Respi - Path
Diunggah oleh
Kimberly KanemitsuDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Respi - Path
Diunggah oleh
Kimberly KanemitsuHak Cipta:
Format Tersedia
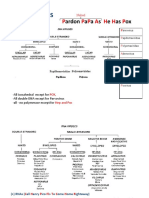
URTI
June 26, 2018 9:06 AM
01 Upper respiratory tract infections
NASOPHARYNX
- Necrotizing lesions of upper airways
○ Rhinocerebral mucormycosis in diabetes, immunosuppressed
○ Wegener's granulomatosis with polyangiitis
- Acute pharyngitis and tonsillitis
○ Rhinovirus, Echovirus, adenovirus, β hemolytic streptococci
Rhinosinusitis Nasal Polyp Sinonasal Schneiderian Angiofibroma Olfactory Neuroblastoma Nasopharyngeal Carcinoma
Papilloma
Descript - Obstruction of sinus drainage into - Protrusion of edematous, - Benign tumor from - Benign tumor of nasal - Tumor from - Malignant tumor of
ion nasal cavity = inflammation, pain inflamed nasal mucosa respiratory mucosa lining mucosa neuroectodermal olfactory nasopharyngeal epithelium
over infected area nasal cavity - Made of blood vessels cells • Pleomorphic, keratin
- Common Cold - Adult males age 30-60 and fibrous tissue - Small round blue cell tumor positive cells in a
• Sneezing, congestion, runny - Adolescent red-headed, background of
nose fair skinned males lymphocytes
• Inflammatory infiltrate with • Enlarged cervical LN
eosinophils
• Associated with asthma,
eczema, sinusitis
Etiology - Rhinovirus - Repeated rhinitis - Age 15 or 50 - EBV
- Allergic Rhinitis - Cystic fibrosis in kids • African children
• Type I hypersensitivity - Aspirin-intolerant asthma • Young Chinese adults
• Asthma + aspirin-
induced
bronchospasms + nasal
polyps
LARYNX
Acute Epiglottitis Laryngotracheobronchitis Diphtheria Vocal Cord Nodule Laryngeal Papilloma Laryngeal Carcinoma
(Croup)
Descrip - Inflamed epiglottis - Inflamed upper airway - Nodule on true vocal cord - Benign papillary tumor of - Squamous cell carcinoma from
tion vocal chord epithelial lining of vocal chord
Etiology - H influenza type B - Parainfluenza - Corynebacterium - Wear and tear (singer) - HPV 6, 11 (Koilocytes change) - Risk factors: alcohol, tobacco
• Immunized, - Single in adults - Arise from laryngeal papilloma
nonimmunized kids - Multiple in children (rare)
Present - High fever, sore throat - Barking cough - Grey pseudomembrane - Bilateral - Hoarseness - Hoarseness
ation - Drooling with dysphagia - Inspiratory stridor - Made of myxoid connective - Cough
- Muffled voice tissue - Stridor
- Inspiratory stridor - Hoarseness
- Risk airway obstruction - Resolves with rest
Respi - Path Page 1
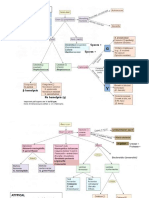
Pulmonary Infections and TB
June 26, 2018 9:22 AM
04 Pulmonary infections - 1, Bronchiectasis, TB
05 Pulmonary infecton - 2 - Lobar, Broncho, Atypical
06 Pulmonary infection - 3 - Aspiration and Fungus
Pneumonia
- Infection of lung parenchyma
- Occurs when normal defenses impaired
○ Impaired cough
○ Damage to mucociliary escalator
○ Mucus plugging
- Fevers, chills, pleuritic chest pain, decreased breathing sounds, dullness to percussion, elevated WBC
- Sputum: productive cough
○ Yellow-green pus
○ Rusty blood
- Diagnose via chest X-Ray, sputum gram stain and culture, blood culture
Lobar Bronchopneumonia Interstitial/Atypical Aspiration - Lung Abscess
Chest X-
Ray
Lung abscess in right lower lobe
Descripti - Consolidation of entire lobe - Scattered patchy consolidation around - Diffuse interstitial infiltrates - Abscess: localized collection of pus
on bronchioles - No major consolidation • Cystic abscess: pus with fibrous wall
- Multi-focal and bilateral - Dry cough because inflammation in interstitium, - Surrounded by destroyed lung parenchyma
not alveoli - Right lung
• Location dependent on patient position
during aspiration
• Superior segment right lower lobe
• (R bronchus less acute angle than the
left)
Caused - Strep Pneumonia: middle age - Staph aureus: 2nd most common cause of - Mycoplasma: most common cause of atypical - Caused by aspiration > cancer
by adults, elderly secondary pneumonia pneumonia • Aspiration: Alcoholics, comatose
- Klebsiella: enteric flora that • Abscess, empyema • Young adults (military, dorm) patients, epileptics, elderly, bronchial
aspirate - H Influenza • Autoimmune hemolytic anemia obstruction
• Elderly, alcoholics • Secondary pneumonia • Cold agglutination
• Currant jelly sputum • Pneumonia superimposed on COPD • Can't visualize on gram stain (no cell wall) - Anaerobic bacteria in oropharynx
• Abscess - Pseudomonas: nosocomial, cystic fibrosis - Chlamydia pneumonia: 2nd most common cause - Bacteroides
patients, immunocompromised of atypical pneumonia in young adults - Fusobacterium
- Moraxella: community-acquired • Seroepidemiologic association with - Pepto coccus
• Pneumonia superimposed on COPD coronary artery disease
- Legionella: community acquired - Chlamydia psittaci: parrot fever
• Organ transplant patient - Respiratory syncytial virus: infants - Foul-smelling purulent sputum
• Pneumonia superimposed on COPD - CMV: post-implant immunosuppressive therapy - Sanguineous sputum
• Transmitted from water source • Owl Eye inclusions - (rule out carcinoma-causes in older individuals)
• Silver stain - Influenza virus: elderly, immunocompromised,
pre-existing lung disease
• Risk superimposed S aureus, H influenza
- Coxiella: Q fever
• Farmers, veterinarians
Diagnosis - Sputum culture - Sputum culture - Sputum culture - Chest-X Ray: air/fluid level
• Abscess filled with pus and air
• Cavitation
Treatme - Antibiotic - Antibiotic - Antibiotic - Clindamycin
nt - Anti-viral - Surgical removal of lung abscess
Natural History of Lobar Pneumonia
Day Findings
1. Congestion 1-2 - Congested vessels: Red-purple
- Partial consolidation of parenchyma
- Exudate mostly bacterial
2. Red Hepatization 3-4 - Red-brown, consolidated
- Exudate filled with neutrophils, fibrin, bacteria, RBC, WBC
3. Gray Hepatization 5-7 - Grey color; RBC degrade in exudate
- Exudate WBC, fibrin
4. Resolution 8+ - Enzymes digest exudate components
Respi - Path Page 2
4. Resolution 8+ - Enzymes digest exudate components
- Type II pneumocyte restore lining
Lung Abscess
- Lung abscess: localized accumulation of pus with destroyed lung parenchyma (alveoli, airway, blood vessel)
○ Cystic abscess: purulent exudates contained by a fibrous wall
- Caused by
○ Aspiration
○ Complication lung cancer (bronchial obstruction)
- Chest X Ray: air/fluid level = abscess filled with pus and air
○ Cavitation: formation of cavity; can be made by fluid
- Inflammation in surrounding pulmonary parenchyma
- Foul-smelling sputum may be expectorated if an abscess is connected to a bronchus
Localized collection of pus in parenchyma Chest X-Ray: air-fluid levels
TB Presentation
Description
Primary TB Pneumonia - Chronic cough with bloody mucous
- Weight loss, night sweats, hemoptysis
- Ghon complex: hilar lymphadenopathy + caseating granuloma in mid/ lower lobe
Healed latent infection - Fibrosis, calcification
- Chronic: Latent for many years
- Positive PPD test
- Nodules on X-ray
Secondary TB: - Reactivate in immunocompromised
- No TNF-α: No T-cell release INF-γ = no macrophage = uncontained TB
- Macrophages: phagocytose, release IL 12, TNF-α = recruit T cells - Fibro caseous cavitary granuloma: apex of right upper lung (aerobic)
○ TNF-α: cachexia Miliary TB: - Disseminated TB
○ IL 12: T cells → Th1 cells - Resemble millet seeds
- Th 1 cells: release INF-γ - Meningitis: cavitary lesion, tuberculoma
○ INF-γ: activate macrophage to wall off bacteria - Pott's disease: TB goes to bones, spinal column
- Caseating Granuloma: calcified mass with necrotic macrophage in - Cement, Putty Kidney: TB goes to kidney
center
- Size of infection = effectiveness of bacterial elimination
Respi - Path Page 3
Pulmonology Infections Micro Overview
July 3, 2018 8:25 PM
By Group
Gram Positive Gram Negative Atypical Bacteria Viral Fungal
- Strep pneumonia - Klebsiella - Legionella - RSV - Pneumocystosis Jirovecci
- Staph aureus - H influenza - Mycoplasma - CMV - Histoplasmosis
- Pseudomonas - TB - Influenza - Blastomycosis
- Moraxella - Chlamydia pneumonia - Coxiella - Coccidioidomycosis
- Bacteroides - Paracoccidioidomycosis
- Fusobacterium - Aspergillosis AAAA
- Peptostreptococcus - Zygomycophyta
By Age
Neonates Children Young Adults Older Adults Elderly
- Group B - RSV - Mycoplasma - Strep pneumoniae - S pneumoniae
Streptococci - Mycoplasma - Chlamydia pneumonia - H influenzae - Influenza virus
- E Coli - C Trachomatis - Staph pneumonia - Anaerobes - Anaerobes
- C pneumonia - Viruses - H influenzae
- Staph pneumonia - Mycoplasma - Gram ⊝ rods
Special Groups
Alcoholics Klebsiella, anaerobes usually due to aspiration (eg, Peptostreptococcus, Fusobacterium, Prevotella, Bacteroides)
IV Drug users S pneumoniae, S aureus
Aspiration Anaerobes
Atypical Mycoplasma, Legionella, Chlamydia
Cystic Fibrosis Pseudomonas, S aureus, S pneumoniae, Burkholderia cepacia
Immunocompromised Staph aureus, enteric gram negative rods, fungi, viruses, P jirovecii (with HIV)
Nosocomial Staph aureus, Pseudomonas, other enteric gram negative rods
Post-viral Strep pneumoniae, Staph aureus, H influenzae
Respi - Path Page 4
Pulmonary Infection: Fungal
July 2, 2018 11:38 AM
06 Pulmonary infection - 3
Systemic Fungus
Histoplasmosis Blastomycosis Coccidioidomycosis
Feature - Spike conidiophore on hyphae - Broad Based Budding Blastomyces BBBB - Spherules: yeast with endospores
s - Cannon ball yeast: Intracellular in macrophage
Epidemi - Ohio/Mississippi, Caribbean - Great Lakes - California, Mexico
ology - Bird, bat droppings (caves) - Decaying organic matter, rotting wood - Soil, dust: Dust storms, Earthquake
Pneumo - Granuloma - Patchy infiltrate on upper lobe - Acute pneumonia
nia - Calcification near hilum region - Large granuloma with central necrosis - X ray: nothing, cavities, nodules
Other - Calcifications in spleen - Verrucous skin lesions: painless cauliflower like - Valley Fever
Present - Erythema nodosum lesions similar to squamous cell carcinoma - Erythema nodosum
ations - Diffuse infiltrates in immunocompromised - Osteomyelitis - Skin, lung infection
- Disseminates in immunocompromised - Meningitis
Treatm - Azoles for local - Surgery - Self-limiting
ent - Amphotericin B systemic - Azoles: local - Azoles: local
- Amphotericin B: systemic - Amphotericin B: systemic
Opportunistic Fungi
Pneumocystosis Jirovecii Aspergillosis AAAA Zygomycosis, Mucormycosis
Feature - Sporocyst; honey comb appearance - Acute Angle branches - Non-septate, wide angle branches mold
s - Extracellular - Conidia fan - Conidia columnella: bulbous swelling at end, spores
Epidemi - Immunocompromised, HIV, AIDS - Hospital air, AC, shower, plant - Bread mold
ology - Immunocompromised - Immunocompromised
- Organ transplant patients with diabetes mellitus +
ketoacidosis
- Iron overload (free iron)
Pneumo - AIDS-defining!!! - Allergic Bronchopulmonary Aspergillosis: - Pulmonary mucormycosis
nia - Diffuse interstitial infiltrates • IgE → inflammation, mucus plugs • Neutropenic patients
- Death by respiratory failure - Aspergilloma: • Fungus ball formation like aspergilloma
• Lower lung, gravity
• COPD, CF patients
Other - Angio-invasive Aspergillosis → disseminate - Rhinocerebral
Present • Necrotizing pneumonia with gray • Proliferate in RBC
ations foci and hemorrhagic borders • Nasal cavity, sinus, cribriform plate, orbit,
• "target lesions" meninges, brain
• Blood vessels • Frontal cortex abscess
Respi - Path Page 5
• Blood vessels • Frontal cortex abscess
Treatm - TMP + SMX - Amphotericin B - Amphotericin B
ent - Pentamidine - Voriconazole
- Surgery
Respi - Path Page 6
Obstructive Lung Disease
June 26, 2018 9:22 AM
02 PFTs, COPD - 1, Bronchitis, Emphysema
03 COPD - 2, Asthma
04 Pulmonary infections - 1, Bronchiectasis, TB
- Group of diseases characterized by airway obstruction
○ Lung does not empty, air is trapped = lung volumes
- Volume of air forcefully expired decreases = FVC
○ Especially during first second of expiration = FEV1
○ Decreased FEV1:FVC ratio
Chronic Bronchitis Emphysema Asthma Bronchiectasis
Thick mucinous glands >50% Curschmann spirals and Charcot-Leyden Crystals Dilated bronchi
Abnormally enlarged alveoli separated by thin septa
Descript - Chronic productive cough for at least 3 - Destruction of alveolar sacs - Bronchial hyper responsive → reversible - Chronic necrotizing infection → permanent
ion months for 2+ years • Lose elastic recoil bronchoconstriction dilation of bronchioles and bronchi
- Hypertrophy of bronchial submucosal • Airways collapse during exhalation = obstruction, • Large radius = turbulent flow
glands air trapping • Loss of airway tone = airway trapping
• (alveoli's elastic recoil keeps airways open during
exhalation)
Etiology - Smoking - Imbalance of protease and anti-protease - Allergic stimuli: Type 1 Hypersensitivity -
• Inflammation: neutrophils and alveolar • Presents in childhood
macrophages release protease • Allergic rhinitis
• α1 antitrypsin A1AT: neutralize protease • Family history of atopy
- Excessive inflammation or lack of A1AT = destroyed - Exercise
alveolar sacs - Viral infection
• Smoking: most common cause - Occupational exposures
• A1AT deficiency: genetic - Cold weather
- Aspirin: aspirin intolerant asthma
• COX inhibition → leukotriene
overproduction = airway constriction
• Asthma + aspirin induced bronchospasms +
nasal polyps
Patholo - Hypertrophy of bronchial mucinous glands - Smoking: inflammation, neutrals release - Allergens induce TH2 in CD4 T cells - Due to chronic necrotizing inflammation =
gy • Leads to increased thickness of proteases/elastase - Th2 cells secrete IL4, IL5, IL10 permanently dilated airways
mucus glands relative to bronchial • Centriacinar emphysema • IL 4: class switch to IgE
wall thickness • Upper lobes • IL 5: eosinophils - Cystic Fibrosis: mucus plugging ↑ infection
• Reid index > 50% - A1AT deficiency: no anti-protease • IL 10: stimulates Th2, inhibit Th1 - Kartagener syndrome: defect in dynein arm in
- Chronic inflammation = T cells and • Pan-acinar emphysema - Re-exposure to allergen = IgE cross-link, activate cilia → impaired ciliary movement
macrophages • Lower lobes mast cells ○ Sinusitis
• Liver cirrhosis • Early phase: Mast cells release histamine, ○ Infertility
○ Misfolded A1AT protein made and leukotriene C4, D4, E4 = ○ Chronic ear infections
accumulates in endoplasmic reticulum in bronchoconstriction, inflammation, edema ○ Situs inversus: position of major organs
hepatocytes ○ Histamine: vasodilate at arterioles reversed
○ Pink globules in hepatocytes PAS+ ○ Leaking fluid: post-capillary fluid, ○ Heart sounds in wrong place
• Degree of severity based on degree of A1AT edema - Tumor, foreign body: block increases risk of
deficiency • Late phase: inflammation (MBP from inflammation
○ PiM: normal allele eosinophils) damage ells and perpetuate - Necrotizing infection
○ PiZ: most common mutation bronchoconstriction - Allergic bronchopulmonary aspergillosis:
○ Heterozygotes: asymptomatic with less - Smooth muscle hypertrophy and hyperplasia; hypersensitivity to Aspergillus = chronic
A1AT; risk when smoke basement membrane thickening inflammatory damage
○ Homozygotes: panacinar emphysema with - Curschmann spirals: spiral-shaped mucus plugs of ○ Patient with asthma, cystic fibrosis
cirrhosis shed epithelium
- Charcot-Leyden crystals: aggregates of MBP from
eosinophil breakdown
Clinical - Productive cough - Dyspnea - Episodic, related to allergen exposure - Cough, dyspnea
Feature • Due to excessive mucus production - Cough with minimal sputum - Productive cough - Foul smelling sputum
s - Cyanosis: blue bloaters - Prolonged expiration with pursed lips - Tachypnea, dyspnea, wheezing • Loaded with inflammatory junk, sitting
• Mucus plug traps CO2 • Pursed lips create backpressure to keep walls - Hypoxemia in lumen
• ↑ PaCO2, ↓ PO2 open - inspiratory/ expiratory ratio - Hemoptysis
- Risk hypoxemia → cor pulmonale • Pink puffers - Pulsus paradoxus: when inspire, exaggerated - Digital clubbing
• ↑ PaCO2, hypoxic shunting - Weight loss drop in blood pressure
• RH pump against high pressure - Barrel chest: increased AP diameter • When inspire, more blood → RV - Risk hypoxemia → cor pulmonale
• Compensates for inward collapse • Increased volume in RV pushes - Risk secondary amyloidosis
- Risk hypoxemia → cor pulmonale interventricular septum to the left • AA released by liver
• LH gets smaller, less blood enters LV
• Less blood then pumped to aorta = drop in
aortic pressure
- Status asthmaticus: severe, unrelenting attack, can
lead to death
Emphysema
Respi - Path Page 7
Centriacinar Panacinar
- Emphysema and normal airspaces in same acinus - All airspaces with acini evenly enlarged
and lobule
- Smokers - α1 antitrypsin deficiency
Respi - Path Page 8
Restrictive Lung Disease
June 26, 2018 9:22 AM
08 Restrictive lung disease -2
RESTRICTIVE LUNG DISEASE
Poor Breathing Mechanics Interstitial Lung Disease
Features - Extrapulmonary - Pulmonary
- Peripheral hypoventilation - Reduced diffusion capacity
- Normal Aa gradient - Increased Aa gradient
Examples - Poor muscle effort - Fibrosing interstitial pneumonia
• Polio - Pneumoconiosis
• Myasthenia gravis - Granulomatous
- Cannot full inhale = lung volumes • Guillain-Barre • Sarcoidosis
- Increased FEV1:FVC ratio - Poor structural apparatus • Hypersensitivity pneumonitis
○ FEV1, FVC • Scoliosis - Pulmonary Langerhans Cell histiocytes
- Patient presents with short shallow breaths • Obesity - Pulmonary Alveolar Proteinosis
- Most commonly caused by interstitial lung disease - Wegener's granulomatosis with polyangiitis
○ Interstitial lung disease: Diffuse fibrosis/granulomatous inflammation - Drug toxicity
of lung parenchyma (alveolar wall, interstitium)
○ If alveoli damaged → hyaline membranes
○ Trichrome stain: stains collagen connective tissue blue
Fibrosing Interstitial Lung Disease
Idiopathic Pulmonary Fibrosis Non-specific Interstitial Pneumonia NIP Desquamative Interstitial pneumonia DIP Cryptogenic Organizing Pneumonia
(Usual Interstitial Pneumonia UIP) Bronchiolitis Obliterans Organizing Pneumonia
BOOP
Patchy dense fibrosis with focal microscopic Loose fibrous tissue in alveoli and bronchioles
honeycomb fibrosis
Descripti - Pulmonary fibrosis - Pulmonary fibrosis - Pulmonary fibrosis (minimal) - Inflamed bronchioles and surrounding tissue
on - Unknown cause → Cyclical lung injury - Secondary to infection, collagen vascular - Seen in smokers, related to respiratory - Non-infectious pneumonia
• Injured pneumocytes release TGF-β disease, hypersensitivity pneumonitis, fibrosing bronchiolitis - Unknown etiology (diagnosis of exclusion)
• TGF β induce fibrosis changes • Inflammation by chronic disease
- 60 year old non-smoker • Rheumatoid arthritis
• Medication side effect: Amiodarone
Pathologi - Aggressive temporal heterogeneity fibrosis - Diffuse, temporarily uniform proliferative and - Minimal fibrosis; alveolar structure - No interstitial fibrosis
cal - Honey-comb lung: scarring fibrosis begins fibrosing changes preserved - Masson bodies: polypoid plugs of loose fibrous
Findings in subpleural → entire lung - Ground glass appearance tissue in alveoli and bronchioles
- Not really desquamation of alveolar
epithelium
• Alveoli are pigment-laden
macrophages
Presentat - Gradual deterioration in pulmonary status - Best prognosis - No sputum, blood culture; no response to
ion despite treatment - Stop smoking antibiotics
- Worst prognosis - May recover spontaneously
- Treat with lung transplantation - May need steroids
Pneumoconiosis
- Interstitial fibrosis due to chronic occupational exposure
- Alveolar macrophages engulf small foreign particles, induce fibrosis to wall off
- Risk cor pulmonale, cancer, Caplan syndrome
- Caplan syndrome: rheumatoid arthritis and any pneumoconiosis with intrapulmonary nodules
○ Rheumatoid nodules: granuloma with central necrosis and outer fibrosis
Asbestosis Berylliosis Coal Worker Silicosis
Asbestos bodies Non-caseating granuloma (sarcoidosis) but Carbon-laden macrophages Fibrotic nodules
with history of beryllium exposure
Exposure - Construction workers, plumbers - Beryllium miners - Carbon dust - Sandblasters
Respi - Path Page 9
Exposure - Construction workers, plumbers - Beryllium miners - Carbon dust - Sandblasters
- Shipyard workers - Aerospace industry - Seen in coal miners - Silica miners
Location Lower lobes Upper lobes Upper lobes Upper lobes
Pathological - Ivory white calcified plaques - Non-caseating granuloma in lung, - Mild exposure (pollution) → Anthracosis: - Silica impairs phagolysosome formation in
Findings • Supradiaphragmatic hilar LN, systemic organs collection of carbon-laden macrophage macrophages
• Pleural • Similar to sarcoidosis but • Not clinically significant - Fibrotic nodules in upper lobes
- Asbestos bodies: Long golden brown fibers caused by beryllium - Black lung: macrophages filled with • Chest X-ray: eggshell calcification of hilar
made of iron carbon → inflammation, fibrosis LN
• Stain Prussian blue
Notes Risk cancer of lung > pleura - Risk lung cancer - Risk for TB: impaired macrophages
• Mesothelioma: cancer of pleura
Granulomatous Interstitial Lung Disease
Sarcoidosis Hypersensitivity Pneumonitis
Non-caseating granuloma with asteroid bodies Potato nodes: bilateral hilar LN
Descript - Non-caseating granulomas in multiple organs - Allergic non-caseating granulomatous reaction to inhaled organic antigens
ion • Bilateral lung hilar LN → restrictive lung disease • Type 3, Type 4 Hypersensitivity
• Eye → uveitis ○ Farmer's lung: actinomycetes
• Skin nodules, erythema nodosum ○ Pigeon breeder's lung
• Lupus pernio ○ Byssinosis: textile, cotton, linen with Monday Morning blues
• Salivary, lacrimal glands (mimic Sjogren syndrome) - Extrinsic allergic alveolitis: prolonged exposure to organic antigen
• Potato nodules • No IgE, no eosinophils
- Systemic disease - Chronic exposure → interstitial fibrosis
- African American females
Patholo - Asteroid bodies: stellate inclusions seen in giant cells of granuloma in lung - Intra-alveolar infiltrate
gical - Schumann bodies: laminated concentration of Ca and proteins - Interstitial pneumonitis and fibrosis
Findings • Eosinophils rare
Note - Elevated serum ↑ ACE
- Hypercalcemia ↑ Ca
• Granulomas have 1 α hydroxylase activity = activate vitamin D
- Hypergammaglobulinemia
- T-cell anergy: Negative response to PPD test
- Treat with steroids
- Resolves spontaneously without treatment
Other Causes of Interstitial Lung Disease
Pulmonary Langerhans Cell Histiocytosis Pulmonary Alveolar Proteinosis Lymphocytic Interstitial Pneumonitis LIP
"Eosinophilic Granuloma"
Description - Tumor of Langerhans histocytes - Surfactant accumulates in intra-alveolar and - Diffuse lymphocyte and plasma
• Do NOT form granulomas bronchiolar spaces infiltration in interstitium and alveolar
- Langerhans cells with eosinophils - Caused by spaces
• Birbeck granules: tennis racket granules in • Defect GM-CSF
Langerhans cells, seen on EM • Pulmonary macrophage dysfunction
- Nodular infiltrates lung, bony sites (ribs) - Heavy lung
- Cough, sputum contain gelatinous material
- PAS +
- Treat with whole lung lavage, GM-CSF therapy
Epid - Young adult smokers - Child: indicates AIDS
- Adult: female predilection
• Sjogren syndrome
• Autoimmune disease
Respi - Path Page 10
Drugs that Cause Interstitial Fibrosis
- Amiodarone
- Bleomycin, busulfan
- Cyclophosphamide
- Methotrexate
- Nitrosurea
Respi - Path Page 11
ARDS
July 1, 2018 8:24 PM
07 Restrictive lung disease - 1, ARDS
Hyaline Membrane
RESPIRATORY DISTRESS SYNDROME
Acute Respiratory Distress Syndrome ARDS Neonatal Respiratory Distress Syndrome
(Diffuse Alveolar Damage) Hyaline Membrane Disease
Diffuse white out Diffuse granularity, ground-glass appearance
Descrip - Diffuse alveolar damage - Respiratory distress due to inadequate surfactant levels
tion - Diagnosis of exclusion
- Patient with normal lungs develop respiratory failure within 1
week alveolar insult, bilateral lung opacities, hypoxemia
Risk - Secondary to diseases - Prematurity:
Factors • Sepsis, infection, shock, aspiration, pancreatitis, • Synthesis begins at week 26, complete at week 35
hypersensitivity reactions, drugs, near drowning • Screen L:S ratio in amniotic fluid to assess lung development
○ Lecithin levels increase as surfactant produced
○ Sphingomyelin remains constant
○ Ratio >2 is adequate
- C-section: lack of stress-induced steroids
• Steroids increase surfactant synthesis
- Maternal diabetes: baby's insulin decreases surfactant production
Patholo - Neutrophils induce protease + ROS damage type I and type III - Surfactant: made by type II pneumocytes
gy pneumocytes ○ Made of lecithin (phosphatidylcholine)
• Endothelial damage = ↑ alveolar capillary permeability ○ Reduces surface tension in lung = prevent alveolar air sac collapse
• Protein-rich fluid leak into alveoli = edema after expiration
• Edema + necrotic epithelial cells = hyaline membrane - No surfactant → atelectasis: lungs collapse, hypoxemia
- Alveolar macrophage digest hyaline membrane ○ CO2 retention → acidosis → pulmonary vasoconstriction and
- Loose fibrosis thickens alveolar septa hypoperfusion
- Get restructure pulmonary parenchyma + cyst ○ Endothelial and epithelial damage → hyaline membrane
Clinical - Hypoxemia and cyanosis with respiratory distress - Increased respiratory effect after birth
Feature • Thick diffusion barrier • Tachypnea
s • Hyaline membrane high surface tension, inward pull = • Accessory muscles
collapse air sacs • Grunting
- Chest X Ray: diffuse white out - Hypoxemia with cyanosis
• Risk PDA
Respi - Path Page 12
• Risk PDA
• Risk necrotizing enterocolitis
- Chest X-Ray: diffuse granularity of lung (ground-glass)
Treatm - Address underlying cause - Supplemental oxygen
ent - Ventilation with positive end-expiratory pressure PEEP • Risk free radial injury
• Leave pressure in lung to prevent collapse when expire ○ Injure retina = blindness
- Recovery may be complicated by interstitial fibrosis ○ Injure heart = intraventricular hemorrhage
• No type II pneumocytes ○ Injure lung = impair development
• Get repair (fibrosis) but no regeneration
Respi - Path Page 13
Pulmonary Vascular Disorders
June 26, 2018 9:22 AM
09 Pulmonary edema, hypertension
10 Pulmonary embolism, pleural disorders
Pulmonary Edema Pulmonary HTN Pulmonary Embolism
Cardiogenic edema: bilateral infiltrate in lung bases with Kerley B lines
Non-cardiogenic edema: bilaterally patchy infiltrates throughout lungs
Westermark's sign: Pulmonary arteries cut off; focal sign of oligemia in one lobe
Smooth muscle hypertrophy with plexiform lesions Hampton's hump: peripheral wedge shape density over diaphragm
Descript - Leakage of interstitial fluid into alveolar space = heavy wet - Normal pulmonary pressure: 10 mmHg - Embolism blocks pulmonary artery
ion lungs - Pulmonary hypertension: 25+ mmHg • Increased Aa gradient
○ Pulmonary trunk atherosclerosis - Saddle embolus: embolus blocks main branches of pulmonary artery
○ Pulmonary artery smooth muscle hypertrophy → sudden death
○ Intimal fibrosis
○ Plexiform lesions in severe, long-standing disease
▪ Capillaries group together
Etiology - Cardiogenic pulmonary edema - Primary pulmonary HTN - DVT → embolize
• LH failure = increases hydrostatic pressure • Young, adult females - Risk factors: Virchow's triad
• Heart failure cells: macrophage with hemosiderin • Mutate BMPR2: proliferate vascular smooth muscle • Stasis
○ RBC extravasate in alveoli - LH disease: systolic/diastolic dysfunction and valve disease • Hypercoagulability
○ Macrophages eat RBC - Lung disease, hypoxia: COPD, lung inflammation/fibrosis, • Endothelial injury
• Jugular venous distention hypoxemic vasoconstriction
• S3 in dilated cardiomyopathy - Recurrent pulmonary embolism
• Chest X-ray: fluid accumulates in basal lobes • cross sectional area of pulmonary vascular bed
• Heart failure cells:
- Alveolar wall injury: direct or blood-transfusion related
- High altitude
Present - Heavy, wet lungs = coughing - Exertional dyspnea - Sudden onset dyspnea and tachypnea
ation - Leads to RV hypertrophy → cor pulmonale - Fever
- Pleuritic chest pain, friction rub
- Expiratory wheezing
Diagnos - Chest X-Ray: normal chest X-Ray
is • Westermark's sign: Pulmonary arteries cut off
• Hampton's hump: wedge shape infiltrate in costodiaphragmatic
corner
- Spiral CT angiography (gold standard)
- Pulmonary angiogram (gold standard to confirm)
- ECG: S1QT3
DIFFUSE PULMONARY HEMORRHAGE SYNDROMES
Goodpasture Syndrome Wegner Granulomatosis with Idiopathic Pulmonary Hemosiderosis
Polyangiitis
Descripti - Autoimmune disease: Anti-GBM bind to pulmonary - Necrotizing granulomatous vasculitis - Intermittent, diffuse alveolar hemorrhage
on alveolar capillary basement membrane hemorrhage with • Lungs
renal failure • Kidney
• Lung • Nasopharynx
• Kidney
- Anti-GBM: circulating auto-antibodies against non-
collagenous domain of α3 chain of collagen type IV
Epidemio - Active smokers - Middle age man with associated organ - Children
logy symptoms
Histology - Lung: focal necrosis of alveolar walls with intra-alveolar
hemorrhages
• Hemosiderin-laden macrophages
- Kidney: crescentic glomerulonephritis
Clinical - Lung: hemoptysis, focal pulmonary consolidation - Lungs: pneumonia, nodular lesions - Insidious onset of cough, hemoptysis, anemia
Features - Kidney: glomerulonephritis, rapidly progressive renal - Kidney: renal disease - focal with diffuse pulmonary infiltrations
Respi - Path Page 14
Features - Kidney: glomerulonephritis, rapidly progressive renal - Kidney: renal disease - focal with diffuse pulmonary infiltrations
failure → hematuria necrotizing/crescentic
glomerulonephritis
- Nasopharynx: sinusitis, ulcers
- Saddle nose
Lab - Anti-GBM - C-ANCA
- Immunofluorescence: linear IF - Immunofluorescence: pauci-immune
- Lung Transplant: for non-neoplastic terminal lung disease
Respi - Path Page 15
Pleural Disorders
June 26, 2018 9:22 AM
10 Pulmonary embolism, pleural disorders
13 Lung cancer - 3, mesothelioma
PLEURAL DISORDERS
- Pleuritis: inflammation of pleura
- Pleural Effusion: fluid accumulates in pleura
- Pneumothorax: air accumulates in pleura
- Mesothelioma: cancer of the pleura
Pleural Effusion
- Accumulation of fluid in pleural space
○ Increased Hydrostatic pressure: CHF
○ Increased Vascular permeability: pneumonia
○ Increased intrapleural negative pressure: atelectasis
○ Decreased Osmotic pressure: nephrotic syndrome
○ Decreased Lymphatic drainage: mediastinal carcinomatosis
- Restrict lung expansion during inspiration
- Effusion:
○ Transudate: clear; due to systemic factors
○ Exudate: cloudy, high in proteins and LDH; due to local factors
▪ Must be drained to avoid infection
- Decreased breath sounds
- Mediastinal shift to opposite side
- Thoracentesis: remove, reduce fluid
Hydrothorax Empyema Hemothorax Malignant Effusion Chylothorax
Fluid Transudate Pus Blood Blood, lymph Lymph, chyle
Associations - Nephrotic syndrome - Bacterial infection - Trauma - lung > breast > lymphoma and - Thoracic duct leak
- Meig's syndrome: ascites, ovarian - Ruptured aortic aneurysm leukemia - Left sided
fibroma, R sided hydrothorax - TAG
Pneumothorax
- Air inside pleural cavity
○ Normally, intrapleural pressure lower than atmospheric pressure = lungs expand, fill with air
○ If air inside pleural cavity, no normal lung expansion
○ Atelectasis: collapsed lung
- Dyspnea, uneven chest expansion
- Symptoms on affected side: chest pain, ↓ tactile fremitus, hyperresonance, diminished breath sounds
○ Pain may radiate to shoulder or back
- Chest X ray: collapsed lung, and can't see vascular markings on that side
Primary Spontaneous Secondary Spontaneous Traumatic Pneumothorax Tension Pneumothorax
Pneumothorax Pneumothorax
- Rupture of apical subpleural bleb - Due to diseased lung - Open: chest wall penetrated, - Air enters pleural space but cannot exit
or cyst (emphysema, infection) outside air enters pleura - Air accumulates inside pleura,
- Tall, thin, young males - Barotrauma: due to mechanical • Air enters through wound, compress lung down
- Collapse portion of lung ventilation with high pressure equalizes pressure - Intrapleural pressure increases >
- Trachea shift towards collapse - Closed: chest wall intact (ex. intrathoracic pressure
Fractured rib) - Trachea shift opposite injury side
- Medical emergency
○ Can put pressure on heart, vital
structures
○ SVC = jugular distention
○ ↑ intrathoracic pressure = ↓ VR,
CO = hypotension
○ Treat with chest tube
Mesothelioma
Solitary Fibrous Tumor Mesothelioma
Respi - Path Page 16
Description - Small tumor attached to pleura by pedicle - Malignant neoplasm of mesothelial cells
- Big, bulky tumours = pleural thickening, encase lung
- Presents with recurrent pleural effusions, dyspnea, chest pain
Histology - Whorls of reticulin - Keratin +
- CD34 + - Epithelial type: calretinin +
- Mesenchymal, sarcamatoid type: spindle cell sarcoma
- Psammoma bodies
Epidemiology - Associated with asbestos exposure
• Lung cancer > mesothelial
• Asbestos bodies stain Prussian blue
Respi - Path Page 17
Lung Cancer
June 26, 2018 9:22 AM
11 Lung cancer -1
12 Lung cancer - 2
13 Lung cancer - 3, mesothelioma
LUNG CANCER
- Most common cause of cancer mortality in US
- Onset age 60+
- Risk factors
○ Cigarette smoke:
▪ 60+ carcinogens: Polycyclic aromatic hydrocarbons, arsenic
▪ Cancer risk related to pack years
○ Radon:
▪ Radon formed by radioactive decay of uranium present in soil
▪ Accumulates in closed spaces, basements
▪ Responsible for most of the public exposure to ionizing radiation
▪ Second most common cause of lung cancer in US
○ Asbestos: lung cancer > mesothelioma
- Non-specific symptoms: cough, hemoptysis, dyspnea, weight loss, post -obstructive pneumonia
- Single Coin lesion on Chest X Ray, noncalcified nodule on CT
- Multiple cannon ball lesions: metastasis from breast, colon; more common than primary lesions
Single Coin Lesions
- Young patients
- Granuloma: TB, histoplasma
- Bronchial harmatoma: benign tumor of lung tissue + cartilage, calcifies in lung
○ Harmatoma: mass of tissue that belongs in that region but is unorganized
○ Popcorn pattern of calcification in lung
Carcinomas
- Arise from single cell type
- Non-small cell carcinoma: surgically resect
- Small cell carcinoma: can't be surgically resected; when present are usually in advanced stage
○ Manage with chemotherapy ± radiation
Small Cell Carcinoma Adenocarcinoma Bronchioalveolar Adenocarcinoma Squamous Cell Carcinoma Large Cell Carcinoma Bronchial Carcinoid Tumor
Histo - Poorly differentiated small cells - Glands or mucin - Columnar cells that grow along - Keratin pearls and - Poorly differentiated large - Well-differentiated
- Arise from Kulchitsky cell - Keratin + pre-existing bronchioles and - Intercellular bridges cells neuroendocrine cells
(neuroendocrine origin) alveoli • Desmosomes connection - No keratin pearls, bridges, • Grow in nests
- Chromogranin + - Arise form Clara cells between squamous cells glands or mucin - Chromogranin +
- Neuron-specific enolase + - Diagnosis of exclusion
Etiology - Male smokers - Non-smokers (most common) - Not related to smoking - Male smokers (most common) - Smoking - Not related to smoking
• Strongest association - Female smokers (most common)
Locatio - Central - Peripheral - Peripheral - Central - Peripheral - Polyp-like mass in bronchus
n
Notes - Rapid growth and early - KRAS, EGFR, ALK - Pneumonia-like hazy consolidation - Hilar mass from bronchus - Poor prognosis - Low grade malignancy
metastasis - Associated with pleural fibrosis, on imaging - Cavitation - Rarely causes carcinoid syndrome
- Myc oncogenes subpleural scars - Excellent prognosis - Paraneoplastic syndrome
- Paraneoplastic syndrome: - May appear irregular until replace • PTHrP: Hypercalcemia - Symptoms due to mass effect or
• ADHSIADH entire lobe (stones, groans, thrones, carcinoid syndrome (flushing,
• ACTH Cushing Syndrome - Associated with hypertrophic psychiatric overtones) diarrhea, wheezing)
• Antibodies against pre- osteoarthropathy: clubbing
synaptic Ca channel →
Eaton-Lambert Syndrome
- If cancer starts with S, it will be associated with smoking, central, and associated with paraneoplastic syndromes
TNM Staging and Complications
T - Size and local extent of tumor
- Block SVC → SVC Syndrome: distended head and neck veins with edema, blue arms and face
- Recurrent laryngeal nerve (of vagus) → hoarseness
- Phrenic nerve → diaphragm paralysis
- Pancoast tumor: apical tumor
N - Regional LN
- Hilar, mediastinal LN
M - May spread to may spread to adrenal gland
- 5 year survival: 15%
Complications
Pancoast Tumor SVC Syndrome
Respi - Path Page 18
Description - Carcinoma in apex of lung, invades cervical - Obstruction SVC impairs blood drainage from upper body
sympathetic chain - Caused by malignancy, mediastinal mass, thrombosis from
indwelling catheters
Presentation - Symptoms due to tumor compressing on local - Upper body edema:
structures • Blanching after finger-tip pressing
- Recurrent laryngeal nerve = hoarseness • Face plethora
- Horner syndrome: ptosis, pinpoint pupil, - Distended jugular vein
anhidrosis - May increase ICP → headache, dizzy, risk aneurysm,
- Brachial plexus: shoulder pain, hand weakness rupture intracranial arteries
- SVC syndrome
- Brachiocephalic vein syndrome:
Respi - Path Page 19
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- HY Neuroanatomy PDFDokumen62 halamanHY Neuroanatomy PDFuhaymidBelum ada peringkat
- HY DermatologyDokumen70 halamanHY DermatologyKimberly KanemitsuBelum ada peringkat
- UW Notes - 3 - MicrobiologyDokumen45 halamanUW Notes - 3 - MicrobiologyKimberly KanemitsuBelum ada peringkat
- HY BiochemDokumen61 halamanHY BiochemKimberly KanemitsuBelum ada peringkat
- DNA Viruses: P P P A H H PDokumen2 halamanDNA Viruses: P P P A H H PKimberly KanemitsuBelum ada peringkat
- Lecturio The 40 Day Study Schedule USMLE Step 1Dokumen20 halamanLecturio The 40 Day Study Schedule USMLE Step 1Kimberly Kanemitsu50% (2)
- Cocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeDokumen2 halamanCocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeKimberly KanemitsuBelum ada peringkat
- Pneumo AlgoDokumen1 halamanPneumo AlgoKimberly KanemitsuBelum ada peringkat
- USMLE Reference Lab ValuesDokumen2 halamanUSMLE Reference Lab ValuesquezacotlBelum ada peringkat
- Renal - PathDokumen23 halamanRenal - PathKimberly KanemitsuBelum ada peringkat
- Path: Pituitary: 01 Pathology of The Pituitary 02 Pathology of The PituitaryDokumen10 halamanPath: Pituitary: 01 Pathology of The Pituitary 02 Pathology of The PituitaryKimberly KanemitsuBelum ada peringkat
- GI - PathDokumen23 halamanGI - PathKimberly KanemitsuBelum ada peringkat
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (120)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- What Is EmphysemaDokumen8 halamanWhat Is EmphysemaHadibah MokhtarBelum ada peringkat
- Revised Curriculum DPT-UHS (15!09!15)Dokumen294 halamanRevised Curriculum DPT-UHS (15!09!15)Iqra Iftikhar50% (2)
- Bronchial Asthma ThesisDokumen33 halamanBronchial Asthma ThesisAbdul Hafiz40% (5)
- High Frequency Ventilation NeorevDokumen16 halamanHigh Frequency Ventilation NeorevLuis Adolfo Gonzalez GomezBelum ada peringkat
- Diagnostic Tests and ProceduresDokumen49 halamanDiagnostic Tests and Procedurespmahi8854Belum ada peringkat
- ABCDE Approach PDFDokumen3 halamanABCDE Approach PDFJohn SmithBelum ada peringkat
- Block 2Dokumen14 halamanBlock 2PaolaBelum ada peringkat
- Blueprint For Final Exam - Doc Health AssessmentDokumen13 halamanBlueprint For Final Exam - Doc Health AssessmentKim DepapeBelum ada peringkat
- Icmcrj 1 1012Dokumen2 halamanIcmcrj 1 1012Shivaramakrishna SriramojuBelum ada peringkat
- Chest Physiotherapy in Mechanically Ventilated Children A ReviewDokumen10 halamanChest Physiotherapy in Mechanically Ventilated Children A Reviewmrizki_1Belum ada peringkat
- Respiratory System Assessment PDFDokumen53 halamanRespiratory System Assessment PDFJay RomeBelum ada peringkat
- GOLD 2023 Teaching Slide Set v1.0 1nov2022Dokumen59 halamanGOLD 2023 Teaching Slide Set v1.0 1nov2022Nattapatt LimloustrakulBelum ada peringkat
- Atlas of The Newborn Volume 5 PDFDokumen229 halamanAtlas of The Newborn Volume 5 PDFAntohi CatalinBelum ada peringkat
- Lec # 2 Non-Respiratory Function of LungsDokumen13 halamanLec # 2 Non-Respiratory Function of LungssamotherlianBelum ada peringkat
- Eaton County Apparent Drowning Death UnidentifiedDokumen5 halamanEaton County Apparent Drowning Death UnidentifiedFergus BurnsBelum ada peringkat
- Pathophysiology of Pneumonia: Amalia Alco N, MD, PHD, Neus Fa'Bregas, MD, PHD, Antoni Torres, MD, PHDDokumen8 halamanPathophysiology of Pneumonia: Amalia Alco N, MD, PHD, Neus Fa'Bregas, MD, PHD, Antoni Torres, MD, PHDVinicius SpazzapanBelum ada peringkat
- Cancer - Rath, Matthias PDF (Pauling-Rath Therapy Protocol: Vitamin C and Lysine)Dokumen84 halamanCancer - Rath, Matthias PDF (Pauling-Rath Therapy Protocol: Vitamin C and Lysine)Anonymous Jap77xvqPKBelum ada peringkat
- Patent Ductus ArteriosusDokumen49 halamanPatent Ductus Arteriosusarchana vermaBelum ada peringkat
- KINE 2031 Test 4 NotesDokumen16 halamanKINE 2031 Test 4 NotesnokiaBelum ada peringkat
- TB Radiology Basic Presentation SlidesDokumen72 halamanTB Radiology Basic Presentation SlidesSherwin ManuekeBelum ada peringkat
- Elmer D. Barber - Osteopathy Complete, 1898Dokumen586 halamanElmer D. Barber - Osteopathy Complete, 1898serpecBelum ada peringkat
- Community-Acquired Pneumonia PathophysiologyDokumen2 halamanCommunity-Acquired Pneumonia PathophysiologyFrancis Adrian83% (12)
- Case - Study (PCAP)Dokumen27 halamanCase - Study (PCAP)Cherry Ann BalagotBelum ada peringkat
- Hospital & Clinical PharmacyDokumen27 halamanHospital & Clinical PharmacyDR.MAHESHBelum ada peringkat
- Emphysema: Symptoms & Causes Diagnosis & Treatment Doctors & Departments PrintDokumen4 halamanEmphysema: Symptoms & Causes Diagnosis & Treatment Doctors & Departments PrintAlfrien Ivanovich LarchsonBelum ada peringkat
- Approaches To Pulmonary Drug Delivery SystemsDokumen8 halamanApproaches To Pulmonary Drug Delivery SystemsonovBelum ada peringkat
- Copd Cad Pathophysiology (Revised)Dokumen3 halamanCopd Cad Pathophysiology (Revised)Israel Soria EsperoBelum ada peringkat
- Ebook Diagnostic Imaging Chest PDF Full Chapter PDFDokumen67 halamanEbook Diagnostic Imaging Chest PDF Full Chapter PDFjade.burrow118100% (32)
- Health and Saftey Notes (Comp)Dokumen44 halamanHealth and Saftey Notes (Comp)brotherkh26Belum ada peringkat
- SyllabusDokumen6 halamanSyllabusRafkha HakamBelum ada peringkat