The Control of Canted Occlusal Plane Using TADs
Diunggah oleh
Phuong LeDeskripsi Asli:
Hak Cipta
Format Tersedia
Bagikan dokumen Ini
Apakah menurut Anda dokumen ini bermanfaat?
Apakah konten ini tidak pantas?
Laporkan Dokumen IniHak Cipta:
Format Tersedia
The Control of Canted Occlusal Plane Using TADs
Diunggah oleh
Phuong LeHak Cipta:
Format Tersedia
The Control of Canted Occlusal Plane Using TADs AAO Annual Meeting May 14 Chicago 10:40am - 11:00am room
375B Speaker: George Anka This lecture is based on the chapter of Thirty-Fourth Annual Moyer Symposium title: Microimplants As Temporary Orthodontic Anchorage. February 24-25, 2007 Ann Arbor, Michigan James McNamara Jr Editor Associate Katherine A, Ribbens Volume 45 Craniofacial Growth Series Department of Orthodontics and Pediatric Dentistry and Center for Human Growth and Development The University of Michigan Ann Arbor, Michigan The content of this paper has been revised to fit with the On-line lecture download system; therefore readers are invited to look after the original book for full text of the paper. Please understand that we have to remove many pictures so that this paper can be used as digital handout. We apologize for the inconveniences. Communication to the author: anka467@poplar.ocn.ne.jp About the author: George Anka D.D.S.,M.S. Northwestern University Orthodontics Graduate and Master of Science Private practice in Tokyo WIOC Advisor Committee member 12008 by the Department of Orthodontics and Pediatric Dentistry,School of Dentistry and Center for Human Growth and DevelopmentThe University of Michigan, Ann Arbor, MI 48109Publishers Cataloguing in Publication DataDepartment of Orthodontics and Pediatric Dentistry andCenter for Human Growth and Development Craniofacial Growth SeriesMicroimplants As Temporary Orthodontic Anchorage ISSN 0162 7279ISBN 0-929921-00-3ISBN 0-929921-40-0No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form by any means, electronic, mechanical, photocopying, re-cording, or otherwise, without the prior written permission of the Editor-in-Chief of the Craniofacial Growth Series or designate. Book can be purchased from: http://www.needhampress.com/ 2 TREATMENT OF THE CANTED OCCLUSAL PLANE George Anka and Duane Grummons Canted occlusal plane treatment has long been a challenge for orthodon-tists. Successful treatment can improve oral function, self-esteem and general quality of life for patients. The recent development of temporary anchorage devices (TADs) offers the possibility of achieving such im-provements by producing better symmetry without surgery. The applica-tion of this technique and its attendant devices is the topic of this chapter. This preliminary report of a method that further refines current techniques for the correction of occlusal plane discrepancies includes discussions of both the concept of treatment in growing and nongrowing patients and actual case histories (Caruso and Rungcharasseung, 2004; Devincenzo, 2006a,b). Facial asymmetry, including a tilted cant of the occlusal plane, is common in orthodontic patients. It is important, therefore, to diagnose facial asymmetry and then integrate its correction into routine orthodontic treatment, if possible. In order to provide our patients with the best facial form and morphology, we first must understand the etiology of an individual patients skeletal pattern; for example, does the patient have a dolichofacial or brachyfacial pattern? We also must understand the degree of difficulty of specific treatment regimens. In the past, we seldom have questioned whether a brachyfacial skeletal pattern could be modified to become less brachyfacial or whether the vertical growth direction in a patient with a dolichofacial skeletal pattern could be decreased by the time adulthood is reached. The inclusion of the TAD in orthodontic treatment protocols can improve the capability of treating these conditions resulting in enhanced oral function, optimal
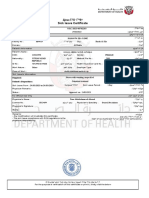
facial symmetry and better orthodontic treatment results. The TAD is a device that temporarily is fixed to bone for the purpose of enhancing orthodontic anchorage to allow the clinician to control tooth movement in three dimensions (Carano et al., 2005) and that subsequently is removed after use. In this chapter we will look primarily at how the TAD can control and influence vertical tooth move-ment as it relates to treatment of the canted occlusal plane, i.e., how it 3 Canted Occlusal Plane enables the clinician to control vertical growth in such a way as to influ-ence the height of the alveolar process through alveolar modification. To correct facial asymmetries in adult patients, the treatment of choice typically is surgery. However, because it appears that nonsurgical treatment of facial asymmetry is most successful in patients who are still growing, we believe that this new technique will be most useful for these patients (McNamara and Brudon, 2001; Grummons and Ricketts, 2004).The clinical use of this technique has just begun; therefore, we need longitudinal studies to prove its long-term stability and value. However, the present clinical findings are promising. This technique provides a practical approach to detecting and modifying occlusal plane cant asymmetry. By first using the frontal analysis of Grummons and Ricketts to de-fine the specific region or quadrant that contains the problem and compar-ing the results of this analysis to our clinical evaluation, we can correctly choose the region to be effectively treated. Currently in young patients, asymmetry is treated using a fixed bite plate to increase the vertical dimension and to relieve interferences that can be best cleared with fluoride releasing ionomer composites. These posterior composite bite lifters can be placed either on the maxillary or mandibular posterior teeth and are described as turbo (Grummons, 2006) or anterior fixed bite plates (Anka, 2004). This technique is not related to the TAD and will not be described in further detail in this paper. In the non-growing patient, the strategy and focus includes all four quadrants of the posterior alveolar bone in order to correct the asymmetry with less effect or burden on the temporomandibular joints. The most important factor in determining where the TAD should be implanted is the amount of interradicular space available. EXAMINATION AND EVALUATION OF OCCLUSAL PLANE ASYMMETRY Evaluation of facial asymmetry is performed using the Ricketts and Grummons frontal cephalometric analyses method (Fig. 1; Grummons and Rickets, 2004; Ricketts and Grummons, 2004; Grummons, 2006). This method compares right and left facial components to determine facial asymmetry. The patient is seated with the interpupillary plane horizontal to the floor. The use of dental floss on the midface is a simple way to create a vertical line relating the upper facial third at the crista galli (Cg) area and soft-tissue nasion (Na) region at the surface of the skin between the eye-brows to the inferior part of the nose (subnasale) that represents the anterior nasal spine (ANS) point. This reference line helps the clinician de -termine whether there is any mandibular shift or midline deviation of the maxillary teeth relative to the facial midline or the mandibular 4 dental mid-line. A frontal clear T template also is a good tool for determining which facial component is deviated (Grummons and Ricketts, 2004). Facial asymmetry involves both the horizontal and vertical aspects of the face; therefore, vertical and horizontal measurements are made so that the clinician can compare both the vertical and horizontal quadrants of the face. The results of such measurements can be compared to patient photographs and frontal cephalometric findings. The lateral aspects of asymmetry may affect the vertical asymmetry and vice versa, such as in a posterior unilateral crossbite. In this kind of case, the lateral transverse aspect should be corrected to effectively help correct the vertical problem. Figure 1. Grummons simplified frontal analysis 5
Canted Occlusal Plane6 Model Analysis The accuracy of patient casts mounted on an articulator depends on the location of the porions. When the porions are not symmetrical, the anterior-posterior and vertical positionings are affected. Therefore, the facebow transfer and the mounted models may not represent the true Frankfort Plane as an area that is normal and to which other landmarks should be compared. However, models do permit good observation of interarch interferences, spacial relationships between the upper and lower teeth, and relationships that can be reproduced outside of the mouth. Centric relations and centric occlusal differences influence the treatment plan. A unilateral crossbite of the posterior region will tip the occlusal plane on one side. A removable bite plate can be used to estimate how the mandible will posture and relocate and what its optimal position at rest will be. A fixed posterior bite plate can be used instead of a removable appliance (Fig. 2; Anka, 2004) while also correcting the transverse problem (Grummons, 2001a,b). Correcting the vertical alveolar height with the TAD is the next step. It is advisable to reduce the fixed bite plate gradually as the alveolar bone is corrected and the asymmetry is lessened. In addition, it is useful to know the width of the mandibular molars when planning treatment such as uprighting mandibular molars. It is advisable to make the mandibular arch the target arch (Grummons and Ricketts, 2004), as the width of the maxilla then can be adjusted to the width of the mandible. The transverse problem definitely affects the vertical problem; therefore, arch width and asymmetric relationships should be examined carefully. An anterior fixed bite plate can be used to continue monitoring the centric relationship as well as to correct overjet and overbite (Figs. 3 and 4). Radiography Measurements taken from both lateral and frontal cephalograms are necessary when diagnosing facial asymmetry. These data, combined with clinical evaluation recordings, will determine the treatment plan. The panoramic radiograph is a simple radiograph containing information about the ramus, condyle, and relationships between the upper and lower teeth (when taken in ICP). The overall condition of the nasal floor and its relation to the teeth, especially the posterior teeth, is important as the 6 TAD could penetrate the nasal cavity in an inferior portion of the maxillary sinus. While this not a contraindication for treatment using the TAD, avoidance of such an incident is important because it could cause chronic sinusitis or cause chronic sinusitis to become acute. The panoramic radi- ograph shows the interradicular space available, necessary information when choosing the TAD placement. Knowing the location of all first molars and canines is very important as it allows comparison of the original and post-treatment locations. We have chosen to use the reference Na-ANS (midsagittal plane) as described earlier. The line that extends to the lower border of the mandible provides information about the location of Menton (ME). We first determine the starting location from the maxillary jugal processes, JR to JL. We then analyze its location relative to a line perpendicular to the Na-ANS line and determine whether it is tilted. The area of JR-JL is not influenced by the method described in this chapter, but it is important to know whether there is a problem in this region initially. Next we analyze the maxillary occlusal plane. This is the area that treatment will influence significantly. Our method can decrease or increase the vertical height of the adjacent alveolar bone, with a maximum of 3 mm impaction potential, and 1 to 2 mm possible in extrusion. Mandibular occlusal plane maneuvering is less effective compared to that of the maxillae. TAD placement is restricted to the lower buccal side of the attached
gingivae, the vertical dimension of which is limited. At present, we are able to intrude the lower occlusal plane (< 2 mm) less than the upper. However, intrusion of up to 3 mm for the lower molars can be accomplished effectively and with relative ease using a skeletal anchorage device (SAS), which is a mini-plate type of TAD, with a relapse of 25% (Sugawara and Baik, 2002). With this limitation in mind, we must choose a realistic treatment plan based on our observations of the problem areas. The importance of frontal cephalometrics has been explained by Ricketts and other researchers (Hilgers, 1988; McNamara and Brudon, 2001). In spite of this, little has been done with the information available from frontal cephalometrics. Lateral cephalograms have been the more popular choice, possibly because clinical applications for frontal cephalometrics were limited. With the emergence of the TAD in clinical practice, 7 however, the use of frontal cephalometrics should become more widespread. MECHANICS RELATED TO MANAGEMENT OF THE CANTED OCCLUSAL PLANE IN THE MAXILLA: TRANSPALATAL ARCH PLUS HOOKS The transpalatal arch (TPA) plus hooks is very effective in controlling the sagittal direction of molars and premolars and the mesial-distal and/or intrusion-extrusion molar movements (Kyung et al., 2003; Lin et al., 2006; Park, 2006). The transpalatal arch consists of a lingual arch and a transpalatal bar the design of which is specific to treatment requirements for the posterior teeth. Figure 2 demonstrates distalization of molars combined with slight intrusion, a typical Class II, division I application. The hooks were attached on the cervical area of the lingual arch and the TADs were placed in the lingual alveolar process about 10 mm below the margin of the cervical gingival line of interradicular bone. This area was chosen as the safest area for TAD placement because the distance between the root of the second premolar and the lingual root of the first molar provided the most space. This location allowed for the needed distalization of molars without requiring reimplantation and reduced the possibility of collision between the TAD and the roots during tooth movement. Extrusion and intrusion requirements determine the location of the hooks and the direction of force from the elastic chains. The hooks can be placed anywhere on the vertical portion of the transpalatal wire. The higher the hooks are placed on the palate, the more extrusive is the force; the opposite creates an intrusive force. The direction of the elastic chain provides a combination of distalization and intrusion or distalization and extrusion. Figure 2. A TPA-plus-hooks configuration. The posterior fixed bite plate, made from blue glass ionomer cement, is used to determine centric relation in a patient with a 8 mandibular shift. The bite plate lessens the interference with the movement of the posterior teeth and prevents cuspal abrasion during treatment. Optimal location of the TAD is 3 to 4 mm from the gingival cervical line up to about a 12 mm distance. This distance varies from case to case and is based on the amount of bone within the alveolar process, which can be determined with either a panoramic or simple dental X-ray film. There is no doubt, however, that 3D CT imaging provides much better data. The midpalatal area is the most superior area that can be used when simple intrusion is the primary objective, as this involves a direct force from the palatal alveolar location to the first molar or to a point in front of the molar on the lingual aspect (Fig. 2). A final consideration is that the gingiva in the palatal region is better attached than in the buccal regions. Thus, the success rate is greater when implantation occurs in the palate. It is, therefore, the preferred site for implantation (Kyung et al., 2003; Park, 2006; Youn, 2006). On the left side of the TAD, an elastic chain is attached to the lingual arch in front of
the first molar and a second elastic chain is attached to the transpalatal bar. These mechanics provide intrusion and distalization of the left molar. On the right side, only the distalization effect is desired. Extrusion of both molars can be done with attachment to the omega loop area of the transpalatal bar, as seen in Figure 3. Figure 3. The anterior fixed bite plate is placed on the lingual side of the central incisors. Both intrusion and distalization occur on the left side, while only distalization occurs on the right side. Figure 4 shows the attachment of both TADs on the palatal alveolar side to the omega loop of the transpalatal bar, the result of which is the extrusion of the molars with some distalization. For pure extrusion of the molars, the TPA can be constructed with finger springs soldered to the band of the first molar and simply connected to the TAD to extrude the molar (Fig. 5). In the case seen in Figure 5, extrusion of the left and/or right molars can be controlled easily to adjust to the specific requirements needed to 9 correct the occlusal plane asymmetry. Figure 4. Connecting the TADs to the omega loop of the TPA will provide extrusive and distalizing forces. Figure 5. Pure extrusion of the posterior molars by means of finger springs. Asymmetry in the anterior region can be handled easily on the buccal side. Such intrusion of the anterior region requires placement of a TAD on the buccal area of the incisors, canine or premolar area, depending on the degree to which the occlusal plane is canted, on the smile dynamics, on the extent of gingival exposure, etc. (Figure was deleted) illustrates intrusion of the four maxillary incisors, with the forces applied on the right and left sides precisely controlled. Intrusion force should not exceed 200 g per side for the four incisors, because intrusion movement will compress the periodontal membrane in, which lessens the capillary blood supply that may cause the teeth to be prone to root resorption. Unilateral intrusion can be provided by engaging on one side only, but for effectiveness the placement of the TAD should be in a more anterior region such as between the canine and lateral. The extrusion of the one area can be achieved either with a finger spring (Figs. 4 and 14) or with an extension finger open-coil spring, which works for mesialization, distalization and/or extrusion, as seen in Figure 6. 10 In Figure 6, the extension compressed open-coil spring is made of a 0.028 round wire and has a coil spring that can be activated to propel and extrude the canine as the spring elongates. The results are extrusion and mesialization of the right canine and adjacent teeth. Figure 6. An open-coil finger spring works for extrusion and mesialization of the canine in a lateral open bite case. Maxillary Expansion: The transverse problem is related closely to the vertical problem (Hilgers, 1988; Grummons and Ricketts, 2004; Park, 2005). Maxillary ex-pansion can be generated by: 1. placing a Hyrax rapid expansion device on the maxillary first molars on both sides of the maxillary alveolar process. 2. placing a TAD directly on both sides of the alveolar regions and producing no tooth-borne anchorage; or 3. using a combination of the two methods, i.e., one side having tooth-borne anchorage and the other side having alveolar bone anchorage. MANDIBULAR INTRUSION In non-growing patients for whom adaptation of the condylar process and TMJ components is limited, it is necessary that the mandibular posterior teeth and alveolar height follow the same pattern of movement as their maxillary counterparts on the same side. For example, if treatment includes extrusion of the posterior maxilla, it also must include intrusion on the same side of the mandible (Bae and Kyung, 2006). The intrusion technique in the mandible has been demonstrated by Sugawara and
co-workers, with the plate type the most successful (Sugawara and Baik, 2002). However, it is limited with the use of the screw type TAD since we only can work in the unattached gingival area. However, improvement in this area will come soon so that we 11 can achieve intrusion effectively in the posterior region of the mandible. With the screw-type TAD, we also can achieve success (Carano et al., 2005; Bae et al., 2006; Lin, 2006). Figure 13 shows an elastic attached to the TAD between the premolar and the molar. The recommended force is less than 200 g. A lingual arch is necessary to prevent tipping of the posterior teeth. Figure 7. Intrusion of the posterior teeth with a triangle elastic attached directly to the TAD. Mandibular Extrusion: Both intrusion and extrusion of the mandibular posterior teeth require a lingual arch to stabilize the posterior teeth and prevent their tipping toward the direction from which the force is applied. The extrusion force should be about 200 g in order to withstand the bite force when extruding a group of posterior teeth. MIDLINE ASYMMETRY Asymmetry influencing the midline can be a challenge when correcting a canted occlusal plane in that the misfit of even one tooth to its opposite will affect the entire occlusal table and the two arches even if they function well. Cuspal interferences often will affect the lower jaw posture and the TMJ condylar position. This situation also affects the complete articulation and masticatory system of the patient. Midline correction is simpler if there is space available such as that provided in an extraction treatment plan. However, nonextraction patients (with the exception of third molar extractions) are increasing in number, and it is more difficult to correct midline asymmetry in these cases. The TAD can be helpful in resolving clinical anchorage problems, enabling molar distalization to become a routine procedure. 12 Figure 8. Extrusion of the posterior teeth using a finger spring. We have adopted the technique of extrusion in the mandible as advocated by Park (personal communication) An asymmetrical midline can be due to a canted occlusal problem. It also can be caused by treatment efforts to correct a canted occlusal table. As the arch of the teeth moves, the midline moves as well, creating an asymmetry of the midlines that probably was not asymmetric initially (Fig. 9). This phenomenon happens because the effect of our mechanics is limited to the alveolar bone area and not the basal bone itself. The center of resistance on the maxilla is on the mid-palate or above (the sinus itself); we must strive to correct the occlusal plane in combination with lateral movement of the entire maxilla to the right side in this example. In addition, there are some treatment choices, although very limited ones that can be used on the lower to compensate (note the midline correction of the mandible). Figure 9. Before (left) and after (right) treatment to correct the canted occlusal plane. Note the change in midline symmetry. Correcting the midline asymmetry includes the movement of all teeth within the arch from one side to the other (Youn, 2006). It may involve correcting one arch or both 13 arches. The choice depends on the clinical examination of the patient and the results of the frontal analysis. Maxillary midline correction is easier than correction of the mandibular midline. The reason for this is that the maxillary palatal bone provides a large area in which to place TAD devices and attachments. MAXILLARY MIDLINE CORRECTION The maxillary midline as well as the mandibular midline will have to move distally on one side and mesially on the other side as we relocate the whole dentition in one
direction. This unidirectional movement can be achieved with indirect force applications. A simple method for applying such a force is the use of a hook soldered onto the band of a molar; usually the first molar is preferred (Figs. 16 and 17). This can be accomplished on the palatal side or the buccal side, depending on the placement of the TAD itself. Palatal placement allows more range of movement and requires less frequent or no reimplantation. Although buccal placement is more popular at present, as the teeth move toward the TAD, collision between the teeth approaching the TAD can cause damage to the periodontal membrane and even the cementum itself, the result of which potentially could be ankylosis. Most of the time, this will not cause fatal harm to the tooth if recognized early. In the premolar area and anterior regions (incisors), buccal placement still is the location of choice. Patients generally are more comfortable having a TAD placed in the buccal side rather than in the anterior maxillary lingual side area. Speech disturbance and irritation of the tongue are the main reasons to avoid placement in this area. The least objectionable and most accepted placement is in the palatal alveolar bone area. Placement in the upper retromolar pad is a good choice, although the risk of TAD fracture during screw removal must be considered. The consequences of such problems are less when TAD placement is in the palatal alveolar bone compared to placement in other areas of the palate. The simplest design for distalization includes an extended arm. The length of the arm can be adjusted to the requirement of the elastic to be used for the power source (Fig. 18). This method is effective for short distance movement, but for longer distances, rotation to the lingual side can occur unless the main archwire is close to a full slot size wire. The other technique that can be effective is the use of a transpalatal bar and hooks, which will maintain the width of the molars as movement occurs. In the anterior region an auxiliary open-coil spring may be needed to provide a distalization force (Fig.13 ), which enhances the movement on the anterior buccal region, to the left in this case. The auxiliary called the propeller. 14 Figure 10. When extended arms are used to distalize the molars, a different amount of force can be applied to each side. Figure 11. Unidirectional movement: the left side of the archwill move distally and the right side will move mesially. - Figure 12. Left: An extended arm of 0.036 stainless steel wire soldered to the molar band. Right: A palatal side extended arm on a dental cast. Figure 13. Left: This patient was treated with an open-coil finger spring with a .016 x .016 rectangular wire. This devise name is "The Propeller" Right: Patient at the end of treatment. 15 MANDIBULAR MIDLINE CORRECTION In the mandible, the TAD is placed on the buccal area only because lingual placement would irritate the tongue for most patients. Use of the extended arm is the most frequently used and the simplest device compared to other devices. The opencoil finger spring is highly adaptable to the curvature of the arch, but it needs modification on the main archwire to keep the device from flaring to the buccal side and irritating the lower lip. Mesialization of molars in the mandible follows the same design as that used in the maxilla, i.e., with hooks soldered on the molars and connected to a TAD that is placed on the buccal alveolar bone, which usually located between the canine and premolar or between the second and first premolar.
Conclusion:
The application of indirect force when using TADs is a valuable treatment approach to correcting asymmetrical occlusal surfaces as it allows the control and direction of the forces needed in three dimensions.
We advocate using such devices as hooks, lingual arches plus hooks, extension arms, and finger open-coil springs in concert with TADs as part of this new technique. A treatment should be planned, the design of the indirect method TADs force of application then established and applied to the canted occlusion to correct the asymmetry and normalize function despite some dentoalveolar compensations. The AP Grummons simplified frontal analysis system used with TAD technology can quantify and locate the deviation and indicate in which direction the treatment should be directed to best improve the asymmetries. This new technique provides anchorage that was difficult to supply in the past such as that needed to treat asymmetric vertical dimension discrepancies. However, screw-type TAD implantation to the attached gingival area of the alveolar bone has a relatively high failure rate when used in the mixed dentition of young patients, considering the rapid cell turnover that takes place (Roberts, 2000). At present, this treatment is limited to patients who have a full dentition from first molar to contralateral first molar. The potential TAD patient should have completed the transition from mixed to permanent dentition. The best result are achieved by using the frontal cephalogram combined with clinical observations to define the problem; by thoroughly evaluating the treatment options made available by using these new TAD techniques; and by understanding the treatment limitations. All of these factors will help produce a positive treatment 16 outcome, i.e., the best possible facial balance and symmetry, the result of which is a more attractive face and functional occlusion. REFERENCES: Anka G. The management of noncompliance of Class II, division 1 extraction cases with jumping appliance forces DPR: A suggestion of the use of Gurin lock and anterior fixed bite plate. Orthodontia 2004;1:122-133. Bae S, Kyung H. Mandibular molar intrusion with miniscrew anchorage.J Clin Orthod 2006;40:107-108.Carano A, Velo S, Leone P, Siciliani G. Clinical applications of the miniscrew anchorage system. J Clin Orthod 2005;39:9-24. Caruso J, Rungcharasseung K. A Practical Guide to the Use of Miniscrew Anchorage.Coeur D Alene, 2006. Devincenzo J. A new non-surgical approach for treatment of extreme dolichocephalic malocclusions. Part 1: Appliance design and mechanotherapy. J Clin Orthod 2006a;XL:161-169. Devincenzo J. A new non-surgical approach for treatment of extreme dolichocephalic malocclusions. Part 2: Case selection and management. J Clin Orthod 2006b;XL:250260. Grummons D. Nonextraction emphasis: Space gaining efficiencies. Part I: World J Orthod 2001a;2:21-32. Grummons D. Nonextraction emphasis: Space gaining efficiencies. Part II: World J Orthod 2001b;2:177-189. Grummons D. Frontal facial asymmetry information. Presented at the Am Assoc Orthod meeting, Las Vegas, May 2006. Grummons D, Ricketts R. Frontal cephalometrics: Practical applications. Part 2. World J Orthod 2004:99-119. Hilgers J. Bioprogressive simplified. J Clin Orthod 1988;12:48-69. Kyung S, Hong S, Park Y. Distalization of maxillary molars with midpalatal miniscrew. J Clin Orthod 2003;1:22-26. Lin J, Liou E, Yeh C. Intrusion of overerupted maxillary molars with miniscrew anchorage. J Clin Orthod 2006;XL:378-383. McNamara JA Jr, Brudon WL.Orthodontics and Dentofacial Orthopedics.Ann Arbor, Needham Press, 2001. Park H. A miniscrew-assisted transpalatal arch for use in lingual orthodontics. J
Clin Orthod 2006;XL:12-16. 17 Park YC. Use of intrusion auxiliaries on the maxilla and extrusion auxiliaries on the mandible to rectify occlusal plane canting and consequent correction of facial asymmetry. Korea Association of Orthodontics Meeting, November 2-3, 2005. Seoul, Korea. Personal communication. Ricketts RM, Grummons D. Frontal cephalometrics: Practical applications, Part 1. World J Orthod 2004;4:297-316. Roberts WE. Orthodontic anchorage with osseointegrated implants: Bone physiology, metabolism, and biomechanics. In: Higuchi KW, ed, Othodontic Application of Osseointegrated Implants. Illinois, Quintessence 2000:161-190. Sugawara J, Baik UB. Treatment and post-treatment dental alveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system (SAS) for open bite correction. Int J Adult Orthodont Orthognath Surg 2002;17:243-253. Youn S. Midline correction with miniscrew anchorage and lingual appliance. J Clin Orthod 2006;40:314-322.
Anda mungkin juga menyukai
- The Physician AssistantDokumen12 halamanThe Physician AssistantThe Physician Assistant LifeBelum ada peringkat
- Drug Discovery Complete NotesDokumen5 halamanDrug Discovery Complete NotesSadiqa ForensicBelum ada peringkat
- Grand Case Presentation GuidelinesDokumen10 halamanGrand Case Presentation Guidelinesscribd_lostandfoundBelum ada peringkat
- Pre Transfusion TestingDokumen57 halamanPre Transfusion TestingDominic Bernardo100% (4)
- Tablanza-Finals Activity 1 (Lab)Dokumen3 halamanTablanza-Finals Activity 1 (Lab)trust nobodyBelum ada peringkat
- Orientation For New ProctorsDokumen104 halamanOrientation For New ProctorsGessle GamirBelum ada peringkat
- A Countdown To Orthognathic SurgeryDokumen5 halamanA Countdown To Orthognathic SurgeryhaneefmdfBelum ada peringkat
- Nursing Leadership and Management Practice TestDokumen1 halamanNursing Leadership and Management Practice TestMikhaela GonzalesBelum ada peringkat
- Shoulder Guidelines AdhesiveCapsulitis JOSPT May 2013 PDFDokumen31 halamanShoulder Guidelines AdhesiveCapsulitis JOSPT May 2013 PDFRulyBelum ada peringkat
- Orthognathic Surgery & Lefort 1 OsteotomiesDokumen71 halamanOrthognathic Surgery & Lefort 1 OsteotomiesNikhilAsokBelum ada peringkat
- A Method of Cephalometric Evaluation Mcnamara 1984Dokumen21 halamanA Method of Cephalometric Evaluation Mcnamara 1984Gaurav Pratap SinghBelum ada peringkat
- Impact of Molar Teeth Distalization With Clear Aligners On Occlusal Vertical Dimension: A Retrospective StudyDokumen5 halamanImpact of Molar Teeth Distalization With Clear Aligners On Occlusal Vertical Dimension: A Retrospective StudykarlaBelum ada peringkat
- Effects of Surgically Assisted Rapid Maxillary Expansion On Mandibular Position - A Three - Dimensional StudyDokumen7 halamanEffects of Surgically Assisted Rapid Maxillary Expansion On Mandibular Position - A Three - Dimensional StudyDaniel Carvalho de AraújoBelum ada peringkat
- Posterior Crossbite With Mandibular Asymmetry Treated With Lingual Appliances, Maxillary Skeletal Expanders, and Alveolar Bone MiniscrewsDokumen21 halamanPosterior Crossbite With Mandibular Asymmetry Treated With Lingual Appliances, Maxillary Skeletal Expanders, and Alveolar Bone MiniscrewsJuliana ÁlvarezBelum ada peringkat
- ALTRAMECARTICULODokumen12 halamanALTRAMECARTICULOAlejandra NietoBelum ada peringkat
- Kim 2023Dokumen11 halamanKim 2023Dela MedinaBelum ada peringkat
- Lip Line Changes in Class III Facial Asymmetry Patients After Orthodontic Camouflage Treatment, One-Jaw Surgery, and Two-Jaw Surgery, Lee 2017Dokumen7 halamanLip Line Changes in Class III Facial Asymmetry Patients After Orthodontic Camouflage Treatment, One-Jaw Surgery, and Two-Jaw Surgery, Lee 2017GeromelBelum ada peringkat
- Dentofacial Changes From Fan-Type Rapid Maxillary Expansion Vs Traditional Rapid Maxillary Expansion in Early Mixed Dentition A Prospective Clinical TrialDokumen9 halamanDentofacial Changes From Fan-Type Rapid Maxillary Expansion Vs Traditional Rapid Maxillary Expansion in Early Mixed Dentition A Prospective Clinical TrialMirza GlusacBelum ada peringkat
- CJN 079Dokumen199 halamanCJN 079SelvaArockiamBelum ada peringkat
- Treatment With Facemask and Removable Upper Appliance Versus Modified Tandem Traction Bow Appliance: The Effects On Mandibular SpaceDokumen6 halamanTreatment With Facemask and Removable Upper Appliance Versus Modified Tandem Traction Bow Appliance: The Effects On Mandibular SpacehelmysiswantoBelum ada peringkat
- Herbst Vs SGTBDokumen8 halamanHerbst Vs SGTBdessy SijabatBelum ada peringkat
- Ortho AlignerDokumen7 halamanOrtho AlignerJuancamilo CamposBelum ada peringkat
- Comparison of Two Protocols For Maxillary Protraction: Bone Anchors Versus Face Mask With Rapid Maxillary ExpansionDokumen8 halamanComparison of Two Protocols For Maxillary Protraction: Bone Anchors Versus Face Mask With Rapid Maxillary ExpansionBeatriz ChilenoBelum ada peringkat
- Tratamento Classe III Com Mini-ImplantesDokumen8 halamanTratamento Classe III Com Mini-ImplantesamcsilvaBelum ada peringkat
- Gorucu Coskuner2017Dokumen8 halamanGorucu Coskuner2017MairenBelum ada peringkat
- Articulo 10Dokumen10 halamanArticulo 10Daniela NarváezBelum ada peringkat
- Nonextraction Treatment of A Skeletal Class III MalocclusionDokumen10 halamanNonextraction Treatment of A Skeletal Class III MalocclusionKanchit SuwanswadBelum ada peringkat
- Use of Palatal Miniscrew Anchorage and Lingual Multi-Bracket Appliances To Enhance Efficiency of Molar Scissors-Bite CorrectionDokumen8 halamanUse of Palatal Miniscrew Anchorage and Lingual Multi-Bracket Appliances To Enhance Efficiency of Molar Scissors-Bite CorrectionTriyunda PermatasariBelum ada peringkat
- Reconstruccion Mandibular Abordaje Intraoral IbrahimDokumen13 halamanReconstruccion Mandibular Abordaje Intraoral IbrahimMarcela GBelum ada peringkat
- Surgically Assisted Rapid Maxillary Expansion Compared With Orthopedic Rapid Maxillary ExpansionDokumen7 halamanSurgically Assisted Rapid Maxillary Expansion Compared With Orthopedic Rapid Maxillary ExpansionmanalrawhiBelum ada peringkat
- Effects of Case Western Reserve University's Transverse Analysis On The Quality of Orthodontic TreatmentDokumen15 halamanEffects of Case Western Reserve University's Transverse Analysis On The Quality of Orthodontic TreatmentIsmaelLouGomezBelum ada peringkat
- A Comparison Between Arbitrary and KinematicDokumen4 halamanA Comparison Between Arbitrary and KinematicsmritinarayanBelum ada peringkat
- Effects of Rapid Maxillary Expansion On Upper Airway Volume: A Three-Dimensional Cone-Beam Computed Tomography StudyDokumen7 halamanEffects of Rapid Maxillary Expansion On Upper Airway Volume: A Three-Dimensional Cone-Beam Computed Tomography StudyVishal SharmaBelum ada peringkat
- Mohler and Tennison RandallDokumen10 halamanMohler and Tennison RandallShaly MaduroBelum ada peringkat
- Cambios Tranvversales, Verticales Anclaje Oseo VS DentosoportadoDokumen12 halamanCambios Tranvversales, Verticales Anclaje Oseo VS DentosoportadoLAURA MARCELA BARRENECHE CALLEBelum ada peringkat
- Factors Related To Microimplant Assisted Rapid PalDokumen8 halamanFactors Related To Microimplant Assisted Rapid PalFernando Espada SalgadoBelum ada peringkat
- Effects of Maxillary Protraction and Fixed Appliance Therapy On The Pharyngeal AirwayDokumen8 halamanEffects of Maxillary Protraction and Fixed Appliance Therapy On The Pharyngeal AirwayAkash AmbhoreBelum ada peringkat
- Comparison of Facemask Therapy Effects Using Skeletal and Tooth-Borne AnchorageDokumen8 halamanComparison of Facemask Therapy Effects Using Skeletal and Tooth-Borne AnchorageMariana SantosBelum ada peringkat
- Effects of Facemask Treatment Anchored With Miniplates After Alternate Rapid Maxillary Expansions and Constrictions A Pilot StudyDokumen8 halamanEffects of Facemask Treatment Anchored With Miniplates After Alternate Rapid Maxillary Expansions and Constrictions A Pilot StudyMariana SantosBelum ada peringkat
- Rapid Maxillary Expansion Compared To Surgery For Assistance in Maxillary Face Mask ProtractionDokumen8 halamanRapid Maxillary Expansion Compared To Surgery For Assistance in Maxillary Face Mask ProtractionMariana SantosBelum ada peringkat
- Skeletal Stability After 2-Jaw Surgery Via Surgery-First Approach in Facial Asymmetry Patients Using CBCTDokumen8 halamanSkeletal Stability After 2-Jaw Surgery Via Surgery-First Approach in Facial Asymmetry Patients Using CBCTPhachara SiripraphonrojBelum ada peringkat
- CirugiaDokumen27 halamanCirugiaalexmtzgBelum ada peringkat
- Nonsurgical Correction of A Class III Malocclusion in An Adult by Miniscrew-Assisted Mandibular Dentition DistalizationDokumen11 halamanNonsurgical Correction of A Class III Malocclusion in An Adult by Miniscrew-Assisted Mandibular Dentition DistalizationNeycer Catpo NuncevayBelum ada peringkat
- Angle Orthod. 2015 85 2 284-91Dokumen8 halamanAngle Orthod. 2015 85 2 284-91brookortontiaBelum ada peringkat
- Lin 2021Dokumen14 halamanLin 2021fabian hernandez medinaBelum ada peringkat
- Skeletal Width Changes After Mini-Implant-Assisted Rapid Maxillary Expansion (MARME) in Young AdultsDokumen6 halamanSkeletal Width Changes After Mini-Implant-Assisted Rapid Maxillary Expansion (MARME) in Young AdultsRolando Huaman BravoBelum ada peringkat
- 9 - Skeletal and Dentoalveolar Effects of Miniscrew-Assisted Rapid Palatal Expansion Based On The Length of The MiniscrewDokumen8 halaman9 - Skeletal and Dentoalveolar Effects of Miniscrew-Assisted Rapid Palatal Expansion Based On The Length of The MiniscrewMariana SantosBelum ada peringkat
- EARLY Intervention in The Transverse DimensionDokumen3 halamanEARLY Intervention in The Transverse DimensionBoboc FlorinBelum ada peringkat
- Nonsurgical Miniscrew-Assisted Rapid Maxillary Expansion Results in Acceptable Stability in Young AdultsDokumen8 halamanNonsurgical Miniscrew-Assisted Rapid Maxillary Expansion Results in Acceptable Stability in Young AdultsAkash AmbhoreBelum ada peringkat
- Class III Comparison BAMP and RME - FM CevidantesDokumen8 halamanClass III Comparison BAMP and RME - FM CevidantesMargarida Maria LealBelum ada peringkat
- Mandibular Symphyseal Distraction and Its Geometrical Evaluation: Report of A CaseDokumen7 halamanMandibular Symphyseal Distraction and Its Geometrical Evaluation: Report of A CasesebitadesantaBelum ada peringkat
- Welcome To Journal Club: Finite Element Method: A Research Tool in OrthodonticsDokumen22 halamanWelcome To Journal Club: Finite Element Method: A Research Tool in OrthodonticsReshamIrshadBelum ada peringkat
- Orthognathic Surgery For Patients With Maxillofacial DeformitiesDokumen25 halamanOrthognathic Surgery For Patients With Maxillofacial DeformitiesahmedatefBelum ada peringkat
- Biomechanical Considerations For Total Distalization of The Mandibular Dentition in The Treatment of Class III MalocclusionDokumen9 halamanBiomechanical Considerations For Total Distalization of The Mandibular Dentition in The Treatment of Class III Malocclusion허성수Belum ada peringkat
- Long Term Effects of Lateral Nasal Wall Anchored FDokumen9 halamanLong Term Effects of Lateral Nasal Wall Anchored FRenan VeigaBelum ada peringkat
- Chairside Options For The TreatmentDokumen6 halamanChairside Options For The TreatmentdiliesdiBelum ada peringkat
- Rapid Maxillary Expansion. Is It Better in The Mixed or in The Permanent Dentition?Dokumen8 halamanRapid Maxillary Expansion. Is It Better in The Mixed or in The Permanent Dentition?Gustavo AnteparraBelum ada peringkat
- Alt Ramec - Estructuras DentalesDokumen8 halamanAlt Ramec - Estructuras DentalesAna Clara ClaveroBelum ada peringkat
- Cambio Esqueletal Asociado A Clases LL ArticuloDokumen7 halamanCambio Esqueletal Asociado A Clases LL ArticuloDavid DíazBelum ada peringkat
- Hayrax Con Mascara Facial PDFDokumen8 halamanHayrax Con Mascara Facial PDFSantos LopBelum ada peringkat
- Surgery-First Orthognathic Approach For The Correction of FacialDokumen8 halamanSurgery-First Orthognathic Approach For The Correction of FacialMario CastellanosBelum ada peringkat
- Openbite MIA AJODODokumen10 halamanOpenbite MIA AJODOscribdlptBelum ada peringkat
- HHHVHF PDFDokumen8 halamanHHHVHF PDFruben dario meza bertelBelum ada peringkat
- Nonsurgical Miniscrew-Assisted Rapid Maxillary Expansion Results in Acceptable Stability in Young AdultsDokumen8 halamanNonsurgical Miniscrew-Assisted Rapid Maxillary Expansion Results in Acceptable Stability in Young AdultsRolando Huaman BravoBelum ada peringkat
- Correction of Late Adolescent Skeletal Class III Using The Alt-RAMEC Protocol and Skeletal AnchorageDokumen11 halamanCorrection of Late Adolescent Skeletal Class III Using The Alt-RAMEC Protocol and Skeletal AnchoragePorchiddioBelum ada peringkat
- Kaya 2011Dokumen8 halamanKaya 2011ortodoncia 2022Belum ada peringkat
- Graftless Solutions for the Edentulous PatientDari EverandGraftless Solutions for the Edentulous PatientSaj JivrajBelum ada peringkat
- Nidcap Vol 11 No1-FinalDokumen26 halamanNidcap Vol 11 No1-FinalDaniel MarvasoBelum ada peringkat
- Sindh Institute of Urology and Transplantation (Siut), Karachi BY Muhammad Asim Halim (Irs)Dokumen4 halamanSindh Institute of Urology and Transplantation (Siut), Karachi BY Muhammad Asim Halim (Irs)asimhalimBelum ada peringkat
- Ass AsDokumen1 halamanAss AsMukesh BishtBelum ada peringkat
- Ug Paying First Prenom Nov2Dokumen225 halamanUg Paying First Prenom Nov2bibash adhikariBelum ada peringkat
- NCP Klippel Trenaunay SyndromeDokumen3 halamanNCP Klippel Trenaunay SyndromePaola Marie VenusBelum ada peringkat
- Damilola Olarewaju Lab 4Dokumen5 halamanDamilola Olarewaju Lab 4api-535000853Belum ada peringkat
- Republic of The Philippines Province of Benguet Municipality of La TrinidadDokumen31 halamanRepublic of The Philippines Province of Benguet Municipality of La Trinidadfunky goodBelum ada peringkat
- REFLEXOLOGYDokumen80 halamanREFLEXOLOGYdonald duckBelum ada peringkat
- Group (DSKTJP) Mini Project DPK20073Dokumen11 halamanGroup (DSKTJP) Mini Project DPK20073Keshini RameshBelum ada peringkat
- Amcp Media List 8Dokumen96 halamanAmcp Media List 8api-407904109Belum ada peringkat
- 321Z3D2 0KD8D6L7P001F6G PDFDokumen13 halaman321Z3D2 0KD8D6L7P001F6G PDFNBC MontanaBelum ada peringkat
- Seminars in Pediatric SurgeryDokumen6 halamanSeminars in Pediatric SurgeryDr Venkatachalapathy T S Ped SurgeonBelum ada peringkat
- EARSS 2005 - tcm61-34899Dokumen147 halamanEARSS 2005 - tcm61-34899api-3760696Belum ada peringkat
- Background of The StudyDokumen3 halamanBackground of The StudyTrixie DacanayBelum ada peringkat
- Practice 7-QuestionsDokumen6 halamanPractice 7-QuestionsLatifah AlsahaleyBelum ada peringkat
- SickLeaveCertificate With and Without Diagnosis 20230402 114713Dokumen2 halamanSickLeaveCertificate With and Without Diagnosis 20230402 114713Obadah AbdulsattarBelum ada peringkat
- 2011 Efficacy and Augmentation During 6 Months of Double-Blind Pramipexole For Restless Legs SyndromeDokumen10 halaman2011 Efficacy and Augmentation During 6 Months of Double-Blind Pramipexole For Restless Legs SyndromeAga_tthaBelum ada peringkat
- Chapter 8 Drug Administration Throughout The LifespanDokumen45 halamanChapter 8 Drug Administration Throughout The LifespanDiane VillegasBelum ada peringkat
- 2,4-Toluene Diisocyanate: Hazard SummaryDokumen4 halaman2,4-Toluene Diisocyanate: Hazard SummaryBeverly RamosBelum ada peringkat
- Special Mouth Care: DefinitionDokumen3 halamanSpecial Mouth Care: DefinitionSHELLAH MARIE MAMAWAG100% (1)
- Honoring Those Who Serve: Support For Military & First Responder FamiliesDokumen9 halamanHonoring Those Who Serve: Support For Military & First Responder Familiesapi-559392378Belum ada peringkat
- Sydney Telischak ResumeDokumen2 halamanSydney Telischak Resumeapi-546817891Belum ada peringkat