Diabetes Melitus Gestasional
Diunggah oleh
Fatimah QonitahHak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Diabetes Melitus Gestasional
Diunggah oleh
Fatimah QonitahHak Cipta:
Format Tersedia
International Surgery Journal
Bhardwaj R et al. Int Surg J. 2018 Sep;5(9):2991-2994
http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902
DOI: http://dx.doi.org/10.18203/2349-2902.isj20183451
Original Research Article
Pre-operative factors for predicting a difficult
laparoscopic cholecystectomy
Rajni Bhardwaj1, Rajandeep Singh Bali1*, Yawar Zahoor2
1
Department of General Surgery, Government Medical College, Jammu and Kashmir, India
2
Department of General Surgery, Maulana Azad Medical College, Delhi, India
Received: 24 July 2018
Accepted: 07 August 2018
*Correspondence:
Dr. Rajandeep Singh Bali,
E-mail: rajandeepbali@gmail.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Background: Laparoscopic cholecystectomy is a very safe procedure yet there are instances where serious
complications can be avoided and better managed if the surgeon is forewarned or prepared in advance for them. So, a
need is felt to identify pre-operative parameters for anticipating a difficult cholecystectomy.
Methods: This study was carried over a period of two years (2007- 2009). Patients having symptomatic cholelithiasis
willing to undergo laparoscopic cholecystectomy were enrolled in the study. The following pre-operative parameters
were evaluated in the study: age, sex, body mass index, history of previous abdominal surgery, history of acute
cholecystitis, history of biliary colic, palpable lump in right hypochondrium, experience of the surgeon and abdominal
ultrasonogram (following parameters were noted increased gallbladder wall thickness, number of stones, size of
largest stone and its location).
Results: Acute cholecystitis, palpable gall bladder, increased gallbladder wall thickness, biliary colic, gall stones >2
cm in size, gall stone impacted at gallbladder neck and BMI >30 kg/m2 had a significant p-value in a difficult
laparoscopic cholecystectomy.
Conclusions: Further research is needed to formulate a score based on the variables mentioned above to predict a
difficult laparoscopic cholecystectomy and hence letting the surgeon be better prepared for any eventualities that he
encounters whilst performing laparoscopic cholecystectomy.
Keywords: BMI, Cholecystectomy, Difficult, Laparoscopic
INTRODUCTION of all the cholecystectomies performed for gall stone
disease are laparoscopic cholecystectomies.4 Although a
In 1882 Carl Johann Langenbuch performed the first safe procedure, instances arise when it becomes a very
open cholecystectomy for cholelithiasis, since then it was difficult and cumbersome procedure due to reasons like
the procedure of choice in the management of gall stone difficulty in accessing the peritoneal cavity, identifying
disease.1 Cholelitiasis is a very common disease with a the relevant anatomy, creating pneumoperitoneum,
prevalence of 4% in India.2 Since the advent of anatomical variations, adhesiolysis, extracting the gall
laparoscopy and the obvious advantages of better bladder from the peritoneal cavity and long duration of
cosmesis, less post-operative pain, early recovery, etc., surgery itself.5 In view of these, laparoscopic
laparoscopic cholecystectomy has become the gold cholecystectomy has been classified by some authors as
standard of treatment for gall stone disease.3 Nearly 80% easy (time taken for surgery <60 minutes, no bile
International Surgery Journal | September 2018 | Vol 5 | Issue 9 Page 2991
Bhardwaj R et al. Int Surg J. 2018 Sep;5(9):2991-2994
spillage, no injury to duct/artery), difficult (time taken for thickness was evaluated as dichotomous variable (≥3mm
surgey is 60-120 mins, bile/ stone spillage, injury to duct, versus ≤3mm). Gall bladder calculus size was defined as
no conversion to open cholecystectomy) and very maximum diameter of the largest stone and was evaluated
difficult (time taken >120 mins, conversion to open as <2 cm versus >2 cm as a dichotomous variable. Gall
cholecystectomy).6 bladder calculus number was defined as solitary or
multiple. Stone mobility was assessed by scanning the
The present study was undertaken to identify various patient in supine and left lateral position. If the gall stone
factors associated with laparoscopic cholecystectomy, moved as the patient’s position changed, the stones were
that may help us in predicting or anticipating a difficult considered mobile. Experience of the surgeon was taken
laparoscopic cholecystectomy beforehand in the pre- as a dichotomous variable (>200 cases versus <200
operative period, hence allowing the surgeon to prepare cases).
in advance for the difficulties encountered during the
procedure, thus reducing the morbidity and mortality with Intra-operative assessment of the difficulty encountered,
a difficult laparoscopic cholecystectomy. if any, was noted in each case. The cases which were
converted to open surgery were noted. The criteria for
METHODS technical difficulty were problems encountered due to
equipment, amount of time taken for completion of
This study was carried over a period of two years (2007- procedure i.e., insertion of veress needle to removal of
2009) at Government Medical College, Srinagar, Jammu last trocar and cannula (more or less than 90 minutes),
and Kashmir. The patients having symptomatic amount of bleeding (mild, moderate or severe), anatomy
cholelithiasis willing to undergo laparoscopic of calot’s triangle (clear/unclear), adhesions
cholecystectomy were enrolled in the study. Patients (partial/dense), difficulty in extracting the gallbladder
having surgical jaundice, choledocholelithiasis or any (present/absent) and spillage of bile or stones in the
contraindication for general anaesthesia were excluded peritoneal cavity (present/absent). All the cases which
from the study. were technically difficult or converted to open
cholecystectomy were grouped into the category of cases
The patients were evaluated prior to undergoing with intra-operative difficulty during laparoscopic
laparoscopic cholecystectomy with a detailed history and cholecystectomy and the cases where no significant
examination followed by all the relevant investigations technical difficulty was encountered were grouped
(complete blood counts, liver function tests, kidney separately as cases with no intra-operative difficulty. The
function tests, blood sugar levels, serum electrolytes, ultrasonographic finding recorded preoperatively were
electrocardiogram, coagulation profile, chest skiagram also confirmed during operative surgery.
and ultrasonography of the abdomen). An abdominal
ultrasound was done preoperatively after overnight The objective of this study was to identify pre-operative
fasting and then within two week of surgery and the data parameters for anticipating a difficult cholecystectomy.
relevant to the study was collected. On the basis of data
collected, the following pre-operative parameters were RESULTS
considered in the study: age, sex, body mass index,
history of previous abdominal surgery, history of acute We operated upon a total of 100 patients, who were
cholecystitis, history of biliary colic, palpable lump in enrolled in our study as subjects. The number of male and
right hypochondrium, experience of the surgeon and on female patients in our study group were 30 and 70
ultrasonography the following parameters were noted respectively.
increased gallbladder wall thickness, number of stones,
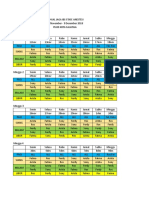
size of largest stone and its location . Table 1: Preoperative variables.
Age and body habitus were evaluated as dichotomous Preoperative variables N
variables, i.e., >65 years and <65 years and obese (BMI Age (> 65 yr) 7
>30 kg/m2) and non-obese (BMI <30kg/m2) respectively. Males 30
BMI (>30 kg/m2) 33
Previous abdominal surgery was categorized as having no H/O previous abdominal surgery 20
previous abdominal surgery and having undergone H/O previous attack of acute cholecystitis 16
previous intra-abdominal surgery. Single attack 52
Multiple attack 32
History of acute cholecystitis was taken as severe right
upper quadrant pain radiating to the inferior angle of H/O biliary colic (> 10 attacks) 10
scapula or shoulder, vomiting, fever, requiring admission Lump in right hypochondrium 6
to the Emergency Department or any previous GB wall thickness (>3 mm) 23
ultrasonographic documentation of an episode of acute Size of largest stone (> 2 cms) 20
cholecystitis within 8 weeks of undergoing the present Impacted stone at neck of gall bladder 20
laparoscopic cholecystectomy. Gall bladder wall Multiple calculi on USG 75
International Surgery Journal | September 2018 | Vol 5 | Issue 9 Page 2992
Bhardwaj R et al. Int Surg J. 2018 Sep;5(9):2991-2994
The age distribution from the youngest to the oldest laparoscopic cholecystectomy (p-value 0.012) and
subject was 15 and 74 years respectively. The commonest insignificant for solitary episode of acute cholecystitis
age group to be operated upon was 25-34 years. The and intraoperative difficulty during laparoscopic
preoperative factors assessed in our study are shown in cholecystectomy (p-value 0.485).
Table 1.
We also found a significant relation between
No significant association was found between the age, intraoperative difficulty during laparoscopic
gender of the patients or history of previous surgery and cholecystectomy and pre-operative palpable gall bladder
intra-operative difficulty during laparoscopic lump (p-value 0.003), increased gall bladder wall
cholecystectomy in our study group. We found a thickness (p-value 0.000), biliary colic (p-value 0.029),
significant relation between acute cholecystitis and size of largest gallstone (p-value 0.00), location of
intraoperative difficulty during laparoscopic gallstone at the neck (impacted) of the gall bladder
cholecystectomy with p-value being 0.024. The relation (0.000) and BMI (p-value 0.005). The comparison of the
was strongly significant between multiple episodes of ultrasonographic and intraoperative findings is shown in
acute cholecystitis and intraoperative difficulty during Table 2.
Table 2: Comparison between ultrasonographic findings and intra-operative findings.
Findings Ultrasonographic Operative p value
Gall stone 100 100 1.000
Gall bladder wall ≥3 mm 23 25
0.741
thickness <3 mm 77 75
>2 cm 20 19
Size of largest calculi 0.858
≤2 cm 80 81
Impacted 20 21
Location of GB stone 0.861
Unimpacted 80 79
Present 75 80
Multiple calculi 0.397
Absent 25 20
Twenty two patients took more than 90 mins intra- was found by us between previous attacks of acute
operative time to undergo the laparoscopic cholesystitis and intra-operative difficulty during
cholecystectomy, difficult anatomy was encountered in laparoscopic cholecystectomy. Similar findings have
14 patients, bleeding (>100 ml) occurred in 11 patients, been corraborated by various authors in litreature.10-12
adhesions with subsequent adhesiolysis was performed in Some authors have reported no significant relation
20 patients, intra-peritoneal gall bladder contents spillage between gall bladder wall thickness and a difficult
occurred in 36 patients (stones along with bile and bile laparoscopic cholecystectomy whilst others have reported
alone were spilled in 10 and 26 patients respectively), it to be significant.8,13 Present study found this relation to
difficulty in gall bladder extraction occurred in 20 be statistically significant.
patients and conversion to open cholecystectomy
happened in 3 cases. Gall stone impacted at the neck of the gall bladder and
size of the largest stone showed a significant relation with
DISCUSSION difficult laparoscopic cholecystectomy. In the litreature
certain authors have reported similar findings whilst
Laparoscopic cholecystectomy is considered as the gold others do not concur with it.8,13 Patients having BMI more
standard for the treatment of cholelithiasis.3 Various than 30 was significantly related to difficult
criteria have been identified for predicting a difficult cholecystectomy, the difficulty arose while gaining intra-
laparoscopic cholecystectomy like male gender, obesity, peritoneal access, dissecting at calots triangle due to
geriartic patients, recurrent episodes of acute excess fat and while extracting the gall bladder and its
cholecystitis, thick walled gall bladder and contracted contents from the peritoneal cavity. Various authors have
gall bladder.7 reported similar findings.6,8
We found no association between age/ gender/ history of CONCLUSION
previous abdominal surgery with intra-operative
difficulty during laparoscopic cholecystectomy in our In the present study, acute cholecystitis, palpable gall
study. These findings are consistent with other studies bladder, increased gallbladder wall thickness, biliary
conducted by various authors.8-10 A significant relation colic, gall stones >2 cm in size, gall stone impacted at
International Surgery Journal | September 2018 | Vol 5 | Issue 9 Page 2993
Bhardwaj R et al. Int Surg J. 2018 Sep;5(9):2991-2994
gallbladder neck and BMI >30 kg/m2 had a significant p- 7. Jansen S, Caplehorn J. Preoperative ultrasound to
value in a difficult laparoscopic cholecystectomy. Further predict conversions in laparoscopic
research is needed to formulate a score based on the cholecystectomy. Surg laparosc Endosc.
variables mentioned above to predict a difficult 1997;7:121-3.
laparoscopic cholecystectomy, hence letting the surgeon 8. Gupta AK, Shiwach N, Gupta S, Gupta S, Goel A,
be better prepared for any eventualities that he encounters Bhagat TS. Predicting difficult laparoscopic
whilst performing laparoscopic cholecystectomy. cholecystectomy. Int Surg J. 2018;5(3):1094-9.
9. Schrenk P, Woisetschlager R. Laparoscopic
Funding: No funding sources cholecystectomy. Surg Endosc. 1995;9:25.
Conflict of interest: None declared 10. Kanaan SA, Murayama KM, Merriam LT, Dawes
Ethical approval: The study was approved by the LG, Rege RV, Joehl RJ. Risk factors for conversion
Institutional Ethics Committee of laparoscopic to open cholecystectomy. J Surg
Res. 2002;106(1):20-4.
REFERENCES 11. Kama NA, Kolongue M, Doganay M, Reis E, Atle
M, Dolapiu M. Risk score conversion from
1. Singh K, Ohri A. Difficult laparoscopic laparoscopic to open cholecystectomy. Am J Surg.
cholecystectomy: A large series from north India. 2001;181:520-5.
Indian J Surg. 2006;68:205-8. 12. Fried GM, Barkun JS, Sigman HH, Joseph L, Uas
2. Tendon R. Diseases of gall bladder and biliary tract. D, Garzon J, et al. Factors determining conversion
In: Shah SN, eds. API Text Book of Medicine. 7th to laparotomy in patient undergoing laparoscopic
Ed. Jaypee Brothers Medical Publishers; 2003:642- choleystectomy. Am J Surg. 1994;167:35-41.
4. 13. Lal P, Agarwal PN, Malik VK, Chakravarti AL. A
3. Ibrahim S, Hean TK, Ho LS, Ravintharan T, Chye difficult laparoscopic cholecystectomy that requires
TN, Chee CH. Risk factors for conversion to open conversion to open procedure can be predicted by
surgery in patients undergoing laparoscopic preoperative ultrasonography. JSLS. 2002;6(1):59.
cholecystectomy. World J Surg. 2006;30:1698-704.
4. Zinner MJ, Ashley SW. Maingots abdominal
Operations. Tata McGraw - Hill Education; 2013.
5. Vivek MAKM, Augustine AJ, Rao R. A
comprehensive predicting scoring method for
difficult laparoscopic cholecystectomy. J Minim Cite this article as: Bhardwaj R, Bali RS, Zahoor Y.
Access Surg. 2014;10(2):62-7. Pre-operative factors for predicting a difficult
6. Randhawa JS, Pujahari Ak. Preoperative prediction laparoscopic cholecystectomy. Int Surg J
of difficult lap chole: a scoring method. Indian J 2018;5:2991-4.
Surg. 2009:71:198-201.
International Surgery Journal | September 2018 | Vol 5 | Issue 9 Page 2994
Anda mungkin juga menyukai
- Laparoscopic Cholecystectomy:An Experience of 200 Cases: Original ArticleDokumen4 halamanLaparoscopic Cholecystectomy:An Experience of 200 Cases: Original ArticleAndrei GheorghitaBelum ada peringkat
- Original Research ArticleDokumen9 halamanOriginal Research ArticleAnand ShanmugaiahBelum ada peringkat
- Laparoscopic Ventral Hernia Repair With Tacker Only Mesh Fixation: Single Centre ExperienceDokumen5 halamanLaparoscopic Ventral Hernia Repair With Tacker Only Mesh Fixation: Single Centre ExperienceMudassar SattarBelum ada peringkat
- A Profile of Fundus First LapaDokumen5 halamanA Profile of Fundus First LapaRony RonyBelum ada peringkat
- JurnalDokumen9 halamanJurnalFrans 'cazper' SihombingBelum ada peringkat
- Cole Dificl - IndiaDokumen3 halamanCole Dificl - IndiaJulioRoblesZanelliBelum ada peringkat
- LaparosDokumen5 halamanLaparosJoyi KimBelum ada peringkat
- Colecistectomia Dificil PredictoresDokumen9 halamanColecistectomia Dificil PredictoresAndres Neira QuezadaBelum ada peringkat
- Role of Endoscopic Stent Insertion On Managmeent of Gastric Twist After Sleeve GastrectomyDokumen6 halamanRole of Endoscopic Stent Insertion On Managmeent of Gastric Twist After Sleeve GastrectomyJorge SalazarBelum ada peringkat
- Is 9Dokumen9 halamanIs 9intan juitaBelum ada peringkat
- Combined Laparoscopic Pyelolithotomy and Endoscopic Pyelolithotripsy For Staghorn Calculi: Long-Term Follow-Up Results From A Case SeriesDokumen6 halamanCombined Laparoscopic Pyelolithotomy and Endoscopic Pyelolithotripsy For Staghorn Calculi: Long-Term Follow-Up Results From A Case SeriesantonBelum ada peringkat
- Evaluation of Early Cholecystectomy For Acute Cholecystitis Within 10 Days of 7780Dokumen5 halamanEvaluation of Early Cholecystectomy For Acute Cholecystitis Within 10 Days of 7780Jemimah BureresBelum ada peringkat
- 01 HepatogastroDokumen3 halaman01 Hepatogastroyacine26Belum ada peringkat
- Lap Chole ArticleDokumen6 halamanLap Chole Articlealaiza13conoconoBelum ada peringkat
- Bun V34N3p223Dokumen6 halamanBun V34N3p223pingusBelum ada peringkat
- Validation of G10 Classification in Laparoscopic Cholecystectomy For The Prediction of Operative Difficulties: An Observational StudyDokumen8 halamanValidation of G10 Classification in Laparoscopic Cholecystectomy For The Prediction of Operative Difficulties: An Observational StudyIJAR JOURNALBelum ada peringkat
- Complicationsoflapmyomectomy ANZ 2010Dokumen7 halamanComplicationsoflapmyomectomy ANZ 2010Nadila 01Belum ada peringkat
- Predictive Factors For Conversion of Laparoscopic CholecystectomyDokumen4 halamanPredictive Factors For Conversion of Laparoscopic CholecystectomyGilang IrwansyahBelum ada peringkat
- A Novel Technique For Treatment of Distal Ureteral Calculi: Early ResultsDokumen4 halamanA Novel Technique For Treatment of Distal Ureteral Calculi: Early ResultsTheQueensafa90Belum ada peringkat
- Acute Intestinal ObstructionDokumen9 halamanAcute Intestinal ObstructionRoxana ElenaBelum ada peringkat
- Laparoscopic Appendicectomy in Appendicular LumpDokumen2 halamanLaparoscopic Appendicectomy in Appendicular LumpinventionjournalsBelum ada peringkat
- Transvaginal MorcellationDokumen8 halamanTransvaginal Morcellationsanjayb1976gmailcomBelum ada peringkat
- 2015 Laparoscopic Surgery in Abdominal Trauma A Single Center Review of A 7-Year ExperienceDokumen7 halaman2015 Laparoscopic Surgery in Abdominal Trauma A Single Center Review of A 7-Year ExperiencejohnnhekoBelum ada peringkat
- 65 Stenoza GDDDokumen7 halaman65 Stenoza GDDGabriela MilitaruBelum ada peringkat
- 2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesDokumen11 halaman2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesOlteanu IonutBelum ada peringkat
- Short-Term Surgical and Long-Term Survival Outcomes After Laparoscopic Distal Gastrectomy With D Lymphadenectomy For Gastric CancerDokumen7 halamanShort-Term Surgical and Long-Term Survival Outcomes After Laparoscopic Distal Gastrectomy With D Lymphadenectomy For Gastric CancerThế VũBelum ada peringkat
- Versus: Laparoscopic Open Appendectomy: Which Way To Go?Dokumen6 halamanVersus: Laparoscopic Open Appendectomy: Which Way To Go?Claudiu Ungureanu ClauBelum ada peringkat
- 5 - Temporary Placement of Covered Self-Expandable Metal Stents PDFDokumen9 halaman5 - Temporary Placement of Covered Self-Expandable Metal Stents PDFMahdi ShareghBelum ada peringkat
- Laparoscopic Repair of Vesicovaginal FistulaDokumen4 halamanLaparoscopic Repair of Vesicovaginal FistulaGloria AteBelum ada peringkat
- Emergency Cholecystectomy in Situs Inversus Totalis: Report of A CaseDokumen3 halamanEmergency Cholecystectomy in Situs Inversus Totalis: Report of A CaseHazel Joy Bragado TungpalanBelum ada peringkat
- Cistectomia Radical Art08 PDFDokumen7 halamanCistectomia Radical Art08 PDFJoshua GardnerBelum ada peringkat
- Surgery Open Digestive Advance: G. Pasinato, J.-M RegimbeauDokumen7 halamanSurgery Open Digestive Advance: G. Pasinato, J.-M RegimbeauRashmeeta ThadhaniBelum ada peringkat
- 2012 Article 625 PDFDokumen5 halaman2012 Article 625 PDFPutri AdimuktiBelum ada peringkat
- International Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. ChitheerDokumen7 halamanInternational Journal of Surgery Open: Tariq Al-Aubaidi, Basim R. Ghadhban, Samer S. Chitheersamer falconBelum ada peringkat
- UEG Week 2014 Poster PresentationsDokumen1 halamanUEG Week 2014 Poster PresentationsAnonymous QvIxEazXGdBelum ada peringkat
- 10.1177 2050640614548980Dokumen474 halaman10.1177 2050640614548980Junaidi Effendi0% (1)
- Southwell2015 PDFDokumen8 halamanSouthwell2015 PDFCharbel HannaBelum ada peringkat
- Sleeve 17 PDFDokumen7 halamanSleeve 17 PDFAlain GarcíaBelum ada peringkat
- Cytoreductive Surgery and IntraperitonealDokumen11 halamanCytoreductive Surgery and IntraperitonealJorge FallasBelum ada peringkat
- Lasers: Outpatient Transurethral Cystolithotripsy of Large Bladder Stones by Holmium LaserDokumen4 halamanLasers: Outpatient Transurethral Cystolithotripsy of Large Bladder Stones by Holmium LaserSteve aokiBelum ada peringkat
- Europian Surgical Abstract 2 PDFDokumen114 halamanEuropian Surgical Abstract 2 PDFDrAmmar MagdyBelum ada peringkat
- Open Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective StudyDokumen3 halamanOpen Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective Study'Adil MuhammadBelum ada peringkat
- Colonic Self Expanding Metallic Stents (SEMS) Indications & ContraindicationsDokumen14 halamanColonic Self Expanding Metallic Stents (SEMS) Indications & Contraindicationssamer falconBelum ada peringkat
- 1 s2.0 S0016510723030390 MainDokumen8 halaman1 s2.0 S0016510723030390 MainJesús MaríñezBelum ada peringkat
- Prediction of Difficulties in Laparoscopic Cholecystectomy On The Base of Routinely Available Parameters in A Smaller Regional HospitalDokumen8 halamanPrediction of Difficulties in Laparoscopic Cholecystectomy On The Base of Routinely Available Parameters in A Smaller Regional Hospitalagha_niceBelum ada peringkat
- Periop UrologyKoubaartikelDokumen4 halamanPeriop UrologyKoubaartikeljustin_saneBelum ada peringkat
- Anatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFDokumen10 halamanAnatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFannisa ussalihahBelum ada peringkat
- Treatmen 3Dokumen6 halamanTreatmen 3Livia GudacBelum ada peringkat
- Art:10.1007/s00192 012 1940 7Dokumen8 halamanArt:10.1007/s00192 012 1940 7Muhammad AL Farisi SutrisnoBelum ada peringkat
- 5 3 27 103Dokumen6 halaman5 3 27 103Khaled MonazeaBelum ada peringkat
- Diagnosing Gastric Volvulus in Chest X-Ray: Report of Three CasesDokumen4 halamanDiagnosing Gastric Volvulus in Chest X-Ray: Report of Three CasesSuraj KurmiBelum ada peringkat
- 10.1007@s11605 018 04090 ZDokumen11 halaman10.1007@s11605 018 04090 ZGabriel RangelBelum ada peringkat
- Jurnal 1 PDFDokumen5 halamanJurnal 1 PDFsabila_chaBelum ada peringkat
- 1 s2.0 S0022480423002895 MainDokumen7 halaman1 s2.0 S0022480423002895 Mainlucabarbato23Belum ada peringkat
- Jurnal Bedah - Elsy MulyaDokumen14 halamanJurnal Bedah - Elsy MulyaariesfadhliBelum ada peringkat
- Ureteral Catheter Placement For Prevention of UreteralDokumen6 halamanUreteral Catheter Placement For Prevention of UreteralKharizmaBelum ada peringkat
- Jandrol 112 016444Dokumen7 halamanJandrol 112 016444Павел ГичакBelum ada peringkat
- Versus Conventional Laparoscopic Cholecystectomy: Randomized Clinical Trial of Laparoendoscopic Single-SiteDokumen8 halamanVersus Conventional Laparoscopic Cholecystectomy: Randomized Clinical Trial of Laparoendoscopic Single-SitepotatoBelum ada peringkat
- Procedural Difficulty Differences According To TumDokumen11 halamanProcedural Difficulty Differences According To TumDaniel Gonzales LinoBelum ada peringkat
- Post-cholecystectomy Bile Duct InjuryDari EverandPost-cholecystectomy Bile Duct InjuryVinay K. KapoorBelum ada peringkat
- Gabungan 3Dokumen69 halamanGabungan 3Fatimah QonitahBelum ada peringkat
- Contact Dermatitis Guidelines 2017Dokumen13 halamanContact Dermatitis Guidelines 2017Imam Muhamad RissandyBelum ada peringkat
- IbdDokumen2 halamanIbdFatimah QonitahBelum ada peringkat
- Demertzi VS2009 PDFDokumen10 halamanDemertzi VS2009 PDFFatimah QonitahBelum ada peringkat
- Peran GNRHDokumen7 halamanPeran GNRHMerliana DebyantiBelum ada peringkat
- FIGO Dosage Chart en 0Dokumen1 halamanFIGO Dosage Chart en 0Rosi Indah100% (1)
- Jadwal Igd NeuroDokumen1 halamanJadwal Igd NeuroFatimah QonitahBelum ada peringkat
- Guidelines For The Treatment of Drug-Susceptible Tuberculosis (TB) and Patient Care 2017 PDFDokumen80 halamanGuidelines For The Treatment of Drug-Susceptible Tuberculosis (TB) and Patient Care 2017 PDFILa' ArmiLa LomatBelum ada peringkat
- Andrews 2018Dokumen64 halamanAndrews 2018Daniar N. Hanifah100% (1)
- LIVER SlidesDokumen144 halamanLIVER SlidesChiiraq EugeneBelum ada peringkat
- The Gallbladder AnatomyDokumen10 halamanThe Gallbladder AnatomyClaudia IlieBelum ada peringkat
- Common Postoperative Findings Unique To Laparoscopic SurgeryDokumen21 halamanCommon Postoperative Findings Unique To Laparoscopic SurgeryMoises MolinaBelum ada peringkat
- Gallstone Case StudyDokumen19 halamanGallstone Case StudyMoNa JbaReenBelum ada peringkat
- Acute CholecystitisDokumen18 halamanAcute CholecystitisOktavia PutriBelum ada peringkat
- 8 - Disorders of The GallbladderDokumen33 halaman8 - Disorders of The Gallbladdersohaib salamehBelum ada peringkat
- Preboard Exam D - Test 3: Medical Surgical Nursing Exam: Answers & RationaleDokumen11 halamanPreboard Exam D - Test 3: Medical Surgical Nursing Exam: Answers & RationaleHasan A AsFourBelum ada peringkat
- Clinical Spotlight Review - Management of Choledocholithiasis - A SAGES PublicationDokumen15 halamanClinical Spotlight Review - Management of Choledocholithiasis - A SAGES PublicationMu TelaBelum ada peringkat
- Case 052: Biliary ColicDokumen4 halamanCase 052: Biliary ColicZauzaBelum ada peringkat
- General Surgery Logbook Survey - Royal College of Surgeons of England - BulletinDokumen6 halamanGeneral Surgery Logbook Survey - Royal College of Surgeons of England - BulletinEd FitzgeraldBelum ada peringkat
- Esophageal DisordersDokumen10 halamanEsophageal DisordersSheema ShBelum ada peringkat
- Laparoscopic Drainage of Pancreatic Pseudocysts 1584 9341 11 3 8Dokumen4 halamanLaparoscopic Drainage of Pancreatic Pseudocysts 1584 9341 11 3 8ciuca bogdanBelum ada peringkat
- Hepatobiliary ExamDokumen15 halamanHepatobiliary ExamEms Rio Bal0% (1)
- Medical Surgical NursingDokumen24 halamanMedical Surgical NursingWilmaBongotanPadawilBelum ada peringkat
- E000675 FullDokumen37 halamanE000675 Fullmartina silalahiBelum ada peringkat
- Cholelithiasis (Case Presentation)Dokumen19 halamanCholelithiasis (Case Presentation)Ian CiarBelum ada peringkat
- Serology and Ultrasound For Diagnosis of Choledocolitiasis 2014Dokumen5 halamanSerology and Ultrasound For Diagnosis of Choledocolitiasis 2014DannyBelum ada peringkat
- Case Study CholeDokumen38 halamanCase Study CholeMerlene Sarmiento Salunga0% (1)
- Konversi Kode Prosedure INACBGs Ke Kode ICD 9-CMDokumen349 halamanKonversi Kode Prosedure INACBGs Ke Kode ICD 9-CMTri Muhammad HaniBelum ada peringkat
- Scheins Common Sense. Prevention and Management of Surgical Complications 2013Dokumen576 halamanScheins Common Sense. Prevention and Management of Surgical Complications 2013Uffie-Isabela Ghe100% (3)
- CholecystectomyDokumen5 halamanCholecystectomydkbjBelum ada peringkat
- Surgery Oral ExamDokumen46 halamanSurgery Oral ExamM Patel100% (9)
- Medicine Colloquium Exam - 2015 ADokumen41 halamanMedicine Colloquium Exam - 2015 ArachaBelum ada peringkat
- Liver MCQ SurgeryDokumen114 halamanLiver MCQ Surgerydrnsatyaprasad100% (3)
- Cholecystectomy 4 PrintingDokumen19 halamanCholecystectomy 4 PrintingKyle Punzalan100% (2)
- Aga Section: American Gastroenterological Association Institute Guideline On Initial Management of Acute PancreatitisDokumen6 halamanAga Section: American Gastroenterological Association Institute Guideline On Initial Management of Acute PancreatitisEdgar LoezaBelum ada peringkat
- Case Presentation On CholelithiasisDokumen24 halamanCase Presentation On CholelithiasisLouie Kem Anthony Babaran100% (1)
- Jaundice: Slide 001Dokumen91 halamanJaundice: Slide 001mel_napsterBelum ada peringkat
- Biliary Dyskinesia PathoDokumen2 halamanBiliary Dyskinesia PathoRaenell CurryBelum ada peringkat
- Jurnal MRCPDokumen18 halamanJurnal MRCPMaharani Eka SaputriBelum ada peringkat