an activity 10 optimal use should be guaranteed in the long term, for delaying
times that of aztreonam alone. Despite this, limited activity has as much as possible the emergence and diffusion of resistance to
been shown against A. baumannii or P. aeruginosa compared novel agents. Despite important progresses, PK/PD optimization
with aztreonam alone (59). of dosages and treatment duration in critically ill patients has
A phase III clinical trial to compare aztreonam/avibactam still some areas of uncertainty requiring further study, that
(with or without metronidazole) with meropenem (with or should take into account also resistance selection as a major
without colistin) for the treatment of HAP, VAP, and cIAI due endpoint. Treatment of severe MDR-GNB infections in critically
to Gram-negative bacteria for which there are limited, or no ill patients in the near future will require an expert and complex
treatment options is ongoing (REVISIT study, NCT03329092). clinical reasoning, of course taking into account the peculiar
Another phase 3 study to determine the efficacy, safety, and characteristics of the target population, but also the need for
tolerability of aztreonam/avibactam vs. best available therapy in adequate empirical coverage and the more and more specific
the treatment of serious infections (cIAI, NP, HAP, VAP, cUTI, enzyme-level activity of novel antimicrobials with respect to the
or BSI) due to MBL–producing Gram-negative bacteria will be different resistance mechanisms of MDR-GNB.
performed starting in April 2020 (NCT03580044).
Aztreonam/avibactam may represent an interesting AUTHOR CONTRIBUTIONS
alternative for infections caused by MBL-producing strains.
All authors contributed equally to the conception and overview
Agents in Earlier Stages of Development of the manuscript content, and also contributed equally to the
Agents in earlier stages of development are not the focus of writing of the manuscript. In addition, MB provided critical
the present review and have been comprehensively summarized revision for intellectual content, and oversight. All the authors
elsewhere (5, 71). Nonetheless, it should be reminded that they approved the final version of the manuscript.
REFERENCES 2. Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos
GL, Cormican M, et al. Clinical epidemiology of the global
1. Bassetti M, Welte T, Wunderink RG. Treatment of Gram-negative pneumonia expansion of Klebsiella pneumoniae carbapenemases. Lancet
in the critical care setting: is the beta-lactam antibiotic backbone broken Infect Dis. (2013) 13:785–96. doi: 10.1016/S1473-3099(13)
beyond repair? Crit Care. (2016) 20:19. doi: 10.1186/s13054-016-1197-5 70190-7
Frontiers in Medicine | www.frontiersin.org 7 April 2019 | Volume 6 | Article 74
Bassetti et al. Gram-Negative Bacteria Infection Treatment
3. Giacobbe DR, di Masi A, Leboffe L, Del Bono V, Rossi M, Cappiello D, retrospective cohort analysis of prevalence, predictors, and outcome of
et al. Hypoalbuminemia as a predictor of acute kidney injury during colistin resistance to all first-line agents. Clin Infect Dis. (2018) 67:1803–14.
treatment. Sci Rep. (2018) 8:11968. doi: 10.1038/s41598-018-30361-5 doi: 10.1093/cid/ciy378
4. Garonzik SM, Li J, Thamlikitkul V, Paterson DL, Shoham S, Jacob J, 19. Zhanel GG, Lawson CD, Zelenitsky S, Findlay B, Schweizer F, Adam H,
et al. Population pharmacokinetics of colistin methanesulfonate and formed et al. Comparison of the next-generation aminoglycoside plazomicin to
colistin in critically ill patients from a multicenter study provide dosing gentamicin, tobramycin and amikacin. Expert Rev Anti Infect Ther. (2012)
suggestions for various categories of patients. Antimicrob Agents Chemother. 10:459–73. doi: 10.1586/eri.12.25
(2011) 55:3284–94. doi: 10.1128/AAC.01733-10 20. Livermore DM, Mushtaq S, Warner M, Zhang JC, Maharjan S, Doumith M,
5. Giacobbe DR, Mikulska M, Viscoli C. Recent advances in the et al. Activity of aminoglycosides, including ACHN-490, against carbapenem-
pharmacological management of infections due to multidrug resistant resistant Enterobacteriaceae isolates. J Antimicrob Chemother. (2011) 66:48–
gram-negative bacteria. Expert Rev Clin Pharmacol. (2018) 11:1219–36. 53. doi: 10.1093/jac/dkq408
doi: 10.1080/17512433.2018.1549487 21. Cloutier DJ, Miller LG, Komirenko AS, et al. Plazomicin Versus
6. Pogue JM, Bonomo RA, Kaye KS. Ceftazidime/avibactam, Meropenem for the Treatment of Complicated Urinary Tract Infection
Meropenem/vaborbactam or both? Clinical and formulary considerations. and Acute Pyelonephritis: Results of the EPIC Study. (Vienna) (2017).
Clin Infect Dis. (2018) 68:519–24. doi: 10.1093/cid/ciy576 doi: 10.1056/NEJMoa1801467
7. Bassetti M, Righi E, Vena A, Graziano E, Russo A, Peghin M. Risk 22. Wagenlehner FME, Cloutier DJ, Komirenko AS, Cebrik DS, Krause KM,
stratification and treatment of ICU-acquired pneumonia caused by Keepers TR, et al. Once-daily plazomicin for complicated urinary tract
multidrug- resistant/extensively drug-resistant/pandrug-resistant bacteria. infections. N Engl J Med. (2019) 380:729–40. doi: 10.1056/NEJMoa1801467
Curr Opin Crit Care. (2018) 24:385–93. doi: 10.1097/MCC.0000000000000534 23. Pankey GA. Tigecycline. Antimicrob Chemother. (2005) 56:470–80.
8. Shields RK, Chen L, Cheng S, Chavda KD, Press EG, Snyder A, et al. doi: 10.1093/jac/dki248
Emergence of ceftazidime-avibactam resistance due to plasmid-borne 24. Rao GG, Ly NS, Diep J, Forrest A, Bulitta JB, Holden PN, et al
blaKPC-3 Mutations during Treatment of Carbapenem-Resistant Klebsiella Combinatorial pharmacodynamics of polymyxin B and tigecycline against
pneumoniae Infections. Antimicrob Agents Chemother. (2017) 61: e02097–16. heteroresistant Acinetobacter baumannii. Int J Antimicrob Agents. (2016)
doi: 10.1128/AAC.02097-16 48:331–6. doi: 10.1016/j.ijantimicag.2016.06.006
9. Sun D, Rubio-Aparicio D, Nelson K, Dudley MN, Lomovskaya O. 25. Tumbarello M, Viale P, Viscoli C, Trecarichi EM, Tumietto F, Marchese
Meropenem-vaborbactam resistance selection, resistance prevention, A, et al. Predictors of mortality in bloodstream infections caused
and molecular mechanisms in mutants of KPC-producing klebsiella by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae:
pneumoniae. Antimicrob Agents Chemother. (2017) 61:e01694–17. importance of combination therapy. Clin Infect Dis. (2012) 55:943–50.
doi: 10.1128/AAC.01694-17 doi: 10.1093/cid/cis588
10. Daikos GL, Tsaousi S, Tzouvelekis LS, Anyfantis I, Psichogiou M, 26. FDA Drug Safety Communication. FDA Warns of Increased Risk of Death
Argyropoulou A, et al. Carbapenemase-producing Klebsiella pneumoniae With IV Antibacterial Tygacil (tigecycline) and Approves New Boxed Warning.
bloodstream infections: lowering mortality by antibiotic combination Available online at: https://www.fda.gov/Drugs/DrugSafety/default.htm
schemes and the role of carbapenems. Antimicrob Agents Chemother. (2014) 27. Wiskirchen DE, Koomanachai P, Nicasio AM, Nicolau DP, Kuti JL. In
58:2322–8. doi: 10.1128/AAC.02166-13 vitro pharmacodynamics of simulated pulmonary exposures of tigecycline
11. Tumbarello M, Trecarichi EM, De Rosa FG, Giannella M, Giacobbe DR, alone and in combination against Klebsiella pneumoniae isolates producing
Bassetti M, et al. Infections caused by KPC-producing Klebsiella pneumoniae: a KPC carbapenemase. Antimicrob Agents Chemother. (2011) 55:1420–7.
differences in therapy and mortality in a multicentre study. J Antimicrob doi: 10.1128/AAC.01253-10
Chemother. (2015) 70:2133–43. doi: 10.1093/jac/dkv086 28. Cancelli F, Oliva A, De Angelis M, Mascellino MT, Mastroianni CM, Vullo
12. Tsuji BT, Pogue JM, Zavascki AP, Paul M, Daikos GL, Forrest A, et al. V. Role of double-carbapenem regimen in the treatment of infections
International consensus guidelines for the optimal use of the polymyxins: due to carbapenemase producing carbapenem-resistant enterobacteriaceae:
endorsed by the American College of Clinical Pharmacy (ACCP), European a single-center, observational study. Biomed Res Int. (2018) 2018:2785696.
Society of Clinical Microbiology and Infectious Diseases (ESCMID), doi: 10.1155/2018/2785696
Infectious Diseases Society of America (IDSA), International Society for Anti- 29. Del Bono V, Giacobbe DR, Marchese A, Parisini A, Fucile C, Coppo E, et al.
infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), Meropenem for treating KPC-producing Klebsiella pneumoniae bloodstream
and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy. infections: Should we get to the PK/PD root of the paradox? Virulence. (2017)
(2019) 39:10–39. doi: 10.1002/phar.2209 8:66–73. doi: 10.1080/21505594.2016.1213476
13. Giacobbe DR, Del Bono V, Trecarichi EM, De Rosa FG, Giannella M, 30. Pea F, Della Siega P, Cojutti P, Sartor A, Crapis M, Scarparo C, et al.
Bassetti M, et al. Risk factors for bloodstream infections due to colistin- Might real-time pharmacokinetic/pharmacodynamic optimisation of high-
resistant KPC-producing Klebsiella pneumoniae: results from a multicenter dose continuous-infusion meropenem improve clinical cure in infections
case-control-control study. Clin Microbiol Infect. (2015) 21:1106.e1–8. caused by KPC-producing Klebsiella pneumoniae? Int J Antimicrob Agents.
doi: 10.1016/j.cmi.2015.08.001 (2017) 49:255–8. doi: 10.1016/j.ijantimicag.2016.10.018
14. Giamarellou H. Epidemiology of infections caused by polymyxin- 31. Zusman O, Avni T, Leibovici L, Adler A, Friberg L, Stergiopoulou
resistant pathogens. Int J Antimicrob Agents. (2016) 48:614–21. T, et al. Systematic review and meta-analysis of in vitro synergy of
doi: 10.1016/j.ijantimicag.2016.09.025 polymyxins and carbapenems. Antimicrob Agents Chemother. (2013) 57:5104–
15. Gonzalez-Padilla M, Torre-Cisneros J, Rivera-Espinar F, Pontes-Moreno 11. doi: 10.1128/AAC.01230-13
A, Lopez-Cerero L, Pascual A, et al. Gentamicin therapy for sepsis due 32. Paul M, Daikos GL, Durante-Mangoni E, Yahav D, Carmeli Y, Benattar
to carbapenem-resistant and colistin-resistant Klebsiella pneumoniae. J YD, et al. Colistin alone versus colistin plus meropenem for treatment of
Antimicrob Chemother. (2015) 70:905–13. doi: 10.1093/jac/dku432 severe infections caused by carbapenem-resistant Gram-negative bacteria: an
16. Bassetti M, Giacobbe DR, Giamarellou H, Viscoli C, Daikos GL, Dimopoulos open-label, randomised controlled trial. Lancet Infect Dis. (2018) 18:391–400.
G, et al. Management of KPC-producing Klebsiella pneumoniae infections. doi: 10.1016/S1473-3099(18)30099-9
Clin Microbiol Infect. (2018) 24:133–44. doi: 10.1016/j.cmi.2017.08.030 33. Grabein B, Graninger W, Rodriguez Bano J, Dinh A, Liesenfeld DB.
17. Panidis D, Markantonis SL, Boutzouka E, Karatzas S, Baltopoulos G. Intravenous fosfomycin-back to the future. Systematic review and meta-
Penetration of gentamicin into the alveolar lining fluid of critically ill analysis of the clinical literature. Clin Microbiol Infect. (2017) 23:363–72.
patients with ventilator-associated pneumonia. Chest. (2005) 128:545–52. doi: 10.1016/j.cmi.2016.12.005
doi: 10.1378/chest.128.2.545 34. Sirijatuphat R, Thamlikitkul V. Preliminary study of colistin versus
18. Kadri SS, Adjemian J, Lai YL, Spaulding AB, Ricotta E, Prevots DR, et al. colistin plus fosfomycin for treatment of carbapenem-resistant Acinetobacter
National institutes of health antimicrobial resistance outcomes research, baumannii infections. Antimicrob Agents Chemother. (2014) 58:5598–601.
difficult-to-treat resistance in gram-negative bacteremia at 173 US hospitals: doi: 10.1128/AAC.02435-13
Frontiers in Medicine | www.frontiersin.org 8 April 2019 | Volume 6 | Article 74
Bassetti et al. Gram-Negative Bacteria Infection Treatment
35. Pontikis K, Karaiskos I, Bastani S, Dimopoulos G, Kalogirou M, Katsiari community pathogens. Antimicrob Agents Chemother. (2013) 57:5548–58.
M, et al. Outcomes of critically ill intensive care unit patients treated with doi: 10.1128/AAC.01288-13
fosfomycin for infections due to pandrug-resistant and extensively drug- 50. Bassetti M, Righi E, Carnelutti A. New therapeutic options for
resistant carbapenemase-producing Gram-negative bacteria. Int J Antimicrob respiratory tract infections. Curr Opin Infect Dis. (2016) 29:178–86.
Agents. (2014) 43:52–9. doi: 10.1016/j.ijantimicag.2013.09.010 doi: 10.1097/QCO.0000000000000251
36. Montravers P, Bassetti M. The ideal patient profile for new beta- 51. Seifert H, Stefanik D, Sutcliffe JA, Higgins PG. In-vitro activity of the
lactam/beta-lactamase inhibitors. Curr Opin Infect Dis. (2018) 31:587–93. novel fluorocycline eravacycline against carbapenem non-susceptible
doi: 10.1097/QCO.0000000000000490 Acinetobacter baumannii. Int J Antimicrob Agents. (2018) 51:62–4.
37. Carmeli Y, Armstrong J, Laud PJ, Newell P, Stone G, Wardman doi: 10.1016/j.ijantimicag.2017.06.022
A, et al. Ceftazidime-avibactam or best available therapy in patients 52. Solomkin J, Evans D, Slepavicius A, Lee P, Marsh A, Tsai L, et al. Assessing
with ceftazidime-resistant Enterobacteriaceae and Pseudomonas aeruginosa the efficacy and safety of eravacycline vs ertapenem in complicated intra-
complicated urinary tract infections or complicated intra-abdominal abdominal infections in the Investigating Gram-Negative Infections Treated
infections (REPRISE): a randomised, pathogen-directed, phase 3 study. Lancet With Eravacycline (IGNITE 1) trial: a randomized clinical trial. JAMA Surg.
Infect Dis. (2016) 16:661–73. doi: 10.1016/S1473-3099(16)30004-4 (2017) 152:224–32. doi: 10.1001/jamasurg.2016.4237
38. Shields RK, Nguyen MH, Chen L, Press EG, Potoski BA, Marini RV, 53. IGNITE2. Eravacycline Inferior to Levofloxacin, but IV Formulation Shows
et al. Ceftazidime-avibactam is superior to other treatment regimens against Promise Healio. Available online at: https://www.healio.com
carbapenem-resistant klebsiella pneumoniae bacteremia. Antimicrob Agents 54. Tetraphase Announces Top-Line Results From IGNITE3 Phase 3 Clinical Trial
Chemother. (2017) 61:e00883–17. doi: 10.1128/AAC.00883-17 of Eravacycline in Complicated Urinary Tract Infections (cUTI). Tetraphase.
39. Tumbarello M, Trecarichi EM, Corona A, De Rosa FG, Bassetti M, Mussini Available online at: https://ir.tphase.com/news-releases/news-release-details/
C, et al. Efficacy of ceftazidime-avibactam salvage therapy in patients with tetraphase-announces-top-line-results-ignite3-phase-3-clinical
infections caused by KPC-producing klebsiella pneumoniae. Clin Infect Dis. 55. Solomkin JS, Gardovskis J, Lawrence K, Montravers P, Sway A, Evans D, et al.
(2019) 68:355–64. doi: 10.1093/cid/ciy492 IGNITE4: results of a phase 3, randomized, multicenter, prospective trial of
40. Gaibani P, Campoli C, Lewis RE, Volpe SL, Scaltriti E, Giannella M, eravacycline vs. meropenem in the treatment of complicated intra-abdominal
et al. In vivo evolution of resistant subpopulations of KPC-producing infections. Clin Infect Dis. (2018). doi: 10.1093/cid/ciy1029
Klebsiella pneumoniae during ceftazidime/avibactam treatment. J Antimicrob 56. Durante-Mangoni E, Signoriello G, Andini R, Mattei A, De Cristoforo M,
Chemother. (2018) 73:1525–9. doi: 10.1093/jac/dky082 Murino P, et al. Colistin and rifampicin compared with colistin alone for the
41. Kaye KS, Bhowmick T, Metallidis S, Bleasdale SC, Sagan OS, Stus V, et al. treatment of serious infections due to extensively drug-resistant Acinetobacter
Effect of meropenem-vaborbactam vs piperacillin-tazobactam on clinical cure baumannii: a multicenter, randomized clinical trial. Clin Infect Dis. (2013)
or improvement and microbial eradication in complicated urinary tract 57:349–58. doi: 10.1093/cid/cit253
infection: the TANGO I randomized clinical trial. JAMA. (2018) 319:788–99. 57. Pfaller MA, Huband MD, Rhomberg PR, Flamm RK. Surveillance of
doi: 10.1001/jama.2018.0438 omadacycline activity against clinical isolates from a global collection
42. Wunderink RG, Giamarellos-Bourboulis EJ, Rahav G, Mathers AJ, Bassetti M, (North America, Europe, Latin America, Asia-Western Pacific),
Vazquez J, et al. Effect and safety of meropenem-vaborbactam versus best- 2010-2011. Antimicrob Agents Chemother. (2017) 61:e00018–17.
available therapy in patients with carbapenem-resistant enterobacteriaceae doi: 10.1128/AAC.00018-17
infections: the TANGO Ii randomized clinical trial. Infect Dis Ther. (2018) 58. Ito A, Nishikawa T, Matsumoto S, Yoshizawa H, Sato T, Nakamura R, et al.
7:439–455. doi: 10.1007/s40121-018-0214-1 Siderophore cephalosporin cefiderocol utilizes ferric iron transporter systems
43. Giacobbe DR, Bassetti M, De Rosa FG, Del Bono V, Grossi PA, Menichetti F, for antibacterial activity against pseudomonas aeruginosa. Antimicrob Agents
et al. Ceftolozane/tazobactam: place in therapy. Expert Rev Anti Infect Ther. Chemother. (2016) 60:7396–401. doi: 10.1128/AAC.01405-16
(2018) 16:1–14. doi: 10.1080/14787210.2018.1447381 59. Wright H, Bonomo RA, Paterson DL. New agents for the treatment of
44. Solomkin J, Hershberger E, Miller B, Popejoy M, Friedland I, Steenbergen infections with Gram-negative bacteria: restoring the miracle or false dawn?
J, et al. Ceftolozane/tazobactam plus metronidazole for complicated intra- Clin Microbiol Infect. (2017) 23:704–12. doi: 10.1016/j.cmi.2017.09.001
abdominal infections in an era of multidrug resistance: results from a 60. Portsmouth S, van Veenhuyzen D, Echols R, Machida M, Ferreira JCA,
randomized, double-blind, phase 3 trial. (ASPECT-cIAI). Clin Infect Dis. Ariyasu M, et al. Cefiderocol versus imipenem-cilastatin for the treatment of
(2015) 60:1462–71. doi: 10.1093/cid/civ097 complicated urinary tract infections caused by Gram-negative uropathogens:
45. Wagenlehner FM, Umeh O, Steenbergen J, Yuan G, Darouiche RO. a phase 2, randomised, double-blind, non-inferiority trial. Lancet Infect Dis.
Ceftolozane-tazobactam compared with levofloxacin in the treatment of (2018) 18:1319–28. doi: 10.1016/S1473-3099(18)30554-1
complicated urinary-tract infections, including pyelonephritis: a randomised, 61. Lucasti C, Vasile L, Sandesc D, Venskutonis D, McLeroth P, Lala M, et al. Phase
double-blind, phase 3 trial (ASPECT-cUTI). Lancet. (2015) 385:1949–56. 2, dose-ranging study of relebactam with imipenem-cilastatin in subjects with
doi: 10.1016/S0140-6736(14)62220-0 complicated intra-abdominal infection. Antimicrob Agents Chemother. (2016)
46. Bassetti M, Castaldo N, Cattelan A, Mussini C, Righi E, Tascini C, et al. 60:6234–43. doi: 10.1128/AAC.00633-16
Ceftolozane/tazobactam for the treatment of serious P. aeruginosa infections: 62. Livermore DM, Warner M, Mushtaq S. Activity of MK-7655 combined
a multicenter nationwide clinical experience. Int J Antimicrob Agents. (2018) with imipenem against Enterobacteriaceae and Pseudomonas aeruginosa. J
5:ofy280. doi: 10.1016/j.ijantimicag.2018.11.001 Antimicrob Chemother. (2013) 68:2286–90. doi: 10.1093/jac/dkt178
47. Munita JM, Aitken SL, Miller WR, Perez F, Rosa R, Shimose LA, et al. 63. Olsen I. New promising beta-lactamase inhibitors for clinical use. Eur
Multicenter evaluation of ceftolozane/tazobactam for serious infections J Clin Microbiol Infect Dis. (2015) 34:1303–8. doi: 10.1007/s10096-015-
caused by carbapenem-resistant pseudomonas aeruginosa. Clin Infect Dis. 2375-0
(2017) 65:158–61. doi: 10.1093/cid/cix014 64. Sims M, Mariyanovski V, McLeroth P, Akers W, Lee YC, Brown ML,
48. Merck’s ZERBAXA
R
(ceftolozane and tazobactam). Met Primary Endpoints et al. Prospective, randomized, double-blind, Phase 2 dose-ranging
of Non-Inferiority Compared to Meropenem in Pivotal Phase 3 Study of Adult study comparing efficacy and safety of imipenem/cilastatin plus
Patients with Hospital-Acquired Bacterial Pneumonia or Ventilator-Associated relebactam with imipenem/cilastatin alone in patients with complicated
Bacterial Pneumonia. Available onlinev at: https://investors.merck.com/news/ urinary tract infections. J Antimicrob Chemother. (2017) 72:2616–26.
press-release-details/2018/Mercks-ZERBAXA-ceftolozane-and-tazobactam- doi: 10.1093/jac/dkx139
Met-Primary-Endpoints-of-Non-Inferiority-Compared-to-Meropenem- 65. Motsch J, de Oliveira C, Stus V, Koksal I, Lyulko O, Boucher H, et al.
in-Pivotal-Phase-3-Study-of-Adult-Patients-with-Hospital-Acquired- RESTORE-IMI 1: a multicenter, randomized, double-blind, comparator-
Bacterial-Pneumonia-or-Ventilator-Associated-Bacterial-Pneumonia/ controlled trial comparing the efficacy and safety of imipenem/relebactam
default.aspx versus colistin plus imipenem in patients with imipenem-non-susceptible
49. Sutcliffe JA, O’Brien W, Fyfe C, Grossman TH. Antibacterial activity bacterial infections. In: Presented in 28th European Congress of Clinical
of eravacycline (TP-434), a novel fluorocycline, against hospital and Microbiology and Infectious Diseases (ECCMID). Madrid (2018).
Frontiers in Medicine | www.frontiersin.org 9 April 2019 | Volume 6 | Article 74
Bassetti et al. Gram-Negative Bacteria Infection Treatment
66. Srinivas N, Jetter P, Ueberbacher BJ, Werneburg M, Zerbe K, 75. Sader HS, Rhomberg PR, Flamm RK, Jones RN, Castanheira M. WCK 5222
Steinmann JB, et al. Peptidomimetic antibiotics target outer-membrane (cefepime/zidebactam) antimicrobial activity tested againstGram-negative
biogenesis in Pseudomonas aeruginosa. Science. (2010) 327:1010–3. organisms producing clinically relevant beta-lactamases. J Antimicrob
doi: 10.1126/science.1182749 Chemother. (2017) 72:1696–703. doi: 10.1093/jac/dkx050
67. Sader HS, Dale GE, Rhomberg PR, Flamm RK. Antimicrobial activity of 76. Mushtaq S, Vickers A, Woodford N, Haldimann A, Livermore DM.
murepavadin tested against clinical isolates of pseudomonas aeruginosa from Activity of nacubactam (RG6080/OP0595) combinations against MBL-
the United States, Europe, and China. Antimicrob Agents Chemother. (2018) producing Enterobacteriaceae. J Antimicrob Chemother. (2018) 74:953–60.
62:e00311–18. doi: 10.1128/AAC.00311-18 doi: 10.1093/jac/dky522
68. Sader HS, Flamm RK, Dale GE, Rhomberg PR, Castanheira M. Murepavadin 77. Castanheira M, Williams G, Jones RN, Sader HS. Activity of ceftaroline-
activity tested against contemporary. (2016-17) clinical isolates of XDR avibactam tested against contemporary Enterobacteriaceae isolates carrying
Pseudomonas aeruginosa. J Antimicrob Chemother. (2018) 73:2400–04. beta-lactamases prevalent in the United States. Microb Drug Resist. (2014)
doi: 10.1093/jac/dky227 20:436–40. doi: 10.1089/mdr.2013.0181
69. Martin-Loeches I, Dale GE, Torres A. Murepavadin: a new antibiotic 78. Crandon JL, Nicolau DP. In vivo activities of simulated human doses
class in the pipeline. Expert Rev Anti Infect Ther. (2018) 16:259–268. of cefepime and cefepime-AAI101 against multidrug-resistant Gram-
doi: 10.1080/14787210.2018.1441024 negative Enterobacteriaceae. Antimicrob Agents Chemother. (2015) 59:2688–
70. Armagantis A, Zakynthinos S, Mandragos C, et al. ISICEM 2017, Poster 94. doi: 10.1128/AAC.00033-15
A459. Brussels.
71. Bassetti M, Righi E, Russo A, Carnelutti A. New antibiotics for pneumonia. Conflict of Interest Statement: Outside the submitted work, MB has received
Clin Chest Med. (2018) 39:853–69. doi: 10.1016/j.ccm.2018.08.007 funding for scientific advisory boards, travel and speaker honoraria from Angelini,
72. Moya B, Barcelo IM, Bhagwat S, Patel M, Bou G, Papp-Wallace KM, AstraZeneca, Bayer, Cidara, Cubist, Pfizer, Menarini, MSD, Nabriva, Paratek,
et al. Potent beta-Lactam Enhancer Activity of Zidebactam and WCK Roche, Shionogi, Tetraphase, The Medicine Company and Astellas Pharma Inc.
5153 against acinetobacter baumannii, including carbapenemase-producing Outside the submitted work, DRG reports honoraria from Stepstone Pharma
clinical isolates. Antimicrob Agents Chemother. (2017) 61:e01238–17. GmbH and an unconditioned grant from MSD Italia.
doi: 10.1128/AAC.01238-17
73. Moya B, Barcelo IM, Bhagwat S, Patel M, Bou G, Papp-Wallace KM, et al. The remaining authors declare that the research was conducted in the absence of
WCK 5107 (Zidebactam) and WCK 5153 are novel inhibitors of PBP2 any commercial or financial relationships that could be construed as a potential
showing potent “beta-Lactam Enhancer” activity against pseudomonas conflict of interest.
aeruginosa, Including Multidrug-Resistant Metallo-beta-Lactamase-
Producing High-Risk Clones. Antimicrob Agents Chemother. (2017) Copyright © 2019 Bassetti, Peghin, Vena and Giacobbe. This is an open-access article
61:e02529–16. doi: 10.1128/AAC.02529-16 distributed under the terms of the Creative Commons Attribution License (CC BY).
74. Sader HS, Castanheira M, Huband M, Jones RN, Flamm RK. WCK The use, distribution or reproduction in other forums is permitted, provided the
5222 (Cefepime-Zidebactam) antimicrobial activity against clinical original author(s) and the copyright owner(s) are credited and that the original
isolates of gram-negative bacteria collected Worldwide in 2015. publication in this journal is cited, in accordance with accepted academic practice.
Antimicrob Agents Chemother. (2017) 61:e072–17. doi: 10.1128/AAC. No use, distribution or reproduction is permitted which does not comply with these
00072-17 terms.
Frontiers in Medicine | www.frontiersin.org 10 April 2019 | Volume 6 | Article 74
Anda mungkin juga menyukai
- AMS Programs in The ICUs in Patients With Infections Caused by MDR GNBDokumen9 halamanAMS Programs in The ICUs in Patients With Infections Caused by MDR GNBGurmeet SinghBelum ada peringkat
- Infections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumDari EverandInfections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumBelum ada peringkat
- Chasing Resistance Analyzing The Fight Agains - 2023 - The Lancet Regional HealDokumen2 halamanChasing Resistance Analyzing The Fight Agains - 2023 - The Lancet Regional HealGraziellia Bianca Huamani MartinezBelum ada peringkat
- Antibiotics 12 00399 With CoverDokumen20 halamanAntibiotics 12 00399 With CoverRAGHAVENDRA VAGYANNAVARBelum ada peringkat
- Fcimb 12 1002406Dokumen13 halamanFcimb 12 1002406Luiz JmnBelum ada peringkat
- Newly Available Armamentarium For G NegativDokumen19 halamanNewly Available Armamentarium For G NegativStacey WoodsBelum ada peringkat
- Diagnosis and Treatment of Multidrug-Resistant TuberculosisDokumen12 halamanDiagnosis and Treatment of Multidrug-Resistant Tuberculosisfeby megaBelum ada peringkat
- José Domínguez Clinical Implications of MolecularDokumen16 halamanJosé Domínguez Clinical Implications of MolecularcarolBelum ada peringkat
- Fmicb 09 02066Dokumen16 halamanFmicb 09 02066Renata CalixtoBelum ada peringkat
- Deelder Et Al. - 2019 - Machine Learning Predicts Accurately Mycobacterium Tuberculosis Drug Resistance From Whole Genome Sequencing DataDokumen9 halamanDeelder Et Al. - 2019 - Machine Learning Predicts Accurately Mycobacterium Tuberculosis Drug Resistance From Whole Genome Sequencing DatafdasffdBelum ada peringkat
- Antibiotics: Antibiotics and Antimicrobials Resistance: Mechanisms and New Strategies To Fight Resistant BacteriaDokumen3 halamanAntibiotics: Antibiotics and Antimicrobials Resistance: Mechanisms and New Strategies To Fight Resistant BacteriaFernamdo GarciaBelum ada peringkat
- Evaluating Bedaquiline As A Treatment Option For Multidrug-Resistant TuberculosisDokumen8 halamanEvaluating Bedaquiline As A Treatment Option For Multidrug-Resistant Tuberculosisa29921Belum ada peringkat
- NIH Public Access: Combination Approaches To Combat Multi-Drug Resistant BacteriaDokumen15 halamanNIH Public Access: Combination Approaches To Combat Multi-Drug Resistant BacteriaValentina RoznovBelum ada peringkat
- Rationalizing Antimicrobial Therapy in The ICU: A Narrative ReviewDokumen18 halamanRationalizing Antimicrobial Therapy in The ICU: A Narrative ReviewajengmdBelum ada peringkat
- Antibiotics 11 01082Dokumen14 halamanAntibiotics 11 01082Koko The good boyBelum ada peringkat
- Comparison Between IDSA and ESCMID - CMI 2022Dokumen5 halamanComparison Between IDSA and ESCMID - CMI 2022drleumgwsBelum ada peringkat
- The "Old" and The "New" Antibiotics For MDR Gram-Negative Pathogens: For Whom, When, and HowDokumen25 halamanThe "Old" and The "New" Antibiotics For MDR Gram-Negative Pathogens: For Whom, When, and HowntnquynhproBelum ada peringkat
- Fmicb 13 820572Dokumen18 halamanFmicb 13 820572I EBelum ada peringkat
- The Challenge of Overcoming Antibiotic ResistanceDokumen16 halamanThe Challenge of Overcoming Antibiotic Resistanceannisa zakiyahBelum ada peringkat
- Antibiotic Resistance and Persistence-Implications For Human Health and Treatment PerspectivesDokumen24 halamanAntibiotic Resistance and Persistence-Implications For Human Health and Treatment PerspectivesserviceBelum ada peringkat
- Efficacy and Safety of Zapnometinib in Hospitalised Adult Patient - 2023 - EclinDokumen12 halamanEfficacy and Safety of Zapnometinib in Hospitalised Adult Patient - 2023 - Eclinronaldquezada038Belum ada peringkat
- Antibiotico en SepsisDokumen15 halamanAntibiotico en SepsisJuan RodriguezBelum ada peringkat
- (M299) RL3Dokumen11 halaman(M299) RL3Jessa Louise TurredaBelum ada peringkat
- Antibiotic Stewardship in CriticalDokumen6 halamanAntibiotic Stewardship in CriticalVíctor C. ValverdeBelum ada peringkat
- Antifungal GuidelineDokumen23 halamanAntifungal GuidelineMr.ShazBelum ada peringkat
- Research Proposal - Lamisa Nur - ID 201406080 - 4th Year 8th SemesterDokumen12 halamanResearch Proposal - Lamisa Nur - ID 201406080 - 4th Year 8th Semesteriksumaiya29Belum ada peringkat
- 1 s2.0 S0924857922001455 MainDokumen13 halaman1 s2.0 S0924857922001455 MainRobert StryjakBelum ada peringkat
- Fmicb 10 00041Dokumen12 halamanFmicb 10 00041Daniel Dario Hernandez TobonBelum ada peringkat
- Antimicrobial Adjuvants Drug Discovery, The Challenge of Avoid The Resistance and Recover The Susceptibility of Multidrug-Resistant StrainsDokumen8 halamanAntimicrobial Adjuvants Drug Discovery, The Challenge of Avoid The Resistance and Recover The Susceptibility of Multidrug-Resistant StrainsjuangbuenoBelum ada peringkat
- Macrocycle-Antibiotic Hybrids: A Path To Clinical CandidatesDokumen16 halamanMacrocycle-Antibiotic Hybrids: A Path To Clinical CandidatesMung MingBelum ada peringkat
- Duration of Antibiotic Therapy in Gram Negative Infections WithDokumen7 halamanDuration of Antibiotic Therapy in Gram Negative Infections WithYorvi hendersson Ilasaca gaonaBelum ada peringkat
- Fighting Pathogenic Bacteria On Two Fronts - Phages and Antibiotics As Combined StrategyDokumen13 halamanFighting Pathogenic Bacteria On Two Fronts - Phages and Antibiotics As Combined Strategygwyneth.green.512Belum ada peringkat
- Jurnal AnestesiDokumen24 halamanJurnal AnestesiSeruni Allisa AslimBelum ada peringkat
- Ijms-22-00735 Id enDokumen28 halamanIjms-22-00735 Id enNur AnisaBelum ada peringkat
- Antibiotics in Critically Ill ChildrenDokumen7 halamanAntibiotics in Critically Ill ChildrenGurmeet SinghBelum ada peringkat
- Tigecycline Alone or in CombinationDokumen13 halamanTigecycline Alone or in CombinationSanjay NavaleBelum ada peringkat
- Review-Pipeline of Anti-Mycobacterium Abscessus Small MoleculesDokumen38 halamanReview-Pipeline of Anti-Mycobacterium Abscessus Small MoleculesMayuriBelum ada peringkat
- 4.targeting DNA Replication and Repair For The Development of NovelDokumen18 halaman4.targeting DNA Replication and Repair For The Development of NovelfeBelum ada peringkat
- 1 s2.0 S1201971221002009 MainDokumen3 halaman1 s2.0 S1201971221002009 MainNia KurniawanBelum ada peringkat
- Clinical Microbiology and Infection: M. Abbas, M. Paul, A. HuttnerDokumen7 halamanClinical Microbiology and Infection: M. Abbas, M. Paul, A. HuttnerKushi Sharma SharmaBelum ada peringkat
- Nanoparticles For Antimicrobial Agents Delivery-AnDokumen23 halamanNanoparticles For Antimicrobial Agents Delivery-AnArmando MejíaBelum ada peringkat
- JurnalDokumen4 halamanJurnalAnonymous pfHZusnBelum ada peringkat
- Mini-Review: Antimicrobial Resistance and COVID-19 Syndemic: Impact On Public HealthDokumen6 halamanMini-Review: Antimicrobial Resistance and COVID-19 Syndemic: Impact On Public HealthJhosua MendezBelum ada peringkat
- Antifungal Stewardship - What We Need To KnowDokumen7 halamanAntifungal Stewardship - What We Need To KnowAkbar SaleemBelum ada peringkat
- Antibiotic Stewardship in Critical Care: Ian Johnson MBCHB Frca and Victoria Banks Mbbs BSC Frca Fficm EdicDokumen6 halamanAntibiotic Stewardship in Critical Care: Ian Johnson MBCHB Frca and Victoria Banks Mbbs BSC Frca Fficm EdicRavi KumarBelum ada peringkat
- Antibiotics 13 00162 With CoverDokumen17 halamanAntibiotics 13 00162 With CoverbcgvpilotBelum ada peringkat
- Recent Improvements in mRNA and ImmunogenicityDokumen2 halamanRecent Improvements in mRNA and ImmunogenicityMediterr J Pharm Pharm SciBelum ada peringkat
- Jurnal Antibiotik 2Dokumen11 halamanJurnal Antibiotik 2Achmad YunusBelum ada peringkat
- Frieri 2016Dokumen10 halamanFrieri 2016Adil AnwarBelum ada peringkat
- Molecules 27 08210Dokumen20 halamanMolecules 27 08210Robert StryjakBelum ada peringkat
- Biomedicines 11 00765Dokumen21 halamanBiomedicines 11 00765lipu1982Belum ada peringkat
- Bacteriostatic Versus Bactericidal Antibiotics For Patients With Serious Bacterial Infections: Systematic Review and Meta-AnalysisDokumen14 halamanBacteriostatic Versus Bactericidal Antibiotics For Patients With Serious Bacterial Infections: Systematic Review and Meta-Analysisblade masterBelum ada peringkat
- JurnalDokumen10 halamanJurnalIkaBelum ada peringkat
- Idsa CreDokumen8 halamanIdsa CreMihai NegutuBelum ada peringkat
- Empirical Decision Making For Antimicrobial Therapy in Critically Ill PatientsDokumen8 halamanEmpirical Decision Making For Antimicrobial Therapy in Critically Ill Patientsal malikBelum ada peringkat
- Pseudomonas Baru 4-1Dokumen29 halamanPseudomonas Baru 4-1Nadia Iriana DewiBelum ada peringkat
- Elective Project - TuberculosisDokumen30 halamanElective Project - TuberculosisKinjal KoshtiBelum ada peringkat
- Fgene 11 575592Dokumen9 halamanFgene 11 575592omniyaBelum ada peringkat
- Stan 2021Dokumen25 halamanStan 2021Monyet...Belum ada peringkat
- Clinical Practice Guidelines For The Diagnosis and Treatment of Patients With Soft Tissue Sarcoma by The Spanish Group For Research in Sarcomas (GEIS)Dokumen14 halamanClinical Practice Guidelines For The Diagnosis and Treatment of Patients With Soft Tissue Sarcoma by The Spanish Group For Research in Sarcomas (GEIS)carolinapolotorresBelum ada peringkat
- Tumores Desmoides en Cohorte DanesaDokumen6 halamanTumores Desmoides en Cohorte DanesacarolinapolotorresBelum ada peringkat
- Review Article: Optimization of The Therapeutic Approach To Patients With Sarcoma: Delphi ConsensusDokumen15 halamanReview Article: Optimization of The Therapeutic Approach To Patients With Sarcoma: Delphi ConsensuscarolinapolotorresBelum ada peringkat
- Drug Therapy For Osteoporosis in Older AdultsDokumen3 halamanDrug Therapy For Osteoporosis in Older AdultscarolinapolotorresBelum ada peringkat
- Pazopanib Tumor Fibroso SolitarioDokumen11 halamanPazopanib Tumor Fibroso SolitariocarolinapolotorresBelum ada peringkat
- Protocolo PreciousDokumen5 halamanProtocolo PreciouscarolinapolotorresBelum ada peringkat
- Management of Acute Pancreatitis Associated With Checkpoint InhibitorsDokumen14 halamanManagement of Acute Pancreatitis Associated With Checkpoint InhibitorscarolinapolotorresBelum ada peringkat
- Cutaneous Manifestations of HIV InfectionDokumen18 halamanCutaneous Manifestations of HIV InfectioncarolinapolotorresBelum ada peringkat
- Clinical and Neurologic Manifestation of Minimal Hepatic Encephalopathy and Overt Hepatic Encephalopathy - 2015 - Clinics in Liver DiseaseDokumen12 halamanClinical and Neurologic Manifestation of Minimal Hepatic Encephalopathy and Overt Hepatic Encephalopathy - 2015 - Clinics in Liver DiseasecarolinapolotorresBelum ada peringkat
- Guias AI OsteopeniaDokumen12 halamanGuias AI OsteopeniacarolinapolotorresBelum ada peringkat
- Breast Cancer in Women Older Than 80 Years: Clinical ReviewDokumen11 halamanBreast Cancer in Women Older Than 80 Years: Clinical ReviewcarolinapolotorresBelum ada peringkat
- Chest AC ParenteralesDokumen20 halamanChest AC ParenteralescarolinapolotorresBelum ada peringkat
- Medicamentos Guia NICEDokumen128 halamanMedicamentos Guia NICEcarolinapolotorresBelum ada peringkat
- Treatment For Ischemic Stroke: From Thrombolysis To Thrombectomy and Remaining ChallengesDokumen4 halamanTreatment For Ischemic Stroke: From Thrombolysis To Thrombectomy and Remaining ChallengescarolinapolotorresBelum ada peringkat
- SHM Glycemic ControDokumen175 halamanSHM Glycemic Controcarolinapolotorres100% (1)
- Hemolytic Anemia - Evaluation and Differential DiagnosisDokumen8 halamanHemolytic Anemia - Evaluation and Differential Diagnosiscarolinapolotorres100% (1)
- Lung Cancer Risk Factors and EpidemiologyDokumen21 halamanLung Cancer Risk Factors and EpidemiologycarolinapolotorresBelum ada peringkat
- 30947630Dokumen12 halaman30947630carolinapolotorresBelum ada peringkat
- U.S. Preventive Services Task Force: Screening For Preeclampsia: Recommendation StatementDokumen3 halamanU.S. Preventive Services Task Force: Screening For Preeclampsia: Recommendation StatementcarolinapolotorresBelum ada peringkat
- Guideline XDokumen104 halamanGuideline XcarolinapolotorresBelum ada peringkat
- Microbiology: Slam Shraf AhmyDokumen9 halamanMicrobiology: Slam Shraf AhmyFahad AlkenaniBelum ada peringkat
- Cellular Control Questions F215Dokumen101 halamanCellular Control Questions F215Miles StacksBelum ada peringkat
- Development of The Nervous System 3rd Edition Sanes Test BankDokumen12 halamanDevelopment of The Nervous System 3rd Edition Sanes Test Bankdrerindavisddsybrqsdmajp100% (16)
- Community Acquired Pneumonia: Ang Gobonseng, Ed Gerard R. MedclerkDokumen66 halamanCommunity Acquired Pneumonia: Ang Gobonseng, Ed Gerard R. MedclerkRyn Anfone100% (2)
- Broad Spectrum AntibioticsDokumen17 halamanBroad Spectrum AntibioticsRabi ShahBelum ada peringkat
- Chronic Inflammation Non-Specific and GranulomatousDokumen47 halamanChronic Inflammation Non-Specific and GranulomatousPradeepBelum ada peringkat
- Leek (Allium Ampeloprasum)Dokumen4 halamanLeek (Allium Ampeloprasum)Guia De OcampoBelum ada peringkat
- Covid-19 Research ?Dokumen414 halamanCovid-19 Research ?Zach Rigby100% (2)
- Microbes and The MindDokumen5 halamanMicrobes and The MindPaula Manalo-SuliguinBelum ada peringkat
- Endocrine Glands PDFDokumen99 halamanEndocrine Glands PDFXochitl ZambranoBelum ada peringkat
- T0610e PDFDokumen344 halamanT0610e PDFShofli Yazid Khoirul RoziqinBelum ada peringkat
- Hormones of The PlacentaDokumen67 halamanHormones of The PlacentagibreilBelum ada peringkat
- M2C The Nucleus QuestionsDokumen10 halamanM2C The Nucleus QuestionsJhanna MooreBelum ada peringkat
- Antibody Structure: Investigating Antibody Structure Igg Molecule Recap Important AreasDokumen13 halamanAntibody Structure: Investigating Antibody Structure Igg Molecule Recap Important Areasohs sehunBelum ada peringkat
- DM Type 1Dokumen14 halamanDM Type 1Yogi SetiawanBelum ada peringkat
- Obsfetrics Gynecology: & DepartmentDokumen222 halamanObsfetrics Gynecology: & DepartmentFatma AlbakoushBelum ada peringkat
- Ud7 (I) : Molecular Cloning: Dra Maria V. MonserratDokumen32 halamanUd7 (I) : Molecular Cloning: Dra Maria V. MonserratAngela MarBelum ada peringkat
- Aplastic AnemiaDokumen52 halamanAplastic AnemiaMARGARET BLANCHE NICOLASBelum ada peringkat
- Lab Testes ListDokumen16 halamanLab Testes ListDjdjjd SiisusBelum ada peringkat
- Nanubala - Subramanyam@gmail - Com 20220326181643Dokumen19 halamanNanubala - Subramanyam@gmail - Com 20220326181643Praveena NanubalaBelum ada peringkat
- Abhay ArabDokumen2 halamanAbhay ArabPrabin PaulBelum ada peringkat
- Department of Molecular Biology. Covid 19 Test Name Result Unit Bio. Ref. Range MethodDokumen2 halamanDepartment of Molecular Biology. Covid 19 Test Name Result Unit Bio. Ref. Range MethodDarpan NegandhiBelum ada peringkat
- IMMUNOLOGICAL AND BIOCHEMICAL RESPONSE FROM OLDER ADULTS WITH URINARY TRACT INFECTION TO UROPATHOGENIC Escherichia Coli VIRULENCE FACTORSDokumen5 halamanIMMUNOLOGICAL AND BIOCHEMICAL RESPONSE FROM OLDER ADULTS WITH URINARY TRACT INFECTION TO UROPATHOGENIC Escherichia Coli VIRULENCE FACTORSjavelezhBelum ada peringkat
- CHAPTER 8 MedtechDokumen17 halamanCHAPTER 8 MedtechKisen DiazBelum ada peringkat
- Monounsaturated Fatty Acids and Immune FunctionDokumen5 halamanMonounsaturated Fatty Acids and Immune FunctionLucas PolizzeliBelum ada peringkat
- Cell and Molecular Biology: Gerald KarpDokumen53 halamanCell and Molecular Biology: Gerald Karppat ongBelum ada peringkat
- Department of Education: Republic of The PhilippinesDokumen2 halamanDepartment of Education: Republic of The PhilippinesEizen DivinagraciaBelum ada peringkat
- Pediatric Drug DosesDokumen27 halamanPediatric Drug DosesAlisha AhmadBelum ada peringkat
- Reference: Chapter 47. Basic and Clinical Pharmacology - 13th Edition. Katzung and Trevor. Lec GuideDokumen8 halamanReference: Chapter 47. Basic and Clinical Pharmacology - 13th Edition. Katzung and Trevor. Lec GuideselflessdoctorBelum ada peringkat
- Protein StructureDokumen10 halamanProtein StructureSzekeres-Csiki KatalinBelum ada peringkat
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Dari EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Penilaian: 3 dari 5 bintang3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDari EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionPenilaian: 4 dari 5 bintang4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDari EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsBelum ada peringkat
- The Age of Magical Overthinking: Notes on Modern IrrationalityDari EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityPenilaian: 4 dari 5 bintang4/5 (32)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDari EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisPenilaian: 4.5 dari 5 bintang4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDari EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDPenilaian: 5 dari 5 bintang5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDari EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePenilaian: 2 dari 5 bintang2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDari EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedPenilaian: 4.5 dari 5 bintang4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDari EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryPenilaian: 4 dari 5 bintang4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDari EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDari EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsPenilaian: 4 dari 5 bintang4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossDari EverandThe Obesity Code: Unlocking the Secrets of Weight LossPenilaian: 4 dari 5 bintang4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDari EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesPenilaian: 4.5 dari 5 bintang4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDari EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsPenilaian: 5 dari 5 bintang5/5 (1)
- The Comfort of Crows: A Backyard YearDari EverandThe Comfort of Crows: A Backyard YearPenilaian: 4.5 dari 5 bintang4.5/5 (23)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Dari EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Penilaian: 4.5 dari 5 bintang4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDari EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityPenilaian: 4 dari 5 bintang4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDari EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsPenilaian: 4.5 dari 5 bintang4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDari EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisPenilaian: 5 dari 5 bintang5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDari EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisPenilaian: 3.5 dari 5 bintang3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDari EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessPenilaian: 4.5 dari 5 bintang4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassDari EverandTroubled: A Memoir of Foster Care, Family, and Social ClassPenilaian: 4.5 dari 5 bintang4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDari EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingPenilaian: 4 dari 5 bintang4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDari EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifePenilaian: 4.5 dari 5 bintang4.5/5 (254)