5H 5T
Diunggah oleh
Felicia SutarliDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
5H 5T
Diunggah oleh
Felicia SutarliHak Cipta:
Format Tersedia
5H 5T
Tachycardias
Narrow QRS Complex – Stable
Regular:
Attempt vagal maneuvers.
first line Rx is: Adenosine 1st dose: 6mg IV then 2nd and 3rd doses: 12mg IV
Other Rx options include: Diltiazem and Beta blockers
Irregular:
Rx options include: Diltiazem and Beta blockers
Narrow QRS Complex – Unstable
Sedate the patient and provide cardioversion.
Tx Atrial Fibrillation: first shock 100-200j
Tx Atrial flutter and SVT: first shock 50-100j
Wide Complex – Stable
Regular:
Ventricular Tachycardia (monomorphic):
Sedate the patient and provide cardioversion.
Amiodarone 150mg IV over 10 min every 3-5 min, with a max of 2.2g in a 24hrs period.
Procainamide 20 to 50 mg/min IV until arrhythmia resolves, hypotension occurs, there is >50%
increase in QRS duration, or the max dose of 17 mg/kg is reached (Maintenance infusion: 1 to 4
mg/min)
Sotalol 1.5 mg/kg over 5 min
Procainamide and sotalol should be avoided in patients with prolonged QT.
SupraVentricular Tachycardia (SVT) with Aberrancy:
Adenosine 1st dose: 6mg IV then 2nd and 3rd doses: 12mg IV.
Irregular:
Atrial Fibrillation with Aberrancy:
Rx options include: Cardizem, Beta Blockers
Atrial Fibrillation with Wolff Parkinson White (delta wave):
Avoid!!!: adenosine, verapamil, cardizem, and digoxin.
Give Amiodarone 150mg IV over 10 min
Toursades de Pointes:
Give magnesium 1 to 2g IV over 2 min
Wide Complex – Unstable
Ventricular Tachycardia (VT) – monomorphic:
If still partially conscious, sedate the patient.
Attempt to cardiovert: 1st attempt with 100j, 2nd attempt with 200j, 3rd attempt with 300j, then
following attempts with 360j
Ventricular Tachycardia (VT) – polymorphic:
Defibrilate the patient at 360j with a monophasic or 120-200j with a biphasic
Pulseless Ventricular Tachycardia / Ventricular Fibrillation (Refractory):
CABD, ABCD
Using defibrillator:
Verify presence of VF: Defibrillate the patient at 360j using monophasic or at the factory
recommended joules for a biphasic.
Drug treatment options:
Epinephrine 1mg IV every 3-5min.
Amiodarone 300mg IVP, repeated once in 3-5 min with following boluses at 150mg.
Magnesium Sulfate: give 1-2gm in 1-2 min
Treat the cause of the arrhythmia.
Bradycardia (Rate < 60)
Stable:
Monitor for changes in the hemodynamic status of the patient.
Unstable:
Give epinephrine 1mg IV every 3-5min until transcutaneous pacing can be initiated.
Initiate transcutaneous pacing until transvenous pacing can be initiated.
If TCP fails or intravenous pacing is delayed consider Epinephrine (2-10 mcg/min IV), Dopamine
(5-20 mcg/kg/min), or Isoproterenol (3-20 mcg/mim).
Treat causes (atropine 0.5-1mg IV may be used if vagal mechanism is suspected).
Asystole
CABD, ABCD
(if lead II is asystolic, confirm rhythm in leads avL and III.)
Drug therapy:
Give epinephrine 1mg IV every 3-5min.
Give atropine 1mg IV every 3-5 min, with a max dose of 3mg.
Pulseless Electrical Activity
CABD, ABCD
Drug Therapy:
Give epinephrine 1mg IV every 3-5min.
Give Atropine if bradycardic arrhythmia is present: 1mg IV every 3-5 min with a max of 3mg.
Treat the cause of the arrhythmia.
Acute Stroke
Initiated treatment within 10 min of arrival to the ER:
CABD, ABCD
Assess patient’s rhythm and treat with appropriate ACLS algorithm.
Attempt to eliminate other causes of symptoms (use patient history).
Obtain neurological assessment and tests by a specialist.
Initiated treatment within 25 min of arrival to the ER:
Establish if onset of symptoms has been less than 3 hours.
Continue neurological exams (non-Contrast CT scan), and monitor hemodynamics.
Determine if fibrinolytic therapy is appropriate.
Anda mungkin juga menyukai
- RBCH - PHT Aminophylline Loading Dose GuidelinesDokumen2 halamanRBCH - PHT Aminophylline Loading Dose GuidelinesAdrian PrasetioBelum ada peringkat
- 4 Weaning Ventilator-NIADokumen31 halaman4 Weaning Ventilator-NIAResyana Widyayani100% (1)
- DKA and HHS The Washington Manual of Critical CareDokumen6 halamanDKA and HHS The Washington Manual of Critical Careمحمد عقيلي100% (1)
- Intern Note 終極版Dokumen168 halamanIntern Note 終極版楊芷Belum ada peringkat
- PHC EmergencyDokumen42 halamanPHC Emergencyمحمداحمد محمدنور ابايزيدBelum ada peringkat
- Case Clerking (Senarai Ubatan)Dokumen3 halamanCase Clerking (Senarai Ubatan)FaRiduddinYaHya100% (1)
- Fluid Management in PediatricsDokumen3 halamanFluid Management in PediatricsZiyadBelum ada peringkat
- AtlsDokumen32 halamanAtlsMahesh RajwalBelum ada peringkat
- Anesthesiology Quick Reference (Adult) : Intubating MaintenanceDokumen2 halamanAnesthesiology Quick Reference (Adult) : Intubating Maintenanceanestesi unpadBelum ada peringkat
- Resuscitation MedicationDokumen1 halamanResuscitation MedicationDen SinyoBelum ada peringkat
- Paediatric Advanced Life Support: Resuscitation Council (UK)Dokumen12 halamanPaediatric Advanced Life Support: Resuscitation Council (UK)zacklim_2000100% (1)
- CVP Guided Deresuscitation in Managing Overload in Icu PDFDokumen57 halamanCVP Guided Deresuscitation in Managing Overload in Icu PDFJonathan Hamm100% (1)
- Anesthesia Drug DosageDokumen13 halamanAnesthesia Drug DosageLuqman HakimBelum ada peringkat
- Paediatric Emergency Drug DosesDokumen1 halamanPaediatric Emergency Drug DosesGloriaaaBelum ada peringkat
- DIC - IMELS (Compatibility Mode)Dokumen30 halamanDIC - IMELS (Compatibility Mode)Astri Arri FebriantiBelum ada peringkat
- Acute MedicineDokumen54 halamanAcute MedicineTipuBelum ada peringkat
- Paediatric Critical Care Infusions Intubation DrugsDokumen2 halamanPaediatric Critical Care Infusions Intubation DrugsА. Сосорбарам100% (1)
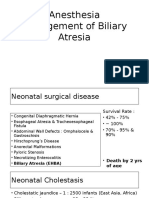
- 19 Anesthesia For Biliary AtresiaDokumen19 halaman19 Anesthesia For Biliary AtresiaDwiki Surya PrayogaBelum ada peringkat
- Yale IIP MICU120-160 2011Dokumen2 halamanYale IIP MICU120-160 2011afm26Belum ada peringkat
- Cakul - Emergency JantungDokumen8 halamanCakul - Emergency JantungRosalia Septaviana RisdiartaBelum ada peringkat
- Anaesthetic Drug Crib Sheet-8 PDFDokumen1 halamanAnaesthetic Drug Crib Sheet-8 PDFaasdf100% (1)
- Resuscitation Council Uk Anaphylaxis AlgorithmDokumen1 halamanResuscitation Council Uk Anaphylaxis Algorithmbrianed231100% (1)
- Mitral Stenosis Mitral RegurgitationDokumen66 halamanMitral Stenosis Mitral RegurgitationMarshellaTriPradilagaBelum ada peringkat
- Acls Study Guide 2016Dokumen2 halamanAcls Study Guide 2016Caridad RodasBelum ada peringkat
- IV Insulin Infusion Protocol TexasDokumen2 halamanIV Insulin Infusion Protocol TexasJohb CaballeroBelum ada peringkat
- Paediatric Anaesthesia GuideDokumen1 halamanPaediatric Anaesthesia GuideAndrewBeckBelum ada peringkat
- Management of Local Anaesthetic Toxicity Update 2009Dokumen6 halamanManagement of Local Anaesthetic Toxicity Update 2009leviosagalBelum ada peringkat
- Adarsh GlaucomaDokumen17 halamanAdarsh GlaucomaAdarshBijapurBelum ada peringkat
- 145 One Lung VentilationDokumen6 halaman145 One Lung VentilationEyad AbdeljawadBelum ada peringkat
- STEMI AnteroseptalDokumen14 halamanSTEMI AnteroseptalJalalludin AnBelum ada peringkat
- Pediatric Doses EdiDokumen3 halamanPediatric Doses EdiLubaid MoideenBelum ada peringkat
- Cme Acs 2. Stemi (Izzah)Dokumen36 halamanCme Acs 2. Stemi (Izzah)Hakimah K. SuhaimiBelum ada peringkat
- DIT High Yield Questions PDFDokumen13 halamanDIT High Yield Questions PDFjoshBelum ada peringkat
- Common DrugDokumen2 halamanCommon DrughengpanhatashiBelum ada peringkat
- Teknik Anestesi UmumDokumen128 halamanTeknik Anestesi UmumAkmalNourBelum ada peringkat
- Physiology CO Guyton ModelDokumen42 halamanPhysiology CO Guyton Modelcovid kojaBelum ada peringkat
- Episode 86 - HyperkalemiaDokumen7 halamanEpisode 86 - HyperkalemiaAlok yadav100% (1)
- Management of Severe Hypertension, Hypertension in Special ConditionDokumen43 halamanManagement of Severe Hypertension, Hypertension in Special Conditionabhandlung100% (3)
- General Rules For Units: Infusion Rate CalculationsDokumen3 halamanGeneral Rules For Units: Infusion Rate CalculationsVicky100% (2)
- Tehnik - Tehnik Analgesia Post OperasiDokumen32 halamanTehnik - Tehnik Analgesia Post OperasiGuntur Aryo PuntodewoBelum ada peringkat
- Anaesthetic Drug Crib Sheet-8Dokumen1 halamanAnaesthetic Drug Crib Sheet-8Tiarnán Byrne0% (2)
- Tesis Terapi Batuk DarahDokumen10 halamanTesis Terapi Batuk DarahAnonymous DxYXYkjTo5Belum ada peringkat
- Basic Concept On NeuroanesthesiaDokumen51 halamanBasic Concept On Neuroanesthesiabrojeem100% (1)
- k.41 ATRIAL FLUTTERDokumen8 halamank.41 ATRIAL FLUTTERjamaliganteng88Belum ada peringkat
- PERDICIDokumen31 halamanPERDICIDeya PrastikaBelum ada peringkat
- Surviving Sepsis Campaign Hour 1 BundleDokumen5 halamanSurviving Sepsis Campaign Hour 1 BundleNadine Noelle AgraviadorBelum ada peringkat
- Acute Myocardial Infarction by DR Gireesh Kumar K PDokumen18 halamanAcute Myocardial Infarction by DR Gireesh Kumar K PAETCM Emergency medicine50% (2)
- Case Presentation On Ischemic Stroke: G.Hari Prakash Pharm.D InternDokumen22 halamanCase Presentation On Ischemic Stroke: G.Hari Prakash Pharm.D InterngeethaBelum ada peringkat
- American Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityDokumen49 halamanAmerican Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityZulkarnainBustamamBelum ada peringkat
- BGA Acid Base Stepwise PradikDokumen43 halamanBGA Acid Base Stepwise PradikZulfadly NuralimBelum ada peringkat
- Algoritma BradycardiaDokumen1 halamanAlgoritma BradycardiaFiya SahrulBelum ada peringkat
- Permanent PacemakerDokumen23 halamanPermanent PacemakeradinsBelum ada peringkat
- Manual of Pediatric Emergency MedicineDokumen28 halamanManual of Pediatric Emergency MedicineRabi Dhakal100% (2)
- Snake Bite ToxiconDokumen14 halamanSnake Bite ToxiconAETCM Emergency medicine100% (1)
- Advanced Cardiac Life Support PDFDokumen9 halamanAdvanced Cardiac Life Support PDFYulias YoweiBelum ada peringkat
- Tatalaksana ArrthytmiaDokumen55 halamanTatalaksana ArrthytmiaJanstine FirstiandyBelum ada peringkat
- Acls Algorithms 2012Dokumen12 halamanAcls Algorithms 2012Prashanth KumarBelum ada peringkat
- ACLS Pocket GuideDokumen5 halamanACLS Pocket Guidedragnu100% (1)
- Acls Algorithms 2012Dokumen12 halamanAcls Algorithms 2012kivuBelum ada peringkat
- ACLS Algorithms Adult 2010 Revised May 31 2011Dokumen12 halamanACLS Algorithms Adult 2010 Revised May 31 2011arturschander3614Belum ada peringkat
- Gupta Et Al. - 2015 - Retinal Anatomy and PathologyDokumen12 halamanGupta Et Al. - 2015 - Retinal Anatomy and PathologyFelicia SutarliBelum ada peringkat
- Upper Gastrointestinal Tract Bleeding Management: Belgian Guidelines For Adults and ChildrenDokumen23 halamanUpper Gastrointestinal Tract Bleeding Management: Belgian Guidelines For Adults and ChildrenFelicia SutarliBelum ada peringkat
- Jia Et Al. - 2016 - Biomechanics of The Sclera and Effects On Intraocu PDFDokumen8 halamanJia Et Al. - 2016 - Biomechanics of The Sclera and Effects On Intraocu PDFFelicia SutarliBelum ada peringkat
- Early View: Trajectory and Mortality of Preserved Ratio Impaired Spirometry: The Rotterdam StudyDokumen39 halamanEarly View: Trajectory and Mortality of Preserved Ratio Impaired Spirometry: The Rotterdam StudyFelicia SutarliBelum ada peringkat
- Lopes2019 PDFDokumen41 halamanLopes2019 PDFFelicia SutarliBelum ada peringkat
- JOralResRev 2018 10 2 87 240919Dokumen7 halamanJOralResRev 2018 10 2 87 240919Felicia SutarliBelum ada peringkat
- Applsci 09 02842 PDFDokumen13 halamanApplsci 09 02842 PDFFelicia SutarliBelum ada peringkat
- Nasal Polyposis: An Overview of Differential Diagnosis and TreatmentDokumen12 halamanNasal Polyposis: An Overview of Differential Diagnosis and TreatmentFelicia SutarliBelum ada peringkat
- Zagor y 2015Dokumen6 halamanZagor y 2015Felicia SutarliBelum ada peringkat
- VAScoreConversionChart PDFDokumen1 halamanVAScoreConversionChart PDFFelicia SutarliBelum ada peringkat
- License AgreementDokumen3 halamanLicense AgreementFelicia SutarliBelum ada peringkat
- Primary Rhegmatogenous Retinal Detachment Surgery in Modern EraDokumen4 halamanPrimary Rhegmatogenous Retinal Detachment Surgery in Modern EraFelicia SutarliBelum ada peringkat
- Patogenesis Polip NasalDokumen30 halamanPatogenesis Polip NasalFelicia SutarliBelum ada peringkat
- Ukdi Preparation I:: Neurogenic Pain Syndromes Peripheral Nerve DisordersDokumen65 halamanUkdi Preparation I:: Neurogenic Pain Syndromes Peripheral Nerve DisordersFelicia SutarliBelum ada peringkat
- Vasco Reconversion ChartDokumen1 halamanVasco Reconversion ChartFelicia SutarliBelum ada peringkat
- Khusbu Keyal 2017 PDFDokumen10 halamanKhusbu Keyal 2017 PDFFelicia SutarliBelum ada peringkat
- 7 Contoh Analytical Exposition Pendek Bahasa InggrisDokumen6 halaman7 Contoh Analytical Exposition Pendek Bahasa InggrisDarsi YujiwatiBelum ada peringkat
- Human Factors and Safety Culture in Maritime Safety (Revised)Dokumen10 halamanHuman Factors and Safety Culture in Maritime Safety (Revised)Al-aayan D. IsmaelBelum ada peringkat
- Format OpnameDokumen21 halamanFormat OpnamerestutiyanaBelum ada peringkat
- CrimPro Cases People Vs LlantoDokumen7 halamanCrimPro Cases People Vs LlantoFatmah Azimah MapandiBelum ada peringkat
- Play Therapy FinalDokumen8 halamanPlay Therapy FinalChandru KowsalyaBelum ada peringkat
- Material Safety Data Sheet: Liquefied Petroleum GasDokumen1 halamanMaterial Safety Data Sheet: Liquefied Petroleum GasardhanhendroBelum ada peringkat
- PNF 8th EditionDokumen7 halamanPNF 8th EditionDanisaWajeBelum ada peringkat
- Risk Assessment Questions and Answers 1624351390Dokumen278 halamanRisk Assessment Questions and Answers 1624351390Firman Setiawan100% (1)
- Shivashaki Organic Menure and TransportDokumen3 halamanShivashaki Organic Menure and TransportShivashakthi MaheshBelum ada peringkat
- ID Virus Avian Influenza h5n1 Biologi Molek PDFDokumen13 halamanID Virus Avian Influenza h5n1 Biologi Molek PDFArsienda UlmafemaBelum ada peringkat
- Zollinger-Ellison Syndrome (Gastrinoma)Dokumen15 halamanZollinger-Ellison Syndrome (Gastrinoma)Huy QuangBelum ada peringkat
- Antitrombotik, PPT 7Dokumen66 halamanAntitrombotik, PPT 7Rizky Saraswati IndraputriBelum ada peringkat
- Eric Liou Contributions PDFDokumen8 halamanEric Liou Contributions PDFteju patneediBelum ada peringkat
- Transform at Home EbookDokumen302 halamanTransform at Home EbookLuckyBelum ada peringkat
- Matter For PGDIPC Course PromotionDokumen1 halamanMatter For PGDIPC Course PromotionAnkur VasudevaBelum ada peringkat
- Cleaning Reusable Medical DevicesDokumen12 halamanCleaning Reusable Medical DevicesDavid Olamendi ColinBelum ada peringkat
- 13fk10 Hav Igg-Igm (D) Ins (En) CeDokumen2 halaman13fk10 Hav Igg-Igm (D) Ins (En) CeCrcrjhjh RcrcjhjhBelum ada peringkat
- Electrical Safety in HealthcareDokumen2 halamanElectrical Safety in HealthcareNur Aqilah IsmailBelum ada peringkat
- Toolbox Talk 9: Critical Risks - ExcavationsDokumen2 halamanToolbox Talk 9: Critical Risks - ExcavationsPravin GowardunBelum ada peringkat
- Architecture For AutismDokumen16 halamanArchitecture For AutismSivaRamanBelum ada peringkat
- Risk Assessment - TemplateDokumen10 halamanRisk Assessment - TemplateJohn KalvinBelum ada peringkat
- Analytical Customer UpdationDokumen16 halamanAnalytical Customer UpdationSathish SmartBelum ada peringkat
- Analysis of Shift in Consumption of Carbonated Beverages To Healthy DrinksDokumen26 halamanAnalysis of Shift in Consumption of Carbonated Beverages To Healthy DrinksAntara JasrotiaBelum ada peringkat
- Revised Week 3Dokumen61 halamanRevised Week 3John Teo DalisaymoBelum ada peringkat
- Definition of Physical EducationDokumen7 halamanDefinition of Physical EducationRose Jane BangisBelum ada peringkat
- Pediatric Blood PressureDokumen28 halamanPediatric Blood PressureGenta Syaifrin Laudza0% (1)
- 16-Week Harvey Walden MarathonTraining PlanDokumen18 halaman16-Week Harvey Walden MarathonTraining PlanKaren MiranoBelum ada peringkat
- Group Activity 1 - BAFF MatrixDokumen1 halamanGroup Activity 1 - BAFF MatrixGreechiane LongoriaBelum ada peringkat
- Professional Teacher - Secondary (Social Studies) - 03-2024Dokumen45 halamanProfessional Teacher - Secondary (Social Studies) - 03-2024PRC BaguioBelum ada peringkat
- The Health Promotion Model (Nola J. Pender) : SupratmanDokumen11 halamanThe Health Promotion Model (Nola J. Pender) : SupratmanNugraha PratamaBelum ada peringkat