Systemic Pathology
Diunggah oleh
goongdeng02Deskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
Systemic Pathology
Diunggah oleh
goongdeng02Hak Cipta:
Format Tersedia
PATHOLOGY NOTES
SYSTEMIC PATH
Note: This material is copyrigbted, All rights reserved,
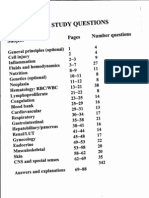
TABLE OF CONTENTS FOR SYSTEMIC PATHOLOGY NOTES
Subject
Hematology: RBC disorders Hematology:
Pages
1-11 11-14 15-18 19-26 27-31 32-77 78-97
Prepare db'Y Edwar dG OL,Jau, MD r
WBe
disorders
Hematology: Lymph node/ plasma cell Hematology: Coagulation disorders Hematology: Immunohematology Cardiova cular pathology Respiratory pathology Gastrointestinal pathology Hepatobiliarylpancreas pathology
98-117 118-134 13'5-154 155-176 177-203 204-223 224-238 239-263 264-266 267-269 270-271 272-276 277 1-48
c
Kidney/L UTMale pathology
Female/Breast pathology Endocrine pathology Musculoskeletal/Soft tissue pathology Skin pathology Central nervous system pathology
~atomy USMLE topic
Microbio}ogyiiUSMrJE topics 'Bioe emistry USMLE topics
Pbarruaco]og,'US1dLE
topics •
-TPbys'ologr USMLE topics,
Comprehensive pathology exam/answers
Note: llbis material
I copyrigbted.
AU rights reserved.
GOLJAN IDGH YIELD NOTES FOR USMLE STEP 1©
Note: This material is copyrighted. All rights reserved. No part of this publication may be reproduced in any Ierm or by any means, electronic or mechanical, including photncepy, recerdtng, 01' any information storage and retrieval system, without permission in writing from the publisher (Edward F. Goljan, M.D.)
Abbreviations commonly used: AD = autosomal dominant; AR = autosomal recessive, COD = cause of death. Dx = diagnosis Me = mast common, MCC = most cemmon cause, PaOz = partial pressure of oxygen in arterial) blood, PB = peripheral blood, Rx = treatment, SaQ2 = oxygen saturation of arterial blood, SXR = sex-linked recessive
Systemic Patholo_gy._
RB(:: di orders
l-
er.·pebera!lblood pJbtlll'ft ~ut1S1'¥JLE': 1. hypersegmeoted neutrophil- foiateIB12 deficiency 2. miCrocytic hypochromic cellsA. RBCs that have increased pallor call be assumed to be microcytic
t1),"~J -/51.
0'
B.
C. D.
Iron deficiency
anemia of chronic disease (ACD)
E.
3. 4.
thalassemia sideroblastic anemia
ickle cells- sickle cell anemia not trait have sickle cells in the peripheral blood target cellsA. bullseye
B. C.
5..
alcoholic liver disease
hemoglobinopathy spherocytea ....
DO
A.
central
area
of pallor'
'c.
6.
A.
B.
congenital spherocytoS1s ABO hemolytic disease of newborn myelofibrosis,
tear dropB. thalassemias
7.
8.
9.
10.
Howell Jolly body- spleen surgically removedor dysfunctional spleen as in HbSS'disease, platelet- small, red anueleate cell lymphocyte- black dot with a thin rim of oytoplasm Ane.r rod- myeloblast with immature nucleus and splinter-like structures in the c toplasm
11.
atypical lymphocytebig cell with abundant, sky blue cytoplasm B. infectious mono/CMV/toxoplas.mosis/'vitai hepatitle/phenytoln eosinophilA. large red granules that do nor cover the nucleus: samecolor as RBCs B. type I hypersensitivity C. invasive helminthic infections A.
12.
Note: Tbis material is cop)'righted. AU rights reserved.
13.
basophil-A. large purple granules tl:i:atdo cover the nucleus: granules 'darkerthan RBCs B. rnyeloprnlifsrative diseases
rouJealcl- REGs with stack ofcoins effect: increased sedlmentation rate ,schistocytes-
14. 15;
A.frtJ,gmented
B.
RBCseen
in microangioparhic hemolytic anemias
C.
16.
thrombotic thrombocytopenic. hemolytic Urem ic s mitome
purpura
D. DIe
B.
reticulocyteA. special supravital stain: thin filaments represent RNA
increased in: (1) hemolytic' anemias (2) 5-7 days-after brood loss,
17.
(3 after Rx of iron deficiency (4) Bt2/fola~c;! eficien ~ d HeinzbodiesA. special stain: large blue inclusions with involvement of the Me membrane
B. G,6PD deficiency coarse basophilic stippling-
18,
A. B.
lie 1.
routine stain: persistent ribosomes Phpo isoning pi'e1lUres oIl1USMLE;
mur(r
A. B.
megJ!lob~ti;c gI,af.F(f.W-
2. 3.
4. 5.
,~o
all the cells appear big due tID large, immature nuclei, e.g., giant band neutrophlls Bn/folate deficiency Jnl'elofibrosi&- marrow is composed of fibrous tis-sue; large cells represent megakaryocytes 3plasticAPe-m.ia- empty marrow with predominantly fat, and islandsef lymphocyres m;uJtipl-e mycl.olD.a- plasmablasts with bright blue cyroplssm.reccenrric nuclei perinuclear
_
,db ed sichwoblastA. B.
Prussian blue stain fat iron; ring ofblue around the nucleus of a normoblast indicate a defect in heme synthesis: sideroblastic anemias due to alcohol _ pyrido,. ine,
Pb poisoning e. Erytbropojesis: _ 1. definition. A. production dfRBCs in the bone-marrow B. dependent on erythropoietin (EFO) synthesized ,in the kidneys
GJ
2.
3.
stimull for EPOA~ low Pa02: hypoxemia B. anemia <7 gm/dl, C~ left shifted oxygen dissociation CUTve (ODC)' peripheral blood (PB} reticuJoc}-1esA. manifestation ofEBO stimulated marrow B. reticulccytes require 24 hours too become mature Ri3Cs C. reticulocytes have RNA filaments: identified with scpravitalstalns
Note: This material is copyrighted. All rights reserved.
retieulocyte count is the. most cost effective method of determining whether the marrow is responding appropriately to anel'l1ia:calle.rleffecttve erythropoiesis E .retieu.Iocyt:e count Is normally reported as R p-ercentage: normal 0.5-1.5 % F. rettculocyte eount is jjr~t corrected for the degree- of anemia (if present) with the following formula: .(1) corrected rerioulocyte count = (patient Hct 145) x reticulocyte .count, Where 45 D.
represents the normal Hct
example: patient'sHct = 15% Reticulocyte count = 9% Corrected count = (15/45 x 9%=3%) G. corrected count >3%" is considered a good response to-anemia: (1) blood loss >7 days (takes marrow -5-7 days to respond) (2)' hemolytic anemias (3) Rx of iron deficiency with iron (4) Rx of B Ii deficiency with B n (5) Rx of folate deficiency with folate a.correCted reticulccyte-eount <211/0 is considered a poor re ponse (something wrong in the bone marrow): (1 iron deficiency (2 anemia of chronic disease (ACD (3) B12/fula~e deficiency (4) aplastic anemia (9) blood loss <1 week (2)
3%
is
S-~gDB and symptoms of anemias:
1. 2. 3. 4. Bl1/folst~ defic-iency- glossitls Bn. deficiency- posterioreolumn/lateraf corticospinal tract signs exercise intolerance dyspnea higb output failure- decreased viscosit of blood Jowers total peripheral resistance koilonychle (spoon Dails)~j,roD deficiency
5.
6.
..-.. t::
o E E o
E o (.l.
in
~ e: ~
d
!oJ
~ ._
= e
.I0;.1
.... ~
"t:I
COl
_,
(J 0;.1:
::l
"CI
=
'''; 'In
U 0
1: ....
,s
Note: This material
is copyrighted.
All rights reserved.
Microcytic anemias:
r:Ifr
see Tables/schematics
Iron studies: 500 400 Iron 300 200 100
...
A 1.
2.
3. 4.
serum iroDA. bar A represents the normal B. area in black is iron bound 'to transferrin: arrow with solid line C. height of the baris the-transferrin level: arrow with interrupted line D. iron concentration is determined by .stripplng it off of the traasferrtn molecules with. acid: iron in bar A = 100 TmC is measured by adding iron to the patient specimen in order to fill up all available biqding sites on transferrin A. iron bound to all the transferrin sites is then measured: nBC in bar A= 300 B. there is an inverse relationship of transferrin with ferritin store in the bone marrow (1) decreased ferritin-stores, increases liver synthesis of transferrin: increases TmC (2 increased ferritin stores, decreases liver synthesis of'transferrin: decreases TIBe: % saturation is a calculation: % saturation of Iron= 'ironITIBC x 100 = 100/300 x 100
5.
6.
S(~h~(e... (0 rJ 'SjfU k A ferritin (storage form of iron) is found in all tissues (particularly in hepatocytes) and in rnaerophages (Largest amount) in the spleen/bone marrov : there is a very small-amount of circulating ferritin that closely correlates with the amount of storage iron thatis available for Hb synthesis B. ferritin is low in iron deficiency, nigh in ACD, and high in iron overload disease iron deficiency- bar B A. serum iron lew: -20 B. TIBC high: -500 (iron stores are decreased) C. % saturation low: 4% anemia of chronic diSease- bar C A. serum iron low: -20
33% serum ferritin-
*'
be ~ +;
1_
f.
;=
B.
C. D.
TIBe
low: -200 (iron stores are increased in ACD)
% saturation [0\\': 20% serum ferritin is high
=:
e
til
CIl
\1 ...
= ~
.:! til
~ =
~ ~ ~
.Ii::
....
.~ ..... = ca
J::
(,.!
'";>...
.C:
~=
~.=
..,
E .~
...
ii;
c
Cl .Q
S 0 ....
<II
E:.
..c J:!
V
= ;g
G
~ ~ ~
e 0
I
Co
.:
'I:
C 0
..::
1::1 0
= E
~
r.I
c:
c ....
E--
= .. e
z
...
~
"::1
~ ~
.lIl -
e =::
m
COl
...:"G
~~
t:; ~.
-< = c
c C
...... (j
""'~
=::~ eLi
III :::l ""l ~ "'CD ::l s:2 • 0 Ii) ~ II'l * -e a.;r ~. a ..... !. ~~ ~ = :i" ::I 2: ~ ~\ Q '1 e, I .., ,. :::r 0~. '* ~. n ell ~ In E!!, ~ 03 III ;l> IT! I »III :::I II'l III ~ .., -< Q. :::I _;1 0' Q 0 a. ::r' n 0 ::::I
~~
0'" "'0'
~.
li>
• ::::1' £C _.1' i' 00 til ::::I .... <
o
,.
I
In
!'I)
g. ~
=
ell
(I) (Il
Q:I :;:!
("l
=
£C
;.
Sf.
:::l
-e ('II .....
('II
..:
"tJ
In
...
ClI
(11
f.J'Q
t:J 0 _,.
..
:::I
l!-
0'
a ;;
s. r
g ..,.
0O'Q
.,
CD
~.
8.... jii'
0 0 ....,.,
.;:1
6' g :> :I CD·
:::l
I ;0:In
~
... COl
C1 ...
.'
-=0 I»
I
•
I
In
Ci)
Ci)
~In
.., 7k
* > =il
.:I 0
..,
=
II'l
III
= _. ~
... .Q Q r.:
IlII Q.. I»
• Q'5; •
a
I
0 <:
...
('II.
.0..
1». ("l
.,
:::I O'IJQ ~ :I
..j"'I
.., m
tI>
('II
1; l?
... 8..
st
E. ;. ; !.
;'
1/
Note: This material is copyrighted. All rights reserved.
7.
iron overload diSe-ases- bar D
A. examples: (l)sideroblasticanemias: Ph poisoning i5
(2)hemocbroma';Ps
B. C. D. E. c:Jr
(3) hemosiderosis serum iron high: -200 TIBe low: -200 (iron stores are high}: note how the % saturation high: 100% serum ferritin is high
serum iron
and nBC are the same
U ~lL scenados: 1. PICA far cia)' and Ice-iron deficiency 2. :2 feu!' old with 94.0/6 litbE';=...
A.
B. C D. E. F.
r:ir
hereditary persistence of Hgb F (variant of j3-tha!assemia) absent j3 and S chain synthesis with a ccnccmirant increase in Hgh F (c:x. and synthesis} HbA and HbAl are absent high HbF pre entscllnical symptoms of thalassemia uniform distribution ofHbF in all RBCs compatible with life
r chain
Differential features of the microcytic anemias: balded areas represent key differentia! points Fe deficiency ACD 0;, J3~,ThaJ minoJ' Slderoblasfic (pb poison)
MCV
me
Serum iron
Low Low
Low
Low
Low Low Low
High
Low Normal Normal
Low High
% Saturation Serum ferritin
RDW RBC count RBC FEP Hb electro.
Low
High High
Low
High Low
jo
Normal
Normal Normal
High
Normal
High
Normal
Absent
Ferritin best
Low High Normal
Normal
Low Higb (Pb peison) Normal
High Normal
cx:-thal: normal ~·-tbal: tHb Al and F Normal Bb electro. gold standard
Marrow
iron
High
Higb
Miscellaneous
Coarse basophilic stippling ringed
FEP = free erythrocyteprotoporphyrin, MCV = mean corpuscular volume TIDe capacity, RDW = red blood cell distribution width
= total iron binding
sideroblasts
Macrocytic anemias: see Nutrition notes see Tables and schematic
r::ir
Sites for reabsorption or iron. folate, Bu: 1. duodenum- iron A. Billroth IT (distal .stomach to jejunum, duodenum blind loop) associated with iron 2.
deficiency B. malabsorption jejuBu.m- folate A. malabsorption syndromes decrease iron reabsorption: e.g. celiac disease syndromes decrease reabsorption
.:ill
:l.
.!!
c.
:f
~
,.
~ ~
"S
.!
.9".-... ,Col s=
Ji
U
-< e
v'J
~ Q
~<S
'>
~
s:
-= S
~
._
:!I =
c c ::
e.
g ,.S
g ....
'to
.,
.~
Gil
.. - • .f R = e - ~.E -5 .s
'
<II
'lIJ
t:(
'~
~.
._!:
e ,2 ~
G:i.;
c;: ... 'C;; 0
0 ..Q
q;I
Q...:=
"D e. ·e -g 'z ·e c:.. c '" •
I
!l ","0
t~
CQ:U' -a >. >. 6-+ _e<Q'""'i' >. c. JiG· 'g < e,
CI;!
c:
>..
.~ 07
tJ
III
1$
::l II>
c:: I~
~
II
t,,;
to
t:i
r.
-41
~ .i ~
;.. I.::
<I:! -(
~ ~ tI ~ ,IQ
«'II
to
Note: This Material is copyright.ed. All rlghts reserved,
B.
birth control pills and alcohol decreases moneglutarnate reabsorption Crohn's disease/resection oftenninal ileum decreases reabsorption also decrease in bile salt reabsorption-e malabsorption
3.
Bll- terminal ile1:1JD
A. B.
Vitamin BlI (cobalamin) and folate: 1. sources ofB12A. meat/dairy products B. not present in vegetables/fruits 2. sources of folateA. beer: cannot become folate deficient by drinking too much beer B. fruits/vegetables C. grains 3. functions of both folate and BIZ- DNA synthesis 4. functions ofBa onlyA. propionate metabelisrn: propionyl-Cox-» methylmalonyl-CoA BI:!--t succinyl-Cc/, B. suceinyl CoA used in: (1) TCA cycle as a substrate for gluconeogenesis (2) heme synthesis 5. function of folate only- l-carbon transfers to other intermediates for the synthesis of: A. amino acids B. purines c. pyrimidines
6.
BI!! metabolism-
A. B.
Bn requires intrinsic factor (IF) for reabsorption in the terminal ileum: IF is synthesized in parietal cells located in the body/fundus Bn is initially bound to R factor in saliva: R factor pre-vents gastric acid destruction of
Bll
pancreatic enzymes cleave offR factor: this allows Ell to bind to IF D. BIl-IF complex is reabsorbed in the terminal ileum E. Bt2 is bound to,transcobalamin in the plasma: delivered to metabolically active cells.or stored in the liver (6~9 y supply) folate metabolismA. folate is in a polyglutarnate form in vegetableszgrains-» (1) converted into moneglutarnates in 01 by intestinal conjugase: enzyme LS, inhibited by phenytoin-e (2) monoglutamate is reabsorbed in jejunum: reabsorption blocked by alcohol and birth control pills ...:,;' (3) folate circulates in blood. as methyhetrahydrcfblare B. 3--4 mths supply of folate in liver: dietary deficiency common in alcoholics Bu/folate in DNA synthesis (see schematic)A. Bl~ removes methyl group from methyltetrahydrofolare (1) methyl transferred to homocysteine: homocysteine converted into mcthicnine (2) rnethyltetrahydrofolate becomes tetrahydrofelare (THJ1) (3) THF converted into N5,IO_ methylenetetrahydrofolate-e (4) NS,10-methylene THF + thymidylate synthetase + deoxyuridine monophosphate --4 dlliydrofolate (Dm) (5) DHF (oxidized form of THF) + deoxythymidine monephosphate (used for DNA syntheslsj-«
C.
7.
8.
Note: This material is copyrighted. All rjghts reserved.
9.
10.
11.
(6) OHF is converted by dibydrofolate reductase back into TIIF (reduced form) causes of B12 deficiencyA. pernicious anemia (P A): (1) MeC (2) autoimmune destruction of parietal cells (3) autoantibodies against IF and parietal cells (4) loss of IF leads to Bn deficiency (5) acblorhydria: increases serum gastrin levels (6) chronic atrophic gastritis of body/fundus: predisposition to gastric adenocarcinoma B. pure vegan diet C. chronic pancreatitis: cannot cleave offR factor D. fish tapeworm E. bacterial overgrowth in, sma11 bowel: (1) bacteria destroy Bi'e-IF complex (2) also destroy bile salts leading to malabsorption of fats F. terminal ileal disease (normal site for BlrlF reabsorption): e.g., Crohn's disease causes of folate deficiencyA. alcoholism: (1) MCC of folate deficieuey (2) notdeficient in folate in a beer drinking alcoholic B. poor diet: elderly C. pregnancy/lactaticn: uses up folate D. disseminated cancer: uses up folate E. phenytoin: blocks intestinal conjugase F. birth control pills/alcohol: block uptake of monoglutamatesin jejunum G. inhibition of dihydrofolate reductase: (1) methotrexate (2) trimethoprim SIS of Bl2/folate deficjcncy- .. A. macrocytic anemia: delayed nuclear maturation of hematopoietic cells B.gJossitis C. diarrhea: (1) malabsorption (2) affects duplication of stem cells in the intestine
12.
SIS unique to 1312 deficiencyA. B. subacute combined degeneration posterior column demyelination (1) lack proprioception (2) Lackvibratory sensation (3) positive Romberg's test lateral corticospinaltract demyelination (1) positive Babinski (2) upper motor neuron disease (3) spasticity dementia unique toPAach lorhydria chronic atrophic gastritis body/fundus
C.
D.
13.
SIS
A. B.
Note: This material is copyrighted. All rights reserved.
C.
1).
gastri.c adenocarcinoma
autoantibodies correctionof Shilling's test with addition ofIP
E.
14.
lab fludlngsln B.\llfolate deficiencyA. large nucleated cells with immature nuc lear features: cells are called megaloblastic
B.
C.
D.
pancytopenia: megaloblastic cells in the bone Ii11aJ:T0W are destroyed by macrophages before they enter the sinusoids hypersegmented neutrophils: (1) >5 nuclear lobes (2) excellent marker for Bnlfolate deficiency increased plasma homocysteine levels: no methyl group to transfer to homocysteine to produce methionine if either 13]2 or folate deficient
15.
16.
lab findings unique to folate deficiencyA. increased formirninoglutamic acid (FrGtu): usually metabolized by THF B. decreased serum folate C. decreased RBC folate: best test for folate deficiency lab findings unique to Bu deijcien.cyA. B. C. decreased serum BI2 increased urine methylmalonic ecid' build-up metbylmalonyl-CoA
proximal to the
block
increased propioaares (odd chained fatty acids) cause demyelination and CNS findings
17.
ScltiDing'B-testnon-radioactive BI2 is first given to bind to all available transcobalamin in the peripheral blood; (1) prevents any reabsorbed radioactive Bll from binding to transcobalamin (2) forces it to be excreted in the urine, B. radioactive BI2 given by mouth followed by 24-11 urine for % radioactive B12 reabsorbed: no radioactive Bil in 24-h urine confirms Bl2 deficiency. C. if corrected with addition of if to ora] radioactive B12: patient has pernicious anemia D. if corrected after antibiotic therapy: patient has bacterial overgrowth E. if corrected with addition of pancreatic extract followed by intake oral radioactive Bn: patient has chronic pancreatitis lb. of folate deficiency- folate in pharmacologic doses can correct B\l deficiency but not the neurologic abnormalities Rx ofBa deficiency- 1M B12 A.
18.
19.
,8
,Note: This material is copyrighted. AJI rights reserved.
Differential deficiency:
comparison
of pernicious
anemia (PA), other causes of anemia Other B12 deficiencies Increased Present' Present Present Absent
1311. deficiency and folate
Folate deficienc
Pernicious
MeV
Pancytopenia Hypersegmented neutrophils Megaloblastic bone marrow Autoantibodies against IF and parietal ceUs Chronic atrophic gastritis (body and fundus)
Increased
Increased
Present Present Present Absent Absent Absent
Present
Present Present Present Present Present Increased Increased Increased Increased Norma!
Absent Absent Normal
None Increased Increased Normal Present Not corrected byaddlng intrinsic factor
Achlo rby_dria
Serum. gastrin levels Risk of stomach adenocarcinoma Plasma bomocysteine Urine methylmalonie acid Urine forminoglutarnic acid (FiGLu) Neurological disease Schilling's test
Normal
None Increased
Normal
Inoreased None Not used
Present
Corrected by addiog intrinsic factor
Normocytic 1. 2. 3. 4. 5. 6.
anemias: see Tables ,r::tr M.LE cenmas; anemia since bjrth,splenOln~alyprobable congenital spherocytosis: do splenectomy cause of . neumoceceus infeCtion in HbSS- autcsplenectomy or functional asplenia Bowell Jolly ~-ody, indicates absent or dysfunctional. spleen primaquine---' often precipitates hemolysisin G6PD deficiency IPs11ent witb b.emolytiCl aDelDia p.ost dapsoD (sulfur drug, used in leprosy) and pirinG6Pl) deficiency pen rneril mear wit,h sickle cells in patient with osts_omyelitis: Salmonella species chart of mechanisms of hemolysis in the hemolytic anemias:
Summary
1.
extravasculsrA. macrophage removal and destruction of RBCs: (1) abnormally shaped RBCs (e.g., spherecytes sicklecells) (2) IgG and or 03 coating RBCs (e.g., autoimmune hemolytic anemia) increase in unconjugated bilirubin intravascular destruction ofRBCs RECs damaged by: (1) calcified aortic valve in aortic stenosis. (1vfCC) (2) fibrin clots in DIC (3) platelet thrombi in thrombotic thrombocytopenic syndrome
2.
B. intravascu]arA. B.
purpura and hemolytic uremic
.= ;9 ...... = 'iii ... e '" ~
V
~.
t =...... J:! II)
:c ~
V'\
"'"' "2 ~ t). .=
... ...
0
,_
V·
Q..
..-
!t;
'" VI
;J
9
ioo
Q
I1l
rn
cc n ~ ii ~ 00 g .9 ;;; CQ ~ co
l-
:I
!=
<ld
8
0
C.'_
ou
"'3
.r:
f
C,.I O;,l
t:: o·
."
r.u
::I
-I e
~..c
,01)
~:OO oa
~0
~ t::
E Q.l
0 z
.5 ~
b on
~
U~
.&:
"0
.$
~ ,... = ... u ~•
~Q -= ._ § .;: ._ :::I
-; e ~..., c::.~ ...... e O.S
II)
= "I:I.E =-c::;
II)
.! ~~
::E
II)
eli
-e
••
fJ:J .;;: ,.5 Q..c
I_
I-
:::l
I.J
II)
E
11,)
-=.
•
.... *.J;
CIS .~ ::
Q,I
== :i ~ C'O
CI
lii
U
'U U
.~
I
11"1
"I,. ii Q.G1 Col .. 0, I: :c ~ 0, U E ,.... Co. CI.I 0 10. -e Q,; ~ !-" .!i:: ~
.! ~~ rIl
-•
- - = ;= 5 -..., == =~. ... = -= =
.co
Q .G
10.
.,. -; ...
(II!
Q,l
- -~..e=
0, 0,
Jr=. ..
~ CJ
0,
."
.~
Ii!
.S
CII
..
10.
Q.
e
r
cd' .-
.t::
10. C!:I G1
E Q,l
(,j
.~ I:
~
CI.I
(II!
b e 1:1
70 .= E
.~
=•
~ E
G;J
C'1i5
<II~
Q) <II
l<;I
"
.~ ,..
0,
C!:I
.c
•••
=e= = -=
• = = • :.c
CIJ
=;
U
Ul
- 53
•
"d
.G
.....
....
C «J
«J <II
== ~ .- IU ~ •.J Q.td > v . E ,0 .£ .s
tI)
-,:)
0 IU
7i
• c..
<I'l
Note: This material is copyrighted. All rights reserved.
C. D. E.
haptoglobin levels decreAsed: haptoglobin blnds. to free Hb in plasma and is removed ~crophages
hemoglobinuria: often leads to iron .deficiency hernosiderinuria
Type of hemolvsis Extravascular
Anemia Congenital spherocytosis Con~n.ital elli_ptocytosis Sickle cell anemia/variants Glucose 6..phosphate dehydrogenase deficiency Autoimmune hemolytic anemia (warm IgG
Extravascular Extravascular (maj,or)~ intravascular (minor)
Intravascular (major) extravascular (minor)
Extravascu lar Intravascular Intravascular
_ty_E_e) Autoimmune hemolytic an-emia (cold IgM
ty2e)
Microsng_iopathic anemia QoestiD-,Q used during the board review:
CJr
C
W'
A J 9-year-old African American woman presents with fatigue and 'exercise intolerance. She has a history of menorrhagia, A eBC reveals a mild microcytic anemia, a low normal WEC count, and a, normal platelet count, A corrected reticulocyte count is <2%. WhiG:h of the following sets of lab oratory d_ best represen ts th e hemato Iozi fi di in ' ata ogle nn mgs III tlus pat lent? ent. % Saturation Serum Jrnn TIDe RBC Count Ferritin normal normal high normal A. normal low low high B. low low high low c. low low low D. high normal hj~ low h-!:g_h normal E. normal normal normal low A = thalassemia, B == AOD, D =: iron overload, E = blood loss
Which of the following characterizes
:,0
pemicicusenernia
rather than.
B12
deficiency from other
causes?
A.
Increased plasma homocysteine levels Increased urine methylmalonic acid c. Decreased vibratory sensation D. Hypersegmented neutrophils E. High serum gastrin levels E (other differences include achlorhydria, autoantibodies correction of Schillings test witb intrinsic factor)
B.
against intrinsic factor and parietal cells
rJr
the emergency room. Physical exam in the emergence room reveals a weak, thready pulse, cold clammy skin, and a 'blood pressure of 60J40 111m Hg. An open right femoral fracture is present as well as tenderness over the left lower ribs, Which of the following would you expect in this patient if a blood sample was draw:p prior to insertion of an IV Hoe with 0;9% normal saline? SELECT 3 A. Normal hemoglobin and hematocrit B. Nanna! effective arterial blood volume C, Increased central venous hydrostatic pressure D. Decreased mixed venous oxygen content E. Decreased pulmonary capillary wedge pressure
A 28-year~oJd man has a motorcycle accidentoutside
A,D,E
]0,
Note: Tbis material is copyrighted. All rights reserved.
i\
1Ja'/
~
J ..
,,' WBC disorders. see- Tables
o::i'"
'-I
A 4 year 'old African American child with sickle cell-anemia presents with a high fever and mrchal rig-idity. Scleral icterus and hepatosplenomegaly are pres-ent A aBC reveals a moderately severe normocytic anemia and a WBe count of 21,,000 CenS/IlL with left shit. A urinalysis is normal. A spinal tap reveals turbidity increased protein and neutrophils. You would expect a gram stain of CSF and a blood culture to reveal ... A. gram positive diplococci B. gram negative diplococci C. gram positive cocci D. gram positive rods E, gram negative coccobacilli A (Streptococcus pneumoniaes
)0
Test for infectious RBCs
mononucleosrs:
heterophileantibody,
which detects antibodies against horse
Classification of polycythemia: Causes/Discussion Subtype of Polycythemia
Absolute polycythemia:
Appropriate: stimulus of tissue hypoxia
Chronic obstructive pulmonary disease: 1.MCC in this category- low j PaOl High altitude residents: I.percentage of oxygen is 21%. but the atmespheric pressure is decreased- low PaOl syndrome): 1.rcsI!_iratory actdosts- low PaO,,Left shifted oxygen d'issociation curve: l.decreased release of oxygen to tissue- A. CO goisoning: (1) low SaOl. (2) normal Pa02_, B.
methemoglobinemia; (1) low Cyanotic eongenital heart disease: 1.l"ight to left shunt-low Hypoventilation syndromes (sleep apnea, Plckwiekiaa Pa02
sse, (l) normal
Pa02, C. increased Hb F
Absolute polycyth.emia: Inappropriate- no hypoxic ~titnulus
P-oiycy_themiarubra vera: normal PaOllSaOl and low erythropoietin Renal disorders: Linereased erytbropoietin- A. normal Pa02/Sa02, B, normal PaO:dSaOz, (1) renal adenocarcinoma/Wilrn's tumor, (2) cysts Endocrine disorders. Cushing s syndrome- cortisol and 17-ketosJew'ds, stimulate ery!hr()poiesi~ MiscelJa,neous: l.uterine leiomyomas- compression of ureters, 2. cerebellar 'Ileman.giobla.stoma- part of Von Hippel disease: increased incidence of renal adenocarcinoma, 3.hepatocellular carcinoma- ectopi
erythropoietin production SlQoker's polycythemia: unexplained effects of carbon monoxide in smoke increases RBC mass- nicotine decreases plasma volume by vasoconstriction Stress polycythemia (Gaisbock's syndrome): individuals under constant stress- typically males-with hypertension and obesity Volume depJetion: volume contraction hemoconcentrates RBes
Relative polycythemia:
due to decreased plasma volume, normal RBC
mass
11
;c;
~
Cl ,~
~,
J!. ~
J::>
=6
0 ~
I::
,0
FJ:
cQ
U ~
1
ei=
.!!!
0 '.:::I u
co:
.Q
s c: -e ti, U" '" ece 0 .:l = '0 a a. =
U)
:I
e =, - e .a "5 11 a'i
2::'
'-I CI :I Q
,~
...
•
~ r:: .-
._
0
I...
.b
III
::I
II)
.s "!I
'1£
c:I
'~
t::
.~
.5 u
'C
oS ,..
«I
,;>,
CII
.c
b
t;,)
::s '3 - .S -= In :E ~ :a }j
<II 0
;:l
-I
0Pl
=E
v
V'l
0 0
0 0
..l.
0
\}
1.0
Q;)
J I:
<If!
.Q
g.
CIj
"CI
-< S •
U 13 (.J
..
co e, ~ ....:J 'S ,13 ca e::I ;.; ::I ~ ..... ~ I: e 0 «I == '2 I: CI.'" Q. c:.;:: e= 0 ~ <I} Vl 1:1 co e 0 'j; ._. t) .S! J:; .!!! ~ .c; I: 0 till ';; ,9 c;: f;;il 0 0 <IJ Q._ 0 «I 0 rIl CIj r-- ~ .... «I ,E QJi ~~ A
!!
.!
c:
0
a)
<n
.c
J 10.0 C'II .0
'':
Q.
~=
.= •
=•
:a
... e '"
0 0 0 0
.!!
~ ~ t.I
0
1:1 I:ll
QJ
s o~
0 0 0
0-
~ .! ~ e
r::::
0.
QJ
;: .'t::
..:.:
U
(d
c;..
,a
I
Q t.I
0 .0
it ..c e .....
~ 5 4J
S
c:r
E U....:l ,_
Q
- B...c. l!
~
4J I:':
;]
loo~
III 0
;Z;
..=
Q
••
==
y
~~
cu
==
==..c o 0.
.~
E
"0 1:1
E cu ~
.~ .!!:
0
e VI ~E IS "; .~ 0 .5 .>. ._ ro Cl ~ ~ ~ 't:: ... c: c: c.o 0 ~ :::I ~ t.I 'C ::::I :> ..... C oj) 0..2 a; -~ <'CI ,.0 .... cu &, >'.2 00 ::l c:: -5 ;£ ; 0. ;;! I:': ~ it ... "C ro ... ro \t.l •::3 Vl 0 ::::l !I.I <'CI ~0 b c.. I, &S .,; .... ~ 0 VJ 0 ~ '2 ~ ~ 0 IlJ "" "0 ~::::: 0 ~ «l co' e .:; ; cu Il) ,_ 0 0 '" .1:: :is ~ e, E 10 8 0,"0 ~
·c ~ o til
t:: .~ ...
of
iii
.0
;:....
~+
Q)
1:1
II)
L,
a<8
- - .. .... .. a 5~
~QOl
I
e=
QI'}
'5
0
t)
";f. v ._
0 1::.
t)
.!:P
:::E
C
.el .el c :;s
0 0
'$..
0 1.0
"s • ~ ....... = g)) .,~ E =Q,J
J,;
--a
.1
'5 0
10
til
0> 0> III 0
.0
til oM'
.."
.~ ~
0.
.0 1 <Il 0 0 10
..!f !
"ii
0
:tI
"'0
-a :l.
<I)
CU Q
C 0
.!!:!
C
::0 .!! 0
.::I C.
CIl (1:1
~ 0
:::I
e ID
'
tIS
C,.)
.... ;,;
o:.l
0 I:
rn
z •
E I-
'0 u .0
:i .~
en
E :~ c 0;.) a 0 ... ~ ';:1 ,.s. 0 <Il ....
I
.0
a
I
-10;
t-1 .!!! ~ ~
_0
..
c..
~
,~
-~
-- 'B - =
cS ru .Q.l 0.. 'ti 0
!: ;I
Q.l
...
ID 0
.... ID .! 0 .::.:: ~~~~
a .9 ~ .!2 "S.
10:::; 0
0
a.l r.ll
==
"" = s
c.
.. = *, = C'lI
c:J
C,.)
,~
cc
.21
t)
0 0 .0
0 s,
c.. ~
I
In I<
~ E c..
.Q.l
5 ...
I ....
cE
= ....
0
!Il.
a _. 0 '0 a i l- 01) e o~ o;.! .fl. tIS e ~ ...... Q.l E .$
0
t:W
<.I
... ...c:::
0
""
Q.l
=
CIl
••
"'t:I
.~
= z :J; 0 ~
I:!:!
0 0
IS U l-
I co
1 1:1
r=
0
'ii
.CoiI
••
-•
••
':E
0 ~ *~ C
u/
0.
III ... 0 \0 "C
~ ~ = Ci '" E... E! d = .:! ~ = E "CI .:t. .!::! 'i.. e ~ .~Zl ~ ..... CI ,= ... .!S .t::! e, ~ = "; "CI a '(!j .... c.. is "1:1 c~ ~=>. - .! = ..~ CI = E c.o .E. .... "" = .c' .r.:. c '0 b E 0 1:1 .... ~ = ".C c: .'\.) ~ U .... = Ii .... '" _t..! .= rJ:l :S .... = ... U ~ l' !! c E ;:Q-E- E -e -< =: = ,til ~ C == :i .~ ~ -= '!i.e .! • ::E .... • = • ~ • • .= 0 • ~ • • • • • • • -=
.e.. ~.
c
'Q,I II)
t!" E ~ = ~ iii ....
...
II)
e - - ... .- ....
.-.!i!
'!C!
iI.)
-..c a E. 1::3 ~ 0E c Q •E ~. \C .... t\ Q. <Il.
;>
c..
!!!
.Col
I-
~ ~
1:1
C\l'
'i ....
CI 1:1
=
(II'
= .;
0.
.... '=i
c.
0 C'
Q,J
e
e:I
.(,1)
t .~
IQ,I
.. ,= .... =
~ E
Q CI:I 0 y
Q,J
iii
E .... e es
III
"C
e
<Il
0 .... ..,.
1:.1
Q
·s ....
.0
~
I
.! E
Q,J
~ = .~ c.. ..c c: e - ~a:.!!!! .= .: is
l1l:I
'.S! E Q,J
c:
= c. ~
Q,J
'0
....
Q,J
"S.
0:1 61:
III
I:)
0 II')
0;:
Q,
- - ..
Q,I
4)
C CI:I
1:1
Ii':
,:-. J! '; e .tt -=
1:1 II.!
Q.l (I:
""!)
iii
'5
Q.l
....
lUI
E <11 EE
<.I
:- ~
Q.l
0 I
e
Ill'
.~
t:W 0 Co
I-
Q,I
QJ
Ii)
;:l
..t::
Q,I
Q,I
Q,I
-Q Q.l
I;i'l'
= ii_ _.
Q
"" .s c...
t)
* -s
• Ii
1':1
IW
Cl)
."'.a.
0 '0
~~
O.
1:1
I::
CI:!. I- Q) U
.5 '" ~
(;,I
'
... J:'
e
'III
....
Q.l
.s
rl'Jl
-a
III
Ii. 1:.1
1:.1 """""
Oil
.;C
0:1
Q,I
C til
"t:I
I:)
lIS
Q,
C.
Col
etI
::i
_'.
E-o E Q;! .::c
s .!!
'= Q,I
=. ~
-e
Note: This material is copyrigbted. All rights reserved.
':ifF'
Differential Condition
diagnosis
of the polycythemia
disorders: Plasma
balded areas represent good differential Erytb ropoietin
RBe mass
PRY =:: polycythemia rubra vera, COPD congenital heart, disease
chronic
=::
cyanotic
--7
How to rccognize1eukemia and leukemia types: 1. acute vs chronicA. bone marrow exam.revealing >30% blast ceUs is acute leukemia tt:.~ __ ~ B. blast count not high in chronic 2. usual profile-A. anemia: usually normocytic B. thrombocytopenia: CI\tJL only leukemia that may have thrombocytosis C. high WEe count with blast cells: may be a normal count, but blast cells will be present D. generalized lymphadenopathy E. hepatosplenomegaly F. bone pain G. fever 3. use age brackets to pick out most- llkear choice--
A.
B. C.
<15 ALL
15-39 AML: look for Allier rod in myeloblast 40-60 AML and eML
D.
>60CLL
(1)
(2)
also MCC of generalized lymphadenopathy in the elderly also Me overall leukemia
tests in hematology: Comments Increased in congenital spherocytosis. Decreased In conditions with target cell (excess RBC membrane). Sugar water test/Ham/a test Sugar water test is the screen and Ham's test the confirmatory test for paroxysmal nocturnal hemoglobinuriaabsent decay accelerating factor. Hemoglobin electrop heres is Gold standard test for identifying an increase in norm 11I Hb (e.g,
Summary of'laboratory Laboratory Test Osmotic fragility
Hb A2 and F in j3-thalassemia) or "an increase in an abnormal Hb
Enzyme assays Serum iron (e.g., Hb SE, Hb SC). Confirmatory test in glucose 6-phosphate deJt)ldrogenase deficiencv in quiescent s1<.!gend pyruvate kinase deficiency. a Decreased in iron' deficiency and anemia of chronic inflammation (A CD}. Increased in sideroblastic anemias (e.g., lead p0isQnin;g) and iron overload conditions (e.g., hemosiderosis, hernochroma-
tosis) ..
12
Note: This material is copyrighted. AUrights reserved.
Total iron binding capacity (TIDe) Percent saturation of transferrtn Serum ferritin Iron stain
Correlates with transferrin levels. Increased in iron deficiencY'l Decreased in ACD and iron overload disease Decreased in iron deficiency and ACD. Increased in iron 'overload
states,
Decrease in irOTI deficiency, Increased in ACD and iron 'overload diseases. Prussian blue stain. Absent iron in iron deficiency. Increased 'iron in ACD, sideroblastic anemia (identifies the ringed sideroblast) and iron overload states. Increased in iron deficiency, ACD,and lead poisoning. Decreased in pyridoxine (B6)deficiencv. Decreased in Bll deficiency and increased in polycythemia rubra vera and chronicmyelogen0us leukemia Decreased in folate deficiency. Increased in folate deficiency. Increased in.B\2 deficiency. Increased in Bt2 and folate deficiency (MCC). Increased in any condition with RBC hemolysis (e.g., intravascular/extravascular hemolytic anemia, ineffective erythropoiesis in Bn/folate deficiency) or ith massive breakdown of cells (e.g. leukemia). Increased in extravascular hemolytic anemias (e.g. congenital spherocytosis, autoimmune hemolytic anemia). Decreased ill' intravascu lar hemolysis and severe extravascular hemolysis (Hb leaks out of phagocytosed RECs). Increased In chronic intrava scular hemolysis (e.g .. rnicroarrgiopathic hemo!xtic anemia, p_8rox:y_sma[ nocturnal hemoglebinuria), Solubility test and metabisulfite test. Positive ill Hb AS Hb SS, Hb SC. Hb S/thalassemia Bithermal antibody. Positive In paroxysmal cold hemoglobinuria Detect IgG, Ig1v1or C3 on the surface of RBCs (direct Coornbsjor detect IgG or IgM .antibodies Hl serum. (e.g . anti-D: indirect Coombs). Gold standard test for autoimmune hemolytic anemias. Positive in ABO and R11 hemolytic disease of the newborn. Supravital stain to identify RNA filaments in young RECs. Gold standard test to evaluate effective erythropoiesls, Increased> 3% in hemolytic anemias treatment phase of iron deficiency . En/folate deficiency and in blood loss> 7 days old. Increased in disorders that metastasize to the marrow (e.g., breast metastasis to' bonejor in primary diseases of the marrow that push reciculocytes out (e.g., acute/chronic leukemia). Decreased <2% in most of the microcytic anemias (excep ions: lead poisoning, severe tL and ~thalassemia), Bn and folate deficiency, aplastic anemia anemia of renal disease, blood loss < 5-7 days. Supravital stain to identify denatured Hb in RBCs secondary to peroxide damage in glucose 6-phosphate dehydrogeaase deficiency.
Free RBe protoporphyrin levels (FKP) . Serum Bu Serum folatelRBC folate Urine forminozlutarnic acid Urine methylmalunic acid Serum homocysteine Serum lactate dehydrogenase (LPB)
Unconjugated
bilirubin
Serum baptoglobin Urine hem.osiderin Sickle cell screen Douath-Landsteiner antibody Direct/Indirect Coombs test
Reticulocyte
count
Heinz body preparation
l3
Note: This material is copyrighted. All rights reserved.
Total iron binding capacity
(TmC)
Percent saturation of
transferrin
Serum ferritin Iron stain
Free RBC prctoporphyrin levels (FEP)_. Serum Bn.
Serum foiate/RBC folate Urine forminoalutarnic acid Urine methylmalonlc acid Serum homocysteine Serum Iacta e dehydrogenase (LDB)
Unconjugated bilirubin Serum haptoglobin Urine hemosiderin
Sickle cell screen
Direct/Indirect
Donath- Landsteiner antibody Coombs test'
Reticulocyte
count
Heinz body preparation
, Correlates .w·ith trans:t~rrin levels. II1~reased m iron de-ficiencY'l Decreased In ACD and Iran overload disease Decreased in iron deficiency and ACD. Increased in iron 'overload states. Decrease in iron deficiency. Increased in ACD and iron overload diseases. Prussian blue stain. Absent iron in iron deficiency, Increased 'iron in ACD, siderohlastic anemia (identifies the ringed sideroblast) and Iron overload states. Increased in iron deficiency, ACD, and lead poisoning. Decreased in pyridoxine (B6) deficiency. Decreased in Bll deficiency and increased in, polycythemia rubra vera and chronic myelogenous leukemia Decreased in folate deficiency. Increased in folate deficiency. Increased in Bl2 deficiency. Increased in B12 and folate deficiency (MCC). Increased in any condition with RBC hemolysis (e.g., intravascular/extravascular hemolytic .anemia, ineffective erythropoiesis in B12/folate deficiency) or with massive breakdown of cells (e.g., leukemia). Increased in -exteavascular hemolytic anemias (e.g .. congenital , spherocytosis, autoimmune hemol:ytic anemia). Decreased H1' intravascular hemolysis aad severe extravascular hemolysis (Hb leaks out of phagocytosed RBCs). Increased In chronic intravascular hemolysis (e.g .. microangiopathic hemolytic anemia,p_aroX)'_smal nocturnal hernogiobinuria). Solubility test and metabisulfite test. Positive in Hb AS Hb SS, Hb SC, Hb S/thalassemia Bithermal antibodv, Positive in paroxysmal oold hemoglobinuria Detect IgG, IglvI or C3 QD the surface of RBCs (direct Coornbsjor detect IgG or 19M antibodies H) serum (e.g, anti-D: indirect Coombs). Gold standard test for autoimmune hemolytic anemias. Positive in ABO and R11 hemolytic disease of the newborn. Supravital stain to identify RNA filaments in young RECs. Gold standard test to evaluate effecti.ve erythropoiesis, Increased> 3% in hemolytic anemias treatment phase of ir011 deficiency, B12{folate deficiency and in blood loss> 7 days old. Increased in disorders that metastasize to the marrow (e.g., breast metastasis to' bone) 01' in primary diseases of the marrow that push reeiculocytes out (e.g., .acute/chronic leukemia). Decreased <2% in most of the microcytic anemias (excep ions: lead poisoning, severe tL and ~thalassemia), Bu and folate deficiency, aplastic anemia anemia of renal disease, blood lOBS < 5-7 days. Supravital stain to identify denatured Hb in RBCs secondary to peroxide damage in glucose 6-phosphate dehydrogenase deficiency.
13
Note: This material is copyrighted. All rights reserved.
Leukocyte alkaline phosphatase (LAP) score Immunophenotyping of lywJ!bocvtes Tartrate resistant acid phosphatase(TRAP}_ stain
Stain ofneutrophilsand score based on the intensity of the stain. Marker of mature neutrophils, Increased ib benign neutrophil disorders but decreased in chronic myelogenous leukemia, Gold standard test to subclassify the type of cell involved in acute lymphoblastic leukemia. Key stain for identifying neoplastic B cells in hairy cell leukemia.
located on chromosome 22 in chronic myelogenous leukemia. Test to identify the unique heterophile antibody III infectious mononucleosis. Heterophile antibodies in mono are against horse RBCs (most sensitive antigen used in slide test), sheep RBCs, and bovine Mes. 1Mantibodies-do not react against guinea pig- kidney (GPK). Blood mixed with GPK does not clump, but when horse RBGs added it does clump. Anti viral capsid antigen-Iglvl and 19G, anti early antigen, anti Epstein-Barr nuclear antigen in the evaluation of heterophile antibody negative infectious mononucleosis. t(9;22)
Phlladelphia chromosome
Heterophile aatibody test
Epstein-Barr
body titer
QDc.stio'hsued duringtlie Board review: A febrile 23 year old college coed presents with fatigue and difficulty with swallowing, Physical exam reveals exudative tonsillitis palatal petechia, cervical lymphadenopathy, and tender
hepatosplenomegaly. A esc reveals a mild microcytic anemia lymphocytic leukocytosis with 20%. of the lymphocytes exhibiting atypical. features, and a mild thrombocytopenia, YOIl would
expect this patient to have. ,, A. a low nBC B. a normal serum ferritin C. an ele ated total' bilirubin D. heterophile antibodies E. normal serum AST and AL T titers
D
r:rr
A 6S·year-old man with an elevated RBC count has a history of gout, frequent headaches. and pruritus after bathing. He pre-sents with a sudden onset of abdominal pain and bloody diarrhea, WI1JCh Q,f [le f.011' . 1 ...1S nati oWIng sets 0 flab oratory d ata b est r6Q_reseotthis j)_attent s hematologic disease? Erythropoietin RBC Mass Plasma Volume 5a02 Decreased Increased Increased Normal A. Normal Normal Increased B. Increased Increased C. ' Increased Normal Low Decreased Normal Normal D. Normal Sa02 "" oxygen saturation C A = COPD, cyanotic GHD, B = ectopic EPO production, D = relative polycythemia (volume depleted)
I I
14
Note: This materia] is copyrighted. All rights reserved. Il ~'J.-. - 53 ._j""l_ Va { ~ .... "T Lympb nodesIPlasqla cellslHistiocytes/Spleen
Reactive lymphadenopathy: I d 1crf,::.5 ; (Iff''+; of' I /JoT IM61VIAe..'j I. ·clinica1~lntlljf 'f Pi (t.e ',ftrltb)l~n ) A. pa infu! lymph node __-?1 B. localized ill localized disease: e.g., tonsillitis C. generalized in systemic disease: e.g., HJV, infectious mono 2. lymph node relationshipsA. germinal follicle contains B cells: absent in Bruton's agammaglobulinemia: also no plasma cells B. parafollicular area contains T cells; absent in DiGeorge syndrome
C.
sinus contains histocytes
(1) (2) (3) increased histiocytes in histiocytosis X sinus histiocytosis in nodes draining cancer histiocytes are CDl positive
Malignancy: J. clinicaJ-
A.*painJe~s hard lymph nodes B. Localized in localized disease: e.g., axillary nodes in breast cancer
C.
generalized in:
(1)
(2)
leukemia
non-Hodgkin's lymphoma in adults of t14;18
Follicular B cell lymphoma: 1. Me malignant lymphoma 2. example of translocation Neoplasia notes
leading
to inactivation
of apoptosis
gene: see
Burkitt's lymphoma:
1. 2, in children located in abdominal cavityA. paraortic lymph nodes B. terminal ileum C. "starry sky" appearance under low power high grade B cell ma Ignancy .A. EBV relationship B. t8; 14 translocation of c-myc oncogene
Me lymphoma
3.
Mycosis fungotdes: 1. c:;D4 T helper cell malignancy 2. skin invasion produces nodular lesions and Pautrier's microabscesses cells) 3. systemic disease 4. called Sezary syndrome when PAS positive T cells are present in blood Histiocytosis X: 1. mainly childhood disease- hisriocytes are CDI positive 2. typesA.. eosinophilic granuloma: (1) benign histioeytes (2) lytic lesions. in bone with pathologic fractures
(malignant
lS
Note: This material
is
copyrighted. All rights reserved.
II
B.
3.
W
Hand-Sehuller-Christian disease (1) malignant (d) Ql (2) triad of exophthalmos diabetes insipidus) lytic lesions in the skull C. Letterer-Siwe disease: (1) malignant: infants and young children (2) diffuse eczematous rash (3) organ involvement (4) lytic lesions in bones USMLE .seen aria- two' year nld with eczematous rash and organorn egaly and biopsy of skin revealed COt positive cells
0)
"?:J l"Ie( "''1 f' 3,
...
...
?J?rJtlf~'-1S
"
a:
Hodgkin s disease (lID): 1. clinica:JA. RS cell is the neoplastic cell: see question #1 p~ 186 of'Review book for picture (1) can be a B or T cell (2) must be present to Dx Hodgkin's B. nodular sclerosing MC type C. fever, night sweats, weight loss often confused with TB D. prognosis corresponds with number ofRS cells and type of Hodgkin's E. death by second malignancies due to alkylating agents: e.g., non-Hodgkin's lymphoma 2. summary of the subtypes of Hodgkin s Disease (HD): note how the types move from those with 'the least number to the greatest number of RS cells, from best. prognosis to poorest prognosis and from a young age to an older age Comments 5% HO. Male dominant. Asymptomatic young male with isolated node or node group (cervical or supraclavicular). Hard to identify RS cells. Usual] stage 1. Best survival (90% 5 year survival). Increased incidence of second malignancy (NHL) .due to .alkylati n_g_gents used in Rx of HD. a 60%H.lil. Female predominant, Stage ITA Me oresentation"'ranterior mediastinal nodes and oerVical/supraclavicuJt-). RS variants are called lacunar cells. Coll!!S:en separates nodular areas. ~70% 5 year survival, 3,0% lID. Male dominant. Middle age. RS cells easy to find. -5.0% 5 year survival. 5% RD. Men >40-50 years old. Most aggressive lID. -20% 5. year survival
Hodgkin's disease subtype Lymphocyte pred omina nt
Nodular
sclerosing
Mixed cellularity
Lymphocyte depleted HD = Hodgkin's disease, RS
= Reed
Sternberg cell
X-ray with multiple lytic lesions in the bip tn a patient with anemia and bypercalcemi.a: 1. multiple myeloma- seetable for description of all monoclonal gammopathies 2. summa_!)' of monoclonal 2a~l1mo.pathies (includes amyloidosis)Comments: Disorder -60% of all cases of MG (1\1GUS is MCC of monoclonal spike). Monoclonal gammopathy Most are an IgG M-spike. Majority pursue a stable course. Some of undetermined develop multiple myelomaor related disorder. s~gnificaDce (MGUS) -20% of aU cases of MG. Me primary malignancy of bone. More Multiple myeloma (MM) common in African-Americans than whites (2: 1). Rare under il0 years old. Increased risk with radiatlcn exposure. M-spike in 80-90% and urine BJ nrotein (light chains) in 60-80%. M-spike usually _IgG..
16
Note: This material is cop righted. All rights reserved.
Sheets
of malignant plasma cells> 10% of cells in, marrow. Increased
B-1 microglobulin portends a pool' survival (con-elates with degree 'of p lasma eel I pro liferad on). S uspec(MM in any m idd Ie aged to elder! y patient with unexplained anemia .. bone pain. pathologic fracture. recurrent infection, unexplained hypercaice-mia or re'na! faiilll'e without hYOe,rteflslon. Skeletal system: I.¥tic lesions ("punched out"). bone pain. pathologic fractures. Hematologic system: anemia, rouleaux, increased, sedimentation rate,
Urinary system: nephrocalcinosis (from hypercalcemia) Mec of acute renal failure. Light chains are to. ic to' tubules and produce a giant ceU reaction, Prone to primary amyloidosis involving kidneys. Endocrine system: hypercalcemia clue to 10ca1 release of osteoclast activating factor by plasma cells. Waldenstrom' macroglobulinemia
thrombocytopenia
Infection ,Me COD. Clinical: monoclonal proliferation secreting excessive IgM.
Clinical:
of
lymphoplasmaeytoid
cell
Heavy chain diseases (ct,
Y" I-l types) Amyloido.si-.s
hyperviscosity syndrome (85-9~%) heparosplenomegaly, lymphadenopathy, anemia. BJ protein in .... 0%. 8 M protein part of heavychain devoid of light chains located in serum and urine, Amyloid is a ilbrillal1' protein that deposits into Interstitial tissue resulting in organ dysfunction. Properties of amylcid: twisted 13- pleated sheet <i3_-fibr.i.Uoses). Congo red positive and demonstrates apple green birefringence (like a Granny-Smith apple) under polarized light. Electron microscopy: linear, non-branching fiber with hollow cores. Derived from different proteins: lilrht chains (association with MM), serum associated Amyloid (8M, all acute phase reactant 11] infla... mmation) prealbumin, B amvloid proteins, and peptide hormones like calcitonin. Two main types of amyloidosis: primarY amyloidosis (light chain derived) and secondary (reactive) amyloidosis (SAA derived" rheumatoid arthritis TB, Leprosy renal adenocarcinoma). Common sites of involvement: heart, spleen tongue adrenals, liver
and kidneys.
Cardiovascular system: restrjotive cardiomvopathylocalized form
in the elderly due to prealbumin-derived amyloid Gastrointestinal system: macroglossia, malabsorption hepatornegalj with increased alkaline phosphatase Musculoskeletal system: earpal tunnel syndrome common. Renal system: renal failure is Me COD (nephrotic syndrome) CNS: Alzheimer's disease (~",amyloid protein coded by chromosome 21. Amyloid toxic to neurons. MC' COD in Down's syndrome patients
>40. Diagnosis! Ex ofrectal mucosa, gingiva, omental fat pad or the organ
involved.
Other types of amyloidosis: medullary carcinoma of thyroid
(calcitonin derived amyloid)_ 17
Note: This material 'is copyrighted. AU rights reserved.
chart of important disorders of the spleen: Comments Disorder Infectious mononueleosls: splenomegaly invariably present. Ruptures with Systemic infections! trauma (contact sports) more than spontaneous. inflammation
Summary
Kala azar: massive splenomegaly in visceral leishmaniasis, Leishmania in macrophages, Malaria: MeC of splenomegaly in third world countries. Autoimmune disease: splenomegaly common m SLE and rheumatoid arthritis. SLE has hyperplastic arteriolosclerosis (onion skinning of the penicillary arteriole).
Neoplastic
disorders
Hypersplenism
Myeloproliferative disease: splenomegaly invariably present (massive In agnogenic myeloid metaplasia). Extramedullary hematopoiesis common (trilineage hematopoiesis in sinusoids). Leukemia: splenomegaly invariably present often massive (chronic lymphocytic leukemia). Red and white pulp involved in most cases. Red pulp only in hairy cell leukemia. Malignant lymphoma: NHL and Fill commonly produce splenomegaly, Metastatic malignant Iymphomas·are splenic malignancy. Hypersplenism is an exaggeration of norma) splenic function. RECs WBCs and platelets, either singly or in combination are sequestered and destroyed. Portal hypertension in cirrhosis is MeC. Felty's syndrome is the combination of rheumatoid arthritis, splenomegaly and autoimmune
rvrC
neutropenia.
Sickle cell disease Sickle cell disease begins with' splenomegaly owing to entrapment of RBes in the cords and sinuses, Spleen non-functional at early age (-2 years old). Markedly reduced in size (infarction)' in late adolescence (called autospleneetomy) . PH most commonly secondary to ctrrhosis. Increased portal vein pressure producescongestive splenomegaly. Hypersplenism common. . Most are pale infarcts secondary to emboli originating in the left side of the beaM (e.g., thrombus, vegetations). Commonly produce left Upper quadrant pain and friction rubs (fibrinous exudate OJ] capsular surface). Congenital asplenia sssociated in >80% of cases with malformations in the heart. Splenectomy (or functional asplenla (sickle eell disea eJ) predisposes to infections (septicemia, peritonitis). Streptococcus pneumoniae foUowed by Hemophilus influenzae are Me infections. Hematolocic abnormalities with splenectomy: presence of nucleated Mes, Howell Jolly bodies (nuclear remnants in the cytoplasm), increased reticuloeytes (RBe membrane is net removed by macrophages), target cells (excess membrane cannot be removed) Heinzbodies (denatl.lred Hbl and an increase i:opla~elets_(thrombocvrosis).
Portal hypertension (PH) Splenic infarction
Congenital Splenectomy
asplenia
18
Note: This material
Is copyrighted.
All rights reserved.
Coagulation:
<ir
see schematic
ec; ,- J
+f2.00. e rJ
,I
IV 111 I
+-HJ!J;""/o
,
".I)
--.11J{
,rc+1 I/;'/""'" r
•
Factor
1. 2.
pre enting small vessel clotting: / heparinenhances antithrombin III (A'I'Ill), which neutralizes coagulation factors: XII, Xl, IX, X prothrombin (IT), thrombin
most
serine
protease
PGlr
A.symhesized by endothel ial cells B. vasodilator C. inhibits platelet aggregation e v. fJ/ protein C and S- ,{ Vi+aw-jN A. Inactivate factors V and vm B. enhance fibrinolysis tissue plasminogen activatorA. release of plasmin B. destroys coagulation factors and clots
3.
K-d f8
I rf-" 9
4.
Factors acting as proeoagulants (form clots) in small vessel injury: 1. thromboxane Ar A. synthesized by platelets B. vasoeonstricten/bronchcconstrictor C. enhances platelet aggregation D. cyclooxygenase blocked by aspirin and NSAIDs 2. von Willebrand factorA. VIILvWF B. synthesized by endothelial cells and megakaryocytes: platelets carry some V1II:vWF C. platelet adhesion factor: platelets have receptors for VU1:vWF 3. extrinsic and intrinsic coagulation system
W
,r::;r
Normal events with small vessel injury: sequence ofev'ents1. vessel injury ~ 2. activation of factor in the extrinsic coagulation system by tissue thromboplastin and activation of factor xn in the '"intrinsic system by exposed collagen (VII can directly activate IX in the intrinsic systemj-» 3. platelets stick to, Vill:vWF in damaged endothelial cells via their receptors (platelet adhesion) ~ 4. stimulus for platelet release of ADP from dense bodies causing platelet aggregation and synthesis afTXA:! ~ 5. temporary platelet plug with fibrinogen draped over It (fibrinogen receptors on platelets) stops bleeding (end of the bleeding timej-» 6. thrombin generated by coagulation pathway stimulation converts fibrinogen into fibrin and forms a stable platelet plug ~ 7. . plasmin destroys the plug and reestablishes blood flow J II Bleeding rime (BT): _DOC's NulCOt{tjtA jll{hotJ fqc+or?, tie! t.ecb' , .
vn
-Jesr lOR.
1.
2.
/
t._ri
cis la!clet abnormalities the (ormation of the teOlora causes of a prolonged BTA. thrombocytopenia B. no Vill:v:WF far platelet adhesion c. patient .on aspirin: MCC due to 00 TXA2 for aggregation D. renal failure
!at.leI plug
19
Note: This material is copyrighted. All rights reserved.
(1) (2) (3)
qualitative platelet disorder clue inhibition of platelet phospholipid reversed with. DDAVP (desmopressin acetate) reversed with birth control pills
Ristocetin cofactor assay: . ) 1. bed test for VIll:vWF Ilr'h,'rrJ, 't 2. ~p when ris.toeetio i.s added to a test tube 3. platelets without vm:vWF or the receptor for "nr:vWF~ Bernard-Soulier (thrombecytopenia and giant platelets) do Dot dump
(4.1'1
disea e
Summary of platelet tests: 1. platelet count: normal number does not always mean they are functionalaspirin 2. bleeding time- tests platelet function 3. ristccetin cofactor assay- detects Vm:vWF or its receptor on platelets
e.g., patient
0)1
Prothrombin time (PT): 1. detects extrinsic coagulation system factors down to formation or a clot- V1I (extrinsic system) -+. X ~ V -+ IT (prothrombin) ~ 1 (fibrinogen) -+ clot 2. international normalized .ratioA. for Ratients on warfa .' B. standardizes the test throughout the world so all test results are the same regardless of the reagent used 3. PT is best test for liver synthetic function • ,... PTT PT .....lotrinsic system •• }([[ ~ :
..
'Ii .''1 ,.,-
II.
'''',i..'
)([
VITI
IX
. . : £ : . • .
'
Partial thromboplastin time (PTT): see above schematic 1. detects intrinsic eoagulatien system factors (XII, XI, IX, VITI) down to formation of a clot- Xll ~ XI -)- IX ~ VIII ~. X ~ V -+ IT(prothrombin) -+ 1 (fibrinogen) -+ clot 2. used ta fallow he arlD therapy and factor deficiencies
r:Iir
Fibrin,olytie 1.
system tests: X, Y. D, E
~4 ~~
~
(jF'
q_fJJ' .-
y(\
fibrin (ogen) split productsor a fibrin clot
fragments after plasmin breakdown of fibrinogen
2.
D-dimersA. B. measu~es cf.oss.-iinked fibrin mODo_rn,ers,ina fib:in clot cross-links indicate factor XIII acnvity in forn~~nga stable clot
US:l\IIJE picture of an elde"'.
patients finding and not a sign of patient .abuse
hands wiOt senile purpura:
normalage-dependem,
20
Note: This material is copyrighted. All rights reserved.
r:r
Signs and symptoms of vessel instability and platelet problems: 1. epistaxis- nosebleeds (Me symptom)
2.
3. 4.
bleeding from superficial easy bruising
s-cratcbes-
110
temporary platelet plug
petechia and eccbymosesA. these_do_n.o:Lbl.aru;hsince they represent bleeding into subcutaneous tissue
B. oapillary hemangiomas and spider angiomas blanch withpressure mucosal bleeding
r:Jt1'"
1.
2.
scenark» 'Q a child followed by epiBtaxisand petec
purpura-
idiqpath.ic thromboeytopentc
A.
B..
MCC of thronrbocytopenia no splenomegaly
in chi Idren
IgG antibody against platelets: type II hypersensitivity megakaryocytes are present in marrow responds well to corticosteroids
C.
D. E.
Autoimmune thrombocytopenla in adults: 1. most commonly associated with SLEA. B. C. IgG antibody against the platelet type II hypersensitivity splenomegaly usually present unlike ITP in children
:R.x: (i)
(3) (4)
corticostercids-s
(2) splenectomy-»
al.kylating agents
IV y-globulin if bleeding cannot be controlled: tbrombocytopeniablocks Fe receptors for IgG on
2.
maorophages other causes of autoimmune
A. drugs:
B.
quinidine (type IIhypersensitivity) (2) heparin (antibody against heparin 'attached to platelet membrane) viruses: H1V (Me hematologic abnormality) (1)
Thrombotic rhrombocytopeulc purpura: 1. small vessel damage (unknown plasma factor) with consumption of plateletsA. possible causes of endothelial cell damage: (;1) infectious diseases (2) diseases: progressive systemic sclerosis, hypertension (3) drugs- e.g, mithramycin, birth control pills (4) anti-phospholipid antibodies (5) preeclampsia platelet thrombi: (1) not DIe, sincecoagulationfactors are not consumed (2) only platelets are consumed (3) abnormal vm:vWF in endothelial cells may contribute to platelet aggregation vasoconstriction (1) endothelia vasoconsrrictor) released i~ damaged endothelial cells (2) decrease in nitric oxide and PGI2- normally. they are vasodilators
B.
C.
21
Note: This material is copyrighted. Ail rights reserved.
2.
3.
4.
5. 6, 7.
microangiopathic hemolytic anemiaA. RBes hit platelet plugs-» B. schistocytes: must be present to secure the Dx fever eNS problems renal failure Rx with plasmapheresis hemolytic uremic syndrome the brain is worst hit
in children-
similar except kidney is worst hit willie in ITP
0157:H7 serotype of E. CQIi: 1. hemolytic uremic syndromeA. renal failure B. amentia with schistocytes C. thrombocytopenia, D. CNS findings: less common than TIP 2. 3. organism proliferates in undercooked unpasteurized apple cider Shigella toxin can also produce beef or produce contaminated witb E.
cott- e.g .•
nus
Thrombocytosis: causes1. chronic iron deficiency: common 2. malignancy: common 3. splenectomy 4. infections 5. myeloproliferative diseases: e.g., polycythemia Signs and symptoms of coaguJation 1. late rebleedingdisorders:
vera
2. 3.
A. temporary .platelet plug is only mechanical block of small vessels B. bleeding after Wisdom tooth removal or from the incision site in any type of surgery 'bleeding into joints (hemarthroses) and closed spaces- only severe types like hemophilia A and B with, very loW factor levels mucous membrane bleeding- G1 and GU bleeds,
Hemophllia A: 1. SXR 2. JabA. prolonged PIT B. normal PT C, lowVTI1:C D. normal Vlll.antigen and VIII: vWF 3. cllnlcal- see previous discussion 4. RxA. reeembinant factor VITI for severe cases
B.
DDA VP (vasopressin) for mild cases: increa-ses' synthesis of all factor VI1J molecules
Classical VWD: 1. AD
2.
labA. B. prolonged bleeding time normal PT
22
Note: This material is copyrighted. All rights reserved.
C.
D. E.
3. 4.
prolonged PTT 1.0'"'" VIII:C low Vlll: antigen
F. low ristocetin cofactor assay: decreased Vill':vWF MC g~netic ccagulopathy
clintcat-
5.
A. menorrhagia B. mucous membrane bleeding' RxA. DDAVP (desmepressin)
B.
C.
birth control _pills iin women with. menorrhagia; estrogen increases synthesis of all VITI molecules
cryoprecipitate: (1) blood preduct containing Vlll, fibrinogen, (2) rarely used PTT: lab findings
xm
inhibitor) and
Patient with antibody against factor VIIl:coagulant
prolonged
1.
(c,ircuiating auricoagulant,
normaJPT
prolonged PIT
2.
3.a£ter
4.
mixing 0.5 ce of normal plasma with O.S ec of patient plasma, the PTT is repeated and is still prolonged: antibodies inhibit Vlll.coagulant in the nOI'IQal plasma as well a true factor Vlll.coagulant deficiencycorrection.of the PTT after adding normal plasma
bOI1J:l,d
AntiphosphoUpid syndrome: 1. definitiou- antibodies directed against phospholipids 2. types of antibodiesA. lupus anticoagu Iant: (2) (3) (4)
to plasma proteins
B.
misnomer: actually causes clotting usually produces a prolonged PTT PIT not corrected with addltioa of normal plasma PIT corrected by~dding phospholipid anticardiolipin antibody; (1) cause of a biologic false positive syphilis serology (2) seen in SLE, m:v other disorders
(1)
3.
(3) causes thrombosis clinical syndl'omesA. repeated abortions: placental bed clots
B. C. D.
strokes thromboembolism hepatic vein thrombosis
Vitamin K deficiency: 1. causes bleeding-
A. B.
2.
vitamin K y·carboxylates n, vn, IX, X, protein C and S y-carboxylation allows calcium to bind to these factors in a clot C. absence of l'.ca:rboxylation leaves vitamin K dependent factors non-functional: is anticoagulated causes of K deficiencyA. newborns lack bacterial colonization for vitamin K synthesis
patient
23
Note:l'b.is
material i.5' copyrighted, AU!1ights reserved.
(1) (2) (3)
require IMinjection
vitamin
of vitamin Kat birth: no vitamin Kin breastrnilk
if newborn is nat protected: called
K levels n011l1a11y decrease between days 2-5
danger
of intracerebral hemorrhage hemorrhagic disease of the newborn
B.
C. D.
malabsorption antibiotic Rx sterilizes bowel: MeC in a hospitalized patient warfarin blocks epoxide reductase (normally keeps vitamin Kin functional Kl state); (1) vitamin K non-functional (2) rat poison contains warfarin
3.
alcoholic with cirrbosUlA. could be problem with liver synthesis of vitamin K: prolonged PT not corrected with 1M vitamin K B. could be problem with malabsorption of vitamin K from bile salt deficiency or chronic pancreatitis: prolonged PT corrected with Th1 vitamin K q.uestioD o-f child taking-Fat poison: contains warfarin- will cause bleeding Rx with 1M vitamin K if not medically signlfican medically significant bleed
""",~~o:..
1.
2.
bleeding-
use fresh frozen plasma jf a
Vitamin abnermallriesasseelated with prolonged PT: L vitamin K deficiency 2. vitamin E to~icity-A. B. inhibits synthesis of vitamin K dependent factors synergistic with warfarin
Patient on warfarin: 1. mechanisro:A. blocks vitamin Ksability to ,(-carboxylate factors II IX X, protein C and S B. blocks epoxide reductase: normally keeps vitamin K in its active K1 state 2. prolonged PT and PTT- PT is better test for following patients than PTT 3. bleeding Me comptieatiouA. if overanticoagulated and seriously bleeding give fresh frozen plasma B. 1M vitamin K, if bleeding not serious 4. r.n1Qu yy-cai'boxylated vitamin, K d -penden1fa.ctors must msapptar before patfeu1 is_ fully anticoagUlated (USMI1FJ)A. reason why heparin is given along Witll warfarin B. VII and protein C have the shortest half-life (6 hOUIS) C. prothrombin has the longest half-life of 3--4 d S. hemorrhagic skin neercsis+ A. usually a patient who is a heterozygote with protein C deficiency and 50% factor level B. when put on warfarin patient w1U have 0% protein C levels in 6 hours due to short half-life of protein C: causes thrombosis of vessels in the skin before the parient is fu lly anti coagu lated
vn
Patient on heparin: 1. prolonged PT and PTT- PIT is the better test to follow patients
2. overanticoagulatedgive protamine .sulfate
3. 4.
heparin is Me drug associated with thrombocytopenia prevents venous clot formationA. does not dissolve the clot
'in the hospital
24
NOte: This material is copyrighted.
All rigbts reserved,
B. C.
can be used in pregnancy
complications:
(1)
(2) (3)
r::F'
bleeding thrornboeytopenia osteoporosis
DIe:
1. pathogenesis--
2. 3.
intravascular consumption of dotting factors B. consumption of fibrinogen V, vm prothrombin, platelets clinical- diffuse oozing of blood from. all breaks in the skin. plus mucous membranes causesA. endotoxic shock: Me B. infections: meningocoocernia
C. rattlesnake envenomation D. amniotic fluid embolism labA. prolonged PT and PTT B. low fibrinogen i1ll:':re'.l8e-d s~Ut proCl_ucts and D:-dime1;: best tests for DIe (U~L"'.L.L..lI!J--)C. thrombocytopenia D. E. schistocytes: RECs bit fibrin clots
A.
4.
5.
RxA.
B. C.
Rx underlying disease causing DIe use blood components to keep the patient alive: basically adding more fuel to the fire hep~n: blo,c~,\ thrombin, hence preventing clots and consumption of coagulation factors ( l~.,..,I'{ tJ.S3...1
Hereditary thrombosis syndromes: 1. cllnlcalA. venous thrombosis and pulmonary emboli at early age B. clots In unusual placesve.g., dural sinuses 2. causes= A. factor V Leiden: (1) Me hereditary thrombosis syndrome (2) protein C and S cannot degrade factor V B. ATill deficiency: (1) no prolongation ofPTI a£t:er starting heparin (2) give massive doses of heparin and the PTT will eventually prolong (3) send home on warfarin (4) birth control pills is Me acquired cause C. protein C and S deficiency; (1) cannot inactivate V and vm (2) start with heparin and very low doses of warfarin so that hemorrhagic
skin
necrosis does not occur
25
Note: This material is copyrighted. All rights reserved.
Examples
of hemostasis Bleeding time Prolonged Prolonged Normal Prolonged
abnormalities: Platelet count
PT
Norma]
Normal
PTT Normal
Proloqge:d Prolonged Normal
In terpretation
a. b. c.
Normal
'Normal
Aspirin or NSAIDs
von Willebrand's Hemophilia A 1TP. TIP, HUS Warfarin or heparin DIC Blood loss
NOrmal
Low Normal
Normal
Normal Prolo1!8_ed Prolo'I!&_ed Normal
d.
e. (ab) (ae)
Normal
Prolonged
Prolon_g~d
Prolonged
Low
Normal the board review:
Nanna!
Normal
Que dons used during
qr
W1iich of the following is more often associated Willebrand's disease? A. Normal PT B.. Prolonged PTT C. Low VID:Ag levels D. Normal bleeding time E. Treatment with desmopressin acetate
with mild hemophilia
than
classical von
D
Clr
A febrile 65-year-old man with urinary retention secondary to prostatic hyperplasia develops ARDS complicated by endotoxic shock. Within 24 hours he has oozing of blood from all puncture sites, extensive ecchymoses, .and muccsal bleeding, Which of the following tests ,is MOST USEFUL as an initial screening test? A. D-dimer assay B. Prothrombin time C. Bone marrow aspirate
D.
E. A (DIC)
Partial thromboplastin time
Examination of the peripheral blood
Vitamin K deficiency is MOST LIKELY present in a patient. .. A. with liver disease who is being treated with a broad spectrum antibiotic B. with traveler'S diarrhea who is being treated with ciprofloxacln C. 00 heparin therapy for prevention ofa pulmonary embolus D. with lactase deficiency who currentlyhas watery stools E. who has taken warfarin 3 hours ago
Note: This material
is copyrighted.
All rights reserved.
1m munohematology
Glycoproteins: 1. proteins to wlrieh are attached short, branch-chained oligosaccharide 2. functions includeA. cell surface antigenicity: e.g., blood group antigens all RBCs 13. components of mucin: e.g., mucous layer covering the stomach mucosa C. tumor markers: e.g., prostate specific antigen
ABO blood groups:
1. 2. 3. II gene--- codes for a transferase that attaches fucose to a glycnlipid to form.H antigen A gene- transferase product attaches N~acetylgalactasamine to. H antigen to produce A antigen B gene- transferase product attaches galactose to H antigen to form B'antigen geneA. inactive B. 0 R:Bes are DAly surfaced by H antigen AB RBCs:- have Hantigen with A or B sugar moieties blood group 0A. universal donor: refers to transfusion of packed RBes not whol€ blood B. no antigens on surface and cannot be destroyed C. must receive 0 blood D. increased incidence of duodenal ulcers E. have 3 antibodies: (1) anti-A 19M (2) anti-B IgM (3) anti-A,B IgG (can cross the placenta] blood group ABA. universal recipient
4.
5. 6.
7.
8.
B. no antibod ies to destroy transfused RBCs blood group AA. has anti-B IgM
;0
9.
10.
B. increased incidence of gastric cancer blood group B-has anti-A IgM ABO typing of mother and father ti) see if the child is tbeirs-
A.
B.
AB parents cannot have an 0 child
0 parents cannot have an AB A, or B child
27
Note: This material is copyrighted. All rights reserved .
. Qr
Type
MlO blood group summary: Antibodies Whites
Blacks 49%
Asians 40%
Native Americans
Comments
1
anti-A IgM anti-B IgM,
IgG (can cross the placenta) anti-A,B
45%
79%
Universal
donor (no' antigens on the surface).
Anti-A B IgG is responsible for ABO incompatibility. Can only receive
0 blood antibodies would destroy AB or
AB blood} Predispcsition for duodenal ulcer disease, A B
anti-B IsM"
anti-AlgM
40% 11%
27% 20% 4%
28% 27%
16%
Predisposition
carcinoma.
for gastric
AB
none preent
4%
5%
4%
<1% Universal recipient (no
antibodies). Rh poslttve:
1. 2. Lewis 1. 2. 3. means the patient bas Dantigen other Rh antig.ens- C, c, E, e, -d (does nat exist) antibodies: naturally occurring Igl'4 antibodies no clinical significance no risk of hemolytic disease of newborn
(HDN)
Duffy antigens:
r.
2.
uncommon in Afrtcan-Americans surface receptor fot' P. vivax- African-Americans against malaria '*
lacking the antigen have protection
] antigens: 1. anti-I A. B. 2.aoti-i A. B.
is a cold agglutinin (lg'l\1)M pneumoniae infections possible cold type of autoimmune hemolytic anemia (IgM)infectious mononucleosis possible cold type of autoimmune hemolytic anemia
Patient who i going to receive a packed RBC transfusion: 1. must perform an antibody screen on patient serum- indirect Coombs test 2. major cressmerehA. purpose is to see if the patient has antibodies that will destroy donor RBCs B. patient serum against donor RBCs
c.
D.
E.
good quality control on whether patient had any antibodies reacting against donor RBC antigens type II hypersensitivity reaction does not prevent patient from: (1 developing antibodies against donor REC antigens
Note: This material is copyrighted. All "ights reserved. patient from getting infection: CMY Me, HCV HN
~rcanJibody
(2)
HEV
in rr.:-S." ,S:MLE)l anti CMV antibody by blood transfusion:
CMV, not HeV, whi h is the MCC
Most common inJection transmitted
of posnransfusion hepatitis
MCC of post-transfusion MC infection blood transmitted hepatitis: HeV by accidental needle stick: HBV, which has a high vi-al burden in
HIV risk post-transfusion: HBV risk post-transfusion:
1:676,000 risk per unit '1 :200,000 risk per unit
Hev
risk post-transfusinn:
1:33'00 risk per unit
Risk of HIV positivity pest-accidental needle stick: 1. 1:300 2. Me way of becoming BIV positive in medical personnel 3. Rx with trtple therap for 6 months + repeat HIV serology ona regular basis Fresh frozen plasma: 1. contains all coagulation factors 2. clinical uses- multiple factor deficiencies:
A.
DIC
3.
B. liver disease C. vitamin K deficiency hepatitis eisk
Packed RBCs: 1. high hematocrit- contains some plasma 2. transfuse only if patient is symptomatic 3. hepatitis risk
and does not respond to medical therapy
PLatelet transfusiea: 1. raises platelet count 5000-10,000 cells/J.lL per unit 2. transfuse platelets only if the patient is symptomatic 3. hepatitis risk
Cryo preci pita te: 1. blood produce containingA. all factor vm molecules
B. fibrinogen
C.
2.
factor XIII, fibronectin
hepatitis risk
Febrile transfusion reaction: 1. patient bas anti-HLA antibcdies against HLAantigens on donor leukocytes 2. causes the release of pyrcgens from destroyed donor leukocytes 3. type n hypersensitivity 4. patients must have previous exposure to foreign HLA leukocyte antigens in order to develop
antibodies A. common in pregnancy- fetal maternal bleeds it spontaneous abortions.
C. previous transfusion
29
Note: This material is copyrighted. All rights reserved.
Allergic transfusion reaction: 1. ,Metype of reaction 2. patient develops hives against proteins in donor unit 3. type I hypersensitivity Hemolytic transfusion reaction: L units are ABO incompatibleA. patient receives wrong blood type (1) e.g., patient A (has anri-B Ig1v1)and donor blood is B----)o
(2) e.g. anti-B IgM attaches to B positive donor cells-s (3) activates complement system-s (4) intravascular hemolysis B. type n hypersensitivity reaction patient has undetected antibodies that react against donor RBC antigensA. extravascular hemolysis B. jaundice, drop in Hb positive direct Coombs: reaction may be delayed in some cases, C. type n hypersensitivity
2.
Hemolytic disease of tbe newborn (HDN) due to ABO incompatibility: 1. 0 mother with A or B babyA. 0 people normally have anti AB IgG which crosses the placenta: (1) antibody attaches to baby RBC antigens and splenic rnaerophages destroy RECs (2) mother's liver handles unconjugated bilirubin released by fetal rnacrophages B.
C. (3) baby develops a mild anemia: weak antibody compared may occur in first pregnancy DO increase in severity with 'future pregnancies
to anti-D
antibodies
2.
labA. spherocytes in cord blood: not present in Rh HDN B. positive direct Coombs on cord blood RECs C. mild hemolytic anemia: rarely requires an exchange transfusion clinicalA. MCC of jaundice in first 24 hs: babies liver cannot handle excess DeB load B. protects against Rh sensitization: (1) 0 patients haveanti-A IgM, anti-B JgM, and anti-Als-Ig (2) anti A 'or B IgMantiboclies immediately destroy fetal RBCs in maternal circulation
3.
Rh immune globulin:
1.
antt-D from pooled human donorsA. passive immunization B. does not cross the placenta C.given to pregnant women who. do not have anti-D at 28th week D. no hepatitie risk
2.
baby is Rh positive and mother
A.
does
Dot have
anti-De-
B. C.
amount ofRh immune globulin to give is based on Kleihauer-Betke test: (1) testis performed on maternal blood (2) detects amount of fetal-maternal bleed (fetal REGs resistantto alkali and acid) give Rh immune-globulin within 3 days immune globulin destroys fetal RBCs in maternal circulation
30
Note: This material ts copyrighted, All rights reserved.
r::ir'
Rb BD N: 1. mother Rb negative and baby Rb positive 2. first pregnancy with Rb + baby bas DO effect on baby 3. mother could be exposed to fetal RBCs with D an igen during delivery and develop antibodies+ purpose.of'Rh immune globulin is to prevent this from occurring 4. iI subsequent pregnancies have Rh+ babi:esA. maternal 8Ji1ti-DIgG antibodies cress placenta-» B. attach to fetal RBCs-+ C. RECs extravascularly removed by fetal rnacrophages in the spleen-s D. unconjugated bilirubin (UeB) is end-product of liemolysis (mother's liver handles
UCB)-+
E. fetus develops anemia {severe anemia, chance of heart failure and hydrops fetalis ~ F~ bilirubin pigment can be detected in amniotic fluid (optical wavelength of 450) and mapped on a Liley graph to determine severity of hernolysis=-eG a delivery. baby cannot handle UCB load and is often exchange transfused to prevent kernicterus exchange transfusion: A. removes VeB B. removes antibodies C. corrects anemia
5.
Cross-section of brainstem with yeUowisb discoloration in a child: probably kernicterus from Rh hemolytic disease of the newbern t!1l&rU'Cfjfljocf b,"ftT_.eI(.b;n./
lie. &/
uestiorused'
during the board.review:
A blood group 0, Rh-negative woman is pregnant with her first child. She has a negative antibody screen and no previous administration ofRh immune globulin. She.delivers a bloodgroup A Rhpositive baby. The baby develops unconjugated hyperbilirubinemiaB hours after birth. Which of the following statements correctly describes this case? A. She is Rh compatible with her baby B. She is ABO compatible with her baby C. She 1S a candidate for Rh immune globulin D. Nega ive direct Coombs of baby',s cord blood E. Jaundice is sec-ondary to Rh incompatibility with destruction offetal cells
31.
Summary of physical diagnostic signs in cardiovascular disease: Abbreviations usetl- $1: first heart sound, 82: second heart sound, Sj: third heart sound, S~: fourtb heart sound, rv.tV: mitral valve, TV: tricuspid valve AV: aortic valve, PV: pulmonic valve, TPR: total peripheral resistance 1. valve locations fOl'auscultatioDA. mitral valve ().i1V)at cardiac apex B. tricuspid valve (TV) along left sternal border C. pulmonic alve (PV) in the left 2nd and 3rd intercosta! space (IeS)
2. D. aortic valve (AV)- in the left sternal border or right 2nd cardiac cycle relationshipsA. P wave: atrial depolarization B. PR Interval: atrieventricular conduction time C. QRS: ventricular depolarization D. S4: comes just before the QRS E. SI: comes at the same time as the QRS F. T wave: ventricular repolarization or recovery G. 82: comes just after the T wave
$1
leS
3.
heart ,soandclosure of the. MY and TV during systo I.e Iv1Vcloses before TV normally not split corresponds with carotid pulse accentuated in early mitral stenosis when valve is still pliable closure of the AV and PV in diastole aortic 'component (A:a) precedes the pulmonic component (Pi.) 82 splits on inspiration owing to blood entering right heart: (1) negative. intrathoracic pressure from diaphragm moving down (2) delayed closure of PV (3) becomes a. single sound on expiration A'l accentuated in essential hypertension P2 accentuated in pulmonary hypertension Inspiration A2 ........... P2 (separates) Expiration A'l P2 (single sound)
A. B.
C. D. E.
4.
8..heart soundA.
B.
c.
D.
E.
5.
paradoxical split of S~A. ,P2comes before A:a and split occurs on expiration rather than inspiration B. due either to delay in AV closure or early closure of PV: e.g., left bundle branch block which delays AV closure)
fixed splitting of S2A. S2 is split during iaspiraticn.Inormal) and expiration (abnormal) B. due to delayed PV closure AV closureAV e.g. atrial septal defect where blood is always moving from the left atrium into the right atrium and PV closes even later than itnormally does
6.
c.
7.
physiologtc 83A. B. normal in children and young adu Its occurs in early diastole
32
Note: This material is copyrighted. AUrigbts reserved.
C.
due to rapid ventricular filling with vibration of valve cusps and ventricular wall or impact of ventricle against chest wall Of sudden limitation ,of longitudinal expansion of
8.
9.
patbologic Sr A. abnormal after 40 y old B. due to blood entering a volume overloaded left or right ventricle (1) e.g., xaJume overloaded left at right ventricle in left heart failure/right heart failure (2) e.g., A V fM:'/ regurgitation or PV rrv regurgitation C. first cardiac sign of congestive heart failure: increased ventricular volume stretches the MY 'or TV rin~ volume overload from mitral/tricuspid regurgitation D. left-sided So increases in intensity on expiration E. right-sided 53 increases on inspiratierr (more blood in right heart 011 inspiration) S4 heart soundA. coincides with atrial contraction in late diastolic filling and the ~ in tbejy_g~ due to increased resistance to ventricular filling (decreased compliance) following vigorous atrial contraction C. decreased compliance may be due to: (1) ventricular hypertrophy (leftlrigbt) or (2) already volume overloaded ventricle (left/rlght) D. S.l is absent in arrialfibrillation E. left-sided 54 increases in intensity on expiration F. right-sided 54 increases on inspiration (more blood in right heart on inspiration) mid-systolic ejection clicks in MV!fV prolapseA.cHck is due to ballooning of excess valve tissue into the atrium during systole B. click is usually followed by a regurgitation murmur C. maneuvers that cause click/murmur to come closer to 8, are those that decrease volume in the left/right ventricle so systole occurs faster: (1) standing up (decreased venous return to the heart) (2) Valsalva maneuver ~ (3) arudety (increased heart rate decreases filling of ventricle in diastole) D. maneuvers that cause click/murmur to come closer to S2 are those that increase the volume of blood in the ventricles so systole takes longer to.occur: (1) lying down (increased venous return to heart) (2) sustained clenching of fist (increases afterload' the ventricles have to contract against) opening snap io MVffV stenosisA. occurs MV lTV (less common) stenosis B. due to nonpliable valve which has difficulty in -opening in diastole until atrial contraction forces it open C. opening soap early tn diastole indicates severe disease: correlates with intense atrial contraction D. opening snap [hat OCCUT~ later in diastole indicates less severe stenosis: correlates with less intense atrial contraction to open the valve heart murmur cbal'acteris1icsA. occur in systole and/or diastole B. mechanisms (1) structural valvular disease B.
LV
~l.}..o.us..:R.9lst.
10.
11.
12.
33
Note: This material is copyrighted. All rights reserved.
(2) (3)
anemia innocent (unrelated to .structueal or physiologic alterations, e.g, normal child)
C.
rnurmurs radiate
(I)
(2)
D.
AV stenosis radiates into the neck radiates into .axilla graded 1 to 6:
MY regurgitation
(1)
gradeI easy-to hear
13.
(2) grade 4 to 6 often accompanied b palpable precordial, thrill (3) grade 6 audible without stethoscope E. murmur/heart sound intensity with, respirations: (1) right-sided murmurs and abnormal heart sounds 'increase 'on inspiration (2) left-sided heart murmurs/abnormal heart sounds increase on expiration continuous murmursA.. occur througb systole and diastole
B.
C.
cervical venous bum in children is MeC
patent ductus arteriosus (l?DA): called a machinery murmur
14.
15.
innocent murmurA. occur in -50% of normal children B. due to turbulent pulmonary artery blood flow in systole C. low grade (lor 2) D best heard with patient in supine position E. decreases with sitting/s anding stenosis murmursA. B. C. D. problems with opening valves valves opening in systole: A VIPV valves opening in diastole: MVITV AV IPV stenosis(1) ejection type (2) crescendo/ decrescendo due to blood forcibly moving through opening (3) produce concentric hypertrophy of left/right ventricle respectively MVITV stenosis- mid-diastolic murmUIOCGUrS after opening snap
constricted
E. 16. A. B.
regurgitation (insufficiency) murmursproblem with closing valves: incompetent valves closing in systole: M\!n'V C. valves closing in diastole: AVIPV D. MV!TV regurgitation: (1) even intensity pansystolic (holosystolic) murmur due to blood refluxing into atria throughout systole (2) volume overload of atria and ventricles (hyp-ertrophy/dilatation) E. AVfPV regurgitation(1) high pitched blowing murmur directly after 82 (2) volume overload of ventricles (hypertrophy/dilatation) Valsalva manenver-A. holding breath against a closed glottis: 'creates positive intrathoracic pressures R physiologic effects: (1) decreases venous return of blood to right heart (2) decreases cardiac output
17.
34
Note: This material iscopyrigbted. AlIl"ights reserved.
C.
l8.
19.
~O.
21.
(3) increases heart rate as.compensation fo~ drop to cardiac, output effect on murmursi (1) increases intensity of systolic murmur in idiopathic hypertrophic subaortic stenosis (hypertrophic cardiomyopathy)': decreases left ventricle volume which accentuates the degree of obstruction to blood flow into the aorta (2) moves systolic click/murmurcloser to SI in mitral valve prolapse (3) decreases intensity of ejection murmur of aortic stenosis: less blood ejected through the stenotic valve Ieft parasternal heaveA.sign of right ventricular hypertrophy B. right ventricle is located under the sternum C. hypertropnydue to: (1) pulmonary hypertension (called oar pulmonale) (2) PV stenosis (3) TV regurgitation pericardia) knockJ\, sign of constrictive pericarctitis B. cardiac chambers bit thickened (often calcified) pericardium when fiUingin diastole C, causes: (1) TB worldwide (2) cardiac surgery ill this country pericardial friction rubA. sign of pericarditis B. scratchy 3 component sound heard on auscultation over the. preoerdiutn: C. due to separation of fibrinous exudate on visceral/parietal pericardialsurface during tbe cardiac cycle D. causes: (1) coxsackievirus infection (MCC) (2) transmural acute myocardial infarction (3) Dressler's autoimmune pericarditis post infarction (4) systemic lupus erythe"matosllS (Me manifestation of SLE) (5) acute rheumatic fever pulse pressureA. difference between systolic and diastolic pressure (normally 30 to 40 mm Hg) B. causes of a narrow pulse preSSl,l1'e-
(1)
decreased stroke volume: a. aortic stenosis b. idiopathic hypertrophic subaortic stenosis. c. shock (cardiogenic, hypovolemic)
C.
increased total peripheral resistance CTPR) due to arteriolar vasoconstric ion: hypertension causes of a widened pulse pressure: (1) increased stroke volume: a. A V fMV regurgitation b. hyperthyroidism (2) decreased TPR due to arteriolar vasodila ation: a. endotoxemia b. thiamine deficiency c. warm shock in metabolic acidosis
(2)
35
Note: This material
is copyrIghted.
All rights reserved.
(3)
increased venous return to the right heart from arteriovenous venous communications that bypass the microcirculation} a. traumatic (MCC)
fistulas (arterial
22.
(4) ar 'erial pulsesA. normal arterial pulse, (1) normal upstroke is due to: a. interaction between the driving farce of left ventricular 'contraction and b. compliance (elasticity) of the vessel (2) initial rapidly ejeoted stroke volume is called anacrotic limb (3) pulse amplitude of upstroke modified by: 3.. elasticity of arterial wall
mosaic bone in Paget's disease decreased TPR due to decreased v iscos ityof blood: severe anemi a
b.
b. c.
(4)
amount of stroke volume total peripheral arteriolar resistance (TPR)
d. blood pressure davin stroke is modified by: a, vessel compliance (elasticity)
B.
b. TPR closure of aortic valve causes a momentary reversal in blood flow: produces a dicrotic notch in the down stroke (6) smaller, secondary positive wave in the down stroke is due to: elastic recoil of the aorta and aortic valve elderly patients:
(5) (1) aorta loses elasticity: a. rigid b. less compliant/less distensibility (2) same strok-e volume is distributed in an aorta with a smaller radius leading to an increased systolic pressure: possibility of systolic hypertension bounding pulses (Corrigan pulse, water hammer pulse): (1) increased' stroke VO] lime:
R.
C.
AVtMV regurgitation
b. (2) (3)
hypertayroidism c. high outpnt cardiac failure decreased TPR: arteriolar vasodilatation (see above) arteriovenous fistulas: see above diminution in amplitude of pulselblood pressure with inspiration: a. drop in blood pressure drop> 1 rum Hg during insp.iration b. normally drops a little on inspiration as blood fillil!.g the RV pushes on the interventricular septum and decreases the LV volume
D.
pulsus paradoxus:
1)
(2)
pathophysiology of PU.JSllS paradoxus: a. due to impedance .of inflew of blood inspiration-sb. c.
into the right be art during
automatically reduces th~ cardiac output and drops the blood pressure-e. neck veins distend on inspiration (called Kussmaul's sign, neck vein should collapse on inspiration as blood is sucked into the right heart by the negative intrathoracic pressure created by the diaphragms moving down)
36
Note: This material is copyrighted. All r:ights reserved,
23.
24.
causes: a. pericardia! effusion (MCC) b. decreased lung compliance: • interstitial edema in severeasthma • severe pulmonary edema • interstitia'! fibrosis Beck's triad- signs of pericardial effusion A. neck vein distention on inspiration: Kyssn'laol's sign B. hypotension: decreased cardiac output C. muffled heart sounds: fluid in the pericardia] cavity jugular venous pulses (JVPs).a v
(3)
A.
normal IVPs
(1)
B.
3 positive waves: a c, and v
(2) 2 negative waves: .x and y a Wave: (1) positive wave due to atria! contraction in late diastole (2) occurs after the P wave ift an ECG (3) disappearsin atrial fibrillation (4) giant a wave: 2. due to restricted filling of right heart b. e.g., TV stenosis, pulmonary hypertension
c wave:
C.
(1) (2) D. (1) (2)
positive wave due'to right ventricular contraction in systole causing bulgingof the tricuspid valve into the right atrium correlates with 8) and upstroke of, carotid pulse
x wave:
E.
F.
large negative wave occupying most of systole due to downward displacement of TV valve when blood is ejected om of the right ventricle into the pulmonary artery wave: (1) positive wave due to right atrial filling in systole when the TV is closed (2) giant c-v wave: due to TV regurgitation as blood refluxes up into the righ! atrium duringsystole y wave: (1) negative wave occupy ing most of d ias to le (2) due to opening of TV with rapid flow of blood into the right ventricle in diastole
37
c:~'(/o,"rt,\:r<.VN£
Note: TIJiB material is c_QPyrighted. A:Urights reserved. Lipoprotein fractions in blood: Lipoprotein Protein TG CH
W
PH 8
Comments Lcarries diet-derived TG- A. saturated fats, B. surfaced by apolipoprotein B4S, C. falsely elevates total
TG level if not fasting D.. small amount oJ CH in chylomicrons does not alter serum C]-I levels: no need to 1
fraction
Chylomlcrons 2 85 3
fast
2.physiologyVLDL 9
55
17
22
LDL
20
]0
45
21
pe,riQ_heraI circuleticn via the lymphatics liver-derived TG- A. also carries liverderived CH, B. surfaced by apolipoprotein H"oa 2.LDL is derived from VLDL in the peripheral blood-capillary lipopro:ein. lipase remo've~ TG from 1 VLDL and leaves CH behind Ill- the LDL fraction V'bad cholesterof"> A. derives from VLDL,. B.surfaced by apol ipoprotein B 100
2 ..LDL att:acliesto LUI.. TOOGptors on cells (USIVlliEJ)-
delivered Lcarries
to the
assembled
in the small
intestine
and
A. inhibits HJvfG GoA reductase: prevents further synthesis of CH. B. decreases LD L receptor synthesis, C. j rrcreasesesterifieation by acyl-Cox acyl tran sferase ~3,.functions of GH {USMLE)::-- A. steroid synthesis, B. vitamin D synthesis, C. bile salt synthesis, D.cell
HDL
50
:3
20
25
apelipoprotein A accompanies I-IDL and paralle Is HD L concentration __". 4ct";v.dE!SL~ AT 2. fUD,ctioDS- A. reservoir for apolipoproteias C and E
that are subsequently attached
to
membrane synthesis 1. "goode:holesterol"'_
circulating
chylom ierons arid VLDL. B. HDL removes
eH
from
atherosclerotic plaques (reverse CH transport), C. delivers CH to the liver for disposal . 3. synthesis increased- A. estrogen, Bvexereise .. C. red wine CH "" cholesterol, l-IDL "'"high density lipoproteins, 1-llv1GCoA = 3~hydrOxy-3~rrtethylglt!taryl coenzyme A LDL = low density lipoproteins. PH = phospholipid, TO = triglyceride VLDL = very low density lipoproteins W Fredrickson Is pbeootypicJgenotypic classification: 1. 2.
type 1- deficiency of APO C U or capillary lipoprotein lipase type 11A. polygenic hypercholesternlernia: 85%'{MC type)
B. C.
t.n,.-,....\--
'y), 1O\J~'J-kI-i W
D.
x-
\~'
~rt{b
CO-Pr
it
6i!.
E.
Re&,lIi,(
W\h;6'f+OK~
familial combined hypercholesterolemia familial. hypercholesterolemia pathogenesis: (1) absent or defective LD L receptorsor (2) defective internalization of LDL complex clinical findings in familial hypercholesterolemia: (1) premature coronary artery disease (CAD) and myocardial infarcts (2) AcbiUes tendon xanthomas B.re pathognomoni.c (75%)
---?
)(q,,1heIQSJ~a.s q~e til~O
38
Set:N
Note: Tbis material is copyrighted. A11rigbts reserved.
F.
laboratory findings: (1) LOL>190 rng/dl, (2) CH >260 rng/dl, (3) normal TG or increased TO (type Ilb if increased)
3.
type ill-
A.
B.
familial dysbetalipoproteinemia:
"remnant disease"
4.
pathogenesis: (1) absent Or defective apo E (.2) .chylomicron and intermediate density lipoprotein (IDL) remnants are not cleared C. laboratory: (1) CH and TO equally elevated (2) identify APO E isofonns type IV-
A.
B. C.
familial hypertriglyceridemia: Me type pathogenesis: decreased catabolism ofVLDL
D.
clinical: (1) increased incidence of atherosclerosis involving coronary arteries and peripheral' vessels (2) eruptive xanthomas (papules' with Tei) laboratory: (1) hypertriglyceridemia turbid infranate-e (2) slightly increased eH
5.
type
V-
A.
familial hypertriglyceridemia with exacerbating faetors like diabetic ketoacidosis or alcoholism B. pathogenesis; combination of type I and type IV (I + IV = V) mechanisms, which combine toequal a type" phenotype C.clinical: (lJ) common in alcoholics and diabetic ketoacidosis (2) hyperchylomicronemia syndrome: a, abdominal pain b. pancreatitis c. eruptive xanthomas D. laboratory: supranate-s (1) markedly increased TO with normal LDLinfrc1l1ate--lo (2) supranate and infranate present: see Lab Medicine notes
Lipid deposits: 1. Achilles tendon xanthoma- familial hypercholesterolemia 2. xantheJasmaA. yellow plaque on eye] id B. consider type II hyperlipidemia 3. arcus senlliaA. rim of white around the outer part of the cornea B. consider increased LOL if a young patient or normal age-related change if older patient 4. eruptive xanthomasA. yellow papular lesions over the body B. due to increased triglyceride: type IV or type V
*"
39
Note: This material i~copyrighted. AU rights reserved.
'Most 1. 2. 3. 4. 5.
common vessels involved in atherosclerosis in descending order: abdominal aorta- no vasa vasorum below orifices of renal arteries
coronary artery poplitealartery
descending thoracic aorta Internal carotid
Atherosclerosis: 1. reaction to injury theory- fact-ors damaging endothelial cells A. chemicals in cigarette smoke e.g., carbon monoxide) B. LDL/oxidized LDL C. previous Chlamydia pneumoniae infection D. increased serum homocysteine: folate deficiency MeC 2. fibrous plaqueA. pathognomonic lesion of atherosclerosis B. smooth muscle cells with CH deposits beneath intima C. macro phages with CH deposits General complications of atherosclerosis: 1. aneurysm forn;tationA. weakening of vessel wall \ ith outpouching due to arterial pressure (1) Law of Laplace states that wall stress increases with increased radius (2).'. all aneurysms must enlarge as wall stress increases 0 V~Sol{ V(fsa,R,(>( t>'1 ~ al1domiul'l!1 aoI1tic anc_urysm:s ia-the Me zype (picture on US_MLE'~ {LeM,{ ~fe~~ C.abdominal aorta is the Me site for atherosclerosis . -ft. \j,~J;I! 2. coronary artery disease- ischemic heart disease . . b {j_e~ A. angina: Me manifestation {<iN e t ~.~ B. acute myocardial infarction l'\'I.Qe.e. I Co sudden card iac death: H- JdtSlI.T l",l/e (1) death. within 1 hour f)IJ//oJ 'bJ '5.tIf1 (2) severe coronary artery atherosclerosis (3) usually nothrombosis present D. chronic ischemic heart disease 3. peripheral vascular diseaseA. predominantly lower extremity disease: may-hear a bruit over involved vessel
qr
WChI
e(/~/'r
f.-til y
~
I
::,
B.
clinical:
(1) pam
(2) (3)
(4) (5) (6) (7) (8)
pulselessness paresthesias
pallor paralysis gangrene: common in diabetics intermittent claudi cation: pain on walking which is,reb eved by resting Lerichesyndrome: a. aortoiliac disease in male with fmpotence(hyp.ogastric arteries involved) b. claudication c. atrophy of calf muscles d. diminished/absent femoral pulses
40
Note: This material is copyrighted. All rlghts reserved.
4.
s.
circle of Willis diseaseA. cerebral infarction (1) usually pale infarct (2) Me type of stroke B. cerebral atrophy: (1) due to laminar necrosis of neurons in layers 3,5 and 6' of the cerebral certex (2) apoptosis of aeurcns- "red" neurons on Hand E stains C.atherosolerotlc aneurysms: e.g., basilar artery
vertebrobasilar
A.
artery disease-
6.
7.
8.
transient ischemic attacks: (1) dizziness (2) vertigo B. brain stem infarction internal carotid artery diseaseA. transient ischemic attacks: due ,to embolization of plaque material with neurologic deficits lasting <24 hours B. atherosclerotic stroke: (1) usually occur at bifurcation of the internal carotid artery (2) due to platelet thrombusoverlying atberoselerotic plaque (3) prevented by aspirin (4) ticlopidine used in aspirin allergy: problem With neutrop "ilia (5) control ofbigb blood pressure is tbe single most important factor that prevents strokes C. embolic stroke: (1) embolism of atheromatous plaque material or (2) emboli from left heart rena] nrtery diseaseA. rencvascularhypertension MCC of secondary hypertension B. elderly men with severe atherosclerosis and uncontrollable hypertension C. high renin hypertension D. epigastric bruit ,; celiac, superior and infeniur mesenteric artery diseaseA. small bowel infarction: (1) usually thrombosis/embolism involving superior mesenteric artery (2) bowel distention/pain (3) bloody diarrhea
B.
large bowel:
(1) (2) (3) (4) symptoms occur in splenic flexure area: overlap area of blood supply involving superior mesenteric/inferior mesenteric artery mesenteric angina: abdominal pain in splenic flexure areaJO minutes after eating ischemic colitis: splenic flexure pain + bloody diarrhea ischemic strictures: healing of infarction by fibrosis leads to large bowel obstruction from stricture formation J;.
Aneurysms 1.
of the vascular system:
abdominal aortic aneurysmA. Me type efaneurysm; 'Piel'ure ,o.IbUSMLE B. Me.in men over the age of 55 c. pathogenesis
'*'" U ~~:t):{rd
i5.f/..e. jolJ
"'f>~,.J~
IeIC
{tYlll~l~
411 e(1i€'4ItyS!'1-*;
4J
Note: This matertal is copyrighted. All rights reserved.
(I) (2)
weakening of the wall by atherosclerosis renal artery orifices
owing to no vasa vasorum below the
D.
Law of LapJace states that as the diameter increases the wall stress progressively increases: further enlargement and rupture is inevitable . (3) oftenacc6mpartied by a popliteal artery aneurysm: .d an ger of thrombosis requiring leg amputation clinical: (1) majority are asymptomatic (2) symptomatic: a. pulsatile mass with mid-abdominal to lower back pain h. abdominal bruit (50%) c. rupture Me complication rupture triad:
(3)
"If
2.
a.abrupt onset of severe b9;ck pain (most 'rupture into, the ,left .... retroperitoneum) -7' 111ft tlllnk:.f~:") hJl qo;cJq ;5 ~JNfalJ+u q+-~IS b. hypotension c. pulsatile mass E. diagnosis: (1) abdominal ultrasound is gold standard test (2) size and risk for rupture color the Rx berry aneurysmA. young or middle aged adults most commonly located at bifurcations of cerebra] vessels: e.g., anterior communicating artery with anterior cerebral artery C. pathogenesis: (1) most are congenital: not usually atherosclerotic in origin (2) vessels lack an internal elastic membrane and muscle wall at bifurcations of cerebral vessels D. associations: any cause of hypertension predisposes to berry aneurysms: (1) essential hypertension (2) adult polycystic disease (10-15%) (3) coarctation of the aorta (increased pressure in cerebral vessels) E. clinical: (1) headache (2) subarachnoid hemorrhage: a. severe, .Qccipital headache b. "worst headache I ever had" followed by a loss of consciousness F. diagnosis (1) CT scan/MRl as a screen (2) angiography confirms mycotic aneurysmsA. weakening of the vessel wall secondary to an infectious processes: (1) e.. ., septic embolism g (2) infeetive e9dQ.carditis (3) fungal vasculitis (Aspergillus, Mucor, Candida are vessel in aders) B. clinical (1) thrombosis (2) rupture
B.
3.
42
Note: Tbis material is copyrIghted. All rights reserved.
4.
syphiHtic
aneu
rysmmanifestation of tertiary Syphilis
A.
males 40-55 ys of age pathogenesis (J)
cardiovascul3r
B.
C.
weakening
leads to ischemia of outer adventrtiaJJmeciial tissue-a
of 8011a-) of the underl
T. pallidum produces endarteritis Obliterans (vasculitis with plasma" oell infiltrate), of vasa vasorum of ascelidiQg and transverse portion' of arch ofaorta
sUrface4 aneurysmal dilatation .of aorta-s
dila.tation of aortic valve ring-e
aortic:: regurgjLation-+
of the endothelial
scar with retraction
ing endothelial
tissue prodwcing "tree barking"
D,
clinical:
(1) (2) (3)
death from hearr fa'ilure or ruptllre with dilatation/hyPertrophyof left ventricle stretched
aortie regurgitation
respiratory difficulties
from ain.vay encroachment
brassy aorta. cough from left recurrent laryngeal nerve irritation:
by dijated
E.
(4) angina: due coronary arteria ostia narrowing by fihr:osis (5) bound rug pu lses (water ham mer p 1.'I1se) diagnosis (1) aortography
5.
(2)caJcifi'catjon in the dissecting aortic aneurysm- arch of aorta highly preciictive of a syphilitic aneurysm
A.
B.
mean age of 60-65 men> Women
C.
D. E.
Me catastrophic
patliogenesis:
disorder
Me aneurysm of ascending
(1) pathology:
8.
9f aorta
..aorta
elastic tissue fragmentation (95%)
b.
mucoid degeneraliotl,:
cystic
mediaJ I'lecrosis
(2)
c, 'Occurs in the middle and outer parr of the media associatioos:
F.
a, -4 Marian's syndrome (defect in fibrilJin) b.--=itEhlers-DanJos syndrome (defect in CoHagen) e, 4" pregnancy (increased plasma volume) d, copper deficiency (cofactor in Jy;syJ oxidase) e. coarctation of aorta. (wall stress) f. trauma cause of dissection; (1) )l':;:hypettension applies a shearing force to the intimal surface~ intimal tear usually within 10 COl of the aortic val ve-» (1) eventual sites of rupture: pericardJal sac (Me COD)
and progresses proximally and/or dist,ally
column of blood dissects under arterial pressure
through theru:eas of weakness
a.
43
Note: This material is copyrighted. All rights reserv.ed.
G.
H.
1.
J.
b. mediastinum c. peritoneum d. reentrythrough another tea! to create a double barreled aorta types of dissections (1) type A aneurysm: a. Me and worst type b. involves ascending aorta (2) type B aneurysm: begin below the subclavian artery and-extend distal] clinical: (1) acute onset severe retrosternal chest pain with radiation into the back (2) AV regurgitation: due to dilatation of aortic valve ring. by aneurysm (3) signs of cardiac tamponade (4) Lossof upper extremity pulse (5) stroke diagnosis: (1) increased aortic diameter on chest x-ray'{80%) (2) retrograde arteriography is gold standard test (3) overall long-term survival 60% patient profile on UBMLEL anterior chest pain, widening of the aortic root on echocardiograrn death in 3 days QYtamponade
Overview of venous system: superficial veins (e.g., superficial saphenous veins) drain into. the deep veins via eommu n ieating (penetrating)' branches. 2. valves preven blood flow from the deep into the superficial venous system- exception is around the ankles, blood flow is from the deep venous system to the superficial system
1.
Phlebothrombosis and thrombophlebitis: 1. pbJebothrornbosisthrombosis ofa vein without inflammation. 2. enous clots in descending order of frequency:
A.
deep vein in the caJI
3.
4.
B. femoral vein > C. popliteal vein D. iliac vein predisposing factors for phLebotbrombosisA. damage to the vessel endothelium (e.g., inflammation, varicose veins) B. stasis of blood flow (e.g., bedrest) c. hypercnagulability (e.g., oral contraceptives), clotting processA. begins in stasis areas such as the venous sinuses of the calf muscles and in the valve cusps B. platelets form the initial clot in the valve cusps C. developing clot extends beyond the next branching point at which juncture the clot becomes a venous clot (red thrombus) consisting of a mixture of RBCs and :fibri:Q D. venous clot propagates towards the heart inthe direction of blood flow: danger of embolization
5.
elinica1A. B. swelling pain, edema distal to the thrombosis development of varicosities and ulceration.
44
Note: This material is copyrighted. All rights reserved.
6.
7.
deep venous thrombosis (DVT) in the lower extremityA. produces deep venous insufficiency: post~phJebitic syndrome B. deep saphenous vein thrombosis leads taan increased venous pressure and increased blood flow to veins around the-ankles which communicate with the superficial system C. veins in the ankles rupture resulting: (1) stasis der atitis (swelling hemorrhage ulcers) (2) secondary varicosities in the superficial saphenous system complication of venous thrombosis includeA. thromboembolism: (1) potential for a pulmonary embolism with infarction (2) femor-al vern Me site for embolization B. thrombophlebiris C. varicose veins Doppler (duplex) uJtrason.ographyA. best-screening test for detection of deep venous thrombosis B. X-ray venography is gold standard test tbrombop.hlebitisA. B.
8.
9.
'iT'
pain and tenderness along the course of a superficial (hot deep) vein .causes: (1) MeC is superficial varicose veins (2) phlebothrombosis (3) intravenous catheters (4) intravenous drug abuse C. clinical: (1) palpable cord (2) pain, induration, heat, 'erythema 10. migratory thrombophleblns- subtype of thrombophlebitis: A. venous thrombi disappear at One site and reappear at another B. may be a paraneoplastic sign of underlying pancreatic cancer (Trousseau's sign) Varicose veins: 1. definitionA. abnormally distended, lengthened and tortuous veins associated with: (1) superficial saphenous veins: Me site (2) distal esophagus in portal hypertension (3) anorectal region (e.g. hernarrhoids) (4) left testicle (varicocele) superficial saphenous vein varicosities in women (1) primary varicose veins are due to a. valvular ineompetence (sentinel valve) b. weakened vessel walls c. positive famiJy history d. occupation ofthe individual: standing (2) secondary varicose veins:
B.
Me
a.
b.
damage of the valves from prey leus thrcmbophiebltls deep vein thrombosis.
or
45
Note: This material is copyrighted. All rights reserved.
Thoracic outlet syndrome: 1. defillition- abnormal compression of the neurovascular cornpartmenu in the neck 2. ca.llses-
A. B.
C.
cervical db spastic scalenus anticus muscle
positional changes in the neck/arms
Subclavian steal syndrome: 1. defmition- due to proxima! obstruction of the first port jon of the subclavian artery: 2. causes reversal of blood flow in tbe vertebral artery (produces cerebral ischemia) to supply blood to the arm Superior vena caval (SVC) syndrome: 1. secondary to extrtnaic compression of the SVC from a primary lung cancer (90%) 2. puffiness and blue to purple dtscolorstlon of the face, arms and shoulders 3, eNS findings of dizziness, convulsions and visual disturbances (congested retinal veins). 4. distended jugular veins Lymphatic disorders: 1. lympbatic vessels have an Incomplete basement membranetumor invasion 2. acute lym.phangitis~ A. jnf1ru:nmation of lymphatics ("red streak") B. Streptococcus pyogenes Mec: e.g., cellulitis 3. lympbedemainterstitial collection of lymphatic fluid due to: A. congenital disease: (1) Milroy's disease (2) Turner's syndrome B. blockage of the lymphatics: (1) radiation post-mastectomy (2 peau d'orange of breast in inflammatory carcinoma (3) filariasis 4. chylous effusioneA. collection of lymphatic fluid in a body cavity: B. containschylornicrons with TG plus mature lymphocytes C. causes of chylous effusions in pleural cavity: (1) MeC is malignant lymphoma (2) trauma to thoracic duct predisposes to Infection and
Benign/m.alignant vascular tumors and tumor-like conditions: 1. Sturge-Weber syndrome (SWS) syndromeA. port wine stain in the distribution ofthe ophthalmic branch ofthe.trigeminal nerve, B. eNS vascular abnormalities often located in the leptomeninges 011 the ipsilateral side: (1) calcify (look like railroad, tracks) (2) bleed (3) fecus for seizure activity C. mental retardation 2. hereditary bemorrhagic telangiectasia (Osler Weber Rendu d'ise.ase)A. AD disease: Me genetic vascular disorder B. small aneurysmal telangiectasias on the skln/rnucous membranes
46
Note: This matertalIs copyrighted. All rights reserved.
C. D. 3.
epistaxis GI bleeds: iron deficiency spider telangiectasiasA. small arteriovenous communications B. associated with hyperestrinism: (1) pregnancy (2) cirrhosis C. compression of the "body' of the spider causes the blood flow to the "legs' disappear: petechia do not blanch U MI:E~
to
4.
aagiomyolipomaA. hamartoma composed of blood vessels, muscle and mature adipose tissue
B.
5.
Me in-kidneys
C. association with tuberous sclerosis bacillary aogiomatosisA. infectious disease caused by Bartonella henselae and Bartonella quintana B. associated with AIDS: simulates Kaposi's sarcoma C. benign capillary proliferation an the skin and/or visceral organs D. silver stains identify them in tissue E. organism also causes cat scratch disease
6.
capinary hemangremaA. B. benign tumor/? hamartoma of mature capillary channels "strawberry type> cemrnonly seen on the face in newborns: (1) slightly raised, bright red lobulated vascular tumors (2)80% totally gone by 8 years (3) no treatment necessary . MLE cavernous hemangiomaA. Me benign tumor of the liver/spleen, and placenta (caned Cholangioma) B. may rupture in Iiver/spleen C. association with von Rippel-Lindau disease: (1) AD disease (2) cavernous hemangiomas of the cerebellum (cerebellar hemangioblastoma) stem, eyes (3) increased incidence.of renal 'adenocarcinoma and pheochromocytoma
7.
brain
8.
anglo areomaA.
B.
9.
sarcoma derived from vessel endothelium liver angiosarcomas: associated w:ith exposure to: (1) vinyl chloride (Me) (2) arsenic (3) thorotrast c. electron microscopy reveals Weieel-Palade bodies: (1) structural hallmark of endothelial cells, (2) contain von Willebrand's factor D, histochemical stains positive for factor VIII Kaposi's sarcomaA. malignant tumor arising from endothel ial cells (some debate on this origin) B. immunodeficiency variant develops in patient's taking immunosuppressi e drugs e.g., renal transplant patient)
C.
AIDS variant:
(1)
Me cancer in AIDS
47
Note: This material is copyrighted. All rights reserved.
(2) (3) (4)
(5)
(6)
AIDS-defi.rting lesion due to Herpesvirus 8 solitary to multiple red-purple lesions that progress from a flat lesion (macule) to a plaque to a nodule that ulcerates rnieroseopie: a. spindle cells (neoplastic elementjwith increased mitotic acti ity b. hemosiderin deposition locations: a. skin (Me location, picture On SMLE) b. mucocutaneous surfaeesforopharynx Me IDeation), c. viscerallocations (lung, 01 tract lymph nodes)
J
(7)
Rx:
A.
B. 10.
chemotherapy intralesional a-interferon
complicates
CU M:LE)
lymphedema due
to
Iympha.ngiosarcoma.mastectomy
chronic
modified'
radical
Large vessel vasculitis: 1. defini rio n: aorta to large/medium sized iR,USCU tar arteries 2. giant cell (temporal) arteritisA. >50 years of age B. women more often involved than men (2: 1) C. rnultifocal granulomatous vasculitiswith multinucleated giant cells D. primarily involves the temporal artery and extra-cranial branches of the carotid artery, E. clinical: ,(I) fever (2 unilateral headache along course of temporal artery: Me s· mptom (3) jaw elaudication (4) temporary/permanent blindness on ipsilateral side (5) polyrnyalgia rheumatica: B. above..signs and symptoms plus pain and morning stiffness (>30 minutes) in neck, shoulders, and hip b. ne elevation of serum CK unlike polymyositis F. lab: (1) elevated erythrocyte sedimentation rate (ESR): best screening test (2) definitive diagnosis: temporal artery biopsy G. Rx: steroids 3. Takayasuarterltts (pulseless disease.)A. Asian women <50 years old B. granulomatous vasculitis involving aortic arch vessels C. clinical: (1) absent upper extremity pulse (2) blood pressure discrepancy between extremities: low in upper 'and higher in lower extremities (3) Raynaud's phenomenon (4) visual disturbances (5) stroke D. diagnosis: angiography
48
Note: This material
is copyrighted.
AU rights reserved,
Cff>
Medium to small muscular artery vaseulltis: 1. polyarteritis nodosa (P AN)A. Me in middle aged men B. necrotizing immune vasculitis of small to medium sized arteries (1) immunocornplex vasculitis: ,'/1s jV<I{t ";'1 11. type ill hypersensitivity b. immunocomplexes may involveHBsAg (2) activation of neutrophils/monoeytes by anti-neutrophil cytoplasrnicantibcdies: p-ANCA type (3) release of enzymes by neutrophi Is contributes to inflammatiea C. pathology: (1) lesionsare in different stages of development: acute or healing stage (Z) focaJ vessel involvement leading to aneurysm (3)oeutrophilTcJeosinophilic infiltrate D. clinical associations: (1) )!BY antig.@emia: 30-40% (2) hypersensitivity to drugs: e.g., Intravenous amphetamines E. target organs (order of decreasing frequency) (1) kidneys: a. vasculitis/ glomernlon ephritis b. infarction (2) coronary arteries: aneurysms (3) liver: calcification of cystic duct artery (4) GI tract: bowel infarction (5) skin: painful nodules representing vasculitis 'in subcutaneous fat (6) lung: not commenly involved in classic PAN F. clinical () fever (2) pain in areas of involvement (3) multisystem diseasJ with infarction G. lab: (1) peripheral neutrophilic leukccytosis/eos inoph ilia (2) anemia (3) positive HBsAg (4) anti-neutruphl] cytoplasmic antibodies with perinuclear staining: p... ANCA (5) hematuria with RBC casts: glomerulonephritis
H.
diagnosis:
2.
(1) arteriography and/or biopsy of palpable noduiations in the skin or organ involved (2) renal failure Me COD Kawasaki DiseaseA. afflicts children <5 years old B. peak incidence in spring C. probable immune mechanisms involved D. transmural inflammation of vessels with neutrophils and mild fibrinoid necrosis: (1) leads to aneurysms/thrombosis (2) coronary artery vasculitis E. clinical: (1) MCC of anacute myocardial Infarctien in children
49
Note: This materialIs copyrighted. AU rights reserved.
(2) (3)
4)
F.
(5) lab:
erytheJ;,natou~rash of trunk and extremities with desquamation at finger tips mucosal inflammation: cracked lips, oral erythema erythema, induration, swelling of hands and feet localized lymphadenopathy
G.
(1) neutrophilic leukocytosis (2) thrombocytosis: characteristic finding (3) high ESR (4) abnormal EeG if myocard rt is present diagnosis: echocardiogram screen for coronary aneurysm
H.
Rx:
3.
(1) intravenous gamma globulin (2) steroids contraindicated: increase risk for coronary aneurysms thromboangiitis .obliterans <_Buerger·.sdi~ease)~ ~1r!5 d.;~8?se. A. young to middle aged cigarette smoking males B. unknown product in tobacco smoke: toxins produce direct damage to endothelium C.iJ1f1ammatory vasculitis: (1) involves the whole neurovascular compartment of medium sized and smau arteries in- the extremities (2) thrombus in vessels contains focal neutrophilic microabscesses: vessels. eventually fibrose D. clinical: (1) claudication-in the feet or hands (2) Raynaud's phenomenon (3) distal gangrene of the digits often requiring amputation (common USMLE picture) E. diagnosis: biopsy F. Rx: early stages of vasculitis frequently cease 01] discontinuation of smoking
r:e=
Small vessel vasculitis: 1. definitionA. involves arterioles, capillaries and venules B. small vessel vasculitis (hypersensitivity vasculitides): (1) Ieukocytoclastic venulitis: vasculitis usually involves post-capillary venules (2) inflammation 'is at the same stage ill all vessels (unlike PAN): a. neutrophilic infiltrate
,1#
b.
nuclear debris
2.
c. fibrinoid necrosis (3) majority are type m immuuocomplex diseases (4) all present with "palpable purpura": purpura due to platelet abnormalities or non-immunologic weakness of small vessels is not palpable Heaoch-Schdnlein purpura (BSP)A. vasculitis in children B. immune vasculitis mostly occurring in children following an upper respiratory
Me
(1) (2)
Infection
19A-C3 immunocornplexes deposited in vessel walls 19A nephropathy (Berger's disease) may be part.ef the syndromecomplex palR_ab·le purp~a.cCimmonJy
f
C.
clinical:
(1) limited to the lower extremities/buttocks
~ll f
Ifr_'"
'e(' --
r\h\IV1~
(01' kt JerD$JDrJ
50
Note: This material
is copyrig'hted.
All rights reserved.
(2) (3)
(4) D.
lab: (1) (2) (3)
polyarthritis abdominal pain: sometimes with melena renal disease: hematuria due to focal proliferative glomerulonephritis
).
neutrophilic leukocytosis normal platelet count increased 19A E. Rx: steroids autoimmune disease and vasculitisA. irnmunocornplex vasculitis B. types of autoimmune disease: (1) SLE (2) rheumatoid arthritis
(3)
C. target (1) (2) (3)
progressive systemic sclerosis
organs: skin kidneys brain
4.
serum sicknessA. prototype of systemic immunocnmplex disease B. soluble immunocomplexes duetoantigen excess
C. particularly common antitoxins: antibodies in the Rx of rattlesnake envenomations are synthesized against foreign antigens with horse-based followed by the
formation of imrnunocornplexes with 'further exposure to antitoxin
D. cllnieal: (1) fever (2) urticaria (3) generalized lymphadenopathy (4) arthritis (5) glomerulonephritis serum sickness-like prodrome in HBV and HeV
E.
MisceUa neons vaseulitid es: 1. Wegener's Granulomatosis (WG)A. childhood to middle age: mean age of 40 B. necrotizing granulomatous inflammation: (1) upper/lower respiratory tract (2) necrotizing granulomatous vasculitis in kidneys (3) anti-neutrophil cytoplasmicalltibodies (c-ANeA
type):
activate neutrophils/
monccytes with subsequent vessel/tissue damage
C. clinical: sinusitis (1) (2) saddle nose deformity:
(3) (4)
nasal cartilage destroyed b. absent nasal hairs upper airway collapse
B.
lung disease: a. recurrent pneumonia b. large angioceutrtc densities
OD
x-ray
51
Note: This material. is copyrighted. All rights reserved.
D.
E.
diagnosis: biopsy
lab: (1) neutrophilic/eosinophilic leukocytosis (2) anti-neutrophil cytoplasmic antibodies with diff-use cytoplasm ie pattern (cANCA): speclfic for Wegener's and marker of disease activity
(5)
necrotizing glomerulonephritis:
renal failure
F.
Rx
(1) and transitional cell
2.
3.
cyclophosphamtde: danger of __@n1orrhagic cystitis carcinoma (2) steroids (3) high mortality if left untreated Iymphoma.toid granulomatosisA. similar to Wegener's granulematosis, B. differences from WO: (1)absen ce of upper respiratory in vo Ivement (2) progresses to a malignant lymphoma in 50% of cases Rayoaud's pbenomenonA. arterial insufficiency Of the digital vessels (1) primary disease (rare) (2) most often secondary to other diseases
B.
pathogenesis:
(1) association with collagen vascular disease:
9.
SLE
progressive systemic sclerosis (first sign): starts as vasculitis and ends with fibrosis CREST syndrome: • of vessels
b. c.
•
• • (1)
galcinosis of finger tips/gentrornere :Q.aynaud's phenomenon esopbageal motility prob ems !Clerodactyly (-fq/~.·1 .4'1t!'.e:.)
antibody
• .!el'angiectasia associaticn with cold reacting (IgM) antibodies/globulins:
3.
C.
cryoglobulinemia: usually 'elderly patient With rheumatoid patient with HCV b. cold agglutinin diseases (3) other associations: 3. thromboangiitisoblitesans b. Takayasu's arteritis c. ergot poisoning (vasoconstriction) d. thoracic outlet syndrome clinical: (1)
arthritis or
4.
cold temperatures.and stress are stimuli that may trigger tile color changes of the fingers-» white-» blue-» red (2) ears and nose cyanotic (3) often relieved by warmth infectious vasculitisA. fungal vasculftis: vessel invading fungi:
(1)
Candida
S2
Note: This material is copyrighted.
All rights reserved.
(2) Aspergillus (3) Mucor species B. Rocky Mountain spotted fever: (1) rickettsial disease caused by Rickettsia rickettsiae (2) transmitted by the hard tick Dermacel"lteJ' andersoni (3) organisms invade vessel endothelium of arteria J.esiveuuJ es: (4) inflammation and rupture of weakened vessel-s classic petechial lesions begin on the sol$ts and Plllms ofhand----7 s read to, trunk (centripetal spread (5) classic triad: 4 -;,f.trA'-ts DAJ a. rash 1'10 (~ --/r:.""f.<t!.,( b. fever c. history oftick bite C. dissemiuated meningococcemia (Neisseria meningitidis): (1) smart vessel vasculitis associated with capillary thrombosis and petechial hemorrhages (2) sepsis precipitates DIC (3) Waterhouse Frideeichsen's syndrome: acute adrenal insufficiency due to hemorrhage D. disseminated gonococcemia (Neisseria gOllorrltoeae) (1) small vessel vasculitis located on the hands wrist and feet (2) septic arthritis: usually knee (3) CS-C9deficiencies E. viral vasculitis: (1) hepatitis Band C: immunocomplex (2) rubella F. infective endocarditis': lmmunocomplex vasculitis: (1) Roth's spots in retina (2) Janeway's lesions on hands (painless) (3) Osler's nodes 011' hands (painful) (4) glomerulonephritis ~ IT: 'MI:E scenarios oOD V cuiar disease: 1. IiIO t ayrpmpriate Rx for an elde~ly woman with it ifieaaacbe JocsIized to tlle_.side of her bead accomp_aoledffy diffuse.muscle aches ana pains and 3.0.ele¥ated ESR A. temporal arteritis with polymyalgia B. Rx with corticosteroids 2. weigJit IiJiteLwitlJ,weakness in the hand numbness -and al)sent..pulseA. thoracic outlet syndrome B. scalenus anticus muscle spasm or cervical rib compresses the subclavian artery and
ff:'t!'iY;--,.:y i+.< !(!Vi(
brachial plexus
3. 4. rpicfilre of h,mangioma on face of -a ehiFd~ leave it alone calcification of d'igital vessels- diabetes mellitus Mt:C"ofan artenloveneus fishila- trauma: A. usually a knife injury B. may cause high output cardiac failure
5.
Classification of hypertension: 1. essential hypertension95%
2.
secondarybypertensionA. renal disease:
53
Note: This material is copyrighted. All rights reserved.
(1)
renovascular disease: MCC secondary
hyperteo ion
B.
C. D.
E.
F.
G. H.
a, elderly male with atherosclerosis b. middle aged female with fibromuscular hyperplasia (2) renal parenchymal disease adrenal disease: (1) Cushing's syndrome (2) pheochromocytoma (3) Conn's (primary aldosteronism) parathyroid disease: primary hyperparathyroidism thyroid disease: (1) severe hypothyroidism: diastolic hypertension (2) Grave's d-isease: systolic hypertension vascular disease.coarctation of the aorta eNSdisease; (I) increased intracranial pressure (2) poliomyelitis gynecologic disease: toxemia of pregnancy: pregnancy induced hypertension drugs: (1) oral contraceptives (MCC in women in reproductive age): estrogen increases liver synthesis of angiotensinogen (2) alcohol (3) cocaine
Essential hypertension; 1. systolic blood pressure correlates with stroke volume 2. diastolic blood pressure correlates with state of contraction of total peripheral resistance (TPR) Ilr'teriol'esA. diastol ic blood pressure is the amount of blood in the arteries while the heart is filling up in diastole B. amount of blood in arteries is related to the arterioles Which control the TPR C. abbreviated Poiseuille's equation states that total peripheral resistance (TPR) :; v iscosity of b 16'0 dI(radi us 'of the arteriole)" (1) vasodiletation of'arterioles hasgreatest effect on lowering TPR (2) vasodilation of arterioles decreases TPR and decreases the qiastPjic blOI:l(:l pressure (3) vasoconstriction of arterioles increases TPR and increases diastolic blood pressure 3. MC type of bypertensionA. high incidence in African-Americans B. pathogenesis in most cases: (1) retention of sodium raises theplasma volume leading to ain, increase in stroke volume (increased systolic pressure) (2) sodium in smooth muscle cells of peripheral resistance vessels (arterioles) opens up calcium channels leading 'to vasoconstriction and an increase 111 diastolic pressure (3) African-Americans have low renin hypertension: due to an increase in. plasma volume C. pathology associated with hypertension: (1) concentric left ventricular hypertrophy:
54
Note: Thi material is copyrighted. All rigbts reserved. a. Me complication b. potential for left heart failure acute myocardial infarction: Me COD hyaline arteriolosclerosis: fl. insudatien of protein into walls-of arterioles by increased luminal pressure narrow vessel lumen b. produces small vessel ischemia nephrosclerosis in the kidneys: a. shrunken kidneys of hypertension b.cortical atrophy due to hyali ne arteriolosclerosis c. eventual proteinuria and chronic renal failure intracranial bleeds in the putamen area: due to ruptured Charcot-Bouchard aneurysms of lenticulostriate vessels lacunar infarcts: a. due to hyaline arteriolosclerosis b.pure motor or sensory strokes accentuated Az
(2) (3)
(4)
(5)
(6)
4.
clinicaJ-
Renovascular bypertension: 1. Me secondar . cause of hypertensionA. pathogenesis:'"
(l)atherosc1er'osis (2) flhrnmuscular
a.
of renal artery orifice in male hyperplasia of renal artery in a woman: hyperplasia of smooth muscle in arteries. narrow lumen
B.
c.
h. "beaded" appearance of arteries noted clinical: (1) severe hypertension (2) epigastric bruit
with arteriogram
(1)
(2)
laboratory:
(3) (4)
aetefll( ~ involved kidney h8§ increased renal vein plasma renin activity uninvolved kidney has suppressed renal vein plasma renin activity captopri I markedly increases basel ine p.1 asma reni 11 activity. a. used as a screening test along with a renal scan b. renal scan shows decreased uptake of affected kidney, decreased size of affected kidney, decreased excretion in affected kidney
1&
higb renin hypertension - b L.
I,
I. / (k]
If(
>(,..1 .J(~,t.,.(
J.t
;0"-A r
CF
Plasma renin activity (PRA) in different conditions: 1. sodium depletion-
A.
B.
increased PRA volume depletion stimulates renin release
2.
upright postureA. increased PRA
B. C. decreases venous return to heart-e decreases cardiac output-s- stimulation of renin
release
recumbent posture does the opposite: increases venous return-s increases cardiac
3.
output-e- decreases renin release catecholaminesA.
B.
increased PRA directly stimulate renin release
55
Note: This material is copyrighted. All rights reserved.
4.
j3-blockers do the opposite captopril (ACE i.nhibitor)A. increased PM B. excellent screen for renovascular hypertension. (1) (2) see exaggerated levels post-stimulation owing to block of angiotensin II and loss of negative feed back on ren in potential for renal failure if bilateral renal artery stenosis is present (USMLE); a. angiotensin IT is primary modulator of intrarenal blood flow in both kidneys
C.
5.
6.
b. ACE inhibitor reduces AT II levels and causes renal failure LasuA. increased PM B. stimulation ofMA system from velurne.depletion aldosterone blocker (spirenolactonsjA. increased FRA B. volume depletion from sodium loss C. loss of negative feedback of aldosterone on renin renovascular bypertenslon- increased PRA malignant bypertension- increased PRA
7. 8.
9.
10.
11.
young hypertensivesA. increased PRA B. sympathetic ,nervous system overactivity African-American hyperten,sivesA. decreased PRA B. increased blood volume from sedium. retention C. reason why diuretics are first choice in Rx sodium overload/primary aldostero,n,islJ1A. B. decreased PRA increased blood volume from sodium retention decreased PRA ... volume overload SUppresses renin
U.
elderly hypertensive~A. B..
Concentric bypertrophy of left ventricle: due to increased afterload1. essential hypertension MCC 2. aortic stenosis Hypertropbyand dilatation of left ventricle: due to volume-overload of the ventricles1. aortic or mitral valve regurgitation 2. left to right shunts with increased return to left heart 3. aortic valve ring dila.tationA. dissection B. aortitis mitral valve dug diIatation-
4.
left heart failure
Left heart failure (L1IF): 1. mechanisms of heart CailoreA. diminished ventricular contraction: (1) ischemia,MeC (2) replacement by fibrous tissue
56
Note: This material
is
copyrighted. AU rights reserved.
B.
C.
D.
(3) myocarditis non-compliant (restricted filling): (1) amyloidosis (2) iron overload (3) glycogen, in Pompe's disease increased workload: (1) increased afterload (2) increased preload (VOhll1W overloaded) blood builds up behind the failed left heart: increase in left ventricular volume/pressure-s increase in left atrial pressure-sincrease in pulmonary venous pressure-s hydrostatic pressure overrides pulmonary capillary edema
oncotic
pressure-»
pulmonary
2.
clinical findingsA. B. D. E.
c.
F.
G.
B.
I.
J.
symptoms outnumber -signs decreased cardiac output: forward failure dyspnea: stimulation of J receptors in pulmonaryinterstitium pulmonary edema: due to increased pulmonary venous hydrostatic pressure left ventricular dilatation: (1) volume overload (2) Frank-Starling mechanisms at work left-sided 83 heart SQuad: volume overloaded left ventricle left-sided S",heart sound: decreased cempliance mitral regurgitation: (1) stretchingof mitral valve ring (2) pansystolic murmur atapex with radiation into axilla (increases with expiration) paroxysmal nocturnal dyspnea and/or pillow orthopnea at night: (1) increased venous .return a.t night due to lack of gravity effect when lying down cannot be handled by the left heart-s blood backs up into the lungs (2) standing up or placing pillows under the bead decreases venous return to the heart cough: (1) sputum rusty colored from alveolar macrophages phagocytosing RBCs (2) "heart failure" cells
due to decreased
3.
systolic dysfunctinn type ofLIDL
A. contractility: (1) ejection fraction (EY) <0.40 (2) EF ~ stroke volume/left ventricular end-diastolic volume (3) normal EF = 80/120 = 0.66 causes: ischemic injury Mec
B.
C.
Rx:
(1)
4.
use of inotropic agents (e.g., digitalis) (2) decrease afterload with vasodilators (e.g., ACE inhibitors) diastolic dysfunction type of LRFA. due to decreased compliance of left ventricle: (1) places increased load on the left atrium (2) pulmonary edema common
57
Note: This material is copyrighted.
An
rights reserved.
(3)
B. (1) (2) (3)
EF >0.40
causes:
5.
C. USMLE scenariosA. chest (1) (2) (3) (4)
left ventricular hypertrophy restrictive cardiomyopathy hypertrophic cardiomyopathy Rx: increase preload by slowing heart rate (e.g., calcium channel blockers, !3-bJockers), x-ray appearance in heart failure: prominent congestion of blood in the upper lobes perihilar congestion: 'bat-wing configuration Kerley lines: represent fluid in the interlobular septa patchy interstitial and alveolar infiltrates
(5) B.
pleural effusion
microscopic appearance of lung in heart failure: (1) pulmonary edema: transudate (2) alveolar rnacrophages with hemosiderin ("heart failure" cells)
Right bear failure (RHF): 1. mechanisms similar to left heart failure (L:HF)~
A.
LHF isMCC
2.
B. right ventricular infarction blood builds up behin.d the failed right heartA. increase "in right ventricular volume/pressure-» B. increase in right atrial pressure-s
C. D. E. increase in jugular venous pressure-s hydrostatic pressure overrides pulmonary capillary oncotic pressure-s dependent pitting edema + ascites signs outnumber symptoms decreased cardiac output: backward failure volume overload, of right ventricle right-sided Sl heart sound: volume overload right-sided S~ heart sound: decreased cornpllance tricuspid regurgitation: (1) stretching of tricuspid valve ring (2) pansystelic murmur at left parasternal border (increases with inspiration) congestive hepatomegaly: (1) nutmeg liver (2) increased LDBs isoenzyme (3) increased serum transaminases increased hydrostatic pressure in venous system: (1) ascites (2) dependent pitting edema (3) jugular neck vein distention
3.
clinicalfmdingsA.
B.
C. D. E.
F.
G.
H.
4.
Rx:
A. B. C.
decrease preload and afterload
ACE inhibitor decreases preload (blocks aldosterone) and afterload (blocks angiotensin TI); spironolactone added owing to eventua I Increase in aldosterone diuretics decrease preload
58
Note: This material is copyrighted. All rights reserved.
D.
restrict salt and water (decreases preload)
IDgh output failure: 1. mechauiems-A. increase stroke volume: (1) hyperthyroidism (2) increase blood volume B. decrease blood viscosity: severe anemia c. vasodilate peripheral resistance arterioles (decrease total peripheral resistance): (1) increases venous return to the heart (2) causes of vasodilatation a. thiamine deficiency b. endotoxic shock in early phases c. metabolic acidosis D. arteriovenous fistula: (1) direct cerutnunicarion of arterial with venous system bypasses the microcirculation (2) increases venous return to. the heart (3) causes of A V fistulas: a. surgically produced in radial artery for renal dialysis b. ,trauma: • knife wound usual cause • pressing afferent vessel causes slowing of heart rate (Branham's sign) • hear bruit over the soft tissue mass c. Paget's disease of bone: arteriovenous fistulas develop ill soft bone 2. tl.sMLE correlatlcn of higb output faJilur:e withPo\seuille's equ,ationA. abbreviated equation: total peripheral resistance (TPR) = viscosity of blood'(redius of the arteriole)" B. vasodilatation has greatest effect QIl lowering TPR: see above causes C. decreasing viscosity, degreases TPR: see anemia
U:ML
1.
ques.tion.ot fetal circUlation (lWow this vel')' wdl): MLE question On w'h-ati:s- lower in umbilical artery blood of a norm_a} fetus ersusmaternal arterial: blood- answer is P02 is lower in the umbilical artery A. 'chorionic villus in the placenta is the primary site of OJC02 exchange for the fetus B. normal alues in pregnancy: (1) normal hematocrit (Hct~ is ~35%
(2)
C. D.
O2 saturation ,(Sa02) is -98%
illi of the
E.
(3) arterial POl is - I05 mm Hg fetal Hb has a high affinity. for O2: ideal for gas exchange in chorienic placenta fetal laboratory. parameters: (I) Hctof-55%: a. higher than mothers b. high Hct also increases viscosity (2) increased percentage of HbF (70% at birth) (3) left-shifted ODe from HbF umbilical ein has an Sa02 -80% arid P02 30-35 mm Hg: (1) it has the highest amount of oxygen in the fetal circulation
59
Note: This material is copyrighted. AU rigbts reserved.
(2) (3)
(4) (5)
it carries 'oxygenated blood from the chorionic villus to the fetal -50% of the umbilical vein blood (Sa02 of ~80%) mixes with blood (Sa02 of 26%), which contains portal vein blood a. Sa02 after mixing of umbilical vein blood Witb sinusoidal b. sinusoids are drained bythe hepatic vein, which empties vena cava (IVC) remaining umbilical vein blood enters ductus venosus: drains
liver hepatic sinusoid blood is -67%
into the inferior
directly into the
(6)
(7)
IVC S,aOl before entering the fetal right atrium is -67%: most IVC-derived blood is directly shunted through 9 patent foramen ovale into the left atrtum (SaOz -60%) most SVC-derived blood enters right ventricle: a.. fetal pulmonary arteries are hypertrophied from chronic vasoconstriction secondary too a low fetal POi b. most b100d entering the pulmonary arteries is shunted into the patent ductus arteriosis and from there into the descending aorta right to left shunt): placenta-derived prostaglandin (POE\) keeps: patent ductus open c. descending aorta 8802 is -58% and theP02 is 20-23 rum Hg blood in the aorta flows towards the placenta via two umbilical arteries, which
rvc
havea-3.
lower PO~ (20-23 mm Hg) than maternal arterial blood (P02 -105 mm
Hg).
b. c. higher 02: affinity than maternal arterial blood, owing to the presence of more HbF in the fetal RBCs, which left-shifts the ODC greater O2 capacity than maternal arterial blood (HbF has a higher affinity for O2 than adu 1t HbA)
Congenital heart disease (CBD) and what oxygen saturations would be in each type: see schematics of all the CHDs 1. step up of oxygen is compatible with a Ieftto rig_ht shunt- oxygenated blood (Sa02 95%) from the left heart enters unoxygenated blood (S302 75%) with a step up of 0, to ~'80% in the right heart J> 2. step down of oxygen is compatible witb a rigbt to left shun,t-uliloxygenated bleed (Sa02 75%) from the right heart enters oxygenated blood (SaOl 95%) with a step down of 01 to -80% in the left heart 3. Eisenmenger's syndromeA. excess blood in the right heart from a left to right shunt causes volume overload, " hich produces: (1) pulmonary hypertension (2) right ventricular hypertrophy B. reversal of shunt occurs when right ventricular hypertrophy overrides left ventricle pressures: patient develops cyanosis (called cyanosis tardive) 4. ventricular septal defect (VSD)A. Me congenital heant disease: (1) usually spontaneously correctsitself (2) defect in the membranous septum {3) associated with criduchat.tpertial deletion of chromosome 5) and trisomy 18 B. initiaUya left to right shunt through a defect in the membranous septum: (1) step up of O2 to 80% in the right ventricle and pulmonary .artery
60
B
F'UlmOriary hypertension (fllH)
PDA leiHoright shunt first, 1l'1ef;) rigntto-:left with PH "
Systemic pressure to Intraoranlal Nessels + st.ibclavlan aJ1ety
t Diameter
AV
of Ao' dilates ring
1 .....
....
/"'--"'
rve
RibRib notching ~
----
Intercostal
artery
FIGURE 10-2. Schematla of congenital heart disease. (A) represents a ventrIcuLar septa! defect (B) an atria! septal d~fec~, (f:J a patent ductus arteriosus (PDA), (D) an adult coarctation of the aorta, (E) tetralogy oi Fallot, and (F) transposition 01 the great vessels. Ao. aorta; ASD, atrial septal defect; AV,aortic valve; DA, ductus arteriosus; NC, Inferior vena cava; LA, left at.rlum; LV, left ventricle; LVH, lett ventricular hypertrophy: MY. mitral valve; PA; pulmonary artery; PDA, patent ductus arteriosus; p.v, pulmonic valve; RA, right atrium; RV, right ventricle; R'\r1o-I, right ventricular nypertrQphy; SVC, superior vena c.ava; TV, tri~uspl~ valve; VSD, ventricular septal delect.
LefHO-rigt'lt shunt !Ilrough
PDA
Subpl;llmonic stem;ilsis key to cyanosis
versus acyanosls
,Right-to-left shunt through VSD
Right-la-left shi.mt through VSD
Note: This material is copyrighted. All rights reserved.
5.
6.
(2) volume overload of right heart may lead to Eisenmenger's syndrome atrial septal defect (ASD)A. MC adult CHD B. association with fetal alcohol syndrome C. initially-a left to right shunt through a patent foramen ovale (1) step up of O2 to -80% in the right atrium right ventricle, and pulmonary artery (2) volume overload of right heart may lead to Eisenmenger's syndrome D. fixed spl j,tting of Sl patent ductus arteriosus (PDA)A. association with congenital rubella B. initially a left to right shunt from the aorta to the pulmonary artery through the ductus arteriosus: (1) step up of O2 to,-80% in the pulmonary artery (2) left atrium has 95% SaOl (3) volume overload of right heart may lead to Eisenmenger's syndrome: a. pulmonary artery empties unoxygenated blood into the aorta (step down in SaO.) b. unoxygenated blood enters aorta distal to the subclavian artery c. patient is pink i11 the upper extremities and c..anotie in the lower extremities
d.
ealled differential cyanosis
7.
8.
tetralogy of FaIlotA. Me cyanotic congenital heart disease B. tetralogy includes: (1) overriding aorta: least common anomaly (2) VSD (3) infravalvular pulmonic stenosis (4) right ventricular hypertrophy C. cyanosis depends on the degree of pulmonary valve stenosis: (1) acyanotic at birth, if the stenosis is not significant, since most 0 the unoxygenated blood enters the pulmonary artery for oxygenation in the lungs (2) cyanosis is present at birth if the stenosis is significant, since the majority .of blood is shunted from right ventricle into the left ventricle and out the aorta D. preselI.Cle of an AsD and PDA,are. c:ardiopt..bteetlve (lJSMLE); (1) left to rigbr shunt of ASD adds oxygenated blood into RA and steps up rightsided 8a02 (2) left to right shunt ofPDA takes unoxygenated blood in the' aorta and dumps the blood into the pulmonary artery for oxygenation in the lungs, complete transposition of the great vesselsA. association witb maternal diabetes B. usually a PDA, ASD, and VSD are present C. pathophysiology: (1) venous blood normally .emptie s into the right atrium via the vena cava CSaOt 75%) (2) oxygenated blood (SaOl 95%) normally enters the left atria, via the pulmonary vein (3) the aorta is transposed and empties the right ventricle (4) the pulmonary artery Is transposed and empties tbe left ventricle (5) oxygen saturations are as follows:
61
Note: This material is copyrighted. AUrights reserved. step Up of Sa02 to -80% in right atrium as oxygenated blood from the left: atrium empties into the right atrium through the ASD right ventricle with Sa~ -80 is emptied by the aorta (patient has cyanosis) some right ventricle blood is shunted right to left through _aVSD into the left ventricle (step down of Sa02 to 80%) left ventricle is emptied by the pulmonary artery for oxygenation ,in the lungs only - essel with Sa02 of9S% 1S the pulmonary vein only chamber with Sa02 of 95% is left atrium
a. b. c. d.
e.
f.
(ffr
Pestductal coarctation: 1. constriction of aorta is distal to the Iigamentumarteriosnm 2. clinicalA. proximal to the aortic constriction: (1) systolic murmur between the shoulder blades (2) increased blood pressure/musculature in upper extremities (3) dilatation of proximal aorta (subject to a dissection) (4) dilatation of aortic valve ring with aortic regurgitation (5) increased incidence of congenital bicuspid aortic valve (6) increased intracranial blood flow: circle of Willis vessels aneurysm formation and rupture B. distal to the aortic constriction: (1) decreased blood 'pressure/musculature oflower extremity
prone to berry
(2)
(3)
leg claudication from ischemia
of
C.
D.
decreased renal blood flow leads to diastalic hypertension: activation renin/angiotensin/aldosterone system collateral circulation: (1) intercostal arteries (rib notching) (2) superficial epigastric artery anastomoses with internal mammary artery Turner's syndrome: preductal coarctation that is symptomaticat birth
r:r
lJSMLE nenarioS' on CBD1. in Ka.rm,geQer\s syndt'om~ (situs inversus, immotile cilia syndrome) 1 ere -trTaDposition,: the heart is totaUy normal but is located on the right side 2. ehm:ber with the hig}est PO;l in aPDA leftatrium or Iefn ventricle or.aorta 3. pulmomlF,Y artery SaOa in a JPn - Step up of Sa.02 to ~80%
no
r:'ir
Major coronary artery risk factors (r ational Cholesterol Education Panel 1993): 1. age is the most important. overall risk factorA. male ~45 y old B. woman ~55 y old 2. family history of premature coronary artery disease (CAD) or stroke 3. current cigarette sm 0 king , enhances atherosclerosischemicals in smoke damage endothelial cells 4. hypertension with blood pressure ~140/9.0 DlJD Hg- CAD is Me COD in hypertension
5.
BDL <35 mg/dLA.
B.
C.
enhances atherosclerosis HDL is tbe major risk factor for women in their reproductive LDt is the major risk factor for males regardless of age
years
62
Note: This material is copyrighted. AJI rights reserved.
6.
A.
7.
8.
diabetes mettttusenhances atherosclerosis B. CAD is MC COD in diabetes LDL~160 mg/dLA. enhances atheroselerosis B. oxidized LDL poses an even greater risk for CAD than native LDL C. vitamin E neutralizes oxidized LDL IIDL :2:60mg/dLA. negative risk factor for·CAD B. subtract 1 risk factor from the above major risk factors
Factors responsible fOT myocardial O2 demand: 1. heart rate (HR)A. as HR increases, contracti lity increases: (1) more action potential per unit time (2) more 0:2, consumption B. reducing fIR, reduces O2 consumption C. Fffi > 180 bpm decreases the length of-diastole, which decreases filling of the coronary arteries and left ventricle 2. ventricularwall pressureA. an increase in wall pressure increases O2 consumption B. wall pressure increases when: (1) ventricles are hypertrophied or (2) when the radius of the ventricle is decreased owing to noncompliant muscle (most often the result of ischemia) Factors responsible for myoeardtal 01 supply: 1. coronary artery blood flowA. most importent factor B. coronary arteries till in diastole C. Clinical correlations: (1) decreased cardiac output in aortic stenosi causes less filling of coronary arteries and the potential for angina (2) aortitis in syphilitic aneurysm leads to narrowing of coronary ostia and angina (3) increasing heart rate decreases time for filling ofcoronary arteries (4) subendocardium gets the least amount of oxygen from the coronary arteries 2. left anterior descending (LAD) coronary arteryA. supplies entire anterior portion of left ventricle : (1) danger of rupture in a transmural myocardial infarction (2) prone to mural thrombosis in anterior myocardial infarctions B. supplies anterior 2/3rds of interventricular septum: (1) danger of permanent bundle branch blocks in anterior myocardial infarctions (2) permanent pacemaker is often required 3. rigbt coronary artery (RCA)A. supplies the entire posterior and inferior part of the left ventricle: responsible for epigastric pain in a myocardial infarction B. supplies the entire right ventricle: right ventricular infarction C. supplies posteromedial papillary musclerdangerof papillary muscle rupture and mitral regurgitation in myocardial infarctions D. supplies most of the blood to the arterioventricular node: danger of sinus bradycardia
63
Note: This material
is copyrighted.
All rights reserv,ed.
U M1m. "picture of coronary--vessel: description-
1. 2.
3.
4.
alberosclerosls:_ lit Iike.spaees d:y,trop-hic,ealcifieatlon: blue blot hes flbTofatty.:plaqy~: dlreetty. beneath endotllelium platelet thrombus: red-mass blocking tbelumen
Types of ischemic heart disease: 1. angina pectoris- MC type
2. 3. acute myocardial infarction- Me COD in the United States sudden cardiac death chronic ischemic heart disease
4.
Angina pectoris variants: 1. exertinnal (classical) an gin aA. MC variant B. severe fixed coronary artery atherosclerosis C. sudden onset of .exercise-induced substernal chest pain lasting 1-15 nun: relieved QY resting and/or nitroglycerin D. Ox: (1) exercise ECG (stress test) reveals ST depression: indicates BU hendccard ial
(2) ischemia confirmed with arteriography: intraccronary artery ultrasound recently used
2.
Prtntzmetal s anginasecondary to coronary artery vasospasm: ? vasoconstrictive effects of thromboxane A2 released from small platelet thrombi overlying non ..occlusive atherosclerotic plaques B. chest pain at rest C. Dx: (1) stress ECG reveals ST'etevatioD (2) represents transmural ischemia unstable (crescendo) aoginaA. severe, fixed, rsultivesscl atherosclerotic disease B. eccentric stenosis of vessels with disrupted plaques with thrombosis present: (1) nonocclusive thrombus (2) release vasoconstrictive compounds like rXA.2 C. frequent bouts of chest pain at rest D. Dx: (1) stress ECG is unsafe (2) -20% ,progress to an acute myocardial infarction in 3 m surgical procedures for Rx of coronary artery dlseaseA. percutaneous transluminal coronary angioplasty (FTCA)- Me procedure B. coronary artery by-pass graft (CABG) A.
3.
4.
Cause of throm bosis after angloplasty: localized dissection Vessels used in the CABG procedure:
1.
internal mammary artel'YA. best graft patency
2.
B. 90% patency rate after 10 years saphenous veinsA. 40-50% patency rate after 10 years
B. arterialization" ofthe vessels, fibrosis and occlusion
64
Note: Tbis material is copyrighted. All rights reserved.
Sudden cardiac deatb: 1. death within 1 h 2. severe atherosclerotic CAD 3. *usuaJly no occlusive vessel thrombus ~ 4. die of ventricular arrhythmia 5. association with smoking and non-Q wave Infarctions Chronic ischemic heart disease: repeated infarcts with replacement tissue leading to systolic dysfunction Gro s (G) and. 1icroscopic (M) changes in an acute myocardial 1. 0--4 hs- no G/!v1 chaage of cardiac tissue by fibrous (AMI):
infarction
2.
4-12bsA. no G change B. M shows coagulation necrosis after 6 lis A.
12-24hsG shows early paHar B. M Shows more advanced coagulation necrosis
3.
4.
5.
1-3dA. G - definite pallor B. M - neutrophilic infiltrate + advanced coagulation necrosis 3-7 dA.period of maximal softness B. time for ruptures C. rnacrophages move in toremove dead tissue
71--10dA. G is the same as 3-7 d B. M shows collagen deposition
6.
AMI complications: 1. arrhythmiasA. Me complication B. ventricular arrhythmias C. MCCOn 2. hea rt failu re- usually it) first 24 h 3. rupture-
A.
B. C.
D.
MC on the 3-rd to 7th day usually anterior waJl rupture with tamponade: thrombosis descending (LAD)cofonary posteromedial papillary muscle rupture: (1) right coronary artery (RCA)th:rombosis (2) acute onset of mitral regurgitation and heart failure ventricular septum rupture:
of the left anterior
4. 5.
(1) LAD thrombosis (2) left to right shunt mural throm bus- danger of embol ization pericarditis-
A.
first week in transmural infarction: (1) friction rub (2) fibrinous pericarditis
6S
Note: This material
is copyrighted.
AU rights reserved.
6.
7.
Dressler's syndrome: (1) autoimmune pericarditis 6-8 wks later (2) systemic signs/symptoms: fever, j oint pain ,friction rub ventricular aneurysmA. late complication B. precordial bulge during systole C. head failure is Me COD progn.osis- depends on ejection fraction unl ike sheets of pale staining
B.
SN[tE- picture of healed tnyoc.ardiBI Infar.C'fio:Q..blotchy fibrosi tissue as in a pale infarction
r:iJ""
Lab abnormallties in an acute m ocardiaJ infarction: 1. increase in CK-MBA. begins it! 4-8 hs B. CK-MB peaks in 2'4 hs C. disappears in 1.5-3 d D. reappearance QfCK-:MB >3 d is a reinfarction 2. increase in troponin-I> A. begins in 2-6 hs B. peaks in 15-24 hs
C.
D. E.
gone in 7 d
will likely replace LDH isoenzymes cannot identify reinfarction
3.
LDH 112 flipbegins to appear in 10 hs: (1) LDH2 is normally> LDHI (2) LDRI has highest concentration in cardiac muscle (3) AMI causes greater release of LDH,j than LDH21eading to an LDHu:! flip B. peaks in 2-3 d C. gone in 7 d D. mainly used toidentify AMI after 3·d increase in ASTA. begins 6-12 hs B. peaks 1-2 d C. gone in 5-9 d with changes on ECG in an acute A.
4.
r::iF'
Sequence or microscopic flndfngs and their correlation myocardial infarction: L peaked T waves- correlates with area of ischemia ill of the infarct 2. ST segment elevationA. correlates with in jured TIl vocardiaJ tissue .around B. roan:y of these cells die during reperfusion: (1) superoxide free radical s (2) called reperfusiorl injurv 3. symmetric T wave inversion- correlates with area of 4. Q wave- area of necrosis
the myocardial tissue at the periphery
area of necrosis
ischemia
66
Anda mungkin juga menyukai
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDari EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifePenilaian: 4 dari 5 bintang4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDari EverandThe Little Book of Hygge: Danish Secrets to Happy LivingPenilaian: 3.5 dari 5 bintang3.5/5 (399)
- The Skilled Helper Ch. 1-14Dokumen240 halamanThe Skilled Helper Ch. 1-14goongdeng0282% (28)
- Supplemental NotesDokumen21 halamanSupplemental Notesgoongdeng02Belum ada peringkat
- Goljan SlidesDokumen383 halamanGoljan Slidesusmle196% (23)
- GOLJAN HY QuestionsDokumen89 halamanGOLJAN HY Questionsgoongdeng02100% (6)
- Goljan's 100 PagesDokumen101 halamanGoljan's 100 Pagesabhaytyagi4130Belum ada peringkat
- Comprehensive Pathology ExamDokumen21 halamanComprehensive Pathology Examgoongdeng02Belum ada peringkat
- GOLJAN HY QuestionsDokumen89 halamanGOLJAN HY Questionsgoongdeng02100% (6)
- General PathologyDokumen233 halamanGeneral Pathologygoongdeng02Belum ada peringkat
- Goljan 5 Days (125 PGS)Dokumen125 halamanGoljan 5 Days (125 PGS)heartofanmd95% (21)
- General PathologyDokumen233 halamanGeneral Pathologygoongdeng02Belum ada peringkat
- Comprehensive Pathology ExamDokumen21 halamanComprehensive Pathology Examgoongdeng02Belum ada peringkat
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDari EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryPenilaian: 3.5 dari 5 bintang3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDari EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RacePenilaian: 4 dari 5 bintang4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Dari EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Penilaian: 4 dari 5 bintang4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeDari EverandShoe Dog: A Memoir by the Creator of NikePenilaian: 4.5 dari 5 bintang4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDari EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FuturePenilaian: 4.5 dari 5 bintang4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDari EverandNever Split the Difference: Negotiating As If Your Life Depended On ItPenilaian: 4.5 dari 5 bintang4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDari EverandGrit: The Power of Passion and PerseverancePenilaian: 4 dari 5 bintang4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDari EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaPenilaian: 4.5 dari 5 bintang4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerDari EverandThe Emperor of All Maladies: A Biography of CancerPenilaian: 4.5 dari 5 bintang4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDari EverandOn Fire: The (Burning) Case for a Green New DealPenilaian: 4 dari 5 bintang4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDari EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersPenilaian: 4.5 dari 5 bintang4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDari EverandTeam of Rivals: The Political Genius of Abraham LincolnPenilaian: 4.5 dari 5 bintang4.5/5 (234)
- Rise of ISIS: A Threat We Can't IgnoreDari EverandRise of ISIS: A Threat We Can't IgnorePenilaian: 3.5 dari 5 bintang3.5/5 (137)
- The Unwinding: An Inner History of the New AmericaDari EverandThe Unwinding: An Inner History of the New AmericaPenilaian: 4 dari 5 bintang4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDari EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyPenilaian: 3.5 dari 5 bintang3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDari EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You ArePenilaian: 4 dari 5 bintang4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Dari EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Penilaian: 4.5 dari 5 bintang4.5/5 (119)
- Her Body and Other Parties: StoriesDari EverandHer Body and Other Parties: StoriesPenilaian: 4 dari 5 bintang4/5 (821)