Nejmoa0707992 en Id
Diunggah oleh
Muhammad NazriJudul Asli
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Nejmoa0707992 en Id
Diunggah oleh
Muhammad NazriHak Cipta:
Format Tersedia
th e engl baru dan jurnal dari obat
artikel asli
Ventilasi noninvasif Akut kardiogenik
paru Edema
Alasdair Gray, MD, Steve Goodacre, Ph.D., David E. Newby, MD, Moyra Masson,
M.Sc., Fiona Sampson, M.Sc., dan Jon Nicholl, M.Sc.,
untuk Trialists 3CPO *
Abstrak
Latar Belakang
Dari Royal Infirmary of Edinburgh, Edinburgh (AG, ventilasi noninvasif (continuous positive airway pressure [CPAP] atau non-invasif ventilasi intermiten
MM), University of Sheffield, Sheffield (SG, FS, JN),
tekanan positif [NIPPV]) tampaknya manfaat dalam pengobatan segera pasien dengan akut edema paru
dan University of Edinburgh, Edinburgh (DEN) -
semua di Inggris. Permintaan alamat cetak ulang Dr
kardiogenik dan dapat mengurangi angka kematian. Kami melakukan penelitian untuk menentukan apakah
Gray di Departemen of Emergency Medicine, Royal ventilasi noninvasif mengurangi angka kematian dan apakah ada perbedaan penting dalam hasil associ-
Infirmary of Edinburgh, Little France, Edinburgh
diciptakan dengan metode pengobatan (CPAP atau NIPPV).
EH16 4SA, Inggris Raya, atau
alasdair.gray@luht.scot.nhs.uk.
metode
Dalam multicenter, terbuka, prospektif, acak, terkontrol, pasien ditugaskan untuk terapi oksigen standar,
* Para peserta di Tiga Intervensi di kardiogenik paru
Edema (3CPO) trial tercantum dalam Lampiran.
CPAP (5 sampai 15 cm air), atau NIPPV (tekanan inspirasi, 8 sampai 20 cm air, tekanan ekspirasi, 4
sampai 10 cm air). Titik akhir primer untuk perbandingan antara ventilasi noninvasif dan terapi oksigen
standar adalah kematian dalam waktu 7 hari setelah memulai pengobatan, dan titik akhir utama untuk
N Engl J Med 2008; 359: 142-51.
Copyright © 2008 Massachusetts Medical Society.
perbandingan antara NIPPV dan CPAP adalah kematian atau intubasi dalam waktu 7 hari.
hasil
Sebanyak 1069 pasien (rerata [± SD] usia, 77,7 ± 9,7 tahun; kelamin perempuan, 56,9%) yang sebagai-
menandatangani kontrak dengan terapi standar oksigen (367 pasien), CPAP (346 pasien), atau NIPPV (356
pasien). Tidak ada perbedaan yang signifikan dalam angka kematian 7 hari antara pasien yang menerima
terapi standar oksigen (9,8%) dan mereka menjalani noninvasif venti- lation (9,5%, P = 0,87). Tidak ada
perbedaan yang signifikan dalam titik akhir gabungan dari kematian atau intubasi dalam waktu 7 hari antara
kedua kelompok pasien yang menjalani ventilasi noninvasif (11,7% untuk CPAP dan 11,1% untuk NIPPV, P =
0,81). Dibandingkan dengan terapi oksigen standar, ventilasi noninvasif dikaitkan dengan perbaikan rata-rata
lebih besar pada 1 jam setelah awal pengobatan di dyspnea pasien yang dilaporkan (pengobatan perbedaan,
0,7 pada skala analog visual mulai dari 1 sampai 10; 95% confidence interval [CI], 0,2-1,3; P = 0,008), denyut
jantung (perbedaan perlakuan, 4 denyut per menit; 95% CI, 1-6; P = 0,004), asidosis (perbedaan perlakuan, pH
0,03; 95% CI, 0,02-0,04; P <0,001), dan (perbedaan perlakuan, 0,7 kPa [5,2 mm Hg]; 95% CI, 0,4-0,9; P
<0,001) hiperkapnia. Tidak ada kejadian ayat ad- terkait pengobatan.
kesimpulan
Pada pasien dengan akut edema paru kardiogenik, ventilasi noninvasif menginduksi peningkatan lebih cepat
dalam gangguan pernapasan dan gangguan metabolisme daripada terapi oksigen standar tetapi tidak
berpengaruh pada kematian jangka pendek. (Current Controlled nomor Trials, ISRCTN07448447.)
142 n engl j med 359; 2 www.nejm.org Juli 10, 2008
The New England Journal of Medicine
Download dari nejm.org pada 16 Maret, 2020. Untuk penggunaan pribadi saja. Tidak ada kegunaan lain tanpa izin.
Copyright © 2008 Massachusetts Medical Society. Seluruh hak cipta.
Ventilasi noninvasif Akut kardiogenik paru Edema
untuk menentukan apakah ventilasi noninvasif im- membuktikan
SEBUAH adalah keadaan darurat medis umum yang penting ac-
hingga 1 juta rumah sakit diskusi-admis- untukparu
edema kondisi akut per
kardiogenik lucu
tahun di Amerika Serikat. 1 Ini adalah penyebab utama rawat inap,
kelangsungan hidup dan apakah NIPPV lebih unggul CPAP.
ac- penghitungan untuk 6,5 juta hari di rumah sakit setiap tahun. 2
metode
kematian di rumah sakit dari akut kardiogenik pul- monary edema pasien
yaitu tinggi (10 sampai 20%), 3 terutama ketika berhubungan Pasien direkrut dari KASIH 26 darurat
dengan infark miokard akut. 4 departemen-departemen di kabupaten dan rumah sakit
Pasien yang tidak memiliki respon terhadap terapi awal sering daerah di Inggris antara Juli 2003 dan April 2007.
membutuhkan intubasi trakea dan ven- tilation, dengan potensi Penelitian dilakukan sesuai dengan Deklarasi Helsinki
terkait untuk kation komplikasi-. 5 metode noninvasif ventilasi dapat dan pedoman Clinical Practice Baik dari United Kingdom
menangkal intubasi trakea dengan meningkatkan asi oksigen, Medi- cal Penelitian Dewan, mematuhi UU Inggris data
Protection 1998, dan ap- dibuktikan dengan mittee
mengurangi kerja pernapasan, dan increas- ing cardiac output. 6-9 Dua
metode noninvasif umum melibatkan tekanan terus-menerus Skotlandia Sebuah Penelitian Etika Communication
positif airway (CPAP) atau non-invasif intermiten tekanan positif (02/0/074, UK).
ventilasi (NIPPV) disampaikan dengan menggunakan masker
wajah. CPAP mempertahankan dukungan tekanan yang sama Kriteria inklusi adalah usia lebih dari 16 tahun, diagnosis
positif-sepanjang siklus pernapasan, sedangkan NIPPV klinis akut edema paru kardiogenik, edema paru ditunjukkan
meningkatkan tekanan udara lebih selama inspirasi dari selama oleh rontgen dada, tingkat pernapasan lebih dari 20 kali per
ekspirasi. Seperti com- dikupas dengan CPAP, NIPPV menit, dan konsentrasi ion hydrogen arteri lebih besar dari
menghasilkan provements im- lebih besar dalam oksigenasi dan 45 nmol per liter (pH <7,35). Kriteria eksklusi adalah suatu
dioksida bersihan karbon dan penurunan lebih besar dalam ketentuan untuk menyelamatkan nyawa atau darurat
pekerjaan bernapas pada pasien dengan edema paru. 10 intervensi, seperti intervensi koroner perkutan primer;
ketidakmampuan untuk persetujuan memberi; atau
rekrutmen sebelumnya ke persidangan. Semua pasien
menerima terapi bersamaan standar untuk akut edema paru.
Studi klinis ventilasi noninvasif pada pasien dengan akut
kardiogenik edema paru termasuk seri kasus dan kecil, acak,
percobaan dikendalikan con-. Kebanyakan membandingkan CPAP Tergantung pada tingkat keparahan penyakit, di- dibentuk
atau NIPPV dengan terapi standar dan menyarankan bahwa tertulis atau menyaksikan persetujuan lisan dari pasien atau
ventilasi noninvasif meningkatkan gejala, fisiologis variabel- ables, persetujuan menyaksikan dari seorang kerabat diperoleh pada
dan tingkat ventilasi invasif. 11-14 Ulang cently diterbitkan ulasan masuk ke penelitian. Setiap kali KEMUNGKINAN ble, persetujuan
sistematis telah menyarankan kematian berkurang pada pasien tertulis atas partisipasi dalam persidangan diperoleh dari pasien
yang diobati dengan CPAP. 15-18 dalam berikutnya 7 hari.
Perbandingan CPAP dengan NIPPV mengungkapkan ada
perbedaan nifikan sig- antara dua intervensi, meskipun Desain studi
keuntungan fisiologis mendalilkan dari NIPPV. Satu Penelitian ini terbuka, acak, terkontrol, kelompok paralel
meta-analisis menyarankan lipatan di- di tingkat infark percobaan dengan tiga kelompok perlakuan: terapi oksigen
miokard akut pada pasien yang diobati dengan NIPPV. 16 standar, CPAP, dan NIPPV. tients Pa- secara acak
ditugaskan untuk salah satu dari tiga perawatan di rasio 1: 1
Untuk saat ini, semua acak, uji coba terkontrol kita kenal dengan penggunaan layanan telepon pengacakan 24- jam: 1.
telah kecil, dan sebagian besar telah con- menyalurkan di Urutan domization random itu bertingkat menurut pusat,
pusat-pusat tunggal. 15-18 Ada con variasi siderable dalam dengan panjang variabel blok.
populasi penelitian, jenis intervensi ventilasi, terapi
bersamaan, dan titik akhir percobaan. 16 Oleh karena itu, tidak
pasti apakah hasil ini baik digeneralisasikan atau kuat. Dalam Intervensi percobaan
terang ketidakpastian ini, kami melakukan, acak, percobaan CPAP dan NIPPV disampaikan melalui masker wajah penuh
terkontrol besar yang melibatkan pa- tients dengan akut oleh ventilator Respironics Sinkroni. Dukungan- plemental
kardiogenik edema paru oksigen disediakan pada tingkat hingga 15 liter per menit
dengan fraksi maksimum
n engl j med 359; 2 www.nejm.org Juli 10, 2008 143
The New England Journal of Medicine
Download dari nejm.org pada 16 Maret, 2020. Untuk penggunaan pribadi saja. Tidak ada kegunaan lain tanpa izin.
Copyright © 2008 Massachusetts Medical Society. Seluruh hak cipta.
th e engl baru dan jurnal dari obat
terinspirasi oksigen dari 0,6 untuk mempertahankan infark miokard. 19 Dua ahli jantung yang tidak menyadari
saturasi oksigen ripheral pe- atas 92%. CPAP dimulai tugas pengobatan dapat diklasifikasikan pasien sebagai
pada 5 cm air dan meningkat menjadi maksimal 15 cm memiliki infark miokard yang pasti, infark miokard
air. NIPPV dimulai pada tekanan udara positif inspirasi mungkin, infark miokard sible pos-, atau tidak ada infark
dari 8 cm air dan tekanan udara positif ekspirasi dari 4 miokard. kasus baru didiagnosis infark miokard
cm air dan meningkat menjadi tekanan inspirasi didefinisikan sebagai kasus infark miokard pasti atau
maksimal 20 cm air dan tekanan maksimum ekspirasi kemungkinan.
dari 10 cm air. Pasien yang diberikan terapi medis
standar yang diterima oksigen tambahan untuk
mempertahankan tions satura- di atas 92% melalui Analisis statistik
masker oksigen variabel-delivery dengan reservoir. Komite data dan pemantauan keamanan memastikan bahwa
Semua pasien menerima pengobatan mereka ditugaskan kriteria untuk terminasi dini karena baik khasiat (menurut garis
selama minimal 2 jam. penggunaan lebih lanjut dari Peto-Haybittle panduan-, dengan kriteria P <0,001) atau
CPAP, NIPPV, atau intubasi (ventilasi sive inva-) adalah merugikan (P <0,05) dari perlakuan tidak dipenuhi.
pada kebijaksanaan dari ing dokter memperlakukan.
Untuk memiliki peluang 80% untuk mendeteksi perbedaan
absolut dari 6% mortalitas (9% vs 15%) dengan menggunakan uji
dua sisi dengan tingkat signifikansi 0,05, kami membutuhkan 400
pasien ditugaskan untuk standar wajah terapi oksigen dan 800
Sidang ini dikoordinasikan dari Edinburgh dan didukung pasien ditugaskan untuk baik CPAP atau NIPPV. Dengan 400
oleh jaringan regional perawat penelitian dan dokter. Untuk tients pa- masing-masing di CPAP dan NIPPV kelompok,
memastikan kompetensi inti dalam penggunaan ventilator percobaan memiliki% kekuatan 80, dengan menggunakan uji dua
noninvasif, pelatihan disampaikan di berbagai tingkat, sisi dengan tingkat signifikansi 0,05, untuk mendeteksi perbedaan
termasuk perawat daerah re- pencarian, pemimpin situs, dan absolut dari sekitar 7% di titik akhir komposit (18% vs 11%) dan
produsen ventilator. dari ap- proxima 6% mortalitas (12% vs 6%).
Respon untuk Terapi Data dianalisis sesuai dengan prinsip tion-to-treat inten-.
analisis Ulangi gas darah arteri yang per- dibentuk 1 jam Analisis com- utama dikupas tingkat kematian 7 hari dalam
setelah perekrutan. denyut nadi, respi- tingkat ratory, setiap kelompok dengan menggunakan model regresi logistik
saturasi oksigen, dan noninvasively diukur tekanan darah dengan derajat kebebasan untuk perbedaan antara ketiga
dicatat pada 1 jam dan 2 jam. Para pasien melaporkan perlakuan didekomposisi menjadi dua atau- thogonal kontras
tingkat mereka dyspnea pada skala analog visual mulai dari dari terapi standar dibandingkan terapi non-invasif (CPAP
0 (tidak ada sesak napas) ke 10 (maksimal sesak napas) di atau NIPPV) dan CPAP dibandingkan NIPPV. kurva survival
rekrutmen dan pada 1 jam. Kaplan-Meier diplotkan untuk perbandingan yang sama, dan
kelangsungan hidup dibandingkan antara kelompok dengan
menggunakan uji log-rank. Tingkat mortalitas 30 hari, infark
hasil Tindakan miokard, intubasi dalam waktu 7 hari, masuk ke unit
Titik akhir primer untuk perbandingan antara usia ventilasi perawatan kritis (perawatan intensif atau koroner), dan titik
noninvasif (NIPPV atau CPAP) dan terapi oksigen standar akhir komposit kematian atau intubasi dibandingkan dengan
adalah kematian dalam waktu 7 hari setelah memulai penggunaan regresi logistik. Pada 1 jam setelah memulai
pengobatan. Titik akhir primer untuk perbandingan antara pengobatan, perubahan dalam skor dyspnea, physiologi-
NIPPV dan CPAP adalah gabungan kematian dalam waktu 7 variabel kal, dan nilai-nilai gas darah arteri dibandingkan
hari atau intubasi trakea dalam waktu 7 hari. Apriori sek- dengan penggunaan tes t. Sebuah dua sisi nilai P kurang dari
ondary titik akhir yang dyspnea, variabel fisiologis, intubasi 0,05 dianggap untuk menunjukkan signifikansi statistik.
dalam waktu 7 hari, lamanya hos- pital tinggal, masuk ke unit
perawatan kritis, dan kematian dalam waktu 30 hari.
infark miokard didefinisikan sesuai dengan 1971 regresi logistik digunakan untuk mengeksplorasi tindakan timbal
kriteria Dunia Kesehatan-lembaga yang lisasi dan kriteria balik antara efek pengobatan (non-invasif ven- tilatory dukungan vs
definisi yang universal terapi standar) dan keparahan
144 n engl j med 359; 2 www.nejm.org Juli 10, 2008
The New England Journal of Medicine
Download dari nejm.org pada 16 Maret, 2020. Untuk penggunaan pribadi saja. Tidak ada kegunaan lain tanpa izin.
Copyright © 2008 Massachusetts Medical Society. Seluruh hak cipta.
Ventilasi noninvasif Akut kardiogenik paru Edema
Tabel 1. Karakteristik dasar dari pasien. *
Pengobatan Oksigen standar CPAP (N NIPPV (N
Characterisic (N = 367) = 346) = 356)
Umur (tahun) 79 ± 9 78 ± 10 77 ± 10
Kelamin jantan (%) 42 45 43
Gejala infark miokard 22 22 22
pada presentasi (%)
penyakit jantung iskemik (%) 64 64 60
gagal jantung kongestif (%) 45 42 47
penyakit jantung katup (%) 12 11 9
penyakit paru obstruktif kronik (%) 19 15 21
Hipertensi (%) 56 55 57
Diabetes mellitus (%) 30 30 33
Hiperkolesterolemia (%) 30 33 31
merokok saat ini (%) 16 19 19
penyakit pembuluh darah perifer (%) 10 11 10
penyakit serebrovaskular (%) 18 17 16
denyut nadi (denyut / menit) 114 ± 24 113 ± 21 112 ± 22
Tekanan darah (mm Hg)
sistolik 161 ± 38 162 ± 35 161 ± 36
diastolik 87 ± 25 89 ± 23 87 ± 24
laju pernapasan (napas / menit) 33 ± 7 32 ± 7 32 ± 7
saturasi oksigen perifer (%) 91 ± 8 90 ± 8 90 ± 8
pH arteri 7.22 ± 0.08 7.21 ± 0.09 7.22 ± 0.09
PaO 2 ( kPa) 13,1 ± 7,6 13,5 ± 7,7 13,4 ± 8,6
PaCO 2 ( kPa) 7,6 ± 2,5 7,5 ± 1,9 7,7 ± 2,3
tingkat bikarbonat serum (mmol / liter) 21 ± 4 21 ± 4 21 ± 5
skor dyspnea † 8,9 ± 1,5 8,9 ± 1,8 8.8±1.6
* Plus–minus values are means ±SD. CPAP denotes continuous positive airway pressure, NIPPV noninvasive intermittent positive-pressure ventilation,
PaCO 2 partial pressure of arterial carbon dioxide, and PaO 2 partial pressure of arterial oxygen. To convert values for PaO 2 and PaCO 2 to mm Hg,
multiply by 7.50062.
† The patients reported their degree of dyspnea on a visual-analogue scale ranging from 0 (no breathlessness) to 10 (maximal breathlessness).
penyakit, yang didefinisikan menurut apriori terhadap baseline ment ke persidangan (lihat pendix Tambahan ap-, tersedia
arteri pH dan post hoc sesuai dengan tekanan darah sistolik. 20,21 dengan teks lengkap artikel ini di www.nejm.org). Tidak ada
analisis eksplorasi lebih lanjut meneliti interaksi antara efek ferences dif- signifikan dalam karakteristik awal antara ketiga
memperlakukan ment dan usia, jenis kelamin, ada atau tidak kelompok (Tabel 1). Para pasien yang lanjut usia (rata-rata [±
adanya gagal jantung sebelumnya, dan ada atau tidak adanya SD] usia, 77,7 ± 9,7 tahun) dan telah ditandai takikardia,
infark miokard akut. takipnea, hipertensi, asidosis, dan hiperkapnia. Sebagian
besar pasien (56,9%) adalah perempuan.
hasil
1842 pasien berpotensi memenuhi syarat, 1511 disaring dan 1156 Intervensi percobaan
pengacakan menjalani. Delapan puluh tujuh pasien dikeluarkan Pasien dan terapi bersamaan secara merata ditugaskan di
setelah isasi random karena tidak memenuhi syarat atau pengadaan seluruh kelompok intervensi (Tabel 2; lihat juga Lampiran
yang sebelumnya Tambahan). Meskipun
n engl j med 359; 2 www.nejm.org Juli 10, 2008 145
The New England Journal of Medicine
Downloaded from nejm.org on March 16, 2020. For personal use only. No other uses without permission.
Copyright © 2008 Massachusetts Medical Society. All rights reserved.
Th e new engl and journal o f medicine
Table 2. Treatment of Patients.*
Standard Oxygen
Treatment (N = CPAP (N NIPPV (N All Patients (N
Variable 367) = 346) = 356) = 1069) P Value†
Initial treatment — % of patients
Nitrates 93 88 91 90 0.11
Diuretics 90 89 89 89 0.89
Opioids 55 50 49 51 0.31
Inspired oxygen — liters/min 12±4 12±4 12±4 12±4 0.44
Ventilation pressure — cm of water — 10±4 Inspiratory 14±5, —
expiratory 7±3
Started assigned treatment — 365/366 (99.7) 337/343 (98.3) 344/354 (97.2) 1046/1063 (98.4) 0.02
no./total no. (%)‡
Completed assigned treatment — 298/363 (82.1) 285/340 (83.8) 267/352 (75.9) 850/1055 (80.6) 0.02
no./total no. (%)§
Changed to new treatment — no.
Intubation 3 1 4
CPAP 43 — 12
NIPPV 13 5 —
Standard treatment — 31 49
New treatment not stated 6 18 20
Reason for not completing assigned
treatment — no. (%)¶
Patient discomfort 1 (0.3) 18 (5.2) 30 (8.4) <0.001
Worsening arterial blood gas values 26 (7.1) 10 (2.9) 15 (4.2) 0.03
Respiratory distress 31 (8.4) 5 (1.4) 12 (3.4) <0.001
Other 18 (4.9) 24 (6.9) 29 (8.1) 0.21
* Plus–minus values are means ±SD. CPAP denotes continuous positive airway pressure, and NIPPV noninvasive intermittent positive-pres- sure ventilation.
† P values are for the comparison among the three groups. ‡ Data were
missing for six patients. § Data were missing for 14 patients.
¶ A patient may have had more than one reason for not completing the assigned treatment.
the overall completion rates were similar, stan- dard oxygen dence interval [CI], 0.63 to 1.48; P = 0.87) (Fig. 1 and Table 3).
therapy was associated with a great- er failure rate due to The 7-day mortality rate in nonre- cruited patients was 9.9%.
respiratory distress, whereas noninvasive ventilation, The rate of the primary composite end point of death or
especially NIPPV, was as- sociated with a higher rate of intubation with- in 7 days (Fig. 1 and Table 4) was similar for
noncompletion due to patient discomfort (Table 2). The mean the CPAP and the NIPPV groups (11.7% and 11.1%, re-
dura- tion of therapy was 2.2±1.5 hours for CPAP and spectively; odds ratio, 0.94; 95% CI, 0.59 to 1.51; P = 0.81).
2.0±1.3 hours for NIPPV.
There were no interactions between treatment effect and
Primary Outcomes severity of illness, as defined by either baseline arterial pH (P
There was no significant difference in the pri- mary end point = 0.94) or systolic blood pressure (P = 0.17). Further
of 7-day mortality between pa- tients receiving noninvasive exploratory subgroup analysis found no interactions between
ventilation (CPAP or NIPPV) (9.5%) and those receiving treatment effect and age (P = 0.52), sex (P = 0.33), presence
standard oxy- gen therapy (9.8%; odds ratio, 0.97; 95% or absence of a history of heart failure (P = 0.28),
confi-
146 n engl j med 359;2 www.nejm.org july 10, 2008
The New England Journal of Medicine
Downloaded from nejm.org on March 16, 2020. For personal use only. No other uses without permission.
Copyright © 2008 Massachusetts Medical Society. All rights reserved.
Noninvasive Ventilation in Acute Cardiogenic Pulmonary Edema
and presence or absence of myocardial infarction at
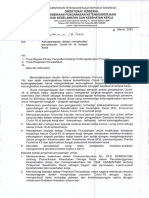
A
presentation (P = 0.93).
100
Secondary Outcomes
There was no significant difference in the 30-day mortality rate 95
between patients receiving standard oxygen therapy and those
Probability of Survival (%)
receiving noninvasive ventilation (16.4% and 15.2%,
90
respectively; odds ratio, 0.92; 95% CI, 0.64 to 1.31; P = 0.64) Noninvasive ventilation
(Table 3). Mortality rates were similar in the CPAP and the (CPAP or NIPPV)
NIPPV groups at 7 days (9.6% and 9.4%, respec- tively; odds 85
ratio, 0.97; P = 0.91) and at 30 days (15.4% and 15.1%, Standard oxygen therapy
respectively; odds ratio, 0.98; P = 0.92) (Table 4).
80
00
5 10 15 20 25 30
Noninvasive ventilation (CPAP or NIPPV) was associated Days
with greater reductions in dyspnea, heart rate, acidosis, and No. at Risk
hypercapnia than was standard oxygen therapy (Table 3). CPAP or NIPPV 667 609 591 583 577 570 567
Standard therapy 348 318 307 301 296 292 291
Patients receiv- ing standard oxygen therapy and those
receiving noninvasive ventilation had similar rates of tra-
cheal intubation, admission to the critical care unit, and B
myocardial infarction. Patients receiving CPAP and those 100
receiving NIPPV also had similar rates of these outcomes
(Table 4).
95
Probability of Survival (%)
Discussion 90
CPAP
Despite early improvements in symptoms and in surrogate
85 NIPPV
measures of disease severity, we found no difference in the
effect on short-term mortal- ity between standard oxygen
therapy and nonin- vasive ventilation. Furthermore, there 80
were no major differences in treatment efficacy or safety 00
5 10 15 20 25 30
between the two noninvasive ventilation treat- ments, CPAP
Days
and NIPPV.
No. at Risk
CPAP 325 298 288 285 282 277 275
Meta-analyses and systematic reviews of im- mediate NIPPV 342 311 303 298 295 293 292
treatment with noninvasive ventilation in patients with acute
Figure 1. Kaplan–Meier Survival Curves.
cardiogenic pulmonary ede- ma have reported a 47%
Panel A shows the comparison between noninvasive and standard oxygen therapy, and Panel
reduction in mortality. 15
B the comparison betweenAUTHOR:
continuousGray
positive
1
airway pressure (CPAP)
RETAKE
and noninvasive
1st
ICM
The Three Interventions in Cardiogenic Pulmonary Oedema intermittent positive-pressure ventilation (NIPPV). The values for 7-day survival2ndare marginally
REG F
FIGURE: of 1
(3CPO) trial was adequately powered to assess an effect of different from those reported as a primary outcome (Tables 3 and 4), because 3rd
data from
CASE Revised
patients who did not consent to follow-up or withdrew after 7 days are not included. Data were
this magnitude and recruited more patients than the total Line H/T 4-C
EMail SIZE
missing for two patients inARTIST:
the NIPPVtsgroup. Combo
number of patients included in these analyses and reviews. Enon
H/T 22p3
Although the 95% confidence intervals overlap with results
AUTHOR, PLEASE NOTE: Figure has been
from meta-analyses, the 3CPO trial showed no effect of redrawn and type has been reset.
Please check carefully.
treatment with noninvasive ventilation on mortality. istics and event rates were similar to those in previous
studies and indicate that we recruited patients with severe
JOB: 35902 ISSUE: 07-10-08
disease. There was no evi- dence of patient-selection bias,
Was the study population inappropriate? On the basis of since the 7-day mortality rates among nonrecruited patients
the results of previous studies, we ap- plied strict inclusion (9.9%) were virtually the same as those among patients who
and exclusion criteria and completed this large trial. The were recruited to the trial (9.6%). In keeping
baseline character-
n engl j med 359;2 www.nejm.org july 10, 2008 147
The New England Journal of Medicine
Downloaded from nejm.org on March 16, 2020. For personal use only. No other uses without permission.
Copyright © 2008 Massachusetts Medical Society. All rights reserved.
Th e new engl and journal o f medicine
Table 3. Primary and Secondary End Points for Patients Receiving Standard Oxygen Treatment and Those Receiving Noninvasive Ventilation
(CPAP or NIPPV).*
Standard Oxygen
Treatment (N CPAP or NIPPV Odds Ratio
Variable = 367) (N = 702) (95% CI) P Value
Death within 7 days (% of patients) 9.8 9.5 0.97 (0.63 to 1.48) 0.87
Death within 30 days (% of patients) 16.4 15.2 0.92 (0.64 to 1.31) 0.64
Intubation within 7 days (% of patients) 2.8 2.9 1.05 (0.49 to 2.27) 0.90
Admission to critical care unit (% of patients) 40.5 45.2 1.21 (0.93 to 1.57) 0.15
Myocardial infarction (% of patients)
WHO criteria 24.9 27.0 1.12 (0.84 to 1.49) 0.46
Universal criteria 50.5 51.9 1.06 (0.82 to 1.36) 0.66
Difference between
Means (95% CI)†
Mean length of hospital stay (days) 10.5 11.4 0.9 (−0.2 to 2.0) 0.10
Mean change at 1 hr after start of treatment‡
Dyspnea score§ 3.9 4.6 0.7 (0.2 to 1.3) 0.008
Pulse rate (beats/min) 13 16 4 (1 to 6) 0.004
Blood pressure (mm Hg)
Systolic 34 38 3 (−1 to 8) 0.17
Diastolic 22 22 0 (−3 to 3) 0.95
Respiratory rate (breaths/min) 7.1 7.2 0.2 (−0.8 to 1.1) 0.74
Peripheral oxygen saturation (%) 3.5 3.0 −0.4 (−1.4 to 0.6) 0.41
Arterial pH 0.08 0.11 0.03 (0.02 to 0.04) <0.001
Arterial PaO 2 ( kPa) 0.7 −0.6 −1.2 (−2.6 to 0.1) 0.07
Arterial PaCO 2 ( kPa) 0.8 1.5 0.7 (0.4 to 0.9) <0.001
Serum bicarbonate level (mmol/liter) 1.7 1.8 0.1 (−0.7 to 1.0) 0.77
* CI denotes confidence interval, CPAP continuous positive airway pressure, NIPPV noninvasive intermittent positive- pressure ventilation, PaCO 2 partial
pressure of arterial carbon dioxide, PaO 2 partial pressure of arterial oxygen, and WHO World Health Organization. To convert values for PaO 2 and
PaCO 2 to mm Hg, multiply by 7.50062. † The difference between means may not equal the difference between the two means for each category of
change be- cause of rounding.
‡ Positive values in the Standard Oxygen Treatment and CPAP or NIPPV columns represent improvement in the variable. § The patients reported their
degree of dyspnea on a visual-analogue scale ranging from 0 (no breathlessness) to 10 (maximal breathlessness).
with previous analyses, 16 there was no interaction between plied portable ventilator that allows both CPAP and NIPPV to
treatment effect and the severity of dis- ease, a result be used and is not affected by leaks around the face mask of
suggesting that the inclusion of those with milder disease did up to 50 liters per minute. Although we did not measure the
not obscure poten- tial benefits in the sickest patients. We concen- tration of inspired oxygen, the circuit delivers oxy-
therefore believe that we targeted and assessed the correct gen in concentrations of up to 60%. There was an apparent
patient population. drop in the partial pressure of arterial oxygen after treatment
with noninvasive ventila- tion at 1 hour, but the size of the
Was the intervention correctly delivered? More than 80% decrease was moderate and of questionable clinical
of the centers had experience with the use of noninvasive relevance. Indeed, in contrast to standard oxygen therapy,
ventilation before the start of the trial. There was a there were no treatment failures due to worsening hypoxia in
comprehensive training pro- gram for all centers to ensure the the noninvasive-ventilation groups. The mean pressures in
competence and consistency of the operators of the ventilation both the CPAP group (10 cm of
de- vices throughout the trial. We used a readily ap-
148 n engl j med 359;2 www.nejm.org july 10, 2008
The New England Journal of Medicine
Downloaded from nejm.org on March 16, 2020. For personal use only. No other uses without permission.
Copyright © 2008 Massachusetts Medical Society. All rights reserved.
Noninvasive Ventilation in Acute Cardiogenic Pulmonary Edema
Table 4. Primary and Secondary End Points for Patients Receiving CPAP and Those Receiving NIPPV.*
CPAP (N NIPPV (N Odds Ratio
Variable = 346) = 356) (95% CI) P Value
Death or intubation within 7 days 11.7 11.1 0.94 (0.59 to 1.51) 0.81
(% of patients)
Death within 7 days (% of patients) 9.6 9.4 0.97 (0.58 to 1.61) 0.91
Death within 30 days (% of patients) 15.4 15.1 0.98 (0.64 to 1.49) 0.92
Intubation within 7 days (% of patients) 2.4 3.5 1.48 (0.60 to 3.67) 0.40
Admission to critical care unit (% of pa- 44.5 45.8 1.06 (0.78 to 1.43) 0.73
tients)
Myocardial infarction (% of patients)
WHO criteria 27.2 26.8 0.98 (0.70 to 1.37) 0.90
Universal criteria 49.1 54.7 1.25 (0.93 to 1.69) 0.14
Difference between
Means (95% CI)†
Mean length of hospital stay (days) 11.3 11.5 0.2 (−1.1 to 1.5) 0.81
Mean change at 1 hr after start of
treatment‡
Dyspnea score§ 4.7 4.5 −0.2 (−0.8 to 0.4) 0.52
Pulse rate (beats/min) 17 15 −2 (−5 to 1) 0.26
Blood pressure (mm Hg)
Systolic 38 37 −1 (−6 to 5) 0.77
Diastolic 23 21 −2 (−6 to 2) 0.31
Respiratory rate (breaths/min) 7.3 7.1 −0.1 (−1.2 to 1.0) 0.82
Peripheral oxygen saturation (%) 3.5 2.6 −0.9 (−2.2 to 0.3) 0.14
Arterial pH 0.12 0.10 −0.01 (−0.02 to 0.00) 0.05
Arterial PaO 2 ( kPa) −1.1 0.0 1.2 (−0.5 to 2.8) 0.16
Arterial PaCO 2 ( kPa) 1.5 1.4 −0.1 (−0.3 to 0.2) 0.67
Serum bicarbonate level (mmol/liter) 2.3 1.3 −0.9 (−1.8 to 0.0) 0.04
* CI denotes confidence interval, CPAP continuous positive airway pressure, NIPPV noninvasive intermittent positive- pressure ventilation, PaCO 2 partial
pressure of arterial carbon dioxide, PaO 2 partial pressure of arterial oxygen, and WHO World Health Organization. To convert values for PaO 2 and
PaCO 2 to mm Hg, multiply by 7.50062. † The difference between means may not equal the difference between the two means for each category of
change be- cause of rounding.
‡ Positive values in the CPAP and NIPPV columns represent improvement in the variable. § The patients reported their degree of dyspnea on a
visual-analogue scale ranging from 0 (no breathlessness) to 10 (maximal breathlessness).
water) and the NIPPV group (inspiratory and ex- piratory fully and appropriately. We acknowledge that the improvement
pressures of 14 cm of water and 7 cm of water, respectively) in dyspnea (0.7 on a 10-point scale) was moderate, 24 but the
were similar to those in pre- vious studies. 15,16 visual-analogue scale used is a crude measure of dyspnea,
and noninvasive ventilation, when not associated with patient
Was the trial intervention ineffective? Irrespec- tive of the dis- comfort, was associated with fewer treatment failures due
method of treatment, noninvasive venti- lation produced a to respiratory distress than was the standard treatment.
greater reduction in respiratory distress and metabolic Finally, despite the theoreti- cal additional benefits of NIPPV
abnormalities. These find- ings are consistent with the as compared with CPAP, 10 we observed no differences in
majority of previous studies investigating the benefits of therapeutic efficacy between the two noninvasive-treatment
CPAP and NIPPV 11-14,22,23 and confirm that the therapeutic methods.
intervention in our trial was delivered success-
n engl j med 359;2 www.nejm.org july 10, 2008 149
The New England Journal of Medicine
Downloaded from nejm.org on March 16, 2020. For personal use only. No other uses without permission.
Copyright © 2008 Massachusetts Medical Society. All rights reserved.
Th e new engl and journal o f medicine
Were the meta-analyses wrong? Recent meta- analyses ship between the rate of myocardial infarction and treatment
and systemic reviews have included nu- merous randomized with either CPAP or NIPPV.
clinical trials. However, the individual trials had small Previous trials have indicated that the physio- logical
treatment groups that ranged from 9 to 65 patients, with improvement seen with noninvasive venti- lation results in a
recruitment rates of only 10 to 30% (as compared with the reduction in the rate of tracheal intubation. 11,12 Pooled data
62% of patients assigned to treatment in the 3CPO trial). In from the meta-analy- sis by Peter et al. suggest that six
the meta-analyses, the total number of outcome events was patients need to be treated with CPAP and seven with NIPPV
below the recommended threshold of 200, 25 which limits the to avert intubation and mechanical ventilation in one patient. 16 In
generalizabil- ity of their findings. There is concern about contrast, the 3CPO trial found no benefit of noninvasive
report- ing, publication, and recruitment bias in individ- ual ventilation in reducing the rate of intubation, a result that may
published studies that will be compounded by pooled reflect the relatively low intubation rates we observed. The
analyses. The discrepancy between the re- sults of our large, reasons for these low rates in our study are un- clear but may
randomized, controlled trial and previous pooled data is not be related to differences between our study and others in
unique, and the limi- tations of meta-analyses have been well patient populations, concomi- tant therapies, and thresholds
docu- mented. 26 for intubation and mechanical ventilation. Given that the
present and previous trials were by necessity open, there is
concern about treatment bias as a result of vari- ous
thresholds for intervention according to treat- ment allocation.
The mortality rate in our trial was higher than the rates For example, patients receiving standard oxygen therapy may
reported in registry data for patients with acute heart failure be more likely to undergo intubation than those already
(6.7% in the EuroHeart Failure Survey II 27 and 4% in the gaining the apparent benefit of noninvasive ventilation.
Acute Decompensated Heart Failure National Registry
[ADHERE] 28), and our participants were older than the
patients in those registries and were predominantly female.
These discrepancies in mortality and in patient characteristics
are likely to be related to differ- ences in the study In conclusion, noninvasive ventilatory support delivered by
populations. Acute heart fail- ure registries include all patients either CPAP or NIPPV safely provides earlier improvement
with decompen- sated heart failure rather than only those and resolution of dyspnea, respiratory distress, and metabolic
with severe pulmonary edema. Indeed, in the EuroHeart abnormalities than does standard oxygen therapy. However,
Failure registry, only 16% of the patients had a qualifying these effects do not result in improved rates of survival. We
diagnosis of acute pulmonary edema. recommend that noninvasive ventila- tion (CPAP or NIPPV)
be considered as adjunctive therapy in patients with acute
cardiogenic pulmo- nary edema who have severe respiratory
Mehta and colleagues prematurely terminated their trial distress or whose condition does not improve with phar-
comparing CPAP with NIPPV because of concerns about an macologic therapy.
increased rate of myocardial infarction in the NIPPV group. 29 A
subsequent study by Bellone et al. did not replicate this finding
Supported by a grant (01/43/01) from the Health Technology Assessment
and showed no effect of NIPPV on the rate of myo- cardial
Programme of the National Institute for Health Research.
infarction. 30 The systematic review by Peter et al. reported a
weak relationship between NIPPV and an increase in the rate No potential conf lict of interest relevant to this article was reported.
of myocardial infarc- tion. 16 This finding was largely the result
The views expressed are those of the authors and do not nec- essarily ref lect
of the weight given to the study by Mehta et al. in the pooled those of the United Kingdom National Health Service or the Department of
data. 26 The 3CPO trial showed no relation- Health.
We thank all emergency department staff who supported this trial by recruiting
patients and Dr. Nicholas Boon for his assis- tance with end-point adjudication.
Appendix
The participants in the 3CPO Trial were as follows (all in the United Kingdom): Trial management group — A. Gray (chief investigator),
D. Newby, C. Kelly, N. Douglas, M. Masson, Royal Infirmary of Edinburgh; S. Goodacre, Northern General Hospital, Sheffield, and University of Sheffield; J. Nicholl,
F. Sampson, K. Paulucy, Y. Oluboyede, K. Stevens, University of Sheffield; S. Crane, York Hospital;
M. Elliott, P. Plant, St. James University Hospital, Leeds; T. Hassan, Leeds General Infirmary. Regional research coordinators — Y. Meades, Leeds General
Infirmary; A. Saunderson, E. Mowat, Royal Infirmary of Edinburgh; V. Lawler, E. Gendall, H. Purvis, Frenchay Hospital, Bristol; E. Norwood, Crosshouse Hospital,
Kilmarnock; T. Woodrow, Z. Gall, Hope Hospital, Salford; C. Roberts, Royal Devon and Exeter Hospital, Exeter; D. Mill, Torbay Hospital, Torquay; J. Groves, J. Gilks,
G. Symmons, Birmingham Heartlands Hos- pital; Y. Whattam, James Cook University Hospital, Middlesbrough. Trial steering group — T. Coats (chair), Leicester
Royal Infirmary;
R. Davies, Oxford University; M. Elliott, St. James University Hospital, Leeds; S. Goodacre, Northern General Hospital, Sheffield, and
150 n engl j med 359;2 www.nejm.org july 10, 2008
The New England Journal of Medicine
Downloaded from nejm.org on March 16, 2020. For personal use only. No other uses without permission.
Copyright © 2008 Massachusetts Medical Society. All rights reserved.
Noninvasive Ventilation in Acute Cardiogenic Pulmonary Edema
University of Sheffield; A. Gray (chief investigator), D. Newby, M. Masson, Royal Infirmary of Edinburgh; T. McDonagh, Royal Bromp- ton Hospital, London; P. Hall,
Edinburgh. Data and safety monitoring committee — R. Prescott (chair), University of Edinburgh; A. Hargreaves, Falkirk and District Royal Infirmary, Falkirk; C.
Selby, Queen Margaret Hospital, Dunfermline; U. MacIntosh, Stirling Royal Infirmary. Recruiting sites and clinical leaders ( numbers of recruited patients in
parentheses) — Royal Infirmary of Edinburgh, A. Gray (161); Southern General Hospital, Glasgow, P. Munro (23); Ninewells Hospital, Dundee, N. Nichol (21);
Crosshouse Hospital, Kilmarnock, C. McGuffie (50); Hairmyres Hospital, Kilmarnock, J. Keaney (28); Northern General Hospital, Sheffield, S. Goodacre (136); York
Hospital, S. Crane (63); St. James University Hospital, Leeds, S. Bush (56); Leeds General Infirmary, T. Hassan (37); Barn- sley Hospital, J. Brenchley (54); Harrogate
Hospital, H. Law (19); Pinderfields Hospital, Wakefield, M. Shepherd (8); Frenchay Hospital, Bristol, J. Kendall (68); Royal United Hospital, Bath, D. Williamson (60);
Bristol Royal Infirmary, J. Benger (32); Royal Devon and Exeter Hospital, Exeter, G. Lloyd (39); Torbay Hospital, Torquay, S. Cope (31); Hope Hospital, Salford, C.
Gavin (29); Manchester Royal Infir- mary, J. Butler (28); Whiston Hospital, Prescot, F. Andrews (29); Wythenshawe Hospital, Manchester, D. Walter (21); Warrington
Hospital, M. Higgins (11); Birmingham Heartlands Hospital, A. Bleetman (19); Selly Oak Hospital, Birmingham, P. Doyle (30); James Cook University Hospital,
Middlesbrough, P. Dissmann (11); Princess Royal University Hospital, Farnborough, I. Stell (5).
References
1. Heart disease and stroke statistics — 11. Bersten AD, Holt AW, Vedig AE, Skow- come in patients hospitalized with acute heart failure.
2005 update. Dallas: American Heart As- sociation, ronski GA, Baggoley CJ. Treatment of se- vere JAMA 2006;296:2217-26.
2005. cardiogenic pulmonary edema with continuous 22. L’Her E, Duquesne F, Girou E, et al.
2. Felker GM, Adams KF Jr, Konstam positive airway pressure deliv- ered by face mask. N Noninvasive continuous positive airway pressure in
MA, O’Connor CM, Gheorghiade M. The problem of Engl J Med 1991; 325:1825-30. elderly cardiogenic pulmo- nary edema patients.
decompensated heart failure: nomenclature, Intensive Care Med 2004;30:882-8.
classification, and risk stratification. Am Heart J 12. Masip J, Betbesé AJ, Páez J, et al. Non-
2003;145: Suppl:S18-S25. invasive pressure support ventilation ver- sus 23. Crane SD, Elliott MW, Gilligan P, Rich-
conventional oxygen therapy in acute cardiogenic ards K, Gray AJ. Randomised controlled comparison
3. Girou E, Brun-Buisson C, Taillé S, Le- pulmonary oedema: a ran- domised trial. Lancet of continuous positive airways pressure, bilevel
maire F, Brochard L. Secular trends in nosocomial 2000;356:2126-32. non-invasive ventilation, and standard treatment in
infections and mortality as- sociated with noninvasive 13. Kelly CA, Newby DE, McDonagh TA, emergency de- partment patients with acute
ventilation in patients with exacerbation of COPD and et al. Randomised controlled trial of con- tinuous cardiogenic pulmonary oedema. Emerg Med J 2004;
pulmonary edema. JAMA 2003;290:2985- positive airway pressure and standard oxygen 21:155-61.
therapy in acute pulmo- nary oedema: effects on
91. Stevenson R, Ranjadayalan K, Wilkin- plasma brain na- triuretic peptide concentrations. Eur 24. Karras DJ, Sammon ME, Terregino
4. Heart J 2002;23:1379-86. CA, Lopez BL, Griswold SK, Arnold GK. Clinically
son P, Roberts R, Timmis AD. Short and long term meaningful changes in quanti- tative measures of
prognosis of acute myocardial infarction since 14. Nava S, Carbone G, DiBattista N, et al. asthma severity. Acad Emerg Med 2000;7:327-34.
introduction of throm- bolysis. BMJ 1993;307:349-53. Noninvasive ventilation in cardiogenic pulmonary
[Erratum, BMJ 1993;307:909.] edema: a multicenter random- ized trial. Am J Respir 25. Flather MD, Farkouh ME, Pogue JM,
Crit Care Med 2003;168:1432-7. Yusuf S. Strengths and limitations of meta-analysis:
5. British Thoracic Society Standards of larger studies may be more reliable. Control Clin
Care Committee. Non-invasive ventilation in acute 15. Masip J, Roque M, Sánchez B, Fernán- Trials 1997;18:568-
respiratory failure. Thorax 2002; 57:192-211. dez R, Subirana M, Expósito JA. Noninva- sive 79. LeLorier J, Grégoire G, Benhaddad A,
ventilation in acute cardiogenic pul- monary oedema: 26.
6. Katz JA, Marks JD. Inspiratory work systematic review and meta-analysis. JAMA Lapierre J, Derderian F. Discrepancies be- tween
with and without continuous positive air- way 2005;294:3124-30. meta-analyses and subsequent large randomised,
pressure in patients with acute respi- ratory failure. 16. Peter JV, Moran JL, Phillips-Hughes controlled trials. N Engl J Med 1997;337:536-42.
Anesthesiology 1985;63: 598-607. JK, Graham P, Bersten AD. Effect of non- invasive
positive pressure ventilation (NIPPV) on mortality in 27. Nieminen MS, Brutsaert D, Dickstein
7. Baratz DM, Westbrook PR, Shah PK, patients with acute cardiogenic pulmonary oedema: a K, et al. EuroHeart Failure Survey II (EHFS
Mohsenifar Z. Effect of nasal continuous positive meta-analysis. Lancet 2006;367:1155-63. II): a survey on hospitalized acute heart failure
airway pressure on cardiac out- put and oxygen patients: description of population. Eur Heart J
delivery in patients with congestive heart failure. 17. Agarwal R, Aggarwal AN, Gupta D, 2006;27:2725-36.
Chest 1992;102: 1397-401. Jindal SK. Non-invasive ventilation in acute 28. Adams KF Jr, Fonarow GC, Emerman
cardiogenic pulmonary oedema. Postgrad Med J CL, et al. Characteristics and outcomes of patients
8. Lenique F, Habis M, Lofaso F, Dubois- 2005;81:637-43. hospitalized for heart failure in the United States:
Randé JL, Harf A, Brochard L. Ventilatory and 18. Collins SP, Mielniczuk LM, Whitting- rationale, design, and preliminary observations from
hemodynamic effects of continuous positive airway ham HA, Boseley ME, Schramm DR, Stor- row AB. the first
pressure in left heart fail- ure. Am J Respir Crit Care The use of noninvasive ventila- tion in emergency 100,000 cases in the Acute Decompen- sated Heart
Med 1997; 155:500-5. department patients with acute cardiogenic Failure National Registry (ADHERE). Am Heart J
pulmonary edema: a systematic review. Ann Emerg 2005;149:209-16.
9. Naughton MT, Rahman MA, Hara K, Med 2006;48:260-9. 29. Mehta S, Jay GD, Woolard RH, et al.
Floras JS, Bradley TD. Effect of continu- ous positive Randomized, prospective trial of bilevel versus
airway pressure on intratho- racic and left ventricular 19. Thygesen K, Alpert JS, White HD. continuous positive airway pres- sure in acute
transmural pres- sures in patients with congestive Universal definition of myocardial infarc- tion. Eur pulmonary edema. Crit Care Med 1997;25:620-8.
heart failure. Circulation 1995;91:1725-31. Heart J 2007;28:2525-38.
20. Tavazzi L, Maggioni AP, Lucci D, et al. 30. Bellone A, Monari A, Cortellaro F,
10. Chadda K, Annane D, Hart N, Gajdos Nationwide survey on acute heart failure in Vettorello M, Arlati S, Coen D. Myocardial infarction
P, Raphaël JC, Lofaso F. Cardiac and re- spiratory cardiology ward services in Italy. Eur Heart J rate in acute pulmonary edema: noninvasive
effects of continuous positive airway pressure and 2006;27:1207-15. pressure support ventilation versus continuous
noninvasive ventila- tion in acute cardiac pulmonary 21. Gheorghiade M, Abraham WT, Albert positive airway pres- sure. Crit Care Med
edema. Crit Care Med 2002;30:2457-61. NM, et al. Systolic blood pressure at ad- mission, 2004;32:1860-5.
clinical characteristics, and out- Copyright © 2008 Massachusetts Medical Society.
n engl j med 359;2 www.nejm.org july 10, 2008 151
The New England Journal of Medicine
Downloaded from nejm.org on March 16, 2020. For personal use only. No other uses without permission.
Copyright © 2008 Massachusetts Medical Society. All rights reserved.
Anda mungkin juga menyukai
- Gudang Soal UKDIDokumen85 halamanGudang Soal UKDIMohammad Izza Naufal FikriBelum ada peringkat
- Dokumen - Tips - Buku Panduan p3k Ditempat Kerjapdf PDFDokumen17 halamanDokumen - Tips - Buku Panduan p3k Ditempat Kerjapdf PDFMuhammad NazriBelum ada peringkat
- Surat Keterangan Tugas-SpvDokumen1 halamanSurat Keterangan Tugas-SpvMuhammad NazriBelum ada peringkat
- Job Desk Satgas Covid 19 PDFDokumen3 halamanJob Desk Satgas Covid 19 PDFMuhammad Nazri100% (1)
- Cuci Tangan Dan Etika BatukDokumen1 halamanCuci Tangan Dan Etika BatukMuhammad NazriBelum ada peringkat
- SE Dirjen Binwasnaker COVID 19Dokumen2 halamanSE Dirjen Binwasnaker COVID 19Muhammad NazriBelum ada peringkat
- Stevina Army R.0009092Dokumen92 halamanStevina Army R.0009092Dhe La VegaBelum ada peringkat
- Laporan Bulan K3l-13a PDFDokumen1 halamanLaporan Bulan K3l-13a PDFFirlli HerdiansyahBelum ada peringkat
- Kumpulan Bahan Safety and Health Talk (FILEminimizer)Dokumen66 halamanKumpulan Bahan Safety and Health Talk (FILEminimizer)Renni Sipahutar50% (2)
- PDFDokumen20 halamanPDFMuhammad NazriBelum ada peringkat