Perioperative Hypothermia in Pediatric Patients: Diagnosis, Prevention and Management
Diunggah oleh
yantiJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Perioperative Hypothermia in Pediatric Patients: Diagnosis, Prevention and Management
Diunggah oleh
yantiHak Cipta:
Format Tersedia
UP
DA P
TE AIN
S
Sp EDI ENS
IN & IN
ec AT IV
P T
ial RI E
Iss C A CA
ue NE RE
SPECIAL ARTICLE
ST
HE
SI
A,
Perioperative hypothermia in pediatric patients:
diagnosis, prevention and management
Sukhminder Jit Singh Bajwa, MD, MBA*, Swati MD**
*Associate Professor, Department of Anesthesiology and Intensive Care, Gian Sagar Medical College & Hospital, Ram Nagar, Banur, Punjab (India).
**Assistant Professor, Govt Medical College and Hospital, Sector-32, Chandigarh, India
Correspondence: Dr.Sukhminder Jit Singh Bajwa, House No-27-A, Ratan Nagar, Tripuri, Patiala, Punjab-147001 (India); Phone:
09915025828, +911752352182; E-mail: sukhminder_bajwa2001@yahoo.com
ABSTRACT
Hpothermia is the most common perioperative disturbance in pediatric patients. Pediatric patients are highly vulnerable
to hypothermia and its associated complications, e.g. respiratory embarrassment, metabolic acidosis, hypoglycemia,
hypoxemia, cardiac disturbances, coagulopathy, and a higher incidence of wound infection etc. This higher vulnerability
is mainly due to increased heat loss from larger head size, thin skin, lack of subcutaneous pad of fat and limited ability of
compensatory thermogenesis from brown fat. As such it is mandatory to design appropriate diagnostic, preventive and
therapeutic strategies which can effectively protect pediatric population from the potential catastrophic complications
associated with hypothermia during perioperative period. The current review aims to refresh the basic mechanism of
hypothermia and discussion of evidence based management strategies to minimize the incidence of hypothermia in
pediatric patients.
Key words: Perioperative, Hypothermia, Thermoregulation, Thermogenesis
Citation: Bajwa SJS and Swati. Peri-operative Hypothermia in pediatric patients: diagnosis, prevention and management.
Anaesth Pain & Intensive Care 2014;18(1):97-100
INTRODUCTION response is characterized by shunt vasoconstriction as an
initial response to cold exposure. The thermoregulatory
Inadvertent hypothermia, defined as a core temperature
threshold is decreased by general anesthetic agents. While
below 36˚C, is the most common form of perioperative
volatile anesthetics cause inhibition nonlinearly, higher
disturbance in pediatric population. The incidence of
concentrations being more effective; propofol and opioids
hypothermia can be up to 20% among patients undergoing
cause a linear inhibition.4-7
major surgical procedures. Perioperative hypothermia is
associated with several complications, which can adversely The most effective thermoregulatory response in infants
affect the patient outcome, especially in high risk patients.1 is nonshivering or brown fat thermogenesis. Brown fat is
A combination of proportionately higher heat loss, a located at nape of the neck, interscapular region, axillae,
diminished ability to produce endogenous heat and a and groin and around the kidneys and adrenals. Oxidation
diminished thermoregulatory response makes infants of triglycerides releases fatty acids to be consumed in
highly vulnerable to developing hypothermia.2 Although, generation of heat which is distributed through the blood
not as well described in literature as in adults, perioperative stream to various parts of the body. Clinically significant
hypothermia has been associated with a number of serious nonshivering thermogenesis is thought to be present
complications in infants.3 The current review aims to up to 2 years of age. It might, however, be inhibited by
discuss the importance of maintaining normothermia in anesthetics agents and this fact may play a critical role in
pediatric patients, predisposing risk factors for inadvertent development of intraoperative hypothermia.8-10
perioperative hypothermia and methods to detect and Minimal development of musculoskeletal mass makes
prevent perioperative hypothermia in children. shivering an insignificant mechanism of thermogenesis in
Thermoregulatory Mechanism during Anesthesia infants. The shivering response probably does not become
important until early childhood, although age dependence
Normal thermoregulation in infants in response to
has never been firmly established.11 Protective mechanisms
hypothermia is primarily augmented by vasoconstrictor
from hypothermia and shivering mechanism even in
response and nonshivering thermogenesis. Vasoconstrictor
ANAESTH, PAIN & INTENSIVE CARE; VOL 18(1) JAN-MAR 2014 97
Perioperative hypothermia in pediatric patients
the higher age group to some extent are influenced by group. Tander et al, evaluated the factors responsible
pharmacogenomics and pharmacogenetic factors.12 for predisposing to intraoperative hypothermia in sixty
neonates and infants.18 The study concluded that infants
Perioperative period is the time when child is exposed
had less decrease in temperature than neonates during
to a cold environment of operating room (OR) due to
both major and minor surgery and that the operating
administration of non-warmed intravenous fluids, and
room temperature below 23˚C could significantly interfere
potential evaporation from the operated areas. However,
with the maintenance of the neonate and infant’s core
these factors alone usually do not cause hypothermia as
temperature during anesthesia.18 A study in children
such. Caution has to be exercised even during the recovery
under 18 years of age by Pearce B et al, revealed that
phase and in postoperative wards which mandates the
hypothermia was significantly associated with preoperative
need for postoperative rounds by the anesthesiologists.13
lower baseline temperature and the type of surgery (major
Although thermoregulatory vasoconstrictive mechanism is
or minor).19
efficient in infants and children, they are functionally similar
to adults in being unable to increase the metabolic rate in
response to even mild hypothermia under anesthesia. In
CONSEQUENCES OF HYPOTHERMIA
fact, it is the failure of effective thermoregulatory defenses If the ongoing hypothermia is not taken care of, many
which induces hypothermia in a child. complications can occur in neonates, infants and children.
Respiratory embarrassment3 or apnea2 can be dangerous
Induction of general anesthesia results in a three-phase
complications. Both non-shivering and shivering
decrease in core temperature; core-to-peripheral heat
thermogenesis increase oxygen consumption leading
redistribution, linear core temperature decline, and core
to hypoxemia and carbon dioxide retention, metabolic
temperature plateau.14 Initially, vasodilatation caused by
acidosis, hypoglycemia and a shift of oxygen dissociation
anesthetic agents results in redistribution of heat from
curve to the left with resultant decreased oxygen delivery
the core to the periphery. Body heat content remains
to the tissues.20 Adult studies have shown that hypothermia
unchanged. Infants and children experience little heat
may cause cardiac problems, impaired platelet function
redistribution because of their small extremities with
and clotting factor enzyme function, thus increasing
respect to torso. As a result, redistribution may have a less
the requirement of allogenic blood transfusion. It also
contribution to intraoperative hypothermia.15
facilitates wound infections. Moreover, there can be altered
The initial phase of redistribution is followed by a stage metabolism of drugs,21 thermal discomfort,22 an impact on
of thermal imbalance in which there is net heat loss the patient outcome and resultant increased costs.23
to environment. The heat is lost mainly by radiation,
convection, conduction and evaporation. Radiation MONITORING OF TEMPERATURE
is responsible for maximum heat loss up to an extent
Continuous temperature monitoring in children receiving
of 40% and is proportional to environment / core
general anesthesia is recommended as per the guidelines
temperature difference. Convection is the other major
laid down by American Society of Anaesthesiologists
source of heat loss and denotes the loss of heat to air
(ASA). Any site which appropriately measures core body
molecules surrounding the body. Conductive heat loss
temperature can be chosen for such diagnostic intervention.
is due to difference in temperature between body and
The choice of method used to measure temperature
surfaces in contact. Evaporation refers to heat loss from
is based on the level of invasiveness and the degree of
skin, respiratory, bowel and wound surfaces. The pediatric
accuracy.24 There are a variety of sites, each with its specific
patients are vulnerable to intraoperative hypothermia
merits and demerits which can be summarized as Table 1.
because of increased heat loss due to their large surface
area to weight ratio, large head with thin scalp and skull,
thin skin which increases evaporative losses and lack of
PREVENTION
subcutaneous fat.16 Prevention is better than cure. This proverb has probably
not been more true in any other situation than in prevention
After three to four hours during intra-operative period,
of hypothermia in infants and children.
core temperature reaches a plateau reflecting a state in
1. Parents/caregivers education to keep the child
which heat loss is equal to heat production. Usually the
warm during preoperative hospital stay as well as
core temperature plateau occurs at a lower temperature,17
during the transfer to the operating room so as to
although the core temperature is maintained during this
avoid the risk of hypothermia and its complications.
phase. This may mask a continuing decrease in body heat
The biopsychosocial perspectives related to various
content as the loss from extremities continues unabated.
anesthetic techniques and drugs have to be explained to
There have been few studies identifying specific risk the parents for their complete.26
factors for intraoperative hypothermia in pediatric age 2. Preoperative assessment should be thorough and
98 ANAESTH, PAIN & INTENSIVE CARE; VOL 18(1) JAN-MAR 2014
special article
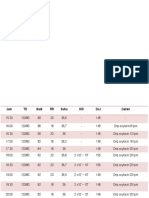
Table 1: Probable sites for temperature monitoring - Active skin warming vs. passive protection.
(i) Forced-Air Warming Devices- are the most
Site/Methodology Clinical Significance
commonly used and efficient active warming
Pulmonary Artery Catheter measures core temperature most accurately systems.31 These consist of an electrically
However it is reserved for patients requiring powered heater blower unit and blanket made
intensive hemodynamic monitoring due to its of paper to cover the patient. It provides
invasiveness and cost of the catheters convective heating to keep body warm.
Distal Esophageal Measures accurately core temperature but To increase the efficiency, prewarming the
may be affected by humidified gases and in
child is desirable and the largest size of the
surgeries where chest cavity is opened like
during open heart or lung surgery blanket that covers maximum body surface
Nasopharyngeal May be affected by inspired gases
is preferred.32 These can increase the core
temperature by almost 0.75°C/hour.
Bladder Efficiency may be affected with low urine
output, lower abdomen procedures
(ii) Resistive heating (electric blankets) are cheaper and
equally efficient as forced-air system.34
Tympanic Non invasive measure of core temperature
(iii) Energy Pads use circulating heated water that
Patency of external auditory meatus is a comes in contact with patient’s skin.
must
(iv) Circulating water mattresses are placed over the
Rectal Accurately reflects the core temperature operating table under the pediatric. This
but results might be effected by stools and
bacteria that generate heat
system maintains an acceptable efficiency in
pediatric patients as it involves warming the
Axillary For accurate measurement probe should be
positioned over the axillary artery and the arm back skin surface which provides larger surface
to be kept at the patient’s side area in children as compared to adults.
Using a simple correction factor of (v) Radiant warmers/ overhead heating units generate
Skin temperature +0.52°C,this is an accurate noninvasive infrared radiation. The effectiveness depends
measured over the carotid measure of nasopharyngeal temperature on the distance between the device and the
artery
Avoid risk of nose bleeding ,infection [25] skin of the patient and its direction. They can
be used during induction of anesthesia until
should specifically aim at: the child is covered with surgical drapes.
- preoperative checking of the temperature Disadvantages of warming devices include
- preoperative warming by covering the child in the risk of burns seen when used incorrectly.35
a cotton blanket or using forced air warming A combination of them increases treatment
system.27,28 Moreover, the preventive measures have costs too.
to be devised on the basis of available resources
Internal Warming Systems
especially in developing nations by innovations and
improvisations.29 Fluid warmers should be used for major surgeries with
3. Maintaining normothermia in intraoperative phase considerable blood loss and massive fluid shifts. Active
by: and passive inspired gas humidification slightly contributes
- maintaining ambient OR temperature ˃23 ̊ C so in maintaining core temperature in anesthetized pediatric
as to reduce radiation and convection losses but it patients. Active airway heating and humidification uses
may be associated with discomfort to OR team. electric humidifiers and passive humidification involves
- induction of anesthesia should not begin unless using heat and moisture exchanger. These preserve cilial
and until the patient’s temperature is 36.0°C or function and prevent bronchospasm. But recent SCIP24 do
above. not recommend their use.
- use of warmed intravenous fluids30 alone may not
prove to be effective. CONCLUSION
- Passive insulation i.e. minimizing heat loss by In conclusion, during pediatric anesthesia infants and
insulating the child from the environment by using small children are prone to perioperative hypothermia
surgical drapes, cotton blankets and metalized due to many inherent factors. This makes it mandatory
plastic covers. The trapped air between the covers to monitor their core temperature. Management should
and child̓̓́ s surface provides the insulation. involve prevention and/or decreasing the risk by use of a
Increasing the number of layers does not provide multimodal approach. This includes preoperatively keeping
further protection .Reduction in heat loss is by the child warm, increasing ambient OR temperature to
approximately 30% and is directly proportional to 23 ̊-25 ̊ C, use of warm intravenous fluids, passive
the covered surface area.30 insulation and use of forced air warming devices.
ANAESTH, PAIN & INTENSIVE CARE; VOL 18(1) JAN-MAR 2014 99
Perioperative hypothermia in pediatric patients
REFERENCES
1. Leslie K, Sessler DI. Perioperative hypothermia and facts. Indian J Anaesth 2013;57:336-7 carotid artery provides an accurate noninvasive
in the highrisk surgical patient. Best Practice & [PubMed] [Free Full Text] doi: 10.4103/0019- estimation of core temperature in infants and
Research Clin Anaesth 2003; 17,4: 485-98. 5049.118517. young children during general anesthesia.
2. Witt L, Dennhardt N, Eich Cet al. Prevention 13. Bajwa SS, Takrouri MM. Post-operative Pediatric Anesthesia 23 (2013) 1109–1116
of intraoperative hypothermia in neonates and anesthesia rounds: Need of the hour. Anesth 26. Bajwa SS, Kalra SA. deeper understanding of
infants: results of a prospective multicentre Essays Res 2013;7:291-3 anesthesiology practice: the biopsychosocial
observational study with a new forced-air 14. Daniel Sessler Perioperative Heat Balance. perspective. Saudi J Anaesth 2014;8:4-
warming system with increased warm air flow. Anesthesiology2000, 92:578 -96 5[PubMed]
Pediatr Anesth 2013; 23: 469–474. 15. Young VL, Watson ME. Prevention of 27. Horn E P, Bein B, Bohm R, Steinfath M, Sahili
3. Sessler DI. Forced-air warming in infants and perioperative hypothermia in plastic N and Hocker J: The effect of short time periods
children. Pediatr Anesth 2013;23:467–468 surgery Aesthet Surg J. 2006 Sep-Oct; of pre-operative warming in the prevention
4. Ozaki M,Sessler DI,Suzuki H, Ozaki K, Tsunoda 26(5):551-71. of peri-operative hypothermia. Anaesthesia
C, Atarashi K. Nitrous oxide decreases the 16. Galante D. Intraoperative hypothermia. Relation 2012;67:612-7 [PubMed] doi: 10.1111/j.1365-
threshold for vasoconstriction less than between general and regional anesthesia, 2044.2012.07073.x. Epub 2012 Feb 29.
sevoflurane or isoflurane. Anesth Analg 1995; upper- and lower-body warming: what strategies 28. Andrzejowski J, Hoyle J, Eapen G, Turnbull D:
80:1212 [PubMed] in pediatric anesthesia? Pediatr Anesth 2007; Effect of prewarming on post-induction core
5. Matsukawa T, Kurz A, Sessler DI, Bjorksten 17: 821–823. temperature and the incidence of inadvertent
AR, Merrifield B, Cheng C. Propofol linearly 17. Kurz A,Sessler DI,Christensen R,Dechert perioperative hypothermia in patients
reduces the vasoconstriction and shivering M:Heat balance and distribution during the core undergoing general anaesthesia. Br J Anaesth
thresholds. Anesthesiology 1995;82:1169 –temperature plateau in anesthetized humans. 2008;101:627-31 [PubMed] doi: 10.1093/bja/
[PubMed] Aneethesiology 83:491,1995 aen272. Epub 2008 Sep 26.
6. Hynson JM, Sessler DI, Belani K, 18. Tander B, Baris S, Karakaya D, Ariturk E, 29. Bajwa SS, Takrouri MM. Innovations,
Washington D, McGuire J, Merrifield B, et Rizalar R, et al. (2005) Risk factors influencing improvisations, challenges and constraints:
al:Thermoregulatory vasoconstriction during inadvertent hypothermia in infants and neonates The untold story of anesthesia in developing
propofol/nitrous oxide anesthesia in humans: during anesthesia. Paediatr Anaesth 15: 574- nations. Anesth Essays Res 2014;8:1-2
threshold and Spo2. Anesth Analg 1992;75:947 579. [PubMed] 30. Sessler DI. Complications and treatment
[PubMed] 19. Pearce B, Christensen R, Voepel-Lewis T of mild hypothermia. Anesthesiology 2001
7. Bissonnette B, Sessler DI. Thermoregulatory (2010) Perioperative Hypothermia in the Aug;95(2):531-43 [Free Full Text]
thresholds for vasoconstriction in pediatric Pediatric Population: Prevalence, Risk Factors 31. Brauer A, English MJ, Steinmetz N, Lorenz
patients anesthetized with halothane and Outcomes. J Anesthe Clinic Res 1:102 N, Perl T, Weyland W, Quintel M. Efficacy
or halothane and caudal bupivacaine. 20. Wetzel RC. Evaluation of children. In: of forced-air warming systems with full body
Anesthesiology 1992;76:387 [PubMed] Longnecker DE, Tinker JH, Morgan Jr GE, eds. blankets. Can J Anaesth 2007;54:34–41
8. Dicker A, Ohlson K, Johnson L, Cannon Principles and Practice of Anesthesiology, 2nd [PubMed]
B, Lindahl SG, Nedergaard J. Halothane edn. Philadelphia: Mosby Publishers, 1999: 32. Bra¨uer A, Quintel M. Forced-air warming:
selectively inhibits nonshivering thermogenesis: 445±447 technology, physical background
possible implications for thermoregulation 21. Blum R, Cote C. Pediatric equipment. In: Blum and practical aspects. Curr Opin
during anesthesia of infants. Anesthesiology R, Cote C, eds. A Practice of Anaesthesia Anaesthesiol. 2009 Dec;22(6):769-74. [PubMed]
1995;82:491–501. [PubMed] for Infants and Children. Philadelphia, PA: doi: 10.1097/ACO.0b013e328331d134.
9. Ohlson KBE, Mohel N, Cannon B, Lindahl Saunders Elsevier, 2009:1099–1101 33. Marta Putzu, Andrea Casati†, Marco
SG, Nedergaard J. Thermogenesis in brown 22. Doufas AG. Consequences of inadvertent Berti, Giovanni Pagliarini, Guido Fanelli
adipocytes is inhibited by volatile anesthetic perioperative hypothermia. Best Pract Res Clin Clinical complications, monitoring and
agents: a factor contributing to hypothermia Anaesthesiol 2003; 17: 535–549 management of perioperative mild
in infants? Anesthesiology 1994;81:176–183. 23. Mahoney CB, Odom J. Maintaining hypothermia: anesthesiological features. Acta
[PubMed] intraoperative normothermia: a meta-analysis Biomed.2007;78:163-169 [PubMed]
10. Plattner O, Semsroth M, Sessler DI et al. of outcomes with costs. AANA J 1999; 67: 34. Negishi C, Hasegawa K, Mukai S, Nakagawa
Lack of nonshivering thermogenesis in infants 155–163 [PubMed] F, Ozaki M, Sessler DI. Resistive heating and
anesthetized with fentanyl and propofol. 24. Joshua W. Sappenfield, Caron M. Hong and forced-air warming are comparably effective.
Anesthesiology 1997; 86: 772–777. Samuel M. Galvagno. Perioperative temperature Anesth Analg 2003;96(6):1683-7. [PubMed]
11. Sessler D. Temperature disturbances. In: Sessler measurement and management:moving beyond 35. D. J. Dewar1, J. F. Fraser, K. L. Choo and R.
D, ed. Pediatric Anesthesia. Philadelphia, PA: the Surgical Care Improvement Project .Journal M. Kimble. Thermal injuries in three children
Churchill Livingstone,2002:53–84. of Anesthesiology and Clinical Science 2013 caused by an electrical warming mattress. Br J
12. Bhaskar S B, Bajwa SS. Pharmacogenomics 25. Ollie Jay, Yannick Molgat-Seon, Shirley Chou Anaesth 2004;93(4):586–9 [PubMed]
and anaesthesia: Mysteries, correlations and Kimmo Murto. Skin temperature over the
100 ANAESTH, PAIN & INTENSIVE CARE; VOL 18(1) JAN-MAR 2014
Anda mungkin juga menyukai
- 6 Steps To Effective Safety Coaching - Ebook MSC 4.0Dokumen24 halaman6 Steps To Effective Safety Coaching - Ebook MSC 4.0walidBelum ada peringkat
- 6 Steps To Effective Safety Coaching V2 PDFDokumen24 halaman6 Steps To Effective Safety Coaching V2 PDFMuneer Alwatani100% (1)
- Clinical Impressions Volume12no2Dokumen33 halamanClinical Impressions Volume12no2audrey100% (1)
- Clinical Audit On Abdominal Pain Triage in EmergencyDokumen23 halamanClinical Audit On Abdominal Pain Triage in EmergencyPrassaad ArujunanBelum ada peringkat
- Review in Clinical MicrosDokumen103 halamanReview in Clinical MicrosSyvelmarie Tinte100% (1)
- Subclinical Atrial FibrilationDokumen23 halamanSubclinical Atrial Fibrilationshahane musayelyanBelum ada peringkat
- Rig SafetyDokumen1 halamanRig Safetymuhammad aldo assaqqafBelum ada peringkat
- FMGE Old QuestionsDokumen156 halamanFMGE Old QuestionsAnonymous S0H8cqgnfi100% (11)
- PERKENI (2021) - Konsensus DM Tipe 2Dokumen119 halamanPERKENI (2021) - Konsensus DM Tipe 2Ammalia RachmiBelum ada peringkat
- Stainless Steel CrownDokumen63 halamanStainless Steel CrownKaran Arora100% (1)
- Guidelines: Sustainability Assessment of Food and Agriculture SystemsDokumen268 halamanGuidelines: Sustainability Assessment of Food and Agriculture SystemspetronilaBelum ada peringkat
- High Alert MedicationsDokumen1 halamanHigh Alert MedicationspucukjayaBelum ada peringkat
- 10 Penyakit Terbanyak Di Upt. Puskesmas BandarDokumen2 halaman10 Penyakit Terbanyak Di Upt. Puskesmas BandarRahayu BudiBelum ada peringkat
- Postpartum Depression Beyond The Baby Blues .7 PDFDokumen8 halamanPostpartum Depression Beyond The Baby Blues .7 PDFAnonymous 8um6M5uBelum ada peringkat
- Scientific American - World View 2016 (Gnv64)Dokumen88 halamanScientific American - World View 2016 (Gnv64)Musa Rahim KhanBelum ada peringkat
- 1115 N. HermitageDokumen24 halaman1115 N. HermitageHannah AlaniBelum ada peringkat
- CL Msexcel Otic AltheaDokumen2 halamanCL Msexcel Otic AltheaLeanTamsiBelum ada peringkat
- Anesthesia UpdateDokumen1 halamanAnesthesia UpdatevkBelum ada peringkat
- Banner 2023Dokumen1 halamanBanner 2023ackonboham2Belum ada peringkat
- 10 Besar DX Penyakit Rawat Inap Bulan Januari 2019Dokumen3 halaman10 Besar DX Penyakit Rawat Inap Bulan Januari 2019Nasta'in AhmadBelum ada peringkat
- 2019-Epilepsy EmergenciesDokumen23 halaman2019-Epilepsy EmergenciesBryanBelum ada peringkat
- PDF - 4311 FibromyalgiaDokumen7 halamanPDF - 4311 Fibromyalgiahekate.yantraBelum ada peringkat
- CCC-1628 DrillingBro A4Dokumen12 halamanCCC-1628 DrillingBro A4Joao AraujoBelum ada peringkat
- SAFASmallApp - Manual-FinalDokumen70 halamanSAFASmallApp - Manual-FinalMauricio Javier Gaitán FuentesBelum ada peringkat
- GRADE 6-HYACINTH 2021-2022 Mapeh: Quarter 1Dokumen1 halamanGRADE 6-HYACINTH 2021-2022 Mapeh: Quarter 1ELEANOR MENDOZABelum ada peringkat
- UNHQ NY Emergency Preparedness Guide-2014Dokumen27 halamanUNHQ NY Emergency Preparedness Guide-2014Mohammed FattoumBelum ada peringkat
- Ict-12 Villafranca: Ea RCH 2 CH PR OJ EC T TO PH ILO SO PY IO N W OR KI M M ER SIO NDokumen1 halamanIct-12 Villafranca: Ea RCH 2 CH PR OJ EC T TO PH ILO SO PY IO N W OR KI M M ER SIO NAngelo VillafrancaBelum ada peringkat
- The Examiner. Vol-66. No-34. 20 - 26 Aug 22Dokumen36 halamanThe Examiner. Vol-66. No-34. 20 - 26 Aug 22swell2Belum ada peringkat
- Bicol Regional Training and Teaching Hospital Hospital Training Office Rizal ST., Legazpi CityDokumen1 halamanBicol Regional Training and Teaching Hospital Hospital Training Office Rizal ST., Legazpi CityAlyssaMarieSyBelum ada peringkat
- CV - Amarjeet ChitkaraDokumen1 halamanCV - Amarjeet ChitkaraMuthu KumarBelum ada peringkat
- Catalogo Welch AllynDokumen40 halamanCatalogo Welch AllynBiomédico CFIMBelum ada peringkat
- Formula 1 Strategic Plan011320Dokumen18 halamanFormula 1 Strategic Plan011320PanBelum ada peringkat
- ColoringDokumen41 halamanColoringJoshua CooperBelum ada peringkat
- Engr. M.Elalfi Eastern Province Area CoordinatorDokumen3 halamanEngr. M.Elalfi Eastern Province Area CoordinatorShahid BhattiBelum ada peringkat
- NETWorks Summer 2009Dokumen40 halamanNETWorks Summer 2009NETParkNetBelum ada peringkat
- Elderly HypertensionDokumen1 halamanElderly HypertensionArista Prima NBelum ada peringkat
- Efecto de Salud Fisica y Mental Del Covid en FMDokumen11 halamanEfecto de Salud Fisica y Mental Del Covid en FMtavo570Belum ada peringkat
- TIGTA Fraud - Poster.SamplesDokumen1 halamanTIGTA Fraud - Poster.SamplesBILLYBelum ada peringkat
- Digital Booklet - Trespassing ADAM LAMBERTDokumen6 halamanDigital Booklet - Trespassing ADAM LAMBERTНики ДимитровBelum ada peringkat
- Abstractbook 14th INTEREST 2020Dokumen523 halamanAbstractbook 14th INTEREST 2020Pelumi AshamuBelum ada peringkat
- Las Piñas Datrc SDP ModelDokumen1 halamanLas Piñas Datrc SDP Modelowen nicerioBelum ada peringkat
- Summary of Quarterly Grades (First Quarter)Dokumen13 halamanSummary of Quarterly Grades (First Quarter)Rudny LabutapBelum ada peringkat
- MBA 530 GROW ModelDokumen5 halamanMBA 530 GROW ModelSchool Purposes OnlyBelum ada peringkat
- Adult Sepsis Pathway Sept 2016 With Watermark PDFDokumen2 halamanAdult Sepsis Pathway Sept 2016 With Watermark PDFAbdul raufBelum ada peringkat
- TSC: Curriculum Design FrameworkDokumen3 halamanTSC: Curriculum Design FrameworkJorielyn ApostolBelum ada peringkat
- 18 - 06 - Poultry SpecialDokumen24 halaman18 - 06 - Poultry SpecialAndreiaAraujoBelum ada peringkat
- Weld Inspection Report: CC Ep T R Ej Ec TDokumen2 halamanWeld Inspection Report: CC Ep T R Ej Ec TSanofar ShamsudeenBelum ada peringkat
- Head Over Meals: IndiaDokumen21 halamanHead Over Meals: IndiaAndrea Rodríguez PabónBelum ada peringkat
- 11-HUMSS: SUMMARY OF GRADES (1st Quarter, 1st Semester 2020-2021)Dokumen11 halaman11-HUMSS: SUMMARY OF GRADES (1st Quarter, 1st Semester 2020-2021)Giancarla Maria Lorenzo DingleBelum ada peringkat
- Synthesis Report of The Nigeria Zero Hunger Strategic Review PDFDokumen66 halamanSynthesis Report of The Nigeria Zero Hunger Strategic Review PDFWirantiBelum ada peringkat
- Va Lue /tim Es Eq Ue Nce Dim en Sio NC Ou NT Im Po Rta Nce Es Tim AteDokumen2 halamanVa Lue /tim Es Eq Ue Nce Dim en Sio NC Ou NT Im Po Rta Nce Es Tim AteoperatedboyBelum ada peringkat
- Region Division School Name: III Pampanga Justino Sevilla High SchoolDokumen4 halamanRegion Division School Name: III Pampanga Justino Sevilla High SchoolArlen GonzalesBelum ada peringkat
- SDR hpch1 PDFDokumen20 halamanSDR hpch1 PDFSunny Music ProductionsBelum ada peringkat
- UVAS Prospectus PDFDokumen48 halamanUVAS Prospectus PDFkashan safdarBelum ada peringkat
- Alobar Holoprosencephaly in One of Twin Neonates NNigerJClinRDokumen4 halamanAlobar Holoprosencephaly in One of Twin Neonates NNigerJClinRAnonymous 9QxPDpBelum ada peringkat
- Homecomingconcert PUB 749 F19Dokumen1 halamanHomecomingconcert PUB 749 F19dmcummingBelum ada peringkat
- Treating Obstructive Sleep Apnea and Snoring: Assessment of An Anterior Mandibular Positioning DeviceDokumen7 halamanTreating Obstructive Sleep Apnea and Snoring: Assessment of An Anterior Mandibular Positioning Device陈延珑Belum ada peringkat
- Summary of GradesDokumen8 halamanSummary of GradesNIKKO NAVAREZBelum ada peringkat
- Deepti Mam IntegreatedDokumen123 halamanDeepti Mam IntegreatedTarannum JindalBelum ada peringkat
- Patel Darshankumar Prabhudas: This Certificate Is Proudly Presented ToDokumen1 halamanPatel Darshankumar Prabhudas: This Certificate Is Proudly Presented Topateldarshan pBelum ada peringkat
- Republic of The Philippines Social Security System - MemberDokumen1 halamanRepublic of The Philippines Social Security System - MemberJhames LenovoūBelum ada peringkat
- SM3053 en EU EU Product CatalogDokumen44 halamanSM3053 en EU EU Product CatalogElectromedycal EQUIPO MEDICOBelum ada peringkat
- Beninca Worldwide CatDokumen125 halamanBeninca Worldwide CatooasysBelum ada peringkat
- 11-HUMSS: Top Performing StudentsDokumen8 halaman11-HUMSS: Top Performing StudentsGiancarla Maria Lorenzo DingleBelum ada peringkat
- TeksDokumen1 halamanTeksyantiBelum ada peringkat
- MR 23 Oktober 2019Dokumen17 halamanMR 23 Oktober 2019yantiBelum ada peringkat
- 17 06 2020 16.55.43Dokumen1 halaman17 06 2020 16.55.43yantiBelum ada peringkat
- MR 21 NovDokumen9 halamanMR 21 NovyantiBelum ada peringkat
- Observasi Pasien 24-11-2019Dokumen2 halamanObservasi Pasien 24-11-2019yantiBelum ada peringkat
- Morning Report: 27 OCTOBER, 2019Dokumen11 halamanMorning Report: 27 OCTOBER, 2019yantiBelum ada peringkat
- BMJ I1753 FullDokumen10 halamanBMJ I1753 Fullrachel0301Belum ada peringkat
- Urits2019 Article AComprehensiveUpdateOfCurrentADokumen10 halamanUrits2019 Article AComprehensiveUpdateOfCurrentAyantiBelum ada peringkat
- Rectovaginal Fistula: What Is The Optimal Strategy?: P 22 A Esa MDokumen7 halamanRectovaginal Fistula: What Is The Optimal Strategy?: P 22 A Esa MyantiBelum ada peringkat
- Screening and Prevention of Preeclampsia: Liona C. Poon, Daljit SahotaDokumen6 halamanScreening and Prevention of Preeclampsia: Liona C. Poon, Daljit SahotayantiBelum ada peringkat
- Thermal Care PaperDokumen11 halamanThermal Care PaperyantiBelum ada peringkat
- Surgical Treatment of Rectovaginal Fistula in Crohn's Disease: A Tertiary Center ExperienceDokumen4 halamanSurgical Treatment of Rectovaginal Fistula in Crohn's Disease: A Tertiary Center ExperienceyantiBelum ada peringkat
- Diving Medicine in Clinical Practice: Lars Eichhorn, Dieter LeykDokumen14 halamanDiving Medicine in Clinical Practice: Lars Eichhorn, Dieter LeykyantiBelum ada peringkat
- DysmorphologyDokumen16 halamanDysmorphologycoassukoyBelum ada peringkat
- Asthma in Pregnancy: Dr. Agus Rusdhy Hariawan Hamid, Spog SMF Obgin Rsup NTBDokumen10 halamanAsthma in Pregnancy: Dr. Agus Rusdhy Hariawan Hamid, Spog SMF Obgin Rsup NTBMartina RizkiBelum ada peringkat
- PDFDokumen55 halamanPDFYahya KhanBelum ada peringkat
- Palatoplasty: Evolution and Controversies: Aik-Ming Leow, MD Lun-Jou Lo, MDDokumen11 halamanPalatoplasty: Evolution and Controversies: Aik-Ming Leow, MD Lun-Jou Lo, MDNavatha MorthaBelum ada peringkat
- Nursing in The Philippines Has A Deep and Enigmatic HistoryDokumen21 halamanNursing in The Philippines Has A Deep and Enigmatic HistoryAnonymous 75TDy2yBelum ada peringkat
- AmSurgCorporation 10K 20110225Dokumen79 halamanAmSurgCorporation 10K 20110225alamnjBelum ada peringkat
- Influence of Posture On Swallowing: A. Lumbau, L. Schinocca, G. ChessaDokumen4 halamanInfluence of Posture On Swallowing: A. Lumbau, L. Schinocca, G. ChessaNini MejíaBelum ada peringkat
- Applying Sullivan's Theory of Anxiety Versus FearDokumen4 halamanApplying Sullivan's Theory of Anxiety Versus Fearkarin24Belum ada peringkat
- ISO Care Unlimited Student Insurance 2019Dokumen14 halamanISO Care Unlimited Student Insurance 2019Ivory PlatypusBelum ada peringkat
- UCSF Self StudyDokumen67 halamanUCSF Self StudyucsfmededBelum ada peringkat
- Drug and Cosmetic ActDokumen15 halamanDrug and Cosmetic ActGorav BhallaBelum ada peringkat
- 2021 - Chronic Isolated Radial Head DislocationDokumen9 halaman2021 - Chronic Isolated Radial Head Dislocationjuan pablo aguirreBelum ada peringkat
- Doctors ListDokumen16 halamanDoctors ListUsman DastgirBelum ada peringkat
- 01-Sdh DH Iphs Guidelines-2022Dokumen244 halaman01-Sdh DH Iphs Guidelines-2022பிரேம் குமார் ராஜாமணிBelum ada peringkat
- EHAQ 4th Cycle Audit Tool Final Feb.10-2022Dokumen51 halamanEHAQ 4th Cycle Audit Tool Final Feb.10-2022Michael Gebreamlak100% (1)
- Circumsision & NursingDokumen2 halamanCircumsision & NursingAhmetBelum ada peringkat
- Anatomy of OesophagusDokumen24 halamanAnatomy of OesophagusLia Restimulia DelfitriBelum ada peringkat
- Ophthalmia NeonatorumDokumen19 halamanOphthalmia NeonatorumSanthu Tvm100% (1)
- Out Patient DepartmentDokumen9 halamanOut Patient DepartmentBiway RegalaBelum ada peringkat
- Long Case OSMFDokumen17 halamanLong Case OSMFVidhi ParekhBelum ada peringkat
- NIH Public Access: Author ManuscriptDokumen24 halamanNIH Public Access: Author ManuscriptireneaureliaBelum ada peringkat
- Case Report A 30 Years Old Man With Ankylosing Spondilitis: Dyah Gita Rambu KareriDokumen24 halamanCase Report A 30 Years Old Man With Ankylosing Spondilitis: Dyah Gita Rambu KareriDhieto Basuki PutraBelum ada peringkat
- 2012 09 Pediatric Report Annex1 2 enDokumen187 halaman2012 09 Pediatric Report Annex1 2 enchancechancechanceBelum ada peringkat
- Narayana Health - Consumer QuestionnaireDokumen3 halamanNarayana Health - Consumer QuestionnairedivijnathBelum ada peringkat