Bipolar Diathermy A Step Ahead of Conventional Monopolar TURP
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Bipolar Diathermy A Step Ahead of Conventional Monopolar TURP
Hak Cipta:
Format Tersedia
Volume 4, Issue 8, August – 2019 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Bipolar Diathermy; A Step Ahead of
Conventional Monopolar TURP
Dr. Muhammad Haroon Ghous Dr. Ali Hassan Dr. Sikander Afzal
Chair; Division of Urology, UCM Senior Registrar, UCM Associate Dean, Admin; UCM
University of Lahore University of Lahore University of Lahore
Abstract I. INTRODUCTION
Objective: BPH (benign prostatic hyperplasia) is an illness of old
To compare the mean perioperative blood loss in age men1. It is categorized by epithelial cells and smooth
monopolar versus bipolar transurethral resection muscle proliferation in prostate gland zone which causes
prostate in patients with benign prostatic hyperplasia symptoms of lower urinary tract2. Prevalence of BPH is
(BPH). 20% in men with age 40-50 and 50% in age 50-60 and it
increases about 90% in men older than 80 years of age. 3
Methodology: Aim of treatment revolves around three aspects to eliminate
This Randomized Controlled Trial was conducted the symptoms of lower urinary tract (LUTS), hamper
at Urology Department, Galway University Hospital, disease progression, and to reduce complications. There are
Galway, Republic of Ireland from 1st January 2018 to many treatment modalities for BPH comprising
31st December 2018. Total 100 patients with benign surveillance, medical therapy and surgical management. 4
prostatic hyperplasia (BPH) were included. The patients First line treatment is medical therapy but surgical
were divided into two groups. Group-A (Monopolar treatment is considered when medical therapy fails or
TURP), while Group-B (Bipolar TURP). Pre-operative patients develop complications due to BPH.5
hematocrit of each study patient was recorded. Patient
were followed up after 24 hours of surgery in which Transurethral monopolar resection is considered to be
hematocrit level was estimated. Blood loss was the Gold standard operation for the surgical management of
calculated by recording pre-operative and post- BPH in light of long term results shown in randomized
operative (after 24 hours) hematocrit level. controlled trials. It involves endoscopic removal, by use of
Perioperative blood loss in both groups was compared diathermy, of inner prostate gland.6 This technique has
through independent t-test. Data were stratified for age, great significance in improving urine flow rate, symptoms
duration of BPH and size of prostate. A p-value <0.05 score and other parameters but it is also linked with
was considered significant. morbidities e.g. TUR syndrome, urinary incontinence,
erectile dysfunction, retrograde ejaculation and peri- and
Results: post-operative bleeding.7 To minimize these TURP linked
One hundred patients fulfilling the inclusion complications many minimal invasive techniques
criteria were included in this study. Patients were introduced e.g. plasma kinetic bipolar loop resection,
divided in two groups i.e. Group-A (Monopolar TURP) Holmium Laser Enucleation of the prostate (HoLEP),
and Group-B (Bipolar TURP). The mean age of patients Photosensitive vaporization etc, which are similar to
in group-A was 65.4±17.4 years and in group-B was monopolar but different in rate of complications. 8
63.6±14.9 years. In group-A, mean peri-operative blood
loss was 351.3±14.84 ml and 299.4±13.01 ml in group-B In bipolar resection of Prostate, a special resectoscope
with a p-value of 0.000001, which is statistically loop used that joins both return and active electrodes, this
significant. method of flow of current minimize the risk of current flow
stay.9 In bipolar we use normal saline as an irrigation fluid
Conclusion: that has theoretical advantage of preventing TUR syndrome
There is a difference of mean perioperative blood and minimizing blood loss. Bleeding has always been a
loss in monopolar versus bipolar transurethral resection significant problem in monopolar TURP and often requires
prostate in patients with benign prostatic hyperplasia blood transfusion.10 Reduced loss of blood in bipolar than
(BPH). monopolar has been focused in many studies.11 In one
study, results demonstrated that in bipolar TURP there is
Keywords:- Monopolar, Bipolar Transurethral Resection less intra-operative blood loss than monopolar TURP
Prostate, Benign Prostatic Hyperplasia (BPH). (238.5±69.43ml vs. 289.6±89.47ml).11 In another study,
Bipolar TURP associated with significantly less blood loss
than monopolar TURP (300.0±2.47ml vs. 349.0±3.5ml).12
Since its introduction, Bipolar TURP has extended
popularity and had challenged monopolar TURP in terms
of less perioperative blood loss but there is no data
IJISRT19AUG982 www.ijisrt.com 793
Volume 4, Issue 8, August – 2019 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
available regarding comparison of amount of blood loss by recording pre-operative and post-operative (after 24
between these two techniques. Rationale of the study is to hours) hematocrit level.
find out if blood loss with bipolar is significantly less. If we
are able to prove this then patients with expectant larger Perioperative Blood loss in the operation and post-
blood loss with monopolar diathermy may be treated with operative period for 24 hours was measured by hematocrit
bipolar TURP. If the role of bipolar diathermy can be and in ml. Benign prostatic hyperplasia was defined as
established in less perioperative bleeding during patients presenting with difficulty in micturition and USG
transurethral resection, we would be able to control an shows enlarged prostate (>30 ml).
important complication (bleeding) linked with monopolar
TURP. Data were analyzed by using SPSS 25. The
quantitative data like age, duration of BPH, size of prostate
Objective: and blood loss were presented in the form of Mean±S.D.
To compare the mean perioperative blood loss in Perioperative blood loss in both groups was compared
monopolar versus bipolar transurethral resection in patients through independent t-test. The value of p <0.05 was
with benign prostatic hyperplasia (BPH). significant.
II. METHODOLOGY III. RESULTS
This Randomized Controlled Trial was conducted at One hundred patients include in this study. Patients
Urology Department, Galway University Hospital, Galway, were divided in two groups i.e. Group-A (Monopolar
Republic of Ireland from 1st January 2018 to 31st December TURP) and Group-B (Bipolar TURP). The patients mean
2018. Total 100 patients with benign prostatic hyperplasia age in group-A was 65.4±17.4 years and in group-B was
(BPH) were included. The inclusion criteria was, patients 63.6±14.9 years.
with age between 55-75 years, having BPH. The exclusion
criteria was Bleeding Disorder (PT, INR >1.5 times In group-A, there were 24(48.0%) in 55-65 years age
deranged), Chronic liver disease (AST, ALT >40 u/l) and group, while 26(52.0%) were in 66-75 years age group. In
Patients with uncontrolled hypertension (140/90 mmHg) group-B, there were 27(54.0%) in 55-65 years age group,
and diabetes mellitus (FBS as 240 mg/dl). while 23(46.0%) were in 66-75 years age group. In group-
A, 30(60.0%) had duration of BPH <2 years, while
The patients were divided into two groups. Group-A 20(40.0%) had >2 years. In group-B, 25(50.0%) had
(Monopolar TURP), while Group-B (Bipolar TURP). duration of BPH <2 years, while 25(50.0%) had >2 years.
Demographic data were recorded. Investigations including
complete blood picture, urine complete and In group-A, 24(48.0%) had size of prostate <45 ml,
ultrasonography of abdomen and pelvis were done. Pre- while 26(52.0%) had >45 ml. In group-B, 25(50.0%) had
operative hematocrit of each study patient was recorded. size of prostate <45 ml, while 25(50.0%) had >45 ml. In
Patient were followed up after 24 hours of surgery in which group-A, mean peri-operative blood loss was 351.3±14.84
hematocrit level was estimated. Blood loss was calculated ml and 299.4±13.01 ml in group-B with a p-value of
0.000001, which is statistically significant.
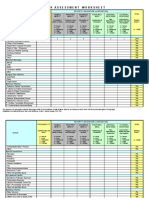
Groups
Age groups Group-A (Monopolar Total p-value
Group-B (Bipolar TURP)
TURP)
24 27 51
55-65 years
48.0% 54.0% 51.0%
26 23 49
66-75 years 0.548
52.0% 46.0% 49.0%
50 50 100
Total
100.0% 100.0% 100.0%
Table 1:- Comparison of Age Distribution between Groups
IJISRT19AUG982 www.ijisrt.com 794
Volume 4, Issue 8, August – 2019 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Groups
Duration of BPH Group-A (Monopolar Group-B (Bipolar Total p-value
TURP) TURP)
30 25 55
<2 years
60.0% 50.0% 55.0%
20 25 45
>2 years 0.315
40.0% 50.0% 45.0%
50 50 100
Total
100.0% 100.0% 100.0%
Table 2:- Comparison of Duration of BPH between Groups
Groups
Size of Prostate Group-A (Monopolar Group-B (Bipolar Total p-value
TURP) TURP)
24 25 49
<45 ml
48.0% 50.0% 49.0%
26 25 51
>45 ml 0.841
52.0% 50.0% 51.0%
50 50 100
Total
100.0% 100.0% 100.0%
Table 3:- Comparison of Size of Prostate between Groups
Groups n Mean Std. Deviation p-value
Peri-operative Blood Group-A (Monopolar
50 351.36 14.85
Loss TURP)
0.000001
Group-B (Bipolar
50 299.40 13.01
TURP)
Table 4:- Comparison of Peri-Operative Blood Loss between Groups
IV. DISCUSSION Hyponatremia and TUR syndrome are caused by using the
non-conducting irrigation fluid glycine (1.5%) in TURP,
BPH commonly affects older men that often leads which is hypo‑osmolar.14-16 Mebust et al. reported a 2%
towards troublesome symptoms and decreased quality of incidence of TUR syndrome during M‑TURP.17
life. For BPH, medical therapy is first line management
then surgery required eventually by men almost 20%.13 TURP’s new modification is B-TURP. Due to current
TURP is the most common performed surgery for BPH and flow mechanism, B-TRUP permits the surgeon to do
a large amount of data has been accumulated over the years resection using saline irrigation., decreasing the risk of
demonstrating its efficacy and safety.13 TUR syndrome and dilutional hyponatremia.18-20 This
method also allows long operation time in the large gland
Even though TURP has a low mortality rate, there is resecting. There is cut and seal effect in B-TURP and this
some concern regarding perioperative morbidity, especially one claimed to get best hemostasis than M-TURP.
hemorrhage, dilutional hyponatremia, and TUR syndrome.
IJISRT19AUG982 www.ijisrt.com 795
Volume 4, Issue 8, August – 2019 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
In our study, the mean prostate size of patients preferences, a real-world scenario. Urology Annals.
undergoing M‑TURP was 39.5±8.3 ml, and the mean 2016;8(3):291.
prostate size of patients undergoing B‑TURP was 45.4±7.2 [5]. Omar M, Lam T, Alexander C, Graham J,
(p=0.001). The difference was statistically significant. In Mamoulakis C, Imamura M et al. Systematic review
contrast to this, at least one study shows a trend toward and meta-analysis of the clinical effectiveness of
operating larger glands using monopolar technology as bipolar compared with monopolar transurethral
compared to bipolar technology, although the difference resection of the prostate (TURP). BJU International.
was not statistically significant.21 2013;113(1):24-35.
[6]. Mandal S, Singh V, Sankhwar S. Re: Huang et al.:
According to other studies reported in the literature, Bipolar Transurethral Resection of the Prostate
the mean prostate size varied from 42 to 82 ml for the Causes Deeper Coagulation Depth and Less Bleeding
M‑TURP group and for the B‑TURP group it varied from Than Monopolar Transurethral Prostatectomy
39 to 82 ml.22-24 Our study shows that there are a fair (Urology 2012;80:1116-1120). Urology.
number of men who present with markedly enlarged 2013;81(2):468.
prostates. [7]. Lv L, Wang L, Fan M, Ju W, Pang Z, Zhu Z et al.
Two-year Outcome of High-risk Benign Prostate
Possible reasons for this might be a lack of awareness Hyperplasia Patients Treated With Transurethral
and lack of access to health care, resulting in late Prostate Resection by Plasmakinetic or Conventional
presentation to a medical facility, by which time prostate Procedure. Urology. 2012;80(2):389-395.
gland would have grown considerably larger. Moreover, [8]. Pal D, Madduri V, Bera M. Monopolar versus bipolar
our study shows a surgeon’s “preference” for operating on transurethral resection of prostate for benign prostatic
the larger gland using bipolar technology. A possible hyperplasia: Operative outcomes and surgeon
explanation for this might be surgeon’s perception that preferences, a real-world scenario. Urology Annals.
“larger glands may be safely operated using bipolar 2016;8(3):291.
technology.”25 [9]. Li S, Kwong J, Zeng X, Ruan X, Liu T, Weng H et al.
Plasmakinetic resection technology for the treatment
In our study, patients who underwent M‑TURP had a of benign prostatic hyperplasia: evidence from a
mean peri-operative blood loss , 351.3±14.84 ml vs systematic review and meta-analysis. Scientific
299.4±13.01 ml who underwent B‑TURP. This was a Reports. 2015;5:12002.
statistically significant difference (p=0.000001). Reduced [10]. Kaplan S. Re: Safety and Efficacy of Bipolar versus
loss of blood in bipolar than monopolar has been focused in Monopolar Transurethral Resection of the Prostate: A
many studies.11 In one study results demonstrated that in Comparative Study. The Journal of Urology. 2017;.
bipolar TURP there is less intra-operative blood loss than [11]. Tawfik A, Soliman M, Aboelenen M. Can transrectal
monopolar TURP (238.5±69.43ml vs. 289.6±89.47ml).11 In intraprostatic injection of local vasoconstrictor
another study, Bipolar TURP associated with significantly reduces blood loss during transurethral resection of
less blood loss than monopolar TURP (300.0±2.47ml vs. moderately enlarged prostate: A randomized
349.0±3.5ml).12 controlled trial. European Urology Supplements.
2016;15(3):971.
V. CONCLUSION [12]. Nour HH, Elkady HW, Hussein M, Kamal AM,
Elganzoury HM, Elbaz AG. Bipolar Transurethral
Bipolar diathermy usage in TURP is found to be a Resection of the Prostate: Perioperative Safety and
very effective alternative to monopolar diathermy in terms Functional Outcome: Prospective Randomized Study.
of reducing blood loss and post-operative morbidity. World J Med Sci. 2014;11(4):439-44.
[13]. Yoon CJ, Kim JY, Moon KH, Jung HC, Park TC.
REFERENCES Transurethral resection of the prostate with a bipolar
tissue management system compared to conventional
[1]. McAninch J, Lue T, Smith D. Smith and Tanagho's monopolar resectoscope: One‑year outcome. Yonsei
general urology. 1st ed. New York: McGraw-Hill Med J 2006;47:715‑20.
Medical; 2013. [14]. Doll HA, Black NA, McPherson K, Flood AB,
[2]. de la Rosette J, Alivizatos G, Madersbacher S, Williams GB, Smith JC. Mortality, morbidity and
Perachino M, Thomas D, Desgrandchamps F et al. complications following transurethral resection of the
EAU Guidelines on Benign Prostatic Hyperplasia prostate for benign prostatic hypertrophy. J Urol
(BPH). European Urology. 2001;40(3):256-263. 1992;147:1566‑73.
[3]. Karadeniz M, Bayazit E, Aksoy O, Salviz E, Tefik T, [15]. Horninger W, Unterlechner H, Strasser H, Bartsch G.
Sanli O et al. Bipolar versus monopolar resection of Transurethral prostatectomy: Mortality and morbidity.
benign prostate hyperplasia: a comparison of plasma Prostate 1996;28:195‑200.
electrolytes, hemoglobin and TUR syndrome. [16]. Uchida T, Ohori M, Soh S, Sato T, Iwamura M, Ao T,
SpringerPlus. 2016;5(1). et al. Factors influencing morbidity in patients
[4]. Pal D, Madduri V, Bera M. Monopolar versus bipolar undergoing transurethral resection of the prostate.
transurethral resection of prostate for benign prostatic Urology 1999;53:98‑105.
hyperplasia: Operative outcomes and surgeon
IJISRT19AUG982 www.ijisrt.com 796
Volume 4, Issue 8, August – 2019 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
[17]. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC.
Transurethral prostatectomy: Immediate and
postoperative complications. A cooperative study of
13 participating institutions evaluating 3,885 patients.
J Urol 1989;141:243‑7.
[18]. Botto H, Lebret T, Barré P, Orsoni JL, Hervé JM,
Lugagne PM. Electrovaporization of the prostate with
the Gyrus device. J Endourol 2001;15:313‑6.
[19]. Eaton AC, Francis RN. The provision of transurethral
prostatectomy on a day‑case basis using bipolar
plasma kinetic technology. BJU Int 2002;89:534‑7.
[20]. Wendt‑Nordahl G, Häcker A, Reich O, Djavan B,
Alken P, Michel MS. The vista system: A new bipolar
resection device for endourological procedures:
Comparison with conventional resectoscope. Eur Urol
2004;46:586‑90.
[21]. Giulianelli R, Albanesi L, Attisani F, Gentile BC,
Vincenti G, Pisanti F, et al. Comparative randomized
study on the efficaciousness of endoscopic bipolar
prostate resection versus monopolar resection
technique 3 year follow‑up. Arch Ital Urol Androl
2013;85:86‑91.
[22]. Erturhan S, Erbagci A, Seckiner I, Yagci F, Ustun A.
Plasmakinetic resection of the prostate versus standard
transurethral resection of the prostate: A prospective
randomized trial with 1‑year follow‑up. Prostate
Cancer Prostatic Dis 2007;10:97‑100.
[23]. Bhansali M, Patankar S, Dobhada S, Khaladkar S.
Management of large (>60 g) prostate gland:
PlasmaKinetic Superpulse (bipolar) versus
conventional (monopolar) transurethral resection of
the prostate. J Endourol 2009;23:141‑5.
[24]. Akçayöz M, Kaygisiz O, Akdemir O, Aki FT, Adsan
O, Cetinkaya M. Comparison of transurethral
resection and plasmakinetic transurethral resection
applications with regard to fluid absorption amounts
in benign prostate hyperplasia. Urol Int
2006;77:143‑7.
[25]. Omar MI, Lam TB, Alexander CE, Graham J,
Mamoulakis C, Imamura M, et al. Systematic review
and meta‑analysis of the clinical effectiveness of
bipolar compared with monopolar transurethral
resection of the prostate (TURP). BJU Int
2014;113:24‑35.
IJISRT19AUG982 www.ijisrt.com 797
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (895)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- Canadian Pharmacy Review Ver1Dokumen6 halamanCanadian Pharmacy Review Ver1Dr-Usman Khan30% (10)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- Advanced Handbook of Systemic Lupus ErythematosusDokumen179 halamanAdvanced Handbook of Systemic Lupus ErythematosusCésar CuadraBelum ada peringkat
- Biology Combined Science Notes: Changamire Farirayi D.T. Form 3 & 4 BiologyDokumen67 halamanBiology Combined Science Notes: Changamire Farirayi D.T. Form 3 & 4 BiologyKeiron Cyrus100% (6)
- Study Assessing Viability of Installing 20kw Solar Power For The Electrical & Electronic Engineering Department Rufus Giwa Polytechnic OwoDokumen6 halamanStudy Assessing Viability of Installing 20kw Solar Power For The Electrical & Electronic Engineering Department Rufus Giwa Polytechnic OwoInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- An Industry That Capitalizes Off of Women's Insecurities?Dokumen8 halamanAn Industry That Capitalizes Off of Women's Insecurities?International Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Factors Influencing The Use of Improved Maize Seed and Participation in The Seed Demonstration Program by Smallholder Farmers in Kwali Area Council Abuja, NigeriaDokumen6 halamanFactors Influencing The Use of Improved Maize Seed and Participation in The Seed Demonstration Program by Smallholder Farmers in Kwali Area Council Abuja, NigeriaInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Unmasking Phishing Threats Through Cutting-Edge Machine LearningDokumen8 halamanUnmasking Phishing Threats Through Cutting-Edge Machine LearningInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Blockchain Based Decentralized ApplicationDokumen7 halamanBlockchain Based Decentralized ApplicationInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Cyber Security Awareness and Educational Outcomes of Grade 4 LearnersDokumen33 halamanCyber Security Awareness and Educational Outcomes of Grade 4 LearnersInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Forensic Advantages and Disadvantages of Raman Spectroscopy Methods in Various Banknotes Analysis and The Observed Discordant ResultsDokumen12 halamanForensic Advantages and Disadvantages of Raman Spectroscopy Methods in Various Banknotes Analysis and The Observed Discordant ResultsInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Smart Health Care SystemDokumen8 halamanSmart Health Care SystemInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Impact of Silver Nanoparticles Infused in Blood in A Stenosed Artery Under The Effect of Magnetic Field Imp. of Silver Nano. Inf. in Blood in A Sten. Art. Under The Eff. of Mag. FieldDokumen6 halamanImpact of Silver Nanoparticles Infused in Blood in A Stenosed Artery Under The Effect of Magnetic Field Imp. of Silver Nano. Inf. in Blood in A Sten. Art. Under The Eff. of Mag. FieldInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Compact and Wearable Ventilator System For Enhanced Patient CareDokumen4 halamanCompact and Wearable Ventilator System For Enhanced Patient CareInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Visual Water: An Integration of App and Web To Understand Chemical ElementsDokumen5 halamanVisual Water: An Integration of App and Web To Understand Chemical ElementsInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Smart Cities: Boosting Economic Growth Through Innovation and EfficiencyDokumen19 halamanSmart Cities: Boosting Economic Growth Through Innovation and EfficiencyInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Parastomal Hernia: A Case Report, Repaired by Modified Laparascopic Sugarbaker TechniqueDokumen2 halamanParastomal Hernia: A Case Report, Repaired by Modified Laparascopic Sugarbaker TechniqueInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Predict The Heart Attack Possibilities Using Machine LearningDokumen2 halamanPredict The Heart Attack Possibilities Using Machine LearningInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Keywords:-Ibadhy Chooranam, Cataract, Kann Kasam,: Siddha Medicine, Kann NoigalDokumen7 halamanKeywords:-Ibadhy Chooranam, Cataract, Kann Kasam,: Siddha Medicine, Kann NoigalInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Insights Into Nipah Virus: A Review of Epidemiology, Pathogenesis, and Therapeutic AdvancesDokumen8 halamanInsights Into Nipah Virus: A Review of Epidemiology, Pathogenesis, and Therapeutic AdvancesInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Implications of Adnexal Invasions in Primary Extramammary Paget's Disease: A Systematic ReviewDokumen6 halamanImplications of Adnexal Invasions in Primary Extramammary Paget's Disease: A Systematic ReviewInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Parkinson's Detection Using Voice Features and Spiral DrawingsDokumen5 halamanParkinson's Detection Using Voice Features and Spiral DrawingsInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- The Relationship Between Teacher Reflective Practice and Students Engagement in The Public Elementary SchoolDokumen31 halamanThe Relationship Between Teacher Reflective Practice and Students Engagement in The Public Elementary SchoolInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Air Quality Index Prediction Using Bi-LSTMDokumen8 halamanAir Quality Index Prediction Using Bi-LSTMInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Quantifying of Radioactive Elements in Soil, Water and Plant Samples Using Laser Induced Breakdown Spectroscopy (LIBS) TechniqueDokumen6 halamanQuantifying of Radioactive Elements in Soil, Water and Plant Samples Using Laser Induced Breakdown Spectroscopy (LIBS) TechniqueInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Investigating Factors Influencing Employee Absenteeism: A Case Study of Secondary Schools in MuscatDokumen16 halamanInvestigating Factors Influencing Employee Absenteeism: A Case Study of Secondary Schools in MuscatInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- An Analysis On Mental Health Issues Among IndividualsDokumen6 halamanAn Analysis On Mental Health Issues Among IndividualsInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Harnessing Open Innovation For Translating Global Languages Into Indian LanuagesDokumen7 halamanHarnessing Open Innovation For Translating Global Languages Into Indian LanuagesInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Diabetic Retinopathy Stage Detection Using CNN and Inception V3Dokumen9 halamanDiabetic Retinopathy Stage Detection Using CNN and Inception V3International Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Dense Wavelength Division Multiplexing (DWDM) in IT Networks: A Leap Beyond Synchronous Digital Hierarchy (SDH)Dokumen2 halamanDense Wavelength Division Multiplexing (DWDM) in IT Networks: A Leap Beyond Synchronous Digital Hierarchy (SDH)International Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Advancing Healthcare Predictions: Harnessing Machine Learning For Accurate Health Index PrognosisDokumen8 halamanAdvancing Healthcare Predictions: Harnessing Machine Learning For Accurate Health Index PrognosisInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- The Making of Object Recognition Eyeglasses For The Visually Impaired Using Image AIDokumen6 halamanThe Making of Object Recognition Eyeglasses For The Visually Impaired Using Image AIInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- The Utilization of Date Palm (Phoenix Dactylifera) Leaf Fiber As A Main Component in Making An Improvised Water FilterDokumen11 halamanThe Utilization of Date Palm (Phoenix Dactylifera) Leaf Fiber As A Main Component in Making An Improvised Water FilterInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Terracing As An Old-Style Scheme of Soil Water Preservation in Djingliya-Mandara Mountains - CameroonDokumen14 halamanTerracing As An Old-Style Scheme of Soil Water Preservation in Djingliya-Mandara Mountains - CameroonInternational Journal of Innovative Science and Research TechnologyBelum ada peringkat
- Reviewer in MCNDokumen16 halamanReviewer in MCNChristian Clyde Noel JakosalemBelum ada peringkat
- Systema Let Every BreathDokumen82 halamanSystema Let Every BreathB Agel100% (1)
- 2018 Surgical Rescue in Medical PatientsDokumen11 halaman2018 Surgical Rescue in Medical PatientsgiseladlrBelum ada peringkat
- Nematodes of The Turkey Meleagris Gallopavo (Galliformes: Phasianidae) From Al-Nasiryah, IraqDokumen6 halamanNematodes of The Turkey Meleagris Gallopavo (Galliformes: Phasianidae) From Al-Nasiryah, IraqMd Ashikur RahmanBelum ada peringkat
- Kelseys ResumeDokumen1 halamanKelseys Resumeapi-401573835Belum ada peringkat
- IC Risk Assessment Worksheet - Kangas-V2.1-Aug.2010 1Dokumen4 halamanIC Risk Assessment Worksheet - Kangas-V2.1-Aug.2010 1Juon Vairzya AnggraeniBelum ada peringkat
- Blood Is Thicker Than WaterDokumen4 halamanBlood Is Thicker Than WateraontreochBelum ada peringkat
- Adult Early Warning Score Observation Chart For Cardiothoracic UnitDokumen1 halamanAdult Early Warning Score Observation Chart For Cardiothoracic UnitalexipsBelum ada peringkat
- Information On The Use of Domperidone To Increase Milk Production in Lactating WomenDokumen3 halamanInformation On The Use of Domperidone To Increase Milk Production in Lactating WomenKhairul HananBelum ada peringkat
- Meralgia ParaestheticaDokumen4 halamanMeralgia ParaestheticaNatalia AndronicBelum ada peringkat
- Cytogenetics - Prelim TransesDokumen15 halamanCytogenetics - Prelim TransesLOUISSE ANNE MONIQUE L. CAYLOBelum ada peringkat
- NCRP 160 PDFDokumen81 halamanNCRP 160 PDFmarkBelum ada peringkat
- 2 - Cannabis Intoxication Case SeriesDokumen8 halaman2 - Cannabis Intoxication Case SeriesPhelipe PessanhaBelum ada peringkat
- 24 Bio Fertilization of BananaDokumen6 halaman24 Bio Fertilization of Bananamiceli57Belum ada peringkat
- Hypnosis For Irritable Bowel SyndromeDokumen3 halamanHypnosis For Irritable Bowel SyndromeImam Abidin0% (1)
- AUB - Microscopic Analysis of UrineDokumen4 halamanAUB - Microscopic Analysis of UrineJeanne Rodiño100% (1)
- A Manual 20199 CompleetDokumen201 halamanA Manual 20199 CompleetJanPerezBelum ada peringkat
- Complications of DiabetesDokumen3 halamanComplications of Diabetesa7wfBelum ada peringkat
- Biology Viral DiseasesDokumen11 halamanBiology Viral DiseasesPrasoon Singh RajputBelum ada peringkat
- DR Ololade 038Dokumen13 halamanDR Ololade 038Andrawus DanjumaBelum ada peringkat
- DSM OcdDokumen2 halamanDSM Ocdnmyza89Belum ada peringkat
- HED 2007 Cellular Molecular, Microbiology & GeneticsDokumen16 halamanHED 2007 Cellular Molecular, Microbiology & Geneticsharyshan100% (1)
- Music Therapy in Nursing HomesDokumen7 halamanMusic Therapy in Nursing Homesapi-300510538Belum ada peringkat
- Sri Lanka - Averting A National Nutrition Anomaly 2Dokumen16 halamanSri Lanka - Averting A National Nutrition Anomaly 2Rushan LakdimuthuBelum ada peringkat
- International Rice Research Notes Vol.18 No.1Dokumen69 halamanInternational Rice Research Notes Vol.18 No.1ccquintosBelum ada peringkat
- Breast Imaging Review - A Quick Guide To Essential Diagnoses (2nd Edition) PDFDokumen264 halamanBreast Imaging Review - A Quick Guide To Essential Diagnoses (2nd Edition) PDFGregorio Parra100% (2)
- 1.11 ANATOMY - The Nose and Paransal SinusesDokumen4 halaman1.11 ANATOMY - The Nose and Paransal SinusesPaolo NaguitBelum ada peringkat