Newborn Assessment Head to Toe
Diunggah oleh
marycrisDeskripsi Asli:
Judul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Newborn Assessment Head to Toe
Diunggah oleh
marycrisHak Cipta:
Format Tersedia
Maternal and Child Health Nursing
Newborn Assessment
MATERNAL and CHILD HEALTH NURSING
NEWBORN ASSESSMENT
Lecturer: Mark Fredderick R. Abejo RN, MAN
______________________________________________________________________
Newborn Assessment
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
Newborn Assessment and Nursing Care Tachypnea - respirations > 60
Persistent irregular breathing
Excessive mucus
Temperature - range 36.5 to 37 axillary Persistant fine crackles
Common variations Stridor
o Crying may elevate temperature
Stabilizes in 8 to 10 hours after Breathing ( ventilating the lungs)
delivery check for breathlessness
o Temperature is not reliable indicator if breathless, give 2 breaths-
of infection ambu bag
A temperature less than 36.5 1 yr old- mouth to mouth, pinch nose
Temp: rectal- newborn – to rule out imperforate < 1 yr – mouth to nose
Anus force – different between baby &
- take it once only, 1 inch insertion child
infant – puff
Imperforate anus Circulation
1. atretic – no anal opening Check for pulslessness :carotid-
2. agenetialism – no genital adult
3. stenos – has opening Brachial – infants
4. membranous – has opening CPR – breathless/pulseless
Earliest sign: Compression – inf – 1 finger breath
1. no mecomium below nipple line or 2 finger breaths
2. abd destention or thumb
3. foul odor breath CPR inf 1:5
4. vomitous of fecal matter Adults 2:30
5. can aspirate – resp problem
Mgt: Surgery with temporary colostomy Blood Pressure - not done routinely
Factors to consider
Heart Rate Varies with change in activity level
range 120 to 160 beats per minute Appropriate cuff size important for accurate
Common variations reading
Heart rate range to 100 when sleeping 65/41 mmHg
to 180 when crying
Color pink with acrocyanosis General Measurements
Heart rate may be irregular with Head circumference - 33 to 35 cm
crying Expected findings
Although murmurs may be due to Head should be 2 to 3 cms larger than the
transitional circulation-all murmurs chest
should be followed-up and referred for Abdominal circumference – 31-33 cm
medical evaluation Weight range - 2500 - 4000 gms (5 lbs. 8oz.
Deviation from range - 8 lbs. 13 oz.)
Faint sound Length range - 46 to 54 cms (19 - 21 inches)
Normal length- 19.5 – 21 inch or 47.5 –
Cardiac rate: 120 – 160 bpm newborn 53.75cm, average 50 cm
Apical pulse – left lower nipple Head circumference 33- 35 cm or 13 – 14 “
Radial pulse – normally absent. If present PDA
Femoral pulse – normal present. If absent COA Hydrocephalus - >14”
Chest 31 – 33 cm or 12 – 13”
Respiration Abd 31 – 33 cm or 12 – 13”
- range 30 to 60 breaths per minute
Common variations
Bilateral bronchial breath sounds Signs of increased ICP
Moist breath sounds may be present 1. abnormally large head
shortly after birth 2. bulging and tense fontanel
Signs of potential distress or deviations 3. increase BP and widening pulse pressure
from expected findings 4. Decreased RR, decreased PR
Asymmetrical chest movements 5. projective vomiting- sure sign of cerebral
Apnea >15 seconds irritation
Diminished breath sounds 6. high deviation – diplopia – sign of ICP older
Seesaw respirations child
Grunting a. 4-6 months- normal eye deviation
Nasal flaring b. >6 months- lazy eyes
Retractions 7. High pitch shrill cry-late sign of ICP
Deep sighing
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
Head to Toe Newborn Assessment
CIRCULATORY UMBILICAL VEIN and DUCTUS VENOSUS constrict after cord id clamped
STATUS DUCTUS ARTERIOSUS constrict with establishment of respiratory function
FORAMEN OVALE closes functionally as respirations established, but anatomic or
permanent closure may take several months
HEART RATE averages 140 b.p.m.
BP 73/55 mmHg
PERIPHERAL CIRCULATION acrocyanosis within 24 hours
RBC high immediately after birth; falls after 1 st week
ABSENCE/ NORMAL FLORA INTESTINE Vitamin K
RESPIRATORY Adequate levels of surfactants (Lecithin and spingomyelin) ensure mature lung
STATUS function; prevent alveolar collapse and respiratory distress syndrome
RR = 30-80 breaths /minutes with short periods of apnea (< 15 seconds) = assess for
1 full minute change noted during sleep or activity
NOTE: Periodic apnea is common in preterm infants. Usually, gentle stimulation is
sufficient to get the infant to breathe
RENAL SYSTEM Urine present in the bladder at birth but NB may not void doe 1st 12-24 hours
Later pattern is 6-10 voidings/ day – indicative of sufficient fluid intake
Urine is pale and straw colored – initial voidings may leave brick-red spots on
diaper ( d/t passage of uric acid crystals in urine)
Infant unable to concentrate urine for the 1st 3 months
DIGESTIVE IMMATURE CARDIAC SPHINCTER – may allow reflux of food, burped,
SYSTEM REGURGITATE- placed NB right side after feeding
Newborn can’t move food from lips to pharynx. Insert nipple well to mouth
FEEDING PATTERS vary
- Newborns may nurse vigorously immediately afterbirth or may need as long as
several days to suck effectively
- Provide support and encouragement to new mothers during this time as infant
feeding is very emotional doe most mothers
NOTE: Distinguishing Neonatal Vomiting from Regurgitation
Vomiting is usually sour, looks like curdled milk due to HCL, with a sour odor, while
regurgitation has no sour odor or curdling of milk, or occurs during or immediately
after feeding.
IMPORTANT CONSIDERATIONS:
Breastfeeding can usually begin immediately after birth; bottle-fed newborns
may be offered few milliliters of sterile water or 5% dextrose 1 to 4 hours after
birth prior to a feeding with formula
An infant with gastrostomy tube should receive a pacifier during feeding
unless contraindicated to provide normal sucking activity and satisfy oral
needs.
At age4-6 months, an infant should begin to receive solid food foods one at a
time and 1 week apart.
FIRST STOOL is MECONIUM
- Black, tarry residue from lower intestine
- Usually passed within 12-24 hours after birth
If the amniotic fluid shows evidence of meconium staining, the physician most likely do
immediately after delivery is to suction the oropharynx immediately after the head is
delivered and before the chest is delivered.
TRANSITIONAL STOOLS thin, brownish green in color
After 3 days MILK STOOLS are usually passed
a. MILK STOOLS for BF infant – loose and golden yellow
b. MILK STOOLS for FORMULATED FED- formed and pale yellow
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
HEPATIC Liver responsible for changing Hgb into conjugated bilirubin, which is further
changed into conjugated (water soluble) bilirubin that can be excreted
Excess unconjugated bilirubin can permeate the sclera and the skin, giving a jaundiced
or yellow appearance to these tissues
TEMPERATURE HEAT PRODUCTION in newborn accomplished by:
a. Metabolism of “ BROWN FAT”
- A special structure in NB is a source of heat
- Increased metabolic rate and activity
Axillary temperature: 96.8 to 99F
Newborn can’t shiver as an adult does to release heat
Newborns are unable to maintain a stable body temperature because they have an
immature vasomotor center, and unable to shiver to increase body heat.
NB’s body temperature drops quickly after birth – after stress occurs easily
Body stabilizes temperature in 8-10 hours if unstressed
Cold stress increases o2 consumption – may lead to metabolic acidosis and
respiratory distress
IMMUNOLOGIC NB develops own antibodies during 1st 3 months but at risk for infection during the
first 6 weeks
Ability to develop antibodies develops sequentially
Neonatal Physical Assessment
Birth weight=2500-400 grams (5 lbs. 8oz. – 8 lbs. 13 oz.)
Length= 45.7 – 55.9 cm. (18-22 inches)
HEAD Head circumference = 33-35 cm (2-3 cm. Greater than chest circumference)
Anterior fontanel (diamond shape) = closes 12-18 months
Posterior fontanel (triangle shape)= closes 2-3 months
NOTE: The posterior fontanel is located at the intersection of the sagittal and
lambdoid suture is the space between the pariental bones; the lambdoid suture
separates the two parietal bones and the occipital bone
Molding- asymmetry of head as a result of pressure in birth cana
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
EYES Blue/ gray d/t scleral thinness; permanent color established w/in 3-12 mos.
Lacrimal glands immature at birth; tearless cry up to 2 months
Absence of tears is common because the neonate’s tear glands are not yet fully
developed
Transient strabismus
Doll’s eye reflex persist for about ten days
Red Reflex: A red circle on the pupils seen when an ophthalmoscope’s light is shining
onto the retina is a normal finding. This indicates that the light is shining onto the
retina.
CONVERGENT STRABISMUS (CROSS EYED)
It is common during infancy until age 6 months because of poor oculomotor
coordination
NOTE : Congenital Glaucoma
It is due to increased intraocular pressure caused by an abnormal outflow or
manufacturing of normal eye fluid.
Unequal size should be reported immediately.
NOSE Nose breathers for first few months of life
MOUTH Scant saliva with pink lips
Epstein’s Pearls - small shiny white specks on the neonate’s gums and hard palate
which are normal
EARS Incurving of pinna and cartilage deposition
NECK Short and weak with deep fold of skin
CHEST Characterized by cylindrical thorax and flexible ribs
NOTE:
appears circular since anteroposterior and lateral diameters are about equal
Respirations appear diaphragmatic
Nipples prominent and often edematous
Milky secretion (witch's milk) common ( effect of estrogen)
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
ABDOMEN Cylindrical with some protrusion; scaphoid appearance indicates diaphragmatic hernia
Umbilical cord is white and gelatinous with two arteries and one vein and begins to dry
within 1-2 hours after delivery
NOTE: Umbilical cord
Three vessels, two arteries and one vein, in cord; if fewer than three vessels
are noted notify the physician
Small, thin cord may be associated with poor fetal growth
Assess for intact cord, and ensure that damp is cured
Cord should be clamped for at least the first 4 hours after birth; clamp can
be removed hen the cord is dried and occluded
Umbilical clamp can be removed after 24 hours
GENITALIA MALE: includes rugae on the scrotum and testes descended into the scrotum
Urinary meatus:
Hypospadias (ventral surface)
Epispadias (dorsal surface)
NOTE:
Meatus at tip of penis
Testes descended but may retract with cold
Assess for hernia or hydrocele
First voiding should occur within 24 hours
FEMALE: labia majora cover labia minora and clitoris
Pseudomenstruation possible (blood-tinged mucus) effect of estrogen
First voiding should occur within 24 hours
EXTREMITIES All neonates have bowlegged and flat feet
NOTE NORMAL FEATURES:
Major gluteal folds even
Creases on soles of feet
Assess for fractures (especially clavicle) or dislocations (hip)
Assess for hip dysplasia; when thighs are rotated outward, no clicks should be
heard
Some neonates may have abnormal extremities:
Polydactyl (more than 5 digits on extremity)
Syndactyl (two or more digits fused together)
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
Polydactyl Syndactyl
SPINE Should be straight and flat
Anus should be patent without any fissure
Dimpling at the base is associated with spina bifida
A degree of hypotonicity or hypertonicity is indicative of central nervous system (CNS
damage)
SKIN Assessment for Jaundice
The #1 technique is to blanch the skin over the bony prominence such as the
forehead, chest or tip of the nose.
NOTE: Jaundice starts at the head first, spreads to the chest, then the abdomen, then the
arms and legs, followed by the hands and feet, which are the last to be jaundiced.
Jaundice in the first 24 hours after the birth is a cause for concern that requires
further assessment. Possible causes of early jaundice are blood incompatibility,
oxytocin induction, and severe hemolytic process.
Mongolian Spots
Gary, blue or black marks that are frequently found on the sacral area, buttocks, arms
shoulders or other areas.
Harlequins Sign
Occurs on one side of the body turns deep red color. It occurs when blood vessels on
one side constrict, while those on the other side of the body dilate.
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
Erythema toxicum
Is an eruption of lesions in the area surrounding a hair follicle that are firm, vary
in size from 1-3 mm, and consist of a white or pale yellow papule or pustule w/ an
erythematous base.
It is often called “newborn rash” or “flea-bite” dermatitis
The rash may appear suddenly, usually over the trunk and diaper area and is
frequently widespread.
The lesions do not appear on the palms of the hands or soles of the feet.
The peak incidence is 24-48 hours of life.
Cause is unknown and no treatment necessary
Acrocyanosis versus Central Cyanosis
Acrocyanosis involves the extremities of the neonate, for example bluish hands
and feet due to neonates being cold or poor perfusion of the blood to the
periphery of the body.
Central cyanosis, which involves the lips, tongue and trunk indicating
HYPOXIA which needs further assessment by the nurse.
Milia are blocked sebaceous glands located on the chin and the nose of the infant.
VERNIX CASEOASA
Should not be removed by oil or hand lotion, because it is a protective layer of the
neonate after birth, and it disappears after birth. Never remove it with alcohol or
cotton balls, unless meconium skinned.
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
BIRTH MARKS
Telangiectatic nevi (stork bites)
Appear as pale pink or red spots and are frequently found on the eyelids, nose,
lower occipital bone and nape of the neck
These lesions are common in NB w/ light complexions and are more noticeable
during periods of crying. These areas have no clinical significance and usually
fade by the 2nd birthday
Hemangioma is benign vascular tumor that may be present on the newborn
3 types Hemangiomas
1. Nevus Flammeus – port wine stain – macular purple or dark red lesions seen
on face or thigh. NEVER disappear. Can be removed surgically
2. Strawberry hemangiomas – nevus vasculosus – dilated capillaries in the
entire dermal or subdermal area. Enlarges, disappears at 10 yo.
3. Cavernous hemangiomas – communication network of venules in SQ tissue
that never disappear with age.
Nevus Flammeus (port-wine stain)
A capillary angioma directly below the epidermis, is a non-elevated, sharply
demarcated, red-to-purple area of dense capillaries.
Macular purple
The size & shape vary, but it commonly appears on the face. It does not grow in
size, does not fade in time and does not blanch. The birthmark maybe concealed by
using an opaque cosmetic cream.
If convulsions and other neurologic problem accompany the nevus flammeus,----
5th cranial nerve involvement.
Nevus vasculosus (strawberry mark)
A capillary hemangioma, consists of newly formed and enlarged capillaries in the
dermal and subdermal layers.
It is a raised,clearly delineated, dark-red, rough-surfaced birthmark commonly
found in the head region.
Such marks usually grow starting the second or third week of life and may not
reach their fullest size for 1 to 3 months; disappears at the age of 1 yr. but as the
baby grows it enlarges.
Providing appropriate information about the cause and course of birthmarks often
relieves the fears and anxieties of the family. Note any bruises, abrasions,or
birthmarks seen on admission to the nursery.
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
GESTATIONAL ASSESSMENT
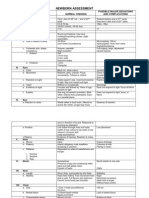
PARAMETER NURSING ‘TERM’ born between ‘PRETERM’ born before 37 weeks
ACTION 37-42 weeks gestation gestation
EAR Fold the pinna Pinna recoils (springs Pinna opens slowly or stays folded
(auricle) forward back) in very premature infants
BREAST TISSUE Measure it 3 mm Less than 3 mm
FEMALE GENITALIA Observe Labia majora cover Labia minora are more prominent;
labia minora vaginal opening can be seen
MALE GENITALIA Observe Scrotal sac very Fewer shallow rugae on the scrotum
wrinkled
HEEL CREASES Observe Extend 2/3 of the way Soles are smoother, creases extend
from the toes to the heel less than 2/3 of the way from the
toes to the heel
NEWBORN REFLEXES
Immature central nervous system (CNS) of newborn is characterized by variety of reflexes
o Some reflexes are protective, some aid in feeding, others stimulate interaction
o Assess for CNS integration
Protective reflexes are blinking, yawning, coughing, sneezing, drawing back from pain
Rooting and sucking reflexes assist with feeding
“What reflexes should be present in a newborn? Reflexes are involuntary movements or actions. Some movements
are spontaneous, occurring as part of the baby's usual activity. Others are responses to certain actions. Reflexes
help identify normal brain and nerve activity. Some reflexes occur only in specific periods of development. The
following are some of the normal reflexes seen in newborn babies””
PALMAR GRASP Newborn’s fingers curl around the examiner’s fingers and the newborn’s toes
REFLEX curl downward.
The palmar grasp reflex is elicited by placing an object in the palm of a
neonate; the neonate's fingers close around it. This reflex disappears between
ages 6 and 9 months.
Palmar response lessens within 3-4 months
Palmar response lessens within 8 months
ROOTING The rooting reflex is elicited by stroking the neonate's cheek or stroking near
REFLEX the corner of the neonate's mouth.
The neonate turns the head in the direction of the stroking, looking for food.
This reflex disappears by 6 weeks.
SUCKING The sucking reflex is seen when the neonate's lips are touched
REFLEX Lasts for about 6 months
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
MORO REFLEX Symmetric & bilateral abduction & extension of arms and hands
Thumb & forefinger form a C
“EMBRACE” reflex
Present at birth, complete response may occur up to 8 weeks
A persistent response lasting more than 6 months may indicate the occurrence
of brain damage during pregnancy
A normal reflex in a young infant caused by a sudden loud noise. It results in drawing
up the legs, an embracing position of the arms, and usually a short cry.
BABINSKI’ SIGN Beginning at the heel of the foot, gently stroke upward along the lateral aspect of
the sole; then the examiner moves the fingers along the ball of the foot
The newborn’s toes hyperextend while the big toe dorsiflexes
Absence of this reflex indicates the need for a neurological examination
The Babinski reflex is elicited by stroking the neonate's foot, on the side of the
sole, from the heel toward the toes.
A neonate will fan his toes, producing a positive Babinski sign, until about age 3
months
STEPPING OR The newborn simulates walking, alternately flexing and extending the feet
WALKING The reflex is usually present 3-4 months
REFLEX
TONIC NECK While the newborn is falling asleep or sleeping, gently and quickly turn the head
REFLEX to one side
As the newborn faces the left side, the left arm & leg extend outward while the
right arm & leg flex
When the head is turned to the right side, the right arm & leg extend outward while
the left arm & leg flex
Usually disappears within 3-4 months
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
CRAWLING Place the newborn on the abdomen
The newborn begins making crawling movements with the arms and legs
The reflex usually disappears after about 6 weeks
BASIC TEACHING NEEDS OF NEW PARENTS
CORD CARE Cleanse the cord with alcohol and sometimes triple dye once a day
Keep the area clean and dry
Keep the newborn’s diaper below the cord to prevent irritation
Signs of infection: redness, drainage, swelling, odor
Notify physician for signs of infection
NOTE:
Note any bleeding or drainage from the cord
Triple dye may be applied for initial cord care because it minimizes
microorganisms and promotes drying; use a cotton-tipped applicator to paint
the dye, one time, on the cord on 1 inch of surrounding skin
Application of 70% isopropyl alcohol to the cord with each diaper change and
at least two r three times a day to minimize microorganisms and promote
drying.
NOTE: The skin is surrounded with alcohol which promotes drying and cleans the area.
The umbilical cord dries and falls off about 14 days. Peroxide and lanolin promote
moisture, which can inhibit drying and allow growth of bacteria. Water doesn’t
promote drying.
It is best to care for the neonate’s umbilical cord area by cleaning it with cotton
pledgets moistened with alcohol. The alcohol promotes drying and helps decrease the
risk of infection. An antibiotic ointment maybe used instead of alcohol, because there
are a lot of bacteria which is resistant against some bacteria. Other agents such as
wipes, sterile water and soap & water are not as effective as alcohol.
CIRCUMCISION Observe for bleeding, first urination
CARE Apply diaper loosely to prevent irritation
Notify physician for signs of infection
BONDING Encourage parent to talk to, hold, and sing to infant
Promotes skin-to-skin contact between parent and infant
Feedings are opportunities for parent-infant bonding
Notify physician for signs of infection
NOTE: Sense of Touch
The most highly developed sense at birth that is why, neonates responds well to
touch.
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
PRE TERM INFANT ( PREMATURE INFANT)
Definition PRE TERM INFANT
A neonate born before 38 weeks age of gestation
Synonym Low birth weight
Contributing factors Low socioeconomic level
Poor nutritional status
Lack of pre natal care
Multiple pregnancy
Prior previous early birth
Race (non whites have a higher incidence of prematurity than
whites)
Cigarette smoking
The age of the mother ( the highest incidence is in mother’s
younger than age 20.)
Order of birth ( early termination is highest in first pregnancies
and in those beyond the forth )
Closely spaced pregnancies
Abnormalities of the reproductive system such as intrauterine
septum
Infections ( specially urinary tract infections)
Obstetric complications such as premature rupture of membranes
or premature separation of the placenta
Early induction of labor
Elective cesarian birth
Appears small and underdeveloped
Cardinal signs The head is disproportionately large ( 3 cm or more greater than
chest size)
Skin is thin with visible blood vessel and minimal subcutaneous
fat pads
Vernix caseosa is absent
Both anterior and posterior fontanelles are small
Abnormal laboratory values Decreased RBC’s
Decreased serum glucose
Increased concentration of indirect bilirubin
Decreased serum albumin
NOTE: The normal range of urine output for a preterm
baby is 1 to 2ml/kg/day. The normal specific gravity for a
preterm baby is 1.020. The normal range for blood glucose
level in a preterm baby is 40 to 60 mg/dl.
Best procedure Resuscitation
NOTE: resuscitation becomes important for infant who fails to
take first breath or difficulty maintaining adequate
respiratory movements on his own.
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
Suctioning
NOTE: allows removing mucus and prevents aspiration of any
mucus and amniotic fluid present in the mouth and
nose of the newborn to establish clear airway.
Intubations
NOTE: head of the infant in neutral position with towel under
shoulder.
Best position Positioning the infant on the back with the head of the mattress
elevated approximately 15 degrees to allow abdominal contents to
fall away from the diaphragm affording optimal breathing space.
Best position for suctioning:
Infant on the back and slide a folded towel or pad under shoulders
to rise, head is in neutral position.
Complications Anemia of prematurity
Hyperbilirubinemia/ kernicterus
Persistent patent ductus arteriosus
Periventricular / intraventricular hemorrhage
Respiratory distress syndrome
Retinopathy of prematurity
Retrolental fibroplasias are a complication that occurs if the
infant is overexposed to high oxygen levels.
Necrotizing enterocolitis
Bedside equipment Preterm size laryngoscope
ET tube
Suction catheter with synthetic surfactant
Isolettes (incubator)
Drug study 1. Naloxone (Narcan)
Nature of the drug:
Narcotic antagonist
Side effects:
Hypertension, irritability, tachycardia
2. Surfactan ( Survanta)
Nature of the drug:
Lung surfactant to improve lung compliance
Side effect:
Transient bradycardia, rales
3. Vitamin K (Aquamephyton)
Use for prophylaxis to treat hemorrhagic disease of the
newborn.
Side effects:
Hyperbilirubinuria
4. Eye prophylaxis
(Erythromycin 0.5% Ilotycin, Tetracycline 1%
Silver Nitrate 1% ( not already used – causes chemical
conjunctivitis)
Prophylactic measure to protect against Neisseria
gonorrhoeae and Chlamydia trachomatis
Side effects:
Silver nitrate can cause chemical conjuctivitis
Nursing diagnosis 1. Impaired gas exchange related to immature pulmonary
functioning
2. Risk for fluid volume deficit related to insensible water loss at
birth and small stomach capacity
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
3. Risk for aspiration related to weak or absent gag reflex a nd/or
administration of tube feedings
4. Hypothermia related to lack of subcutaneous and brown fat
deposits, inadequate shiver response, immature
thermoregulation center, large body surface area in relation to
body weight, and/or lack of flexion of extremities toward the
body.
5. Risk for infection related to immature immune response, stasis of
respiratory secretions, and/ or aspiration
6. Imbalanced nutrition: less than body requirements related to
lack of energy to suck and/or weak or absent sucking reflex
Nursing intervention The nurse’s first priority in preparing a safe environment for a
preterm newborn with low Apgar scores is to prepare
respiratory resuscitation equipment. Airway maintenance is the
first priority.
Give the mother oxygen by mask during the birth to provide the
preterm infant with optimal oxygen saturation at birth ( 85-90%).
Keeping maternal analgesia and anesthesia to a minimum also
offers the infant the best chance of initiating effective respiration.
Bedside larngyoscope, endotracheal tube, suction catethers and
synthetic surfactant to be administered by the endotracheal tube.
Infant must be kept warm during resuscitation procedures so he
or she is not expending extra energy to increase the metabolic
rate to maintain body temperature.
Observe for changes in respirations, color and vital signs
Check efficacy of Isolette: maintain heat, humidity and oxygen
concentration, administer oxygen only if necessary
Maintain aseptic technique to prevent infection
Adhere to the techniques of gavage feeding for safety of infant
Observe weight-gain patterns
Determine blood gases frequently to prevent acidosis. Institute
phototherapy when hyperbilirubinemia occurs
Support parents by letting them verbalize and ask questions to
relieve anxiety.
Provide liberal visiting hours for parents, allow them to
participate in care.
Arrange follow-up before and after discharge by a visiting nurse.
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
POST TERM INFANT
Definition POST TERM INFANT
A neonate born after 42 weeks age of gestation
Low socioeconomic level
Contributing factors Poor nutritional status
Lack of pre natal care
Multiparous mother’s
Cigarette smoking
The age of the mother (the highest incidence is in mother’s younger
than age 20.)
Mother’s with diabetes mellitus
Congenital abnormalities such as omphalocele.
Body is covered with lanugo
Old man facies
Classic signs Intrauterine weight loss, dehydrations and chronic hypoxia “old
man faces’
Long & thin with cracked skin which is loose, wrinkled and
strained greenish yellow, with no vernix nor lanugo
Long nails with firm skull
Wide eyed alertness of one month old baby
Abnormal laboratory Increased total no. of RBC’s
values Increased hematocrit level
Decreased serum glucose
Screening test Sonogram
Resuscitation
Best procedure NOTE: resuscitation becomes important for infant who fails to take
first breath or difficulty maintaining adequate respiratory
movements on his own.
Suctioning
NOTE: allows removing mucus and prevents aspiration of any
mucus and amniotic fluid present in the mouth and nose of the
newborn.
To establish clear airway.
Intubations
NOTE: head of the infant in neutral position with towel under
shoulder.
Positioning the infant on the back with the head of the mattress
Best position elevated approximately 15 degrees to allow abdominal contents
Complications Meconium aspiration syndrome
Respiratory distress syndrome
NOTE: Post mature neonates have difficulty maintaining glucose
reserves. Other common problems include Meconium aspiration
syndrome, polycythemia, congenital anomalies, seizure activity and cold
stress.
NOTE: The infant who are exposed to high blood-glucose levels in
utero may experience rapid and profound hypoglycemia after birth
because of the cessation of a high in-utero glucose load. The small-for-
gestational-age infant has use up glycogen stores as a result of
intrauterine malnutrition and has blunted hepatic enzymatic response
with which to carry out gluconeogenesis.
Newborn Assessment Abejo
Maternal and Child Health Nursing
Newborn Assessment
NOTE: The patient with post-term pregnancy is at high risk for
decreased placental functioning, therefore increasing the risk of
inadequate oxygen circulation to the fetus
Bedside equipment ET tube
Suction catheter
Drug study
1. Vitamin K (Aquamephyton)
Use for prophylaxis to treat hemorrhagic disease of the newborn
Side effects:
Hyperbilirubinuria
2. Eye prophylaxis
(Erythromycin 0.5% Ilotycin, Tetracycline 1% Silver Nitrate 1%
Prophylactic measure to protect against Neisseria gonorrhoeae and
Chlamydia trachomatis
Side effects:
Silver nitrate can cause chemical conjuctivitis
Nursing diagnoses 1. Ineffective airway breathing
2. Risk for fluid volume deficit related to insensible water loss at birth
3. Ineffective infant feeding pattern
Nursing interventions Assess newborn’s respiratory rate, depth and rhythm. Auscultate
lung sound.
Note: Meconium stained syndrome of POST MATURE neonates
Aspiration of meconium is best prevented by suctioning the neonate’s
nasopharynx immediatelt after the head is delivered and before the
shoulders and chest are delivered. As long as the chest is
compressed in the vagina, the infant will not inhale and aspirate
meconium in the upper respiratory tract. Meconium aspiration
blocks the air flow to the alveoli, leading to potentially life
threatening respiratory complications.
Suction every 2 hours or more often as necessary
Position newborn on side or back with the neck slightly extended
Administer O2, anticipate the need for CPAP or PEEP
Continue to assess the newborn’s respiratory status closely.
Encourage as much parental participation in the newborn’s care as
condition allows
Administer IV fluids after birth to provide Glucose to prevent
hypoglycemia, monitor closely the infusion rate.
Kept the infant under a radiant heat warmer to preserve energy
Monitor baby’s weight, serum electrolytes and ensure adequate
fluid intake
Measure urine output by weighing diapers
Check for blood stools to evaluate for possible bleeding from
intestinal tract.
Keep a restful environment.
Anticipate the infants need to be breastfeed
Demonstrate technique for feeding to mother, note proper
positioning of the infant, “latching on” technique, rate of delivery
of feeding and frequency of burping
Provide a relaxed environment during feeding
Adjust frequency and amount of feeding according to infants
response
Alternate feeding procedure (nipple and gavage feeding) according
to infants ability.
Monitor mother’s effort, provide feedback and assistance as needed
Suggest mother to monitor infants weight periodically
Newborn Assessment Abejo
Anda mungkin juga menyukai
- NEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideDari EverandNEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideBelum ada peringkat
- NEONATAL NURSE PRACTITIONER: Passbooks Study GuideDari EverandNEONATAL NURSE PRACTITIONER: Passbooks Study GuideBelum ada peringkat
- Perinatal Manual of Southwestern OntarioDokumen6 halamanPerinatal Manual of Southwestern OntarioƦя de GuzмѧN100% (1)
- Initial Newborn AssessmentDokumen14 halamanInitial Newborn Assessmentaclark831Belum ada peringkat
- Assessment of NeonateDokumen11 halamanAssessment of NeonateAbhishek GirdharBelum ada peringkat
- Newborn AssessmentDokumen7 halamanNewborn Assessmentapi-232728488Belum ada peringkat
- Assessment of The Normal NewbornDokumen6 halamanAssessment of The Normal Newborndhalal100% (2)
- Newborn AssessmentDokumen7 halamanNewborn AssessmentMJ Amarillo100% (6)
- Maternal and Child Health Nursing Care of The NewbornDokumen5 halamanMaternal and Child Health Nursing Care of The NewbornJeanilynTanBelum ada peringkat
- Neonatal NursingDokumen53 halamanNeonatal Nursingkrishnasree100% (1)
- Newborn AssessmentDokumen15 halamanNewborn Assessmentmarie97% (35)
- Newborn AssessmentDokumen3 halamanNewborn AssessmentValerie Ybañez Peñalber100% (2)
- Managing High-Risk NewbornsDokumen19 halamanManaging High-Risk Newbornssantosh s u100% (1)
- Essential Newborn Resuscitation StepsDokumen27 halamanEssential Newborn Resuscitation StepsAnusha Verghese100% (1)
- 986 Assessment of New Born NursingDokumen91 halaman986 Assessment of New Born NursingkrishnaBelum ada peringkat
- Care of The Newborn PDFDokumen5 halamanCare of The Newborn PDFzhai bambalan100% (2)
- New Born CareDokumen22 halamanNew Born Caredexter100% (8)
- Pediatric NursingDokumen37 halamanPediatric Nursingjairize100% (5)
- Labor and DeliveryDokumen7 halamanLabor and Deliveryplethoraldork100% (20)
- Assessment of NewbornDokumen33 halamanAssessment of Newbornmehta shivaniBelum ada peringkat
- Admission of Neonates in Nicu & Nursing ManagementDokumen30 halamanAdmission of Neonates in Nicu & Nursing ManagementMonika shankarBelum ada peringkat
- Newborn AssessmentDokumen24 halamanNewborn Assessmentvincentsharon100% (2)
- Newborn AssessmentDokumen8 halamanNewborn Assessmentapi-283260051Belum ada peringkat
- Assessing Preterm BabyDokumen5 halamanAssessing Preterm BabyJoyce Kathreen Ebio LopezBelum ada peringkat
- Normal NewbornDokumen30 halamanNormal NewbornLekshmi Manu100% (3)
- Newborn Assessment ToolDokumen5 halamanNewborn Assessment ToolReana AbillarBelum ada peringkat
- Principles of Postpartum Nursing CareDokumen2 halamanPrinciples of Postpartum Nursing CareZaire DylanBelum ada peringkat
- Pediatric DR PDFDokumen135 halamanPediatric DR PDFVinu Poojapranavam100% (1)
- Brain 16-ObDokumen1 halamanBrain 16-ObNurse Betty100% (2)
- Maternity Study GuideDokumen43 halamanMaternity Study Guidepgmanski100% (23)
- Care of The NewbornDokumen5 halamanCare of The Newbornbuzz Q100% (2)
- Neonatal SepsisDokumen63 halamanNeonatal SepsisDemewoz Fikir100% (2)
- Immediate Newborn Care-DOH 2010Dokumen2 halamanImmediate Newborn Care-DOH 2010fegerilene100% (2)
- High Risk NeonateDokumen85 halamanHigh Risk NeonateWed Lod100% (1)
- BubbleDokumen12 halamanBubblekarloeguiareyesBelum ada peringkat
- PEDIATRIC NURSING NOTESDokumen23 halamanPEDIATRIC NURSING NOTESQuennie Gumapac-PabloBelum ada peringkat
- Pediatrics Study GuideDokumen22 halamanPediatrics Study GuideElizabeth McKee100% (1)
- Newborn Assessment NORMALDokumen2 halamanNewborn Assessment NORMALVanessaMUellerBelum ada peringkat
- Caring for High-Risk Newborns and Their FamiliesDokumen14 halamanCaring for High-Risk Newborns and Their FamiliesElaisa Mae Delos Santos100% (1)
- Routine New Born Care GNMDokumen55 halamanRoutine New Born Care GNMLeena Pravil100% (3)
- EngDokumen54 halamanEngAiralyn Chavez Alaro100% (1)
- Nicu Must KnowsDokumen7 halamanNicu Must KnowsCyfern100% (2)
- NICU Survival GuideDokumen14 halamanNICU Survival Guidesedaka26Belum ada peringkat
- Introduction To Modern Concept of Childcare & History, Principles & Scope of Child Health NursingDokumen17 halamanIntroduction To Modern Concept of Childcare & History, Principles & Scope of Child Health Nursingsuper cool100% (2)
- Essential Newborn Care GuideDokumen120 halamanEssential Newborn Care Guidejuly3ciaBelum ada peringkat
- Newborn Assessment ChecklistDokumen57 halamanNewborn Assessment Checklistmuiz muhammadBelum ada peringkat
- Newborn CareDokumen282 halamanNewborn CarecikiricaBelum ada peringkat
- Nursing Care For A High Risk NewbornDokumen16 halamanNursing Care For A High Risk NewbornAj MacotoBelum ada peringkat
- Congenital Heart DiseasesDokumen6 halamanCongenital Heart DiseasesMox SwanBelum ada peringkat
- High Risk NewbornDokumen20 halamanHigh Risk Newborndmrdy50% (2)
- Normal Postpartum Changes Parameter First 24 H Clinical Heart RateDokumen14 halamanNormal Postpartum Changes Parameter First 24 H Clinical Heart RatemiacajBelum ada peringkat
- Amniiotic Band Syndrome Cleft Lip/palate Congenital Limb Defects Duodenal AtresiaDokumen18 halamanAmniiotic Band Syndrome Cleft Lip/palate Congenital Limb Defects Duodenal AtresiaMJ Amarillo100% (3)
- Pediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)Dari EverandPediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)Belum ada peringkat
- LOW RISK NEONATAL NURSING: Passbooks Study GuideDari EverandLOW RISK NEONATAL NURSING: Passbooks Study GuideBelum ada peringkat
- Inpatient Obstetric Nurse Exam Prep 2020-2021: A New Study Guide for Certification Including 300 Test Questions and Answers with Full Explanations (RNC-OB)Dari EverandInpatient Obstetric Nurse Exam Prep 2020-2021: A New Study Guide for Certification Including 300 Test Questions and Answers with Full Explanations (RNC-OB)Belum ada peringkat
- Intensive Parenting: Surviving the Emotional Journey through the NICUDari EverandIntensive Parenting: Surviving the Emotional Journey through the NICUBelum ada peringkat
- Newborn Resuscitation GuideDokumen40 halamanNewborn Resuscitation GuideAnggun Permata Sari SuknaBelum ada peringkat
- Principles of Physical AssessmentDokumen58 halamanPrinciples of Physical AssessmentAnna Fayeziah YussophBelum ada peringkat
- Apgar Scoring Description: 2 Points 1 Point 0 Points Point/SDokumen6 halamanApgar Scoring Description: 2 Points 1 Point 0 Points Point/SksjsellsBelum ada peringkat
- Fitting A Logistic Curve To DataDokumen12 halamanFitting A Logistic Curve To DataXiaoyan ZouBelum ada peringkat
- Cost Accounting - LabourDokumen7 halamanCost Accounting - LabourSaad Khan YTBelum ada peringkat
- HED - PterygiumDokumen2 halamanHED - Pterygiumterry johnsonBelum ada peringkat
- Synthesis of The ArtDokumen2 halamanSynthesis of The ArtPiolo Vincent Fernandez100% (1)
- English Literature RevisionDokumen61 halamanEnglish Literature RevisionAlex Cobain Glinwood100% (1)
- WritingSubmission OET20 SUMMARIZE SUBTEST WRITING ASSESSMENT 726787 40065 PDFDokumen6 halamanWritingSubmission OET20 SUMMARIZE SUBTEST WRITING ASSESSMENT 726787 40065 PDFLeannaBelum ada peringkat
- Bullish EngulfingDokumen2 halamanBullish EngulfingHammad SaeediBelum ada peringkat
- Zeal Study 10th English Synonym Unit 1 - 7Dokumen24 halamanZeal Study 10th English Synonym Unit 1 - 7viaanenterprises2008Belum ada peringkat
- IkannnDokumen7 halamanIkannnarya saBelum ada peringkat
- OutliningDokumen17 halamanOutliningJohn Mark TabbadBelum ada peringkat
- A Comparative Look at Jamaican Creole and Guyanese CreoleDokumen18 halamanA Comparative Look at Jamaican Creole and Guyanese CreoleShivana Allen100% (3)
- Referensi Blok 15 16Dokumen2 halamanReferensi Blok 15 16Dela PutriBelum ada peringkat
- Fundamentals of Analytics in Practice /TITLEDokumen43 halamanFundamentals of Analytics in Practice /TITLEAcad ProgrammerBelum ada peringkat
- Untitled Document 3Dokumen10 halamanUntitled Document 3api-457501806Belum ada peringkat
- How Should Management Be Structured British English StudentDokumen7 halamanHow Should Management Be Structured British English Studentr i s uBelum ada peringkat
- TOTAL Income: POSSTORE JERTEH - Account For 2021 Start Date 8/1/2021 End Date 8/31/2021Dokumen9 halamanTOTAL Income: POSSTORE JERTEH - Account For 2021 Start Date 8/1/2021 End Date 8/31/2021Alice NguBelum ada peringkat
- Life of a VoyageurDokumen8 halamanLife of a VoyageurBruce GuthrieBelum ada peringkat
- Aditya Birla - FATCA and CRS - UBO - NON INDIVIDUALS PDFDokumen2 halamanAditya Birla - FATCA and CRS - UBO - NON INDIVIDUALS PDFHoaccounts AuBelum ada peringkat
- 1 Minute Witness PDFDokumen8 halaman1 Minute Witness PDFMark Aldwin LopezBelum ada peringkat
- Credit Suisse AI ResearchDokumen38 halamanCredit Suisse AI ResearchGianca DevinaBelum ada peringkat
- Eng 188 Change in Ap, Ae, and ErrorsDokumen5 halamanEng 188 Change in Ap, Ae, and Errorsmkrisnaharq99Belum ada peringkat
- Eng9 - Q3 - M4 - W4 - Interpret The Message Conveyed in A Poster - V5Dokumen19 halamanEng9 - Q3 - M4 - W4 - Interpret The Message Conveyed in A Poster - V5FITZ100% (1)
- Good Paper On Time SerisDokumen15 halamanGood Paper On Time SerisNamdev UpadhyayBelum ada peringkat
- Master ListDokumen26 halamanMaster ListNikhil BansalBelum ada peringkat
- Glowing Stones in Ancient LoreDokumen16 halamanGlowing Stones in Ancient LorerippvannBelum ada peringkat
- Work, Energy and Power: Checkpoint 1 (p.194)Dokumen12 halamanWork, Energy and Power: Checkpoint 1 (p.194)U KILLED MY DOGBelum ada peringkat
- How to use fireworks displays at Indian weddings to create magical memoriesDokumen3 halamanHow to use fireworks displays at Indian weddings to create magical memoriesChitra NarayananBelum ada peringkat
- Pharmacology of GingerDokumen24 halamanPharmacology of GingerArkene LevyBelum ada peringkat
- Sikkim Public Works Liability of Government and Contractor Act 1983Dokumen11 halamanSikkim Public Works Liability of Government and Contractor Act 1983Latest Laws TeamBelum ada peringkat